Abstract
Objective: The aim of this study was to examine the prevalence and experience of early childhood caries among 5- to 6-year-old children in Southeast Asia. Methods: A literature search was conducted of three electronic databases (PubMed, EMBASE and ISI Web of Science) to identify publications from the years 2006 to 2015. Additional hand searches of government reports and national studies were performed. Both primary and secondary data sources were included in the study. The inclusion criterion was the findings reported on the caries prevalence and/or caries experience in decayed, missing or filled tooth (dmft) or decayed, missing or filled surface (dmfs) scores of 5- to 6-year-old children in Southeast Asian countries. The papers retrieved were assessed by two independent reviewers, and the final decision was made by consensus. Results: The search identified 320 papers for screening; 293 were excluded and 27 full papers were retrieved and reviewed. Of those, 12 were included. Among the countries, variations were found in caries prevalence and caries experience. The caries prevalence of 5- to 6-year-old children ranged from 25% to 95%, and the caries experience (given as mean dmft score) ranged from 0.9 to 9.0. The median caries prevalence and caries experience (mean dmft score) of children 5–6 years of age were 79% and 5.1, respectively. Conclusion: Based on the included studies, which are limited in quality and quantity, there is evidence that caries prevalence and experience are high amongst preschool children in Southeast Asia.
Key words: Dental caries, preschool children, primary teeth, Southeast Asia
Introduction
Dental caries affecting the primary teeth in preschool children [also known as early childhood caries (ECC)] is prevalent, especially among underprivileged groups in developing countries1., 2.. Dental caries has often been described as a global pandemic disease characterised by a high proportion of untreated carious lesions3. ECC can affect the general health of children, as well as their quality of life4. Such problems are potentially serious, and may even be life-threatening5. Although the caries status of permanent teeth in 12-year-old children in the Southeast Asian region has been documented in the database of the World Health Organization (WHO)6, epidemiological data on ECC are limited. Studies have reported trends of ECC in Arab League countries7, Latin America and the Caribbean8, but there are no such findings for Southeast Asian countries.
In Southeast Asia, there are around 600 million people, or approximately 9% of the world's population, with Indonesia having the largest population in the region and the fourth largest population in the world9. The demographic, socio-economic and health-care profiles of the Southeast Asian countries are summarised in Table 1. The definition of ‘Southeast Asia’ mostly refers to the areas represented by 11 sovereign states, namely Brunei, Burma (Myanmar), Cambodia, Indonesia, Lao People's Democratic Republic (Lao PDR), Malaysia, Philippines, Singapore, Thailand, Vietnam and Timor-Leste (East Timor)10. Ten countries (all except Timor-Leste) are members of the Association of Southeast Asia Nations (ASEAN)11. Most countries in Southeast Asia are classified as developing countries, which are defined according to their gross national income (GNI) per capita per year of US$ 11,905 or less12. The diversity in economics and politics across and within countries in Southeast Asia may contribute to the disparate health status and the diversity of the health systems, which are at different stages of evolution9.
Table 1.
Profiles of Southeast Asian countries
| Country | Capital name | Land (km2) | Population | Life expectancy (year) | Underweight of children under 5 years (%) | Health expenditure (% of GDP) | GDP per capita (PPP) USD | GNI per capita USD53 |
|---|---|---|---|---|---|---|---|---|
| Brunei Darussalam | Bandar Seri Begawan | 5,765 | 430,000 | 77 | – | 2.5 | 73,200 | 37,320 |
| Cambodia | Phnom Penh | 181,035 | 15,709,000 | 64 | 29 | 7.5 | 3,300 | 1,020 |
| Indonesia | Jakarta | 1,904,569 | 255,994,000 | 72 | 20 | 3.1 | 10,600 | 3,630 |
| Lao PDR | Vientiane | 236,800 | 6,912,000 | 64 | 27 | 2 | 5,000 | 1,650 |
| Malaysia | Kuala Lumpur | 329,847 | 30,514,000 | 75 | 13 | 4 | 24,700 | 10,760 |
| Myanmar | Yangon | 676,578 | 56,320,000 | 66 | 23 | 1.8 | 4,700 | 1,270 |
| Philippines | Manila | 300,000 | 100,998,000 | 69 | 20 | 4.4 | 7,000 | 3,470 |
| Singapore | Singapore | 697 | 5,674,000 | 85 | – | 4.6 | 82,800 | 55,150 |
| Thailand | Bangkok | 513,120 | 67,946,000 | 74 | 9 | 4.6 | 14,400 | 5,370 |
| Timor Leste | Dili | 14,874 | 1,231,000 | 68 | 45 | 1.3 | 4,900 | 3,120 |
| Vietnam | Hanoi | 331,210 | 94,349,000 | 73 | 12 | 6 | 5,600 | 1,890 |
Source of information: www.cia.gov54.
