Summary
Productivity growth is a key measure against which National Health Service (NHS) achievements are judged. We measure NHS productivity growth as a set of paired year‐on‐year comparisons from 1998/1999–1999/2000 through 2012/2013–2013/2014, which are converted into a chained index that summarises productivity growth over the entire period. Our measure is as comprehensive as data permit and accounts for the multitude of diverse outputs and inputs involved in the production process and for regular revisions to the data used to quantify outputs and inputs. Over the full‐time period, NHS output increased by 88.96% and inputs by 81.58%, delivering overall total factor productivity growth of 4.07%. Productivity growth was negative during the first two terms of Blair's government, with average yearly growth rate of −1.01% per annum (pa) during the first term (to 2000/2001) and −1.49% pa during the second term (2000/2001–2004/2005). Productivity growth was positive under Blair's third term (2004/2005–2007/2008) at 1.41% pa and under the Brown government (2007/2008–2010/2011), averaging 1.13% pa. Productivity growth remained positive under the Coalition (2010/2011–2013/2014), averaging 1.56% pa. © 2016 The Authors Health Economics Published by John Wiley & Sons Ltd.
Keywords: productivity growth, total factor productivity, NHS outputs and inputs
1. Introduction
The English National Health Service (NHS) provides care to millions of patients every year, with almost everyone having at least some form of contact with the health service annually. The NHS is also the single largest employer in England, accounting for 1 out of 18 in the workforce (Office for National Statistics, 2015). In 2013/2014, health spending (including spending by central government departments) amounted to £113 billion and accounted for 9.3% of gross domestic product (GDP) (Harker, 2015). As such an important part of the economy, it is essential to understand what the NHS achieves from the resources devoted to it.
Productivity is one of the key measures against which NHS achievements can be judged and is often cited in evidence when claims are made about the performance of the health system, in justifying the resources devoted to it, or in appealing for additional funding (Chope and Ellison, 2015; House of Commons, 2015; NHS England, 2014). We follow national accounting conventions to measure the change in NHS productivity over time (Eurostat, 2001). This involves comparisons of changes in the total amount of health care output produced with changes in the total amount of input used to produce this output. Output comprises the total volume of services provided to all NHS patients treated in all settings, together with quality of care measured by waiting times, survival rates, health outcomes and blood pressure control. Inputs include the labour, equipment and capital resources that contribute to the production of care. Productivity change is measured by comparing year‐on‐year growth in output against year‐on‐year growth in inputs.
We identify and resolve two particularly salient practical issues in producing measures of NHS productivity over time: how to aggregate the multitude of diverse outputs and inputs involved in the production process and how to deal with the periodic and wholesale revisions to the underlying data used to quantify health care outputs and inputs. We construct a set of paired year‐on‐year comparisons from 1998/1999–1999/2000 through 2011/2012–2012/2013. These paired comparisons are then converted into a chained index that summarises productivity growth over the entire period. We set out the methodological framework in the next section, followed by a description of our data.
Results are then presented and summarised for each of the five parliamentary terms covered by the period, namely, the first of the Labour governments led by Prime Minister Tony Blair (up to 2000/2001), his second and third terms (2000/2001–2004/2005, 2004/2005–2007/2008), the period in which Gordon Brown became Prime Minister, having taken over from Blair (2007/2008–2010/2011) and the Conservative‐Liberal Democrat Coalition government led by David Cameron (2010/2011‐2012/13‐2013/14). Table 1 provides contextual details about each of these parliamentary terms, including the annual average real terms change in expenditure and key NHS policies expected to have influenced NHS productivity. These policies are derived from the governments NHS choices website that provides a history of the NHS in England (NHS Choices, 2015). The final section discusses the findings and the limitations of the work.
Table 1.
Key features of each Parliamentary term
| Parliamentary term/ | Average | Average | |
|---|---|---|---|
| Party Prime Minister | annual real | annual GDP | |
| /start date | terms change | growth (%) | |
| (majority/seats) | in NHS ex‐ | ||
| penditure (%) | Key new NHS policies that might impact on provider productivity | ||
| Labour | 5.5 | 3.32 | 1997: Private Finance Initiative enacted to fund NHS capital investment |
| Tony Blair | 1998: launch of NHS Direct telephone advice service | ||
| 1‐May‐1997 | 2000: creation of walk‐in centres and minor injuries units | ||
| (179/659) | 2001: 18‐month maximum wait for inpatient treatment | ||
| Labour | 7.95 | 2.73 | 2002: 4‐hour waiting time target to be seen in A&E |
| Tony Blair | 2003: start of phased introduction of prospective payment (Payment by Results) for hospital activity | ||
| 7‐Jun‐2001 | 2003: new contract for hospital doctors (consultants) | ||
| (167/659) | 2004: new GP contract | ||
| 2004: introduction of Agenda for Change contract for NHS staff (except doctors) | |||
| 2004: First ten foundation trusts established | |||
| 2004: First contracts allowing NHS patients to be treated in private (independent sector) treatment centres | |||
| 2005: 6‐month maximum wait for inpatient treatment | |||
| Labour | 4.15 | 2.79 | 2006: patients offered choice of at least four hospitals for planned care |
| Tony Blair | |||
| 5‐May‐2005 | |||
| (66/646) | |||
| Labour | 5.67 | −1.06 | 2008: choice extended to any hospital for planned care |
| Gordon Brown | 2009: maximum 18‐week waiting time embodied in new NHS Constitution | ||
| 27‐Jun‐2007 | |||
| (na) | |||
| Conservative‐Liberal Democrat Coalition; | 1.18 | 1.84 | 2011: ‘Quality, Innovation, Productivity and Prevention’ challenge to save £15–20bn from 2011 to 2014 |
| David Cameron | 2012: choice of any qualified provider | ||
| 6‐May‐2010 | 2012: Health and Social Care Act | ||
| (78/650) | 2013: Substantial re‐organisation of NHS enacted |
Term dates and seats from (Wikipedia, 2015).
Expenditure up to 2010/2011 from (Harker, 2012) up to 2013/2014 from (Her Majesty's Treasury, 2014) GDP from (Office for National Statistics, 2015).
GDP, gross domestic product; NHS, National Health Service; GP, general practitioner.
2. Methodology and Conceptual Framework
The terms productivity and efficiency are often used interchangeably by non‐economists, but they are distinct concepts. Triplett (Triplett, 2011) argues that the conventional framework of productivity growth measurement rests inherently on the concept of an underlying production function – a systematic relationship between outputs and inputs as shown in a stylised example in Figure 1.
Figure 1.
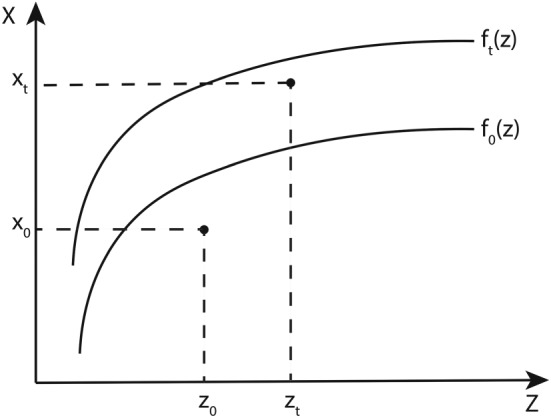
Stylised production functions
To start with, we assume a production function relating to a single type of input used to produce a single type of output. Following (Coelli and Prasada Rao, 1998), let x 0, x t and z 0, z t represent the observed quantities of output (x) and input (z) produced in a base period 0 and subsequent time period t, respectively. From this information alone, it is possible to calculate total factor productivity growth (ΔTFP) between the two periods as follows:
| (1) |
In the depicted example, up to the flattening off point of each function, a relatively small increase in input is exceeded by a relatively large increase in output. Consequently, up to this point ΔT F P is positive.
