Abstract
Background:
Based on the microRNA (miRNA) signature of bladder cancer (BC) by deep sequencing, we recently found that several double-stranded mature miRNAs derived from the same pre-miRNAs were sufficiently expressed and acted as tumour suppressors by regulating common target genes in BC. Our deep-sequencing signature of BC showed that all miR-199 family members (miR-199a-3p/-5p and miR-199b-3p/-5p) were also downregulated. We hypothesised that these miRNAs may function as tumour suppressors by regulating common target genes.
Methods:
Functional assays of BC cells were performed using transfection of mature miRNA. In silico analyses and luciferase reporter analyses were applied to identify target genes of these miRNAs. The overall survival of patients with BC in The Cancer Genome Atlas (TCGA) database was evaluated by the Kaplan–Meier method.
Results:
Restoration of these miRNAs significantly inhibited cell migration and invasion in BC cells. Integrin α3 (ITGA3) was directly regulated by these miRNAs. The Cancer Genome Atlas database showed that patients with low pre-miR-199 family (miR-199a-1/-2 and miR-199b) expression exhibited significantly poorer overall survival compared with patients with high pre-miR-199 family expression.
Conclusions:
miR-199 family miRNAs functioned as tumour suppressors in BC cells by targeting ITGA3 and might be good prognostic markers for predicting survival in patients with BC.
Keywords: microRNA, miR-199, ITGA3, bladder cancer, tumour suppressor
Bladder cancer (BC) is the ninth most commonly diagnosed cancer worldwide in 2012 (Torre et al, 2015; Antoni et al, 2017). In the United States of America, it was estimated that ∼76 960 cases were diagnosed and 16 390 patients died in 2016 (Siegel et al, 2016). Bladder cancer can be classified into two groups: non-muscle-invasive BC (NMIBC) and muscle-invasive BC (MIBC). More than 70% of patients with BC are diagnosed with NMIBC (Miller et al, 2016). However, patients with NMIBC tend to have a high rate of recurrence, as high as 50–70% (Kaufman et al, 2009). Patients with localised MIBC are managed by radical cystectomy. However, despite potential curative surgery, ∼50% of patients develop metastatic disease within only 2 years (Sternberg et al, 2013). Patients with advanced BC are generally treated with systemic combination chemotherapy of cisplatin and gemcitabine; however, the therapeutic effects are insufficient (Kaufman et al, 2009; Sternberg et al, 2013). Most clinical trials of chemotherapeutics with other drugs for advanced BC have shown limited benefits and a short median survival period of only ∼9.3–15.8 months (Bellmunt et al, 2012; De Santis et al, 2012). Moreover, there are no more reliable markers other than urine cytology for BC diagnosis, and this approach has relatively low sensitivity (30–40%) (Enokida et al, 2016). Therefore, novel prognostic markers and effective treatment strategies based on RNA network studies are urgently needed to improve outcomes in patients with BC.
MicroRNAs (miRNAs) are endogenous small noncoding RNAs of 19–22 nucleotides in length that negatively regulate protein-coding genes by binding to the 3′-untranslated region (UTR) of the target mRNA, thereby inhibiting transcriptional or post-transcriptional expression (Bartel, 2004; Carthew and Sontheimer, 2009). Previous studies have demonstrated that miRNAs are aberrantly expressed in various types of cancer and have the critical roles in cancer cell behaviour (Di Leva and Croce, 2010). Therefore, the detection of aberrantly expressed miRNAs and their target genes could provide important insights into the elucidation of miRNA-mediated oncogenic pathways.
In miRNA biogenesis, the guide-strand of miRNA integrates into the RNA-induced silencing complex (RISC), whereas the passenger strand is inactivated through degradation (Chendrimada et al, 2007; Carthew and Sontheimer, 2009). However, our previous analysis of miRNA signatures in BC by deep sequencing revealed that the opposite strands of miR-144-5p/-3p, miR-145-5p/-3p, and miR-139-5p/-3p function as dual-strand tumour-suppressor miRNAs (Matsushita et al, 2015, 2016;Yonemori et al, 2016). Based on our additional analysis of the miRNA signature, we also found another set of downregulated miRNAs, the miR-199 family (miR-199a-3p/-5p derived from pre-miR-199a-1/-2 and miR-199b-3p/-5p derived from pre-miR-199b) (Itesako et al, 2014). The sequence of miR-199a-3p (guide strand) is the same as that of miR-199b-3p (guide strand), and the sequence of miR-199a-5p (passenger strand) is very similar to that of miR-199b-5p (passenger strand) (only two bases differ). Therefore, we hypothesised that these miRNAs may function as tumour suppressors by regulating common target genes. Several previous studies have shown that miR-199 family members function as tumour suppressors in various types of cancer (Hu et al, 2014; Li et al, 2015; Sun et al, 2016). With regard to miR-199a-5p, some reports have shown that this miRNA functions as a tumour suppressor in BC (Su et al, 2013; Song et al, 2015). However, the role of miR-199 family members in BC is still unclear.
The aim of this study was to investigate the antitumour effects of miR-199 family members and to determine their regulatory targets in BC. The elucidation of molecular targets regulated by tumour-suppressive miR-199 family member will provide important new insights into the potential mechanisms of BC oncogenesis and progression.
Materials and methods
Clinical specimens and cell culture
The tissue specimens for quantitative real-time reverse transcription–polymerase chain reaction (qRT–PCR) were collected from BC patients (n=32) at Kagoshima University Hospital between 2004 and 2013. Normal bladder epithelia (NBE) (n=12) were derived from patients with noncancerous disease. The specimens were staged according to the American Joint Committee on Cancer-Union Internationale Contre le Cancer tumour node metastasis classification and histologically graded (Sobin and Compton, 2010). Our study was approved by the Bioethics Committee of Kagoshima University; written prior written consent and approval were obtained from all patients. Patient details and clinicopathological characteristics are summarised in Supplementary Table 1.
We used human BC cell lines: T24 and BOY. These cell lines were described in our previous studies (Itesako et al, 2014).
Tissue collection and RNA extraction
Tissues were immersed in RNA later (Thermo Fisher Scientific, Waltham, MA, USA) and stored at −20 °C until RNA extraction. Total RNA, including miRNA, was extracted using a mirVana miRNA Isolation Kit (Thermo Fisher Scientific) following the manufacturer's protocol.
Quantitative real-time reverse transcription–polymerase chain reaction
Stem-loop RT–PCR (TaqMan MicroRNA Assays; P/N: 000498 for miR-199a-5p, P/N: 000500 for miR-199b-5p, and P/N: 002304 for miR-199a-3p/miR-199b-3p; Applied Biosystems, Foster City, CA, USA) was used to quantify miRNAs according to previously published conditions (Ichimi et al, 2009). We used human RNU48 (P/N: 001006; Applied Biosystems) as an internal control, and the ΔCt method was used to calculate the fold changes. As for integrin α3 (ITGA3), we applied a SYBR-green quantitative PCR-based array approach; each sequence is listed in Supplementary Table 2. The experimental procedures followed the protocol recommended by the manufacturer. Quantitative real-time reverse transcription–polymerase chain reaction was performed with 500 ng of total RNA using Power SYBR Green Master Mix (cat. no. 4367659; Applied Biosystems) on a 7300 Real-time PCR System (Applied Biosystems). The specificity of amplification was monitored using the dissociation curve of the amplified product. All data values were normalised to GUSB, and the ΔCt method was used to calculate the fold change.