GDP (PPP), gross domestic product (purchasing power parity); GNI, gross national income; USD, US dollars.
In 2006, the Global Child Dental Health Taskforce (GCDHT) was established in response to the Declaration on Child Oral Health that was signed by the chief dental officers of most European countries, along with a representative from the WHO13. The GCDHT aims to raise the profile of the global crisis of dental caries among disadvantaged children. In addition, global goals for oral health in 2020 have been recently established by the WHO, World Dental Federation (FDI) and the International Association of Dental Research (IADR)14. A summary of epidemiological data for oral diseases is required to determine risks to populations, respond with prevention and intervention, and plan for the future. Small epidemiological surveys carried out in Cambodia (2003–2007)15 and in Lao PDR (2010)16 indicate that the prevalence of ECC is very high. Because the cultural and social contexts of the health system in Southeast Asia are unique, up-to-date oral health data from the region are needed in order to develop effective oral health programmes that are suitable for the needs of Southeast Asian populations. This study aimed to summarise the updated data about the caries prevalence and severity of ECC of 5- to 6-year-old children in Southeast Asia. The term ‘ECC’ in the present study was defined as the presence of one or more decayed cavitated lesions or missing (as a result of caries) or filled tooth surfaces in any primary tooth in a child 5–6 years of age.
Materials and Methods
Search strategy
Identification of studies to be considered for inclusion was based on a systematic search of three common electronic databases (PubMed, EMBASE and ISI Web of Science). The keywords and MeSH headings were combined using three main concepts: Dental caries [MeSH Terms] AND Children [MeSH Terms] AND Southeast Asia [MeSH Terms] OR Thailand [MeSH Terms] OR Cambodia [MeSH Terms] OR Vietnam [MeSH Terms] OR Indonesia [MeSH Terms] OR Malaysia [MeSH Terms] OR Singapore [MeSH Terms] OR Philippines [MeSH Terms] OR Brunei [MeSH Terms] OR Myanmar [MeSH Terms] OR ‘Lao PDR’ OR ‘Laos’ OR East Timor [MeSH Terms]. The search was restricted to reports written in English. Data from secondary sources, such as government reports, conference proceedings and statistics, accessed through the websites of national institutes, were searched. Additional records were identified by contacting the delegates of the Southeast Asian delegates in the South East Association for Dental Education (SEAADE). Inclusion and exclusion criteria were applied by examining the title and abstract. Lists of eligible references were manually searched.
Study selection
Publications were included if they fulfilled the following inclusion criteria:
-
•
Cross-sectional studies or prospective cohort studies
-
•
Primary or secondary data analyses
-
•
Papers published from 2006–2015
-
•
Examination of children, 5–6 years of age, in Southeast Asian countries
-
•
Reporting caries prevalence and/or caries experience of primary teeth. Caries prevalence was expressed as a percentage of the child population affected by dental caries, whereas caries experience of primary teeth was expressed as mean decayed, missing and filled teeth or tooth surfaces (dmft and/or dmfs score).
The literature searches of the three common electronic databases were performed independently by two reviewers (D.D. and S.S.G.). Titles and abstracts of the publications were identified for eligibility. Papers were excluded if a group of samples was not reasonably representative of the general population of children, such as groups of disabled children. Data of randomised controlled clinical trials were excluded. Where doubts existed over the inclusion of a study based on the title or abstract, the full paper was retrieved. For example, if the abstract reported a wide range of participant ages, the full text of this article was retrieved and then checked for available data (children 5 and 6 years of age) for subgroup analysis. Duplicated reports or studies using the same data were excluded.
In addition, the references of the included studies considered eligible were searched manually in order to find other relevant studies in the final analysis. A summary of each record was made according to: (i) countries; (ii) sources of information (year of publication); (iii) area/detail of study; (iv) year of survey; (v) sampling method; (vi) caries diagnostic criteria; (vii) sample size; (viii) age of participants; (ix) caries prevalence (expressed in per cent); and (x) mean dmft score.
