INTRODUCTION
Amblyopia is the most common cause of monocular vision loss in children1 with an estimated prevalence of approximately 2% in the United States.2–4 A developmental disorder of spatial vision, amblyopia is clinically defined as decreased best-corrected visual acuity (VA) in one, or less frequently both eyes, in the absence of any obvious structural anomalies or ocular disease. It is associated with abnormal visual experience, most commonly strabismus, anisometropia, or form deprivation that occurs during a sensitive period of visual development in infancy or early childhood.
Signs, Symptoms, and Quality-of-Life Concerns
In addition to reduced best-corrected VA, there are a plethora of visual function deficits of the amblyopic eye, including abnormal contour interaction,5 reduced contrast sensitivity,6 positional uncertainty,7 spatial distortion,8 poor accommodation,9 abnormal eye movements,10 and suppression.11 Because of good vision in their non-amblyopic (sound) eye, persons with unilateral amblyopia typically do not complain of blurred or poor vision under habitual binocular viewing conditions; however, recent studies have reported reduced reading speed12 and compromised fine-motor skills13 even with both eyes open.
There are important public health consequences when amblyopia is left untreated. Patients with amblyopia are more likely to become visually disabled because of an increased risk of their sound eye becoming visually impaired,14,15 with their estimated lifetime risk of visual impairment being at least 1.2%.15 Vision loss in the sound eye, often caused by trauma, can have a significant effect on quality of life with many employed individuals no longer being able to work because of inadequate visual function.15,16 Although amblyopic eye VA can sometimes improve in adults after vision loss of their sound eye, most remain visually disabled.17 Furthermore, the presence of unilateral amblyopia has a deleterious effect on binocularity, including stereopsis. Because good VA in each eye and/or normal stereoacuity are often prerequisite for careers in the military, aviation, surgery, law enforcement, firefighting, as well as obtaining a commercial driver’s license,18 amblyopic individuals are often precluded from participating in such occupations.19
Historical Perspective on Amblyopia Treatment
Historically, the mainstay of amblyopia treatment has been patching of the sound eye. Treatment regimens have been a matter of individual preference based on the training, observations, and clinical impressions of the treating optometrist or ophthalmologist. Generally, when it came to patching, the adage was “time was of the essence”, so patching was prescribed in conjunction with the refractive correction because of the notion that treatment beyond a certain age (variously stated as between 6 to 9 years) would not be beneficial.20 The-more-the-better-principle was followed by many eye care providers with full-time patching thought to be preferred, if not imperative, for a successful outcome, particularly for severe amblyopia. Atropine penalization was not considered to be a first-line treatment modality and thus generally advocated only for young children with moderate levels of amblyopia who had failed patching.
Amblyopia Treatment Studies
The Pediatric Eye Disease Investigator Group (PEDIG) is a clinical network of pediatric optometrists and ophthalmologists funded by the National Eye Institute to conduct clinical research studies related to pediatric eye conditions. Thus far, the majority of the PEDIG studies have focused on evaluating the comparative effectiveness of different amblyopia treatment regimens for children and adolescents. These studies are known as the Amblyopia Treatment Studies (ATS), and their results have dramatically changed amblyopia clinical practice patterns for many eye care providers. Herein, this article summarizes the key findings from these studies and provide our perspective in regard to the most relevant clinical implications.
RESULTS & CLINICAL IMPLICATIONS
Key features of the ATS studies are:
They are randomized clinical trials (RCT) or prospective observational studies.
The studies of unilateral amblyopia comprise participants with anisometropic, strabismic, or combined-mechanism (anisometropic and strabismic) amblyopia and the bilateral amblyopia study enrolled children with isoametropic amblyopia; children with deprivation amblyopia have been not been studied.
Amblyopic eye VA of 20/40 or worse with an interocular difference of at least 3 lines was required for enrollment for most of the unilateral amblyopia studies.
The primary outcome measure is best-corrected VA of the amblyopic eye, which is measured in a standardized fashion by examiners who are masked to participants’ treatment assignment.
VA is measured using a standardized computerized testing method that presents single-surrounded optotypes at logMAR intervals on the Electronic Visual Acuity (EVA)21 tester using HOTV optotypes for children 3 to 6 years old22 and the Early Treatment Diabetic Retinopathy Study (ETDRS) letters for children 7 years of age and older.23
The magnitude of VA improvement found at the mostly 4- to 6-month primary outcome examinations is not the maximum benefit expected to be achieved for all participants, but instead the maximum length of time that the prescribed treatment regimens could be maintained before investigators would insist on a change of treatment in cases of poor outcome; in many cases, VA can improve further with continued treatment.
RCT results are based on the "prescribed” treatment regimens determined by randomization, not the “actual” treatment completed.
Prescribing Guidelines for Refractive Error Correction
The following prescribing guidelines have been implemented in these studies:
Refractive error determination is based on a cycloplegic refraction using cyclopentolate.
Full correction of astigmatism, myopia, and anisometropia is prescribed with the goal of providing equally clear retinal images.
Hyperopia is either fully corrected (e.g., in cases of esotropia) or undercorrected (e.g., in cases without esotropia) by no more than +1.50 D spherical equivalent (SE), with any reduction in plus sphere reduced symmetrically in the two eyes.
Optical Treatment Studies
1. Optical Correction for Unilateral Amblyopia
Two ATS studies have evaluated the effectiveness of optical correction alone as a treatment modality for previously untreated unilateral amblyopia in 3 to <7 year-old children.24,25 The first study enrolled children with anisometropic amblyopia of 20/40 to 20/25024 and the second study enrolled those with strabismic or combined-mechanism amblyopia of 20/40–20/400,25 with the following key findings:
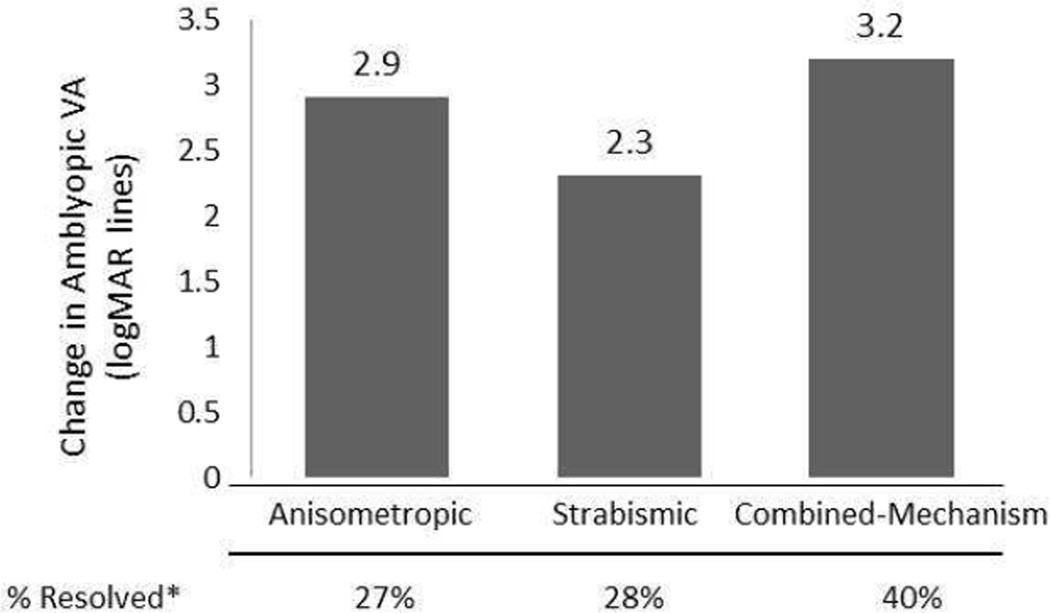
Mean amblyopic eye VA improvement was approximately 3 lines and occurred in both moderate and severe cases of amblyopia (Figure 1).
