Abstract
This systematic review was conducted to develop a conceptual framework that addresses various factors associated with return to work among cancer survivors. Databases Medline, EMBASE, ProQuest, PubMed and ScienceDirect were systematically searched using medical subject headings [MeSH] for studies published in English from 1990 to 2013. Studies that described adult cancer patients’ self-reported data or patients’ point of view on factors associated with return to work or employment status following cancer diagnosis were included. Articles selection was conducted in three steps: selection based on title and abstract, retrieval of full text and additions of articles from reference lists and recommendations from experts. Disagreement in data extraction was solved by consultation of third reviewer. Out of twenty seven articles, breast cancer was the most studied type of cancer (30%) while colorectal cancer was studied independently in two articles (7.4%). Conceptual framework on return to work identifies factors under environmental, personal, work demand, work ability, health status and financial factors. Extensive search of scientific databases over last 24 years and the development of the conceptual frame-work are the strength of this review. Conceptual framework reveals the various factors including non-medical factors associated with return to work upon cancer diagnosis. It serves as a reminder to the policy makers to focus on modifiable factors as potential areas for intervention to assist cancer survivors return to work, especially those with little financial assistance and health insurance.
Keywords: Cancer survivorship, Return to work, Employment, Workplace integration
Introduction
Cancer is no longer considered as a disease afflicting the elderly as many of those diagnosed with cancer annually are from the working population (1), due to advancements in cancer screenings, enhanced cancer treatments, the aging trend in the global population and the current trend that most people work longer before retirement (2). Therefore, cancer has been considered as a chronic disease that patients live with and cancer survivors are becoming more common in the workforce (3). As a result, public health research has turned to assessing survivorship issues after cancer treatment with the management of cancer survivorship focusing beyond the usual clinical care model (4).
Cancer survivor refers to any person who has been diagnosed with cancer, starting from the time of diagnosis through the remaining years of life. Cancer survivorship can be categorized into three different phases, i.e. beginning from diagnosis till end of initial treatment; the transition from treatment to extended survival; and long term survival. In reality, the concept of survivorship is often referred to the period upon which active treatment completes. Interestingly, it encompasses a wide range of cancer status, from being cancer-free; living with intermittent periods of active disease requiring treatment; to living with cancer continuously without disease-free period (5).
According to GLOBOCAN 2012, there were 14.1 million new cancer cases, 8.2 million cancer deaths and 32.6 million people living with cancer (within 5 years of diagnosis) in 2012 worldwide. Almost a quarter of the cancer survivors (24%) are within the working age group, below 60 years old (6, 7) though the actual prevalence of cancer among working population is unknown and the true extend of the work related issues could not be assessed (8).
Following cancer, many patients experienced change of employment status, prolonged sick leave, unemployment, and work cessation due to various factors (9). Work participation in a society can define an individual’s self-worth, identity and societal role, besides contributing to financial security (10). The experience of being diagnosed with cancer could potentially become a source of distress in addition to the disruption in the work role and expensive medical bills. All these factors affect the health-related quality of life (HRQoL). Returning to work after cancer treatment is important for cancer survivors in maintaining a sense of normalcy, improves quality of life (QoL) and control, while failure to stay in employment could deprive an individual of social contact and well-being (11, 12).
Approximately two-thirds of cancer survivors had returned to work, suggesting that many cancer survivors can resume work successfully (8, 13). However, there is no systematic review done on the relationship among the various factors associated with return to work or remain in employment (8, 14). The International Classification of Functioning, Disability and Health (ICF) (15) is a universal classification that focuses on the ‘components of health’ concerning all individuals, though it has been primarily focused on impairment element of disabilities. Under this classification, all aspects of health are described in terms of health domains and health-related domains (Fig. 1) (16).
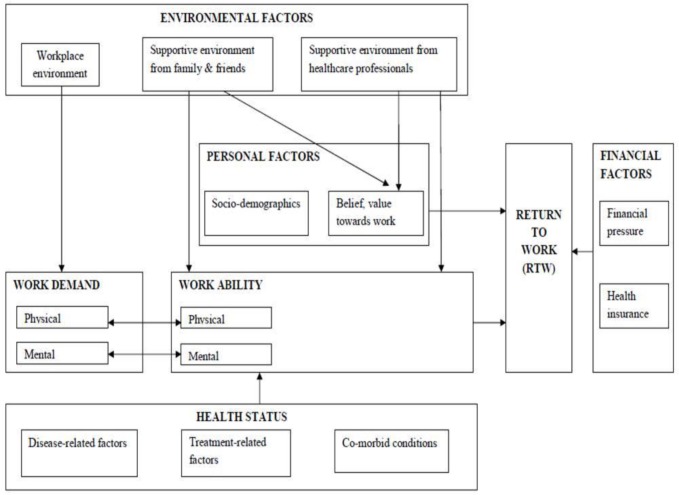
Fig. 1.
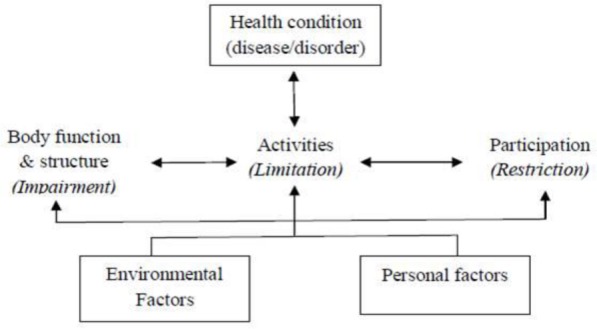
Interactions between the components of ICF
This study aimed to examine these domains and explored the relationship between other relevant factors that were not mentioned in this ICF model. A new conceptual framework is developed from patients’ point of views which would further assist policy makers in reviewing the current healthcare delivery system and introducing intervention that addresses the issues pertaining to return to work among the employees.