To further understand the drivers of ΔT F P, it is necessary to look beyond measurement and disentangle the components of productivity growth. Let f 0(z) and f t(z) represent the production functions at time 0 and t. These functions represent the maximum output that could be obtained in the relevant time period for each level of input. In our example, f t(z) lies above f 0(z) indicating that there has been technical progress between the two time periods, resulting in an upward shift of the production function, which now allows for greater output at all input levels. As the observed level of output x t would not have been possible under the old production function, f 0(z), no matter what level of input, one may conclude that at least some of the observed output growth is due to technical change, that is, an upward shift of the production function.
In addition, note that both x 0 and x t lie beneath their respective production functions. This suggests technical inefficiency in production because the observed input/output levels fall below the technically feasible levels as indicated by the production functions in each period. In both periods, the contemporary technology allows for a higher level of output to be achieved with the same amount of input. The magnitude of this inefficiency can be measured by the vertical difference between the observed and the potentially achievable output on the production function. In Figure 1, notice that x t lies closer to f t(z) than x 0 does to f 0(z). This implies that there has been an improvement in efficiency from one time period to the next. Thus, improved efficiency also contributes to positive ΔT F P.
Finally, notice that the shape of the production functions exhibit, firstly, increasing returns to scale and, then, diminishing returns to scale. As production levels are currently located within the steep increasing returns section of the production function, the increase in inputs from z 0 to z t, all other things being equal, produces a substantial increase in output.
The practical challenge in disentangling the components of productivity growth is that the production function is unobservable. Without knowledge of the production function and how it changes over time, it is not possible to disentangle the technical change, efficiency and scale components of ΔT F P. Typically, this has led to empirical studies making assumptions about the nature of the unobservable production function of which the two most common are as follows: (1) absence of technical inefficiencies and (2) presence of constant returns to scale (CRS) (Coelli and Prasada Rao, 1998). We shall discuss the validity of these assumptions and their implications for interpretation of ΔT F P in due course.
3. Multiple Outputs and Inputs
Rarely does the single input/output situation apply. Therefore, in calculating ΔT F P, it is necessary to combine a variety of outputs into an overall output growth index (X) and inputs into an input growth index (Z). TFP growth ΔT F P is calculated by comparing the growth rate in outputs with the growth rate in inputs such that
| (2) |
If expressed simply as , the equation would imply a baseline of 1. So by subtracting 1 from the ratio, a value of 0.02 can be interpreted as 2% increase in TFP. Even with just two outputs, this specification amounts to an aggregate production function. Irrespective of whether multiple outputs are produced by a single firm, or the industry as a whole, aggregation imposes the assumption of CRS and requires a means of valuing diverse outputs so that they can be combined into a single index (Felipe and McCombie, 2005; Fisher, 2005). For the health system, quantification and valuation of health care output is a challenge. Patients have varied health care requirements and receive very different packages of care, so it is necessary to classify patients into homogenous output groupings. Then, in order to aggregate different types of output into a single index, some means of assessing their relative value is required. Usually prices are used to assess value, but in most countries prices are not available for the vast majority of health services for which people do not have to pay the full cost at point of use. In common with the treatment of other non‐market sectors of the economy, in the national accounts, therefore, costs are used to indicate the value of health services. Costs reflect producer rather than consumer valuations of outputs, but have the advantage of being readily available (Eurostat, 2001). As costs are not believed to truly reflect consumers' valuations, Atkinson (2005) suggests supplementing costs with information about the quality of output. One way of doing this is by adding a scalar to the output index that captures changes over time in different dimensions of quality (Castelli et al., 2007a, Castelli et al., 2011). Thus, following Castelli et al. (2011), the output growth index (in its Laspeyres form) can be formulated as
| (3) |
We define x j as the number of patients who have output type j, where ; c j indicates the cost of output j; q j represents a unit of quality for output j and v j is the value of this unit of quality; 0 indicates the base period and t the current period. Consequently, x j0 c j0 represents the cost‐weighed volume of patients of type j in the base period. The term in brackets allows changes in the quality to be incorporated in the output index. Of course, this general form can be specified in numerous ways. In England, the specific form was agreed upon following methodological research published in 2005 that explored various options for quality adjustment based on available data (Dawson et al. 2005). The form was adopted officially by the Office of National Statistics in assessing the contribution of the health sector to national output (Office for National Statistics, 2006), and this form is applied in what follows.
Our measures of quality q j include inpatient and outpatient waiting times, survival rates following hospitalisation, estimated change in health outcomes following hospital treatment and blood pressure management in primary care (Derbyshire et al., 2007, Castelli et al., 2011). The quality adjustment is designed to capture changes in the expected discounted sum of lifetime QALYs conditional on patients surviving treatment. Longer waiting times are considered to have adverse health consequences and formulated as a scaling factor multiplying the health effect (Castelli et al. 2011). The value v j reflects the expected contribution that a unit change in quality measure j has on lifetime Quality Adjusted Life Years (QALYs), albeit imperfectly measured (Castelli et al. 2011). Detail about each of these components and how they are combined into a single index is provided in Castelli et al. (2007b). Output increases if there are reductions in waiting times and improvements (increases) in the other measures.
Turning to the denominator of (2), inputs into the health care system consist of labour, intermediate goods and capital. Growth in the use of these factors of production can be calculated directly or indirectly (OECD, 2001). A direct measure of input growth can be calculated when data both on the volume and price of inputs are available. In its Laspeyres form, this can be calculated as
| (4) |
where z n is the volume of input of type n, ω n is the price of input type n with 0 indicating the base period and t the current period.
However, data about the volume of inputs are rarely available. It is, therefore, a common practice to calculate input growth using expenditure data. Expenditure data capture changes in both the volume and price of inputs used. Hence, to isolate the volume effect, it is necessary to convert nominal into constant expenditure using a deflator π. This deflator reflects the underlying trend in price for the input in question, such that ω n0=π n ω nt. If expenditure data and deflators are available, the input growth index can be specified as
| (5) |
Where E n indicates expenditure on input n. As shown, and are equivalent, provided that deflators capture correctly the trend in prices for each input.
4. Total Factor Productivity Over Time
The earlier equations consider output or input growth from one period to the next. Usually, there is interest in assessing productivity growth over longer periods of time. There are two ways to do this. The first is by means of a fixed base index, which applies the same set of output weights (c j) and input weights (ω n), usually that of the base year, throughout the full series. This has the advantage of using a single set of weights across all periods and is a common practice when calculating growth rates for a specified basket of goods and services (Diewert, 1998).
The drawback of this approach is that it requires the contents of the basket to remain unchanged over the full period. If this requirement cannot be met, an alternative is to use a chained index. This approach has long been recommended (Lehr, 1885, Marshall, 1887) as a way to overcome the problems arising when new commodities appear and old commodities disappear, making the use of weights of the base year practically impossible. By updating the weights in every period, it is possible to account for ongoing changes in the composition of the outputs and inputs (Diewert et al. 2010). The main advantages of using a chained index over a fixed base index are
ease of handling changes in the type of outputs produced and inputs utilised, as these only need to be common across two adjacent periods rather than for the full series (Balk, 2010);
regular updates of the weights better reflect actual price and volume changes (De Boer et al. 1997); and
the difference (or spread) between the Laspeyres and Paasche formulations of the indices is lower than it would be if using a fixed index (Hill, 2006).
Using the Laspeyres output index as defined in Equation (3), a chain index will take the following form:
| (6) |
This notation can be simplified as
| (7) |
where each link is represented by Equation (3) with the time index updated for the relevant two consecutive time periods. An analogous construction applies to the chained input index:
| (8) |
or in a simplified version:
| (9) |
5. Dealing With Inconsistent Data Series
The use of a chained index is particularly important in contexts in which the underlying data used to describe outputs and inputs are subject to periodic revision. This makes it difficult to measure things in a consistent fashion over time. In the English NHS, wholesale revisions are made regularly to how outputs are defined and to the underlying data to describe inputs. The extent of the output re‐categorisations can be appreciated in Table 2.
Table 2.
