Abstract
Aim
As a result of mutations in TSC1 (9q34) and TSC2 (16p13.3) tumor supressor genes, the mammalian target of the rapamycin (mTor) signaling pathway is overactivated in patients with tuberous sclerosis. Abnormal cell proliferation and differentiation is responsible for the growth several different tumors. The aim of this study was to review tumors in our patients with tuberous sclerosis.
Material and Methods
Thirty-six patients with tuberous sclerosis were reviewed retrospectively in terms of age, sex, family history, clinical findings, presence of tumors, and treatments.
Results
Our study included 36 patients (18/18:M/F) aged between two days and 17 years with a median age of 6 years. There were hypopigmented spots in 30 patients, seizures in 28 patients, and a family history in 11 patients. Tumors related to tuberous sclerosis were renal angiomyolipomas in 21 patients, cardiac rhabdomyomas in 11, subependymal giant cell astrocytomas in seven, and non renal hamartoma in one patient. Everolimus treatment was used in only two patients because of hemodynamic instability.
Conclusions
Tuberous sclerosis is a multisystemic disease characterized by the presence of various benign tumors and neurologic disorders. Renal angiomyolipomas, cardiac rhabdomyomas, and subependymal giant cell astrocytomas are commonly observed in patients with tuberous sclerosis. mTOR inhibitors such as everolimus and sirolimus have been increasingly used in the treatment of these tumors. However, the duration and optimal dose of mTOR inhibitors is still controversial and should be used in selected cases.
Keywords: Angiomyolipoma, rhabdomyoma, subependymal giant cell astrocytoma, tuberosclerosis, tumor
Introduction
Tuberous sclerosis complex (TSC) is a condition which may involve many organs including the brain, retina, kidneys, heart, skin and lung. In tuberous sclerosis which has an autosomal dominant inheritance, mutations in the TSC1 (Tuberous sclerosis complex 1) and TSC2 (Tuberous sclerosis complex 2) genes lead to involvement of hamartin and tuberin proteins which are products of these genes. These proteins inhibit the mTOR pathway which regulates cell growth and differentiation. The mTOR pathway is activated in relation with defect in hamartin and tuberin proteins. As a result of this tumor supression, cell growth and cell differentiation are impaired (1, 2). 9q34 (TSC1) and 16p13 (TSC2) loci were specified for these two genes (3). In conclusion, hamartomas occuring in many systems constitute the characteristics of the disease. Subependimal giant cell astrocytoma (SGCA) which develops in the brain, angiomyolipomas in the kidney and rhabdomyomas in the heart are the tumors which may lead to clinical symptoms. In this retrospective study, it was aimed to evaluate the clinical fidnings and the tumors observed in the patients with tuberous sclerosis who were followed up in our clinic.
Material and Methods
A total of 36 patients who were being followed up with a diagnosis of tuberous sclerosis in the Pediatric Oncology Clinic of our hospital between 2005 and 2015 were included in the study. Ethics committee approval was obtained from the Clinical ResearchEthics Committee of the Ministry of Health Ankara Children’s Hematology and Oncology Education and Research Hospital (2016 034/11.4.2016). The records of the patients included in the study were examined retrospectively and the ages, genders, involvement site, familial history, imaging findings and presence of tumor were recorded. The diagnosis was specified according to the international diagnostic criteria for tuberous sclerosis complex (TSC) which were updated in 2012 (Table 1) (4).
Table 1.
Diagnostic Criteria for Tuberous Sclerosis (2012)
| Major Criteria | Minor Criteria |
|---|---|
| Cortical tubers | Non-renal hamartoma |
| Subependymal nodules | Confetti-like skin lesions |
| Hypomelanocytic macule (at least 3 or more and larger than 5 mm) | Multiple renal cysts |
| Shagreen patch | Hypopigmented patch in the retina |
| Angiofibroma in the face (more than three) | |
| Ungal and periungal fibromas | |
| Retinal hamartomas | |
| Rhabdomyoma in the heart | |
| Lymphangiomatosis in the lung | |
| Angiomyolipoma in the kidney (more than two) |
Definite diagnosis: 2 major or 1 major + >2 minor criteria
Possible diagnosis: 1 major or >2 minor criteria
Statistical analysis
The data obtained from the files were entered in the Statistical Package for the Social Sciences 15,0 for Windows (SPSS Inc.; Chicago, IL, USA) program. The grouping, percentages and differences of the patients with tuberous sclerosis were examined.
