Abstract
Objectives
To evaluate mechanically superior method of pilon fracture fixation by comparing axial stiffness between anterolateral and medial tibial locking plates in a cadaveric fracture model.
Methods
Eight matched pairs of fresh frozen cadaver specimens (lower limb after through-knee disarticulation) were used to eliminate confounder of bone quality. Simulated pilon fractures were created so that each pair represented either varus or valgus fracture pattern (AO 43-A2) with associated fibular fractures (transverse or comminuted). Specimens were plated with DePuy anterolateral or medial locking plate and axial load applied, measuring displacement at the fracture site. Each lower extremity was tested with a fracture wedge in place and removed to mimic comminution. Average force at which failure occurred was compared between the two fixation methods, for varus and valgus fracture pattern respectively, with the use of a Mann-Whitney U test.
Results
On average, medial plate fixation of varus fractures resulted in 2.27 times (range of 1.6–3.9) greater load prior to failure as compared to anterolateral plate. Similarly, valgus simulated fractures tolerated 1.6 times (range 1.12–2.34) higher force prior to failure if anterolateral plate was applied versus medial plate. Analysis utilizing the Mann-Whitney U test for fracture patterns vs plate configuration approached statistical significance (p = 0.081 varus failure and p = 0.386 valgus failure).
Conclusions
Lateral plate fixation is biomechanically superior for pilon fractures resulting from valgus force as evident by comminuted fibular fracture. Similarly, medial plate location resulted in improved stiffness in compression for varus type fractures, evident by transverse fibular fracture. We approached statistical significance, however our lack of power regarding adequate sample size is an issue that is consistent with other biomechanical studies in this area.
Keywords: Pilon, Distal tibia, Distal tibia plate location, Fracture pattern
1. Introduction
Pilon fracture is a fracture that occurs as a result of high energy axial loading in which talus impacts the distal part of the tibia. This fracture was first described in 1911 by Desot, and to this day, these fractures are not common accounting for <10% of all fractures of the lower extremity.1, 2 Since its description, there have been numerous advancements in treatment methods, most notably appreciation for the role of soft tissues in fracture healing.3, 4 Better understanding of the role of soft tissues in fracture healing, has led to the development of minimally invasive plating techniques and low profile contoured plates. Similarly, evaluation of soft tissue envelope became one of the major determinants for surgical approach, together with fracture pattern and surgeon’s preference.1
Historically, medial approach to the distal tibia has been utilized for the majority of tibial pilon fractures due to ease of exposure and extensive visualization.1 However, concerns for anteromedial skin flap and desire for improved soft tissue coverage, led to the development of lateral operative approach with the placement of an anterolateral plate.5 Recent reports even propose use of the same lateral approach for fixation of fibula and tibia at same time,6 making lateral plating more appealing. Although some studies are encouraging, we continue to see high rates of complications associated with fixation of this complex fracture.7, 8, 9, 10, 11
While location of plating has been debated, no definitive protocol exists. We propose standardization of treatment based on the evaluation of the fibular component as a major determinant for location of plate placement during surgical fixation provided adequate soft tissue envelope.
The importance of fibular evaluation is well documented in treatment of pilon fractures and makes up one of the basic treatment principles discussed by Ruedi and Allgower.12 Comminuted fibular fractures are known to occur as a result of valgus stresses while transverse fractures are seen with varus angulation.1, 13 In a review paper, Sirkin briefly mentions assessment of the fibular fracture for the location of the tibial plate placement to resist forces originally seen at the time of injury, however no research supports this claim.13 Yenna et al. performed a biomechanical study with the use of sawbones to evaluate the strongest plate construct and concluded no difference between medial vs. lateral plating.14 This study represents an important cornerstone in evaluation of pilon fracture fixation, however, there are major limitations. Use of sawbone tibiae and the absence of the fibular and soft tissue components, which we believe to play a crucial role in stabilization of the fracture, may have resulted in altered outcomes.
In our study, we aim to evaluate the axial stiffness of medial and lateral plate construct for fixation of pilon fracture in cadaveric fracture model. We hypothesized the medial plate fixation to be more stable for pilon fractures failing in varus, as evident by transverse fibular fracture. Similarly, we expected lateral fixation to be superior for pilon fractures failing in valgus, as evident by comminuted fibular fracture.