Resolution of amblyopia, defined as equal VA or amblyopic eye VA within 1 line of sound eye VA, occurred in 25–33% of cases (Figure 1).
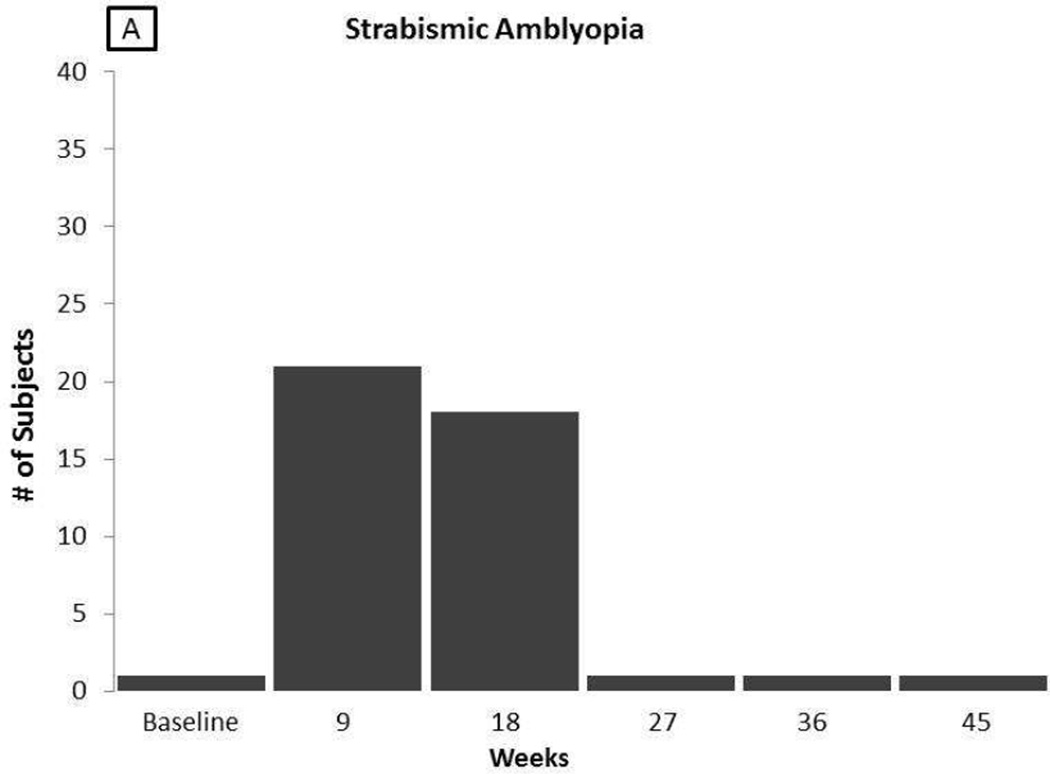
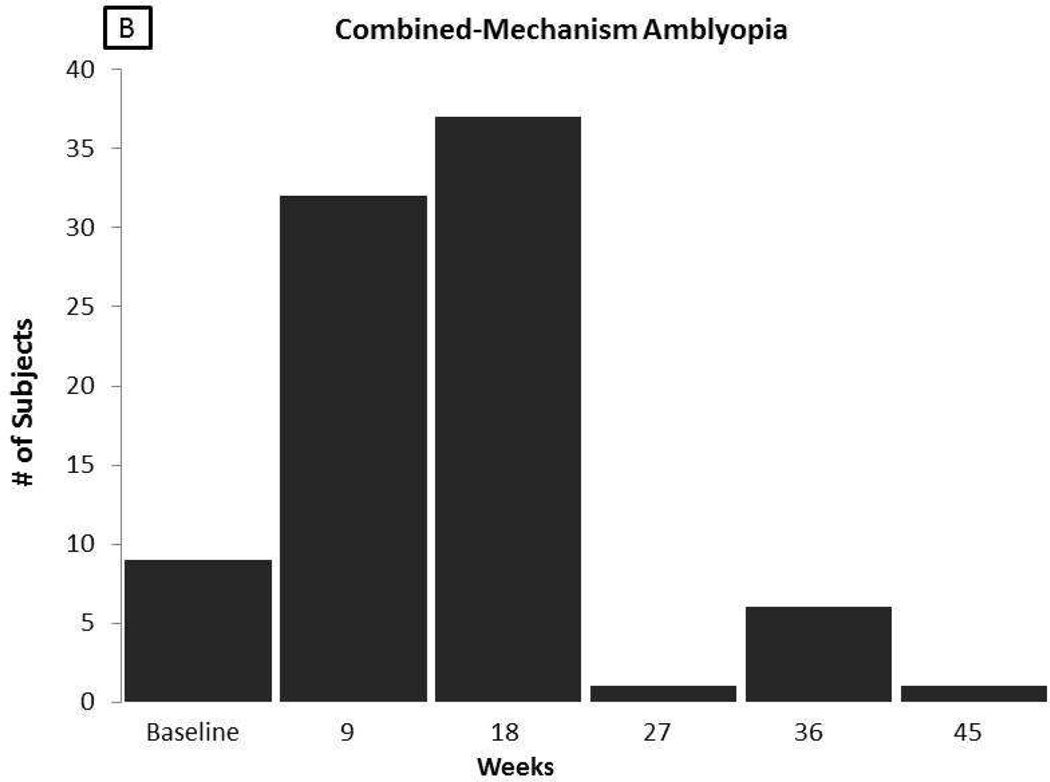
Generally, the optical treatment effect occurred within the first 16 to 18 weeks after optical correction; however, in some children VA continued to improve for up to 45 weeks (Figure 2).