Transfection with mature miRNA and siRNA
As described elsewhere (Ichimi et al, 2009), T24 and BOY cells were transfected with Lipofectamine RNAiMAX transfection reagent (Thermo Fisher Scientific) and Opti-MEM (Thermo Fisher Scientific) with 10 nM mature miRNA or small interfering RNA (siRNA). Mature miRNA precursors (hsa-miR-199a-5p, product ID PM10893; hsa-miR-199b-5p, product ID: PM10553; hsa-miR-199a/b-3p, product ID: PM11779; Thermo Fisher Scientific) and negative-control miRNA (product IDs: AM17110, AM17111; Thermo Fisher Scientific) were used in gain-of-function experiments, whereas ITGA3 siRNA (cat nos. HSS105529 and HSS105531; Thermo Fisher Scientific) and negative-control siRNA (D-001810-10; Thermo Fisher Scientific) were used in loss-of-function experiments.
Cell proliferation, migration, and invasion assays
Cell proliferation was determined by XTT assay according to the manufacturer's instructions. Cell migration activity was evaluated with wound-healing assays. Cell invasion assays were performed using modified Boyden chambers consisting of Transwell-precoated Matrigel membrane filter inserts with 8-mm pores in 24-well tissue culture plates (BD Biosciences, Bedford, MA, USA). The experimental procedures were performed as described in our previous studies (Tatarano et al, 2011; Yoshino et al, 2011). All experiments were performed in triplicate.
Western blot analysis
After transfection (72 h), protein lysates were separated on NuPAGE on 4–12% Bis-Tris gels (Invitrogen, Carlsbad, CA, USA) and transferred to PVDF membranes. Immunoblotting was carried out with diluted (1 : 1000) anti-ITGA3 antibodies (HPA008572; Sigma-Aldrich, St Louis, MO, USA) and anti-β-actin antibodies (bs-0061R; Bioss, Woburn, MA, USA). Specific complexes were visualised using an echochemiluminescence detection system (GE Healthcare, Little Chalfont, UK) as described previously (Yoshino et al, 2011).
Immunohistochemical analysis
A tissue microarray of BC samples was obtained from US Biomax Inc. (product ID: BL 1002; Rockville, MD, USA). Detailed information on all tumour specimens can be found at http://www.biomax.us/index.php. The tissue microarray was immunostained following the manufacturer's protocol with an Ultra Vision Detection System (Thermo Scientific). Primary rabbit polyclonal antibodies against ITGA3 (HPA008572; Sigma-Aldrich) were diluted 1 : 20. Immunostaining was evaluated according to the scoring method described previously (Yoshino et al, 2011). Each case was scored on the basis of the intensity and area of staining. The intensity of staining was graded on the following scale: 0, no staining; 1+, mild staining; 2+, moderate staining; and 3+, intense staining. The area of staining was evaluated as follows: 0, no staining of cells in any microscopic field; 1+,<30% of cells stained positive; 2+, 30–60% stained positive; 3+,>60% stained positive. The immunostaining scores (intensity+extent) were combined and analysed. All samples were independently scored by two of the authors (T Sakaguchi and K Miyamoto), who were blinded to the patient status.
In silico analysis for the identification of genes regulated by miR-199a-3p/-5p and miR-199b-3p/-5p
To obtain candidate target genes regulated by miR-199a-3p/-5p and miR-199b-3p/-5p, we used TargetScan database Release 7.0 (http://www.targetscan.org). These candidate target genes data were adapted to the KEGG pathway categories by the GENECODIS program (http://genecodis.cnb.csic.es). Additionally, the Gene Expression Omnibus (GEO) database (accession numbers: GSE11783 and GSE31684) was used to identify upregulated genes in BC specimens.
Plasmid construction and dual-luciferase reporter assays
Partial wild-type sequences of the 3′-UTR of ITGA3 or sequences with deletion of the miR-199a-5p/miR-199b-5p target sites and miR-199a-3p/miR-199b-3p target site were inserted between the XhoI and PmeI restriction sites in the 3′-UTR of the hRluc gene in the psiCHECK-2 vector (C8021; Promega, Madison, WI, USA). T24 and BOY cells were transfected with 50 ng vector and 10 nM miR-199a-5p or miR-199b-5p or miR-199a/b-3p. The procedure for dual-luciferase reporter assay was described previously (Yoshino et al, 2013a).
Analysis of the BC cohort in TCGA data sets
The Cancer Genome Atlas (TCGA) cohort database was used to analyse ITGA3 mRNA expression levels in normal and BC samples and to determine if there was a clinical relationship between miR-199a/b or ITGA3 expression and overall survival. RNA-seq expression data (normalised RSEM) and miRNA-seq data (reads per million mapped reads) were used for gene and miRNA quantification (Li and Dewey, 2011). mRNA expression by whole-exome sequencing data was available for 408 patients with BC. Full sequencing information and clinical information were acquired using cBioPortal (http://www.cbioportal.org/public-portal/) and TCGA (https://tcga-data.nci.nih.gov/tcga/) (Cerami et al, 2012; Gao et al, 2013; Cancer Genome Atlas Research N, 2014). This study meets the publication guidelines provided by TCGA (http://cancergenome.nih.gov/publications/publicationguidelines).
Statistical analysis
The relationships between two groups were analysed using Mann–Whitney U-tests. The relationships between three variables and numerical values were analysed using Bonferroni-adjusted Mann–Whitney U-tests. Spearman's rank tests were used to evaluate the correlations between the expression of miR-199a-5p or miR-199b-5p and miR-199a/b-3p. χ2 tests were used to analyse the relationships between ITGA3 expression in Immunohistochemical (IHC) staining and clinicopathological characteristics. The overall survival of patients with BC from the TCGA cohort was evaluated by the Kaplan–Meier method. Patients were divided into two or three groups based on the number of patients in the cohort, and differences between the two groups were evaluated by log-rank tests. All analyses were carried out using Expert StatView software, version 5.0 (Cary, NC, USA).
Results
Expression levels of miR-199a-5p, miR-199b-5p, and miR-199a/b-3p in BC
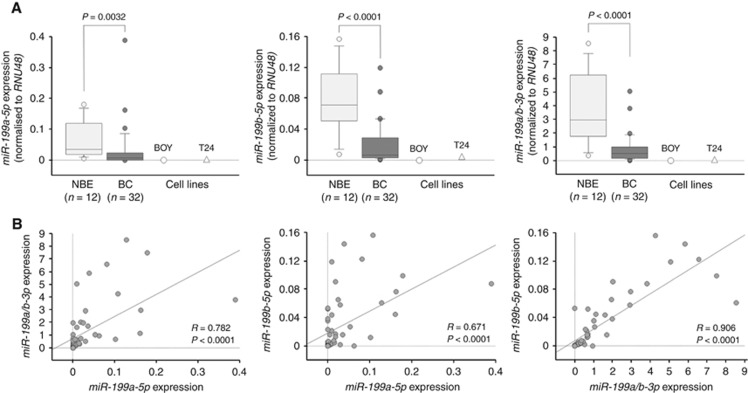
First, we evaluated the expression levels of miR-199a-5p, miR-199b-5p, and miR-199a/b-3p in BC tissues (n=32) and NBE (n=12) by qRT–PCR. The expression levels of these mature miRNAs were significantly reduced in BC tissues compared with those in the NBE (P=0.0032, P<0.0001, and P<0.0001, respectively; Figure 1A). Spearman's rank test revealed significant positive correlations between the expression levels of these miRNAs (each P<0.0001; Figure 1B). We found no significant relationships between the clinicopathological parameters (i.e., tumour stage, grade) and the expression levels of miR-199a-5p, miR-199b-5p, and miR-199a/b-3p (data not shown).
Figure 1.