Methods
A review protocol that takes into account of the search strategy, studies selection and data extraction is drafted. The Preferred Reporting Items for Systematic Reviews (PRISMA statement) have been referred as formal guidelines for systematic review.
Search strategy
Electronic databases were searched using Medline, EMBASE, ProQuest, PubMed and ScienceDirect with restriction on articles in English, published in 1990-2013. The following main medical subject headings [MeSH] were used for the search: “cancer survivors” AND “return to work”. These medical subject headings were then completed with other medical subject headings, text words which are synonyms for “cancer” and “return to work”.
Occupational cancers and childhood cancers are both excluded as these cancers have different concerns pertaining to return to work. Occupational cancer may warrant employees to work at different workplace in order to avoid the occupational hazards, if returning to workplace ever takes place. Besides that, occupational cancer takes years and decades to develop upon exposing to workplace carcinogens. As a result, employees may be diagnosed with occupational cancer at or after retirement age. Hence, issue of returning to work is of no significance to them. As for individual with history of childhood cancers, getting employed during adulthood is not a major issue.
To exclude irrelevant articles on occupational cancer, occupational diseases, childhood cancer, screening for cancer, intervention, treatment and prevention, the search was refined by introducing medical subject headings as “NOT-terms”.
Selection of articles
Article selection was conducted in three steps. All searches were carried out by one reviewer (Chow SL) and reviewed by another (Su TT). EndNote X7 software was used for screening of duplicate studies. First, articles were independently selected by two reviewers (Chow SL and Su TT) based on the title and abstract after excluding the duplicate articles. It was followed by the retrieval of full text which met the inclusion criteria. Finally, the references of the selected articles and review papers were searched for additional references along with consultation with experts. Authors of selected articles were contacted to identify additional studies on the topic. Then, reviewers met to discuss the selected studies.
The following inclusion criteria were applied for selecting the full text articles.
-
i)
Types of Participants
Adults (18 years and above) of both genders who were diagnosed with cancer of any types, except occupational and childhood cancer.
-
ii)
Types of Studies
Both qualitative and quantitative studies which consist of cancer patients’ self-reported data or patients’ point of view on factors associated with return to work or employment.
-
iii)
Year of publication
Full articles that were published in journals for the past 24 years (1990-2013).
Data extraction
Using a pre-designed data extraction form, the data were extracted by one reviewer (Chow SL) and checked by another (Su TT). Disagreement in data extraction was solved by consultation of the third reviewer (Su AT).
Criteria for quality appraisal
Quality appraisal tools are usually based on individual aspects or components of study design, conduct and analysis for which there is theoretical evidence of bias. Different quality assessment tools with quality ratings were used based on the type of study design.
Randomisation technique, double blind and description of withdrawals, and drop outs are the important aspects in randomised trail study (17). For observational studies, selection, comparability and the outcome were assessed using Newcastle Ottawa Scale, NOS (18). Appropriate research design, appropriate recruitment strategy, response rate reported, sample representative of similar population, objective and reliable measurements used, power calculation and appropriate statistical analysis were looked into when evaluating the quality of cross-sectional studies. National CASP Appraisal Tool was used as assessment tool for qualitative study which examined rigour, credibility and relevance (19).
The quality assessment was carried out independently by two reviewers (Chow SL and Su TT) and consultation of third author (Su AT) in the event of disagreement.
Results
Literature search yielded a total of 1836 articles and after excluding for duplications, 1668 articles were identified. A total of 1615 articles were excluded based on title and abstract. Of the 53 remaining articles, 20 articles were included after reading the full text. Articles that focused only on QoL and physical disability following cancer were excluded. Nine additional articles were identified through the references of the selected articles and the review papers. A total of 27 articles were included in this review.
Study and patient characteristics
Table 1 summarises the patient characteristics of the 27 selected articles. Eighteen articles (66.7%) were published in the last 5 years. Nine articles (33.3%) were cross sectional study, one randomised trial (3.7%), nine longitudinal studies (33.3%) and eight qualitative studies (30%). Six articles (22.2%) recruited participants from cancer registries compared to cancer support group (11.1%). Two articles (7.4%) focused only on male patients with cancer of stomach, liver and colorectal, while nine articles (33.3%) focused only on female patients, among which eight articles (30%) exclusively studied breast cancer. Breast cancer alone was the most studied type of cancer (30%), colorectal cancer (7.4%), and cancer of various types (55.5%).
Table 1.