Number of output categories by year and care setting
| Inpatient | Outpatient | Mental healtha | Community care | Other activity | Primary care | Prescribing | |
|---|---|---|---|---|---|---|---|
| 1998/1999 | 1137 | — | — | — | 10 | 4 | 178 |
| 1999/2000 | 1137 | 93 | — | — | 11 | 4 | 178 |
| 2000/2001 | 1135 | 300 | 14 | 3 | 60 | 4 | 178 |
| 2001/2002 | 1134 | 300 | 22 | 13 | 104 | 5 | 184 |
| 2002/2003 | 1138 | 143 | 29 | 47 | 502 | 5 | 188 |
| 2003/2004 | 1273 | 175 | 66 | 104 | 1224 | 5 | 188 |
| 2004/2005 | 1193 | 290 | 95 | 120 | 1327 | 5 | 184 |
| 2005/2006 | 1188 | 469 | 99 | 122 | 1306 | 5 | 198 |
| 2006/2007 | 1186 | 1388 | 140 | 132 | 3577 | 5 | 199 |
| 2007/2008 | 3469 | 1419 | 138 | 138 | 1419 | 6 | 8769 |
| 2008/2009 | 2453 | 1487 | 135 | 138 | 1329 | 6 | 8276 |
| 2009/2010 | 2479 | 1748 | 137 | 151 | 1563 | 6 | 8072 |
| 2010/2011 | 2621 | 1871 | 138 | 154 | 1559 | 6 | 7860 |
| 2011/2012 | 2750 | 1870 | 130 | 171 | 9876 | 6 | 7856 |
| 2012/2013 | 2750 | 6979 | 125 | 149 | 8861 | 6 | 7699 |
| 2013/2014 | 4200 | 8055 | 136 | 174 | 1856 | 6 | 7699 |
Includes community and admitted hospital mental health.
Table 2 shows the number of categories by which healthcare outputs are defined according to broad health care settings since 1998/1999. For instance, the Healthcare Resource Groups (HRGs) used to describe hospital outputs have been substantially revised over time to the extent that comparisons cannot be made readily between the years when the revised systems were introduced (Grašič et al., 2015). Similarly, the categories for outpatient, mental health, community care and other NHS activity have changed dramatically, undergoing periodic re‐classifications, disaggregation of existing categories and complete overhauls in how such activities are described. These revisions are reflected in the varying number of categories used to describe outputs in each setting.
When there are few categorisation changes and/or these involve refinement to the underlying categorisation system, these can be dealt with by mapping old and new categories. This was the approach we used to take (Dawson et al. 2005) and is still currently used by Office for National Statistics (Office for National Statistics, 2009). But where changes are more comprehensive, mapping is both impractical and likely to induce error (Castelli et al. 2011). This is because the purpose of a wholesale re‐categorisation exercise is to fundamentally re‐define what activities should be considered similar types of output. Some activities previously considered similar will now be categorised as different outputs; other activities formerly considered dissimilar might now be considered the same type of outputs (Castelli et al. 2008).
An alternative approach is to treat new categories as completely new types of output and include them in the calculation of Equation (3). The difficulty is that there are no weights for these new outputs in the period prior to their appearance. In Castelli et al. (2011), we proposed imputing the requisite missing weights for new categories by deflating current weights to derive those that would most likely have obtained in the previous periods. For ease of exposition, if we ignore quality and consider cost weights only, then for a Laspeyres output index, we can re‐specify Equation (3) as
| (10) |
where refers to categories that were defined at time 0, refers to those categories newly defined at time t, is the imputed value for c j0 and is the cost deflator. By extension, the chain index Equation (6) becomes
| (11) |
This can be expanded to include an output‐specific quality adjustment, the requirement being a judgement about how quality might have evolved between the two adjacent time periods. As we have previously demonstrated (Castelli et al. 2008), the imputation and mapping approaches will produce the same estimates of output growth only if the old and new categories can be mapped exactly.
6. Data
6.1. Output data
Output consists of the volume and quality of all health care services provided to NHS patients. We capture the volume of NHS outputs provided across health care sectors as comprehensively as data permit. The units of output vary by setting and data source but include the number of the following: patients treated in hospital, attendances in outpatient and A&E departments, bed days in community care and mental health facilities, consultations in primary care, prescriptions dispensed and diagnostic tests performed. A summary of the different data sources used to populate the output indices from 1998/1999 to 2013/2014 is provided in Table 3.
Table 3.
Summary of NHS output data sources, 1998/1999–2013/2014
| Output type1 | Year | Activity source | Cost source | Quality | Notes |
|---|---|---|---|---|---|
| Inpatient | 1998/1999–2013/2014 | HES | RC | 30‐day survival health | The quality adjustors are |
| outcomes waiting times | calculated from HES | ||||
| Outpatient | 1998/1999–2010/2011, | RC | RC | Average waiting | Waiting times up until |
| 2013/2014 | time (weeks) | and including 2009/2010 | |||
| were provided by | |||||
| the Department of Health, | |||||
| National Inpatient and | |||||
| Outpatient waiting times, | |||||
| England | |||||
| 2011/2012 | OPMD | For 2009/2010 onwards, | |||
| we use the HES Outpatient | |||||
| Minimum Dataset | |||||
| Mental health | 1998/2009–2013/2014 | HES and RC | RC | 30‐day survival | |
| Health outcomes | |||||
| Waiting times | Quality adjustment applied | ||||
| to Hospital Mental Health | |||||
| activity only | |||||
| Community care | 1998/1999–2013/2014 | RC | RC | n/a | |
| Primary care | 1998/1999–2003/2004 | General Household | PSSRU's Unit | n/a | |
| Survey | Costs of | ||||
| Health and | |||||
| Social Care | |||||
| 2003/2004–2008/2009 | QResearch | Prevalence and achievement | |||
| rates in reducing blood | |||||
| pressure for patients with | |||||
| CHD, stroke and hypertension | |||||
| (Quality Outcome Framework) | |||||
| 2008/2009– 2013/2014 | GP Patient Survey | ||||
| Prescribing | 1998/1999–2013/2014 | PPA | PPA | n/a | Switched from using BNF |
| chapters to chemical | |||||
| composition in 2008/2009 | |||||
| Ophthalmology | 1998/1999–2013/2014 | HSCIC | HSCIC | n/a | |
| and dentistry | |||||
| Other NHS activity | 1998/1999–2013/2014 | RC | RC | n/a |
, Hospital Episode Statistics; RC, reference costs; OPMD, outpatient minimum dataset; PSSRU, Personal Social Services Research Unit; PPA, Prescription Pricing Authority; BNF, British National Formulary; CHD, coronary heart disease; HSCIC, Health and Social Care Information Centre.
The Hospital Episode Statistics (HES) is the source of data for both the amount of activity and for the measures of quality for elective and non‐elective activity, including mental health care delivered in hospitals. HES comprised almost 19.3 million patient records for 2013/2014. We convert HES records, defined as Finished Consultant Episodes, into continuous inpatient spells (CIPS), which capture time from admission to discharge. We then count the number of CIPS in each HRG, which forms the basic means of describing different types of hospital output. The HES records include age and waiting times and can be linked to Office for National Statistics death registry records and life expectancy tables. This allows us to calculate waiting times and 30‐day survival rates that are used to assess the quality of hospital care.
Reference costs (RC) were used to measure outpatient activity (Castelli et al. 2008), but because of the abolition of Primary Care Trusts, RC outpatient data were incomplete in 2011/2012, and we turned to the HES Outpatient Minimum Dataset to assess outpatient activity from that year. A comparison of historical values in both datasets prior to 2011/2012 indicates a very close match in volumes of activity, and therefore, there is no major consequence of this change. Outpatient waiting times up until 2009/2010 were based on data published on the Department of Health performance website, but this collection has since been discontinued. From 2010/2011, we calculate waiting times for first attendances using the HES Outpatient Minimum Dataset. These waiting times are somewhat higher than those reported previously, but year‐on‐year trends are virtually identical.
