Abstract
Objective: To identify potential risk factors associated with rehospitalization among Medicare recipients with heart failure (HF) receiving telehomecare. Materials and Methods: This study is a nonexperimental, cross-sectional secondary data analysis of the Centers for Medicare and Medicaid (CMS) mandated assessment called the Outcome and Assessment Information Set (OASIS)–C, provided by a large home care company. A total of 526 patients who received telehomecare from January 1, 2011 to August 31, 2013 were included in the analyses, which used multiple logistic regression. Results: The overall rate of rehospitalization was 36% while patients were receiving telehomecare. Moderately frail health status (p = 0.01), the presence of severe pain (p = 0.01), the presence of dermatologic problems (p = 0.03), and independence in dressing one's lower body (compared to slightly dependent [p = 0.01] or mostly dependent patient groups [p = 0.02]) were identified as risk factors for rehospitalization. Conclusions: The risk factors identified from this study may be used to drive more effective telehomecare placements, and referrals for additional services among telehomecare patients with HF.
Keywords: : home health monitoring, cardiology, cardiovascular disease, medical records, telehealth
Introduction
Nearly 75% of heart failure (HF) patients enter home care services after hospital discharge,1 and HF is the most common Medicare diagnosis in the home care setting.2,3 Home care services are available for supporting patients with HF in returning to normal life after hospitalization and have integrated telemonitoring services (telehomecare). By monitoring patients' physiological data, such as vital signs and weight, using telehomecare on a daily basis, home care providers and patients can identify early signs of HF exacerbation to prevent rehospitalization.4–8 Although telehomecare has been widely used, the majority of telehomecare clinical trials conducted in the United States for the HF population have yielded mixed results.7,8 One potential way to optimize the use of telehomecare in HF patients is to identify risk factors for rehospitalization from the start of care, to facilitate early recognition of those individuals who need additional support while receiving telehomecare.
To date, little is known about patient-level characteristics of HF patients receiving telehomecare that are associated with rehospitalization. This study aims to identify risk factors for rehospitalization among HF patients receiving telehomecare services. Patient-level characteristics were derived from Centers for Medicare and Medicaid Services mandated assessment tool called the Outcome and Assessment Information Set (OASIS). The purpose of this study was to identify potential risk factors for all-cause first rehospitalization during the home care episode in Medicare recipients with HF receiving telehomecare. Determining these characteristics will assist in tailoring telehomecare interventions to those individuals requiring additional support.
Materials and Methods
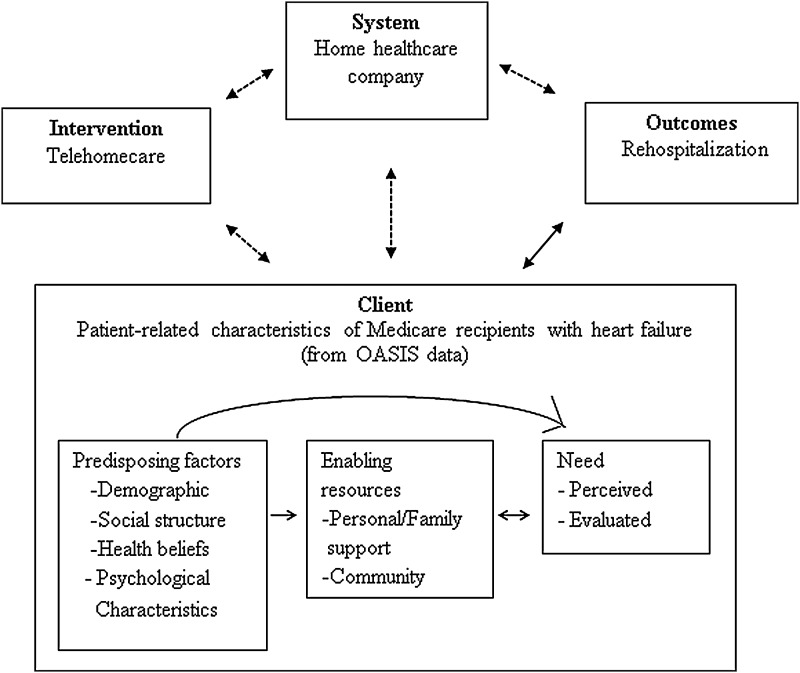
This study was a non-experimental, cross-sectional secondary data analysis using OASIS-C items collected on patients with HF receiving telehomecare services from a large home care company from January 1, 2011 to August 31, 2013. The diagnosis of HF was verified with the following HF International Classification of Disease, Ninth Revision (ICD-9) codes from the OASIS dataset: 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 428.00–428.99. The conceptual framework for this study was developed by triangulating the Quality Health Outcomes Model (QHOM) and the Initial Behavioral Model (IBM) to guide the development of a predictive model of potential risk factors for all-cause first rehospitalization (Fig. 1). The structure of the QHOM was adopted to explain the relationship between the concepts as a primary structure: client, intervention, system, and outcomes. The three components (predisposing, enabling resources, and need characteristics) from the IBM were adopted to organize client (i.e., patient) characteristics. This study was approved by the Institutional Review Board of the researchers' institution, and a data use agreement was signed with the home care company.