There was no relationship between amblyopic eye VA improvement and the presence or magnitude of strabismus pre- or post-spectacle correction.
Figure 1.
Mean visual acuity improvement and proportion of children reaching resolution of amblyopia with refractive correction based on type of amblyopia.
* Resolved = amblyopic eye VA equal to or within 1 line of sound eye VA
Figure 2.
Time course of maximum VA from optical treatment alone for children with strabismic amblyopia (A) and combined-mechanism amblyopia (B).
Clinical Implications
There is an actual amblyopia treatment effect that occurs over time from solely wearing an appropriate refractive correction that is distinct from the immediate VA gain that occurs initially from eliminating optical blur.
It is reasonable to start amblyopia treatment with the refractive correction alone for young children with anisometropic, strabismic, and combined-mechanism amblyopia.
A follow-up interval of 6 to 8 weeks, until improvement in the amblyopic eye VA plateaus, is a practical schedule for monitoring children for an optical treatment effect.
Children still needing additional amblyopia treatment after improved VA from an optical treatment effect have better amblyopic eye VA at the start of the next treatment phase, which can result in less treatment burden and better compliance.
Some children (i.e., those with amblyopia resolution) may not need additional amblyopia treatment beyond optical correction.
2. Optical Correction for Bilateral Refractive Amblyopia
The PEDIG conducted a prospective observational study to determine the amount and time course of VA improvement with refractive correction alone in 3 to <10-year-old children with previously untreated isoametropic amblyopia of 20/40–20/100 associated with high hyperopia (≥4.00D SE) and/or astigmatism (≥2.00D). The primary outcome measure was binocular VA. The key findings were:26
The mean improvement in binocular VA was approximately 4 lines.
Of the 113 participants, 74% achieved binocular VA of 20/25 or better.
Continued VA improvement was seen for up to 1 year in some children.
The worse the child’s VA at the start of treatment, the greater the number of lines of improvement in VA.
A majority of children also showed an improvement in near stereopsis.
Clinical Implications
The time frame for VA improvement varies but can take up to 1 year; it is possible that additional improvement may occur beyond 1 year (but this was not studied).
Although participants were corrected with spectacles, it is reasonable to expect that similar improvements would occur with contact lens corrections.
Forms of Occlusion
When patients do not respond to refractive correction alone, or VA ceases to improve, occlusion treatment such as part-time patching, atropine penalization, or Bangerter filters may be prescribed.
Patching Dosage
Patching dosage was evaluated in 2 concurrent clinical trials of children 3 to <7 years of age. The effectiveness of 2 hours of daily patching was compared to 6 hours of daily patching in children with moderate amblyopia of 20/40 to 20/8027 and 6 hours of daily patching was compared to full-time daily patching in children with severe amblyopia of 20/100 to 20/400.28 The key findings were:
In cases of moderate amblyopia, prescribing 2 hours of daily patching with 1 hour of near activities is as effective as prescribing 6 hours of daily patching with 1 hour of near activities (Table 1).
In cases of severe amblyopia, prescribing 6 hours of daily patching and 1 hour of near activities is as effective as prescribing full-time daily occlusion and 1 hour of near activities (Table 1).
There was no difference in the rate of improvement between the groups randomized to the lower and higher patching dosages.
Table 1.
Mean visual acuity (VA) improvement by prescribed treatment in moderate and severe amblyopia in 3 to <7 years in old children.
| Depth of Amblyopia | Prescribed Treatment | Mean VA Improvementa (logMAR lines) |
Post-Treatment Mean VA |
≥ 2 Lines of Improvement from Baseline (%) |
|---|---|---|---|---|
| Moderate Amblyopia | 2 hours patching | 2.4 | 20/32 | 79 |
| 6 hours patching | 2.4 | 20/32−1 | 76 | |
| Severe Amblyopia | 6 hours patching | 4.8 | 20/50 | 93 |
| Full-time patching | 4.7 | 20/50−2 | 85 | |
| Moderate Amblyopia | ≥ 6 hours patching | 3.16 | 20/30 | 87 |
| Daily atropine | 2.84 | 20/30−2 | 82 | |
At the primary outcome visit; does not indicate maximum improvement achieved
It is noteworthy that in a subsequent clinical trial, there were children with severe amblyopia who responded to 2 hours of patching.29
Clinical Implications
Full-time patching is not always needed for a successful treatment outcome. Prescribing lesser amounts of patching may promote better overall compliance with treatment.
When patching is prescribed, it is reasonable to prescribe 2 hours of daily patching for moderate amblyopia and 6 hours of daily patching for severe amblyopia.
Some children with severe amblyopia will respond to as little as 2 hours of patching.
In young children, using an adhesive patch should be strongly considered so that peeking is less likely to occur.
Atropine Treatment
Another amblyopia treatment modality is pharmacological penalization by the instillation of the long-acting topical cycloplegic agent, atropine sulfate (1%), into the sound eye of a child with amblyopia. The resultant cycloplegia prevents accommodation in the sound eye resulting in blurred vision at near, and in instances when the full hyperopic correction is not worn, blurred vision at distance as well.
1. Atropine vs. Patching for Moderate Amblyopia
The first ATS30 compared the effectiveness of daily administration of 1 drop of 1% atropine in the sound eye to ≥ 6 hours of daily patching in children 3 to <7 years old with moderate amblyopia of 20/40 to 20/100 and found the following:
Both treatment groups showed a similar improvement in amblyopic eye VA (Table 1).
VA improvement was slower with atropine penalization compared to patching, but the magnitude of VA improvement at 6 months was similar.
Treatment effect did not differ by age, cause of amblyopia, or depth of amblyopia.
A switch in near fixation preference from the atropinized sound eye to the amblyopic eye was not observed in a number of children with significant amblyopic eye VA improvement.31
Both treatments were well tolerated with parents reporting a slightly higher degree of acceptability with atropine treatment.
2. Atropine Regimens for Moderate Amblyopia
A subsequent RCT compared less frequent administration of 1% atropine drops (weekend only) to daily atropine in children 3 to <7 years old with moderate amblyopia of 20/40 to 20/80 and found the following:32
Amblyopic eye VA improvement was essentially identical (2.3 lines) in both groups at 4 months.
Among participants, 80% reached their maximum VA improvement by 4 months, but some continued to show VA improvement for up to 10 months.