Results
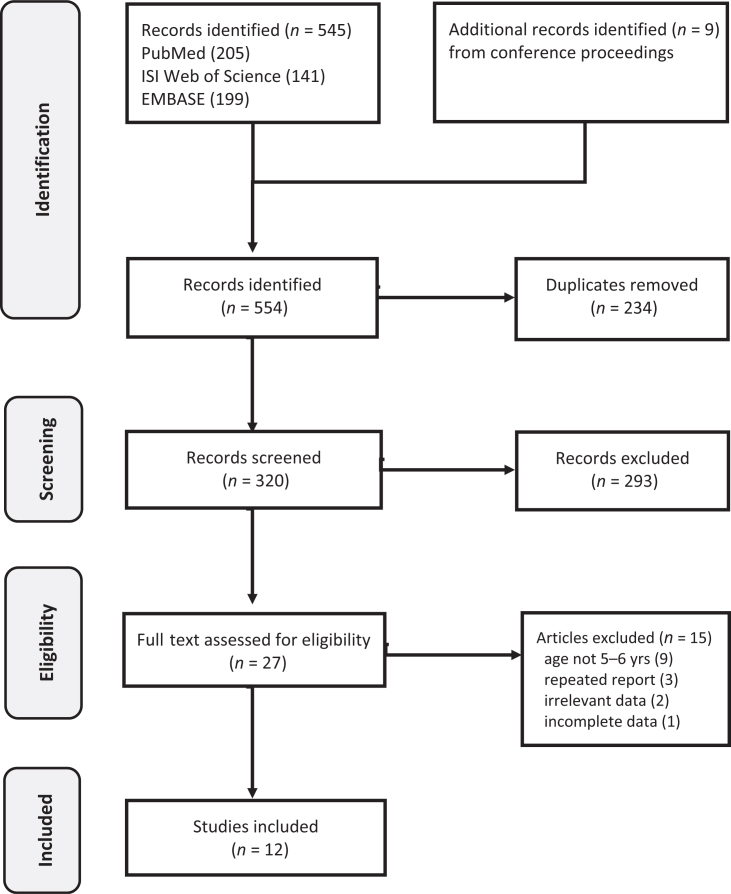
A total of 545 publications were found in the literature search of the three databases (PubMed, EMBASE and ISI Web of Science). Nine additional records from conference proceedings were identified. From this, 320 de-duplicated records were screened manually on the basis of the title, keywords and abstract. Among these, 293 did not meet the inclusion criteria, such as reporting only caries status in permanent teeth, being published in earlier years and assessing the oral health of children with disabilities. Consequently, 27 full papers were retrieved and reviewed. No cross-referencing studies were found. Of these 27 papers, 15 were excluded, the majority because of the ages of the children studied and repeated data. The remaining 12 publications were included in the present study. A flow chart of identification and study selection is shown in Figure 1.
Figure 1.
Flow diagram for identification, screening and study selection.
The details contained in the included studies on the caries status of primary teeth in preschool children are summarised in Table 2. Of the 12 studies included, only four (33%) were primary data analyses15., 17., 18., 19.. Regarding the data from secondary sources, data of national oral health surveys on preschool children were found for five countries, namely Malaysia, Thailand, Philippines, Lao PDR and Cambodia. All included studies reported both caries prevalence and experience (dmft score). Most (92%) of the included studies indicated the year of the survey. Regarding the type of study, all were cross-sectional. Of 12 studies, only four (33%) described the sampling methods and caries diagnostic criteria15., 17., 18., 19..
Table 2.
Caries prevalence and caries experience in primary teeth of 5- to 6-year-old children in Southeast Asia
| Country | Authors/year | Area/details of study | Year of survey | Sampling method | Diagnostic criteria | Sample size | Age/year | % Caries | dmft (SD) |
|---|---|---|---|---|---|---|---|---|---|
| Brunei Darussalam | Hua20 | Schools | 2012 | – | – | – | 5 | 59 | 3.9 |
| Cambodia | Souen et al.28 | National Oral Health Survey | 2011 | – | – | – | 5–6 | 93 | 9.0 |
| Chu et al.15 | Rural areas | 2003–2007 | Convenience sample | WHO | 120 | 6 | 91 | 7.9 (5.2) | |
| Indonesia | – | – | – | – | – | – | – | – | – |
| Lao PDR | Phommavongsa & Senesombath27 | National Oral Health Survey | 2010 | – | – | – | 6 | 89 | 8.0 |
| Malaysia | Khairiyah et al.21 | National Oral Health Survey | 2007 | – | – | – | 6 | 75 | 3.9 |
| Myanmar | Chu et al.18 | Rural areas | 2009 | Convenience sample | WHO | 95 | 5 | 25 | 0.9 (2.3) |
| San22 | City areas | 2006–2007 | – | – | 1,571 | 5 | 75 | 4.6 | |
| Philippines | Centeno26 | National Oral Health survey | 2011 | – | – | 586 | 5 | 88 | 5.6 |
| Singapore | Gao et al.17 | Kindergartens in Singapore | 2005 | Stratified cluster random sample | WHO | 697 | 5–6 | 49 | 2.0 (3.1) |
| Thailand | Krisdapong et al.19 | Bangkok | – | Stratified cluster random sample | WHO | 503 | 5–6 | 79 | 6.2 (5.2) |
| Jienmaneechotechai et al.23 | National Oral Health Survey | 2012 | – | – | – | 5–6 | 79 | 4.4 | |
| Timor-Leste | – | – | – | – | – | – | – | – | – |
| Vietnam | Hai & Khanh25 | Hanoi and Lao Cai | 2007 | – | – | 75 | 6 | 95 | 6.3 |
| FluoridatedA and non-fluoridatedB areas in Ho Chi Minh | 2010 | – | – | – | 5 | 62A 84B |
3.4A 6.8B |
A, Fluoridated area; B, Non-fluoridated area; dmft, decayed, missing and filled teeth index for the primary dentition; SD, standard deviation; WHO, World Health Organisation.
