The advantages of Programmed Intermittent Epidural Bolus (PIEB) for the maintenance of labor analgesia have been clearly established. Numerous studies have highlighted benefits including improved patient satisfaction, reduced local anesthetic consumption and a shorter duration of labor (1). Despite the argument used by Carvalho and Riley (2) to minimize the clinical utility of these differences from traditional delivery of labor analgesia, the authors feel that these outcomes would matter to a laboring parturient. Until the advent of PIEB most centers providing obstetrical care have used Continuous Epidural Infusion (CEI) with or without Patient Controlled Epidural Analgesia (PCEA) for labor analgesia. The analgesic solution usually consists of a dilute local anesthetic, with or without an opioid. CEI has proved to achieve adequate labor analgesia and is advocated by obstetrical anesthesia task forces (3). Until the introduction of PIEB, there had been no major advances in the delivery of labor analgesia. Therefore, the documented clinical advantages of PIEB should not be dismissed so easily by Carvalho and Riley. Any improvement, even if statistically small, may be considered important to a laboring woman when the outcomes include improved satisfaction, shorter duration of labor and reduced risk of instrumental delivery (1, 4). In the era of shared-care decision making and patient-centered care, an intervention that can improve labor pain, which is consistently ranked high on pain rating scales compared to other painful life experiences (5), would likely be sought after by patients. Clearly, the decision to stray from an established therapy requires careful deliberation. Converting the maintenance of labor analgesia to PIEB technology warrants a review of the cited clinical advantages, consideration of patient safety, ease of implementation, need for caregiver education, and assessment of financial burden. As the toted clinical advantages have been highlighted in the first part of the debate, the ease in which PIEB can be implemented will be outlined based on experienced garnered from the author’s care institution.
In the autumn of 2014, the IWK Health Centre implemented the CADD®-Solis PIEB pumps to administer labor analgesia. As administering labor analgesia requires the engagement of nursing, midwifes, physicians and patients, it was imperative that all parties were aware of the clinical consequences of changing delivery mechanisms. Implementation of the PIEB pumps was preceded by education sessions to all birth unit staff. Informal orientation sessions were provided by CADD®-Solis pump representatives to address the technical differences in delivering labor analgesia (i.e. pump programming, line priming, and drug delivery). Clinical implications were conveyed to birth unit nurses and anesthesia assistants by a staff anesthesiologist. The clinical concerns covered the need for routine monitoring of motor and sensory block and blood pressure to detect the presence of high block and hypotension, respectfully. The importance of the education sessions cannot be overstated when introducing a novel device. However, as all parties were invested in learning about a device that may improve labor analgesia for their patients, providing the required education was instituted with relative ease.
To provide labor analgesia using the CADD® PIEB pump there are several parameters that must be programmed into the epidural pump software. The PIEB bolus interval (the amount of time that elapses from the beginning of one intermittent bolus to the beginning of the next bolus), the time to the first PIEB bolus after starting the pump (referred to as the “NEXT bolus”), the PIEB volume of local anesthetic (with or without opioid), and the PCEA volume and lockout period must all be determined. One further decision had to be made before pump initiation. The CADD® pump has two options for the way the PIEB bolus interacts with the PCEA function. In the first option, a delivered PCEA dose delays the beginning of the next PIEB by the PCEA lockout time (Figure 1). With the second option, a delivered PCEA dose delays the beginning of the next PIEB by the PIEB bolus interval time (Figure 2) (6). At the IWK Health Centre the first option was chosen because of concerns of prolonged PIEB lockouts with repetitive PCEA uses. The anesthesiologists recognized that attempts to time the PCEA requests to the PIEB settings could lead to delays in treating breakthrough pain and impact efficiency.
Figure 1.
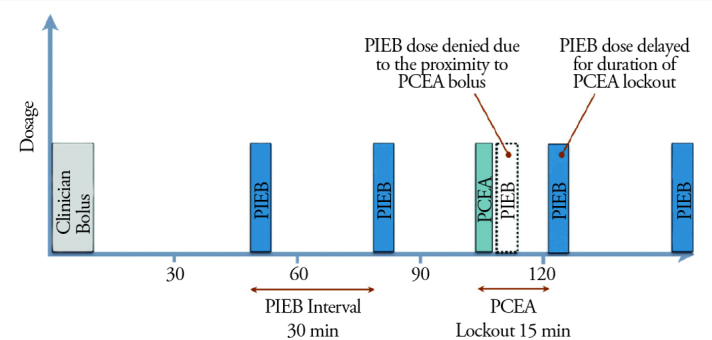
Programmed Intermittent Epidural Bolus (PIEB) with the bolus interval set to patient-controlled epidural analgesia (PCEA) lockout delay (5)
Figure 2.
