Abstract
Improved practice in the management of hypertension depends on an understanding of existing patterns of treatment. To describe the management of newly diagnosed hypertension in British general practice and the effectiveness of current prescribing patterns we conducted a retrospective observational study using data from a computerized general practitioner record database (DIN-LINK).
21 024 patients were first treated for newly diagnosed hypertension between January 1993 and December 1997, and were followed for 4 years. Diuretics or beta-blockers were the most widely prescribed first-line treatments, used in 54% of patients. The mean continuation rate for first-line therapy was 69% at 12 months: the continuation rate was highest for angiotensin converting enzyme inhibitors/angiotensin II receptor antagonists. After 12 months of treatment the mean blood pressure reduction was 19/10 mmHg. Blood pressure targets were met in only 14% of patients. After 48 months of treatment 34% of patients had not improved in band of blood pressure severity. Many patients with severe hypertension at 12 months were still being prescribed only one drug.
The lack of aggression in antihypertensive treatment, indicated by the low number of agents prescribed and the failure to achieve targets, is disappointing. Prescribing patterns for first-line therapy corresponded to guidelines. Continuation rates on first-line therapy were higher than often reported. The choice of drug for additions to or switches from first-line therapy had no clear pattern. Routinely collected computerized data could be used to support clinical governance activities in primary care.
INTRODUCTION
The British Hypertension Society (BHS) and others have published guidelines for blood pressure targets and suitable choices for monotherapy, combination therapy and switches of therapy.1-4 Despite this, community surveys continue to record many patients with inadequate control or treatment.2,5-7 Observational studies have provided evidence on which drugs are used initially to treat hypertension8 but few have analysed the patient characteristics that influence the choice of first-line therapy. Adherence to recommendations in the long term is unclear and studies from other countries show poor compliance with such guidelines.9,10 Rates of change or discontinuation of antihypertensive therapy are high,11,12 and may suggest that poor control is due to poor adherence to prescribed medication. Furthermore, there is a paucity of information on long-term treatment patterns, including the discontinuations, additions and switches made to first-line therapy and the subsequent effects on blood pressure.
The aims of this study were to identify patterns of short and long term antihypertensive prescribing in the UK, to describe determinants of the choice of antihypertensive therapy, and to investigate the effect of these choices on blood pressure control.
PARTICIPANTS AND METHODS
Data source
Data were obtained from a general practitioner patient record database, DIN-LINK,13 which contains medical information from over 200 general practices and 900 000 patients in England and Wales. Data are collected longitudinally from routine patient records and compiled monthly. The DIN-LINK database is nationally representative and has been used in previous published studies.14
Study population
We studied patients in primary care treated for a new diagnosis of hypertension between January 1993 and December 1997. Hypertension was defined by diagnostic Read codes in the patient record. Absence of a blood pressure reading at baseline did not exclude patients provided there was a new hypertension Read code and first use of antihypertensive treatment.
To ensure a new diagnosis, patients were excluded if before the reference episode they had had any diagnosis of hypertension or had used any antihypertensive drug (even if for another indication, such as a beta-blocker for angina) before the reference episode. For this reason, we did not include patients for whom medical data went back less than 6 months. Patients who had less than 48 months' follow-up data available by December 2001 were also excluded.
Design
This was a retrospective observational study. Data were recorded at baseline (before antihypertensive therapy) and monthly thereafter for 48 months. Recorded data included demographic details, blood pressure, comorbidities, and antihypertensive prescribing. A descriptive analysis characterized the population studied and subgroups according to blood pressure and first-line therapy. The continuation rates and changes to therapy were identified. Comparison between the mean baseline blood pressure and subsequent blood pressure readings allowed assessment of the effect of particular therapeutic strategies on blood pressure. Patients were only included in this analysis if they had a blood pressure measurement at baseline and at the reference time point.
Drugs were grouped in five major classes of antihypertensive monotherapy15—diuretics, beta-blockers, angiotensin converting enzyme (ACE) inhibitors and angiotensin II receptor antagonists (AIIRAs), calcium channel blockers (CCBs), or others. Combination therapy was analysed separately. Monotherapy was defined as a prescription for one agent, or two within the same drug class (to cover the widely used diuretic combination formulation co-amilozide). Combination therapy was defined as a prescription for more than one agent from two classes, including two agents in one formulation.
