Abstract
Background: Immunization coverage data and determinants for completion are not well described for Pakistan. This study determines immunization coverage rates and timeliness based on the 2006–07 Pakistan Demographic and Health Survey (DHS) and identifies determinants for completion of immunizations.
Methods: DHS data from 9177 randomly selected households from across Pakistan were analyzed to assess immunization coverage and timeliness for children aged 0–5 years, and to investigate determinants of immunization completion through logistic regressions.
Results: The proportion of children immunized for a third dose of the oral poliovirus vaccine (OPV3) was 80.3%, and combination diphtheria, tetanus, and pertussis vaccines (DTP3) was 55.9%. Measles coverage was 62.5%. Late immunizations were most likely to occur for third doses of the OPV (65.5%) and DTP series (65.5%). Early doses were most likely to be administered for measles (21.9%). The proportion of children not immunized for any vaccine was 6.2%. Receiving a dose of maternal tetanus was a major determinant for immunization completion for OPV3 (OR 1.35, 95% CI: 1.14–1.60), DTP3 (OR 2.54, 95% CI: 2.13–3.02), and measles (OR 2.78, 95% CI: 2.27–3.40). Other independent variables associated with improved immunization completion included higher household wealth and maternal education.
Conclusion: Poor routine immunization coverage and timeliness were identified through the DHS in Pakistan. Encouraging maternal tetanus uptake among women of child-bearing age and greater integration of immunization services with antenatal care may help improve childhood immunization completion.
Keywords: immunization timeliness, immunization coverage, immunization determinants, Demographic Health Survey, Pakistan
Introduction
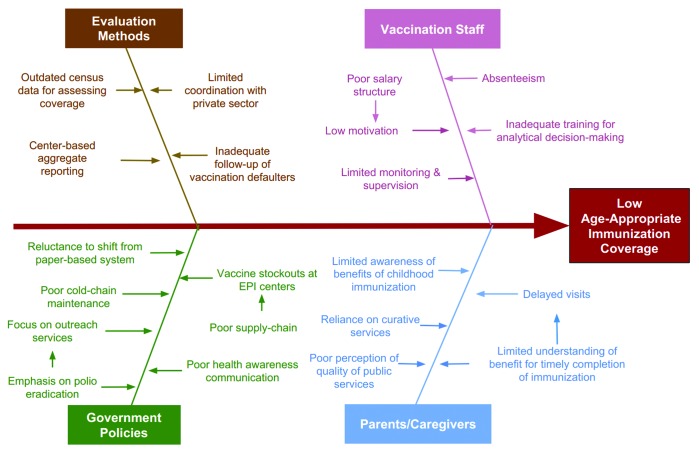
Pakistan's large birth cohort of 5 million infants annually has important consequences for vaccine delivery in an already constrained health systems infrastructure.1 Achieving 90% national immunization coverage and at least 80% coverage in every district requires a deeper understanding of current challenges, policy revisions, and pragmatic decision-making (Fig. 1).2,3 Several recent developments, including the devolution of the Expanded Programme on Immunization (EPI) to the provinces, a nationwide measles outbreak and deadly attacks by extremist militants on polio immunization staff and volunteers have renewed government and public focus on EPI and toward addressing its deficiencies. To generate the appropriate evidence-base for facilitating this process, the determinants of immunization uptake in Pakistan need to be more rigorously explored.
Figure 1. Factors contributing to low age-appropriate immunization coverage in Pakistan.
Polio eradication and elimination of neonatal tetanus and measles remain priority goals of the government administered EPI. Vaccines are delivered via a network of 5310 Basic Health Units, 561 rural health centers, 5673 maternal-child health centers and dispensaries, and 948 secondary and tertiary care facilities.4 Public sector officials often operate in collaboration with private sector and conduct outreach activities and mass-immunization campaigns in areas of low-coverage. Part of the challenge in improving immunization coverage arises from methodological issues by which administrative coverage rates (number of doses administered relative to target population) are calculated from a large number of reporting sites (Fig. 1). Public officials rely upon paper-based registries that are time-consuming to fill, prone to data-recording errors and do not adequately capture timeliness of vaccine administration. In addition, target population estimations (the denominator in vaccine coverage calculations (arise since they are based on a census conducted in 19985. Delayed immunizations increase the length of time a child remains susceptible to disease during infancy, whereas early immunizations fail to generate a protective antibody response.6
Demographic and Health Surveys (DHS), conducted on a nationwide sampling of households, provide useful information on individual level immunization coverage and timeliness, as well as a range of determinants that might influence immunization practices. Previous studies from the country have investigated immunization determinants in small geographic settings, often as part of interventional studies with limited generalizability.7-12 The aim of this paper is to describe immunization coverage rates and timeliness based on data reported from the DHS and to investigate determinants for completion of immunizations.
Methodology
Data collection
Details of the sampling methodology and data collection procedure of the 2006–07 DHS have been described elsewhere.13 Briefly, a multi-stage sampling methodology was utilized to select households across Pakistan, excluding federally administered areas in the north and northwest and restricted military cantonments. In the first stage of sampling, 1000 clusters were selected with probability proportional to size within the strata (Fig. 2). The second stage of sampling involved selecting 105 households from each cluster using systematic random sampling resulting in a total sample size of 102 060 households. This resulted in a sample that was weighted more toward urban centers and less populated provinces. This allowed for a sample that was more representative of the population at the national level.