Among participants, 50% had resolution of amblyopia (i.e., equal VA or amblyopic eye VA within 1 line of sound eye VA).
3. Atropine Augmentation with a Plano Lens for the Sound Eye
The PEDIG evaluated whether there was an additional treatment effect by augmenting weekend atropine with a plano lens for the sound eye in children aged 3 to < 7 years with moderate amblyopia of 20/40 to 20/100.33 Because all participants had hyperopic refractive error in their sound eye, those randomized to the atropine plus plano lens group had blurred distance vision in addition to increased blur at near. The key findings were as follow:
There was no difference in mean amblyopic eye VA improvement between the two groups at 18 weeks; mean improvement was approximately 2.5 lines.
More children in the atropine with plano lens group reached 20/25 or better amblyopic eye VA than those in the atropine only group (40% vs. 29%, respectively).
4. Atropine for Severe Amblyopia
Historically, atropine penalization has been reserved for children with moderate amblyopia, because, presumably, treatment would not be effective if sound eye VA was not worse than amblyopic eye VA. Nevertheless, PEDIG RCTs included children with severe amblyopia of 20/125 to 20/400 who were treated with weekend atropine.33–35 While the studies were not powered to compare treatment groups, the following noteworthy results were observed:
In children 3 to <7 years, the average VA improvement was 4.5 to 5.1 lines.
In children 7 to 12 years, VA improved by 1.5 lines with prescribed weekend atropine.
5. Miscellaneous Issues with Atropine Treatment for Amblyopia
Reverse Amblyopia
Although a few children had reduced sound eye VA at follow-up visits, there were no cases of persistent reverse amblyopia after discontinuation of atropine.33,35 Initially apparent reverse amblyopia was suspected in some children, but it was then determined that sound eye VA had not been assessed through the full hyperopic correction. Because atropine can uncover additional hyperopia than found on a cyclopentolate refraction, it is important to determine if uncorrected hyperopia is present in the atropinized eye, and if so, to measure sound eye VA through the full plus prescription at follow-up visits.
Systemic Side Effects
Systemic side effects (dryness, flushing of skin, fever, confusion, unusual behavior, and irritability) that can be associated with atropine penalization rarely occurred.30,32,33 However, when such cases occur, daily instillation of 5% homatropine eye drops can be substituted for atropine.
Clinical Implications
Atropine penalization has a similar treatment effect as 2 and 6 hours of prescribed patching; thus, it can be considered for first-line amblyopia treatment or for patching failures.
Daily atropine administration is not necessary; a twice-per-week schedule is also effective. There is no reason to believe that atropine needs to be administered only on weekend days or that the days need to be sequential.
Weekend atropine penalization has been shown to be effective in treating both moderate and severe amblyopia.
Retinoscopy should be performed over the current refractive correction of the sound eye for children on atropine to determine if there is residual uncorrected hyperopia that should be corrected before measuring sound eye VA.
Parent education regarding atropine penalization for the amblyopia treatment is listed in [Table 2].
Table 2.
Parent education regarding atropine penalization for the treatment amblyopia
| Drop Administration | Administer in morning; if problematic, instill drop before child wakes |
| Sun Protection / Comfort | Wear brimmed hat and sunglasses when outside, particularly if sunny |
| Storage | Store securely out of reach of children |
| Systemic Reaction | Discontinue and call if facial flushing, fever, dry mouth, irritability, or confusion |
| Other Health Care Visits | Inform of atropine use at office visits, particularly if at emergency room |
Bangerter Filter Treatment
A Bangerter filter (Ryser Optik AG, St. Gallen, Switzerland) is a translucent filter that is applied to the sound eye’s spectacle lens for full-time wear for amblyopia treatment. There are different density filters, which produce different degrees of image defocus that degrade sound eye VA to predictable levels. An RCT to evaluate the effectiveness of Bangerter filters in in children 3 to <10 years with moderate amblyopia (20/40 to 20/80) found the following:36
Full-time wear of Bangerter filter provided VA improvement (1.8 lines) similar to 2 hours of daily patching (2.3 lines).
Parents reported fewer adverse effects and better compliance with the Bangerter filters than with patching.
Clinical Implications
Bangerter filters can be considered for first-line amblyopia treatment or for patients who do not comply with patching or atropine treatment.
- Potential advantages of Bangerter filters are the following:
-
◦The ability to change the density of the filter to modulate the degree of degradation.
-
◦The possibility of better compliance because the filter is not readily apparent to casual observers.
-
◦The filter may be less disruptive to binocular vision than patching, albeit 2 to 4 hours of part-time patching should not be very disruptive to binocular vision.
-
◦
- Potential disadvantages of Bangerter filters are the following:
-
◦Peeking around the filters is relatively easy.
-
◦Filters may not uniformly degrade VA to the predicted level reported by manufacturer.37
-
◦
Clinicians should consider changing the filters periodically because the amount of degradation with filters tends to decrease over time.37
Treatment of Older Children with Amblyopia
Historically, there has been little consensus on the effectiveness of amblyopia treatment in older children, with many eye care professionals believing that amblyopia treatment was ineffective after some upper age limit (e.g., 6–7 years or 9 or 10 years), that any VA improvements were likely to be lost after the cessation of treatment, and that intractable diplopia was of concern.
1. Do Older Children with Amblyopia Respond to Treatment?
In an RCT investigating the effectiveness of amblyopia treatment in 2 cohorts of children (7–12 years and 13–17 years) with amblyopia of 20/40–20/400,38 participants were randomized to optical correction alone (control group) or optical correction augmented with 2 to 6 hours of daily patching, 1 hour of near activities when patched, and 1% daily atropine in the 7–12 year cohort. The primary outcome was the proportion of treatment “responders,” which was defined as ≥ 2 lines improvement in amblyopic eye VA. Data were analyzed separately for the two age groups.
In children aged 7–12 years, 53% in the augmented treatment group showed a treatment response compared to 25% in the control group.
In children aged 13–17 years, there was no difference in the proportion of children in the 2 treatment groups who met the responder criteria (25% and 23%, in the augmented and control groups, respectively).
In children aged 13–17 years who had not been previously treated for amblyopia, the outcome was essentially the same as that found in children aged 7–12 years (47% in the augmented group versus 20% in the control group).
No patients developed intractable diplopia.
2. Single Treatment Modality
Given that 7 to 12-year-old children prescribed a combined treatment regimen of daily part-time patching and 1% atropine responded to treatment, the PEDIG subsequently compared the effectiveness of 2 hours of daily patching versus weekend administration of 1% atropine in children of this age with amblyopia of 20/40–20/100 and found the following:34
Mean VA improvement was essentially the same (approximately 1.5 lines) in both groups after 17 weeks of treatment.