Fig. 1.
Triangulated conceptual framework from the quality health outcomes model and the initial behavioral model.
Power Analysis
The sample size determination was based on the following assumptions: a two-sided alpha equal to 0.05, and the percentage of female patients (74%) as an independent variable of interest in the telehomecare group.8 A sample of 499 subjects was found to achieve 80% power to detect an odds ratio as high as 0.53, which corresponds to a 10% point reduction in the rehospitalization rate from 25% in women (i.e., to 15% in men), using a logistic regression model that is statistically significant at an alpha level of 0.05. Thus, a sample of 552 in this study was sufficient to achieve 80% power to detect significance. PASS11 was used to determine sample size requirements.
Instrument
OASIS is a CMS mandated and comprehensive patient assessment instrument collecting administrative and clinical data for home care agencies based on Medicare requirements to evaluate quality improvement and patient outcomes, including case-mix adjustment for factors affecting those outcomes.9–15 Multiple versions of OASIS have been developed and validated over time; the OASIS-C that was initiated in 201013 was used in this study. A report by the U.S. Department of Health and Human Services to Congress stated that the OASIS-C outcome measures capture differences in patient characteristics during the course of a home care episode, including past treatment and risk adjustment.16
The OASIS items as potential risk factors for rehospitalization were divided into three categories in this study: (1) predisposing characteristics are defined as attributes that are inherently personal and relatively unchangeable (i.e., age or ethnicity); (2) enabling resources are defined as characteristics that influence a person's ability to procure healthcare (i.e., family support); and (3) need characteristics refer to factors that may influence the patients' requirements for healthcare (i.e., health or functional status).17–19
Data Source
This study used the Start of Care (i.e., upon admission to home care services), Transfer, and Discharge OASIS-C assessment files. First, identification of in-patient hospitalization before starting home care was determined from the OASIS-C item “in-patient discharge date.”20 To determine whether the patient had a hospital stay during the home care episode, the items, “To which inpatient facility has the patient been admitted?” and “Discharge/transfer/death date” were used from the transfer OASIS-C dataset.20 The Transfer OASIS assessment is completed when patients are transferred to an inpatient facility.20 If the patient did not return to home care from a rehospitalization occurring during the initial home care episode, the item “Discharge/transfer/death date” in the discharge OASIS-C assessment captured the status of rehospitalization.20 This study used the start of care OASIS-C items to identify potential risk factors for all-cause rehospitalization during the home care episode.
Data Analysis
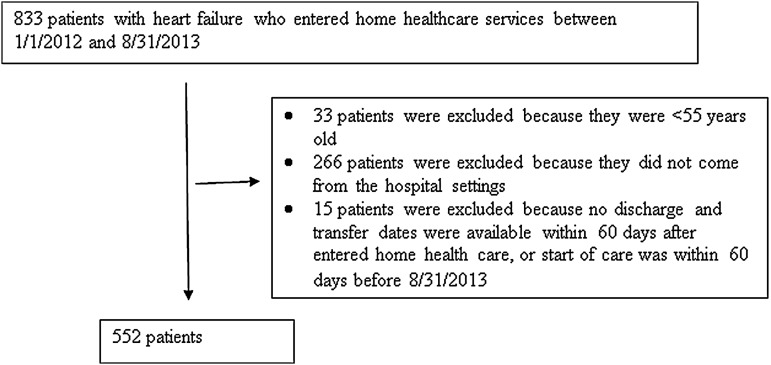
All data analyses were completed in SAS™ version 9.4. Descriptive statistics were used to evaluate characteristics of patients in this study. After the final sample was obtained based on study inclusion and exclusion criteria (Fig. 2), the normality of the distributions for each of the variables in the dataset were examined individually using box plots and histograms. Bivariate logistic regression analyses using PROC GENMOD were conducted to select variables at the alpha level of 0.2 for inclusion in the stepwise regression model. A multiple logistic regression model was built using PROC GENMOD to determine the relative strength of any group associations with adjustment for significant (p < 0.05) covariates. The values of the area under the receiver-operating characteristic curve (AUC) were used to assess the reliability of the final model.