A drug was considered discontinued when it had not been prescribed for 120 days. Switching of drug was defined as the prescription of a new drug preceding or coinciding with the discontinuation of another in the previous month.12,16 Adding of a new drug was defined as prescription of a new drug coinciding with the continuing prescription of another.
Statistics
Only descriptive statistics are reported (means with 95% confidence intervals). Further analysis was inappropriate.
RESULTS
21 024 eligible patient records were identified (Table 1).
Table 1.
Baseline patient characteristics
| Characteristic | N=21 024 |
|---|---|
| Age and gender | |
| Mean age years (95% CI) | 62.0 (61.8, 62.1) |
| N (%) of male patients | 8790 (42.0) |
| N (%) of patients over 65 years | 7608 (36.2) |
| N (%) of male patients who were >65 years | 2678 (30.5) |
| N (%) of female patients who were >65 years | 4932 (40.3) |
| Severity of hypertension at diagnosis* | N=14 694 |
| Mean SBP mmHg (95% CI) | 172.7 (172.3, 173.1) |
| Mean DBP mmHg (95% CI) | 98.4 (98.2, 98.6) |
| N (%) normal (SBP ≤ 139 DBP ≤ 89) | 525 (3.6) |
| N (%) mild (SBP ≥ 140 ≤ 159 DBP ≥ 90 ≤ 99) | 1943 (13.2) |
| N (%) moderate (SBP ≥ 160 ≤ 199 DBP ≥ 100 ≤ 109) | 7738 (52.7) |
| N (%) severe (SBP ≥ 200 ≥ 110) | 4488 (30.5) |
| Comorbidities | N=21 024 |
| N (%) asthma | 1776 (8.4) |
| N (%) diabetes mellitus | 1258 (6.0) |
| N (%) angina | 1538 (7.3) |
| N (%) heart failure | 505 (2.4) |
| N (%) COPD | 423 (2.0) |
| N (%) history of MI | 725 (3.4) |
CI=confidence interval; COPD=chronic obstructive pulmonary disease;
MI=myocardial infarction
Blood pressure severity defined by highest systolic (SBP) or diastolic (DBP) according to 1999 guidelines for the management of hypertension
Choice of first-line antihypertensive therapy and influencing factors
Diuretic and beta-blocker monotherapy accounted for almost 55% of first-line treatment (Table 2). This varied by age and gender; older patients tended to be prescribed diuretics, and younger patients beta-blockers or ACE inhibitors/AIIRAs; women were more likely to be prescribed a diuretic than men (data not shown).
Table 2.
Choice of first-line therapy by age and blood pressure severity at baseline
|
N (%) of patients in each age group (years) prescribed each drug class
|
N (%) of patients in each band of blood pressure severity prescribed each drug class
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug | <55 (N=7788) | 55-64 (N=5628) | 65-74 (N=5198) | 75+ (N=2410) | Total (N=21024) | Normal < 139/≤89 (N=525) | Mild 140-59/90-99 (N=1943) | Moderate 160-199/100-109 (N=7738) | Severe ≥200/≥110 (N=4488) |
| Diuretic | 1892 (24.3) | 1700 (30.2) | 1991 (38.3) | 1154 (47.9) | 6728 (32.0) | 98 (18.7) | 541 (27.8) | 2939 (38.0) | 1297 (28.9) |
| Beta-blocker | 2336 (30.0) | 1266 (22.5) | 832 (16.0) | 234 (9.7) | 4667 (22.2) | 157 (29.9) | 516 (26.6) | 1708 (22.1) | 924 (20.6) |
| CCB | 849 (10.9) | 765 (13.6) | 785 (15.1) | 318 (13.2) | 2712 (12.9) | 81 (15.4) | 267 (13.7) | 918 (11.9) | 546 (12.2) |
| AIIRA/ACE | 1269 (16.3) | 737 (13.1) | 509 (9.8) | 229 (9.5) | 2754 (13.1) | 59 (11.2) | 238 (12.2) | 1056 (13.6) | 658 (14.7) |
| Alpha/other | 102 (1.3) | 51 (0.9) | 57 (1.1) | 29 (1.2) | 231 (1.1) | 10 (1.9) | 34 (1.7) | 62 (0.8) | 37 (0.8) |
| Combination | 1340 (17.2) | 1109 (19.7) | 1024 (19.7) | 446 (18.5) | 3932 (18.7) | 120 (22.9) | 347 (17.9) | 1054 (13.6) | 1026 (22.9) |
CCB=Calcium channel blocker; AIIRA=angiotensin II receptor antagonists; ACE=angiotensin converting enzyme
Initial blood pressure and choice of initial treatment were related in some instances; for example, beta-blocker monotherapy was more likely to be prescribed to patients with mild hypertension than in those with moderate to severe hypertension and the converse was true for ACE inhibitors/AIIRAs (Table 3).