The expression levels of miR-199 family members in clinical BC specimens. (A) The expression levels of miR-199a-5p, miR-199b-5p, and miR-199a/b-3p, as determined by qRT–PCR, were significantly lower in BC specimens than in NBE specimens (P=0.0032, P<0.0001, and P<0.0001, respectively). (B) Spearman's rank test demonstrated that these miRNAs expression levels were positively correlated (each P<0.0001).
Effects of miR-199a-5p, miR-199b-5p, and miR-199a/b-3p restoration on cell proliferation, migration, and invasion activities in BC cell lines
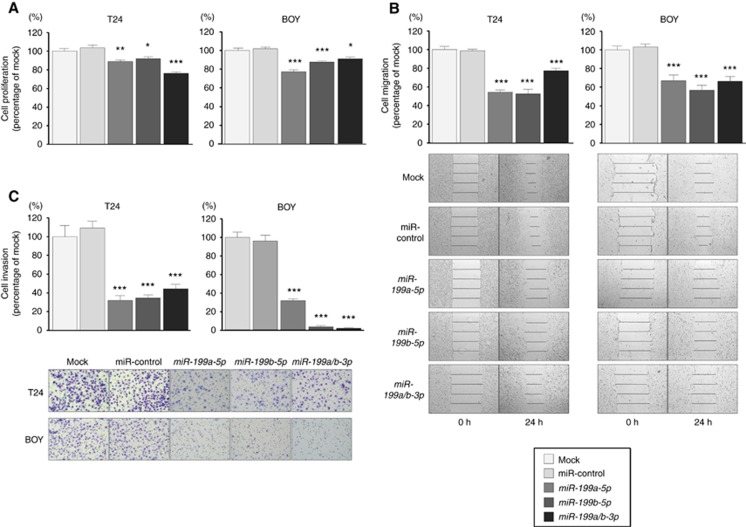
We performed gain-of-function studies using T24 and BOY cells transfected with miR-199a-5p, miR-199b-5p, or miR-199a/b-3p to investigate their functional roles. XTT assays revealed significant inhibition of cell proliferation in T24 and BOY cells transfected with miR-199a-5p, miR-199b-5p, and miR-199a/b-3p in comparison with mock or miR-control transfectants (T24: P<0.05, P=0.0007, and P<0.0001, respectively; BOY: P<0.0001, P<0.0001, and P<0.05, respectively; Figure 2A). Moreover, wound-healing assays demonstrated that cell migration activity was significantly inhibited in these miRNA transfectants in comparison with that in mock or miR-control transfectants (each P<0.0001; Figure 2B). Finally, Matrigel invasion assays demonstrated that the number of invading cells was significantly decreased in these miRNA transfectants compared with mock or miR-control transfectants (each P<0.0001; Figure 2C). These data suggested that miR-199 family members functioned as tumour suppressors in BC cells.
Figure 2.
Effects of miR-199a-5p, miR-199b-5p, and miR-199a/b-3p transfection in BC cell lines.(A) Cell proliferation was determined by XTT assays. (B) Cell migration activity was determined with wound-healing assays. (C) Cell invasion activity was determined using Matrigel invasion assays. *P<0.05; **P=0.0007; ***P<0.0001.
Identification of common target genes regulated by miR-199 family members in BC cells
Next, in silico analysis was used to gain additional insights into the molecular mechanisms and pathways regulated by tumour-suppressive miR-199 family members in BC cells. Supplementary Figure 1 shows our strategy to narrow down the common target genes of miR-199 family members. Candidate genes of miR-199-5p and miR-199-3p (4195 and 3013 genes, respectively) were identified using TargetScan database Release 7.0 (http://www.targetscan.org). Among these candidate genes, we identified 1127 common candidate target genes of miR-199-5p and miR-199-3p. Moreover, these candidate target genes were categorised into KEGG pathways using GENECODIS analysis (http://genecodis.cnb.csic.es). Our analysis indicated that these genes were implicated in 64 significantly enriched pathways (Supplementary Table 3). Among these pathways, we focused on ‘pathways in cancer', because the greatest number of genes (29 genes) was listed within this pathway. Of these 29 genes, 10 genes were upregulated in the GEO database (accession numbers: GSE11783 and GSE31684; Supplementary Table 4). Finally, among these 10 genes, we focused on the ITGA3 gene because miR-199 family members significantly inhibited cancer cell migration and invasion. Molecular target searches suggested that ITGA3 was a promising candidate target regulated by the miR-199 family in BC cells.
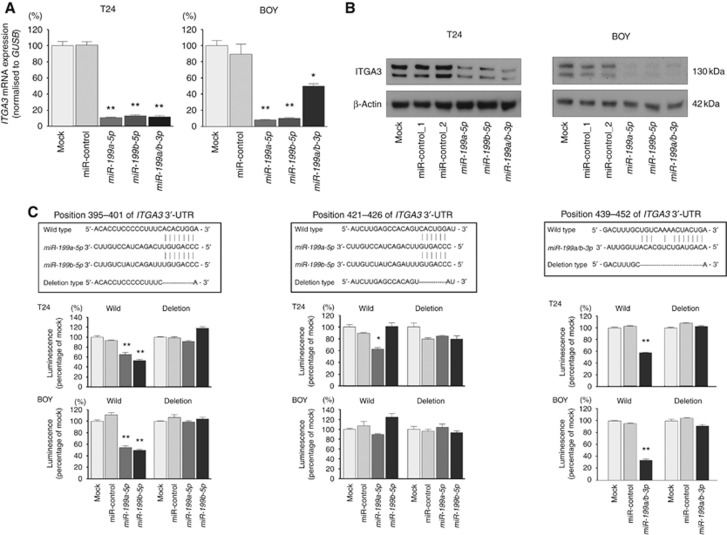
ITGA3 was directly regulated by miR-199a-5p, miR-199b-5p, and miR-199a/b-3p in BC cells
We performed qRT–PCR and western blot analyses to confirm that restoration of miR-199a-5p, miR-199b-5p, and miR-199a/b-3p downregulated ITGA3 mRNA expression in T24 and BOY cells. ITGA3 mRNA levels were markedly and significantly reduced in these miRNA transfectants in comparison with those in mock or miR-control transfectants (P<0.0001 and P=0.0002; Figure 3A). Moreover, the expression of ITGA3 protein was markedly repressed in these miRNAs transfectants in comparison with mock or miR-control transfectants (Figure 3B). Two bands were observed on western blots and were found at the expected sizes for ITGA3 at around 130 kDa. These two bands could be the two isoforms of ITGA3 (α3A and α3B) (de de Melker et al, 1997). Another possibility is that aberrantly modified ITGA3 may be expressed. In fact, the expression of aberrantly glycosylated ITGA3 in BC has been reported (Li et al, 2014, 2016a).
Figure 3.
Direct regulation of ITGA3 by miR-199a/b-5p and miR-199a/b-3p. (A) The expression of ITGA3 mRNA was significantly repressed in these miRNAs transfectants in comparison with that in mock or miR-control transfectants. GUSB was used as an internal control. *P=0.0002; **P<0.0001. (B) The expression of ITGA3 protein was markedly repressed in these miRNAs transfectants in comparison with that in mock or miR-control transfectants. β-Actin was used as a loading control. (C) Dual-luciferase reporter assays using vectors encoding putative miRNA target sites for wild-type or deleted regions. Normalised data were calculated as ratios of Renilla/firefly luciferase activities. The luminescence intensity was significantly reduced by co-transfection with miR-199a/b-5p or miR-199a/b-3p and the vector carrying the wild-type sequences at positions 395–401 and 439–452 in the ITGA3 3′-UTR. *P<0.0001, **P=0.0001.