2. Methods
Eight matched pairs of fresh frozen cadaver specimens (lower limb after a through-knee disarticulation) were used in this study for a total of 16 specimens. Matched pairs, right and left lower extremity from the same cadaver, were utilized to eliminate confounder of bone quality. An even number of valgus and varus fractures (AO 43-A2) were created by removing a wedge of bone with horizontal osteotomy placed 3 cm proximal to ankle joint and oblique osteotomy starting 5 cm proximal to the ankle joint.14 To mimic valgus fractures, apex of the fracture wedge was on the medial side of the tibia, in contrast to varus fractures where the apex of the wedge was located on the lateral side of the tibia (Fig. 1). Associated fibular fractures were created based on fracture type. Valgus fractures received a “comminuted” fibular fracture by removing 1 cm of bone starting 5 cm proximal to the joint line, as well as interruption of the syndesmotic membrane. Varus fractures received a “transverse” fibular fracture by simple transverse osteotomy at the level of the ankle joint without any damage to the syndesmotic membrane.
Fig. 1.
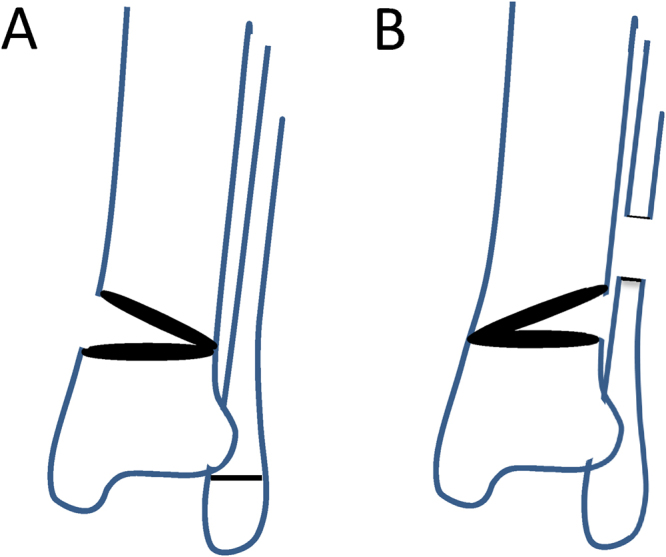
(A) Varus fracture pattern (AO 43-A2) with representative osteotomies. (B) Valgus fracture pattern (AO-A2) with representative osteotomies.
Each pair of specimens was plated medially on one extremity and laterally on the other matched pair, with the wedge in place, utilizing standard operative technique. DePuy medial and anterolateral distal tibial locking 15 hole plates were used for plating. The lateral plate was secured to the tibia using four 3.5 mm locking screws in the distal piece, ensuring bicortical purchase. Proximally, four 3.5 mm cortical screws were used in holes 3, 5, 9, and 13, once again, ensuring bicortical purchase. Medial plate was affixed with three 3.5 mm locking screws distally in the inverse triangle formation while diaphyseal fixation was similar to lateral plate with holes 3, 5, 9, and 13 being filled with 3.5 mm cortical screws. Additionally, “comminuted” fibula fracture for valgus mechanism was plated as well. After plating, the specimens were placed into MTS machine (MTS 858 Mini Bionix II) and loaded with axial force.
Two protocols were created for each specimen. One was executed with a created fracture wedge fixed in place (to mimic a well reduced fracture without bone loss) and another with the fracture wedge removed (to mimic severe comminution). Initially, the specimens were preloaded to 20N and subsequently loaded for ten cycles each to 100N, 250N, 400N, 600N, 800N and 1000N (wedge-in protocol). After each loading cycle, the specimen was relaxed to 20N prior to subsequent application of axial force. Upon completion of the “wedge-in” protocol, the fracture wedge was removed to mimic comminution 20 and a “wedge-out” protocol was initiated. The specimen was once again pre-loaded to 20N and a similar progression of force was applied at 10 cycles per each level of force. This protocol continued past 1000N at 200N increments until 2000N of force was reached. If no failure occurred up to this point, progressively increasing load to failure was applied. For each cycle described above, vertical fracture displacement measurements were recorded as motion measured at the mid-point of the tibia in the coronal plane.