Table 3.
Choice of first-line therapy by comorbidity
|
N (%) of patients
|
||||||
|---|---|---|---|---|---|---|
| Antihypertensive | Diabetes (N=1258) | Angina (N=1538) | MI (N=725) | CHF (N=505) | Asthma (N=1776) | COPD (N=423) |
| Diuretic | 168 (13.4) | 281 (18.3) | 144 (19.9) | 188 (37.2) | 673 (37.9) | 159 (37.6) |
| Beta-blocker | 142 (11.3) | 372 (24.2) | 182 (25.1) | 27 (5.3) | 171 (9.6) | 23 (5.4) |
| CCB | 238 (18.9) | 410 (26.7) | 119 (16.4) | 74 (14.7) | 336 (18.9) | 90 (21.3) |
| AIIRA/ACE | 521 (41.4) | 142 (9.2) | 87 (12) | 75 (14.9) | 290 (16.3) | 59 (13.9) |
| Others | 23 (1.8) | 12 (0.8) | 5 (0.7) | 8 (1.6) | 22 (1.2) | 5 (1.2) |
| Combination | 166 (13.2) | 321 (20.9) | 188 (25.9) | 133 (26.3) | 284 (16.0) | 87 (20.6) |
MI=Myocardial infarction; CHF=congestive heart failure; COPD=chronic obstructive pulmonary disease; CCB=calcium channel blocker; AIIRA=angiotensin II receptor antagonists; ACE=angiotensin converting enzyme
While there were indications of selective prescribing (e.g. diabetic patients more likely to receive ACE inhibitors/AIIRAs, and patients with angina more likely to receive a beta-blocker or a CCB), the overall concordance with published guidelines for prescribing in patients with comorbidity was low. Only 41% of patients with diabetes were prescribed an ACE inhibitor/AIIRA, despite compelling indications, and only 25% of patients with a history of myocardial infarction were prescribed a beta-blocker. Furthermore, 9.6% of patients with asthma were prescribed a beta-blocker.
Continuation with first-line therapy
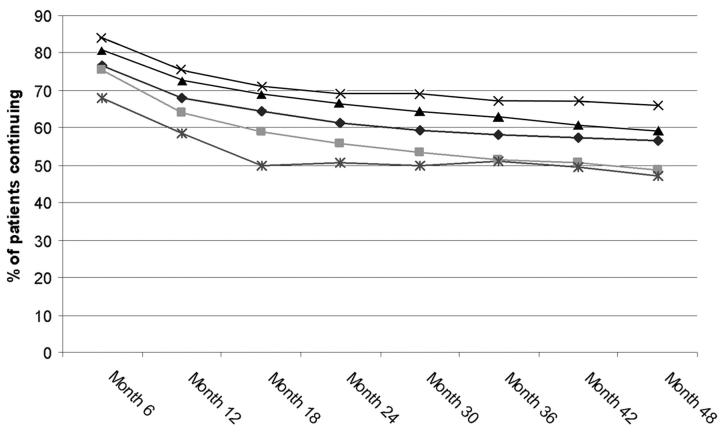
The continuation rates for first-line therapy declined most sharply over the first year (at which point average continuation rates reached 69%). The rate of average decline levelled between months 18 and 48 (Figure 1). Whilst these patterns were similar for the different classes of drug, continuation rates for ACE inhibitors/AIIRAs were significantly greater than for other classes at 18 and 48 months (P < 0.01, chi-squared=64.80 at 12 months and 130.04 at 48 months, with one degree of freedom).