Within the included studies published in 2006–2015, there was a wide range of caries prevalence (25–95%) and caries experience (dmft score = 0.9–9.0) in 5- to 6-year-old children in Southeast Asia; for the same age group, the median caries prevalence was 79% and caries experience (in dmft) was 5.1. In Singapore and Brunei, caries prevalence and caries experience (expressed as mean dmft score) of preschool children in Brunei and Singapore were lower than those of other countries in the region, while preschool children in the Philippines, Lao PDR and Cambodia had very high caries prevalence (>85%). The distribution of up-to-date-caries prevalence (%) and caries experience (mean dmft score) in 5- to 6-year-old children in Southeast Asian countries in 2006–2015 are shown in Figure 2.
-
•
Singapore: Caries prevalence was 49%. Caries experience in mean dmft and dmfs scores were 2.0 and 4.4, respectively17. Approximately 90% of the affected teeth were decayed teeth. A skewed distribution of dental caries was found
-
•
Brunei Darussalam: Only one review was found20. It reported a decline in caries prevalence in 5-year-old children from 89% in 1999 to 59% in 2012, and the mean dmft scores decreased from 7.0 to 3.9
-
•
Malaysia: There was a national oral health survey on 6-year-old children in 200721. Caries prevalence decreased from 81% in 1997 to 75% in 2007. Overall, the mean dmft score was 3.9 in 2007. The ‘filling’ component (0.5) remained quite low, indicating a treatment need in relation to the high ‘decay’ component (3.2) in young children in Malaysia
-
•
Myanmar: There was no report on the national oral health survey. However, there were oral health surveys sponsored by an international organisation (Asia Oral Health Promotion Fund) in collaboration with the Myanmar Dental Association. Caries prevalence varied between 25% and 75%, with the mean dmft scores ranging between 0.9 and 4.618., 22.
-
•
Thailand: National oral health surveys are conducted regularly (about every 5 years)23. The latest national survey, in 2012, showed that 79% of 5-year-old children had dental caries experience. Another study by Krisdapong et al.19 reported similar findings. Overall, dental caries was highly prevalent, with the mean dmft score ranging from 4.4 to 6.2
-
•
Vietnam: The national oral health survey published in 201124 was excluded as participants were older than 6 years of age. Only one review reported the caries status of preschool children in some provinces25. In Ho Chi Minh City, the caries prevalence of 5- to 6-year-old children in a non-fluoridated area was higher (84%) than that in a fluoridated area (63%). In Hanoi and Lao Cai provinces, caries prevalence was very high (95%), with a mean dmft score of 6.3
-
•
Philippines: A review of the national oral health survey in 2011 indicated that caries prevalence (88%) was high amongst 5-year-old children, with a mean dmft score of 5.626
-
•
Lao PDR: Results of the national oral health survey in 2010 reported high caries prevalence (89%), and the mean dmft score was 8.027
-
•
Cambodia: Two studies were identified in the literature search. Caries prevalence in both studies was over 90%, and the mean dmft scores of 5-year-old children ranged between 7.9 and 9.015., 28.. Very few primary teeth had been restored or extracted in Cambodia
-
•
Indonesia and Timor-Leste: No studies conducted on children 5–6 years of age were found.
Figure 2.
Caries prevalence (%) and caries experience [decayed, missing and filled teeth (dmft) index] of primary teeth in children 5–6 years of age in Southeast Asia in 2006–2015.