Results
Eighteen (50%) of 36 patients in the study were male and 18 (50%) were female. The median age at the time of diagnosis was found to be 6 years (2 days–17 years). Twenty three patients (64%) had been diagnosed in the first year of life. Eleven patients had a positive familial history of TSC. Mental retardation was found in 23 of the patients. The most common cause of presentation was skin lesions in 30 patients (83%). Among these lesions, facial angiofibroma (adenoma sebaceum) was found in 19 patients and “shagreen” patch was found in 10 patients. Brain involvement was found in 31 patients. The most common finding was subepandimal periventricular nodules. Sixteen patients had cortical tubers. Radiological findings were interpreted as subepandimal giant cell astrocytoma in seven patients (Figure 1). The mean age at the time of diagnosis was found to be 6,5 years in seven patients who were found to have subepandimal giant cell astrocytoma; three of these patients were female and four were male. Six patients presented with seizure and infantile spasm was found in one of these patients. The tumor was excised in one patient, because hydrocephaly developed and ventriculoperitoneal shunt operation was performed. Everolimus treatment was initiated in one patient, because the mass which was radiologically defined to be SGCA was enlarged (Table 3). This patient had used everolimus in the neonatal period because of cardiac rhabdomyoma. Everolimus was discontinued three months later because of incompliance with treatment. The patient was monitored without a change in the mass size.
Figure 1.
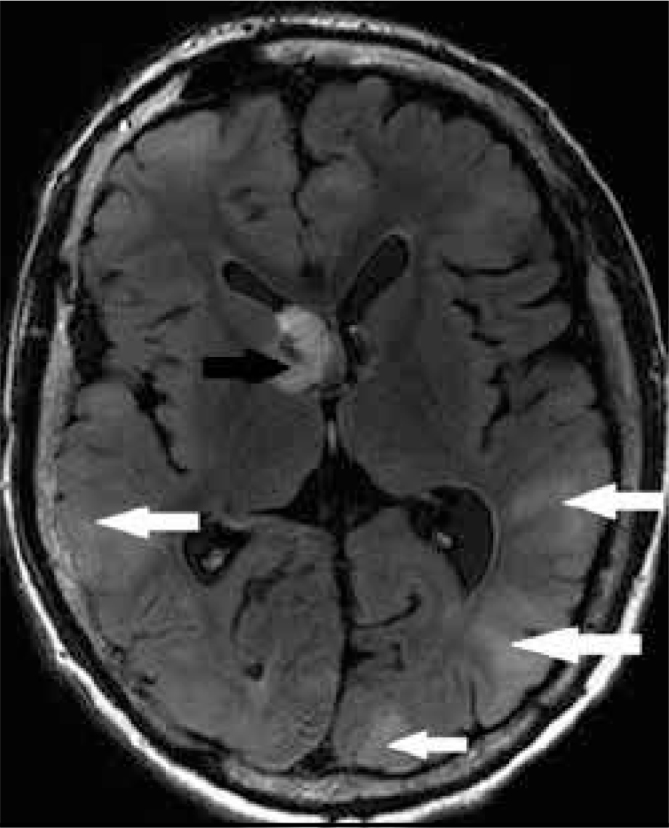
Cortical tubers and subependymal giant cell astrocytoma in magnetic resonance imaging
Table 3.