Figure 1.
Continuation rates for each first-line monotherapy drug class. ⋄ Diuretic; □ beta, ▴ CCBs, x AIIRA/ACE; * alpha/other
Alterations to initial prescription
Overall, 11 321 (66%) patients who started on monotherapy experienced some alteration to their original prescription in the first year. Of these, 3205 patients (19%) had a dose increase and 941 (6%) a dose decrease. In all 39% (n=1515) of switches and 35% (n=1013) of additions to first-line monotherapy were not in accordance with guidelines.1,2,4 Intraclass switches were experienced by 13% (n=351) of patients who switched from first-line monotherapy, whereas 6% (n=187) of additions involved two drugs from the same class.
Blood pressure control
At one year, the mean blood pressure was 154/88 (CI 153.6, 154.2/87.9, 88.2) mmHg and reduction in blood pressure was 19/10 (CI 18.5, 19.2/10.2, 10.6) mmHg. At this time only 14.2% (n=2082) of patients reached guideline-determined blood pressure targets (systolic ≤ 139 mmHg, diastolic ≤ 89 mmHg),2 with 42% (n=6140) still having moderate to severely raised blood pressure (Table 4). Overall, 40% (n=5872) of patients did not improve in band of blood pressure severity after 12 months of treatment. After 48 months of treatment 34% (n=4992) of patients did not improve in band of blood pressure severity (data not shown).
Table 4.
Number (%) of patients who moved from original blood pressure severity band to another band
|
Blood pressure at 12 months
|
|||||
|---|---|---|---|---|---|
| Original blood pressure | N | Normal ≤139/≤89 | Mild 140-159/90-99 | Moderate 160-199/100-109 | Severe ≥200/≥110 |
| Normal | 524 | 284 (54.2) | 196 (37.4) | 42 (8.0) | 2 (0.4) |
| Mild | 1944 | 405 (20.8) | 1189 (61.2) | 341 (17.5) | 9 (0.5) |
| Moderate | 7728 | 986 (12.8) | 3434 (44.4) | 3186 (41.2) | 122 (1.6) |
| Severe | 4485 | 407 (9.1) | 1640 (36.6) | 1911 (42.6) | 527 (11.8) |
| Total | 14681 | 2082 (14.2) | 6459 (44.0) | 5480 (37.3) | 660 (4.5) |
There was no relation between initial drug choice and blood pressure at 12 months or 48 months. Patients whose blood pressure was initially severe were likely to receive more medications (data not shown). Severity of blood pressure was only weakly related to the number of agents prescribed at month 12 (Table 5) or 48 (data not shown). Of those patients with moderate/severe hypertension at 12 months, 66% (n=3345) were still receiving a single agent with a further 28% (n=1435) being prescribed two antihypertensive agents (Table 5).
Table 5.
Number of agents and severity of blood pressure at month 12
|
No. (%) of patients
|
||||
|---|---|---|---|---|
| No. of agents | Normal ≤139/≤89 | Mild 140-159/90-99 | Moderate 160-199/100-109 | Severe ≥200/≥110 |
| 1 (N=8383) | 1206 (72.7) | 3832 (71.5) | 2982 (67.1) | 363 (56.8) |
| 2 (N=3176) | 398 (24.0) | 1343 (25.0) | 1228 (27.6) | 207 (32.4) |
| 3 (N=485) | 45 (2.7) | 173 (3.2) | 212 (4.8) | 55 (8.6) |
| 4+ (N=63) | 10 (0.6) | 14 (0.3) | 25 (0.5) | 14 (2.2) |
| Totals | 1659 | 5362 | 4447 | 639 |
Chi squared=139; d.f.=9; P<0.0001; Cramer V for association 0.0619
The average blood pressure reduction achieved by switching or adding drugs within the same class was 2/1 mmHg—less than the average blood pressure reduction for the main cross-class switches (4/2 mmHg) or additions (5/3 mmHg). Blood pressure control was no better in patients with comorbidities (data not shown).