We defined failure as screw breakage, screw pullout or fracture collapse greater than 3 mm, as averaged over 10 cycles in order to minimize measurement error. Force at which failure of the construct occurred was recorder for each specimen. Consistency between timing of specimen defrosting and plating was followed to complete biomechanical analysis prior to 50 h mark post defrosting to eliminate degradation of tissue as a confounding variable.15
2.1. Data analysis
Average force at which failure occurred was compared between the two fixation methods, for varus and valgus fracture pattern respectively, with the use of Mann-Whitney U test.
3. Results
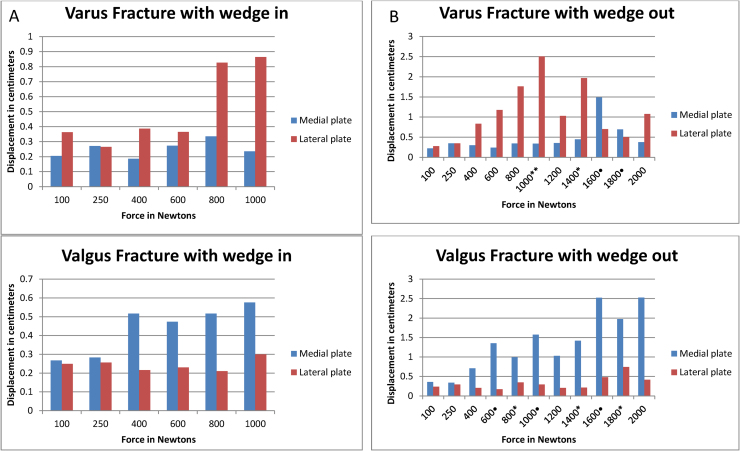
Wide variety of bone quality was encountered within the fresh frozen cadaver specimens, ranging from severe osteoporosis to normal bone based on bone quality during plating and wedge resection. Fracture displacement measurement of four valgus pairs and four varus pairs were noted after application of axial load. With fracture wedge in place, there was no difference in amount of displacement between medial and lateral plate construct, in any of the specimens, as tested up to 1000N of force, although plates placed improperly were consistently allowing increased motion with compression (Fig. 2A).
Fig. 2.
(A) Average displacements for specimens plate medially and laterally with the fracture wedge in place for each compressive load. (B) Average displacements for specimens plate medially and laterally with the fracture wedge removed for each compressive load. * denotes failed specimen plated laterally; • denotes failed specimen plated medially.
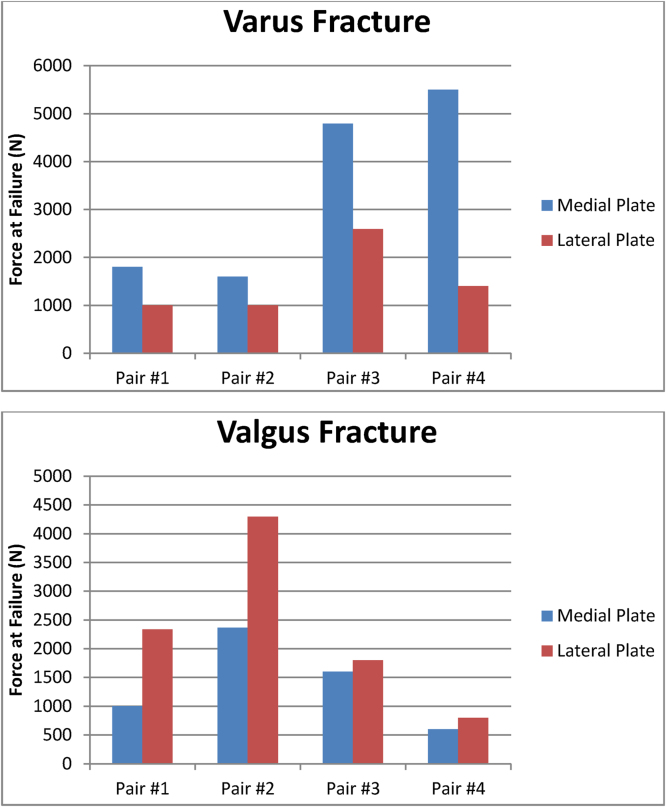
Once fracture wedge was removed, difference in displacement was noted (Fig. 2B). For varus fractures, all specimens plated medially consistently were able to tolerate more load than those plated laterally. On average, medial plate fixation of varus fractures resulted in 2.27 times (range of 1.6–3.9) greater load prior to failure as compared to anterolateral plate. Similarly, valgus simulated fractures tolerated higher force prior to failure if anterolateral plate was applied versus medial plate. Valgus fractures fixed with anterolateral plate were able to handle 1.6 times (range 1.12–2.34) more load comparative to medial plate fixation (Fig. 3). Statistical analysis evaluating medial and lateral plating utilizing the Mann-Whitney U test for varus and valgus fractures, however, were not statistically significant (p = 0.081 and p = 0.386 respectively) due to low number of samples tested. Post-hoc analysis showed both groups to be underpowered. Varus group power was calculated at 0.33 while power for valgus group was at 0.15.
