Abstract
Background
While developmental surveillance programs promote early identification of child developmental problems, evidence has indicated suboptimal uptake. This study aimed to identify predictors of developmental surveillance completion at 6 months postpartum.
Methods
Questionnaires were administered to the parents of 510 infants who were born in south western Sydney, Australia over a 22‐month period. Attendance for developmental screening and completion of the Parents' Evaluation of Developmental Status (PEDS) at 6 months postpartum were modelled separately using multivariable logistic regression.
Results
Developmental surveillance attendance was predicted by higher levels of maternal education, annual income and being informed about checks. PEDS completion at 6 months of age was predicted by higher income and being informed, as well as being married, employed, speaking English at home, full‐term birth and the professional status of the practitioner completing the check.
Conclusions
Barriers to developmental surveillance included low socioeconomic status, linguistic diversity and possible gaps in parental knowledge and professional education. Developmental surveillance rates may be increased by the addition of targeted parental and professional support within current universal frameworks.
Keywords: cultural and linguistic diversity, developmental surveillance, Parents' Evaluation of Developmental Status, socioeconomic disadvantage
Background
Child developmental problems represent an ever increasing health and economic concern (Jarbrink et al. 2003; Matson & Kozlowski 2011; Lavelle et al. 2014). While early intervention may reduce the impact of developmental disorders (McConachie & Diggle 2007; Rogers & Vismara 2008; Howlin et al. 2009; Einfeld et al. 2013), timely identification of children who could benefit remains a significant challenge (Chung et al. 2006; Eapen et al. 2014).
Developmental surveillance (DS) is a means of identifying children at risk of developmental problems and promoting early diagnosis (Committee on Children With Disabilities 2001; National Health and Medical Research Council 2002). In New South Wales (NSW), regular child health screening commences at 1–4 weeks postpartum (Ministry of Health‚ New South Wales 2013; Eapen et al. 2014), and is usually provided by a Child and Family Health Nurse or general practitioner (GP). The DS schedule is contained in the child's Personal Health Record (PHR), given to parents at the birth of their child, and verbal information about DS is provided opportunistically during the perinatal period.
The Parents' Evaluation of Developmental Status (PEDS) is included in the PHR at each surveillance ‘check’ from 6 months to 4 years of age, and is also available in multiple languages online (Glascoe 1999; Ministry of Health‚ New South Wales). This brief 10‐question screening tool aids detection of developmental problems by exploring parents' concerns about their child's development (Glascoe 2006; Schonwald et al. 2009). It should be completed by parents prior to each scheduled ‘check’ or otherwise the questions should be asked during the check and filled out in the PHR.
Despite the availability of DS programs, their uptake is suboptimal. The 2009–2010 report on child health from the Centre for Epidemiology and Research in NSW (2008) found that 50% of children aged less than 12 months had attended an early childhood health centre, and only 15% of non‐attendees reported use of another services. Between 1 and 4 years of age, attendance decreased to 33%, with similar rates observed internationally (Chung et al. 2006).
While previous research has identified numerous barriers to universal healthcare uptake, little is known about the barriers specific to DS. Risk factors for reduced universal healthcare uptake include low socioeconomic status (SES)(Comino & Harris 2003; Fort Harris et al. 2004), and cultural and linguistic diversity (Carbone et al. 2004; Fort Harris, Harris, & Roland; Murray & Skull 2005; Schyve 2007; Woolfenden et al. 2014), which represent key potential barriers to DS in ethnically diverse and economically disadvantaged regions like south western Sydney (Sydney South West Area Health Service 2005).
The present study aimed to identify predictors of non‐attendance at 6‐month DS, and predictors for non‐completion of the PEDS, using the Andersen Behavioural Model of Health Service Use as a framework (Andersen 1995; Andersen & Davidson 2007). This model has been extensively applied in studies of health service use (Babitsch et al. 2012; Woolfenden et al. 2014).