Summary of included studies and participants’ characteristics
| Reference | Country | Study Design | Number of Subjects (n) | Age of subjects (years) | Cancer Type |
|---|---|---|---|---|---|
| (35) | USA | Cross sectional Using questionnaire (person, disease and work related factors) | n=250 Men: 46.5% Women: 53.5% | 30-59 | Colorectal |
| (29) | Korea | Cross sectional with reference group Using questionnaire (employment status, demographic data and clinical variables) | n=1594 Women |
20-60 | Breast |
| (34) | UK | Cross sectional Using Brief Illness Perceptions Questionnaire (perceived impact of cancer and its treatment on work) | n=194 Men (40%) Women (60%) |
51 | Breast Urological Gynaecological Head and Neck |
| (25) | France | Cross sectional Using questionnaire (on personal, disease-related and occupational characteristics) | n=379 Women | 18-60 | Breast |
| (26) | USA | Longitudinal Using telephone interview (12 and 18 months post diagnosis) | n=416 Women |
30-64 | Breast |
| (20) | Korea | Longitudinal Prospective Cohort Using employment questionnaire (every 3 months for 24 months) | n=305 Men | ≥18 | Stomach (32%) Liver (38%) Colorectal (30%) |
| (9) | Australia | Population-based longitudinal Using telephone survey | n= 975 Men: 64% Women: 36% | 20-80 | Colorectal |
| (39) | Netherlands | Longitudinal Follow up | n=195 Men:40% Women:60% | 18-58 | Breast (26%) Haematological (12%) Gastrointestinal (12%) Female genitals (22%) Genitourinary (22%) Others (6%) |
| (30) | Canada | Longitudinal Telephone interview (4 and 15 months after diagnosis) | n: 2422 Men: 53% Women: 47% | ≥21 | Lung (34%) Colorectal (66%) (Non-metastatic) |
| (21) | Sweden | Randomised trial (Follow up for 24 months) | n=222 Women |
29-54 | Breast |
| (31) | Sweden | Qualitative: In-depth interview, Retrospective narration |
n=16 -recurrent-free women -50% women RTW -50% women not yet RTW |
44- 58 | Breast |
| (23) | UK | Qualitative: Individual interview (n=19) Focus group (n=4, n=6) | n=29 Women:93% Men: 7% | 52.6 N |
Breast (83%), on-Hodgkin’s lymphoma (7%), Uterus (7%) Larynx (3%) |
| (12) | USA | Qualitative: Focus group | n=7 women | 18-55 | Breast (57%) Lung (14%) Acute Myeloid Leukemia (14%) Ovarian cancer (14%) |
| (24) | USA | Qualitative, Face to face structured interview | n=28 Men: 50%; Women:50% |
24-63 | Gastrointestinal (17.9%) Brain (10.7%) Leukemia/ Lymphoma (10.7%) Lung (10.7%) Thyroid (10.7%) Breast (7.1%) Urinary tract (bladder) (7.1%) Male genital tract (7.1%) Skin (7.1%) Head and neck (7.1%) Female genital tract (3.6%) |
| (38) | UK | Qualitative, Telephone interview | n=26 Men:38% Women:62% | 31-61 | Breast (35%) Prostate (15%) Lymphoma (12%) Ovaries (12%) Oesophageal (4%) Renal (4%) Bladder (4%) Brain tumour (4%) Colon (4%) Thyroid (4%) Pancreatic (4%) |
| (28) | Netherlands | Longitudinal study (sickness absence and full RTW after 2yrs post diagnosis) | n=5074 Men: 35.5% Women: 64.5% | 18-60 | Breast (31.1%) Female genitals (16.9%) Gastro-intestinal (14.2%) Lung (8.8%) Male genitals (8%) Skin (6%) Blood (5.8%) Other (9.12%) |
| (37) | Netherlands | Longitudinal study | n=5234 Men: 36% Women: 64% | 18-60 | Breast (31.1%) Female genitals (16.9%) Gastro-intestinal (14.2%) Lung (8.8%) Male genitals (8%) Skin (6%) Blood (5.8%) Other (9.12%) |
| (36) | Sweden | Qualitative Focus group (x4) | n=23 Women |
20-63 | Breast |
| (33) | Belgium | Qualitative In-depth interview | n=22 Women | 42-55 | Breast |
| (32) | UK | Qualitative Semi-structured interview | n=50 Men | 18-65 | Prostate |
| (17) | Germany | Longitudinal Follow up at end of rehabilitation, t1(3weeks) and t2(12 months after rehabilitation) | n=750 Men:14.3% Women: 85.7% | 18-60 | Breast (59.5%) Gynaecological (14.5%) Head and neck cancer (8.9%) Skin (6.1%) Colorectal (5.6%) Lung (3.1%) Haematological (2.3%) |
| (27) | Denmark | Cross-sectional | n=1490 Men: 36% Women: 64% |
18-80 | Breast (37%) Gastro (8%) Lung (3%) Gynaec (12%) Prostate (3%) Urinary (2%) Head and neck (4%) Lymphoma (12%) Leukaemia (6%) Other (15%) |
| (49) | USA | Cross-sectional with reference group | Cancer survivors, n=100 Non cancer, n=103 |
45 | Breast |
| (50) | Finland | Cross-sectional with reference group | Cancer survivors, n=591 Women:74% Men:26% |
25-57 | Women Breast cancer (90%) Lymphoma (10%) Men Lymphoma (41%) Prostate (30%) Testicular (29%) |
| (51) | Korea | Cross-sectional with reference group | Cancer survivors n=408 General population n=994 |
18-65 | Stomach cancer |
| (22) | USA | Population-based longitudinal | Cancer survivors n=4991 General population n=1334 |
25-55 | Oral (2.1%) Stomach (26.3%) Colorectal (11.7%) Liver (16.3%) Pancreas (2.3%) Lung (8.4%) Breast (8.3%) Cervix and uterus (3.7%) Kidney (3.3%) Bladder (2.4%) Brain & CNS (3.1%) Thyroid (7.0%) Non Hodgkin’s (2.3%) Leukemia (2.7%) |
| (52) | USA | Cross-sectional with reference | Cancer survivors n=7531 Men: 47% Women: 53% | 55-64 | Mixed |
Quality assessment of selected articles
Common methodological weaknesses observed were no mention of power and sample size calculation, unjustified recruitment strategy and choice of location as well the issue of transferability of the research findings. Only a few studies included the population-based follow up with a group of cancer patients and controlled potential confounders (9, 20). A lack of common standardized measures has been reported in assessing work ability and employment outcomes in various studies.