The RC returns are used to capture activity performed in health care settings including accident and emergency departments, mental health and community care settings and diagnostic facilities. Activities are reported in various ways: attendances, bed days, contacts and number of tests. The RC data also provide information on unit costs for all of these activities, as well as activity performed in hospitals.
Comprehensive data on the activities performed in primary care settings are unavailable. In their absence, nationally representative survey data are used instead. For the period 2003/2004 to 2008/2009, the volume of general practitioner (GP) consultations was obtained from QResearch (Fenty et al., 2006; QResearch, 2009). When this survey was discontinued, we used the General Lifestyle Survey instead, for the years 2009/2010 and 2010/2011 (Bojke et al. 2012), and, since 2010/2011, we have used data from the GP Patient Survey (NHS England, 2015). We derive information on costs of primary care activity from the annual estimates calculated by Personal Social Services Research Unit, which are available online (Curtis, 2014). To assess the quality of primary care activity, we use blood pressure management of patients with coronary heart disease, stroke and hypertension, data about which are collected as part of the Quality Outcomes Framework (Derbyshire et al. 2007).
Data about community prescribing are taken from the Prescription Cost Analysis system, supplied by the Prescription Pricing Authority via the Health and Social Care Information Centre (HSCIC) Prescription Drugs Team. The data capture all prescriptions dispensed in the community, summarised into 199 British National Formulary chapters up to 2006/2007 and subsequently using 8000 categories defined according to chemical composition. Information about ophthalmology and dentistry is also derived from the HSCIC. Dental activity is differentiated into dental bands, reflecting the relative costs of different courses of treatments.
6.2. Input data
Inputs into the health care system consist of labour, such as doctors, nurses, technicians and managers; intermediate goods and services, such as drugs and clinical supplies; and capital, such as buildings and equipment with an asset life of more than a year. We use workforce and expenditure data to construct a comprehensive index of input growth.
Labour input was computed from the workforce census data up to 2006/2007, which categorised all staff into 26 groups. Since then, we have switched to the NHS iView database, which draws directly from the Electronic Staff Records and combined Payroll and Human Resources system from the NHS. The data report full‐time equivalent staff and wages for 585 occupational groups.
With regular changes to organisational structures in the NHS, it is not surprising that the form in which expenditure data are reported has changed over time. From before 1998/1999, expenditure by NHS hospitals was recorded in the trust financial returns (TFRs), which were also submitted by Strategic Health Authorities and Primary Care Trusts. TFRs provided detailed breakdowns of expenditure on different types of input. However, in 2003/2004, hospitals that became Foundation Trusts were no longer required to submit TFRs, but filed annual accounts instead, that contain less‐detailed expenditure data. TFRs were discontinued entirely in 2011/2012, so since then we have analysed expenditure as summarised in the aggregated Financial Monitoring Accounts. These are much less detailed than the TFRs, reporting information for more aggregated categories of input. Expenditure on general medical (including GPs and practice staff), dental and ophthalmic services and central administration are provided by the Department of Health. Table 4 summarises data sources used to calculate input use and information about deflators used to wash out price effects.
Table 4.
Summary of NHS input data sources, 1998/1999–2013/2014
| Input type | Year | Activity source | Data description | Deflator |
|---|---|---|---|---|
| Direct labour | 1998/1999–2006/2007 | Workforce Census | Numbers of full time equivalent staff | HSCI Pay Index |
| 2007/2008–2013/2014 | Electronic Staff Record (iView) | |||
| 2007/2008–2013/2014 | Payroll and Human Resources system | Earnings by staff group | HSCI Pay Index | |
| Agency staff | 1998/1999–2011/2012 | NHS Hospital Trusts financial returns | Expenditure on agency staff | HSCI Pay Index |
| 2003/2004–2011/2012 | NHS Foundation Hospital Trusts financial returns | HSCI Pay Index | ||
| 2003/2004–2011/2012 | SHAs, PCTs financial returns | HSCI Pay Index | ||
| 2012/2013–2013/2014 | DH Agency spend data | HSCI Pay Index | ||
| Intermediates | 1998/1999–2011/2012 | NHS Hospital Trusts financial returns | Information on expenditure on drugs, gases, clinical | NHS Price Index |
| supplies, catering, hotel services, laundry bedding | ||||
| 2003/2004–2013/2014 | NHS Foundation Hospital Trusts financial returns | NHS Price Index | ||
| 2003/2004–2011/2012 | SHAs, PCTs financial returns | |||
| 2012/2013 | NHS Hospital Trusts and PCTs Annual Financial Accounts | NHS Price Index | ||
| 2013/2014 | NHS Hospital Trusts and NHS England Group | HSCI Price Index | ||
| Annual Financial Accounts | ||||
| Capital | 1998/1999–2011/2012 | NHS Hospital Trusts financial returns | Information on establishment and | ONS MM17 capital deflators |
| premises costs, costs for equipment | ||||
| 2003/2004–2011/2012 | NHS Foundation Hospital Trusts financial returns | |||
| 2003/2004–2011/2012 | SHAs, PCTs financial returns | HSCI Price Index | ||
| 2012/2013 | NHS Hospital Trusts and PCTs Annual Financial Accounts | HSCI Price Index | ||
| 2013/2014 | NHS Hospital Trusts and NHS England | HSCI Price Index | ||
| Group Annual Financial Accounts | ||||
| Prescription drugs | 1998/1999–2006/2007 | Number of prescription | FHS deflator | |
| 2007/2008–2013/2014 | Number of items | CHE Pharmacy Price Index | ||
| DH administration | 2003/2004–2012/2013 | DH Financial accounts | DH admin costs | HSCI Pay and Price Index |
For the years 1998/1999–2003/2004, FTE numbers were adjusted to reflect experience and qualifications.
Health Service Cost Index; ONS MM17, Office for National Statistics, price index numbers for current cost accounting; FHS, Family Health Services; CHE, Centre for Health Economics; DH, Department of Health; PCT, Primary Care Trust; SHA, Strategic Health Authority.
7. Results
7.1. Output growth
Output in all NHS settings has experienced sustained growth over the time period considered, as shown in Figure 2. Inpatient output contributes the biggest share in overall output value (32.61% in 2013/2014 and similar values in previous years). Inpatient output captures both the volume and quality of activity and has increased by 74.39% over the full period, with an average growth rate of 3.80% pa. Growth in inpatient output was 1.13% pa during the Blair's first term in office (data period covered 1998/1999–2000/2001); it increased to an average of 5.04% pa during his second term (2000/2001–2004/2005) and 5.83% during his third term (2004/2005–2007/2008), amounted to 3.46% pa during the Brown administration (2007/2008–2010/2011) and 2.25% pa during the first years of the Coalition government (2010/2011–2013/2014).
Figure 2.
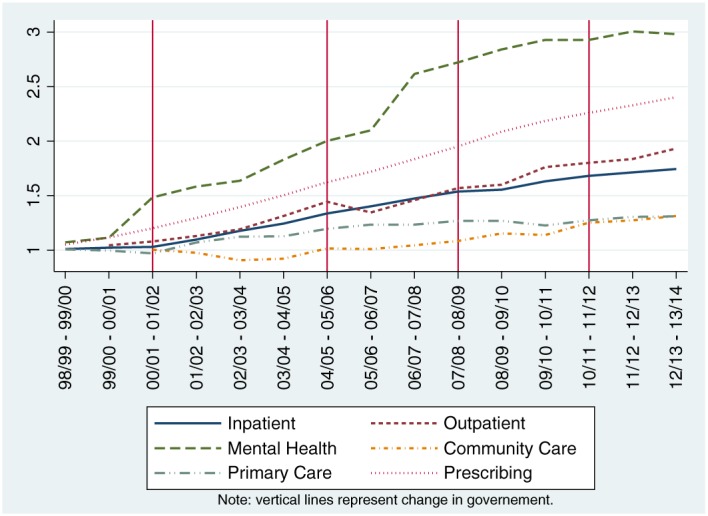
Chained output growth index by sectors; rebased to 1998/1999. Primary care is not quality adjusted until 2002/2003–2003/2004. Community care output growth rate for 2003/2004–2004/2005 is equal to the average of the growth rates for 2002/2003–2003/2004 and 2004/2005–2005/2006. [Colour figure can be viewed at wileyonlinelibrary.com]
The next three biggest contributors to overall output are outpatient activity, primary care activity and prescribing, contributing 10.70%, 14.67% and 10.63%, respectively, to overall output value in 2013/2014. Over the years, the output produced in outpatient and primary care settings has increased by 93.77% (4.93% pa) and 30.98% (1.86% pa), respectively. Prescribing has increased by 140.26% over the full series and 6.03% pa. Outpatient output increased year‐on‐year throughout the three Blair terms (averaging 4.44% pa, 5.92% pa and 3.85% under each, respectively) and the Brown government (6.55% pa), but the average growth rate fell to 3.24% pa during the Coalition government.