Methods
Participants and ethical approval
Participants comprised the parents of 510 infants born in south western Sydney between October 2011 and July 2013. These were a subsample of a birth cohort recruited for the ‘Watch Me Grow’ study, a mixed methods study of developmental risk and surveillance in NSW. Recruitment methods have been detailed elsewhere (Eapen et al. 2014; Woolfenden et al. 2016). Participants who had completed the first two study components (baseline and 6‐month follow‐up) at the time of analysis were selected for inclusion. Retention at 6 months was 75%, with 3% declining to continue and 22% unreachable by telephone. While largely representative of the culturally diverse and economically disadvantaged population of south western Sydney, the ‘Watch Me Grow’ cohort demonstrated higher instances of specific risk factors for developmental problems (Woolfenden et al. 2016), making this sample ideal for the examination of risk factors for DS uptake. Ethical approval was granted by the Human Research Ethics Committees of the University of New South Wales and South Western Sydney Local Health District.
Measurement tools
Sociodemographic and health service use information was obtained using a baseline questionnaire at birth and a follow‐up telephone interview at 7 to 12 months postpartum. Both questionnaires were developed in collaboration with local healthcare providers, and incorporated questions from other Australian birth cohort studies (Nicholson & Sanson 2003; Comino et al. 2010; The SEARCH Investigators 2010). For participants who could not complete the baseline questionnaire during recruitment, it was completed retrospectively during the follow‐up interview (n = 77). As part of this interview, the 6‐month PEDS was completed with the parent if answers had not been recorded previously in the PHR.
Statistical analyses
All analyses were conducted in SPSS version 22. Group differences were examined using the chi‐square and non‐parametric Mann–Whitney U tests (because of non‐normal distribution).
Single predictor binary logistic regression models were used to investigate sociodemographic and service use characteristics associated with two separate dependant variables: attendance of the 6‐month DS and completion of 6‐month PEDS in the PHR for those who attended a well child check. All independent variables were selected from one of the two study questionnaires on the basis of previous research highlighting their value in predicting healthcare uptake. These factors were semantically categorised according to the Andersen model (Tables 1 and 2). Multi‐categorical variables were dichotomised based on group differences from previous research, or socially and economically relevant groupings. Assuming equal sized groups, we had at least 80% power (with alpha of .05) to detect differences in prevalence between 10 and 15%. For each dependent variable, any factor with p < .25 in a single predictor logistic regression model was included in a multivariable logistic regression model. The final model was determined using the backward selection method, and discriminatory power was measured by the coefficient of discrimination statistic (Tjur 2009).
Table 1.
Attendance rates at 6‐month developmental screening and completion of 6‐month Parents' Evaluation of Developmental Status (for those who attended screening) by Andersen Model Factor and categorical group