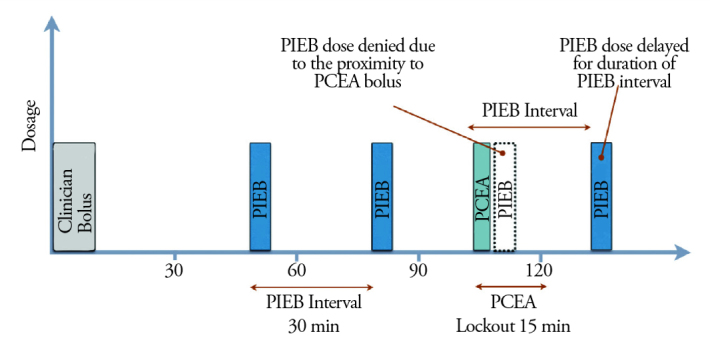
Programmed Intermittent Epidural Bolus (PIEB) with the bolus interval set to PIEB interval delay (5)
Initial pump settings at the IWK Health Centre were guided by the current CEI hourly ropivacaine dose and primary work by Wong et al. (7) examining the optimal PIEB bolus volume and lockout period. Initial pump parameters also considered the evidence that PIEB labor analgesia has a higher threshold for motor blockade because the intraneural concentration is reduced as local anesthetic diffuses out of the nerve between boluses (8). Therefore, despite an established CEI program which provided 6 mL h−1 of ropivacaine 0.1% + fentanyl 2 μg mL−1, initial PIEB pump settings were chosen at 6 mL every 30 minutes. Quality improvement processes including nursing feedback and data downloads from the pumps suggested potential increased motor block and reduced PCEA use. To address these concerns, the PIEB interval was increased from 30 to 45 minutes and the bolus volumes increased correspondingly. The adjusted and current delivery method provides 8 mL every 45 min with the first bolus provided 15 minutes after pump initiation. These setting more closely reflected the findings of Wong et al. (7) who noted a trend toward local anesthetic sparing without a sacrifice in analgesia by increasing the volume and time between scheduled intermittent boluses. PCEA was programmed with the established regimen of 6 mL of the epidural maintenance solution with a 10 minute lockout. The standard flow rates for the CADD® pump are 0 to 500 mL min−1, so the median flow rate was chosen for bolus delivery (250 mL min−1).
The emphasis on continuous quality improvement is of the utmost importance when transitioning to a new technique of providing maintenance analgesia for labor. The bolus delivery method of PIEB may be associated with more abrupt physiological changes such as hypotension and motor block compared with CEI (6). A theoretical concern specific to PIEB delivery relates to the delay in the first dose, the “NEXT bolus”. It is possible that pump occlusion or unintentional intrathecal catheter placement may only become apparent when this bolus is initiated, anywhere from 15–45 minutes after epidural completion (6). However, there have been no documented cases of high block or inadequate analgesia due to this delay noted thus far. When initiating PIEB pump settings, routine physiologic monitoring should be in place to detect any of these undesired side effects and dose adjustments completed if warranted. Increased vigilance is required when monitoring blood pressure, sensory and motor block, and fetal heart rate, but assessments should not be more cumbersome or burden health care providers more than required for standard practice (6). To date, there does not appear to be any additional risk associated with PIEB versus CEI combined with PCEA delivery (6).
Skeptics may argue that the cost of implementation may not be justified until pump parameters are established. The cost of purchasing additional pumps, software, and tubing does need to be weighed against the perceived benefits when considering PIEB implementation. However, between ongoing institutional quality improvement inquiries and evidence provided from dose finding studies (7, 9), the authors feel there is sufficient support to initiate the program. Authors in the field have suggested maintaining current hourly local anesthetic dose or reducing the dose by 10%–25% if the current hourly CEI doses is high or a more concentrated local anesthetic solution (6). High flow rates should be maintained to increase the bolus spread within the epidural space (10). Pump settings such as those used at the IWK Health Centre may be employed. These parameters have been supported in the literature by a recent study that indicated the optimal PIEB interval is approximately 40 minutes (9).