Only one study addressed the selection bias by means of randomisation (21) and two studies were carried out in a population-based setting (9, 22).
Reference groups of non-cancer individuals were also compared to the cancer group in cross-sectional studies (22).
Potential bias involved in qualitative research was recall bias among the interviewees. To improve the validity of the findings, authors independently coded the interview transcript and followed by in-depth analysis across the transcripts. Finally, discussion was carried out on notations and interpretations of the findings to finalise the themes (12, 23, 24).
Identified components of conceptual model under five categories I) Personal factors Personal socio-demographic
Elderly cancer patients had more difficulties in coping with work, emotional distress and continuing hospital appointments. Return to work rate was reported lower among older breast cancer women throughout the period of follow-up (25, 26). A study looking at various types of cancer agreed that older patients were at higher risk of losing employment, resulting in economic consequences on the individual and societal level (27). Similarly, cancer survivors were more likely to lose their jobs after cancer diagnosis and were less likely to be re-employed than the general population. However, there was no association of age and gender to full return to work, except for blood malignancy and genital cancer (28).
Educational level and household income consistently determined the employment outcome of cancer patients after cancer treatment (29). Higher educational level correlated with higher return to work rate (25, 20) while less educated and lower income patients were particularly at risk of departing from workforce (29, 30). Mehnert and Koch (2013), attributed the favourable working condition to higher educated and higher social class people who work in better working environments, earn and lead a better living condition. Hence, they achieved higher rate of return to work and absence of sick leave.
Higher employment rate correlated with single women and women who were separated, divorced or widowed (29).
Similarly, those who were married were more likely to leave the workforce as compared to those unmarried (30).
Personal belief and value towards work
Personal belief and value towards work were crucial determinants in the decision to return to work. For those cancer survivors who return to work, they perceived the value of having a job, part of their identity (12, 31, 32) besides serving as a healthy distraction from their illness or treatment to regain a sense of normality (23, 24, 32, 33) as an essential part of the healing process (12).
The cancer journey has changed the survivors’ perception of work, helped them to re-examine their priorities and rethink the meaning of work and life. Some chose to lower their professional ambitions and devote more time to their family, friends and to themselves. Many cancer survivors reported that they chose not to allow themselves to get stressed at the workplace (12, 23, 32, 33). However, continuing employment was often necessary for financial reasons despite the altered attitude and perceptions, which might be indicative of changes in outlook and priorities as a whole.
II) Health status Treatment-related factors
Except the study by Bouknight (2006), all studies reported negative effects of chemotherapy on return to work. The duration required by survivors to return to work was significantly influenced by chemo-therapy. Survivors who received chemotherapy were three times more likely to delay their return to work due to fatigue, continuing hospital appointments and lack of understanding from colleagues (34). Chemotherapy was also reported to limit the return to work among breast cancer survivors(25), impaired work ability and was associated with work cessation among women colorectal cancer survivors (9). Cognitive dysfunction as a result of long term effects of chemotherapy besides fatigue, distress and depression had been associated with delay in full return to mentally demanding job (28).
Mastectomy was associated with unemployment among breast cancer survivors, while surgery for breast cancer may cause arm morbidity and delayed work resumption (21, 25). Post-surgery side-effects like urinary incontinence was the main concern, affecting prostate cancer patients’ daily life, decision to resume work and also perception of masculinity (32).
Radiotherapy to regional lymph nodes was found to increase arm morbidity and thus limit the return to work (25) as compared to radiotherapy only on the breast parenchyma (21). Radiation therapy in men with colorectal cancer was found to be strongly associated with work cessation (9).
Disease-related factors
Advanced stage of cancer had unfavourable employment outcome (17, 26, 29) and was negatively associated with employment status among cancer patients of stomach, liver and colorectal (20).
Breast cancer survivors were more likely to perceive difficulties at work performance (34) while among breast cancer patients; those with smaller tumour size had better chance of early return to work (21). Higher risk of departing the workforce was seen in lung cancer and head and neck cancer (17, 27, 30) with exception of thyroid cancer. Testicular cancer and skin cancer had the best return to work prognosis up to 88% and 87% respectively, given the excellent survival rate (28).
Co-morbid conditions
Health status was much affected by the number of co-morbid diseases and the effect of the cancer along with its treatment. Cancer survivors who had other medical problems most often reported impaired work ability. The decisions about return to work were greatly affected by health status and symptoms burden. As a result of the difficulty coping with physical symptoms, some chose early retirement (23, 24).
Poor health status was negatively associated with return to work. Breast cancer patients with co-morbid diseases were more likely associated with unemployment (29). Fatigue symptoms were more likely to delay return to work among colorectal cancer patients (35) and delayed return to work among breast cancer survivors (21). Frequent time off from work required for minor illnesses as a result of increased susceptibility to infections were disruptive and made transition back to workplace a real challenge (23).