| Six‐month Developmental Surveillance attendance | Six‐month Parents' Evaluation of Developmental Status completion | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Andersen Model Factor | Characteristic | N | Missing | n | % | p | n | % | p | |
| Predisposing characteristics | ||||||||||
| Gender (child) | Male | 239 | 0 | 205 | 86 | .92 | 91 | 48 | .27 | |
| Female | 271 | 230 | 86 | 116 | 54 | |||||
| Marital status (mother) | Married | 406 | 0 | 355 | 88 | <.01 | 164 | 50 | .29 | |
| Not married | 104 | 80 | 78 | 43 | 57 | |||||
| Have second parent (child) | Yes | 480 | 3 | 412 | 86 | .18 | 199 | 52 | .06 | |
| No | 27 | 20 | 77 | 5 | 28 | |||||
| Country of birth (mother) | Australia | 224 | 3 | 192 | 86 | .90 | 109 | 61 | <.01 | |
| Other | 283 | 240 | 86 | 97 | 44 | |||||
| Country of birth (father) | Australia | 208 | 23 | 177 | 85 | .57 | 101 | 61 | <.01 | |
| Other | 278 | 239 | 87 | 99 | 45 | |||||
| Education level (mother) | Tertiary | 332 | 5 | 297 | 90 | <.01 | 146 | 53 | .23 | |
| Below Tertiary | 173 | 133 | 78 | 59 | 47 | |||||
| Education level (father) | Tertiary | 309 | 30 | 271 | 88 | .19 | 129 | 51 | .73 | |
| Below Tertiary | 170 | 142 | 84 | 70 | 53 | |||||
| Employment status (mother) | Employed | 323 | 4 | 288 | 89 | <.01 | 156 | 58 | <.01 | |
| Unemployed | 183 | 144 | 80 | 50 | 37 | |||||
| Employment status (father) | Employed | 483 | 26 | 373 | 86 | .84 | 185 | 53 | .15 | |
| Unemployed | 27 | 41 | 87 | 15 | 41 | |||||
| Number of children in family | Single | 297 | 5 | 241 | 82 | <.01 | 106 | 48 | .10 | |
| Multiple | 208 | 189 | 91 | 99 | 56 | |||||
| English spoken at home | Yes | 345 | 1 | 297 | 87 | .40 | 155 | 56 | <.01 | |
| Never | 164 | 137 | 84 | 51 | 41 | |||||
| Enabling resources | ||||||||||
| Annual income | ≥$25 000 | 396 | 45 | 351 | 89 | <.01 | 178 | 54 | <.01 | |
| <$25 000 | 69 | 46 | 68 | 12 | 29 | |||||
| Income covers costs | Yes | 461 | 13 | 398 | 87 | .04 | 197 | 53 | .02 | |
| No | 36 | 26 | 74 | 7 | 28 | |||||
| Six‐month immunisation complete | Yes | 487 | 4 | 416 | 86 | .38 | 200 | 52 | .06 | |
| No | 19 | 15 | 79 | 3 | 23 | |||||
| Perceived support | Get enough | 433 | 21 | 364 | 85 | .22 | 179 | 33 | .01 | |
| Don't get enough | 56 | 51 | 91 | 16 | 53 | |||||
| Informed about developmental surveillance | Yes | 235 | 32 | 212 | 90 | <.01 | 120 | 61 | <.01 | |
| No | 243 | 195 | 82 | 77 | 42 | |||||
| Practitioner who completed 6‐month screening | Child and Family Health Nurse | 121 | 0 | — | — | — | 94 | 84 | <.01 | |
| Other | 314 | — | — | 113 | 39 | |||||
| Need | ||||||||||
| Physical health problems in first 6 months (child) | Yes | 103 | 7 | 90 | 87 | .60 | 46 | 54 | .45 | |
| No | 400 | 338 | 85 | 156 | 49 | |||||
| Health problems pre pregnancy (mother) | Yes | 68 | 0 | 62 | 91 | .19 | 36 | 64 | .04 | |
| No | 442 | 373 | 85 | 171 | 49 | |||||
| Health problems during pregnancy (mother) | Yes | 136 | 1 | 112 | 84 | .36 | 59 | 57 | .16 | |
| No | 373 | 322 | 87 | 148 | 49 | |||||
| Premature birth (child) | Full‐term | 473 | 0 | 402 | 85 | .16 | 193 | 52 | .30 | |
| Premature | 37 | 33 | 94 | 14 | 42 | |||||
| Family history of psychosocial problems | Yes | 81 | 5 | 70 | 86 | .87 | 40 | 61 | .09 | |
| No | 424 | 360 | 86 | 164 | 49 | |||||
| Smoked during pregnancy (mother) | Yes | 43 | 4 | 34 | 79 | .19 | 16 | 50 | .90 | |
| No | 463 | 397 | 86 | 189 | 51 | |||||
| Alcohol consumption during pregnancy (mother) | Yes | 22 | 4 | 19 | 86 | .94 | 10 | 59 | .52 | |
| No | 484 | 412 | 86 | 195 | 51 | |||||
| Breastfed after birth | Yes | 455 | 0 | 394 | 87 | .03 | 186 | 51 | .72 | |
| No | 55 | 41 | 76 | 21 | 54 | |||||
Table 2.