Discussion
This systematic review demonstrates a paucity of up-to-date data on the prevalence and severity of ECC in Southeast Asian countries in the last 10 years. Based on the data available and its limitations, the present review demonstrates high caries prevalence with a high level of caries severity (dmft score) for ECC in Southeast Asia. Compared with other countries in Asia, the prevalence of ECC in Southeast Asia was more likely to be higher than that in Hong Kong (51%)29, China (66%)30 and India (54%)31. When comparing the prevalence of ECC in developed countries, studies in Southeast Asia reported a much higher prevalence of ECC than those in developed countries, such as the USA (23%)32 or the UK (28%)33. Regarding the oral health status of children in other regions, a systematic review in Arab League countries reported a mean dmft score of 4.5 in 2- to 7- year-old children7. In South Africa and Swaziland, the prevalence of ECC among 5- to 6-year-old children was comparatively low (57%), and the mean dmft score was 3.1. Compared with these findings, the overall caries status of preschool children in Southeast Asian countries is worse than for those in diverse parts of the world. These high-caries-risk children, especially those from the less-developed countries in Southeast Asia, such as Cambodia and Lao PDR, should receive special attention. In addition, the high level of untreated caries in the primary dentition is of major concern. This phenomenon is almost universal in Southeast Asia. A recent systematic review indicated that untreated caries in primary teeth is prevalent, affecting over 600 million children worldwide34. Regrettably, studies on ECC and risk factors in Southeast Asia remain largely under-represented in the literature35, although this region shoulders a disproportionate caries burden36. Globally, oral disease is the fourth most expensive disease to treat; there is a challenge to develop effective oral health-care strategies in a way that respects cultural sensitivities and socio-economic constraints37.
Variations exist in the trends of ECC across countries. Within Southeast Asian countries, preschool children in countries with a low GNI (e.g. Cambodia and Lao PDR)12 are more likely to have higher caries prevalence than are those in countries with a high GNI (e.g. Singapore and Brunei). The results of the present review agree with Do38 that caries experience is more widespread within populations of lower socio-economic status. This may be a result of the distinct risk profiles across countries, such as availability of oral health care37, socio-economic status and probably a lack of political attention, particularly in low-income and middle-income countries39. The population-to-dentist ratio in Southeast Asia ranges widely, from 1,700 to 50,00040. Besides the shortage of dental health workers, problems of maldistribution of health professionals are present in all countries in Southeast Asia, and remote areas are often underserved and understaffed41. This calls for action and strategy to address the inequalities in child oral health in the region. Questions remain about how to improve the oral health of disadvantaged children in vulnerable communities. The results of this study could provide the updated baseline information that is an important prerequisite for oral professionals and policy makers when developing effective approaches for the child populations across the nations in Southeast Asia.
Certain limitations in the present review should be borne in mind when interpreting the results. The first is the age of the child population. Ideally, oral health surveys on primary dentition should be performed on children 5 years of age, as recommended by the WHO42, because at this age children have fully erupted primary teeth without natural tooth exfoliation. Studies on 6-year-old children were also considered in this review in order to include more data. For better comparison, a more specific age group may be needed because caries experience is more likely to increase with increasing age of children. In addition, data on younger children with incomplete primary dentition or on older children with mixed dentition may not be comparable with data on 5- to 6-year-old children. The second limitation is language bias, which might be present because we focussed on papers published in English. Although data of national oral health surveys might be accessible from the survey documentations in some countries, the language restriction of this review would preclude studies or national surveys that were not published in English. Only four studies that had collected primary data were found in the databases for the time period spanning 2006 to 2015. Surprisingly, no ECC study on children 5–6 years of age in Indonesia was found in this review, despite its relatively large population. Also, Timor-Leste, which is a new country, had no publications on ECC. Official statistics, such as national surveys published in English in peer-reviewed by journals, were also rare.
Fortunately, a number of publications included from the conference ‘Caries Control throughout Life in Asia’, held in Southeast Asia, were found and included in the review. Compared with primary data, secondary data, including information from the national population, are more likely to be representative. However, details of survey methods, such as sample size calculation, caries diagnostic criteria and calibration of examiners, were absent from the included studies that used secondary data. Owing to the methodological diversity of the oral health surveys and incomplete analyses of secondary data, further analysis could not be performed. It was also impossible to assess the quality of the included studies that used secondary data. Regarding the definition of ‘Southeast Asia’, 11 sovereign states, which are commonly recognised as Southeast Asian nations, were all included in this review. However, some small dependent territories, such as Christmas Island and the Coco Islands, which are geographically considered as part of Southeast Asia, were not included in the present study10. In addition, the scope of this review was limited to papers published in the last 10 years (2006–2015) in order to summarise the up-to-date information available on ECC. Any ECC trends in earlier years should not be extrapolated from the present findings.