Characteristics of the Tumors Observed in Patients with Tuberous Sclerosis
| Tumor type | Number |
|---|---|
| Subependymal giant cell astrocytoma astrocytoma | 7 |
| Treatment | |
| Follow-up | 5 |
| Surgery (shunt+tumor excision) | 1 |
| Everolimus | 1 |
| Renal angiomyolipoma | 28 |
| Treatment | |
| Follow-up | 27 |
| Nephrectomy | 1 |
| Cardiac rhabdomyoma | 11 |
| Asymptomatic | 5 |
| Murmur | 3 |
| Cyanosis | 2 |
| Arrythmia | 1 |
| Treatment | |
| Surgery | 2 |
| Everolimus | 2 |
| Spontaneous regression | 7 |
Renal angiomyolipoma (AML) was found in 21 patients (58%) and renal cyst was found in 10 patients (28%). Unilateral nephrectomy was performed in only one patient because of hypertension and hematuria. Nonrenal hamartoma was diagnosed following surgical excision in one patient who had a retroperitoneal mass.
Cardiac rhabdomyoma was found in a total of 11 patients. Four of these were diagnosed with prenatal fetal echocardiography. The mean age of the patients with cardiac rhabdomyoma was found to be 3,5 years (1 week–15 years). Multiple rhabdomyomas were found in five patients (Figure 2). Five patients were asymptomatic. Murmur, arrythmia and cyanosis were found in the other patients. Surgery was performed in two patients at the age of two months and five months because of severe right ventricule outlet obstruction and hemodynamic disorder. In one patient who was diagnosed prenatally, multiple rhabdomyomas obstructing the right ventricular outlet were found in the right and left ventricles. This patient who had severe cyanosis and arryhtmia had no chance for surgery because of intramural localization of the tumors. Everolimus which inhibits mTOR was used in this patient. Everolimus was given orally at a dose of 0.25 mg two times a day two days a week. Treatment was continued such that the blood everolimus level was kept between 5 and 15 ng/mL. The patient responded markedly to this treatment. Two of eight rhabdomyomas disappeared completely in two months. The others were reduced to about a half. Treatment was discontinued after a total period of 2.5 months. The second patient who was diagnosed prenatally presented with apnea and cyanosis at the age of 15 days. Everolimus was used because of arrythmia. When partial reduction in the rhabdomyomas was provided at the end of two months, the treatment was discontinued. In the other patients, rhabdomyomas showed spontaneous regression (Table 3). All patients who underwent surgery and received medical treatment are still being followed up in an asymptomatic state.
Figure 2.
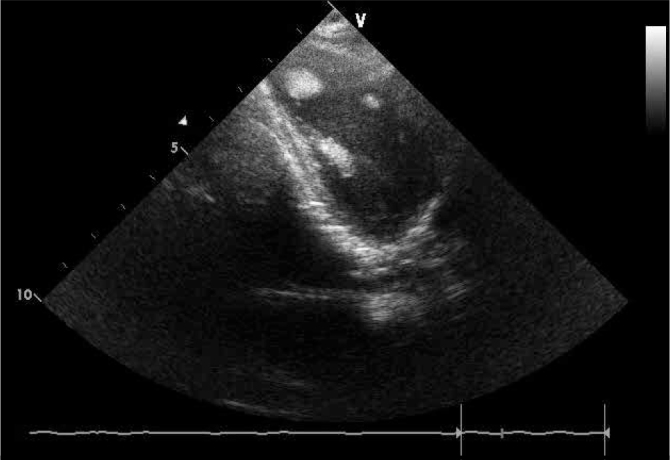
Echocardiographic appearance of multiple cardiac rhabdomyomas
Discussion
Tuberous sclerosis is mainly characterized by mental retardation, epilepsy, central nervous system involvement, and skin involvement. The majority of patients are diagnosed below the age of 15 months and the incidence decreases as age increases (5, 6). The prevalence ranges between 1:5000 and 1:10,000 (5, 6). Sirolimus and everlimus, which are among the drugs developed based on the fact that the gene disorders in tuberous sclerosis excessively activate the mTOR pathway, are currently used in the treatment (7).