Children who showed improvement in amblyopic VA at the 17-week follow-up visit were monitored until reaching maximal VA improvement, which was a mean of 2.2 lines in both groups.
Clinical Implications
Amblyopia can be successfully treated in 7 to 12 year-old children using either 2 hours of daily patching or weekend atropine as the initial treatment.
Although many older children respond to treatment, a meta-analysis of 4 PEDIG RCTs showed that amblyopia is more responsive to treatment in children younger than 7 years of age compared with children 7 to 12 years of age.39
Among children in the optical correction alone group, 25% showed ≥ 2 lines of VA improvement: thus, the optical treatment effect from simply wearing the refractive correction is not limited to younger children.
The authors think that it is unlikely that the difference in treatment response between children 7 to 12 and 13 to 17 years was because of a difference in visual plasticity. The authors hypothesize that the lesser treatment effect in children 13 to 17 years might be because it was more difficult for them to comply with 2 to 6 hours of daily patching with their overscheduled lives and/or they were not prescribed atropine.
There was significant individual variability in treatment response, with some 13 to 17-year-old children showing significant improvement with treatment, even with a history of prior treatment. Therefore, the authors think that one should not withhold treatment from children aged 13 to 17 years, even with a history of prior treatment.
Residual Amblyopia
Because many children have residual amblyopia after treatment, the PEDIG has evaluated several treatment approaches for residual amblyopia.
Younger Children (3 to <8 years)
1. Increasing Patching Dosage
The key findings from an RCT evaluating the effectiveness of increasing patching from 2 hours to 6 hours in children 3 to <8 years old who were originally treated with 2 hours of daily patching for at least 12 weeks, but still had stable residual amblyopia (20/32–20/160) were as follows:40
Mean VA improvement at 10 weeks was 1.2 lines in the group that increased patching from 2 hours to 6 hours and 0.5 lines in the group that continued with 2 hours of patching.
Among children in the increased patching dosage group, 40% showed at least 2 lines of VA improvement compared to 18% in the group who were to continue with patching for 2 hours.
2. Adding a Plano Lens to Atropine Treatment
In an RCT to evaluate the effectiveness of adding a plano lens to atropine treatment for 3 to <8-year-old children with stable residual amblyopia (20/32 to 20/63), children were randomly assigned to treatment with weekend atropine with or without a plano lens over the sound eye.41 The main findings were as follows:
Mean VA improvement was 1.1 lines in the atropine with plano lens group and 0.6 line in the atropine only group at 10 weeks.
Although there may be a small benefit from augmenting atropine therapy with a plano lens over the fellow eye, the study results are not definitive because the difference in amblyopic eye VA improvement between the two groups was not statistically significant and the confidence interval was large.41
3. Combining Patching and Atropine Treatments
The PEDIG evaluated whether an intensive final push with combined patching and atropine could improve VA in children 3 to <10 years with residual amblyopia of 20/32 to 20/63 after 12 weeks of treatment with 6 hours of daily patching or daily atropine.42 Children were randomized to either an intensive combined treatment group (6 hours of daily patching combined with daily atropine) or a control group in whom treatment was weaned (i.e., daily patching reduced from 6 hours to 2 hours or daily atropine reduced to once-weekly atropine for 4 weeks, followed by no treatment other than spectacles alone).
Mean VA improvement was 0.5 lines in both groups after 10 weeks.
Clinical Implications
If an amblyopic patient does not respond fully to the prescribed treatment, verify compliance with treatment and consider repeating the cycloplegic refraction and re-examining the ocular structures to ensure there is no residual uncorrected refractive error or subtle ocular pathology present.
When amblyopic eye VA stops improving with 2 hours of daily patching, increasing the patching dosage to 6 hours is a reasonable next approach.
When amblyopic eye VA stops improving with weekend atropine, adding a plano lens over the sound eye may result in further improvement.
Combined treatment of patching and atropine did not seem to further improve VA in those with residual amblyopia; however, these results should not be generalized to children with more severe residual amblyopia or those who have stopped improving after less intense treatment.
In cases of residual amblyopia, changing the treatment modality (e.g., changing patching to atropine or changing atropine to patching) can be considered. Alternatively, active vision therapy procedures can be prescribed to improve deficiencies in accommodation, form discrimination, fixation, as well as to eliminate suppression.43–45 Although there are no controlled trials that have evaluated these treatment approaches for residual amblyopia, the PEDIG is currently conducting an RCT that includes children with residual amblyopia to evaluate the effectiveness of a type of binocular anti-suppression treatment on an iPad.46
Older Children (7 to 12 years)
Treatment of Residual Amblyopia with Oral Levadopa
Because levodopa, an oral medication used to supplement dopamine deficiency in adults with Parkinson’s disease and children with dopamine-response dystonia, had been used by some clinicians for amblyopia treatment, the PEDIG conducted a RTC in children 7 to 12 years old with residual amblyopia of 20/50 to 20/400 after patching treatment to assess levodopa’s efficacy and short-term safety as an adjunctive treatment to patching. Children were randomized to oral levodopa or placebo administered 3 times daily with patching prescribed for 2 hours per day. The key findings were as follows:
There was no clinically or statistically meaningful improvement in VA from adding oral levodopa to patching compared with placebo and patching.
Clinical Implication
There is no meaningful benefit from adding oral levodopa to part-time patching for the treatment of residual amblyopia.
Recurrence of Amblyopia
Amblyopia that is successfully treated can reoccur once treatment is discontinued, particularly if the amblyogenic factor is still present. Amblyopia recurrence rate was evaluated in children 3 to <8 years old47 and children 7 to <13 years old48 in two separate studies. Recurrence was defined as a loss of ≥2 lines of VA in the amblyopic eye.
In children 3 to <8 years who had been successfully treated with patching or atropine:
Approximately 25% experienced a recurrence during the first year off treatment.
The risk of recurrence was similar for amblyopia treated with patching and atropine.
Most recurrences occurred within 3 months after the cessation of treatment.
The recurrence rate was 3 times greater in children who had 6 to 8 hours of patching that was stopped abruptly than in children who had 6 to 8 hours of patching that was tapered to 2 hours prior to cessation or for children who initially had been prescribed 2 hours of patching without weaning.
In children 7 to 12 years of age who responded to a treatment regimen of 2 to 6 hours of patching, atropine, and near activities:
Only 7% of children experienced a recurrence during the first year off treatment.
Clinical Implications
Because a majority of recurrences in children <8 years old occur within 3 months after the cessation of treatment, early follow-up is critical.