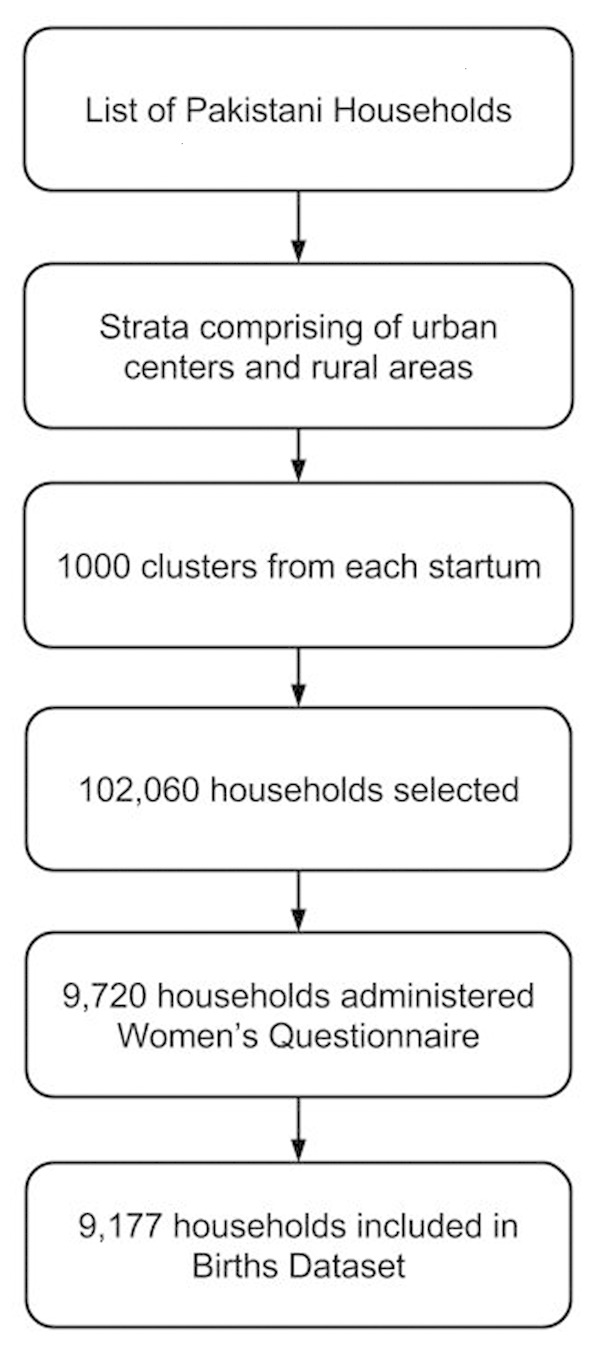
Figure 2. Selection of households for the 2006–07 Pakistan Demographic and Health Survey.
Immunization data was captured through the “Women’s Questionnaire” that was administered to a subset of 9720 households. Data for analyses was obtained from the “Births” data set that included information from 9177 of these households. Eligible ever-married women ages 12–49 y residing in these households were interviewed regarding demographics, education, reproductive history, fertility practices, literacy, and household income. Childhood immunizations and other health related indicators were ascertained for the last child born in each house.
Immunization coverage and timeliness definitions
EPI immunization cards were available in just 10% of cases and the remaining immunization records were assessed through historical recall of the mother. Dates of births for children were recorded in month and year only; the median day of each month (15th) was assigned as the day of birth for each child. The age range of children in the dataset was from birth up to 5 y of age. Immunization coverage was defined as a binary variable based on whether or not a child had received an immunization, assessed through historical recall or the EPI card. Immunization coverage proportions were calculated based on the recommended age used for each immunization dose as per EPI schedule (Table 1).14 Children younger than the recommended age for each vaccine were excluded from the denominator in the calculations.
Table 1. Recommended and minimum acceptable ages for routine immunizations in the expanded program for immunizations (2002–2007) in Pakistan.
| Antigen and dose | Minimum age | Recommended | Timely | Early | Late |
|---|---|---|---|---|---|
| OPV0/ BCG | Birth | 0 wk / 0 d | 0–28 d | — | >28 d |
| OPV1/ Penta1 | 6 wk | 6 wk / 42 d | 39–70 d | <39 d | >70 d |
| OPV2/Penta2 | 10 wk | 10 wk / 70 d | 67–98 d | <67 d | >98 d |
| OPV3/Penta3 | 14 wk | 14 wk / 98 d | 95–126 d | <95 d | >126 d |
| Measles | 26 wk | 39 wk / 273 d | 270–301 d | <270 d | >301 d |
Timeliness of immunizations could only be ascertained for children where the vaccination history card was available. Immunizations were classified as “early” if there were administered 3 d prior to the recommended age. Immunizations were defined as “late” if they were administered greater than 4 wk after the recommended age. The remaining vaccinations within these time frames were categorized as “timely.” Sensitivity analyses for immunization timeliness were performed using the first and last days of each month along with the recorded month and year of birth to calculate the date of birth. These were utilized to provide a range of estimates for the proportion of immunizations falling within each timeliness category.
Statistical analysis
Frequency analysis of baseline characteristics of the survey respondents was performed by province. Proportions were used to assess immunization coverage and timeliness for each immunization. Determinants for immunization completion were investigated for the third dose of oral polio vaccine (OPV3), third dose of combined diphtheria, tetanus, and pertussis (DTP3) and measles vaccinations. Determinants selected from the DHS dataset were based on a priori knowledge from medical and public health literature and biological plausibility. These included age, gender, ethnicity, wealth, maternal education household size, antenatal healthcare-seeking, and breastfeeding practices. Bivariate associations were explored for each of the determinants through survey-weighted logistic regressions. Adjusted analyses were subsequently performed through survey-weighted backward step-wise logistic regressions using Akaike's Information Criteria (AIC) to select the final, parsimonious model. Modified goodness-of-fit tests for survey-weighted logistic regression were utilized to assess the final model.15 All statistical analyses were performed using Stata 12.1 (College Station, TX: StataCorp LP).