Fig. 2.
The flowchart of sample selection.
The AUC is a rank-based test to measure how well a model differentiates between two groups (i.e., those with and without the event, or with and without an intervention) based on the outcome of interest, which reflects the accuracy of the model.21 If the value of the AUC is greater than 0.7, the model is considered reliable; the closer the value is to 1.0, the more reliable the model.14,22–28 If the value is less than 0.5, the model lacks predictive accuracy and is “no better than chance.”22,23,26
Missing Data
Missing data is a common problem that almost all researchers face.29 Multiple imputation replaces each missing value with a set of plausible values that represent the uncertainty about the value to impute.30 In this study, 15 observations were considered to have missing data because the dates of rehospitalization were unclear. Those with missing outcomes data were excluded. The SAS Multiple Imputation procedure was applied to the subjects with missing data.
Results
A total of 552 patients were included in the data analyses. The AUC value for the final model was 0.63. The results of the multiple logistic regression model are presented in terms of the three categories outlined in the conceptual model guiding this study: predisposing, enabling resources, and need characteristics. Overall, the median age was 79.0 years (interquartile range 15.0). Approximately half the patients who received telehomecare were female, and the majority of patients were White (83%). Patients living with other person(s) were 74%. Nearly 36% of patients had a rehospitalization during the 60 days after being discharged to home care from an in-patient facility. More than half of rehospitalized patients required hospitalization due to HF complications (27%) and other heart disease (26%) (Table 1).
Table 1.
Five Top Reasons for Rehospitalization
| FOR WHAT REASON(S) DID THE PATIENT REQUIRE HOSPITALIZATION? | REHOSPITALIZED (N = 198) COUNT (%) |
|---|---|
| Heart failure | 54 (27) |
| Other heart disease | 51 (26) |
| Respiratory infection | 22 (11) |
| Cardiac dysrhythmia | 16 (8) |
| Other respiratory problem | 16 (8) |
Final Multiple Logistic Regression Model
The full wording of the significant variables in the OASIS-C dataset, and the “term” for each question's responses, are presented in Table 2 for the purpose of interpretation. All the significant variables were in the need characteristics category; that is, patients' current health status, the presence of severe pain, the presence of skin problem(s) (e.g., pressure ulcers, skin lesions or open wounds), and the ability to dress one's lower body.20
Table 2.
Full Wording of the Significant Variables in the OASIS-C Dataset, and the “Term” for Each Question's Possible Responses23
| OASIS-C QUESTION (DEFINITION) | “TERM” FOR EACH QUESTION'S POSSIBLE RESPONSES |
|---|---|
| Which description best fits the patient's overall status? (defined as the patient's current health status) | 1. “Stable” means when a patient is stable without heightened risk (s) for serious complications and deatha |
| 2. “Mildly frail” means when a patient is having high health risk (s) for a short time and is more likely to return to stable status without heightened risk (s) for serious complications and deatha | |
| 3. “Moderately frail” means when a patient is still in frail condition and currently at high risk(s) for serious complications and death | |
| 4. “Very frail” means when a patient has a serious condition(s) that may possibly lead to death within a year | |
| Results of a formal pain assessment using a standardized pain assessment tool (defined as the presence of severe pain) | 1. No standardized, validated assessment doneb |
| 2. Assessment done, but a patient does not complain of severe pain | |
| 3. Assessment done, and a patient complaints of severe pain | |
| The existence of a skin lesion or open wound, excluding bowel ostomy (defined as the presence of skin problems) | 1. No |
| 2. Yes | |
| The capability to dress lower body (with or without dressing aids) including undergarments, slacks, socks or nylons, shoes (defined as capability in dressing lower body) | 1. “Independent” means when a patient is able to dress their lower body without help |
| 2. “Slightly dependent” means when a patient is able to dress their lower body without help, if clothing and shoes were arranged or handed to them | |
| 3. “Mostly dependent” means when a patient requires help to put on undergarments, slacks, socks or nylons, and shoes | |
| 4. “Entirely dependent” means when a patient requires another person to dress their lower body |
In the patient's current health status, the stable and mildly frail groups were combined into one category with regards to patients' current health status.