DISCUSSION
The patterns of prescribing of first-line drugs are similar to those previously reported in the UK.11,17 Like the previous researchers, we found no clear patterns for subsequent prescribing for patients who do not respond to first-choice therapy or who have adverse effects. In particular, intraclass switches (13% of monotherapy switches) seem less rational, were found to be less effective and may delay adequate treatment. The first-line agent was influenced by comorbidity (e.g. diabetic patients more likely to receive ACEI/AIIRA, angina patients and patients after myocardial infarction more likely to receive beta-blockers) but there were some areas of less rational or even dangerous prescribing such as use of beta-blockers in patients with asthma.
We found patient continuation with first-choice therapy higher than in similar studies.11,12,16,18,19 There were differences between drugs: some studies show the highest continuation rates for ACE inhibitors/AIIRA,11,19,20 as here, but others find diuretics the best tolerated.21 The three published trials that directly compared the major classes of drugs22-24 found no difference in rates of adverse effects, intolerance or efficacy of control. Similarly the recent ALLHAT study found little difference between chlorthalidone, lisinopril and amlodipine.25 However, it is effectiveness rather than efficacy that should interest the doctor and the patient. Effectiveness—the ability to lower blood pressure in common practice—depends in part on the efficacy of the drug in the controlled environment of the clinical trial but also on adherence to treatment, adverse effects, convenience and patient selection and monitoring. In our study, the similar effectiveness of the main classes of drugs and similar continuation rates are consistent with these trials.
Poor persistence with drug therapy has been considered a cause of poor control of blood pressure.16 While adverse reactions are most commonly given by general practitioners as the reason for changing therapy,17 lack of effectiveness has also been cited and may confound this interpretation. Changes in therapy were most likely to occur early, in this study. Subsequent therapy seemed relatively stable, more so than in other studies of newly diagnosed hypertensives.20 More recent work3,4 provides a scientific rationale for what may be appropriate changes or additions of therapy in patients who are unresponsive to first-line therapy or who have adverse effects on drugs. This work requires replication in larger more naturalistic trials, but we believe it to be a valuable approach (of which, in our experience, few generalist doctors are aware).
Blood pressure control
The quality of blood pressure control was poor (only 14% met BHS targets after 12 months of treatment) and was similar to that reported in the general population in the USA,26 although better results (up to 23% well controlled) have been seen in specific US populations with good access to healthcare. We used the 1993 BHS guidance2 as our standard in assessing quality of control, this being current at the time of the data collection. Later BHS guidance sets more rigorous targets.4
Most patients experienced some fall in blood pressure: the typical fall in diastolic blood pressure in this study was around 10 mmHg. Some of this effect may be due to simple regression to the mean, since it was proportionately greater in those with the highest blood pressures; this phenomenon is well recognized in studies of hypertension and is particularly likely to have occurred in this study since we depended on the general practitioner's diagnosis of hypertension, which was not made according to any fixed protocol but according to usual practices.
Few physicians were energetically pursuing published targets. In particular, 65% of patients with moderate to severe hypertension were receiving only one agent, despite the acknowledged benefits of adding a second drug. A further 28% were receiving only two agents despite the likely benefit of using three. Whether the general practitioners' targets in treating hypertension are in fact a particular level of blood pressure or a particular level of blood pressure reduction is unclear, and merits further study.
Our study showed clear selection of drugs based on comorbidity, age and sex. However, it is not obvious that level of blood pressure or risk reduction was considered in the same way. In particular, diabetic patients were not treated more aggressively, as BHS guidelines suggest they should be, and they received ACE inhibitors or AIIRAs less often than would be expected. The greatest reduction of blood pressure is seen in the most severely affected patients: these patients had the greatest numbers of drugs prescribed simultaneously and, even with allowance for regression to the mean, some of this apparent reduction is likely to be due to more aggressive therapy.
The period covered by this study is similar to that represented by the two reports of the Health Survey for England.6,27 The more recent report described similar patterns of initial prescribing and suggested levels of control of blood pressure of only 9% compared with the 14% here. The differences may lie in the systematic measurement of blood pressure in the survey, compared with the unvalidated recordings accepted in our study. Either result reflects inadequate management.