Results
Baseline characteristics of respondents
Data for a total of 9177 respondents was available in the data set of which 40.4% were from Punjab, 22.9% were from Sindh, 19.5% were from Khyber-Pakhtunkhwa (KPK) and 11.3% were from Baluchistan (Table 2). Maternal tetanus coverage was highest in Punjab (66.1%), followed by Sindh (57.6%), KPK (51.3%), and Baluchistan (31.9%) provinces. The prevalence of home deliveries was higher in Baluchistan (78.9%) and KPK (66.9%) as compared with other provinces. Similarly respondents from Baluchistan and KPK were least likely to receive antenatal visits (56.3% and 45.2% respectively) compared with the other provinces.
Table 2. Baseline characteristics of survey respondents in the Pakistan demographic and health survey (2006–2007).
| Punjab | Sindh | KPK | Baluchistan | Total | |
|---|---|---|---|---|---|
| n | 3705 | 2649 | 1787 | 1036 | 9177 |
| (%) | (40.4) | (22.9) | (19.5) | (11.3) | (100) |
| Child median age in wk | 126 | 126 | 126 | 130 | 126 |
| (IQR) | (56.57–187.14) | (56.57–191.14) | (60.85–191.28) | (60.85–187.21) | (56.57–187.28) |
| Male (%) | 52 | 52 | 53 | 53 | 52 |
| Ethnicity | |||||
| Punjabi (%) | 62.8 | 5.1 | 0.7 | 1.0 | 27.1 |
| Mohajir (%) | 7.2 | 9.7 | 1.0 | 1.9 | 6.1 |
| Sindhi (%) | 0.0 | 47.0 | 0.1 | 10.1 | 14.7 |
| Pakhtun (%) | 2.3 | 3.9 | 77.7 | 45.8 | 22.4 |
| Balochi (%) | 0.3 | 7.1 | 0.0 | 26.0 | 5.1 |
| Seraiki (%) | 24.7 | 13.6 | 6.2 | 3.3 | 15.5 |
| Other (%) | 2.7 | 13.7 | 14.3 | 12.0 | 9.2 |
| Urban (%) | 34.5 | 38.3 | 30.7 | 29.3 | 34.3 |
| Wealth | |||||
| Lowest Quintile (%) | 17.5 | 33.4 | 14.6 | 33.1 | 23.3 |
| 2nd Quintile (%) | 17.2 | 20.4 | 31.4 | 23.8 | 21.6 |
| 3rd Quintile (%) | 22.2 | 14.5 | 21.2 | 25.8 | 20.2 |
| 4th Quintile (%) | 21.5 | 17.1 | 17.4 | 9.7 | 18.1 |
| Highest Quintile (%) | 21.6 | 21.6 | 14.5 | 15.6 | 16.8 |
| Telephone connection (%) | 46.0 | 38.4 | 47.9 | 33.0 | 42.7 |
| Median household size | 8 | 9 | 9 | 10 | 9 |
| (IQR) | (6–11) | (6–12) | (7–13) | (7–16) | (6–12) |
| Median number of children Under 5 y of age | 2 | 2 | 2 | 2 | 2 |
| (IQR) | (1–3) | (2–3) | (2–3) | (2–4) | (1–3) |
| Median highest maternal y of education | 5 | 5 | 4 | 4 | 5 |
| (IQR) | (3–5) | (3–5) | (3–5) | (3–5) | (3–5) |
| Median breastfeeding duration in mo | 15 | 14 | 16 | 16 | 15 |
| (IQR) | (7–24) | (7–24) | (8–24) | (9–24) | (7–24) |
| Received at least 1 dose of Maternal tetanus (%) | 66.2 | 57.6 | 51.3 | 31.9 | 56.8 |
| Male household head (%) | 91.5 | 95.6 | 90.0 | 98.4 | 93.2 |
| Home delivery (%) | 64.4 | 57.9 | 66.9 | 79.0 | 64.7 |
| Antenatal visits | |||||
| 0 (%) | 32.3 | 27.5 | 42.2 | 56.3 | 35.7 |
| 1–5 (%) | 48.7 | 55.1 | 46.6 | 40.8 | 49.2 |
| 6–10 (%) | 16.0 | 14.5 | 10.1 | 2.6 | 12.9 |
| >10 (%) | 3.0 | 2.9 | 1.1 | 0.3 | 2.3 |
Immunization coverage and timeliness indicators
In children aged 0–5 y, oral polio vaccine at birth (OPV0) was administered to 50.5% compared with 75.4% for Bacillus Calmette–Guérin (BCG) (Table 3). The OPV3 completion was 80.3% with OPV1 to OPV3 dropout rate of 7.7% as compared with DTP3 completion of 55.9%, with DTP1 to DTP3 dropout rate of 14%. The measles vaccine completion was 62.5%. Proportion of children not immunized for any vaccine was 6.2%.