Primary care output shows an erratic growth rate over the five governmental periods considered. The initial average negative growth of −0.21% pa during the first Blair government was followed by a period of positive growth (3.26% pa and 3.05%) during his second and third terms in office. The Brown years were characterised by average negative growth of −0.18% pa, followed by a period of positive growth averaging 2.24% pa under the Coalition government. Prescribing increased by an average of 5.66% pa during the first Blair government, rising to 7.71% pa and 6.88% under his second and third terms. The rate of growth in prescribing averaged 6.01% pa under Brown and fell to 3.20% pa during the first 4 years of the Coalition government.
Mental health activity contributed almost 7.96% to overall output value in 2013/2014. The amount of output has increased by 198.12% (8.46% pa) over the whole time series. Average annual growth was 5.58% pa under Blair's first term, 13.75% pa under his second and 12.96% under his third, but fell to 3.83% pa under Brown's government and to 0.92% pa under the Coalition.
Finally, output produced in community care settings contributed 4.99% of total output value in 2013/2014, with the amount of this output increasing by 31.31% since 1998/1999, at an average growth rate of 2.22% pa. Community care activity only started to be recorded in a consistent manner from the beginning of the second Blair government, growth falling by an average of −1.96% pa during this term but growing by an average of 4.36% pa during his third term. The average growth rate amounted to 2.97% pa during Brown's time in office and to 4.92% pa under the Coalition.
Over the 15‐year period, the 30‐day survival rates following hospital treatment have steadily improved, contributing positively to NHS output (Figure 3). Waiting times for hospital admission and outpatient appointments decreased up to 2008/2009, but since then they have been growing longer (Figure 4).
Figure 3.
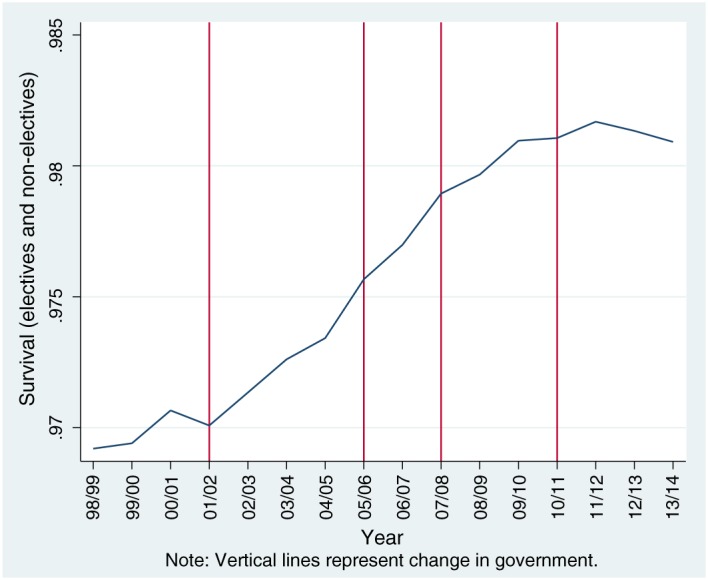
30‐day survival rates. [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 4.
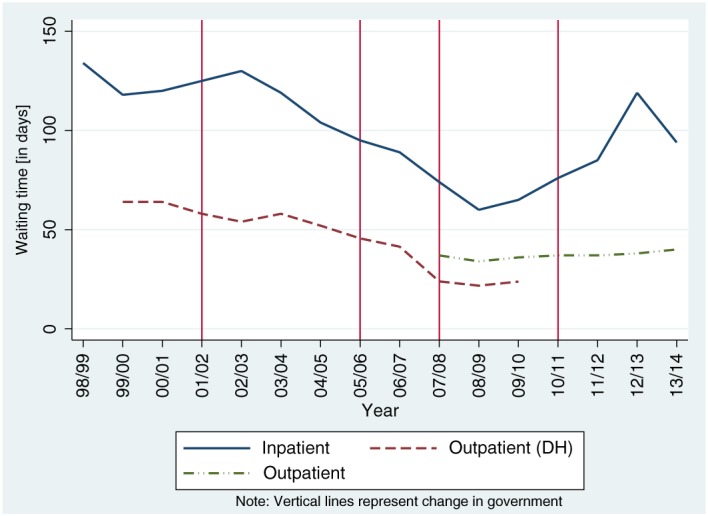
The 80th percentile and mean waiting times (days), 1998/1999–2013/2014. [Colour figure can be viewed at wileyonlinelibrary.com]
Taken together, the overall output of the NHS, comprising both the volume and quality of care, increased by 89.02% over the full 16years. The net contribution of the quality adjustment to overall NHS output amounted to 0.41% in the years between 1998/1999 and 2005/2006, increasing to 0.55% since then.
Average annual output growth was 2.24% pa from 1998/1999 to 2000/2001 (first Blair government). The second and third Blair terms witnessed the highest year‐on‐year growth in the whole time period, with average growth rates of 5.22% pa and 5.76%, respectively. This slowed down during the Brown government, at 4.81% pa. In the first 4years of the Coalition government, average yearly growth decreased to 2.72%.
7.2. Input growth
NHS staff accounts for the largest share of overall NHS input, accounting for 42.18% in 2013/2014. As Figure 5 shows, growth in employment of staff has been irregular over time, with periods of retrenchment (1999/2000–2002/2003), stability (2003/2004–2007/2008), increased recruitment (2008/2009–2010/2011), and further retrenchment recently. The patterns are somewhat different if calculations of NHS staff input are based on workforce/Electronic Staff Records data or expenditure data. This implies that the data used to construct the and forms of the input index are not equivalent.
Figure 5.
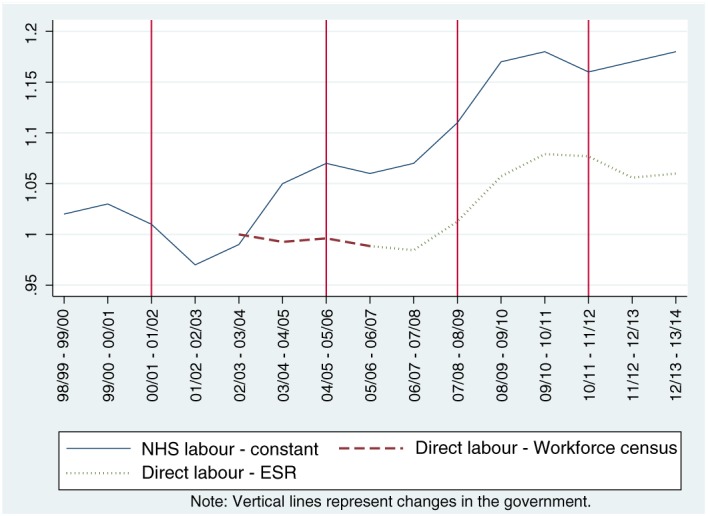
Chained labour indices, both expenditure and full‐time equivalents. [Colour figure can be viewed at wileyonlinelibrary.com]
Agency staff represents a relatively low share of total expenditure at around 2.48% in 2013/2014. The use of agency staff over time is highly volatile, and although utilisation has increased by a factor of 4.42 over the full period, there have been periods in which the use of such staff was substantially reduced (Figure 6). These periods (2004/2005–2006/2007 and 2009/2010–2011/2012) coincide with times during which the hospital sector, in particular, was under pressure to reduce deficits (Street, 2014).