III) Financial factors Financial pressure
Financial pressure, the fear of being sacked, and being too old for new job, were primary reasons to return to work (23, 24, 32). Some cancer survivors despite having received temporary disability pensions still hoped to remain in the labour market due to their perception that it was difficult for them to get employed again (31, 33).
Health insurance
The interaction of cancer survivorship with health insurance was significant in predicting labour force exits, job changes and transitions to part-time employment for both genders. Tunceli K (2009) found that job-related health insurance represents an additional economical and psychological burden on survivors. Maintaining health insurance coverage upon cancer diagnosis was a challenge to most cancer survivors. Economic or health insurance factors were the prime reasons for returning to work (12, 24). Many cancer survivors also understood that it was not easy to get insured again upon cancer diagnosis, thus the pressure to secure the current health insurance influenced their decision to continue working (24). Such pressure was more intense when the cancer survivors were the breadwinners in the family and the only source for health insurance for the family (12). In countries where the healthcare system was publicly financed, employees do not depend on employer to pay for health insurance to get treatment (27).
Having no private health insurance was a factor predicting work cessation for both genders with colorectal cancer. However, some senior cancer survivors could still benefit from public insurance or insurance through family members, thus making them more likely to leave work (30). Married women of lower incomes had more flexibility to leave the workplace, because the spouse was the primary source of health insurance or income in the family (30).
IV) Environmental factors Supportive environment from family and friends
Moral support from family and friends at the end of the treatment was a crucial factor related to returning to work (24, 25). Patients were encouraged to return to work for various reasons, such as, part of the healing process, being productive in life again and be social with friends again. By disclosing their cancer diagnosis, cancer patients received advice and support from friends, especially those who had undergone a similar experience. Many reported that such interaction to be supportive and informative and were therefore positive about their decision to disclose their own diagnosis (32).
Workplace environment
Work-related factors were studied under different themes, i.e. types of occupations, physically demanding jobs, duration of working hours, work-place support from employer and colleagues. Work that involved heavy lifting was associated with a lower likelihood of returning to work (26), and the workers were at risk of losing job after diagnosis (20). Hence, some cancer survivors were unable to perform to the same extent as previously, and thus, have not yet returned to work after 2 years (21).
Organizational constraints, rather than the physical constraints, contributed to the delayed return to the work-place (25). Support from the workplace was of great importance for successful return to work (12, 17, 23, 24, 31, 36). Vocational rehabilitation initiated by employer (24), frequent contact from employer during sick leave (23), work accommodation and adjustments offered by employer based on flexibility, gradual assimilation and changes in work tasks (12, 17, 23, 24, 36) were helpful for cancer survivors returning to the work-force.
Weak support from colleagues coupled with hostile working environment, changes in work situation and difficulties with employer or colleagues did not favour early return to work (31), while strong co-workers support could compensate for an employer’s inadequate response to transition back to work and better equip employees to handle their situation (12, 36). The sense of responsibility to work, especially in smaller workplace was a prominent factor in deciding to return to work (23, 33).
Skilled employees of larger companies resumed working earlier than those unskilled workers in smaller companies given the provision of return to work policy in the large company. Furthermore, it is easier for large companies to accommodate work tasks and working hours to the work ability and vulnerability of cancer survivors. Employees of public sector (regardless of occupation) and senior employees were more likely to fully return to work later than those from private sectors and junior employees (37).
Supportive environment from healthcare professionals
Healthcare providers played a critical role in the employees’ positive evaluation of their recovery process and offered encouragement to return to work among survivors (12). Many employees acknowledged that they did not receive much guidance and advice on work issues and rehabilitation from healthcare professionals (36) while some reported they had different view on work issues from the physicians. Thus, doctors allowed the patients to decide for themselves whether to return to work (23, 24).
Provision of evening treatment sessions by healthcare personnel helped in reducing sickness absence from work (36). Communication and support between and from occupational health doctors, line managers and colleagues focused on cancer patients’ decision to return to work strengthened the relationship and confidence in the line managers and occupational health doctors. Such communication facilitated the provision of helpful guidance and advice from occupational health doctors upon return to work (38).
V) Work ability Vs. work demand
The work ability of the patients must match with the work demand in order to delay loss of employment. Impaired work ability as a result of chemotherapy or presence of co-morbid conditions did not favour employment outcome.
Survivors working in stressful jobs reported more difficulties when returning to work (23, 33). Many survivors were concerned about work capability and performance following treatment and period of being away from work (32, 33). Gender, treatment-related factors and disease-related factors determine work ability score. Men scored higher than women on work ability until 1 year after first day of sick leave while haematological cancer patients had lower scores. Individuals who underwent chemotherapy consistently showed lower work ability scores (39).
Work ability scores among cancer patients improved significantly over the time. The score at sixth monthafter diagnosis predictedstrongly the likelihood of return to work independent of age and clinical factors (39).
Discussion
Work reintegration upon cancer treatment is an important milestone and determinant of QoL which affects an individual’s physical health, psychological state, level of independence, social relationships, personal beliefs and their relationship to salient features of their environment in a complex manner (40). It has intangible components such as overall well-being and happiness, being employed is no doubt part of it (41).