In the presence of severe pain, the category of “no formal pain assessment done” was considered as missing data because eight patients in the dataset were recognized as nonrecipients of a formal pain assessment.
OASIS-C, Outcome and Assessment Information Set.
Table 3 presents the odds ratios for the final risk factor variables, which could be used to determine a particular patient's risk factors for rehospitalization and to compare the magnitude of the effects of various factors on risk for rehospitalization. In terms of patients' current health status, the odds of being rehospitalized for moderately frail status patients were 1.65 times greater than the odds of rehospitalization in stable or mildly frail patients, with a statistically significant difference between the non-rehospitalized and rehospitalized group (p = 0.01). For patients who were provided a formal pain assessment using a standardized pain assessment tool, the odds of being rehospitalized if they reported severe pain were 1.84 times greater than the odds of rehospitalization in patients without severe pain (p = 0.01).
Table 3.
Odds Ratios and 95% Confidence Interval of the Final Risk Factors
| ODDS RATIO | 95% CONFIDENCE INTERVAL | p-VALUE | |
|---|---|---|---|
| Current health status | 0.03 | ||
| Stable or mildly frail group (reference) | — | — | — |
| Moderately frail group | 1.65 | 1.13, 2.41 | 0.01 |
| Very frail group | 1.61 | 0.84, 3.09 | 0.15 |
| The presence of severe pain | |||
| Without severe pain (reference) | — | — | — |
| With severe pain | 1.84 | 1.14, 2.96 | 0.01 |
| The presence of dermatologic problems | |||
| No (reference) | — | — | — |
| Yes | 1.98 | 1.08, 3.62 | 0.03 |
| The ability in dressing lower body safely | 0.02 | ||
| Independent (reference) | — | — | — |
| Slightly dependent | 0.37 | 0.18, 0.76 | 0.01 |
| Mostly or entirely dependent | 0.46 | 0.25, 0.87 | 0.02 |
Adjusted for these patient-level characteristics: age, expected number of therapy visits (combined total), patient living situation, a change in urinary incontinence, multiple hospitalizations more than two times in the past 12 months, and hospital risk-other risks.
In terms of the presence of dermatologic problems, the odds of being rehospitalized for patients with dermatologic problem(s) were approximately two times greater than for those patients without dermatologic problem(s) (p = 0.03). The odds of being rehospitalized for patients who were slightly dependent for dressing their lower body were 63% lower than those in the independent group (p-value = 0.01); the odds of being rehospitalized among either those in the mostly dependent group or those who were entirely dependent for dressing their lower body were 54% lower than for those in the independent group (p-value = 0.02).
Discussion
A greater proportion of rehospitalizations in this study were related to cardiac diagnoses (54% of rehospitalizations vs. 42% in a previous study). HF was the primary cause of rehospitalization among Medicare recipients with HF receiving telehomecare in this study, followed by other cardiac diseases and cardiac dysrhythmia. This finding is similar to the findings of other studies, in which HF was the principle reason for rehospitalization among Medicare recipients.31,32 Four risk factors for all-cause first rehospitalization were identified in this sample of Medicare recipients with HF receiving telehomecare during their home care episode; the moderately frail health status, the presence of severe pain, the presence of dermatologic problem(s), and independence in dressing the lower body.
Patients' Current Health Status
Before this study, patients' current health status has not been reported as a risk factor for adverse events such as rehospitalizations among home care patients, because it is a new item added in the OASIS-C. Based on the results of this study, telehomecare may not be a sufficient intervention to prevent rehospitalization for the moderately frail, due to the patients' high potential for deterioration. These patients may have needed more intensive interventions, such as continuous maximum Medicare required in-person visits even though patients become stable enough over the course of the home care episode. One suggestion to future versions of the OASIS dataset is to move the current health status items to the end of the OASIS-C assessment instead of placing this item in the beginning of the assessment, to allow home healthcare providers to complete more of the assessment before answering that question and therefore formulate a more accurate assessment of the patient's overall health status. Thus, home care providers could use their clinical judgments to assign each patient to a current health status category in the OASIS-C dataset based on the patients' stability or potential for health decline.