Figure 6.
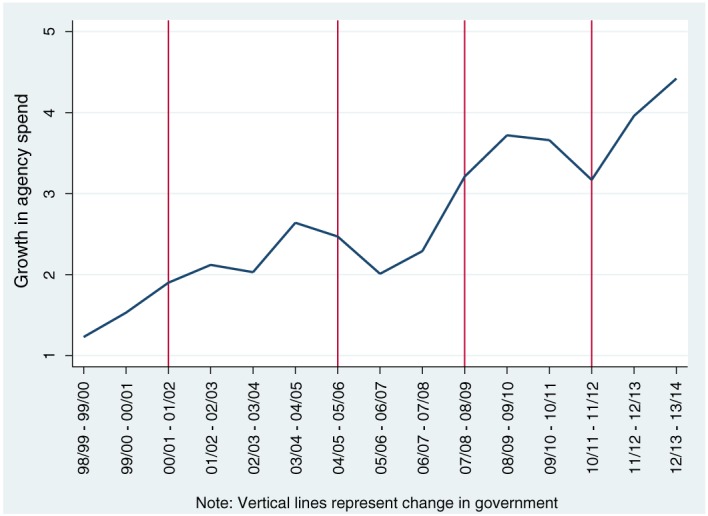
Chained growth index in agency staff expenditure. [Colour figure can be viewed at wileyonlinelibrary.com]
Changes in the use of intermediate and capital inputs are depicted in Figure 7. Major changes in the data used to measures these inputs occurred in 2003/2004, hence the broken series at this point. Intermediate inputs accounted for around 21.32% of overall inputs in 2013/2014. Over the years, we observe a steep increase in utilisation of such inputs, with an average growth of more than 10.18% pa. Capital has the smallest input share, accounting for 13.08% in 2013/2014. Average growth amounts to about 1.99% pa, but there are noticeable year‐on‐year variations, and growth in the use of capital inputs has been falling since 2006/2007.
Figure 7.
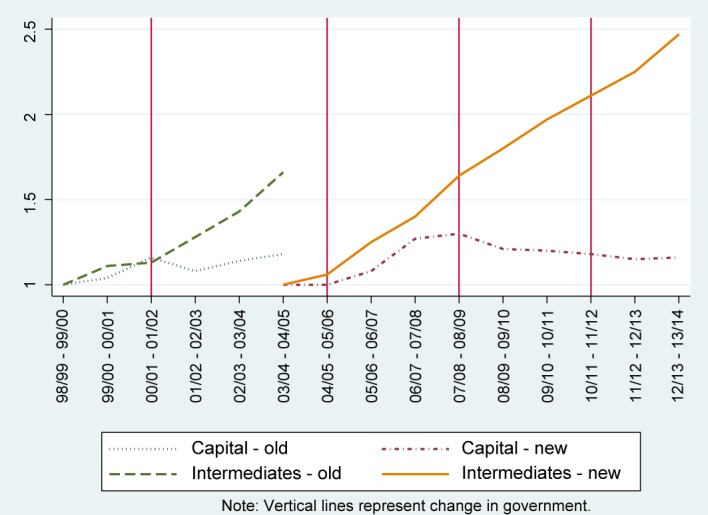
Growth in capital and intermediates expenditure. [Colour figure can be viewed at wileyonlinelibrary.com]
Taking all inputs together, overall growth amounted to 81.58% over 16years, an average of 4.09% pa. The rate of increase was fastest under the Blair government, with an average input growth of 3.31% pa in his first term, increasing to 6.82% pa during his second turn and remaining relatively high at 4.33% pa under his third term. Input growth decreased somewhat under the Brown government, increasing by 3.66% pa. Input growth was substantially lower under the Coalition government, averaging 1.14% pa.
7.3. Productivity
Table 5 reports our estimates of year‐on‐year and chained output, input and productivity growth and Figure 8 plots the output and input indices in the style of a hypothetical production function as illustrated in Figure 1. A 45‐degree line is included, indicating a CRS production function on the index scales. This provides a reference to see how year‐on‐year growth rates compare with the situation that would have obtained were all changes over time to have derived solely from scale effects, but not technical changes or technical efficiencies.
Table 5.
Output, input and productivity, year‐on‐year growth and chained growth index
| Output growth | Chained output | Input growth | Chained input | Productivity | Chained productivity | |
|---|---|---|---|---|---|---|
| Total NHS | Equation (10) | index Equation (11) | Equation (4) | index Equation (8) | growth Equation (2) | index |
| 1 | 1 | 1 | ||||
| 1998/1999–1999/2000 | 2.22% | 102.22% | 5.07% | 105.07% | −2.71% | 97.29% |
| 1999/2000–2000/2001 | 2.26% | 104.53% | 1.55% | 106.70% | 0.69% | 97.97% |
| 2000/2001–2001/2002 | 3.74% | 108.44% | 6.10% | 113.21% | −2.22% | 95.79% |
| 2001/2002–2002/2003 | 5.78% | 114.71% | 7.06% | 121.20% | −1.19% | 94.65% |
| 2002/2003–2003/2004 | 4.93% | 120.37% | 7.63% | 130.44% | −2.51% | 92.28% |
| 2003/2004–2004/2005 | 6.44% | 128.12% | 6.50% | 138.92% | −0.05% | 92.23% |
| 2004/2005–2005/2006 | 7.11% | 137.23% | 7.19% | 148.91% | −0.07% | 92.16% |
| 2005/2006–2006/2007 | 6.50% | 146.15% | 1.92% | 151.76% | 4.50% | 96.3% |
| 2006/2007–2007/2008 | 3.66% | 151.49% | 3.88% | 157.64% | −0.21% | 96.1% |
| 2007/2008–2008/2009 | 5.73% | 160.18% | 4.23% | 164.32% | 1.44% | 97.48% |
| 2008/2009–2009/2010 | 4.11% | 166.76% | 5.43% | 173.24% | −1.25% | 96.26% |
| 2009/2010–2010/2011 | 4.57% | 174.39% | 1.33% | 175.54% | 3.21% | 99.35% |
| 2010/2011–2011/2012 | 3.15% | 179.89% | 1.00% | 177.29% | 2.13% | 101.46% |
| 2011/2012–2012/2013 | 2.34% | 184.10% | 1.98% | 180.80% | 0.36% | 101.83% |
| 2012/2013–2013/2014 | 2.64% | 188.96% | 0.43% | 181.58% | 2.24% | 104.07% |
Figure 8.
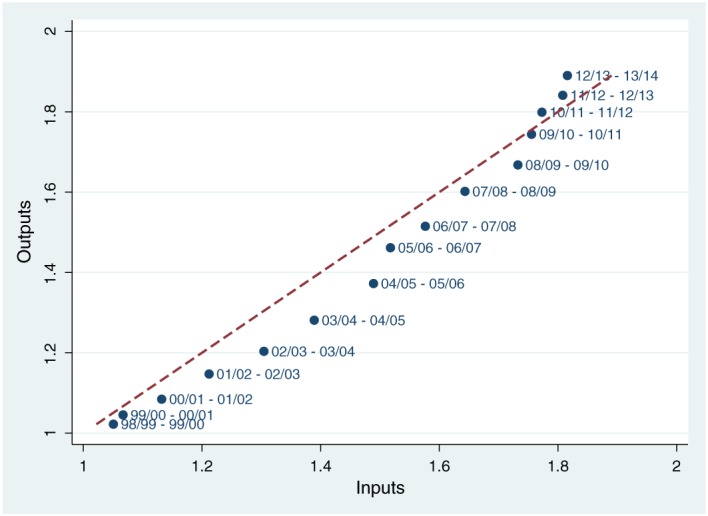
Plot of the input and output indices. [Colour figure can be viewed at wileyonlinelibrary.com]
Since 1998/1999, there has been a substantial increase in NHS activity, improvements in the quality of care and a growth in inputs. Over the full time period, NHS output has increased by 88.96%, while inputs have increased by 81.58%, indicating overall TFP growth of 4.07%.