Dental public health interventions need tailoring to achieve effective caries-prevention strategies and reduce any social gradient in oral health43. Despite the limitations discussed, this current systemic review thus fills an epidemiological information gap and can provide an updated overall picture of caries prevalence and level of caries severity in young children. Because of the lack of high quality studies and small numbers of oral health surveys in preschool children in Southeast Asia, methodologically rigorous surveys carried out at regular time intervals are needed to create a more accurate profile of ECC in the region. Common risk factors affecting ECC in Southeast Asia should be further investigated.
It is hoped that the results of the present study will help to raise awareness of the burden of ECC and inequalities in child oral health in Southeast Asia, as well as elicit interest and support of local government and other policy-making authorities in promoting oral health in this region. Population approaches to primary caries prevention are required. Because no cooperation of the population is needed, these measures have a significant impact, particularly in disadvantaged and deprived populations44. Water-fluoridation programmes have proven successful in dental caries reduction in many countries45. Similarly, the effect of water fluoridation on caries reduction was also reported in Southeast Asian countries, such as in Malaysia21, Brunei Darussalam20, Singapore17 and Vietnam25. Besides this population-based preventive measure, oral self-care by daily toothbrushing with a fluoridated toothpaste is important for preventing and arresting dental caries in preschool children46. Surprisingly, only 44% of 6-year-old children had brushed their teeth in Cambodia. Affordable fluoridated toothpaste should be promoted in less-developed nations. Well-organised community-based programmes and dissemination of appropriate oral health messages through different means should be combined to improve oral health in young children.
For secondary-prevention measures, advances in oral health science, which are usually unaffordable or inaccessible, may not benefit poor and disadvantaged child populations. Discerning how to manage the heavy burden of untreated dental caries in the young child population is challenging47. Caries management with minimally invasive approaches and low cost is of utmost importance. Atraumatic restorative treatment with high-viscosity glass ionomer cements and the use of silver diamine fluoride have recently been considered as therapeutic options for caries control in young children. This is because of their efficacy and feasibility of implementation in communities48., 49., 50.. More studies are needed to confirm the effectiveness of these interventions in high-caries-risk preschool children in Southeast Asia.
The lack of fully effective mechanisms for regional health cooperation remains in Southeast Asia51. Eliminating oral health inequalities cannot be accomplished by isolating oral health from overall health52. Framing oral health as an essential part of general health is required to integrate oral health into a broader global health that facilitates interactions with other health professions and with other public sectors. In addition, partnerships must be strengthened amongst oral health professionals, both regionally and internationally.
Conclusion
Based on the evidence stemming from the included studies that are of limited quantity and quality, there is a wide variation in caries status of preschool children across countries. The prevalence and severity of ECC remains substantial in most countries in Southeast Asia. More attention should be drawn to reducing the burden of ECC, especially in less developed countries.
Acknowledgements
This research is funded by the General Research Fund (number: 17107315) of the University Grant Council, Hong Kong.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Tinanoff N, Reisine S. Update on early childhood caries since the Surgeon General's Report. Acad Pediatr. 2009;9:396–403. doi: 10.1016/j.acap.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwendicke F, Dorfer CE, Schlattmann P, et al. Socioeconomic inequality and caries: a systematic review and meta-analysis. J Dent Res. 2015;94:10–18. doi: 10.1177/0022034514557546. [DOI] [PubMed] [Google Scholar]
- 3.Edelstein BL. Solving the problem of early childhood caries: a challenge for us all. Arch Pediatr Adolesc Med. 2009;163:667–668. doi: 10.1001/archpediatrics.2009.107. [DOI] [PubMed] [Google Scholar]
- 4.Wong HM, McGrath CP, King NM, et al. Oral health-related quality of life in Hong Kong preschool children. Caries Res. 2011;45:370–376. doi: 10.1159/000330231. [DOI] [PubMed] [Google Scholar]
- 5.Chu CH. Treatment of early childhood caries: a review and case report. Gen Dent. 2000;48:142–148. [PubMed] [Google Scholar]
- 6.Country Area Project Profile, Malmo University. Oral Health Database. Available from: https://www.mah.se/CAPP/Country-Oral-Health-Profiles/According-to-Alphabetical/Global-DMFT-for-12-year-olds-2011/. Accessed 08 Oct 2015.
- 7.Khan SQ. Dental caries in Arab League countries: a systematic review and meta-analysis. Int Dent J. 2014;64:173–180. doi: 10.1111/idj.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cleaton-Jones P, Fatti P, Bonecker M. Dental caries trends in 5- to 6-year-old and 11- to 13-year-old children in three UNICEF designated regions–Sub Saharan Africa, Middle East and North Africa, Latin America and Caribbean: 1970–2004. Int Dent J. 2006;56:294–300. doi: 10.1111/j.1875-595x.2006.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 9.Chongsuvivatwong V, Phua KH, Yap MT, et al. Health and health-care systems in southeast Asia: diversity and transitions. Lancet. 2011;377:429–437. doi: 10.1016/S0140-6736(10)61507-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wikipedia. Southeast Asia. Available from: https://en.wikipedia.org/wiki/Southeast_Asia. Accessed 18 Nov 2015.