Attendance rates at 6‐month developmental screening and completion of 6‐month Parents' Evaluation of Developmental Status (for those who attended screening) by Andersen Model Factor for continuous predictors
| P values | ||||||
|---|---|---|---|---|---|---|
| Andersen Model Factor | Characteristic | Missing | Median | Range | Six‐month Developmental Surveillance attendance | Six‐month Parents' Evaluation of Developmental Status completion |
| Predisposing characteristics | ||||||
| Mother's age (years) | 3 | 30.0 | 13 – 46 | .10 | .64 | |
| Father's age (years) | 28 | 33.5 | 16 – 67 | .42 | .07 | |
| Number of sources for child development information | 4 | 3.0 | 1 – 14 | <.01 | <.01 | |
| Need | ||||||
| Number of Parents' Evaluation of Developmental Status concerns | 28 | 0.0 | 0 – 8 | .83 | <.01 | |
| Child birth weight (g) | 1 | 3335.0 | 838 – 4880 | .19 | .85 | |
Results
Sample characteristics
Tables 1 and 2 provide the distribution and simple logistic regression results for all factors. The majority of parents were married, born overseas, educated above secondary level and employed at baseline. English was never spoken at home for 32% of the sample, and 15% reported an annual household income below the poverty line (<$25 000). DS checks were completed primarily by a GP (65%), a Child and Family Health Nurse (28%) or a paediatrician (4%). Only 46% of parents reported being told about DS checks.
Attendance for 6‐month Developmental Surveillance
For the total sample, the 6‐month DS attendance rate was 85% (Table 1). The final regression model included three significant predictors of attendance (Table 3), representing one predisposing characteristic and two enabling resources (Fig. 1). Increased odds of DS attendance were observed for mothers with a tertiary education (OR = 2.09, p = .02), families with an annual income over $25 000 (OR = 2.55, p = .02) and parents who were informed about DS (OR = 2.22, p = .01). The estimated coefficient of discrimination was D = .08 (Tjur 2009), suggesting low explanatory power.
Table 3.
Final multivariable logistic regression models
| Model | Predictor | OR | 95% CI |
|---|---|---|---|
| Six‐month Developmental Surveillance attendance | Maternal education (tertiary and above vs. below tertiary) | 2.09 | 1.11 – 3.94 |
| Annual income ($25 000 and above vs. below $25 000) | 2.56 | 1.15 – 5.66 | |
| Informed about developmental surveillance (informed vs. uninformed) | 2.22 | 1.18 – 4.2 | |
| Six‐month Parents' Evaluation of Developmental Status completion | Marital status (married vs. unmarried) | 2.17 | 1.02 – 4.64 |
| Maternal employment (employed vs. unemployed) | 3.09 | 1.71 – 5.61 | |
| English spoken at home (English vs. no English) | 2.06 | 1.13 – 3.77 | |
| Full‐term birth (full‐term vs. preterm) | 2.87 | 1.11 – 7.37 | |
| Professional who complete 6‐month check (Child and Family Health Nurse vs. other) | 8.12 | 4.04 – 16.34 | |
| Annual income ($25 000 and above vs. below $25 000) | 3.38 | 1.13 – 10.05 | |
| Informed about developmental surveillance (informed vs. uninformed) | 1.96 | 1.15 – 3.33 |
Figure 1.