We then performed dual-luciferase reporter assays in BC cells to determine whether ITGA3 was directly regulated by these miRNAs. The TargetScan database predicted that there were two binding sites for miR-199a/b-5p (positions 395–401 and 421–426) and one binding site for miR-199a/b-3p (position 439–452) in the ITGA3 3′-UTR. We used vectors encoding the partial wild-type sequence of the 3′-UTR of ITGA3, including the predicted miR-199a/b-5p and miR-199a/b-3p target sites. We found that the luminescence intensity was significantly reduced by co-transfection with these miRNAs and the vector carrying the wild-type sequences at positions 395–401 and 439–452 in the ITGA3 3′-UTR (each P<0.0001), whereas transfection with the deletion vector (in which the binding site had been removed) and the wild-type sequence at positions 421–426 in the ITGA3 3′-UTR blocked the decrease in luminescence (Figure 3C). These data suggested that miR-199a/b-5p and miR-199a/b-3p were directly bound to specific sites in the 3′-UTR of ITGA3 mRNA.
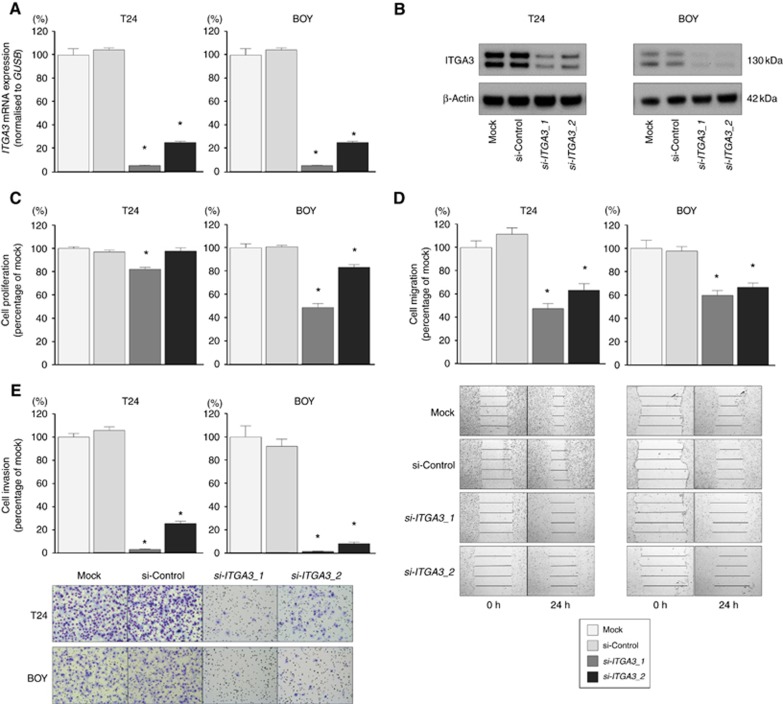
Effects of ITGA3 knockdown on cell proliferation, migration, and invasion in BC cell lines
To investigate the functional role of ITGA3 in the BC cells, we performed loss-of-function studies using cells transfected with two si-ITGA3 constructs (si-ITGA3_1 and si-ITGA3_2). We evaluated the knockdown efficiency of si-ITGA3 transfection in BC cells. Quantitative real-time reverse transcription–polymerase chain reaction and western blot analyses showed that these siRNAs effectively downregulated ITGA3 mRNA and protein expression in both cell lines (each P<0.0001; Figures 4A and B). Additionally, in this experiment, we also observed two bands on western blot analysis for ITGA3, similar to the results described in the previous section. XTT assays demonstrated that BOY cell proliferation was inhibited in si-ITGA3 transfectants in comparison with that in mock or si-control transfectants (each P<0.0001). Although si-ITGA3_1 inhibited cell proliferation significantly in T24 cells, no significant inhibition was observed in si-ITGA3_2-transfected T24 cells (Figure 4C). In contrast, wound-healing assays demonstrated that cell migration activity was significantly inhibited in si-ITGA3 transfectants in comparison with that in mock or si-control transfectants (each P<0.0001; Figure 4D). Moreover, Matrigel invasion assays demonstrated that cell invasion activity was significantly inhibited in si-ITGA3 transfectants in comparison with that in mock or si-control transfectants (each P<0.0001; Figure 4E).
Figure 4.
Effects of si-ITGA3 transfection on BC cell lines.(A) The expression of ITGA3 mRNA was significantly repressed in si-ITGA3 transfectants in comparison with that in mock or si-control transfectants. GUSB was used as an internal control. *P<0.0001. (B) The expression of ITGA3 protein was markedly repressed in si-ITGA3 transfectants in comparison with that in mock or si-control transfectants. β-Actin was used as a loading control. (C) Cell proliferation was determined by XTT assays. (D) Cell migration activity was determined using wound-healing assays. (E) Cell invasion activity was determined with Matrigel invasion assays. *P<0.0001.
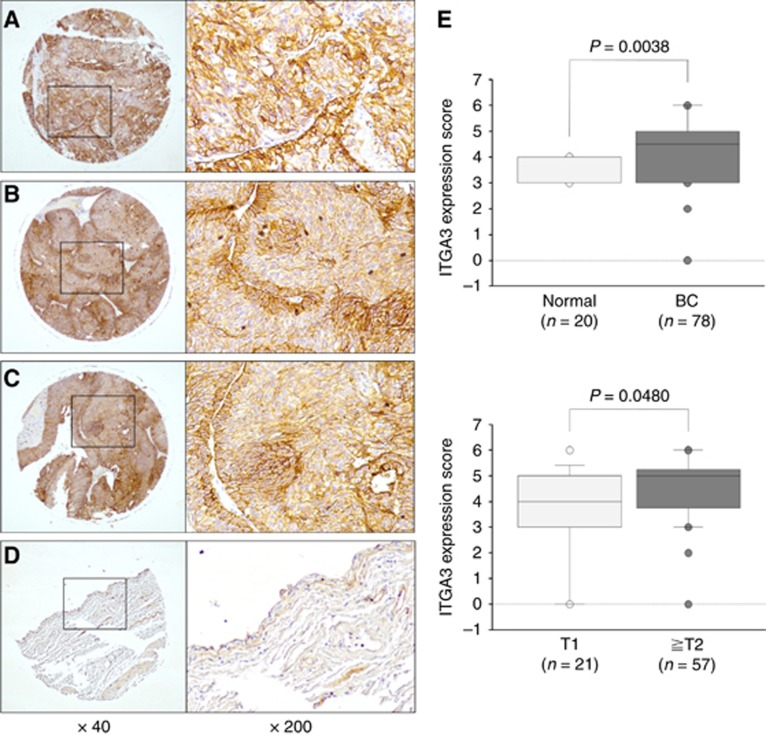
IHC analysis of ITGA3 in a tissue microarray
Next, we examined the expression level of ITGA3 in BC specimens by IHC staining. ITGA3 was strongly expressed in several tumour lesions, whereas low expression was observed in the normal tissue (Figures 5A–D). Tissue microarray analysis revealed that the IHC score of tumours was significantly higher than that of normal tissues (Mann–Whitney U-test; P=0.0038, χ2 test; P<0.0001; Figure 5E, upper and Supplementary Table 5). In addition, we also found that ITGA3 expression in T2 or greater BCs was significantly higher than that in T1 BCs (P=0.048; Figure 5E, lower). However, we found no significant difference between the ITGA3 expression score and other pathological parameters (histological grade and pathological diagnosis) of BC patients (Supplementary Table 5).
Figure 5.