- 11.Association of Southeast ASEAN Nations. ASEAN Member States 2015. Available from: http://www.asean.org/asean/asean-member-states. Accessed 08 Oct 2015.
- 12.The International statistical institute. Developing countries 2015. Available from: http://www.isi-web.org/component/content/article/5-root/root/81-developing. Accessed 08 Oct 2015.
- 13.Global Child Dental Fund. Global child dental fund-The story so far: 2006–2010. Available from: http://www.gcdfund.org/sites/default/files/images/The%20story%20so%20far.pdf. Accessed 11 Nov 2015.
- 14.Hobdell M, Petersen PE, Clarkson J, et al. Global goals for oral health 2020. Int Dent J. 2003;53:285–288. doi: 10.1111/j.1875-595x.2003.tb00761.x. [DOI] [PubMed] [Google Scholar]
- 15.Chu CH, Wong AWY, Lo ECM, et al. Oral health status and behaviours of children in rural districts of Cambodia. Int Dent J. 2008;58:15–22. doi: 10.1111/j.1875-595x.2008.tb00172.x. [DOI] [PubMed] [Google Scholar]
- 16.Besseling S, Ngonephady S, van Wijk AJ. Pilot survey on dental health in 5- to 12-year-old school children in Laos. J Investig Clin Dent. 2013;4:44–48. doi: 10.1111/j.2041-1626.2012.00136.x. [DOI] [PubMed] [Google Scholar]
- 17.Gao XL, Hsu CY, Loh T, et al. Dental caries prevalence and distribution among preschoolers in Singapore. Community Dent Health. 2009;26:12–17. [PubMed] [Google Scholar]
- 18.Chu CH, Chau AM, Wong ZS, et al. Oral health status and behaviours of children in Myanmar - a pilot study in four villages in rural areas. Oral Health Prev Dent. 2012;10:365–371. [PubMed] [Google Scholar]
- 19.Krisdapong S, Somkotra T, Kueakulpipat W. Disparities in early childhood caries and its impact on oral health-related quality of life of preschool children. Asia Pac J Public Health. 2014;26:285–294. doi: 10.1177/1010539512438608. [DOI] [PubMed] [Google Scholar]
- 20.Hua M. Brunei Darussalum. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 117–120.
- 21.Khairiyah A, Wan Mohd Nasir B, Yaw S et al. Malaysia. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 190–206.
- 22.San M. Myanmar. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 210–223.
- 23.Jienmaneechotechai S, Ungchusak C, Dalodom S et al. Thailand. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 268–286.
- 24.Do L, Spencer A, Roberts-Thomson K, et al. Oral health status of Vietnamese children: findings from the National Oral Health Survey of Vietnam 1999. Asia Pac J Public Health. 2011;23:217–227. doi: 10.1177/1010539509340047. [DOI] [PubMed] [Google Scholar]
- 25.Hai T, Khanh N. Vietnam. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 288–311.
- 26.Centeno M. Philippines. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 236–254.
- 27.Phommavongsa K, Senesombath S. Lao PDR. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 186–188.
- 28.Soeun S, Durward C, Hak S et al. Cambodia. Conference proceedings of International Dental Conference on “Caries Control throughout Life in Asia”. Krabi, Thailand; 2013. p. 122–136.
- 29.Department of Health, Government of the Hong Kong Special Administrative Region . 1st ed. Department of Health; Hong Kong: 2013. Oral Health Survey 2011; pp. 28–29. [Google Scholar]
- 30.Hu DY, Hong X, Li X. Oral health in China–trends and challenges. Int J Oral Sci. 2011;3:7–12. doi: 10.4248/IJOS11006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahejabeen R, Sudha P, Kulkarni SS, et al. Dental caries prevalence among preschool children of Hubli: Dharwad city. J Indian Soc Pedod Prev Dent. 2006;24:19–22. doi: 10.4103/0970-4388.22829. [DOI] [PubMed] [Google Scholar]
- 32.Dye B, Thornton-Evans G, Li X, et al. Dental caries and sealant prevalence in children and adolescents in the United States, 2011–2012. NCHS Data Brief. 2015;191:1–8. [PubMed] [Google Scholar]
- 33.Health and Social Care Informatic Center, National Statistics. Children's oral health report 2015. Available from: http://www.hscic.gov.uk/catalogue/PUB17137/CDHS2013-England-Report.pdf. Accessed 08 Oct 2015.