Patching dosage should be gradually tapered rather than abruptly terminated in young children who initially patch ≥6 hours per day.
Amblyopia recurrence is less common in older children than in younger children.
Long Term Follow-Up
A follow-up study that included a proportion of participants from the original ATS trial that compared atropine vs. patching for treatment of moderate amblyopia was conducted to evaluate the durability of treatment benefit found the following:
The mean amblyopic eye VA after 6 months of treatment at study outcome was approximately 20/32 in both groups; approximately 25% of participants underwent additional treatment using the alternative treatment (atropine switching to patching, or vice versa) during the following 2 years.49
At age 15 years, mean amblyopic VA was approximately 20/25 and 60% of children had 20/25 or better in their amblyopic eyes. VA at 15 years was similar between the two original treatment groups.50
Clinical Implications
VA improvements occurring with amblyopia treatment before 7 years of age are typically maintained until at least 15 years of age (but it is wise to monitor for regression).
Mild residual amblyopia is common.
Role of Near Activities
In many of the RCTs discussed previously, 1 hour of near activities were prescribed to be done during patching based on the clinical assumption that these activities stimulate the visual system and enhance amblyopia outcomes. Subsequently, an RCT was conducted where children 3 to <7 years old with amblyopia of 20/40–20/400 were randomized to 2 hours of daily patching with near activities (e.g., crafts, reading, writing, computer or video games) or 2 hours of daily patching with far activities (e.g., watching TV, outdoor play),29 with the following main result:
There was no difference in treatment effect based on whether near or far activities were prescribed.
Clinical Implication
The activities prescribed to be performed at near in this RCT were “common” near activities. More highly structured vision therapy activities and, specifically aimed at improving accommodation, form discrimination, and fixation, and for eliminating suppression were not evaluated.43–45 The degree of effectiveness of active vision therapy procedures has not yet been evaluated in an RCT.
Amblyopia iNet (http://www.visiontherapysolutions.net/ambp.php), a software-based system of amblyopia therapy for home use, has visual activities (e.g., form discrimination and eye movements) that can be performed using the amblyopic eye only or under “monocular fixation in binocular field” (MFBF) conditions to address suppression.44 Monocular perceptual learning activities that are performed at near have shown good promise as an adjunct to traditional amblyopia treatment.51 Neither of these treatment approaches, however, has been examined critically in a carefully controlled trial.
CONCLUSIONS
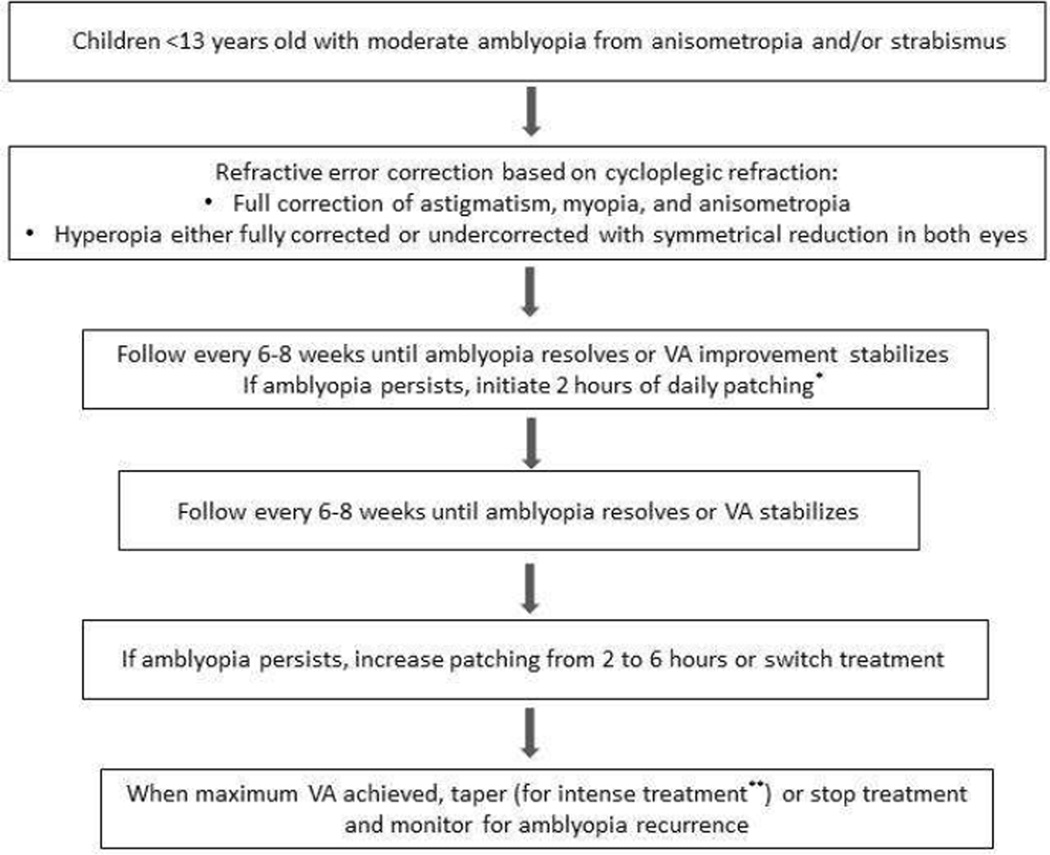
The results from the PEDIG studies, discussed previously, have dramatically changed the amblyopia treatment landscape. Many long-held beliefs regarding amblyopia treatment, which were based primarily on observations and clinical impressions, did not stand the test of time once evaluated in a rigorous manner. Table 3 provides an overview of long-held amblyopia treatment dogma that has been challenged and mostly supplanted by the ATS results reported herein. Figure 3 shows an evidence-based sequential treatment approach for moderate amblyopia in young children that is based on the results of these PEDIG studies.
Table 3.
Amblyopia treatment approaches: Historical versus current evidence-based approach
| Historical Dogma | Current Perspective | |
|---|---|---|
| The mainstay of amblyopia treatment |
Patching | Optimal refractive correction |
| Timing of refractive correction and occlusion (patching or atropine) |
Simultaneous | Occlusion prescribed subsequent to gains from optical treatment effect |
| Patching dosage for moderate amblyopia |
Generally, the more the better; usually ≥ 5–6 hours |
Start with 2 hours; can increase dosage if needed |
| Patching dosage for severe amblyopia |
Full-time or most waking hours | Start with 6 hours; 2 hours is effective in some cases |
| Atropine penalization use | Patching failures only | First-line treatment as alternative to patching or for patching failures |
| Atropine penalization guidelines | ||
| Amblyopia severity | Only for moderate amblyopia | Both moderate & severe cases |
| Age of child | Only in young children | Younger and older children |
| Age after which amblyopia can no longer be treated |
Approximately 6–9 years of age | Upper age limit not established; albeit generally greater VA gains if <7 years of age |
| Recurrence of amblyopia after treatment cessation in 9 to <13- year-old children |
High likelihood of regression | Vast majority (>90%) do not regress |
Figure 3.