IHC staining of ITGA3 in tissue specimens.(A) Strong positive staining in a tumour lesion (grade 2, T3N0M0), (B) strong positive staining in a tumour lesion (grade 1, T2N0M0), (C) strong positive staining in a tumour lesion (grade 2, T1N0M0), and (D) weak positive staining in normal bladder tissue. (E) ITGA3 expression scores in IHC staining; upper, ITGA3 expression in normal bladder tissues and BC; lower, correlation between ITGA3 expression and tumour status in BC.
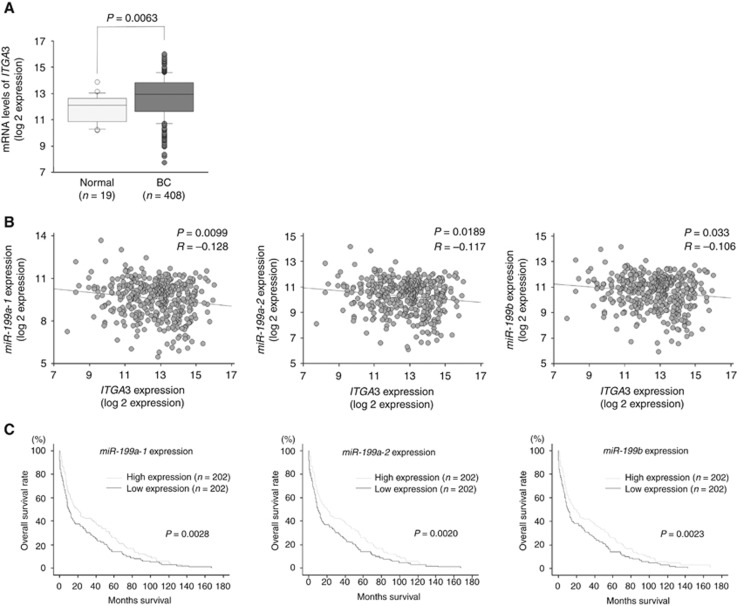
Analysis of the clinical BC specimens in TCGA data sets
We investigated ITGA3 mRNA expression levels and the correlations between pre-miR-199 family members and ITGA3 expression in BC samples using the TCGA database. Among the BC cohort in TCGA, we investigated patients for whom ITGA3 expression data could be obtained. The expression level of ITGA3 was significantly upregulated in patients with BC (n=408) compared with that in normal patients (n=19; P=0.0063; Figure 6A). Specifically, there was a significant negative correlation between miR-199a-1 or miR-199a-2 or miR-199b and ITGA3 expression (P=0.0099, R=−0.128; P=0.0189, R=−0.117; and P=0.033, R=−0.106, respectively; Figure 6B).
Figure 6.
Analysis of the clinical BC specimens in TCGA data sets.(A) The expression level of ITGA3 mRNA was significantly upregulated in BC tissues compared with that in normal bladder tissues (P=0.0063). (B) Negative correlations between ITGA3 expression and miR-199a-1, miR-199a-2, and miR-199b expression in BC tissues (P=0.0099, R=−0.128; P=0.0189, R=−0.117; and P=0.033, R=−0.106, respectively). (C) Overall survival was significantly prolonged in patients with high miR-199a-1, miR-199a-2, and miR-199b expression compared with that in patients with low expression of these miRNAs (P=0.0028, P=0.0020, and P=0.0023, respectively).
We examined the correlation of pre-miR-199 family expression levels with overall survival using the TCGA database. Among the BC cohort in TCGA, we investigated 404 patients for whom pre-miR-199 family expression and survival time data could be obtained. The cohort was divided into two groups based on the number of patients. Importantly, we found that patients with low miR-199 family expression (n=202) had poor survival compared with patients with high miR-199 family expression (n=202). Kaplan–Meier analysis showed that the low miR-199a-1, miR-199a-2, and miR-199b expression groups had significantly lower overall survival rates than patients with high expression of these pre-miRNA groups. The median overall survival times were 8.46, 8.46, and 8.48 months in the low miR-199a-1, miR-199a-2, and miR-199b expression groups versus 11.44, 11.44, and 11.41 months in the high expression groups (P=0.0028, P=0.0020, and P=0.0023, respectively; Figure 6C). Next, we examined the correlation of ITGA3 expression level with overall survival. Among the BC cohort in TCGA, we investigated 403 patients for whom ITGA3 expression and survival time data could be obtained. The cohort was divided into three groups according to the number of patients. Kaplan–Meier analysis showed that patients in the high ITGA3 expression group (n=134) exhibited lower overall survival rates compared with those in the low expression group (n=134); however, this difference was not significant (P=0.0823). Moreover, there were no significant differences between the medium ITGA3 expression group (n=135) and the high or low expression groups (Supplementary Figure 2).
Discussion
MicroRNAs are vitally important regulators that contribute to numerous physiological processes, such as cell proliferation, differentiation, development, and apoptosis (Croce, 2009; Di Leva and Croce, 2010). MicroRNAs are unique in their ability to regulate multiple protein-coding genes. Recently, bioinformatics predictions have indicated that miRNAs may regulate more than 60% of the protein-coding genes in the human genome (Friedman et al, 2009). Additionally, in human cancer, miRNAs are aberrantly expressed and have important roles in cancer initiation, development, and metastasis (Nelson and Weiss, 2008; Yoshino et al, 2013b). Many genome-wide miRNA expression signatures, including deep-sequencing analysis, have revealed aberrantly upregulated or downregulated expression of miRNAs in BC (Han et al, 2011; Chen et al, 2013). Subsequently, many studies have demonstrated that aberrantly downregulated miRNAs can function as tumour suppressors by regulating different target genes and cancer pathways. Therefore, identification of tumour-suppressive miRNAs and the molecular pathways mediated by these miRNAs is important to improve our understanding of cancer mechanisms.
In general, the guide-strand RNA from duplex miRNA is retained for direct recruitment of the RISC to target mRNAs, whereas the passenger-strand RNA is degraded (Chendrimada et al, 2007; Carthew and Sontheimer, 2009). In our previous study of PCR-based miRNA screening in BC, only miR-199a-5p and miR-199b-5p were indicated as downregulated miRNAs (Yoshino et al, 2011). However, in the present study, deep-sequencing analysis showed that all miR-199 family members (miR-199a-3p/-5p and miR-199b-3p/-5p) were downregulated in BC tissues in comparison with normal bladder tissues. In addition, in our other studies of deep-sequencing analysis, we also found that some passenger strands were not degraded and acted as tumour suppressors (Matsushita et al, 2016; Yonemori et al, 2016). Thus, deep-sequencing analysis seemed to be superior to array- and PCR-based methods and is likely to become the gold standard for comprehensive miRNA analysis in cancer genomics (Enokida et al, 2016). The molecular mechanism of how miR-199 family members are downregulated in BC remains unclear. However, a recent study demonstrated that the RNA-binding protein HuR, also known as ELAVL1 suppresses the maturation of miR-199a in hepatocellular carcinoma (Zhang et al, 2015). ELAVL1 mRNA expression level was significantly upregulated in BC samples compared with normal bladder samples in TCGA database (Supplementary Figure 3A). Moreover, there was a significant negative correlation between miR-199 family and ELAVL1 expression (Supplementary Figure 3B). These data suggested that ELAVL1 expression might be responsible for the downregulation of miR-199 family in BC. Further studies are necessary to determine this mechanism.