Skin lesions are among the most commonly observed findings in patients with tuberous sclerosis and found in approximately 90% of patients (8–10). Among these, the most commonly observed lesions are hypomelanotic macules with different sizes, which are generally oval in shape and frequently observed on the trunk and extremities. Presence of at least three macules has been found significant for the diagnosis because one or two hypomelanotic macules may be observed in the normal population (8–10). Hypomelanotic macules were present in 83% of the patients in our clinic. The lesions with characteristics of angiofibroma as pink-red papules, which were previously named adenoma sebaceum, are localized on the face and observed in 75% of patients (8–10). They are typically observed between the ages of 2 and 5 years. Presence of three or more of these lesions are considered a major criterion for the diagnosis of TSC (11–14). “Shagreen” patches are generally observed in the first decade in approximately 50% of patients and typical for TSC (8–11). In our study, “shagreen” patches were found with a frequency of 28%.
The most important findings that affect morbidity and mortality rates in tuberous sclerosis include findings related with the central nervous system (4). These include neuropsychiatric diseases related with brain structure, tubers, tumors, and TSC (4). A part of the neurologic findings are among the major and minor criteria used in the diagnosis (4, 9). Subependymal nodules and SGCA are among the major findings. Subependymal nodules are observed in 80% of patients and SGCA is observed in 5–15% of patients (12). There is a risk for subependymal nodules to transfrom into SGCA. The risk factors for transformation to SGCA include localization near the foramen monro, calcification, visualization with gadolinium, and size larger than 5 mm (12). Tubers were found in 16 (44%) of our patients and SGCA was found in seven (19%). The neurologic findings in patients with tuberous sclerosis are mostly in the form of epilepsy. One third of the clinical picture of epilepsy is in the form of infantile spasm, and 69% of this group had their first seizure before the age of one year (13). Intellectual development is generally affected; the frequency and time of onset of the seizures has a direct effect on intellectual development. Mental retardation is observed in 50% of patients and this renders control of seizures difficult (13). Twenty-eight (78%) of our patients had some kind of seizure. Angiomyolipomas are benign tumors that contain vascular, smooth muscle, and adipose tissues (14–16). Renal cystic disease, angiomyolipoma (renal angiolipoma), polycystic renal disease, and rarely, renal cell carcinoma are observed in 80% of pediatric patients with tuberous sclerosis. Renal lesions may lead to hypertension and chronic renal failure in untreated patients (14–16). Renal angiomyolipoma was present in 21 (58%) of our patients. Renal cysts were present in ten patients. Only one of our patients was symptomatic. Nephrectomy was performed in this patient because of hypertension and severe hemorrhage. Renal anomalies were observed in a total of 21 patients (86%) and this rate was compatible with the literature (14–16). Although most renal lesions are asymptomatic, they may lead to symptoms and renal failure with a higher rate in adulthood. Monitoring of renal functions, hypertension control, radiologic imaging, and monitoring of renal lesions should be performed regularly in these patients.
Cardiac rhabdomyoma, which is observed in tuberous sclerosis, is a benign cardiac tumor. It is the most common cardiac finding in tuberous sclerosis (17, 18). Thirty to fifty percent of rhabdomyomas show spontaneous regression at about the age of 2–4 years (17, 18). Some may lead to cardiac muscle injury, rhythm disturbance or obstruction by affecting the cardiac region where they are localized (18). Although they usulally do not cause severe problems, they are among the major findings. Problems may occur if they are localized near the valves. They may be specified in the fetal period. Similarly, four (40%) of our patients’ rhabdomyomas were diagnosed prenatally. Cardiac rhabdomyomas generally regress in the first six years. Cardiac rhabdomyomas can be treated with medication and rarely surgery, if they lead to hemodynamic impairment (19). In recent years, a significant increase in treatment response has been observed with mTor inhibtor drugs. We found cardiac rhabdomyoma in 11 (28%) patients who were being followed up for tuberous sclerosis in our clinic. Two of our patients with rhabdomyoma received ever-olimus treatment in early infancy following prental diagnosis because of rhabdomyomas that caused hemodynamic impairment. Both patients responded dramatically positively to treatment.
Although hamartomas that occur in tuberous sclerosis are benign, they may lead to life-threatening conditions depending on the area of involvement. Treatment is recommended in case of involvement of functions of vital organs including the brain and heart, and in the presence of renal lesions that could lead to renal failure. In treatment, one tries to improve the dysfunction of the relevant organ depending on the condition of the disease.