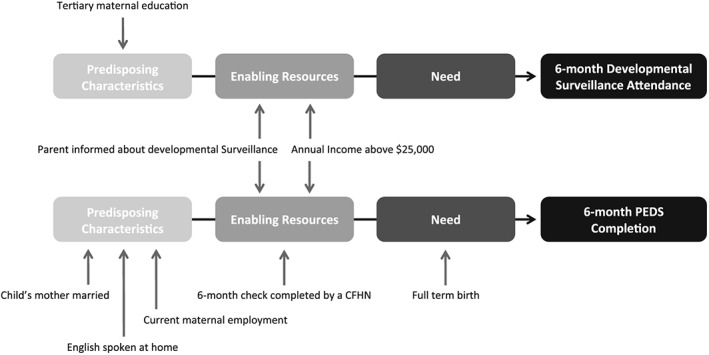
Andersen Behavioural Models of 6‐month developmental surveillance attendance and Parents' Evaluation of Developmental Status completion, with predictors based on final multivariable logistic regression models.
Completion of PEDS in the Personal Health Record
Amongst 6‐month DS attendees, 51% reported completion of the PEDS in the PHR (Table 1), with an additional 7% reporting that the PEDS questions were asked by a health practitioner but not recorded in the PHR. Seven factors were associated with increased PEDS completion in the final regression model (Table 3): mothers who were unmarried (OR = 2.17, p = .05) or unemployed (OR = 3.09, p < .01), English spoken at home (OR = 2.06, p = .02), annual income over $25 000 (OR = 3.38, p = .03), being informed of DS (OR = 1.96, p = .01), full‐term birth (OR = 2.87, p = .03) and Child and Family Health Nurse completing DS (OR = 8.12, p < .01). Within the Anderson Behavioural Model, these predictors represented three predisposing characteristics, one enabling resource and one need factor (Fig. 1). The estimated coefficient of discrimination was D = .28 (Tjur 2009), indicating low explanatory power.
Discussion
The rate of self‐reported DS attendance for a 6‐month check (85%) was more promising than the 65% reported by the Centre for Epidemiology and Research (2008); however, there was disparity between DS attendance and PEDS completion at 6 months (51%). It is possible that a separate PEDS form was used in some cases, as 7% of parents recalled the PEDS questions being asked when it was not filled out in the PHR. However, the issue of the remaining 42% of attendees with uncompleted PEDS requires further examination.
Predictors of increased DS attendance and PEDS completion included multiple factors previously identified as providing protection from child developmental problems (Najman et al. 1992; To et al. 2004). Families with an annual income over $25 000 were more likely to attend DS and have the PEDS recorded in the PHR, supporting previous reports of less universal healthcare service use amongst those of low SES (Fort Harris et al. 2004). In accordance with Comino and Harris (2003), tertiary maternal education predicted DS attendance, while significantly more PEDS forms were completed for employed mothers and children born at term. As low SES and preterm birth are well‐established predictors of developmental problems (Najman et al. 1992), these patterns of attendance and PEDS completion indicate the presence of the inverse care law (Tudor Hart 1971) with those at greatest developmental risk not accessing or receiving the recommended care. These findings demonstrate the importance of targeted solutions to support DS within these vulnerable populations.
Another potential target for improving DS uptake is parental awareness. While only 46% of parents reported being told about DS, this factor significantly increased attendance by 12% and PEDS completion by 19%. Increased information about DS and regular reminders of upcoming checks may provide a simple means of bolstering uptake.
While the strongest predictor of PEDS completion was having a Child and Family Health Nurse conduct the 6‐month developmental screen, the majority of DS (65%) was conducted by GPs. PEDS completion may therefore be increased by improving parental awareness of the Child and Family Health Nurse's role, and increasing access to standardised training in DS administration by all primary health professionals. This is supported by the work of Woolfenden et al. (2015) who found that one third of a sample of 277 NSW GPs and practice nurses felt that their training in childhood development was poor, and 90% desired further training.
The increased PEDS completion in English‐speaking households adds to the body of research suggesting cultural and linguistic barriers to universal healthcare uptake (Carbone et al. 2004; Fort Harris, Harris, & Roland; Woolfenden et al. 2014), and is pertinent to ethnically diverse areas. Expanding upon the methods of disseminating PHR translations may increase DS access within CALD populations.