Table 3. Immunization completion in children aged 0–5 y old, 2002–2007 in Pakistan.
| BCG | Polio | DTP | Measles | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OPV0 | OPV1 | OPV2 | OPV3 | DTP1 | DTP2 | DTP3 | |||
| na | 8329 | 8419 | 8306 | 8192 | 7970 | 8080 | 7886 | 7733 | 6815 |
| Card (%) | 16.00 | 11.76 | 14.62 | 13.15 | 11.57 | 15.06 | 13.49 | 12.05 | 10.17 |
| History (%) | 59.35 | 38.69 | 73.39 | 72.12 | 68.75 | 54.83 | 49.71 | 43.81 | 52.34 |
| Either dource (%) | 75.35 | 50.45 | 88.01 | 85.27 | 80.32 | 69.89 | 63.20 | 55.86 | 62.51 |
aRepresents total number of children due for vaccination based on age calculated from birth date
BCG immunizations were timely in 70.1% of children as compared with 77.1% for OPV0; 48.0% of OPV1 immunizations were timely as compared with 36.4% of OPV2 and 27.4% of OPV3 (Table 4). For DTP1 immunizations, 49.0% were timely for DTP1 as compared with 35.5% for DTP2, and 27.4% for DTP3. The proportion of timely measles immunizations was 41.4%. Early immunizations were most frequently reported for measles (22%) followed by OPV1 (16.7%) and DTP1 (10.7%). Late immunizations were most frequently reported for OPV3 and DTP3 (65.5%).
Table 4. Timeliness of Immunizations in Children aged 0–5 y old, 2002–2007 in Pakistan.
| BCG | Polio | DTP | Measles | ||||||
|---|---|---|---|---|---|---|---|---|---|
| BCG % |
OPV0 % |
OPV1 % |
OPV2 % |
OPV3 % |
DTP1 % |
DTP2 % |
DTP3 % |
Measles 1 % |
|
| n | 1330 | 981 | 1213 | 1054 | 909 | 1199 | 1053 | 824 | 689 |
|
Earlya (estimated range)b |
- | - | 16.74 (6.68–34.54) |
10.67 (4.78–20.22) |
7.07 (3.04–14.24) |
14.93 (6.08–34.59) |
10.34 (4.61–19.74) |
7.09 (3.33–14.72) |
21.95 (8.27–42.67) |
|
Timely (estimated range) |
70.08 (50.75–77.59) |
77.06 (55.45–85.12) |
47.98 (35.94–39.49) |
36.42 (21.16–41.20) |
27.39 (14.57–32.50) |
48.96 (36.57–39.28) |
35.53 (20.96–40.88) |
27.39 (14.61–31.69) |
41.42 (29.32–42.67) |
|
Latec (estimated range) |
29.92 (22.41–49.25) |
22.94 (14.88–44.55) |
35.28 (25.97–57.38) |
52.90 (38.58–74.06) |
65.54 (53.26–82.39) |
36.11 (26.13–57.35) |
54.14 (39.38–74.44) |
65.52 (53.60–82.06) |
36.63 (28.01–49.06) |
Early defined as vaccine administered 3 d before due date calculated from birth. Estimated Range for immunization timeliness calculated using first and last day of each month as the individual's birth-date. Late defined as vaccine administered greater than 4 wk after due date calculated from birth.
Determinants of immunization completion
Receipt of one or more doses of maternal tetanus was the strongest determinant (Table 5) for immunization completion in the final adjusted models for immunization completion of OPV3 (OR 1.4, 95% CI: 1.1–1.6), DTP3 (OR 2.5, 95% CI: 2.1–3.0), and measles (OR 2.8, 95% CI: 2.3–3.4). The wealthiest quintile was nearly twice as likely to have completed DTP3 (OR 1.9, 95% CI: 1.3–2.7) and measles (OR 1.8, 95% CI: 1.2–2.7) immunizations compared with the lowest wealth quintile. While higher education for mothers was a strong determinant for completion of DTP3 (OR 1.9, 95% CI: 1.2–2.8) and measles (OR 2.4, 95% CI: 1.4–4.3) vaccinations compared with receiving no education, there were no differences in immunization completion. Age, gender, ethnicity, and antenatal visits were not associated with increased immunization completion.
Table 5. Determinants of Immunization Completion in Children aged 0–5 y old, 2002–2007 in Pakistan.