Presence of Severe Pain
We found that the presence of severe pain identified by formal pain assessment using a standardized pain assessment tool at the start of care was associated with rehospitalization. In general, pain is not well understood in the HF population and it has not been typically reported as the typical hallmark symptoms of shortness of breath, fatigue, and edema have.33,34 In addition, evidence demonstrates that pain in patients with stable HF is correlated with fatigue and depression and may restrict daily activity, self-management, and quality of life.34–39
Pain as reported by patients is a subjective experience.40 It is considered the fifth vital sign and is a complex condition to address clinically.41 Unresolved pain usually influences physiological responses, for example by increasing cardiac workload and oxygen demand.35 However, there are many barriers to effective pain management for specific populations, such as a lack of knowledge about pain assessment41 and concerns about intolerance to pain.40 Pain management using pharmacological approaches is difficult in the HF population because of the adverse effects of nonsteroidal anti-inflammatory drugs, such as weight gain, due to interactions with diuretics.40,42 Thus, pain assessment and management in the HF population in the home care setting needs to be developed based on available resources, perhaps by evaluating pain in addition to vital signs and weight through telehomecare.
Presence of Dermatologic Problem(s)
Among home care patients, pressure ulcers or skin problems significantly increase risk for hospitalization18,19,23,43 and constitute an intensive care need.18 This study aligns with previous research18,19,23,43 that has found that patients with dermatologic problems, such as pressure ulcers, skin lesions, or open wounds, are at higher risk for rehospitalization than those patients without dermatologic problems. A common dermatologic manifestation of HF complications, such as pitting edema in the lower extremities, is elephantiasis nostras verrucosa (ENV).44,45 Severe lower extremity edema is associated with decreased cardiac output and can cause other skin problems, such as weeping superficial skin ulceration and inflammation.44,45
Once life-threatening complications are addressed, HF patients may be discharged from the hospital with dermatologic problems such as pitting edema and ENV, and they may be less aggressive about seeking treatment for these problems, since patients often receive more education about managing typical HF symptoms at home. However, if ENV remains untreated and the disease progresses, it can cause infections that may lead to sepsis requiring hospitalization.44,46,47 Treating ENV is a challenge because there is no standardized treatment approach44 (B), even though there are simple and conservative treatments available for lower extremity edema, such as using compression bandages or embolic stockings on the affected areas.44,48 Home care providers may need to be more vigilant in caring for HF patients with dermatologic problems at the start of care and monitor these conditions along with vital signs and weight through telehomecare.
The Ability in Dressing Lower Body
The ability to dress the lower body is one measure of patients' functional status in the OASIS dataset.24 Researchers reported that the ability to dress one's lower body was one of the best indicators of functional dependence in the HF population, followed by the ability to self-bathe.24 In our study, patients who were able to dress their lower bodies independently were more likely to be rehospitalized compared to those patients with some degree of dependency, which was an unanticipated finding of this study. In general, it is assumed that if a telehomecare patient is independent in dressing their lower body, then they should also be able to weigh themselves and be capable of recognizing weight gain earlier than other patients. If this is true, recognition of their weight gain may have triggered the more independent patients to return to the hospital earlier, before they began experiencing clinical deterioration. Another assumption is that those who are more functionally dependent might have better caregiver support and help with meds and diet than those who are independent and perhaps not aware of symptoms. Unfortunately, clear information about whether those with independence had different reasons for rehospitalization from those who were dependent was not available from the OASIS-C data. Future research using the OASIS data is warranted to consider assessing the time of rehospitalization by using survival analysis methods.
The Use of Oasis to Predict the Risk of Rehospitalization
In this study, the AUC value from the final model was 0.63, which is similar to previous studies that used the values of AUC to evaluate the predictive ability of models of rehospitalization or hospitalization built using earlier versions of the OASIS dataset.14,49,50 One study compared the effectiveness of predictive models of rehospitalization between the OASIS dataset and the Probability of Rehospitalization (Pra) instrument, based on the values of the AUC.49 The researchers found that the value of the AUC for the OASIS dataset was 0.60.49 Another study that evaluated a predictive model of hospitalization during the home care episode using the OASIS dataset showed that the value of the AUC was 0.59.14 Although the AUC value from our study does not show that the model generated in our study is ideal (i.e., the AUC was not greater than 0.7), they are consistent with the AUC values from previous studies that have developed predictive models for rehospitalization from home care.14,48,51,52
The findings of our study and other future research using the OASIS can be used to improve the content of the OASIS and to identify risk factors for hospitalization. In particular, policy makers ought to consider adding a variable related to the use of technology to the OASIS dataset to assist researchers in identifying patients receiving any specific interventions. Also, if future studies use rehospitalization as a binary outcome, using larger sample sizes, such as obtaining OASIS data from multiple home care agencies that use telehomecare, might be helpful to maximize model performance. However, as evidence demonstrates that administrative data could be useful to identify patients at risk during the transition home after hospital care,23,53 OASIS data can be an important instrument for predicting rehospitalization risk for HF patients after hospital discharge. In addition, future research is warranted to identify risk factors for rehospitalization using OASIS-C data among both non-telehomecare and telehomecare users.