Productivity growth was negative during the first two terms of Blair's government, with average yearly growth rate of −1.01% pa during the first term and −1.49% pa during the second term. These periods were characterised by sustained growth in the NHS budget, with real terms annual increases of 5.5% in the first term and of 7.95% in the second (Table 1), both well above average growth in GDP. Expenditure increases helped fund capital investment through the Private Finance Initiative and the creation of new forms of service delivery, such as the NHS Direct telephone advice service, walk‐in‐centres and minor injuries unit, intended to relieve pressure on accident and emergency departments and primary care.
Payment reform featured prominently in Blairs second term, with the introduction of prospective payment, and revised contracts for staff that offered improved pay and conditions. Hospitals had to ensure that patients faced a wait for inpatient treatment of no more than 18 months by the end of March 2001, this target decreasing by 3months each year until a maximum of 6months in March 2005 (Propper et al. 2008).
Productivity growth increased in Blair's third term to 1.41% pa, during which time the growth in overall NHS expenditure had slowed to 4.15% a year, albeit still greater than the 2.79% average growth in GDP. There were no fundamental changes to NHS policy during this term, although patients seeking hospital treatment were offered the choice of at least four providers.
Productivity growth stayed positive under Brown's administration, with average yearly growth rate of 1.13% pa. NHS expenditure grew at a rate of 5.67% a year, despite the economy going into recession, average GDP growth over the period being negative at −1.06%. Patient choice of provider was further extended, and a promise that patients would face a waiting time of no more than 18weeks from referral to treatment was enshrined in the new NHS constitution.
Productivity growth remained positive under the Coalition, averaging 1.56% pa, and the economy returned to growth, GDP increasing by an average of 1.84%. Austerity was the government's watchword, with NHS expenditure growth limited to 1.14%. NHS policy was dominated by the ‘Quality, Innovation, Productivity and Prevention’ challenge to save £15–20bn between 2011 and 2014 and by the development and passing of the Health and Social Care Act, described as the largest ever re‐organisation of the NHS (Timmins, 2012).
8. Discussion
In attempting to measure NHS outputs and inputs as comprehensively as possible, we use several datasets that may not always be consistent throughout the years. As well as the data sources, the output and input categorisations and the quality of the data all have changed considerably over time. Our solution has been to adopt a chained index approach that constructs a time series from pairwise comparisons of financial years. We argue that this approach best accommodates the changing nature of the data, thereby maximising the probability of accurately calculating changes in productivity.
Over the period considered, there will undoubtedly have been technical improvements to the processes involved in the production of the multitude of outputs produced by the NHS. However, as neither production functions for specific outputs nor the overall NHS production function can be observed, it is not possible to determine where the NHS has operated in relation to each period's production function or, by extension, the extent of technical inefficiency in the production process. This is an issue that is not limited to our research and has been a feature of much of the productivity literature. The traditional solution has been to simply assume CRS and zero inefficiency and therefore that any productivity gains are a result of technical innovation. Although there is some cross‐sectional evidence suggesting that an assumption of CRS is tenable among NHS commissioners (Bojke and Gravelle, 2001) and NHS hospitals (Castelli et al. 2015), the absence of technical inefficiencies in the NHS would seem an unsupported assumption. That said, in terms of simply measuring productivity growth, no such assumptions are necessary, it is only when we attempt to explain the sources of growth that we need to either make assumptions and/or identify supporting evidence. This situation is merely a reflection of the view that ‘Specifications of aggregate production functions, using value data, may be nothing more than approximations to an accounting identity and hence can convey no information, per se, about the underlying technology of the representative firm’ (Felipe and Mccombie, 2005).
There is a major limitation with the productivity measure that stems from the use of cost weights to value different activities. Suppose a cheaper way of delivering a particular service is introduced. This might be due to the development of a less costly technology or a change in delivery setting. With cost weights used to reflect the value of such activity, the substitution of the more expensive delivery mode with the cheaper alternative would be captured as a decrease in output, all else equal. The way to avoid such an implication is to apply the same cost weight to those services that are deemed substitutes. We are able to do this for those types of service where it is possible to determine the nature of the substitution. For example, equivalent activity in inpatient and day‐case settings is assigned the same HRG cost weight; branded and generic pharmaceutical products are weighted similarly according to their chemical composition, not their price. But for some services, it is not possible to identify which services have substituted for others. For example, it has been claimed that community care services have substituted for some types of inpatient care, but because these are recorded in completely different ways, it is not possible to determine which services have been substituted and which patients have been affected. In the absence of this information, the productivity measure will be biased downwards.
However, even casual inspection of the volumes of activity in hospital and community settings suggest little evidence of wholesale substitution. Between 2004/2005 and 2013/2014, there was a 13.61% increase in volume of activity in community care. But the growth rate of elective activity has been much faster in the same period: with a 45.20% increase in the number of elective patients treated in hospital (6.43 million to 9.34 million patients). This is unlikely to be due solely to increased need of the population (Quality Watch, 2014). If it were, elective and non‐elective activity would have increased by similar proportions: however, non‐elective activity increased by just 18.30% (6.01 million to 7.11 million patients).
Over the whole time period, the overall picture that emerges is one in which the growth in inputs has been broadly matched by the growth in outputs, with output growth of 88.96% being somewhat greater than growth in inputs 81.58%, yielding positive productivity growth over the full 15years of 4.07%. Productivity growth was negative during the first two terms of Blair's government, with average yearly growth rate of −1.01% pa during the first term (to 2000/2001) and −1.49% pa during the second term (2000/2001–2004/2005). Productivity growth was positive under Blair's third term (2004/2005–2007/2008) at 1.41% pa, and under the Brown government (2007/2008–2010/2011), averaging 1.13% pa. Productivity growth remained positive under the Coalition (2010/2011–2013/2014), averaging 1.56% pa.
In addition, there are two other, possibly related, features of the output and input series that we note. The first is that, as the more policy amenable instrument, inputs show greater variation than outputs. Secondly, output growth appears to be more closely related to lagged input growth than current input growth. As a consequence, the returns of input growth on output may not all be observed immediately, with some of the impact being realised in subsequent periods. This may help explain the observation that productivity growth tends to be positive when input growth has been relatively low. This also implies that positive productivity growth is driven primarily by contractions in input growth. The extent to which this can be continued in the future is doubtful.
Acknowledgements
We thank John Bates and Keith Derbyshire for their assistance, and the journal's referees for their insightful comments on an earlier version of the paper. This is an independent study commissioned and funded by the Department of Health in England as part of a programme of policy research at the Centre for Health Economics (070/0081 Productivity; 103/0001 ESHCRU). The views expressed are those of the authors and not necessarily those of the Department of Health. The Hospital Episode Statistics are copyright © 1998/99 ‐ 2013/14, reused with the permission of The Health & Social Care Information Centre. All rights reserved.
Bojke, C. , Castelli, A. , Grašič, K. , and Street, A. (2017) Productivity Growth in the English National Health Service from 1998/1999 to 2013/2014. Health Econ., 26: 547–565. doi: 10.1002/hec.3338.
Footnotes
In 1998/1999, only NHS Hospital Trusts' inpatient, outpatient (four specialties only) and critical care services activity and their relative unit cost data were included in the RC data collection. The type of NHS activity included has since gradually expanded to include services provided in the following settings: accident and emergency services, radiotherapy, community services, specialist services (e.g. renal dialysis and bone marrow transplant), pathology, radiology, mental health, chemotherapy, diagnostic tests, ambulance services, high‐cost drugs, rehabilitation services, specialist palliative services, hospital travel cost schemes and coronary care services.