| OPV 3 | DTP 3 | Measles | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Unadjusted OR | 95% CI | Adjusted OR | 95% CI | Unadjusted OR | 95% CI | Adjusted OR | 95% CI | Unadjusted OR | 95% CI | Adjusted OR | 95% CI |
| Age | 1.00 | 1.00–1.00 | 1.00 | 1.00–1.00 | 1.00 | 1.00–1.00 | 1.00 | 1.00–1.00 | 1.00 | 1.00–1.00 | ||
|
Gender (male reference) |
0.94 | 0.81–1.08 | 0.88 | 0.79–0.99 | 0.87 | 0.74–1.02 | 0.92 | 0.82–1.04 | 0.84 | 0.70–1.01 | ||
| Ethnicity | ||||||||||||
| Balochi (reference group) |
||||||||||||
| Punjabi | 1.33 | 0.93–1.89 | 3.37 | 2.47–4.60 | 1.68 | 1.15–2.45 | 3.50 | 2.34–5.23 | 1.71 | 1.13–2.57 | ||
| Mohajir | 1.76 | 1.15–2.70 | 4.20 | 2.82–6.28 | 1.36 | 0.85–2.19 | 3.95 | 2.48–6.29 | 1.13 | 0.65–1.95 | ||
| Sindhi | 1.32 | 0.91–1.91 | 1.46 | 1.03–2.06 | 1.02 | 0.67–1.55 | 1.19 | 0.78–1.82 | 0.82 | 0.53–1.27 | ||
| Pushto | 0.92 | 0.64–1.33 | 2.03 | 1.43–2.90 | 1.58 | 1.05–2.36 | 1.71 | 1.09–2.67 | 1.31 | 0.84–2.05 | ||
| Seraiki | 1.53 | 1.02–2.30 | 1.15 | 0.83–1.61 | 0.87 | 0.59–1.28 | 1.06 | 0.70–1.61 | 0.86 | 0.57–1.30 | ||
| Other | 0.93 | 0.63–1.39 | 1.44 | 0.99–2.11 | 1.06 | 0.70–1.62 | 1.50 | 0.95–2.35 | 1.22 | 0.76–1.94 | ||
| Urban vs rural | 1.22 | 1.03–1.44 | 2.00 | 1.69–2.37 | 2.14 | 1.77–2.58 | ||||||
| Wealth | ||||||||||||
| Lowest quintile (reference) | ||||||||||||
| 2nd Quintile | 1.20 | 0.96–1.51 | 1.24 | 0.90–1.47 | 1.60 | 1.28–1.99 | 1.18 | 0.93–1.51 | 1.53 | 1.21–1.93 | 1.19 | 0.92–1.55 |
| 3rd Quintile | 1.20 | 0.97–1.48 | 1.15 | 0.91–1.45 | 2.45 | 1.96–3.06 | 1.39 | 1.08–1.80 | 2.66 | 2.09–3.38 | 1.47 | 1.11–1.95 |
| 4th Quintile | 1.50 | 1.18–1.91 | 1.23 | 0.92–1.64 | 0.9754716 1.60 | 3.04–4.82 | 1.74 | 1.33–2.28 | 4.17 | 3.26–5.33 | 1.93 | 1.44–2.58 |
| Highest quintile | 2.00 | 1.53–2.60 | 1.46 | 1.01–2.11 | 5.68 | 4.35–7.42 | 1.88 | 1.31–2.70 | 5.94 | 4.41–8.00 | 1.77 | 1.17–2.67 |
| Telephone connection | 1.07 | 0.99–1.15 | 1.10 | 1.03–1.17 | 1.15 | 1.07–1.24 | ||||||
| Household Size | 1.00 | 0.98–1.01 | 1.00 | 0.98–1.01 | 0.99 | 0.98–1.01 | ||||||
| Children 5 and under | 0.97 | 0.92–1.02 | 0.97 | 0.92–1.02 | 0.95 | 0.90 -1.01 | ||||||
| Maternal education | ||||||||||||
| None (reference) | ||||||||||||
| Primary | 1.31 | 1.01–1.71 | 1.17 | 0.90–1.50 | 2.35 | 1.93–2.88 | 1.37 | 1.08–1.73 | 2.31 | 1.83–2.90 | 1.25 | 0.97–1.62 |
| Secondary | 1.76 | 1.36–2.29 | 1.20 | 0.88–1.63 | 3.31 | 2.64–4.14 | 1.55 | 1.21–2.00 | 3.89 | 2.96–5.11 | 1.62 | 1.18–2.22 |
| Higher | 2.16 | 1.49–3.14 | 1.57 | 0.98–2.52 | 5.43 | 4.06–7.27 | 1.85 | 1.23–2.79 | 7.08 | 4.81–10.41 | 2.43 | 1.38–4.29 |
| Received maternal tetanus | 1.59 | 1.35–1.86 | 1.35 | 1.14–1.60 | 3.36 | 2.84–3.96 | 2.54 | 2.13–3.02 | 3.76 | 3.08–4.59 | 2.78 | 2.27–3.40 |
|
Breastfeeding (mo) |
1.01 | 1.00–1.01 | 1.00 | 1.00–1.00 | 0.99 | 0.99–1.00 | ||||||
| Female head of Household | 0.93 | 0.72–1.22 | 1.23 | 0.95–1.61 | 1.06 | 0.78–1.43 | 1.36 | 1.03–1.79 | 1.33 | 0.95–1.86 | ||
| Hospital delivery | 1.17 | 1.00–1.36 | 2.17 | 1.89–2.49 | 1.12 | 0.93–1.34 | 2.42 | 2.07–2.82 | 1.23 | 1.01–1.50 | ||
| Antenatal visits | ||||||||||||
| 0 (reference) | ||||||||||||
| 1–5 | 1.31 | 1.11–1.54 | 1.04 | 0.87–1.25 | 1.87 | 1.57–2.22 | 1.14 | 0.94–1.40 | 1.94 | 1.61–2.33 | 1.08 | 0.87–1.32 |
| 6–10 | 1.66 | 1.26–2.19 | 1.08 | 0.78–1.49 | 3.27 | 2.50–4.26 | 1.26 | 0.92–1.73 | 3.70 | 2.74–4.99 | 1.25 | 0.88–1.77 |
| >10 | 1.63 | 0.91–2.92 | 0.99 | 0.54–1.80 | 4.94 | 2.95–8.26 | 1.59 | 0.87–2.90 | 6.42 | 3.07–13.43 | 1.55 | 0.68–3.53 |
| Goodness of fit F-statistic (P value) |
0.64 (0.76) |
1.08 (0.37) |
0.28 (0.98) |
|||||||||
Discussion
Pakistan faces a number of important challenges in improving immunization coverage. However, constraints in estimating vaccination coverage are not commonly cited as an important consideration. The rapid spread of a recent measles outbreak in the country in high immunization coverage areas as reported by EPI, underscores the limitations of the current approach. While certain reports have attributed this to erroneous reporting, it may also be possible that due to programmatic constraints, current data collection is insufficiently detailed and inadequate for effective coverage estimation and for decision-making. Since such approaches are unable to capture robust, individual level data with appropriate assessments of defaulting children and immunization timeliness, accurate estimation of effective immunization coverage may not be possible and program implementers may not have the necessary information to intervene in areas at risk for outbreaks.16,17
The Demographic and Health Surveys provided the most representative national samples of immunization coverage available and also allow for regional comparisons. The 2007 DHS from Bangladesh, reported a DTP3 coverage of 91.1%, OPV3 coverage of 90.8% and measles coverage of 83.1%, all of which were higher than those reported from Pakistan.18 The 2006 National Health Survey from India showed coverage rates that were comparatively similar to Pakistan’s, reporting a DTP3 coverage of 55.3%, OPV3 coverage of 73.2% and a measles coverage of 58.8%.19 Among surveys conducted in Pakistan, an EPI performance evaluation by the World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) determined immunization coverage of approximately 80% for both DTP3 and measles in 2006.4 The Pakistan Social and Living Standards Measurement Survey in 2006 showed DTP3 coverage of 82% and measles coverage of 77%.5