Limitations
One limitation of this study was that the data were not collected for the specific purpose of this research question, and the dataset was limited to Medicare recipients only. Although the OASIS-C data are required for the assessment of home care patients receiving Medicare benefits, these data do not provide detailed information related to patients' socioeconomic status or ability to use telehomecare. Although this dataset contained data from multiple agencies managed under one home care company, the specific characteristics and effectiveness of the providers in those agencies were unknown. Also, the findings of this study may not be generalizable because the sample was limited to patients with a completed OASIS-C assessment from one home care company. In addition, the process for obtaining two OASIS-C items—patients' current health status and formal pain assessment using a standardized pain assessment tool—was unclear. There was a lack of information from the participating home care company about whether all of the admitting home care providers used the same standardized pain assessment tools among several tools that are available for use. Lastly, due to the nature of secondary data analysis, it was difficult to assess underlying factors.
Conclusions
The findings of this study provide preliminary evidence for the potential role of several risk factors for rehospitalization among Medicare recipients with HF receiving telehomecare. The identified risk factors, such as the presence of severe pain and dermatologic problems at the time of admission to home care services, could be used by home care providers when making clinical judgments about those for whom telehomecare alone is sufficient and those who may need additional support while receiving telehomecare. If home care providers were given guidance regarding the type of patients who would need additional support to prevent rehospitalization, this information would provide a valuable supplement to their care plans involving telehomecare at the start of care.
Acknowledgments
This study was supported by the Ruth L. Kirchenstein National Research Service Training Award for predoctoral students (1F31NR014403), Sigma Theta Tau International Small Grants, Sigma Theta Tau XI chapter, and Frank Morgan Jones Fund at the University of Pennsylvania School of Nursing, Office of Nursing Research. This study was also supported in part by the National Institute of Nursing Research, Aging and Informatics Training Program at the University of Washington School of Nursing (Grant No. T32NR014833). The authors would like to acknowledge the home care company that provided the OASIS–C dataset.
Disclosure Statement
No competing financial interests exist.
References
- 1.Madigan EA. People with heart failure and home health care resource use and outcomes. J Clin Nurs 2008;17:253–259 [DOI] [PubMed] [Google Scholar]
- 2.Bowles KH, Holland DE, Horowitz DA. A comparison of in-person home care, home care with telephone contact and home care with telemonitoring for disease management. J Telemed Telecare 2009;15:344–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delaney C, Apostolidis B. Pilot testing of a multicomponent home care intervention for older adults with heart failure: An academic clinical partnership. J Cardiovasc Nurs 2010;25:E27–E40 [DOI] [PubMed] [Google Scholar]
- 4.Browning SV, Clark RC, Poff RM, Todd D. Telehealth monitoring: A smart investment for home care patients with heart failure? Home Healthc Nurse 2011;29:368–374 [DOI] [PubMed] [Google Scholar]
- 5.Bui AL, Fonarow GC. Home monitoring for heart failure management. J Am Coll Cardiol 2012;59:97–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai AS, Stevenson LW. Rehospitalization for Heart Failure: Predict or prevent? Circulation 2012;126:501–506 [DOI] [PubMed] [Google Scholar]
- 7.Radhakrishna K, Bowles K, Zettek-Sumner A. Contributors to frequent telehealth alerts including false alerts for patients with heart failure: A mixed methods exploration. Appl Clin Inform 2013;4:465–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madigan E, Schmotzer BJ, Struk CJ, et al. Home health care with telemonitoring improves health status for older adults with heart failure. Home Health Care Serv Q 2013;32:57–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madigan EA, Tullai-McGuinness S, Fortinsky RH. Accuracy in the outcomes and assessment information set (OASIS): Results of a video simulation. Res Nurs Health 2003;26:273–283 [DOI] [PubMed] [Google Scholar]