Limitations
The current work is observational and there may be unrecorded confounders for choice of drug and for quality of control. We used only newly diagnosed patients, in contrast to Jones et al.11 who asked a different question around drug persistence. The blood pressures and comorbidities were as recorded by the general practitioners: there was no defined protocol for measuring blood pressure, and the prevalence of diabetes in this hypertensive population seems low. Other limitations are our inability to validate diagnosis of hypertension or of comorbidities, individual blood pressure recordings, or even that the patient ever took the prescribed drug. These drawbacks are unavoidable in studies which use routinely collected data from medical records rather than a prospective design. However, the data presented here are exactly the information on which physicians are basing their treatment decisions.
Our categorization of drugs may hide differences in tolerability between individual drugs within a class: this is particularly true for calcium channel blockers where there is diversity in the adverse effects of the individual dihydropyridines. Our analysis also hides differences in response arising from changes in dosing. Further analyses of the current data are clearly possible.
CONCLUSION
Despite these limitations, this is the largest study of clinical practice in hypertension in the UK. It shows that guidelines are followed in some aspects but not others. Large numbers of patients are poorly controlled on one or two drugs only, and there is clearly room for improvement by more aggressive use of multiple drug therapy.27 There also seemed to be no clear plan in changes in therapy. The use of dangerous or contraindicated drugs is also a cause for concern.
The key question remains how we can improve blood pressure control in the community. A better understanding of general practitioners' prescribing habits and their outcomes could assist in targeting education and their other interventions to improve the management of hypertension. Here we examined only patients diagnosed by the end of 1997, so that we could report long-term follow-up. Our later data on treatment of new patients from 1998-2001 from the same source (unpublished) suggest little change in quality of control. In the past 2-3 years, however, there has been a substantial rise in the prescribing of antihypertensive medicines in the UK,28 perhaps as a result of the increased focus on the prevention of coronary and cerebrovascular disease in National Service Frameworks.29 It is not clear yet that this translates into better control. Hypertension remains a key area for clinical governance by primary care trusts. Routinely collected computerized data of the type used in this study will prove useful in achieving this through local audits.
Note This project was funded by an unrestricted educational grant from Novartis. The Department of Pharmacology and Therapeutics receives research grants from Novartis. Abacus International has previously performed paid consultancy work for Novartis.
References
- 1.Sever P, Beevers G, Bulpitt C, et al. Management guidelines in essential hypertension: report of the second working party of the British Hypertension Society. BMJ 1993;306: 983-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramsay L, Williams B, Johnston G, et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society. J Hum Hypertens 1999;13: 569-92 [DOI] [PubMed] [Google Scholar]
- 3.Dickerson JE, Hingorani AD, Ashby MJ, Palmer CR, Brown MJ. Optimisation of antihypertensive treatment by crossover rotation of four major classes. Lancet 1999;353: 2008-13 [DOI] [PubMed] [Google Scholar]
- 4.Lip G, Beevers M, Beevers D. The ‘Birmingham Hypertension Square’ for the optimum choice of add-in drugs in the management of resistant hypertension. J Hum Hypertens 1998;12: 761-3 [DOI] [PubMed] [Google Scholar]
- 5.Burr AJ. Comparing hypertension guidelines. Audit in Mid-Glamorgan also shows major problems with management of hypertension. BMJ 1996;313: 1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colhoun HM, Dong W, Poulter NR. Blood pressure screening, management and control in England: results from the health survey for England 1994. J Hypertens 1998;16: 747-52 [DOI] [PubMed] [Google Scholar]