Our findings based on the Pakistan 2006 DHS data set suggest significantly lower immunization coverage than previously reported. Across provinces, coverage of DTP, in particular of the third dose, was considerably lower than polio immunizations (55.9% for DTP3 compared with 80% for OPV3). The steady decline in coverage of immunizations from birth suggests a constantly increasing dropout rate. Efforts will be required to ensure newborns and infants, once enrolled, continue to return to immunization centers. This is especially important to decrease the need for mass immunization catch-up campaigns in areas of low-coverage or following outbreaks. Mass-immunization campaigns are resource-intensive and frequently target a single vaccine, most frequently polio or measles. The modestly higher measles coverage observed in the DHS data set as compared with DTP3 suggests that they have not be effective in significantly improving or sustaining high measles coverage.
Immunization timeliness is not analyzed as part of routine EPI assessments and to the best of our knowledge this paper presents the most extensive such analysis from Pakistan. Late immunizations impact child survival by extending the period of time an infant remains vulnerable to diseases.20 Our results suggest that the delays progressively increase for DTP and OPV immunizations. Since these vaccines require a minimum of a 4-wk interval between doses, infants delayed for the first doses remain delayed for subsequent age-appropriate immunizations. Another study from Pakistan similarly observed timely immunization of DTP1 helped ensure timeliness for DTP2 and DTP3.21 Efforts therefore need to be made to ensure that DTP1 immunizations are timely so that infants are not delayed for the follow-up doses. Our findings also suggest early immunizations are an important problem in Pakistan, particularly for measles where over one-fifth of immunizations were early. EPI recommendations allow for measles immunizations as early as 6 mo of age during supplementary immunization campaigns, however, 9 mo is the recommended age during routine immunizations. While immunization campaigns seek to target large number of infants, the older age recommendation for routine immunizations aims for greater immune response to the vaccine. Immunizations administered before 9 mo have therefore been classified as early since infants may not be adequately protected for measles. Other causes of early immunizations require greater investigation but may be attributed to a lack of refresher trainings for vaccinators, inappropriate counseling provided by vaccinators, incorrect assignment of due-dates, seasonal migration between urban and rural areas and administration of immunizations during other health visits in infancy. Importantly, early immunization events are captured as part of coverage estimates resulting in overestimated vaccination coverage. Periodic assessments of immunization timeliness should therefore be introduced to help further identify priority areas of low coverage or those at risk of outbreaks. Greater understanding of the causes of early immunizations and developing strategies to address this issue will help EPI with cost-savings over the longer term.
Our study showed that receiving at least one dose of maternal tetanus immunizations was the strongest determinant for completing the final doses of OPV and DTP as well as the measles immunizations. This may seem naturally intuitive but is of relevance given that much of the current debate is focused around differences in childhood immunization coverage due to ethnicity, education, income status, and health access.11,22,23 Studies that have previously investigated determinants of immunization from Pakistan have attributed differences in coverage to socioeconomic and ethnic variables.21,24,25 Furthermore, although our findings suggest maternal education is important, no significant differences were observed between education levels. The degree to which maternal tetanus immunization is associated with childhood immunization completion, after adjusting for the effects of confounders suggests that providing immunization services to the mother during the antenatal period may lead to better immunization outcomes for the child. This supports the increasing body of literature for the integration of child health services as part of a continuum of maternal, neonatal, and child healthcare (MNCH). Integration of immunization services with comprehensive MNCH can also help bridge the trust deficit that is crucially lacking in many communities where outreach immunization services are the often the only form of government supported healthcare.