miR-199 family members have been shown to have strong anticancer effects in several types of cancer, including breast cancer, colorectal cancer, and thyroid cancer, through the regulation of oncogene (Hu et al, 2014; Li et al, 2015; Sun et al, 2016); however, few studies have examined these miRNAs in BC. Some few previous studies have suggested that miR-199a-5p functions as a tumour suppressor in BC. Song et al (2015) reported that miR-199a-5p functions as a tumour suppressor by regulating MLK3/NF-κB pathway. However, the roles of miR-199a-3p and miR-199b-3p/-5p in BC remain unknown. Thus, in this study, we revealed, for the first time, that miR-199 family members (miR-199a-3p/-5p and miR-199b-3p/-5p) functioned as tumour-suppressive miRNAs in BC. Interestingly, several previous reports showed that elevated miR-199a levels were associated with improved survival in patients with diffuse large B-cell lymphoma (Troppan et al, 2015) and patients with breast cancer (Li et al, 2016b). Furthermore, another report demonstrated that a panel of eight miRNAs, including miR-199a, may be a useful biomarker for predicting survival in BC (Zhou et al, 2015). Notably, in our present study using the TCGA data set, we revealed that patients with low expression of miR-199a or miR-199b exhibited poorer overall survival than patients with high expression of these miRNAs. Therefore, we speculated that these miRNAs may be effective prognostic markers in patients with BC. However, despite the observed significant correlations between miR-199 family members and survival, our data did not reveal any significant correlations between ITGA3 and survival. This discrepant observation may be explained by the fact that miR-199 family members have many target genes that influence patient prognosis in addition to ITGA3. Therefore, there may not be any correlations between ITGA3 expression and survival in patients with BC. Future studies are needed to identify other target genes of miR-199 family members.
We performed in silico analysis and finally obtained 10 candidate target genes of miR-199 family. E2F3 was at the top of the list (Supplementary Table 4), and TCGA database also showed higher E2F3 mRNA expression in BC samples than that of normal bladder samples (Supplementary Figure 4A). In general, E2F3 is critical for G1/S transition and has major roles in regulating tumour cell proliferation (Humbert et al, 2000). However, in this study, we could not find strong efficacy of inhibiting cell proliferation in the miR-199s transfectants as compared with that of inhibiting cell migration or invasion. In terms of KLK3 and SLC2A1, TCGA database showed no significant differences in their mRNA expressions between BC and normal bladder samples. (Supplementary Figures 4B and C). Therefore, we focused on ITGA3 as the candidate target of miR-199 family even though it was the fourth position on the list.
Nonetheless, our findings also demonstrated that ITGA3 has important roles in BC cell progression and may be a molecular target for BC treatment. Integrins are heterodimeric transmembrane receptors that mediate adhesion to the extracellular matrix (ECM) and immunoglobulin superfamily molecules (Desgrosellier and Cheresh, 2010). Integrin heterodimers are formed by the combination of α- and β-subunit. Many different integrin heterodimers can be expressed on a single cell, and each can interact with multiple intracellular signalling cascades (Goodman and Picard, 2012). Integrin α3 and β1-subunits have been identified as laminin-binding receptors, for example, laminin-5 and laminin-10/-11 (Kreidberg et al, 1996). Extracellular matrix proteins, such as collagen, laminin, and fibronectin, regulate tissue homeostasis, organ development, inflammation, and diseases, such as cancer (Miyamoto et al, 2016). Integrins are essential for cell migration and invasion, because they directly mediate adhesion to these ECM proteins (Hood and Cheresh, 2002). Therefore, aberrant expression of ITGA3 results in promoting cancer cell migration and invasion. The Cancer Genome Atlas database analysis revealed that ITGA3 mRNA expression in BC was significantly upregulated. However, mRNA expression of integrin β1 (ITGB1) that compose integrin α3β1 heterodimer with ITGA3 was not significantly changed between BCs and normal bladder tissues (Supplementary Figure 4D). Our speculation is that ITGA3 composes integrin α3β1 heterodimer only with ITGB1. On the other hand, ITGB1 composes many integrin heterodimers with integrin α1–2, α4–11, and αV as well as ITGA3 (Jin and Varner, 2004). The Cancer Genome Atlas database revealed that the mRNA expression levels of these integrin α-subunits, except for ITGA3, were either not significantly changed or significantly downregulated in BCs compared with normal bladder tissues (Supplementary Figure 5). These facts imply that total expression of ITGB1 in BC cells might balance out because of the low expression of other integrin α-subunits that bind to ITGB1. Overexpression of ITGA3 has been reported in various human cancers, such as prostate cancer, breast cancer, glioma, and oral squamous cell carcinoma (Ghosh et al, 2006; Nakada et al, 2013; Shirakihara et al, 2013; Kurozumi et al, 2016). Ghosh et al (2006) showed that decreased integrin α3β1 expression was consistent with lower invasive tumour behaviour. Moreover, several studies have shown that ITGA3 is involved in cancer progression, cell migration, metastasis, and invasiveness in BC (Litynska et al, 2002; Mitsuzuka et al, 2005; Pochec et al, 2006; Behnsawy et al, 2011; Li et al, 2014, 2016a). Li et al (2014, 2016a) reported that aberrantly glycosylated integrin α3β1 is a new biomarker of BC and that a monoclonal antibody against this integrin heterodimer has potent antitumour activities in BC. Additionally, ITGA3 has been suggested to have a major role in modulation of other integrin receptors in BC (Litynska et al, 2002). Interestingly, another report showed that ITGA3 expression was significantly associated with the incidence of intravesical recurrence after TURBT (Behnsawy et al, 2011). A recent report showed that tumour exosome integrins may be good biomarkers to predict organ-specific cancer metastasis (Hoshino et al, 2015). Thus, further studies are needed to determine the cancer molecular networks associated with integrins.
Conclusions
Downregulation of dual-stranded miR-199 family members (miR-199a-3p/-5p and miR-199b-3p/-5p) was frequently observed in BC cells, and these miRNAs significantly inhibited cancer cell migration and invasion. To the best of our knowledge, this is the first report demonstrating that tumour-suppressive miR-199a-3p/-5p and miR-199b-3p/-5p directly regulated ITGA3 and may be good prognostic markers for survival in patients with BC. The discovery of molecular targets mediated by tumour-suppressive miRNAs provides important insights into potential mechanisms, new therapeutics, and new biomarkers in BC.
Acknowledgments
We thank Mutsumi Miyazaki for excellent laboratory assistance. This study was supported by the KAKENHI (B) 26293354 and (C) 10642613.
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
The authors declare no conflict of interest.
