Regional analgesia is currently the most effective form of pain relief for women in labor and may include an epidural, a spinal or a combination of the two techniques. The evolution of maintenance of epidural analgesia has progressed from manually delivered intermittent boluses to continuous epidural infusion (CEI), to the addition of patient-controlled epidural analgesia (PCEA) boluses for breakthrough pain and now programmed intermittent epidural bolus (PIEB). PIEB has evolved as a superior method for delivering labor analgesia due to reduced hourly local anesthetic consumption, less need for clinician intervention, and improved maternal pain and satisfaction scores.
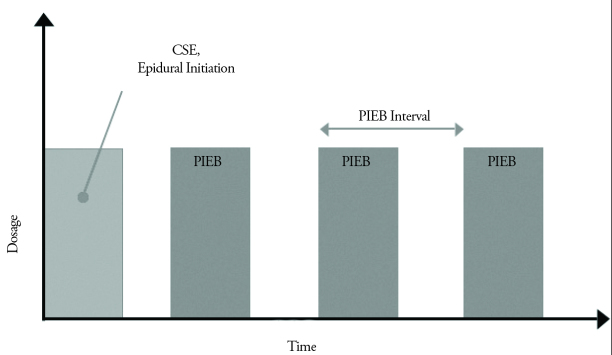
Intermittent boluses of the epidural catheter allows a wider spread throughout the epidural space, which may contribute to better quality of analgesia in the clinical setting (1). Higher injection pressure with boluses produced a more uniform spread of solution within the epidural space compared with continuous infusions (1–3). Initial studies evaluating the PIEB technique used non-commercial programmed bolus devices or provided intermittent epidural boluses manually. In 2014, in the USA Smith Medical released the CADD Solis Epidural Pump (Smiths Medical, St. Paul, MN, USA) which could provide PIEB along with PCEA. This pump can be programmed to deliver small, regularly timed intermittent boluses for maintenance of labor analgesia and specify “lockout” intervals to ensure patient safety (Figure 1). This pump ensures specific limits are set to not allow “stacking” of boluses and potentially unsafe administration of local anesthetics; a feature that was observed with previous design attempts.
Figure 1.
Prorgammed Intermittent Epidural Bolus (PIEB)
Several early studies found clinical advantages of PIEB when compared to CEI with and without PCEA for labor analgesia. A systematic review in 2013 showed that the use of intermittent epidural bolus was associated with several clinically important outcomes such as improved patient satisfaction, reduced local anesthetic consumption and possibly the need for decreased interventions for inadequate analgesia (4). Since implementing the new delivery pump, further studies have complemented these initial findings.
Intermittent epidural bolus delivery has been associated with reduced hourly bupivacaine consumption (5–7). Results from the meta-analysis showed there was a statistically significant reduction in total local anesthetic delivered with PIEB (MD, −1.2 mg h-1 bupivacaine; 95% CI, −2.2 and −0.3) (4). Although this difference is small, reduced local anesthetic consumption could translate into clinically significant outcomes for patients, such as reducing the incidence of motor block and the need for instrumental delivery. Pooled results from the systematic review approached, but did not achieve statistical significance, for a reduction of instrumental delivery rate with PIEB (OR, 0.59; 95% CI, 0.35–1.00) (4). One study by Capogna et al. (8), unlike the others included in the analysis, was designed and powered to detect a difference in instrumental delivery rates (8). This study reported a significant reduction with PIEB compared with CEI (7% vs. 20%; p=0.03). Interestingly this large study that examined incidence of motor block as the primary outcome, reported a greater incidence of motor blockade with CEI using the modified Bromage score. The authors attribute the higher rates of instrumental delivery to greater motor blockade present in the CEI group. This finding may in fact reflect the total levobupivacaine consumption, number of patients requiring additional PCEA boluses, and mean number of PCEA boluses per patient which were lower in the PIEB group (p<0.001) (8).
Further support for the reduction in total local anesthetic consumption is observed when evaluating the need for rescue clinician boluses. It has been documented that PIEB is associated with less need for clinician intervention for inadequate pain control. There has been observed an increase in time to the first rescue bolus (5–7, 9, 10) and a lower number of manual boluses (5, 11, 12) in several studies. This has impact for both the parturient and the anesthesia work load. The occurrence of breakthrough pain requiring a clinician administered rescue bolus results in increased workload for the anesthesiologist and may lead to a delay in pain relief for the patient. A reduction in the number of women requiring clinician boluses was demonstrated in a recent retrospective analysis by McKenzie et al. (13) Fewer patients in the PIEB group required rescue clinician boluses compared to the CEI group (12% vs. 19%, p=0.012). The authors concluded that this difference would be expected to reduce workload and positively impact a busy clinical service. In addition, there has been no study to date that has observed an increased need for clinician boluses using a PIEB regimen for labor analgesia.
Improved pain score is often the primary outcome in studies comparing PIEB to tradiational CEI for labor analgesia. There is some evidence to suggest that pain scores may be improved with PIEB delivery. Chua et al. (9) found lower pain scores when PIEB was compared to CEI while Lim et al. (11) demonstrated a lower incidence of breakthrough pain in the PIEB group. Although a majority of studies have not demonstrated a clinically significant difference in support of improved pain scores with PIEB delivery, there certainly has not been a study that showed inferior labor analgesia.