Recommended evidence-based approach to treating moderate amblyopia in children <13 years of age.
*Alternative treatments include atropine penalization of the sound eye 2 times per week or full-time wear of a Bangerter filter over the sound eye.
**Intense treatment is ≥ 6 hours of daily patching
The PEDIG studies to date have principally addressed monocular approaches to amblyopia treatment. Recently there has been an increased interest in evaluating treatments that are designed to decrease suppression and enhance binocularity.52–54 The PEDIG is currently conducting a RCT comparing this type of binocular treatment administered daily on an iPad versus 2 hours of daily patching in children 5 to <17 years.51 There are a number of other amblyopia treatment modalities currently under investigation and the authors are hopeful that 10 years from now, they will be writing a paper discussing amblyopia treatment regimens that are even more effective than those that exist at present.
SYNOPSIS.
A series of randomized clinical trials and prospective observation studies, the Amblyopia Treatment Studies (ATS), have recently been conducted by the Pediatric Eye Disease Investigator Group (PEDIG) to provide an evidence base for treating childhood amblyopia. Herein, we review the major findings and clinical implications from these studies that have addressed important amblyopia treatment issues, such as optical treatment, patching dosage, atropine penalization, treatment of older children, and residual amblyopia.
Acknowledgments
We would like to acknowledge the National Eye Institute for funding the studies through the PEDIG network (EY011751, EY018810), and also acknowledge the dedication of the Jaeb Coordinating Center (Tampa, Florida) staff and participating PEDIG investigators and coordinators. We also acknowledge that the aforementioned PEDIG studies are not the only rigorous large-scale studies that have been conducted in recent years; however, the scope of this manuscript was limited to PEDIG studies. The interpretation of the data presented herein are solely our own and do not represent those of the PEDIG, the National Eye Institute, Marshall B. Ketchum University, or any other professional organization to which we belong.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Angela M. Chen, Southern California College of Optometry at Marshall B. Ketchum University, 2575 Yorba Linda Blvd. Fullerton, CA 92831, angelachen@ketchum.edu, Phone number: (714) 449-7432.
Susan A. Cotter, Southern California College of Optometry at Marshall B. Ketchum University, 2575 Yorba Linda Blvd. Fullerton, CA 92831, scotter@ketchum.edu, Phone number: (714) 449-7488.
References
- 1.Ederer F, Krueger DE. Report on the National Eye Institute's Visual Acuity Impairment Survey pilot study. Washington, DC: National Eye Institute; 1984. pp. 81–84. [Google Scholar]
- 2.McKean-Cowdin R, Cotter S, Tarczy-Hornoch K, et al. Prevalence of amblyopia or strabismus in Asian and non-Hispanic white preschool children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013;120:2117–2124. doi: 10.1016/j.ophtha.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months the multi-ethnic pediatric eye disease study. Ophthalmology. 2008;115:1229–1236. e1. doi: 10.1016/j.ophtha.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Friedman DS, Repka MX, Katz J, et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:2128–2134. e1–e2. doi: 10.1016/j.ophtha.2009.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simmers AJ, Gray LS, McGraw PV, Winn B. Contour interaction for high and low contrast optotypes in normal and amblyopic observers. Ophthal Physiol Opt. 1999;19:253–260. [PubMed] [Google Scholar]
- 6.McKee S, Levi D, Movshon J. The pattern of visual deficits in amblyopia. J Vis. 2003;25:1445–1457. doi: 10.1167/3.5.5. [DOI] [PubMed] [Google Scholar]
- 7.Fronius M, Sireteanu R, Zubcov A, Buttner A. Preliminary report: Monocular spatial localization in children with strabismic amblyopia. Strabismus. 2000;8:243–249. doi: 10.1076/stra.8.4.243.683. [DOI] [PubMed] [Google Scholar]
- 8.Bedell HE, Flom MC. Monocular spatial distortion in strabismic amblyopia. Invest Ophthalmol Vis Sci. 1981;20:263–268. [PubMed] [Google Scholar]
- 9.Manh V, Chen A, Tarczy-Hornoch K, et al. Accommodative performance of children with unilateral amblyopia. Invest Ophthalmol Vis Sci. 2015;56:1193–1207. doi: 10.1167/iovs.14-14948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Regan D, Giaschi D, Kraft SP, Kothe AC. Method for identifying amblyopes whose reduced line acuity is caused by defective selection and/or control of gaze. Ophthal Physiol Opt. 1992;12:425. [PubMed] [Google Scholar]
- 11.Narasimhan S, Harrison E, Giaschi D. Quantitative measurement of interocular suppression in children with amblyopia. Vision Res. 2012;66:1–10. doi: 10.1016/j.visres.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Stifter E, Burggasser G, Hirmann E, Thaler A, Radner W. Monocular and binocular reading performance in children with microstrabismic amblyopia. Br J Opthalmol. 2005;89:1324–1329. doi: 10.1136/bjo.2005.066688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Connor A, Birch E, Anderson S, Draper H. Monocular and binocular reading performance in children with microstrabismic amblyopia. Optom Vis Sci. 2010;87:942–947. doi: 10.1097/OPX.0b013e3181fd132e. [DOI] [PubMed] [Google Scholar]
- 14.Tommilla V, Tarkkanen A. Incidence of loss of vision in the healthy eye in amblyopia. Br J Ophthalmol. 1981;65:575–577. doi: 10.1136/bjo.65.8.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rahi JS, Logan S, Timms C, et al. Risk, causes and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population based study. Lancet. 2002;360:597–602. doi: 10.1016/s0140-6736(02)09782-9. [DOI] [PubMed] [Google Scholar]
- 16.Chua B, Mitchell P. Consequences of amblyopia on education, occupation, and long term vision loss. Br J Ophthalmol. 2004;88:1119–1121. doi: 10.1136/bjo.2004.041863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rahi JS, Logan S, Boria MC, et al. Prediction of improved vision in the amblyopic eye after visual loss in the non-amblyopic eye. Lancet. 2002;360:621–622. doi: 10.1016/S0140-6736(02)09775-1. [DOI] [PubMed] [Google Scholar]
- 18.Qualifications of drivers and longer combination vehicle (LCV) driver instrutors. [Accessed January 6, 2016]; at https://www.fmcsa.dot.gov/regulations/title49/section/391.43.