Supplementary Material
References
- Antoni S, Ferlay J, Soerjomataram I, Znaor A, Jemal A, Bray F (2017) Bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol 71(1): 96–108. [DOI] [PubMed] [Google Scholar]
- Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116(2): 281–297. [DOI] [PubMed] [Google Scholar]
- Behnsawy HM, Miyake H, Abdalla MA, Sayed MA, Ahmed Ael F, Fujisawa M (2011) Expression of integrin proteins in non-muscle-invasive bladder cancer: significance of intravesical recurrence after transurethral resection. BJU Int 107(2): 240–246. [DOI] [PubMed] [Google Scholar]
- Bellmunt J, von der Maase H, Mead GM, Skoneczna I, De Santis M, Daugaard G, Boehle A, Chevreau C, Paz-Ares L, Laufman LR, Winquist E, Raghavan D, Marreaud S, Collette S, Sylvester R, de Wit R (2012) Randomized phase III study comparing paclitaxel/cisplatin/gemcitabine and gemcitabine/cisplatin in patients with locally advanced or metastatic urothelial cancer without prior systemic therapy: EORTC Intergroup Study 30987. J Clin Oncol 30(10): 1107–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research N (2014) Comprehensive molecular characterization of urothelial bladder carcinoma. Nature 507(7492): 315–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carthew RW, Sontheimer EJ (2009) Origins and mechanisms of miRNAs and siRNAs. Cell 136(4): 642–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, Jacobsen A, Byrne CJ, Heuer ML, Larsson E, Antipin Y, Reva B, Goldberg AP, Sander C, Schultz N (2012) The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov 2(5): 401–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YH, Wang SQ, Wu XL, Shen M, Chen ZG, Chen XG, Liu YX, Zhu XL, Guo F, Duan XZ, Han XC, Tao ZH (2013) Characterization of microRNAs expression profiling in one group of Chinese urothelial cell carcinoma identified by Solexa sequencing. Urol Oncol 31(2): 219–227. [DOI] [PubMed] [Google Scholar]
- Chendrimada TP, Finn KJ, Ji X, Baillat D, Gregory RI, Liebhaber SA, Pasquinelli AE, Shiekhattar R (2007) MicroRNA silencing through RISC recruitment of eIF6. Nature 447(7146): 823–828. [DOI] [PubMed] [Google Scholar]
- Croce CM (2009) Causes and consequences of microRNA dysregulation in cancer. Nat Rev Genet 10(10): 704–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Melker AA, Sterk LM, Delwel GO, Fles DL, Daams H, Weening JJ, Sonnenberg A (1997) The A and B variants of the alpha 3 integrin subunit: tissue distribution and functional characterization. Lab Invest 76(4): 547–563. [PubMed] [Google Scholar]
- De Santis M, Bellmunt J, Mead G, Kerst JM, Leahy M, Maroto P, Gil T, Marreaud S, Daugaard G, Skoneczna I, Collette S, Lorent J, de Wit R, Sylvester R (2012) Randomized phase II/III trial assessing gemcitabine/carboplatin and methotrexate/carboplatin/vinblastine in patients with advanced urothelial cancer who are unfit for cisplatin-based chemotherapy: EORTC study 30986. J Clin Oncol 30(2): 191–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desgrosellier JS, Cheresh DA (2010) Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer 10(1): 9–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Leva G, Croce CM (2010) Roles of small RNAs in tumor formation. Trends Mol Med 16(6): 257–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enokida H, Yoshino H, Matsushita R, Nakagawa M (2016) The role of microRNAs in bladder cancer. Investig Clin Urol 57(Suppl 1): S60–S76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman RC, Farh KK, Burge CB, Bartel DP (2009) Most mammalian mRNAs are conserved targets of microRNAs. Genome Res 19(1): 92–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, Cerami E, Sander C, Schultz N (2013) Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6(269): pl1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh S, Johnson JJ, Sen R, Mukhopadhyay S, Liu Y, Zhang F, Wei Y, Chapman HA, Stack MS (2006) Functional relevance of urinary-type plasminogen activator receptor-alpha3beta1 integrin association in proteinase regulatory pathways. J Biol Chem 281(19): 13021–13029. [DOI] [PubMed] [Google Scholar]
- Goodman SL, Picard M (2012) Integrins as therapeutic targets. Trends Pharmacol Sci 33(7): 405–412. [DOI] [PubMed] [Google Scholar]
- Han Y, Chen J, Zhao X, Liang C, Wang Y, Sun L, Jiang Z, Zhang Z, Yang R, Chen J, Li Z, Tang A, Li X, Ye J, Guan Z, Gui Y, Cai Z (2011) MicroRNA expression signatures of bladder cancer revealed by deep sequencing. PLoS ONE 6(3): e18286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood JD, Cheresh DA (2002) Role of integrins in cell invasion and migration. Nat Rev Cancer 2(2): 91–100. [DOI] [PubMed] [Google Scholar]
- Hoshino A, Costa-Silva B, Shen TL, Rodrigues G, Hashimoto A, Tesic Mark M, Molina H, Kohsaka S, Di Giannatale A, Ceder S, Singh S, Williams C, Soplop N, Uryu K, Pharmer L, King T, Bojmar L, Davies AE, Ararso Y, Zhang T, Zhang H, Hernandez J, Weiss JM, Dumont-Cole VD, Kramer K, Wexler LH, Narendran A, Schwartz GK, Healey JH, Sandstrom P, Labori KJ, Kure EH, Grandgenett PM, Hollingsworth MA, de Sousa M, Kaur S, Jain M, Mallya K, Batra SK, Jarnagin WR, Brady MS, Fodstad O, Muller V, Pantel K, Minn AJ, Bissell MJ, Garcia BA, Kang Y, Rajasekhar VK, Ghajar CM, Matei I, Peinado H, Bromberg J, Lyden D (2015) Tumour exosome integrins determine organotropic metastasis. Nature 527(7578): 329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y, Liu J, Jiang B, Chen J, Fu Z, Bai F, Jiang J, Tang Z (2014) MiR-199a-5p loss up-regulated DDR1 aggravated colorectal cancer by activating epithelial-to-mesenchymal transition related signaling. Dig Dis Sci 59(9): 2163–2172. [DOI] [PubMed] [Google Scholar]
- Humbert PO, Verona R, Trimarchi JM, Rogers C, Dandapani S, Lees JA (2000) E2f3 is critical for normal cellular proliferation. Genes Dev 14(6): 690–703. [PMC free article] [PubMed] [Google Scholar]
- Ichimi T, Enokida H, Okuno Y, Kunimoto R, Chiyomaru T, Kawamoto K, Kawahara K, Toki K, Kawakami K, Nishiyama K, Tsujimoto G, Nakagawa M, Seki N (2009) Identification of novel microRNA targets based on microRNA signatures in bladder cancer. Int J Cancer 125(2): 345–352. [DOI] [PubMed] [Google Scholar]
- Itesako T, Seki N, Yoshino H, Chiyomaru T, Yamasaki T, Hidaka H, Yonezawa T, Nohata N, Kinoshita T, Nakagawa M, Enokida H (2014) The microRNA expression signature of bladder cancer by deep sequencing: the functional significance of the miR-195/497 cluster. PLoS ONE 9(2): e84311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H, Varner J (2004) Integrins: roles in cancer development and as treatment targets. Br J Cancer 90(3): 561–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman DS, Shipley WU, Feldman AS (2009) Bladder cancer. Lancet (London, England) 374(9685): 239–249. [DOI] [PubMed] [Google Scholar]
- Kreidberg JA, Donovan MJ, Goldstein SL, Rennke H, Shepherd K, Jones RC, Jaenisch R (1996) Alpha 3 beta 1 integrin has a crucial role in kidney and lung organogenesis. Development (Cambridge, England) 122(11): 3537–3547. [DOI] [PubMed] [Google Scholar]
- Kurozumi A, Goto Y, Matsushita R, Fukumoto I, Kato M, Nishikawa R, Sakamoto S, Enokida H, Nakagawa M, Ichikawa T, Seki N (2016) Tumor-suppressive microRNA-223 inhibits cancer cell migration and invasion by targeting ITGA3/ITGB1 signaling in prostate cancer. Cancer Sci 107(1): 84–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B, Dewey CN (2011) RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinformatics 12: 323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Du Y, Yang Z, He L, Wang Y, Hao L, Ding M, Yan R, Wang J, Fan Z (2016. a) GALNT1-mediated glycosylation and activation of sonic hedgehog signaling maintains the self-renewal and tumor-initiating capacity of bladder cancer stem cells. Cancer Res 76(5): 1273–1283. [DOI] [PubMed] [Google Scholar]