Limitations and strengths
The possibility of recall bias for questionnaires completed retrospectively is a potential limitation (15%). Retention at 6 months was 75%, and it is possible that DS was higher in this sample because of factors associated with continued research engagement. Strengths of this research included sample diversity and the inclusion of low SES families who were broadly representative of the population of south western Sydney.
Conclusion
Recent advances have highlighted the benefit of programs aimed at early identification of children at developmental risk (Oberklaid et al. 2013). However, our findings indicate barriers to implementation, particularly within low SES and linguistically diverse populations. This research provides an argument and policy focus for universal access to programs promoting healthy child development along with targeted support commensurate with additional needs.
Key messages.
Child developmental problems present a significant health and economic concern.
Developmental surveillance programs aim to identify children at risk of developmental problems and lead to early and accurate diagnosis.
Socioeconomic disadvantage, linguistic barriers and gaps in parental knowledge and professional education contribute to suboptimal uptake of developmental surveillance.
A policy focus on the provision of targeted support within a universal framework may facilitate timely identification of children who could benefit from early intervention.
Funding
Funding for this project was provided by the National Health and Medical Research Council and the New South Wales Ministry of Health. In kind funding was provided by the University of New South Wales, La Trobe University, Sydney South West Area Health Service and Sydney Children's Hospital Network. Logistic support was provided by the Ingham Institute for Applied Medical Research.
Appendix A.
Overs, B. J. , Woolfenden, S. , Williams, K. , Jalaludin, B. , Axelsson, E. L. , Dissanayake, C. , Descallar, J. , Harvey, S. , Beasley, D. , Murphy, E. , Eapen, V. , and the ‘Watch Me Grow’ Study Group (2017) Predictors of developmental surveillance completion at six months of age in south western Sydney. Child: Care, Health and Development, 43: 307–315. doi: 10.1111/cch.12425.
See Appendix A.
Contributor Information
B. J. Overs, Email: bronwyn.overs@gmail.com
V. Eapen, Email: v.eapen@unsw.edu.au
References
- Andersen, R. & Davidson, P. L. (2007) Improving access to care in America: individual and contextual indicators In: Changing the U.S. Health Care System: Key Issues in Health Services Policy and Management (eds Andersen R., Rice T. H. & Kominski G. F.) (Eds.),, 3rd edn, pp. 3–32. Jossey‐Bass, San Francisco. [Google Scholar]
- Andersen, R. M. (1995) Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 36, 1–10. DOI:10.2307/2137284. [PubMed] [Google Scholar]
- Babitsch, B. , Gohl, D. , & von Lengerke, T. (2012). Re‐revisiting Andersen's Behavioral Model of Health Services Use: a systematic review of studies from 1998–2011. Psychosoc Med, 9, Doc11. doi: 10.3205/psm000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbone, S. , Fraser, A. , Ramburuth, R. , & Nelms, L. (2004). Breaking Cycles, Building Futures. Promoting inclusion of vulnerable families in antenatal and universal early childhood services: a report on the first three stages of the project. Retrieved 08/27/2014, from https://www.eduweb.vic.gov.au/edulibrary/public/beststart/ecs_breaking_cycles_best_start.pdf.
- Centre for Epidemiology and Research . (2008). 2005–2006 Report on Child Health from the New South Wales Population Health Survey. Retrieved 07/01/2015, from http://www.health.nsw.gov.au/surveys/child/Publications/hsc_0506.pdf.