- 7.Cranney M, Barton S, Walley T. Auditing the management of hypertension in British general practice: a critical literature review. Br J Gen Pract 1998;48: 1424-8 [PMC free article] [PubMed] [Google Scholar]
- 8.Hobbs F. Modern management of hypertension and heart failure: evidence and practice. Heart 2000;84(suppl 1): 135-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegel D, Lopez J. Trends in antihypertensive drug use in the United States: do the JNC V recommendations affect prescribing? Fifth Joint National Commission on the Detection, Evaluation, and Treatment of High Blood Pressure. JAMA 1997;278: 1745-8 [DOI] [PubMed] [Google Scholar]
- 10.Tu K, Mamdani MM, Tu JV. Hypertension guidelines in elderly patients: is anybody listening? Am J Med 2002;113: 52-8 [DOI] [PubMed] [Google Scholar]
- 11.Jones JK, Gorkin L, Lian JF, Staffa JA, Fletcher AP. Discontinuation of and changes in treatment after start of new courses of antihypertensive drugs: a study of a United Kingdom population. BMJ 1995;311: 293-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bourgault C, Rainville B, Suissa S. Antihypertensive drug therapy in Saskatchewan: patterns of use and determinants in hypertension. Arch Intern Med 2001;161: 1873-9 [DOI] [PubMed] [Google Scholar]
- 13.DIN-Link database: Compufile Ltd [www.compufile.co.uk]
- 14.Warner JO. Review of prescribed treatment for children with asthma in 1990. BMJ 1995;311: 663-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.British Medical Association. British National Formulary (BNF). London: BMA, Royal Pharmaceutical Society of Great Britain, 2002
- 16.Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. Can Med Assoc J 1999;160: 31-7 [PMC free article] [PubMed] [Google Scholar]
- 17.Martin R, Kerry S, Hilton S. Initial treatment choices, second-line therapy, and reasons for stopping medication in the treatment of hypertension by general practitioners in England, Scotland and Wales: 1990-1995. Pharmacoepidemiol Drug Safety 1997;6: 253-61 [DOI] [PubMed] [Google Scholar]
- 18.Degli Esposti E, Sturani A, Degli Esposti L, et al. Pharmacoutilization of antihypertensive drugs: a model of analysis. Int J Clin Pharmacol Ther 2001;39: 251-8 [PubMed] [Google Scholar]
- 19.Bloom BS. Continuation of initial antihypertensive medication after 1 year of therapy. Clin Ther 1998;20: 671-81 [DOI] [PubMed] [Google Scholar]
- 20.Caro JJ, Speckman JL, Salas M, Raggio G, Jackson JD. Effect of initial drug choice on persistence with antihypertensive therapy: the importance of actual practice data. Can Med Assoc J 1999;160: 41-6 [PMC free article] [PubMed] [Google Scholar]
- 21.Olsen H, Klemetsrud T, Stokke HP, Tretli S, Westheim A. Adverse drug reactions in current antihypertensive therapy: a general practice survey of 2586 patients in Norway. Blood Pressure 1999;8: 94-101 [DOI] [PubMed] [Google Scholar]
- 22.Materson BJ, Reda DJ, Cushman WC, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med 1993;328: 914-21 [DOI] [PubMed] [Google Scholar]
- 23.Neaton JD, Grimm RH, Prineas RJ, et al. Treatment of Mild Hypertension Study. Final results. Treatment of Mild Hypertension Study Research Group. JAMA 1993;270: 713-24 [PubMed] [Google Scholar]
- 24.Philipp T, Anlauf M, Distler A, Holzgreve H, Michaelis J, Wellek S. Randomised, double blind, multicentre comparison of hydrochlorothiazide, atenolol, nitrendipine, and enalapril in antihypertensive treatment: results of the HANE study. HANE Trial Research Group. BMJ 1997;315: 154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blockers vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288: 2981-97 [DOI] [PubMed] [Google Scholar]
- 26.He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the general population of the United States. Arch Intern Med 2002;162: 1051-8 [DOI] [PubMed] [Google Scholar]
- 27.Primatesta P, Brookes M, Poulter N. Improved hypertension management and control: results for the Health Survey for England 1998. Hypertension 2001;38: 827-32 [PubMed] [Google Scholar]
- 28.Department of Health, England. Prescriptions Dispensed in the Community 1991-2001 [http://www.doh.gov.uk/pdfs/sb0214.pdf], accessed 21 April 2003
- 29.Department of Health. National Service Framework for Coronary Heart Disease [http://www.doh.gov.uk/nsf/coronary.htm], accessed 21 April 2003