- 34.Kassebaum NJ, Bernabe E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94:650–658. doi: 10.1177/0022034515573272. [DOI] [PubMed] [Google Scholar]
- 35.Chaffee BW, Cheng A. Global research trends on early-life feeding practices and early childhood caries: a systematic review. J Oral Dis. 2014;2014:675658. doi: 10.1155/2014/675658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petersen PE. The burden of oral disease: challenges to improving oral health in the 21st century. Bull World Health Organ. 2005;83:3. [PMC free article] [PubMed] [Google Scholar]
- 37.Glick M, Monteiro da Silva O, Seeberger GK, et al. FDI Vision 2020: shaping the future of oral health. Int Dent J. 2012;62:278–291. doi: 10.1111/idj.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Do LG. Distribution of caries in children: variations between and within populations. J Dent Res. 2012;91:536–543. doi: 10.1177/0022034511434355. [DOI] [PubMed] [Google Scholar]
- 39.Benzian H, Hobdell M, Holmgren C, et al. Political priority of global oral health: an analysis of reasons for international neglect. Int Dent J. 2011;61:124–130. doi: 10.1111/j.1875-595X.2011.00028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.WHO. World Health Statistics 2011. Available from: http://www.who.int/whosis/whostat/EN_WHS2011_Full.pdf. Accessed 16 Nov 2015.
- 41.Kanchanachitra C, Lindelow M, Johnston T, et al. Human resources for health in southeast Asia: shortages, distributional challenges, and international trade in health services. Lancet. 2011;377:769–781. doi: 10.1016/S0140-6736(10)62035-1. [DOI] [PubMed] [Google Scholar]
- 42.World Health Organization (WHO) 4th ed. WHO; Geneva: 1997. Oral Health Surveys: Basic Methods. [Google Scholar]
- 43.Pitts N, Amaechi B, Niederman R, et al. Global oral health inequalities: dental caries task group–research agenda. Adv Dent Res. 2011;23:211–220. doi: 10.1177/0022034511402016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Petersen PE, Phantumvanit P. Perspectives in the effective use of fluoride in Asia. J Dent Res. 2012;91:119–121. doi: 10.1177/0022034511429347. [DOI] [PubMed] [Google Scholar]
- 45.Petersen PE, Baez RJ, Lennon MA. Community-oriented administration of fluoride for the prevention of dental caries: a summary of the current situation in Asia. Adv Dent Res. 2012;24:5–10. doi: 10.1177/0022034511429349. [DOI] [PubMed] [Google Scholar]
- 46.Lo EC, Schwarz E, Wong MC. Arresting dentine caries in Chinese preschool children. Int J Paediatr Dent. 1998;8:253–260. doi: 10.1046/j.1365-263x.1998.00094.x. [DOI] [PubMed] [Google Scholar]
- 47.Frencken JE, Peters MC, Manton DJ, et al. Minimal intervention dentistry for managing dental caries - a review: report of a FDI task group. Int Dent J. 2012;62:223–243. doi: 10.1111/idj.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holmgren CJ, Roux D, Domejean S. Minimal intervention dentistry: part 5. Atraumatic restorative treatment (ART)–a minimum intervention and minimally invasive approach for the management of dental caries. Br Dent J. 2013;214:11–18. doi: 10.1038/sj.bdj.2012.1175. [DOI] [PubMed] [Google Scholar]
- 49.Duangthip D, Jiang M, Chu CH, et al. Non-surgical treatment of dentin caries in preschool children–systematic review. BMC Oral Health. 2015;15:44. doi: 10.1186/s12903-015-0033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosenblatt A, Stamford TCM, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet”. J Dent Res. 2009;88:116–125. doi: 10.1177/0022034508329406. [DOI] [PubMed] [Google Scholar]
- 51.Acuin J, Firestone R, Htay TT, et al. Southeast Asia: an emerging focus for global health. Lancet. 2011;377:534–535. doi: 10.1016/S0140-6736(10)61426-2. [DOI] [PubMed] [Google Scholar]
- 52.Williams DM. Global oral health inequalities: the research agenda. Adv Dent Res. 2011;23:198–200. doi: 10.1177/0022034511402014. [DOI] [PubMed] [Google Scholar]
- 53.World Bank. Gross national income per capita 2014. Available from: http://databank.worldbank.org/data/download/GNIPC.pdf. Accessed 16 Nov 2015.
- 54.Central Intelligence Agency. The World Fact Book. Available from: https://www.cia.gov/library/publications/the-world-factbook/. Accessed 18 Nov 2015.