Fig. 3.
Ultimate force at failure for varus and valgus fracture patterns plated medially and laterally.
In an attempt to minimize tissue degradation associated with thawing of fresh frozen cadavers, all biomechanical testing were performed within 50 h of removal from freezer.15 Attempts were made to keep timing to testing constant between specimens. In this study, all specimens were tested within a seven hour window between 25 and 32 h after removal from the freezer.
Majority of specimens failed within the 2000N testing protocol for both varus and valgus fractures. Two of the varus fractures plated medially required progressive load to failure past 2000N and only one specimen plated laterally needed the same. Ranges of force at failure for medially plated varus fracture were 1600N to 5499N, while laterally plated varus fractures failed from 1000N to 2594N. In valgus group, results were similar in this respect. Two specimens with lateral plate exceeded 2000N mark while only one specimen with medial plate did so in the valgus group. Ranges of force at failure for medially plated valgus fracture were 600N to 2368N, while laterally plated varus fractures failed from 800N to 4295N. Of note, severely osteoporotic specimen in valgus group failed within 1000N in both lateral and medial plate fixation with the wedge out.
4. Discussion
In our tertiary referral center, we continue to see patients presenting with post-operative complications and implant failures after fixation of tibial pilon fracture. While several papers describe utilization of a specific surgical approach,5, 6, 16 we were not able to find any research evaluating differences between medial and lateral plating of the pilon fracture based on the fibular component in cadaveric models. Yenna et al. demonstrated no difference with respect to axial stiffness between medial and lateral plating of simulated pilon fractures. Their study utilized Sawbone tibia models which do offer consistency between all specimens, however they are not completely representative of cadaveric tibia and do not account for a spectrum of bone quality encountered clinically. Secondly, fibular contribution to the stability of the pilon fracture could not be assessed. Ruedi and Allgower recognized the importance of the fibula in the treatment of the pilon fracture early on indicating fibular fracture fixation as one of the basic treatment principles.12 Fibula may also contribute to resistance of loads,17, 18 not to mention various soft tissue structures providing stability which are not replicated with sawbone tibia. Thus, ignoring the fibular and soft tissue components may lead to erroneous results. Finally, in the study by Yenna et al. the tibiae were tested to a maximum load of 400N which is not near physiologic value as forces across the ankle joint reach about 5 times the body weight during parts of stance phase.19 In our study, the matched pair with severely osteoporotic bone did not demonstrate a difference between medial and lateral plating until 600N of force was applied. This could be yet another reason for showing no difference between the two plating methods.
Our study did not show statistical significance (p > 0.05) in fracture motion between the two plating locations for either valgus or varus fractures with fracture wedge in place. This suggests that fracture reduction leading to good bony apposition is able to handle the majority of the load regardless of plate position. This should be interpreted with some caution as the maximum load applied for “wedge-in” protocol was 1000N and majority of the specimens did not fail until greater than 1000N of force was applied during the “wedge-out” protocol.