References
- Atkinson T. 2005. Atkinson Review: Final Report. Measurement of Government Output and Productivity for the National Accounts. Basingstoke: Palgrave Macmillan. [Google Scholar]
- Balk BM. 2010. An assumption‐free framework for measuring productivity change. Review of Income and Wealth 56:224–256. [Google Scholar]
- Bojke C, Castelli A, Goudie R, Street A, Ward P. 2012. Productivity of the English National Health Service 2003–4 to 2009–10. Centre for Health Economics: York. [Google Scholar]
- Bojke C, Gravelle H. 2001. Is bigger better for primary care groups and trusts? BMJ 322: 599–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castelli A, Dawson A, Gravelle H, Street A. 2007a. Improving the measurement of health system output growth. Health Economics 16: 1091–1107. [DOI] [PubMed] [Google Scholar]
- Castelli A, Dawson D, Gravelle H, Jacobs R, Kind P, Loveridge P, Martin S, O'Mahony M, Stevens P, Stokes L, Street A, Weale M. 2007b. A new approach to measuring health system output and productivity. National Institute Economic Review 200: 105–117. [Google Scholar]
- Castelli A, Laudicella M, Street A. 2008. Measuring NHS output growth, York. Centre for Health Economics research paper 43. [Google Scholar]
- Castelli A, Laudicella M, Street A, Ward P. 2011. Getting out what we put in: productivity of the english national health service. Health Economics, Policy and Law 6: 313–35. [DOI] [PubMed] [Google Scholar]
- Castelli A, Street A, Verzulli R, Ward P. 2015. Examining variations in hospital productivity in the English NHS. The European Journal of Health Economics 16: 243–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chope C, Ellison J. 2015. NHS: productivity:written question – 224314. (Available from: http://www.parliament.uk/business/publications/written-questions-answers-statements/written-question/Commons/ 2015-02-11/224314/) [Accessed on 18 December 2015].
- Coelli T, Prasada Rao DS. 1998. An Introduction to Efficiency and Productivity Analysis. Springer: New York. [Google Scholar]
- Curtis L. 2014. Unit costs of health and social care 2014. (Available from: http://www.pssru.ac.uk/project-pages/ unit-costs/2014/) [Accessed on 18 December 2015, 2014].
- Dawson D, Gravelle H, O'Mahony M, Street A, Weale M, Castelli A, Jacobs R, Kind P, Loveridge P, Martin S, Stevens P, Stokes L. 2005. Developing new approaches to measuring NHS outputs and productivity, Final Report, York. Centre for Health Economic research paper 6. [Google Scholar]
- De Boer S, Van Dalen J, Verbiest P. 1997. Chain Indices in the National Accounts. The Dutch Experience: Statistics Netherlands. [Google Scholar]
- Derbyshire K, Zerdevas P, Unsworth R, Haslam M. 2007. Further Developments in Measuring Quality Adjusted Healthcare Output. Department of Health: Leeds. [Google Scholar]
- Diewert WE. 1998. Index number issues in the consumer price index. The Journal of Economic Perspectives 12: 47–58. [Google Scholar]
- Diewert We, Balk Bm, Fixler D, Fox Kj, Nakamura A. 2010. Price and Productivity Measurement:– Index Number Theory, Vol. 6 Trafford Press: Hitsville, USA. [Google Scholar]
- Eurostat. 2001. Handbook on Price and Volume Measures in National Accounts. Office for Official Publications of the European Communities: Luxembourg. [Google Scholar]
- Felipe J, Mccombie JSL. 2005. How sound are the foundations of the aggregate production function Eastern Economic Journal 31(3): 467–488. [Google Scholar]
- Fenty J, Coupland C, Hippisley‐Cox J, Gravelle H. 2006. Determinants of Consultation Rates Over Time: Implications for Estimating the National Volume of Consultations. QRESEARCH University of Nottingham: Nottingham. [Google Scholar]
- Fisher FM. 2005. Aggregate production functions – a pervasive, but unpersuasive, fairytale. Eastern Economic Journal 31(3): 489–491. [Google Scholar]
- Grašič K, Mason A. 2015. Paying for the quantity and quality of hospital care: the foundations and evolution of payment policy in England. Health Economics Review 5: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harker R. 2015. Health expenditure: social indicators page; Commons briefing papers SN02640. (Available from: http://researchbriefings.parliament.uk/ResearchBriefing/Summary/SN02640) [Accessed on 18 December 2015].
- Harker R. 2012. NHS expenditure; commons briefing papers SN00724. (Available from: http://researchbriefings. parliament.uk/ResearchBriefing/Summary/SN00724) [Accessed on 18 December 2015].
- Hill RJ. 2006. When does chaining reduce the Paasche–Laspeyres spread? An application to scanner data. Review of Income and Wealth 52: 309–325. [Google Scholar]
- Her Majesty's Treasury. 2014. Public expenditure statistical analyses. 2014 10/12/2015; (Available from: https: //www.gov.uk/government/statistics/public-expenditure-statistical-analyses-2014) [Accessed on 18 December 2015].
- House of Commons. 2015. NHS funding and productivity: key issues for the 2015 parliament.;(Available from: http://www.parliament.uk/business/publications/research/key-issues-parliament-2015/health/nhs-funding/) [Accessed on 18 December 2015].
- Lehr J. 1885. Beiträge zur Statistik der Preise Frankfurt.
- Marshall A. 1887. Remedies for fluctuations of general prices. Contemporary Review 51: 355–375. [Google Scholar]
- NHS Choices. 2015. The history of the NHS in England.;(Available from: http://www.nhs.uk/NHSEngland/thenhs/ nhshistory/Pages/the-nhs\%20history.aspx) [Accessed on 18 December 2015].
- NHS England. 2014. Five Year Forward View. NHS England: London. [Google Scholar]
- NHS England. 2015. GP Patient Survey. (Available from: https://gp-patient.co.uk/) [Accessed on 18 December 2015, 2015].
- Oecd. 2001. OECD Productivity Manual: A Guide to the Measurement of Industry‐level and Aggregate Productivity Growth. Organisation for Economic Cooperation and Development: Paris. [Google Scholar]
- Office for National Statistics. 2006. Sources and Methods for Public Service Productivity: Health 2006. Office for National Statistics: London. [Google Scholar]
- Office for National Statistics. 2009. Health Care Output 1995–2007. Office for National Statistics: London. [Google Scholar]
- Office for National Statistics 2015. 2012. Public service productivity estimates: healthcare. Newport, Wales, Office for National Statistics.
- Office for National Statistics. 2015. Key economic time series data: gross domestic product. (Available from: http: //www.ons.gov.uk/ons/site-information/using-the-website/time-series/index.html\#1) [Accessed on 18 December 2015].
- QResearch. 2009. Trends in consultations rates in general practice 1995–2008 tables. NHS Information Centre for Health and Social Care.
- Quality Watch. 2014. Cause for Concern – Qualitywatch Annual Statement, 2014. The Health Foundation and the Nuffield Trust: London. [Google Scholar]
- Propper C, Sutton M, Whitnall C, Windmeijer FE. 2008. Did 'targets and terror' reduce waiting times in England for hospital care? The B. Journal of Economic Analysis & Policy 8(2): 1935–1682. [Google Scholar]
- Street A. 2014. Living through the NHS's famine years. British Medical Journal g6536(349): 1–2. [DOI] [PubMed] [Google Scholar]
- Timmins N. 2012. Never Again? The Story of the Health and Social Care Act 2012. The King's Fund and Institute for Government: London. [Google Scholar]
- Triplett JE. 2011. Health System Productivity. In The Oxford Handbook of Health Economics. [Google Scholar]
- Wikipedia. 2015. List of United Kingdom general elections.;(Available from: https://en.wikipedia.org/wiki/List_ {o}f_{U}nited_{K}ingdom_{g}eneral_{e}lections) [Accessed on 18 December 2015].