If Pakistan is to meet its development targets, including those for immunizations and child-survival, it must build a consensus toward innovation in vaccine services delivery or risk failure. Similar to other public health programs across the developing world, EPI suffers from persistent failures in key areas of service delivery such as logistics and supply-chain management, poor health-worker motivation and incentives, fragmented governance, and limited accountability, inadequate information systems for decision-making, inadequate integration with other primary-health care services, low population awareness and limited focus on demand creation. Novel approaches to increasing routine immunization coverage warrant consideration. In response to poor quality of care at public facilities, private healthcare has rapidly increased in the country and accounts for nearly three-quarters of all healthcare expenditure.26 It is essential to harness these additional resources (e.g., infrastructure, personnel) and leverage operational efficiencies in private healthcare delivery (e.g., performance driven remuneration) to improve supply-side constraints by realigning incentives toward public health. Private sector engagement could range from cooperative ventures around improving reporting processes through use of mobile health technology to formalized partnerships for performance-based awards to private-sector facilities. Currently, public-private initiatives are at best limited in their scale and routine immunization remains disproportionately within the domain of the public sector (over 95% of childhood immunizations).4 Greater alignment between the 2 could significantly reduce fragmentation of services, and as our results suggest, integration with pubic and private MNCH services may have positive impacts on immunization completion. Other health market innovations such as condition-cash transfers and incentives linked to immunizations have been shown to increase immunization uptake in Pakistani communities.9,27 Innovative strategies such as the use of SMS Reminders may help prevent dropout rates and improve timeliness of immunizations.28 Vouchers for future healthcare or other types of health insurance in exchange for routine immunizations and antenatal healthcare are also being explored.29
This study was limited by the constraints of a cross-sectional survey including potential sampling errors, selection biases and historical recall of the mother as the primary source for assessing immunization coverage. As data collection was performed in 2006–07, the analysis is not representative of current trend of childhood immunization coverage in Pakistan, but illustrative of systematic challenges. Similar analyses using the DHS data sets may therefore be of benefit if applied to other countries in particular where routine reporting systems are of poor quality. The absence of a day of birth for children prevented more accurate calculations of coverage and timeliness of immunizations. However, sensitivity analysis suggests variance in estimated timeliness does not significantly affect the overall findings. Finally, a cross-sectional analysis prevented establishment of causation of the observed associations. Further prospective-design studies investigating association of maternal tetanus administration on subsequent childhood immunizations are needed to confirm and better understand this positive association. Randomized evaluations of interventions such as conditional-cash transfers, SMS text reminders, and immunization counseling initiated at maternal tetanus doses compared with those initiated at BCG may also provide further insight on the impact of maternal immunizations on childhood immunizations.
Conclusion
Pakistan has poor up-to-date routine immunization coverage, and ensuring timely administration for the first doses of DTP and OPV can reduce delayed immunizations. Emphasis on early childhood immunizations, increased access to antenatal care, incorporation of tetanus immunizations as standard of care during antenatal visits and appropriate counseling during maternal tetanus immunization campaigns could improve immunization coverage in Pakistan.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Financial Disclosure
This study did not receive any institutional support or external funding.
Glossary
Abbreviations:
- AIC
Akaike's Information Criteria
- DHS
Demographic and Health Surveys
- BCG
Bacillus Calmette–Guérin
- DTP1
diphtheria, tetanus and pertussis first dose
- DTP2
diphtheria, tetanus and pertussis, second dose
- DTP3
diphtheria, tetanus and pertussis, third dose
- EPI
Expanded Programme on Immunization
- KPK
Khyber-Pakhtunkhwa
- MNCH
maternal, neonatal and child healthcare
- OPV0
oral polio vaccine at birth
- OPV1
oral polio vaccine first dose
- OPV2
oral polio vaccine second dose
- OPV3
oral polio vaccine third dose
- SMS
Short Message Service
- UNICEF
United Nations Children’s Fund
- WHO
World Health Organization
References
- 1.United Nations Department of Economic and Social Affairs-Population Division. [cited 11/12/2012]. Available from: http://www.unpopulation.org.
- 2.Ahmad R, Alvi SS, Hassan M, Kamin M, Malik M, Sarwar L, Sohail H, Wahab H, Zafar M, Iqbal S. Availability of expanded programme of immunization services provided to children in a rural Pakistani village. J Pak Med Assoc. 2011;61:415–8. [PubMed] [Google Scholar]
- 3.Siddiqi N, Khan A, Nisar N, Siddiqi AE. Assessment of EPI (expanded program of immunization) vaccine coverage in a peri-urban area. J Pak Med Assoc. 2007;57:391–5. [PubMed] [Google Scholar]
- 4.Hasan Q, Bosan AH, Bile KM. A review of EPI progress in Pakistan towards achieving coverage targets: present situation and the way forward. East Mediterr Health J. 2010;16(Suppl):S31–8. [PubMed] [Google Scholar]
- 5.Masud T, Navaratne KV. The expanded program on immunization in pakistan. recommendations for Improving performance. Health, nutrition and population (HNP) discussion paper. The World Bank. 2012. Available from: http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627-1095698140167/EPIinPakistan.pdf