Finally, as the health care practices evolve toward patient centered care and physician enagagement, consideration of patient satisfaction with their labor analgesia is paramount. PIEB has gained considerable attention for the ability to improve patient satisfaction with their labor experience (6, 11). The systematic review identified greater maternal satisfaction in the PIEB groups when evaluated by using a verbal rating scale (VRS) (4). Improved maternal satisfaction may loosely reflect improved analgesia and in many studies represents a surrogate measure of analgesia (4). However, maternal satisfaction may encompass maternal involvement in decision making, perception of emotional control and maternal expectations (4) which may make it the more clinically relevant research goal. The clear advantage of PIEB delivery for improved maternal satisfaction has been complemented in the most recent studies. One recent study compared maternal satisfaction, with PIEB at different local anesthetic concentrations, to standard CEI in labor analgesia and found that PIEB was associated with equally high maternal satisfaction and no adverse outcomes (14).
The recent increase in implementation and research in PIEB delivery has generated support for it being a superior method of maintenance labor analgesia. Evidence supports advantages for both the health care team, with decreased work load requirements, and for the patient with less local anesthetic consumption and improved maternal satisfaction when compared to conventional CEI.
References
- 1.Kaynar AM, Shankar KB. Epidural infusion: continuous or bolus? Anesth Analg. 1999;89:534. doi: 10.1097/00000539-199908000-00063. https://doi.org/10.1213/00000539-199908000-00063. [DOI] [PubMed] [Google Scholar]
- 2.Hogan Q. Distribution of solution in the epidural space: examination by cryomicrotome section. Reg Anesth Pain Med. 2002;27:150–6. doi: 10.1053/rapm.2002.29748. https://doi.org/10.1097/00115550-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Power I, Thorburn J. Differential flow from multihole epidural catheters. Anaesthesia. 1988;43:876–8. doi: 10.1111/j.1365-2044.1988.tb05605.x. https://doi.org/10.1111/j.1365-2044.1988.tb05605.x. [DOI] [PubMed] [Google Scholar]
- 4.George RB, Allen TK, Habib AS. Intermittent epidural bolus compared with continuous epidural infusions for labor analgesia: a systematic review and meta-analysis. Anesth Analg. 2013;116:133–44. doi: 10.1213/ANE.0b013e3182713b26. https://doi.org/10.1213/ANE.0b013e3182713b26. [DOI] [PubMed] [Google Scholar]
- 5.Fettes PD, Moore CS, Whiteside JB, McLeod GA, Wildsmith JA. Intermittent vs continuous administration of epidural ropivacaine with fentanyl for analgesia during labour. Br J Anaesth. 2006;97:359–64. doi: 10.1093/bja/ael157. https://doi.org/10.1093/bja/ael157. [DOI] [PubMed] [Google Scholar]
- 6.Leo S, Ocampo CE, Lim Y, Sia AT. A randomized comparison of automated intermittent mandatory boluses with a basal infusion in combination with patient-controlled epidural analgesia for labor and delivery. Int J Obstet Anesth. 2010;19:357–64. doi: 10.1016/j.ijoa.2010.07.006. https://doi.org/10.1016/j.ijoa.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 7.Sia AT, Lim Y, Ocampo C. A comparison of a basal infusion with automated mandatory boluses in parturient-controlled epidural analgesia during labor. Anesth Analg. 2007;104:673–8. doi: 10.1213/01.ane.0000253236.89376.60. https://doi.org/10.1213/01.ane.0000253236.89376.60. [DOI] [PubMed] [Google Scholar]
- 8.Capogna G, Camorcia M, Stirparo S, Farcomeni A. Programmed intermittent epidural bolus versus continuous epidural infusion for labor analgesia: the effects on maternal motor function and labor outcome. A randomized double-blind study in nulliparous women. Anesth Analg. 2011;113:826–31. doi: 10.1213/ANE.0b013e31822827b8. https://doi.org/10.1213/ANE.0b013e31822827b8. [DOI] [PubMed] [Google Scholar]
- 9.Chua SM, Sia AT. Automated intermittent epidural boluses improve analgesia induced by intrathecal fentanyl during labour. Can J Anaesth. 2004;51:581–5. doi: 10.1007/BF03018402. https://doi.org/10.1007/BF03018402. [DOI] [PubMed] [Google Scholar]
- 10.Davies AO, Fettes IW. A simple safe method for continuous infusion epidural analgesia in obstetrics. Can Anaesth Soc J. 1981;28:484–7. doi: 10.1007/BF03010363. https://doi.org/10.1007/BF03010363. [DOI] [PubMed] [Google Scholar]
- 11.Lim Y, Sia AT, Ocampo C. Automated regular boluses for epidural analgesia: a comparison with continuous infusion. Int J Obstet Anesth. 2005;14:305–9. doi: 10.1016/j.ijoa.2005.05.004. https://doi.org/10.1016/j.ijoa.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Wong CA, Ratliff JT, Sullivan JT, Scavone BM, Toledo P, McCarthy RJ. A randomized comparison of programmed intermittent epidural bolus with continuous epidural infusion for labor analgesia. Anesth Analg. 2006;102:904–9. doi: 10.1213/01.ane.0000197778.57615.1a. https://doi.org/10.1213/01.ane.0000197778.57615.1a. [DOI] [PubMed] [Google Scholar]
- 13.McKenzie CP, Cobb B, Riley ET, Carvalho B. Programmed intermittent epidural boluses for maintenance of labor analgesia: an impact study. Int J Obstet Anesth. 2016;26:32–8. doi: 10.1016/j.ijoa.2015.11.005. https://doi.org/10.1016/j.ijoa.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Nunes J, Nunes S, Veiga M, Cortez M, Seifert I. A prospective, randomized, blinded-endpoint, controlled study - continuous epidural infusion versus programmed intermittent epidural bolus in labor analgesia. Rev Bras Anestesiol. 2016;66:439–44. doi: 10.1016/j.bjane.2014.12.006. https://doi.org/10.1016/j.bjan.2015.10.003. [DOI] [PubMed] [Google Scholar]