- Chung, P. J. , Lee, T. C. , Morrison, J. L. & Schuster, M. A. (2006) Preventive care for children in the United States: quality and barriers. Annual Review of Public Health, 27, 491–515. DOI:10.1146/annurev.publhealth.27.021405.102155. [DOI] [PubMed] [Google Scholar]
- Comino, E. , Craig, P. , Harris, E. , McDermott, D. , Harris, M. , Henry, R. , Pulver, L. J. , Kemp, L. & Knight, J. (2010) The Gudaga Study: establishing an Aboriginal birth cohort in an urban community. Australian and New Zealand Journal of Public Health, 34, S9–17. [DOI] [PubMed] [Google Scholar]
- Comino, E. J. & Harris, E. (2003) Maternal and Infant Services: examination of access in a culturally diverse community. Journal of Paediatrics and Child Health, 39, 95–99. [DOI] [PubMed] [Google Scholar]
- Committee on Children With Disabilities (2001) Developmental surveillance and screening of infants and young children. Pediatrics, 108, 192–195. [DOI] [PubMed] [Google Scholar]
- Eapen, V. , Woolfenden, S. , Williams, K. , Jalaludin, B. , Dissanayake, C. , Axelsson, E. L. , Murphy, E. , Eastwood, J. , Descallar, J. , Beasley, D. , Crncec, R. , Short, K. , Silove, N. , Einfeld, S. & Prior, M. (2014) “Are you available for the next 18 months?”—methods and aims of a longitudinal birth cohort study investigating a universal developmental surveillance program: the ‘Watch Me Grow’ study. BMC Pediatrics, 14, 234 DOI:10.1186/1471-2431-14-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einfeld, S. L. , Tonge, B. J. & Clarke, K. S. (2013) Prevention and early intervention for behaviour problems in children with developmental disabilities. Current Opinion in Psychiatry, 26, 263–269. [DOI] [PubMed] [Google Scholar]
- Fort Harris, M. , Harris, E. & Roland, M. (2004) Access to primary health care: three challenges to equity. Australian Journal of Primary Health, 10, 21–29. [Google Scholar]
- Glascoe, F. P. (1999) Using parents' concerns to detect and address developmental and behavioral problems. Journal for Specialists in Pediatric Nursing, 4, 24–35. [DOI] [PubMed] [Google Scholar]
- Glascoe, F. P. (2006) If you don't ask, parents may not tell: noticing problems vs expressing concerns. Archives of Pediatrics & Adolescent Medicine, 160, 220–221. [DOI] [PubMed] [Google Scholar]
- Howlin, P. , Magiati, I. , Charman, T. & MacLean, J. W. E. (2009) Systematic review of early intensive behavioral interventions for children with autism. American Journal on Intellectual and Developmental Disabilities, 114, 23–41. [DOI] [PubMed] [Google Scholar]
- Jarbrink, K. , Fombonne, E. , Knapp, M. , Jarbrink, K. , Fombonne, E. & Knapp, M. (2003) Measuring the parental, service and cost impacts of children with autistic spectrum disorder: a pilot study. Journal of Autism and Developmental Disorders, 33, 395–402. [DOI] [PubMed] [Google Scholar]
- Lavelle, T. A. , Weinstein, M. C. , Newhouse, J. P. , Munir, K. , Kuhlthau, K. A. & Prosser, L. A. (2014) Economic burden of childhood autism spectrum disorders. Pediatrics. DOI:10.1542/peds.2013-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson, J. L. & Kozlowski, A. M. (2011) The increasing prevalence of autism spectrum disorders. Research in Autism Spectrum Disorders, 5, 418–425. [Google Scholar]
- McConachie, H. & Diggle, T. (2007) Parent implemented early intervention for young children with autism spectrum disorder: a systematic review. Journal of Evaluation in Clinical Practice, 13, 120–129. [DOI] [PubMed] [Google Scholar]
- Ministry of Health‚ New South Wales . (2013). Child personal health record (blue book) release of revised version 2012/2013. Retrieved 08/28/14, from http://www0.health.nsw.gov.au/policies/ib/2013/pdf/IB2013_028.pdf.