The advantages of PIEB for labor analgesia: the local anesthetic–sparing effect (fewer instrumental vaginal deliveries, less motor blockade, and shorter duration of labor) and improvement in maternal satisfaction cannot be ignored. If epidural pumps are required to be purchased or upgraded, the institution should consider pumps capable of providing PIEB with PCEA. As outlined, the implementation of the new technique requires care-giver education, pump programming guided by evidence available in the literature and a quality improvement mechanism to make dose adjustments as required to ensure patient safety. This program was easily established at the IWK Health Centre, with minimal adjustments required. The ease of transitioning from an established regimen of CEI maintenance of labor analgesia should motivate other obstetrical centers to pursue PIEB as a possibly superior method of delivering labor analgesia.
References
- 1.George RB, Allen TK, Habib AS. Intermittent epidural bolus compared with continuous epidural infusions for labor analgesia: a systematic review and meta-analysis. Anesth Analg. 2013;116:133–44. doi: 10.1213/ANE.0b013e3182713b26. https://doi.org/10.1213/ANE.0b013e3182713b26. [DOI] [PubMed] [Google Scholar]
- 2.Riley ET, Carvalho B. Programmed Intermittent Epidural Boluses (PIEB) for Maintenance of Labor Analgesia: A Superior Technique to Continuous Epidural Infusion? Turk J Anaesthesiol Reanim. 2017;45:65–6. doi: 10.5152/TJAR.2017.09031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Practice Guidelines for Obstetric Anesthesia: An Updated Report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology. 2016;124:270–300. doi: 10.1097/ALN.0000000000000935. https://doi.org/10.1097/ALN.0000000000000935. [DOI] [PubMed] [Google Scholar]
- 4.Capogna G, Camorcia M, Stirparo S, Farcomeni A. Programmed intermittent epidural bolus versus continuous epidural infusion for labor analgesia: the effects on maternal motor function and labor outcome. A randomized double-blind study in nulliparous women. Anesth Analg. 2011;113:826–31. doi: 10.1213/ANE.0b013e31822827b8. https://doi.org/10.1213/ANE.0b013e31822827b8. [DOI] [PubMed] [Google Scholar]
- 5.Melzack R. The myth of painless childbirth. Pain. 1984;19:321–37. doi: 10.1016/0304-3959(84)90079-4. https://doi.org/10.1016/0304-3959(84)90079-4. [DOI] [PubMed] [Google Scholar]
- 6.Carvalho B, George RB, Cobb B, McKenzie C, Riley ET. Implementation of Programmed Intermittent Epidural Bolus for the Maintenance of Labor Analgesia. Anesth Analg. 2016;123:965–71. doi: 10.1213/ANE.0000000000001407. https://doi.org/10.1213/ANE.0000000000001407. [DOI] [PubMed] [Google Scholar]
- 7.Wong CA, McCarthy RJ, Hewlett B. The effect of manipulation of the programmed intermittent bolus time interval and injection volume on total drug use for labor epidural analgesia: a randomized controlled trial. Anesth Analg. 2011;112:904–11. doi: 10.1213/ANE.0b013e31820e7c2f. https://doi.org/10.1213/ANE.0b013e31820e7c2f. [DOI] [PubMed] [Google Scholar]
- 8.Capogna G, Stirparo S. Techniques for the maintenance of epidural labor analgesia. Curr Opin Anaesthesiol. 2013;26:261–7. doi: 10.1097/ACO.0b013e328360b069. https://doi.org/10.1097/ACO.0b013e328360b069. [DOI] [PubMed] [Google Scholar]
- 9.McKenzie CP, Cobb B, Riley ET, Carvalho B. Programmed intermittent epidural boluses for maintenance of labor analgesia: an impact study. Int J Obstet Anesth. 2016;26:32–8. doi: 10.1016/j.ijoa.2015.11.005. https://doi.org/10.1016/j.ijoa.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Kaynar AM, Shankar KB. Epidural infusion: continuous or bolus? Anesth Analg. 1999;89:534. doi: 10.1097/00000539-199908000-00063. [DOI] [PubMed] [Google Scholar]