- 10.Hittle DF, Shaughnessy PW, Crisler KS, et al. A study of reliability and burden of home health assessment using OASIS. Home Health Care Serv Q 2004;22:43–63 [DOI] [PubMed] [Google Scholar]
- 11.Kinatukara S, Rosati RJ, Huang L. Assessment of OASIS reliability and validity using several methodological approaches. Home Health Care Serv Q 2005;24:23–38 [DOI] [PubMed] [Google Scholar]
- 12.Tullai-McGuinness S, Madigan EA, Fortinsky RH. Validity testing the outcomes and assessment information set (OASIS). Home Health Care Serv Q 2009;28:45–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deitz D, Dowell RN, Madigan EA, Richard A. OASIS-C: Development, testing, and release: An overview for home healthcare clinicians, administrators, and policy makers. Home Healthc Nurse 2010;28:353–362 [DOI] [PubMed] [Google Scholar]
- 14.Monsen KA, Swanberg HL, Oancea SC, Westra BL. Exploring the value of clinical data standards to predict hospitalization of home care patients. Appl Clin Inform 2012;3:419–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tao H, Ellenbecker CH. Is OASIS effective in predicting rehospitalization for home health care elderly patients? Home Health Care Manage Pract 2013;25:250–255 [Google Scholar]
- 16.Report to the Congress: Medicare Payment Policy. 2012. Available at www.medpac.gov/documents/reports/march-2012-report-to-the-congress-medicare-payment-policy.pdf (last accessed March1, 2014)
- 17.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav 1995;36:1–10 [PubMed] [Google Scholar]
- 18.Fortinsky RH, Madigan EA, Sheehan TJ, Tullai-McGuinness S, Fenster JR. Risk factors for hospitalization among Medicare home care patients. West J Nurs Res 2006;28:902–917 [DOI] [PubMed] [Google Scholar]
- 19.Fortinsky RH, Madigan EA, Sheehan TJ, Tullai-McGuinness S, Kleppinger A. Risk factors for hospitalization in a national sample of medicare home health care patients. J Appl Gerontol 2014;33:474–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Outcome and Assessment Information Set (OASIS). Centers for Medicare & Medicaid Services Web site. Available at www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/homehealthqualityinits/downloads/hhqioasiscalltimepoint.pdf (last accessed March1, 2014)
- 21.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation 2007;115:928–935 [DOI] [PubMed] [Google Scholar]
- 22.Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med 2000;45:23–41 [DOI] [PubMed] [Google Scholar]
- 23.Rosati RJ, Huang L. Development and testing of an analytic model to identify home healthcare patients at risk for a hospitalization within the first 60 days of care. Home Health Care Serv Q 2007;26:21–36 [DOI] [PubMed] [Google Scholar]
- 24.Scharpf TP, Madigan EA. Functional status outcome measures in home health care patients with heart failure. Home Health Care Serv Q 2010;29:155–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Westra BL, Savik K, Oancea C, Choromanski L, Holmes JH, Bliss D. Predicting improvement in urinary and bowel incontinence for home health patients using electronic health record data. J Wound Ostomy Continence Nurs 2011;38:77–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: A systematic review. JAMA 2011;306:1688–1698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Madigan EA, Gordon NH, Fortinsky RH, Koroukian SM, Pina I, Riggs JS. Rehospitalization in a national population of home health care patients with heart failure. Health Serv Res 2012;47:2316–2338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han SJ, Kim HK, Storfjell J, Kim MJ. Clinical outcomes and quality of life of home health care patients. Asian Nurs Res 2013;7:53–60 [DOI] [PubMed] [Google Scholar]
- 29.Allison PD. Sage university papers series on quantitative applications in the social sciences. In: Allison PD, ed. Missing data. Thousand Oaks, CA: Sage, 2001:136 [Google Scholar]
- 30.Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons, 2009 [Google Scholar]