In light of current information, mTOR inhibitor drugs (sirolimus, everolimus) are used for treatment based on the fact that the condition arises from excessive action of the mTOR pathway. Therefore, there is an increased number of studies reporting that these drugs are being used in lesions related with tuberous sclerosis in the literature. However, mTOR inhibitors should only be used in children in the presence of life-threatening symptoms, cardiac hemodynamic impairment, and SGCA, which may cause rapidly growing hydrocephaly, because the long-term adverse effects are not known, especially in children. In conclusion, renal angiomyolipoma, cardiac rhabdomyoma, and SGCAs observed in 36 patients with tuberous sclerosis were evaluated in this study. mTOR inhibitor everolimus was used in only two patients because of life-threatening symptoms. The other patients are being clinically followed up in an asymptomatic state.
Table 2.
Characteristics of the Patients with Tuberous Sclerosis
| Number of patients (n) | 36 |
|---|---|
| Age (year) (median, range) | 6 (0–17) |
| Sex (M/F) | 18/18 |
| Presentation findings (n) | |
| Epilepsy | 28 (78%) (5 infantile spasm) |
| Prenatal | 4 |
| Age (year) at the time of diagnosis (median, range) | 6 years (2 days–17 years) |
| Familial history | 11 (%31) |
| Skin findings (n) | |
| Hypomelanocytic macules | 30 |
| “Shagreen” patch | 10 |
| Facial angiofibroma | 19 |
| Brain findings (n) | 31 (23 patients MMR) |
| Subependymal nodules | 27 |
| Cortical tuber | 16 |
| SGCA | 7 |
| Heart involvement (n) | 11 |
| Renal involvement (n) | 28 |
MMR: mental motor retardation; SGCA: subependymal giant cell astrocytoma
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from Ankara Pediatrics Training and Research Hospital (11/04/2016 - 034).
Informed Consent: Written informed consent was not received due to the retrospective nature of this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.E, F.E.; Design - S.E., Ş.H.; Supervision - S.E., F.E., A.D., D.Ö.; Materials - S.E., F.E., İ.Ç., A.G.; Data Collection and/or Processing - F.E., S.E., A.G.; Analysis and/or Interpretation - S.E., F.E., D.Ö.; Literature Review - S.E., Ş.H.; Writing - S.E., Ş.H.; Critical Review - D.Ö., İ.Ç., A.D.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med. 2006;355:1345–56. doi: 10.1056/NEJMra055323. https://doi.org/10.1056/NEJMra055323. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz RA, Fernández G, Kotulska K, Józwiak S. Tuberous sclerosis complex: advances in diagnosis, genetics, and management. J Am Acad Dermatol. 2007;57:189–202. doi: 10.1016/j.jaad.2007.05.004. https://doi.org/10.1016/j.jaad.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Ng KH, Ng SM, Parker A. Annual review of children with tuberous sclerosis. Arch Dis Child Educ Pract Ed. 2015;100:114–21. doi: 10.1136/archdischild-2013-304948. 30. https://doi.org/10.1136/archdischild-2013-304948. [DOI] [PubMed] [Google Scholar]
- 4.Hope N, Darcy AK. Tuberous sclerosis complex diagnostic criteria update. Pediatr Neurol. 2013;49:243–54. doi: 10.1016/j.pediatrneurol.2013.08.001. https://doi.org/10.1016/j.pediatrneurol.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devlin LA, Shepherd CH, Crawford H, Morrison PJ. Tuberous sclerosis complex: clinical features, diagnosis, and prevalence within Northern Ireland. Develop Med Child Neurol. 2006;48:495–9. doi: 10.1017/S0012162206001058. https://doi.org/10.1017/S0012162206001058. [DOI] [PubMed] [Google Scholar]