Analysis of axial displacement during the “wedge-out” protocol, designed to mimic severe comminution consistently demonstrated increased ability of a medial plate to handle greater loads for varus type fracture and lateral plate to resist greater forces for valgus fracture. These results support our hypothesis. This proves the importance of re-establishing the tension band and resisting the original deforming forces in order to provide the greatest biomechanical stability possible.
Majority of surgeons will not allow immediate weight bearing after fixation of pilon fractures. Theoretically, the patient would only apply axial force upon initiation of ambulation after adequate bony healing takes place. However, clinical reality is often vastly different and patients are not compliant with weight bearing status.20 Biomechanical construct best able to tolerate physiologic loads is most superior and should be utilized whenever possible.
4.1. Limitations
Our study does have some limitations. As is often the case with biomechanical studies, the study was underpowered due to low number of samples tested. While the trend toward statistical significance, and the fact that correctly plated fractures consistently handled greater loads, is undeniable, lack of power (0.15 and 0.33) complicates interpretation of the results. Nonetheless, we believe that our results showing 2.27 times (varus) and 1.6 times (valgus) increase in load tolerance with appropriate plate location should not be ignored.
Use of fresh frozen cadavers can be viewed as a limitation due to concerns of tissue and bone quality. It is well known that tissue degrades after thawing,15 however all measures were taken to ensure the most uniform experimental conditions with respect to timing and all specimens were tested prior to 50 h mark as described by Cartner et al. Furthermore, use of fresh frozen cadaver matched specimens can be viewed as a strength as various bone qualities were represented, thus mimicking clinical situations.
We only tested AO 43-A2 fracture type whereas majority of pilon fractures are intra-articular and have more pronounced comminution. This fracture pattern was chosen due to ease and consistency of reproducibility between specimens, which is imperative during biomechanical testing. Similarly, biomechanical forces (varus and valgus) resulting in this fracture pattern can be applied to other pilon fractures as well. Thus, AO-A2 fracture type was thought to be an adequate model for biomechanical testing.
Finally, another possible limitation was the use of 15 hole plates. Such long plates are seldom used, and increase in lever arm may lead to increased axial resistance compared to shorter plates. Nonetheless, consistency between screw placements, as well as utilization of the same implant for both extremities eliminates plate length as a confounder. Since the goal of our study was to compare medial to lateral plating and not to evaluate specific stiffness of the construct, generalization of medial versus lateral plating still holds true.
While some specimen failures may have been above the physiologic load, it may be a result of our definition of failure. Non-union may result prior to 3 mm of motion, however, as mentioned previously, the definition of failure was consistent between medial and lateral plating thus allowing the comparison. Also, large amount of displacement prior to “failure” minimized the potential for measurement error between cycles of compression.
5. Conclusion
Our results demonstrate that medial plate fixation is consistently superior to anterolateral plating of varus type fractures in terms of resisting axial load. Similarly, lateral plating is best for valgus type fracture patterns, thus supporting our hypothesis. Evaluation of fibular component in pilon fractures may provide information regarding best plating location to resist deforming forces, thus resulting in lower complication rates such as non-unions, mal-unions, and implant failure. Further patient-based trials in the clinical arena are needed to support our findings.
Funding
Biomet provided required implants for this study including distal tibial plates and screws. Fresh frozen cadaver specimens were provided by the University Medical School Anatomy Department.
