Abstract
Objective
To evaluate causes and predictors of readmission after new ileostomy creation.
Summary Background
New ileostomates have been reported to have higher readmission rates compared to other surgical patients, but data on predictors are limited.
Methods
1114 records at two associated hospitals were reviewed to identify adults undergoing their first ileostomy. Primary outcome was readmission within 60 days of surgery. Multiple logistic regression was used to identify independent predictors; receiver-operator characteristics (AUC) were used to evaluate age-stratified models in secondary analysis.
Results
407 patients underwent new ileostomy. 58% had cancer, 31% IBD; 49% underwent LAR, 27% colectomy, 14% proctocolectomy. Median length-of-stay was 8 days. 39% returned to hospital; 28% were readmitted (n=113) at median of 12 days post-discharge. The most common causes of readmission were dehydration (42%), intra-peritoneal infections (33%), and extra-peritoneal infections (29%). Dehydration was associated with later, longer, and repeated readmission. Independent significant predictors of readmission were Clavien-Dindo complication grade 3–4 (OR 6.7), Charlson comorbidity index (OR 1.4 per point), and loop stoma (OR 2.2); longer length-of-stay (OR 0.5) and age 65 or older (OR 0.4) were protective. Cohort stratification above or below age 65 revealed that older patient readmissions were more predictable (AUC 0.84) with more preventable causes; younger patient readmissions were difficult to predict or prevent (AUC 0.65).
Conclusions
Readmissions are most commonly caused by dehydration, and are predicted by serious complications, comorbidity burden, loop stoma, shorter length-of-stay, and age. Readmissions in older patients are easier to predict, representing an important target for improvement.
INTRODUCTION
Hospital readmissions are carefully monitored by national agencies as a quality indicator and a target for improvement in outcomes and costs. Unplanned readmissions represented 17% of overall Medicare spending in 2004, with a 22% 60-day post-operative readmission rate for Medicare beneficiaries1. The Hospital Readmission Reduction Program of the Affordable Care Act went into effect in 2012, mandating Medicare reimbursement penalties for excessive readmissions. In 2013, the program expanded to include elective arthroplasties, suggesting that additional surgical procedures could also face future penalization.
The Centers for Medicare & Medicaid Studies (CMS) and the National Surgical Quality Improvement Program (NSQIP) have specifically designated colorectal surgery outcomes among the top five areas for improvement, recommending their use as quality indicators. Readmission rates among colectomy patients at 30 days post-discharge have been reported at 11.4 to 16%2,3,4, similar to other surgical populations. However, rates for patients undergoing ostomy creation are far higher—a recent series reported 43% in ostomates vs. 15% in non-ostomates at 60 days post-discharge 5. High readmission rates have been described in small cohorts5,6,7,8,9 of new ileostomy patients, and one population study reported readmission10 ranging from 17 to 49% at 30 days to several months post-operatively. These rates project as many as 20,000 readmissions in the US per year11, representing a substantial opportunity for quality improvement.
Dehydration has been reported as the most common cause of readmission of new ileostomates, occurring in 44% of readmissions8. The presence of a stoma has been shown to consistently impair renal function, with clinical renal failure occurring in 20% of ileostomates12. Although readmissions are often multifactorial, dehydration represents a prevalent and potentially preventable target. To implement preventive strategies on patients at risk for dehydration and readmission, however, they must first be identified, preferably prior to discharge.
Literature on factors predictive of readmission in new ileostomates is limited, and results are inconsistent. In this study, we rigorously analyzed a large cohort of new ileostomy patients, with the objective of definitively establishing the causes and predictors of readmission. We hypothesized that dehydration would be the leading cause of readmission, and that variables relating to dehydration, ileostomy output, and frailty, assessable at time of discharge, would be predictive of readmission within 60 days of surgery.
METHODS
Cohort composition
With Institutional Review Board approval, a cohort was assembled from two large, adjacent urban hospitals (a general hospital and a cancer center), both academically-affiliated and sharing conferences, house staff, and many management principles. All patients undergoing surgeries including ileostomy creation, over a 30 month period (2010–2012) were retrospectively identified from billing records, using a pre-specified list of 25 Current Procedural Terminology (CPT) 2012 codes. An overly-comprehensive CPT code list was developed to capture all potential ileostomates. All of the included surgeons held academic appointments. Neither hospital consistently used a formal enhanced recovery after surgery (ERAS) program at the time of this study; however, many post-operative management principles were practiced, including use of mechanical bowel preparation, pre-incision antibiotics, intravenous or epidural patient-controlled analgesia, incentive spirometry, early ambulation, deep vein thrombosis prophylaxis, and education by a wound ostomy certified nurse (WOCN).