- 6.Hong CH, Darling TN, Lee CH. Prevalence of tuberous sclerosis complex in Taiwan: a national population-based study. Neuroepidemiol. 2009;33:335–41. doi: 10.1159/000254569. https://doi.org/10.1159/000254569. [DOI] [PubMed] [Google Scholar]
- 7.Curatolo P, Moavero R. mTOR inhibitors in Tuberous sclerosis complex current. Neuropharmacol. 2012;10:404–15. doi: 10.2174/157015912804143595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vanderhooft S, Francis J, Pagon R, Smith L, Sybert V. Prevalence of hypopigmented macules in a healthy population. J Pediatr. 1996;129:355–61. doi: 10.1016/s0022-3476(96)70066-5. https://doi.org/10.1016/S0022-3476(96)70066-5. [DOI] [PubMed] [Google Scholar]
- 9.Erol İ, Savaş T, Şekerci S, et al. Tuberous sclerosis complex; single center experience. Turk Ped Arch. 2015;50:51–60. doi: 10.5152/tpa.2015.2138. https://doi.org/10.5152/tpa.2015.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jozwiak S, Schwartz RA, Janniger CK, Bielicka-Cymerman J. Usefulness of diagnostic criteria of tuberous sclerosis complex in pediatric patients. J Child Neurol. 2000;15:652–9. doi: 10.1177/088307380001501003. https://doi.org/10.1177/088307380001501003. [DOI] [PubMed] [Google Scholar]
- 11.Jozwiak S, Schwartz RA, Janniger CK, Michalowicz R, Chmielik J. Skin lesions in children with tuberous sclerosis complex: their prevalence, natural course, and diagnostic significance. Int J Dermatol. 1998;37:911–7. doi: 10.1046/j.1365-4362.1998.00495.x. https://doi.org/10.1046/j.1365-4362.1998.00495.x. [DOI] [PubMed] [Google Scholar]
- 12.Baron Y, Barkovich J. MRI imaging of tuberosclerosisin neonates and young infants. AJNR Am J Neuroradiol. 1999;20:907–16. [PMC free article] [PubMed] [Google Scholar]
- 13.Saltık S, Karatoprak EY, Taşel B. Tüberoskleroz kompleksi tanılı hastalarda epilepsinin özellikleri ve klinik seyri. Turk Arch Ped. 2013;48:123–30. https://doi.org/10.4274/tpa.116. [Google Scholar]
- 14.Bissler J, Henske E. Renal manifestations of tuberous sclerosis complex. In: Kwiatkowsi D, Whittemore V, Thiele E, editors. Tuberous sclerosis complex: genes, clinical features, and therapeutics. Weinheim: Wiley-Blackwell; 2010. pp. 302–7. https://doi.org/10.1002/9783527630073.ch15. [Google Scholar]
- 15.Ewalt DH, Sheffield E, Sparagana SP, Delgado MR, Roach ES. Renal lesion growth in children with tuberous sclerosis complex. J Urol. 1998;160:141–5. https://doi.org/10.1097/00005392-199807000-00066. [PubMed] [Google Scholar]
- 16.Bernstein J. Renal cystic disease in the tuberoussclerosis complex. Pediatr Nephrol. 1993;7:490–5. doi: 10.1007/BF00857581. https://doi.org/10.1007/BF00857581. [DOI] [PubMed] [Google Scholar]
- 17.Kocabas A, Ekici F, Çetin İ, et al. Cardiac rhabdomyomas associated with tuberous sclerosis complex in 11 children: Presentation to outcome. Pediatric Hematol Oncol. 2013;30:71–9. doi: 10.3109/08880018.2012.734896. https://doi.org/10.3109/08880018.2012.734896. [DOI] [PubMed] [Google Scholar]
- 18.Freedom RM, Lee KJ, MacDonald C, Taylor G. Selected aspects of cardiac tumors in infancy and childhood. Pediatr Cardiol. 2000;21:299–316. doi: 10.1007/s002460010070. https://doi.org/10.1007/s002460010070. [DOI] [PubMed] [Google Scholar]
- 19.Demir HA, Ekici F, Erdem AY, Emir S, Tunç B. Everolimus: a challenging drug in the treatment of multifocal inoperable cardiac rhabdomyoma. Pediatrics. 2012;130:e243–7. doi: 10.1542/peds.2011-3476. https://doi.org/10.1542/peds.2011-3476. [DOI] [PubMed] [Google Scholar]