- 31.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418–1428 [DOI] [PubMed] [Google Scholar]
- 32.Psotka MA, Teerlink JR. Strategies to prevent postdischarge adverse events among hospitalized patients with heart failure. Heart Fail Clin 2013;9:303–320, vi. [DOI] [PubMed] [Google Scholar]
- 33.Goebel JR, Doering LV, Shugarman LR, et al. Heart failure: The hidden problem of pain. J Pain Symptom Manage 2009;38:698–707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evangelista LS, Sackett E, Dracup K. Pain and heart failure: Unrecognized and untreated. Eur J Cardiovasc Nurs 2009;8:169–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Godfrey C, Harrison MB, Medves J, Tranmer JE. The symptom of pain with heart failure: A systematic review. J Card Fail 2006;12:307–313 [DOI] [PubMed] [Google Scholar]
- 36.Goodlin SJ, Wingate S, Pressler SJ, Teerlink JR, Storey CP. Investigating pain in heart failure patients: Rationale and design of the pain assessment, incidence & nature in heart failure (PAIN-HF) study. J Card Fail 2008;14:276–282 [DOI] [PubMed] [Google Scholar]
- 37.Rustøen T, Stubhaug A, Eidsmo I, Westheim A, Paul SM, Miaskowski C. Pain and quality of life in hospitalized patients with heart failure. J Pain Symptom Manage 2008;36:497–504 [DOI] [PubMed] [Google Scholar]
- 38.Goodlin SJ, Wingate S, Albert NM, et al. Investigating pain in heart failure patients: The pain assessment, incidence, and nature in heart failure (PAIN-HF) study. J Card Fail 2012;18:776–783 [DOI] [PubMed] [Google Scholar]
- 39.Conley S, Feder S, Redeker NS. The relationship between pain, fatigue, depression and functional performance in stable heart failure. Heart Lung 2015;44:107–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wheeler M, Wingate S. Managing noncardiac pain in heart failure patients. J Cardiovasc Nurs 2004;19(6 Suppl):S75–S83 [DOI] [PubMed] [Google Scholar]
- 41.Lynch M. Pain as the fifth vital sign. J Intraven Nurs 2001;24:85–94 [PubMed] [Google Scholar]
- 42.Bleumink GS, Feenstra J, Sturkenboom MC, Stricker BH. Nonsteroidal anti-inflammatory drugs and heart failure. Drugs 2003;63:525–534 [DOI] [PubMed] [Google Scholar]
- 43.Rosati RJ, Huang L, Navaie-Waliser M, Feldman PH. Risk factors for repeated hospitalizations among home healthcare recipients. J Healthc Qual 2003;25:4–10 [DOI] [PubMed] [Google Scholar]
- 44.Baird D, Bode D, Akers T, Deyoung Z. Elephantiasis nostras verrucosa (ENV): A complication of congestive heart failure and obesity. J Am Board Fam Med 2010;23:413–417 [DOI] [PubMed] [Google Scholar]
- 45.Liaw FY, Huang CF, Wu YC, Wu BY. Elephantiasis nostras verrucosa: Swelling with verrucose appearance of lower limbs. Can Fam Physician 2012;58:e551–e553 [PMC free article] [PubMed] [Google Scholar]
- 46.Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: A review. Am J Clin Dermatol 2008;9:141–146 [DOI] [PubMed] [Google Scholar]
- 47.Yoho RM, Budny AM, Pea AS. Elephantiasis nostras verrucosa. J Am Podiatr Med Assoc 2006;96:442–444 [DOI] [PubMed] [Google Scholar]
- 48.Iwao F, Sato-Matsumura KC, Sawamura D, Shimizu H. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg 2004;30:939–941 [DOI] [PubMed] [Google Scholar]
- 49.Bowles KH, Cater JR. Screening for risk of rehospitalization from home care: Use of the outcomes assessment information set and the probability of readmission instrument. Res Nurs Health 2003;26:118–127 [DOI] [PubMed] [Google Scholar]
- 50.O'Connor M, Davitt JK. The outcome and assessment information set (OASIS): A review of validity and reliability. Home Health Care Serv Q 2012;31:267–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kossovsky MP, Sarasin FP, Perneger TV, Chopard P, Sigaud P, Gaspoz J. Unplanned readmissions of patients with congestive heart failure: Do they reflect in-hospital quality of care or patient characteristics? Am J Med 2000;109:386–390 [DOI] [PubMed] [Google Scholar]
- 52.Ross JS, Mulvey GK, Stauffer B, et al. Statistical models and patient predictors of readmission for heart failure: A systematic review. Arch Intern Med 2008;168:1371–1386 [DOI] [PubMed] [Google Scholar]
- 53.Coleman EA, Min SJ, Chomiak A, Kramer AM. Posthospital care transitions: Patterns, complications, and risk identification. Health Serv Res 2004;39:1449–1465 [DOI] [PMC free article] [PubMed] [Google Scholar]