Selected articles were characterized by a high degree of heterogeneity in terms of patients’ characteristics, cancer sites and mode of treatment, the return to work rate varied from 45% to 89% with average 2 years after diagnosis. Despite the advanced medical treatments, a proportion of cancer survivors ended up unemployed, retired early or changed jobs more often than those without cancer, instead of returning to their work (42–44). The reasons for not returning to work were not medically related, i.e. issues on health insurance, lack of understanding from colleagues at workplace, and the physical nature of their work were among other problems which led to survivors leaving the job (45). The loss of income as a result of unemployment could lead to a decline in standard of living of the individual or entire household, affecting both the physical and mental health of unemployed workers (46). Being unemployed not only results in a drop in status among friends, family and the society, it could potentially lead to a loss of self-esteem (46, 47).
Most of the existing studies examined the factors in relation to return to work under personal factors, disease-related factors and work-related factors (8, 48), while this review aimed at identifying various factors beyond these three themes in the span of 24 years. To our best knowledge, this is the first systematic review that examined qualitative and quantitative studies, given that qualitative studies could offer valuable insight into areas not covered in quantitative research: support from friends and family (24, 32), priority and perception towards work (12, 23, 31), advice from healthcare professionals (12, 23, 36, 38) and self-perceived work ability (23, 33).
ICF model by WHO describes work as a role which one can participate in the society which emphasises on health condition, environmental factors and personal factors in relation to work participation. From this review, it has been shown that the decision to return to work was based on more than these three factors, and more importantly, some of the factors were not medically-related and not easily modifiable (Fig.2).
Fig. 2.
Conceptual framework on return to work among cancer survivors
The new conceptual framework describes the return to work among cancer survivors under five different categories: environmental factors, personal factors, work demand-work ability, health status, and financial factors.
The environmental factors are one of the modifiable factors that should be targeted via various work accommodations and job rotations in order to reduce the work demand required physically and mentally. The likelihood of successful return to work is high when the work demand can be matched with the physical and mental work ability of the survivors.
Cancer survivors’ belief and value towards work has also been identified as an important factor to consider before deciding to resume work duty, which can be influenced by external environment. Thus, this conceptual framework serves as a reminder to policy makers the need to involve the healthcare professionals and family in advocating the return to work programme for survivors. Cancer survivorship is a new milestone and return to work during survivorship is possible if the healthcare professionals consider discussing work related issues during the clinic follow-up and encourage survivors to resume work after treatment. Family, friends and society at large can be facilitators for cancer survivors in re-joining workforce if only they are aware of the benefits of work to survivors as part of recovery and dismiss the myths attached to working after cancer.
The physical and mental work ability of cancer survivors can determine the outcome of survivors’ employment status. With the advanced and new cancer treatment modalities coupled with vocational rehabilitations, more and more cancer survivors can expect good QoL after cancer. Hence, resuming work after treatment is possible if the health and status of well-being of the survivors are all being managed holistically.
Intervention should focus on individuals with cancer from low socio-demographic with little financial support and health insurance. These groups of individuals need more attention and assistance in keeping their employment status.
Recommendations
Future research on cancer should begin with qualitative studies, exploring the work-related issues prior to, during and after return to work. Similarly, the perceptions from those who are involved in treating and managing cancer patients should be sought in designing the intervention to facilitate return to work among cancer survivors.
It is recommended that Cancer Registries to record patients’ employment status before and after cancer. Job task should be described beyond the scope of manual and sedentary work, or blue and white collar working classes. With this information, intervention may focus and plan to achieve the tasks that patients are expected to perform upon their return to work.
Classification like the International Standard Classification of Occupations (ISCO) by International Labour Organisation (ILO) should be used to categorise the patients’ occupations in all cancer registries to facilitate the estimation of prevalence of cancer in the respective working population and comparethe prevalence of cancer among employees between countries.
Outcome measures for employment status can be examined beyond the return to work rate such as changed of job or task, early retirement, unemployment and reemployment. Standardised outcome measures on the impact of cancer and assessment tool like work ability index allow reliable and valid assessment, thus improving the comparability of the findings.
Conclusion
The conceptual framework highlights the groups of survivors who should not be neglected in return to work intervention. At the same time, it also exposes the potential areas of intervention at various modifiable factors like environmental factors, survivors’ perceptions towards work, work demand, work ability and the health status. Intervention should focus on modifiable factors like improving health status through healthy lifestyle, promoting work ability through work-directed rehabilitation, enhancing the involvement of employer and healthcare professionals, and creating a supportive working environment.
Ultimately, these interventions could lead to a better QoL and function, improve the return to work, reduce the unemployment due to cancer and better employment outcome for cancer survivors.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgements
The authors declare that there is no conflict of interests.