- Murray, S. B. & Skull, S. A. (2005) Hurdles to health: immigrant and refugee health care in Australia. Australian Health Review, 29, 25–29. [DOI] [PubMed] [Google Scholar]
- Najman, J. M. , Bor, W. , Morrison, J. , Andersen, M. & Williams, G. (1992) Child developmental delay and socio‐economic disadvantage in Australia: a longitudinal study. Social Science & Medicine, 34, 829–835. [DOI] [PubMed] [Google Scholar]
- National Health and Medical Research Council . (2002). Child Health Screening and Surveillance: a critical review of the evidence. Retrieved 08/26/2014, from https://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/ch42_child_health_screening_surveillance_131223.pdf.
- Nicholson, J. M. & Sanson, A. (2003) A new longitudinal study of the health and wellbeing of Australian children: how will it help? (Commentry). The Medical Journal of Australia, 178, 282–284. [DOI] [PubMed] [Google Scholar]
- Oberklaid, F. , Baird, G. , Blair, M. , Melhuish, E. & Hall, D. (2013) Children's health and development: approaches to early identification and intervention. Archives of Disease in Childhood, 98, 1008–1011. [DOI] [PubMed] [Google Scholar]
- Rogers, S. J. & Vismara, L. A. (2008) Evidence‐based comprehensive treatments for early autism. Journal of Clinical Child & Adolescent Psychology, 37, 8–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonwald, A. , Huntington, N. , Chan, E. , Risko, W. & Bridgemohan, C. (2009) Routine developmental screening implemented in urban primary care settings: more evidence of feasibility and effectiveness. Pediatrics, 123, 660–668. DOI:10.1542/peds.2007-2798. [DOI] [PubMed] [Google Scholar]
- Schyve, P. (2007) Language differences as a barrier to quality and safety in health care: the joint commission perspective. Journal of General Internal Medicine, 22, 360–361. DOI:10.1007/s11606-007-0365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sydney South West Area Health Service . (2005). A health profile of Sydney South West. Retrieved 08/28/2014, from http://www.sswahs.nsw.gov.au/agm/DemProfile.pdf
- The SEARCH Investigators (2010) The Study of Environment on Aboriginal Resilience and Child Health (SEARCH): study protocol. BMC Public Health, 10, 287 DOI:10.1186/1471-2458-10-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjur, T. (2009) Coefficients of determination in logistic regression models—a new proposal: the coefficient of discrimination. The American Statistician, 63, 366–372. [Google Scholar]
- To, T. , Guttmann, A. , Dick, P. T. , Rosenfield, J. D. , Parkin, P. C. , Tassoudji, M. , Vydykhan, T. N. , Cao, H. & Harris, J. K. (2004) Risk markers for poor developmental attainment in young children: results from a longitudinal national survey. Archives of Pediatrics & Adolescent Medicine, 158, 643–649. [DOI] [PubMed] [Google Scholar]
- Tudor Hart, J. (1971) The inverse care law. The Lancet, 297, 405–412. [DOI] [PubMed] [Google Scholar]
- Woolfenden, S. , Eapen, V. , Axelsson, E. , Hendry, A. , Jalaludin, B. , Dissanyake, C. , Overs, B. , Descallar, J. , Eastwood, J. , Einfield, S. L. , Silove, N. , Short, K. , Beasley, D. , Črnčec, R. , Murphy, E. , Williams, K. & Group, W. M. G. S. (2016) Who is our cohort: recruitment, representativeness, baseline risk and retention in the “Watch Me Grow” study? BMC Pediatrics, 16 DOI:10.1186/s12887-016-0582-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolfenden, S. , Posada, N. , Krchnakova, R. , Crawford, J. , Gilbert, J. , Jursik, B. , Sarkozy, V. , Perkins, D. & Kemp, L. (2014) Equitable access to developmental surveillance and early intervention—understanding the barriers for children from culturally and linguistically diverse (CALD) backgrounds. Health Expectations. DOI:10.1111/hex.12318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolfenden, S. , Short, K. , Blackmore, R. , Pennock, R. & Moore, M. (2015) How do primary health‐care practitioners identify and manage communication impairments in preschool children? Australian Journal of Primary Health, 21, 176–181. [DOI] [PubMed] [Google Scholar]