References
- 1.Barei D.P. Pilon fractures. In: Rockwood C.A., Green D.P., Bucholz R.W., editors. Rockwood & Green's Fractures in Adults. 7th ed. Lippincott, Williams & Wilkins; Philadelphia, PA: 2010. [p. xvii, 2174 p.] [Google Scholar]
- 2.Egol K.A., Wolinsky P., Koval K.J. Open reduction and internal fixation of tibial pilon fractures. Foot Ankle Clin. 2000;5:873–885. [PubMed] [Google Scholar]
- 3.Patterson M.J., Cole J.D. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999;13:85–91. doi: 10.1097/00005131-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Sirkin M., Sanders R., DiPasquale T., Herscovici D., Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999;13:78–84. doi: 10.1097/00005131-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Grose A., Gardner M.J., Hettrich C. Open reduction and internal fixation of tibial pilon fractures using a lateral approach. J Orthop Trauma. 2007;21:530–537. doi: 10.1097/BOT.0b013e318145a227. [DOI] [PubMed] [Google Scholar]
- 6.Femino J.E., Vaseenon T. The direct lateral approach to the distal tibia and fibula: a single incision technique for distal tibial and pilon fractures. Iowa Orthopaedic J. 2009;29:143–148. [PMC free article] [PubMed] [Google Scholar]
- 7.Brumback R.J., McGarvey W.C. Fractures of the tibial plafond: evolving treatment concepts for the pilon fracture. Orthop Clin North Am. 1995;26:273–285. [PubMed] [Google Scholar]
- 8.Joveniaux P., Ohl X., Harisboure A. Distal tibia fractures: management and complications of 101 cases. Int Orthop. 2010;34:583–588. doi: 10.1007/s00264-009-0832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lau T.W., Leung F., Chan C.F., Chow S.P. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32:697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCann P.A., Jackson M., Mitchell S.T., Atkins R.M. Complications of definitive open reduction and internal fixation of pilon fractures of the distal tibia. Int Orthop. 2011;35:413–418. doi: 10.1007/s00264-010-1005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boraiah S., Kemp T.J., Erwteman A., Lucas P.A., Asprinio D.E. Outcome following open reduction and internal fixation of open pilon fractures. J Bone Joint Surg Am. 2010;92:346–352. doi: 10.2106/JBJS.H.01678. [DOI] [PubMed] [Google Scholar]
- 12.Ruedi T. Fractures of the lower end of the tibia into the ankle joint: results 9 years after open reduction and internal fixation. Injury. 1973;5:130–134. doi: 10.1016/s0020-1383(73)80089-0. [DOI] [PubMed] [Google Scholar]
- 13.Sirkin M.S. Plating of tibial pilon fractures. Am J Orthop (Belle Mead NJ) 2007;36:13–17. [PubMed] [Google Scholar]
- 14.Yenna Z.C., Bhadra A.K., Ojike N.I. Anterolateral and medial locking plate stiffness in distal tibial fracture model. Foot Ankle Int/Am Orthopaedic Foot Ankle Soc Swiss Foot Ankle Soc. 2011;32:630–637. doi: 10.3113/FAI.2011.0630. [DOI] [PubMed] [Google Scholar]
- 15.Cartner J.L., Hartsell Z.M., Ricci W.M., Tornetta P., 3rd. Can we trust ex vivo mechanical testing of fresh?frozen cadaveric specimens? The effect of postfreezing delays. J Orthop Trauma. 2011;25:459–461. doi: 10.1097/BOT.0b013e318225b875. [DOI] [PubMed] [Google Scholar]
- 16.Chen L., O'Shea K., Early J.S. The use of medial and lateral surgical approaches for the treatment of tibial plafond fractures. J Orthop Trauma. 2007;21:207–211. doi: 10.1097/01.bot.0000246410.25423.3e. [DOI] [PubMed] [Google Scholar]
- 17.Kumar A., Charlebois S.J., Cain E.L., Smith R.A., Daniels A.U., Crates J.M. Effect of fibular plate fixation on rotational stability of simulated distal tibial fractures treated with intramedullary nailing. J Bone Joint Surg Am. 2003;85-A:604–608. doi: 10.2106/00004623-200304000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Thambyah A., Pereira B.P. Mechanical contribution of the fibula to torsion stiffness in the lower extremity. Clin Anat. 2006;19:615–620. doi: 10.1002/ca.20234. [DOI] [PubMed] [Google Scholar]
- 19.Stauffer R.N., Chao E.Y., Brewster R.C. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin Orthop Relat Res. 1977:189–196. [PubMed] [Google Scholar]
- 20.Hurkmans H.L., Bussmann J.B., Selles R.W., Benda E., Stam H.J., Verhaar J.A. The difference between actual and prescribed weight bearing of total hip patients with a trochanteric osteotomy: long-term vertical force measurements inside and outside the hospital. Arch Phys Med Rehabil. 2007;88:200–206. doi: 10.1016/j.apmr.2006.11.005. [DOI] [PubMed] [Google Scholar]