- 19.Adams G, Karas M. Effect of amblyopia on employment prospects. Br J Ophthalmol. 1999;83:380. doi: 10.1136/bjo.83.3.378c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flynn JT, Schiffman J, Feuer W, Corona A. The therapy of amblyopia: an analysis of the results of amblyopia therapy utilizing the pooled data of published studies. Trans Am Ophthalmol Soc. 1998;96:431–453. [PMC free article] [PubMed] [Google Scholar]
- 21.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–909. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 22.Holmes JM, Beck RW, Repka MX, et al. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–1353. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 23.Cotter SA, Chu RH, Chandler DL, et al. Reliability of the Electronic Early Treatment Diabetic Retinopathy Study testing protocol in children 7 to <13 years old. Am J Ophthalmol. 2003;136:655–661. doi: 10.1016/s0002-9394(03)00388-x. [DOI] [PubMed] [Google Scholar]
- 24.Pediatric Eye Disease Investigator Group. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006;113:895–903. doi: 10.1016/j.ophtha.2006.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Writing Committee for the Pediatric Eye Disease Investigator Group. Cotter S, Foster N, et al. Optical treatment of strabismic and combined strabismic-anisometropic amblyopia. Ophthalmology. 2012;119:150–158. doi: 10.1016/j.ophtha.2011.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pediatric Eye Disease Investigator Group. Treatment of bilateral refractive amblyopia in children three to less than 10 years of age. Am J Ophthalmol. 2007;144:487–496. doi: 10.1016/j.ajo.2007.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–611. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 28.Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110:2075–2087. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Pediatric Eye Disease Investigator Group. A randomized trial of near versus distance activities while patching for amblyopia in children aged 3 to less than 7 years. Ophthalmology. 2008;115:2071–2078. doi: 10.1016/j.ophtha.2008.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–278. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 31.Pediatric Eye Disease Investigator Group. The course of moderate amblyopia treated with atropine in children: experience of the Amblyopia Treatment Study. Am J Ophthalmol. 2003;136:630–639. doi: 10.1016/s0002-9394(03)00458-6. [DOI] [PubMed] [Google Scholar]
- 32.Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–2085. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 33.Pediatric Eye Disease Investigator Group. Pharmacological plus optical penalization treatment for amblyopia: results of a randomized trial. Arch Ophthalmol. 2009;127:22–30. doi: 10.1001/archophthalmol.2008.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pediatric Eye Disease Investigator Group. Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Arch Ophthalmol. 2008;126:1634–1642. doi: 10.1001/archophthalmol.2008.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Repka MX, Kraker RT, Beck RW, et al. Treatment of severe amblyopia with weekend atropine: results from 2 randomized clinical trials. J AAPOS. 2009;13:258–263. doi: 10.1016/j.jaapos.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pediatric Eye Disease Investigator Group Writing Committee. A randomized trial comparing Bangerter Filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010;117:998–1004. doi: 10.1016/j.ophtha.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rutstein RP, Foster NC, Cotter SA, et al. Visual acuity through Bangerter filters in nonamblyopic eyes. J AAPOS. 2011;15:131–134. doi: 10.1016/j.jaapos.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123:437–447. doi: 10.1001/archopht.123.4.437. [DOI] [PubMed] [Google Scholar]
- 39.Holmes J, Lazar E, Melia B, et al. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol. 2011;129:1451–1457. doi: 10.1001/archophthalmol.2011.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pediatric Eye Disease Investigator Group. Wallace DK, Lazar EL, et al. A randomized trial of increased patching for amblyopia. Ophthalmology. 2013;120:2270S–2277S. doi: 10.1016/j.ophtha.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pediatric Eye Disease Investigator Group. Wallace DK, Lazar EL, et al. A randomized trial of adding a plano lens to atropine for amblyopia. J AAPOS. 2015;19:42–48. doi: 10.1016/j.jaapos.2014.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pediatric Eye Disease Investigator Group. Wallace DK, Kraker RT, et al. Randomized trial to evaluate combined patching and atropine for residual amblyopia. Arch Ophthalmol. 2011;129:960–962. doi: 10.1001/archophthalmol.2011.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garzia RP. Efficacy of vision therapy in amblyopia: a literature review. Am J Optometry Physiological Optics. 1987;64:399–404. doi: 10.1097/00006324-198706000-00003. [DOI] [PubMed] [Google Scholar]
- 44.Cohen AH. Monocular fixation in a binocular field. J Am Optom Assoc. 1981;52:801–806. [PubMed] [Google Scholar]
- 45.Frantz K. Rationale for refractive correction, occlusion, activie therapy for amblyopia treatment. Journal of Behavioral Optometry. 1995;6:14, 8–9. [Google Scholar]
- 46.Study of binocular computer activities for treatment of amblyopia (ATS18) [Accessed January 22, 2016]; at https://clinicaltrials.gov/ct2/show/NCT02200211?term=ATS18&rank=1.
- 47.Pediatric Eye Disease Investigator Group. Risk of amblyopia recurrence after cessation of treatment. J AAPOS. 2004;8:420–428. doi: 10.1016/S1091853104001612. [DOI] [PubMed] [Google Scholar]
- 48.Pediatric Eye Disease Investigator Group. Stability of visual acuity improvement following discontinuation of amblyopia treatment in children aged 7 to 12 years. Arch Ophthalmol. 2007;125:655–659. doi: 10.1001/archopht.125.5.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia: follow-up at age 10 years. Arch Ophthalmol. 2008;126:1039–1044. doi: 10.1001/archopht.126.8.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rekpa M, Kraker R, Holmes J, et al. Atropine vs. patching for treatment of moderate amblyopia: follow-up at 15 years of a randomized clinical trial. JAMA Ophthalmol. 2014;132:799–805. doi: 10.1001/jamaophthalmol.2014.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Levi D, Li R. Improving the performance of the amblyopic visual system. Philosophical Transactions of the Royal Society. 2009;364:399–407. doi: 10.1098/rstb.2008.0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hess RF, Thompson B, Black JM, et al. An iPod treatment of amblyopia: an updated binocular approach. Optometry. 2012;83:87–94. [PubMed] [Google Scholar]
- 53.Birch E, Li S, Jost R, et al. Binocular iPad treatment for amblyopia in preschool children. J AAPOS. 2015;19:6–11. doi: 10.1016/j.jaapos.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li S, Reynaud A, Hess R, et al. Dichoptic movie viewing treats childhood amblyopia. J AAPOS. 2015;19:401–405. doi: 10.1016/j.jaapos.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]