- Li SQ, Wang ZH, Mi XG, Liu L, Tan Y (2015) MiR-199a/b-3p suppresses migration and invasion of breast cancer cells by downregulating PAK4/MEK/ERK signaling pathway. IUBMB Life 67(10): 768–777. [DOI] [PubMed] [Google Scholar]
- Li W, Wang H, Zhang J, Zhai L, Chen W, Zhao C (2016. b) miR-199a-5p regulates beta1 integrin through Ets-1 to suppress invasion in breast cancer. Cancer Sci 107(7): 916–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Yang Z, Du Y, Tang H, Chen J, Hu D, Fan Z (2014) BCMab1, a monoclonal antibody against aberrantly glycosylated integrin alpha3beta1, has potent antitumor activity of bladder cancer in vivo. Clin Cancer Res 20(15): 4001–4013. [DOI] [PubMed] [Google Scholar]
- Litynska A, Przybylo M, Pochec E, Laidler P (2002) Adhesion properties of human bladder cell lines with extracellular matrix components: the role of integrins and glycosylation. Acta Biochim Pol 49(3): 643–650. [PubMed] [Google Scholar]
- Matsushita R, Seki N, Chiyomaru T, Inoguchi S, Ishihara T, Goto Y, Nishikawa R, Mataki H, Tatarano S, Itesako T, Nakagawa M, Enokida H (2015) Tumour-suppressive microRNA-144-5p directly targets CCNE1/2 as potential prognostic markers in bladder cancer. Br J Cancer 113(2): 282–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsushita R, Yoshino H, Enokida H, Goto Y, Miyamoto K, Yonemori M, Inoguchi S, Nakagawa M, Seki N (2016) Regulation of UHRF1 by dual-strand tumor-suppressor microRNA-145 (miR-145-5p and miR-145-3p): inhibition of bladder cancer cell aggressiveness. Oncotarget 7(19): 28460–28487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, Stein KD, Alteri R, Jemal A (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66(4): 271–289. [DOI] [PubMed] [Google Scholar]
- Mitsuzuka K, Handa K, Satoh M, Arai Y, Hakomori S (2005) A specific microdomain (‘glycosynapse 3') controls phenotypic conversion and reversion of bladder cancer cells through GM3-mediated interaction of alpha3beta1 integrin with CD9. J Biol Chem 280(42): 35545–35553. [DOI] [PubMed] [Google Scholar]
- Miyamoto K, Seki N, Matsushita R, Yonemori M, Yoshino H, Nakagawa M, Enokida H (2016) Tumour-suppressive miRNA-26a-5p and miR-26b-5p inhibit cell aggressiveness by regulating PLOD2 in bladder cancer. Br J Cancer 115(3): 354–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakada M, Nambu E, Furuyama N, Yoshida Y, Takino T, Hayashi Y, Sato H, Sai Y, Tsuji T, Miyamoto KI, Hirao A, Hamada JI (2013) Integrin alpha3 is overexpressed in glioma stem-like cells and promotes invasion. Br J Cancer 108(12): 2516–2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson KM, Weiss GJ (2008) MicroRNAs and cancer: past, present, and potential future. Mol Cancer Ther 7(12): 3655–3660. [DOI] [PubMed] [Google Scholar]
- Pochec E, Litynska A, Bubka M, Amoresano A, Casbarra A (2006) Characterization of the oligosaccharide component of alpha3beta1 integrin from human bladder carcinoma cell line T24 and its role in adhesion and migration. Eur J Cell Biol 85(1): 47–57. [DOI] [PubMed] [Google Scholar]
- Shirakihara T, Kawasaki T, Fukagawa A, Semba K, Sakai R, Miyazono K, Miyazawa K, Saitoh M (2013) Identification of integrin alpha3 as a molecular marker of cells undergoing epithelial–mesenchymal transition and of cancer cells with aggressive phenotypes. Cancer Sci 104(9): 1189–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1): 7–30. [DOI] [PubMed] [Google Scholar]
- Sobin LH, Compton CC (2010) TNM seventh edition: what's new, what's changed: communication from the International Union Against Cancer and the American Joint Committee on Cancer. Cancer 116(22): 5336–5339. [DOI] [PubMed] [Google Scholar]
- Song T, Zhang X, Yang G, Song Y, Cai W (2015) Decrement of miR-199a-5p contributes to the tumorigenesis of bladder urothelial carcinoma by regulating MLK3/NF-kappaB pathway. Am J Transl Res 7(12): 2786–2794. [PMC free article] [PubMed] [Google Scholar]
- Sternberg CN, Bellmunt J, Sonpavde G, Siefker-Radtke AO, Stadler WM, Bajorin DF, Dreicer R, George DJ, Milowsky MI, Theodorescu D, Vaughn DJ, Galsky MD, Soloway MS, Quinn DI (2013) ICUD-EAU International Consultation on Bladder Cancer 2012: chemotherapy for urothelial carcinoma-neoadjuvant and adjuvant settings. Eur Urol 63(1): 58–66. [DOI] [PubMed] [Google Scholar]
- Su SF, Chang YW, Andreu-Vieyra C, Fang JY, Yang Z, Han B, Lee AS, Liang G (2013) miR-30d, miR-181a and miR-199a-5p cooperatively suppress the endoplasmic reticulum chaperone and signaling regulator GRP78 in cancer. Oncogene 32(39): 4694–4701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun D, Han S, Liu C, Zhou R, Sun W, Zhang Z, Qu J (2016) Microrna-199a-5p functions as a tumor suppressor via suppressing connective tissue growth factor (CTGF) in follicular thyroid carcinoma. Med Sci Monit 22: 1210–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatarano S, Chiyomaru T, Kawakami K, Enokida H, Yoshino H, Hidaka H, Yamasaki T, Kawahara K, Nishiyama K, Seki N, Nakagawa M (2011) miR-218 on the genomic loss region of chromosome 4p15.31 functions as a tumor suppressor in bladder cancer. Int J Oncol 39(1): 13–21. [DOI] [PubMed] [Google Scholar]
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2): 87–108. [DOI] [PubMed] [Google Scholar]
- Troppan K, Wenzl K, Pichler M, Pursche B, Schwarzenbacher D, Feichtinger J, Thallinger GG, Beham-Schmid C, Neumeister P, Deutsch A (2015) miR-199a and miR-497 are associated with better overall survival due to increased chemosensitivity in diffuse large B-cell lymphoma patients. Int J Mol Sci 16(8): 18077–18095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonemori M, Seki N, Yoshino H, Matsushita R, Miyamoto K, Nakagawa M, Enokida H (2016) Dual tumor-suppressors miR-139-5p and miR-139-3p targeting matrix metalloprotease 11 in bladder cancer. Cancer Sci 107(9): 1233–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshino H, Chiyomaru T, Enokida H, Kawakami K, Tatarano S, Nishiyama K, Nohata N, Seki N, Nakagawa M (2011) The tumour-suppressive function of miR-1 and miR-133a targeting TAGLN2 in bladder cancer. Br J Cancer 104(5): 808–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshino H, Enokida H, Itesako T, Kojima S, Kinoshita T, Tatarano S, Chiyomaru T, Nakagawa M, Seki N (2013. a) Tumor-suppressive microRNA-143/145 cluster targets hexokinase-2 in renal cell carcinoma. Cancer Sci 104(12): 1567–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshino H, Seki N, Itesako T, Chiyomaru T, Nakagawa M, Enokida H (2013. b) Aberrant expression of microRNAs in bladder cancer. Nat Rev Urol 10(7): 396–404. [DOI] [PubMed] [Google Scholar]
- Zhang LF, Lou JT, Lu MH, Gao C, Zhao S, Li B, Liang S, Li Y, Li D, Liu MF (2015) Suppression of miR-199a maturation by HuR is crucial for hypoxia-induced glycolytic switch in hepatocellular carcinoma. EMBO J 34(21): 2671–2685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H, Tang K, Xiao H, Zeng J, Guan W, Guo X, Xu H, Ye Z (2015) A panel of eight-miRNA signature as a potential biomarker for predicting survival in bladder cancer. J Exp Clin Cancer Res 34: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.