References
- de Boer AG, Taskila T, Ojajärvi A, van Dijk FJ, Verbeek JH (2009). Cancer survivors and unemployment: a meta analysis and meta-regression. JAMA, 301(7): 753–762. [DOI] [PubMed] [Google Scholar]
- Crepaldi C, Barbera M, Ravelli F (2008). Cancer and in general long term illnesses at the work-place. Policy Department Economic and Scientific Policy. IP/A/EMPL/FWC/2006–05/SC3. [Google Scholar]
- Tamminga SJ, de Boer AG, Verbeek JH, Frings-Dresen MH (2010). Return-to-work interventions integrated into cancer care: A systematic review. Occup Environ Med, 67(9): 639–648. [DOI] [PubMed] [Google Scholar]
- Feuerstein M (2007). Handbook of Cancer Survivorship. Springer, pp.: 3–6. [Google Scholar]
- Mullan F (1985). Seasons of survival: reflections of a physician with cancer. NEJM, 313(4): 270–273. [DOI] [PubMed] [Google Scholar]
- American Cancer Society (2000). Cancer Facts & Figures, 2000. Atlanta: American Cancer Society. [Google Scholar]
- American Cancer Society (2012). Cancer Treatment and Survivorship Facts & Figures 2012–2013. Atlanta: American Cancer Society. [Google Scholar]
- Spelten ER, Sprangers MAG, Verbeek JHAM (2002). Factors reported to influence the return to work of cancer survivors: a literature review. Psycho-Oncol, 11(2): 124–131. [DOI] [PubMed] [Google Scholar]
- Gordon L, Lynch BM, Newman B (2008). Transitions in work participation after a diagnosis of colorectal cancer. Aust NZ J Pub Health, 32(6): 569–574. [DOI] [PubMed] [Google Scholar]
- Ferrell BR, Grant MM, Funk B, Otis-Green S, Garcia N (1997). Quality of life in breast cancer survivors as identified by focus groups. Psycho-Oncol, 6: 13–23. doi: 10.1002/(SICI)1099-1611. [DOI] [PubMed] [Google Scholar]
- Peteet J (2000). Cancer and the meaning of work. Gen Hosp Psychiat, 22: 200–205. [DOI] [PubMed] [Google Scholar]
- Nachreiner NM, Dagher RK, McGovern PM, Baker BA, Alexander BH, Gerberich SG (2007). Successful return to work for cancer survivors. AAOHN J, 55(7): 290–295. [DOI] [PubMed] [Google Scholar]
- Steiner JF, Cavender TA, Main DS, Bradley CJ (2004). Assessing the impact of cancer on work outcomes what are the research needs? Cancer, 101(8): 1703–1711. [DOI] [PubMed] [Google Scholar]
- Waddell G, Burton A, Kendall N (2008). Vocational Rehabilitation: What works for whom and when? Commissioned by the Vocational Rehabilitation Project Group in association with the Industrial Injuries Advisory Council. [Google Scholar]
- WHO (2001). International Classification of Functioning, Disability and Health, WHO: Geneva, 10–21. [Google Scholar]
- Stewart DE, Cheung AM, Duff S, Wong F, McQuestion M, Cheng T, Purdy L, Bunston T (2001). Long-term breast cancer survivors: confidentiality, disclosure, effects on work and insurance. Psycho-Oncol, 10(3): 259–263. [DOI] [PubMed] [Google Scholar]
- Mehnert, Koch (2013). Predictors of employment among cancer survivors after medical rehabilitation-a prospective study. Scand J Work Environ Health, 1: 76–87. [DOI] [PubMed] [Google Scholar]
- Torp S, Nielsen RA, Gudbergsson SB, Dahl AA (2012). Worksite adjustments and work ability among employed cancer survivors. Support Care Cancer, 20(9): 2149–2156. [DOI] [PubMed] [Google Scholar]
- Thijs KM, de Boer AG, Vreugdenhil G, van de Wouw, Houterman S, Schep G (2012). Rehabilitation using high-intensity physical training and long term return to work in cancer survivors. J Occup Rehabil, 22(2): 220–229. [DOI] [PubMed] [Google Scholar]
- Choi KS, Kim EJ, Lim JH, Kim SG, Lim MK, Park JG, Park EC (2007). Job loss and re-employment after a cancer diagnosis in Koreans - A prospective cohort study. Psycho-Oncol, 16(3): 205–213. [DOI] [PubMed] [Google Scholar]
- Johnsson A, Fornander T, Olsson M, Nystedt M, Johansson H, Rutqvist LE (2007). Factors associated with return to work after breast cancer treatment. Acta Oncol, 46(1): 90–96. [DOI] [PubMed] [Google Scholar]
- Park JH, Park JH, Kim SG (2009). Effect of cancer diagnosis on patient employment status: a nationwide longitudinal study in Korea. Psycho-Oncol, 18(7): 691–699. [DOI] [PubMed] [Google Scholar]
- Kennedy F, Haslam C, Munir F, Pryce J (2007). Returning to work following cancer: A qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care, 16(1): 17–25. [DOI] [PubMed] [Google Scholar]
- Main DS, Nowels CT, Cavender TA, Etschmaier M, Steiner JF (2005). A qualitative study of work and work return in cancer survivors. Psycho-Oncol, 14(11): 992–1004. [DOI] [PubMed] [Google Scholar]
- Fantoni SQ, Peugniez C, Duhamel A, Skrzypczak J, Frimat P, Leroyer A (2010). Factors related to return to work by women with breast cancer in Northern France. J Occup Rehabil, 20(1): 49–58. [DOI] [PubMed] [Google Scholar]
- Bouknight RR, Bradley CJ, Luo Z (2006). Correlates of return to work for breast cancer survivors. J Clin Oncol, 24(3): 345–353. [DOI] [PubMed] [Google Scholar]
- Ross L, Petersen MA, Johnsen AT, Lundstroem LH, Carlsen K, Groenvold M (2012). Factors associated with Danish cancer patients’ return to work. A report from the population-based study ‘The Cancer Patient's World’. Cancer Epid, 36: 222–229. [DOI] [PubMed] [Google Scholar]