- 6.Fadnes LT, Jackson D, Engebretsen IM, Zembe W, Sanders D, Sommerfelt H, Tylleskär T, PROMISE-EBF Study Group Vaccination coverage and timeliness in three South African areas: a prospective study. BMC Public Health. 2011;11:404. doi: 10.1186/1471-2458-11-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andersson N, Cockcroft A, Ansari NM, Omer K, Baloch M, Ho Foster A, et al. Evidence-based discussion increases childhood vaccination uptake: A randomised cluster controlled trial of knowledge translation in pakistan. BMC Int Health Hum Rights. 2009 Oct 14;9 Suppl 1:S8 [DOI] [PMC free article] [PubMed]
- 8.Anjum Q, Omair A, Inam SN, Ahmed Y, Usman Y, Shaikh S. Improving vaccination status of children under five through health education. J Pak Med Assoc. 2004;54:610–3. [PubMed] [Google Scholar]
- 9.Chandir S, Khan AJ, Hussain H, Usman HR, Khowaja S, Halsey NA, Omer SB. Effect of food coupon incentives on timely completion of DTP immunization series in children from a low-income area in Karachi, Pakistan: a longitudinal intervention study. Vaccine. 2010;28:3473–8. doi: 10.1016/j.vaccine.2010.02.061. [DOI] [PubMed] [Google Scholar]
- 10.Owais A, Hanif B, Siddiqui AR, Agha A, Zaidi AK. Does improving maternal knowledge of vaccines impact infant immunization rates? A community-based randomized-controlled trial in Karachi, Pakistan. BMC Public Health. 2011;11:239. doi: 10.1186/1471-2458-11-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loevinsohn B, Hong R, Gauri V. Will more inputs improve the delivery of health services? Analysis of district vaccination coverage in Pakistan. Int J Health Plann Manage. 2006;21:45–54. doi: 10.1002/hpm.824. [DOI] [PubMed] [Google Scholar]
- 12.Usman HR, Akhtar S, Habib F, Jehan I. Redesigned immunization card and center-based education to reduce childhood immunization dropouts in urban Pakistan: a randomized controlled trial. Vaccine. 2009;27:467–72. doi: 10.1016/j.vaccine.2008.10.048. [DOI] [PubMed] [Google Scholar]
- 13.National institute of population studies (NIPS) [pakistan], and macro international inc. 2008. Pakistan demographic and health survey 2006-07. Iislamabad, Pakistan: National Institute of Population Studies and Macro International Inc. Available from: http://dhsprogram.com/pubs/pdf/FR200/FR200.pdf
- 14.Expanded programme on immunization (EPI). Immunization schedules in the WHO eastern Mediterranean region, 1995. Wkly Epidemiol Rec. 1996;71:173–6. [PubMed] [Google Scholar]
- 15.Archer KJ, Lemeshow S, Hosmer DW. Goodness-of-fit tests for logistic regression models when data are collected using a complex sampling design. Comput Stat Data Anal. 2007;2007:4450–64. doi: 10.1016/j.csda.2006.07.006. [DOI] [Google Scholar]
- 16.Riaz H. Public health failings behind Pakistan’s measles surge. Lancet. 2013;381:189. doi: 10.1016/S0140-6736(13)60072-0. [DOI] [PubMed] [Google Scholar]
- 17.Kazi AN. Measles epidemic exposes inadequate vaccination coverage in Pakistan. BMJ. 2013;346:f245. doi: 10.1136/bmj.f245. [DOI] [PubMed] [Google Scholar]
- 18.National Institute of Population Research and Training (NIPORT), Mitra and Associates, and Macro International. 2009. Bangladesh: demographic and health survey 2007. Dhaka, Bangladesh and Calverton, Maryland, USA: National Institute of Population Research and Training, Mitra and Associates, and Macro International. Available from: http://www.unicef.org/bangladesh/BDHS2007_Final.pdf
- 19.International Institute for Population Sciences (IIPS) and Macro International. 2007. National Family Health Survey (NFHS-3), 2005–06: India: Volume I. Mumbai: IIPS. Available from: http://dhsprogram.com/pubs/pdf/SR128/SR128.pdf
- 20.Akmatov MK, Mikolajczyk RT. Timeliness of childhood vaccinations in 31 low and middle-income countries. J Epidemiol Community Health. 2012;66:e14. doi: 10.1136/jech.2010.124651. [DOI] [PubMed] [Google Scholar]
- 21.Usman HR, Rahbar MH, Kristensen S, Vermund SH, Kirby RS, Habib F, Chamot E. Randomized controlled trial to improve childhood immunization adherence in rural Pakistan: redesigned immunization card and maternal education. Trop Med Int Health. 2011;16:334–42. doi: 10.1111/j.1365-3156.2010.02698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saleem T. Improving childhood vaccination: roadblocks and hurdles. J Pak Med Assoc. 2010;60:791. [PubMed] [Google Scholar]
- 23.Mitchell S, Andersson N, Ansari NM, Omer K, Soberanis JL, Cockcroft A. Equity and vaccine uptake: A cross-sectional study of measles vaccination in lasbela district, Pakistan. BMC Int Health Hum Rights. 2009 Oct 14;9 Suppl 1:S7 [DOI] [PMC free article] [PubMed]
- 24.Usman HR, Kristensen S, Rahbar MH, Vermund SH, Habib F, Chamot E. Determinants of third dose of diphtheria-tetanus-pertussis (DTP) completion among children who received DTP1 at rural immunization centres in Pakistan: a cohort study. Trop Med Int Health. 2010;15:140–7. doi: 10.1111/j.1365-3156.2009.02432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siddiqui NT, Owais A, Agha A, Karim MS, Zaidi AK. Ethnic disparities in routine immunization coverage: a reason for persistent poliovirus circulation in Karachi, Pakistan? Asia Pac J Public Health. 2014;26:67–76. doi: 10.1177/1010539513475648. [DOI] [PubMed] [Google Scholar]
- 26.Nishtar S. The Gateway Paper--financing health in Pakistan and its linkage with health reforms. J Pak Med Assoc. 2006;56(Suppl 4):S25–42. [PubMed] [Google Scholar]
- 27.Rawlings LB. A new approach to social assistance: Latin America's experience with conditional cash transfer programs. Social Protection Discussion papers 30165, the World Bank. 2004. Available from: http://info.worldbank.org/etools/docs/library/49187/0416.pdf
- 28.Wakadha H, Chandir S, Were EV, Rubin A, Obor D, Levine OS, Gibson DG, Odhiambo F, Laserson KF, Feikin DR. The feasibility of using mobile-phone based SMS reminders and conditional cash transfers to improve timely immunization in rural Kenya. Vaccine. 2013;31:987–93. doi: 10.1016/j.vaccine.2012.11.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA. 2007;298:1900–10. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]