- Roelen CA (2011). Sickness absence and full return to work after cancer: 2-year follow-up of register data for different cancer sites. Psycho-Oncol, 20: 1001–1006. [DOI] [PubMed] [Google Scholar]
- Ahn E, Cho J, Shin DW, Park BW, Ahn SH, Noh DY, Nam SJ, Lee ES, Yun YH (2009). Impact of breast cancer diagnosis and treatment on work-related life and factors affecting them. Breast Cancer Res and Treat, 116(3): 609–616. [DOI] [PubMed] [Google Scholar]
- Earle CC, Chretien Y, Morris C, Ayanian JZ, Keating NL, Polgreen LA, Wallace R, Ganz PA, Weeks JC (2010). Employment among survivors of lung cancer and colorectal cancer. JCO, 28(10): 1700–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnsson A, Fornander T, Rutqvist LE, Olsson M (2010). Factors influencing return to work: A narrative study of women treated for breast cancer. EJC, 19(3): 317–323. [DOI] [PubMed] [Google Scholar]
- Grunfeld EA, Drudge-Coates L, Rixon L, Eaton E, Cooper AF (2013). “The only way I know how to live is to work”: A qualitative study of work following treatment for prostate cancer. Health Psychol, 32: 75–82. [DOI] [PubMed] [Google Scholar]
- Tiedtke EA (2012). Survived but feeling vulnerable and insecure: a qualitative study of the mental preparation for RTW after breast cancer treatment. BMC Public Health, 12: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunfeld EA, Low E, Cooper AF (2010). Cancer survivors’ and employers’ perceptions of working following cancer treatment. Occup Med, 60(8): 611–617. [DOI] [PubMed] [Google Scholar]
- Sanchez KM, Richardson JL, Mason HRC (2004). The return to work experiences of colorectal cancer survivors. AAOHN J, 52(12): 500–510. [PubMed] [Google Scholar]
- Nilsson EA (2011). Return to work after breast cancer: Women's experiences of encounters with different stakeholders. EJON, 15: 267–274. [DOI] [PubMed] [Google Scholar]
- Roelen CA, Koopmans PC, Schellart AJ, van der Beek AJ (2011). Resuming work after cancer: A prospective study of occupational register data. J Occup Rehabil, 2(3): 431–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarker J, Munir F, Bains M, Kalawsky K, Haslam C (2010). The role of communication and support in return to work following cancer-related absence. Psycho-Oncol, 19(10): 1078–1085. [DOI] [PubMed] [Google Scholar]
- de Boer AG, Verbeek JHAM, Spelten ER, Uitterhoeve ALJ, Ansink AC, de Reijke TM, Kammeijer M, Sprangers MAG, van Dijk FJH (2008). Work ability and return-to-work in cancer patients. Br J Cancer, 98(8): 1342–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (1997). WHOQOL Measuring Quality of Life in Programme on Mental Health. Division of Mental Health and Prevention of Substance Abuse, pp.: 10–20. [Google Scholar]
- Mueller M (2012). What researchers mean by quality of life in at Work, Spring, pp.: 2–7. [Google Scholar]
- Maunsell E, Drolet M, Brisson J, Brisson C, Mâsse B, Deschênes L (2004). Work situation after breast cancer: results from a population-based study. J National Cancer Inst, 96(24): 1813–1822. [DOI] [PubMed] [Google Scholar]
- Bradley CJ, Bednarek HL (2002). Employment patterns of long-term cancer survivors. Psycho-Oncol, 11(3): 188–198. [DOI] [PubMed] [Google Scholar]
- Short PF, JJ Vasey, Tunceli K (2005). Employment pathways in a large cohort of adult cancer survivors. Cancer, 103(6): 1292–1301. [DOI] [PubMed] [Google Scholar]
- Feldman F (1978). Work and cancer health histories: a study of experiences of recovered blue collar workers. American Cancer Society, Atlanta. [Google Scholar]
- Bjorklund A (1985). Unemployment and mental health: some evidence from panel data. J Hum Resour, 20(4): 469–483. [Google Scholar]
- Helliwell JF and Putnam R (2004). The social context of well-being. Philosophical Transactions of the Royal Society, pp.: 1435–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taskila T, ML Lindbohm (2007). Factors affecting cancer survivors’ employment and work ability. Acta Oncol, 46(4): 446–451. [DOI] [PubMed] [Google Scholar]
- Hansen JA, Feuerstein M, Calvio LC, Olsen CH (2008). Breast cancer survivors at work. Occup Environ Med, 50(7): 777–784. [DOI] [PubMed] [Google Scholar]
- Taskila T, Martikainen R, Hietanen P, Lindbohm ML (2007). Comparative study of work ability between cancer survivors and their referents. Eur J Cancer, 43(5): 914–920. [DOI] [PubMed] [Google Scholar]
- Lee MK, Lee KM, Bae JM, Kim S, Kim YW, Ryu KW, Lee JH, Noh JH, Sohn TS, Hong SK, Yun YH (2008). Employment status and work-related difficulties in stomach cancer survivors compared with general population. Bri J Cancer, 98(4): 708–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunceli K, Short PF, Moran JR, Tunceli O (2009). Cancer survivorship, health insurance and employment transitions among older workers. Inquiry, 46(1): 17–32. [DOI] [PMC free article] [PubMed] [Google Scholar]