Exclusion Criteria
Records were preliminarily reviewed and excluded if 1) patient did not actually undergo ileostomy creation, despite their CPT billing code; 2) records were duplicate (single patient with multiple CPT codes from single operation); 3) patient had documentation of previous ostomy; 4) age was less than 18 years; 5) readmission within 60 days was impossible due to inpatient death or length-of-stay greater than 60 days; 6) operation was undertaken for a non-gastrointestinal diagnosis (e.g. urologic or gynecologic); 7) ileostomy was created with documented palliative intent.
Data Collection
Each medical record, from pre-operative planning through 60 days post-operation, was assessed by a single, surgically-trained reviewer. Predictor and outcome variables were selected for extraction a priori based on clinical expertise and literature review. An exhaustive examination of each patient’s chart was performed, recording patient, operative, and post-operative factors. The date of surgery was considered the date of ileostomy creation; if ileostomy was created to deal with complications of a prior procedure, the patient was coded as having a history of previous surgery less than 60 days ago and the ileostomy creation date was considered the index surgical date. Charlson Comorbidity Index, a comorbidity summarization score linearly associated with 1-year mortality13, and the modified Clavien-Dindo Complication scoring system, classifying post-operative complications by therapy required14, was calculated for each patient.
Outcome Measures
Readmission for any cause within 60 days of ileostomy creation was chosen a priori as the primary outcome, a window incorporating the Medicare-tracked 30-day post-discharge endpoint, and capturing as much readmission burden as was consistently feasible, given that the surgeons involved generally waited a minimum of 60 days before reversing temporary ileostomies. Readmission was defined by the presence of an admission order with corroborating documentation. Details of readmissions to other institutions were inferred, when possible, from primary institution records; outside institution records were reviewed only if included in primary institution records. Secondary outcomes included visits to the Emergency Department (ED) that did not result in readmission, administration of intravenous (IV) fluids outside of the inpatient setting (in ED, clinic, or total parenteral nutrition at home), and specific causes of readmission, which were defined operationally and applied non-exclusively. Readmission with dehydration was of special interest and a robust, objective definition was developed (Table 1).
Table 1.
Operational Definitions of Causes of Readmission
| Causes of Readmission | Criteria met during readmission | |
|---|---|---|
| Dehydration | Meets criteria 1 or 2+3 | Positive item meets that criteria |
OR
AND
|
Urine sodium < 20mEq/L Fractional excretion of sodium < 0.5% Urine osmolality > 450 Diagnosis of dehydration High stoma output described Poor oral intake or vomiting described BUN/creatinine ratio >20 Creatinine >= 150% of baseline Bicarbonate < 20 Hyperkalemia > 5.0 or Hypokalemia < 3.4 Hypernatremia > 149 or Hyponatremia < 133 Sinus tachycardia > 110 Mean Arterial Pressure < 65 Documented orthostatic hypotension |
|
| Ileus/Obstruction | Nasogastric tube placement during readmission | |
| Intra-peritoneal Infections | Drainage procedure intraoperatively, endoscopically, or via interventional radiology (ie anastomotic leaks or intra-abdominal abscesses) | |
| Extra-peritoneal Infections | Infections not requiring operative drainage but requiring administration of antibiotics for 48 hours or longer (eg UTIs, wound infections, etc) | |
| Major stomal complication | Stoma revision or early closure procedure | |
| Minor stomal complication | Stoma obstruction by food bolus, parastomal dermatitis or cellulitis, or parastomal hernia listed in admission or discharge notes | |
| Other medical cause | Any other cause for readmission listed in admission or discharge notes* | |
except acute renal failure, electrolyte abnormalities, cardiac arrhythmias or failure to thrive when occurring concurrently with dehydration (presumed secondary to dehydration)
Statistical Considerations
The study was powered to allow observation of medium-sized effects with as many as 20 variables in multiple regression15,16, requiring a sample size of at least 265 patients (N>104+8m); more patients or fewer variables enhanced power to observe smaller effects.
Univariate and multivariate associations of predictor variables with outcomes were assessed using uncorrected Chi-Square tests, mid-P exact tests, and logistic regression, with log transformation of variables where appropriate. Predictor variables deemed clinically important by investigators, and all variables significantly associated with the primary outcome on univariate analyses, were selected for potential inclusion in multivariable predictor models. For these, Pearson’s coefficients were calculated to assess pairwise variable correlations and linear regression variance inflation factors were analyzed to assess multicollinearity, with some variables removed due to excessive redundancy.
Remaining variables were entered into multivariable logistic regression; forward and backward automated stepwise regressions were applied to assess model stability and reduce models to include only variables with p values <= 0.10, to optimize bias-variance tradeoff. Additional regression analysis of stratified data was used to assess age, due to observation of the mixed effects of this variable. Receiver-operator characteristic (ROC) curves were plotted for models to assess predictive power.
RESULTS
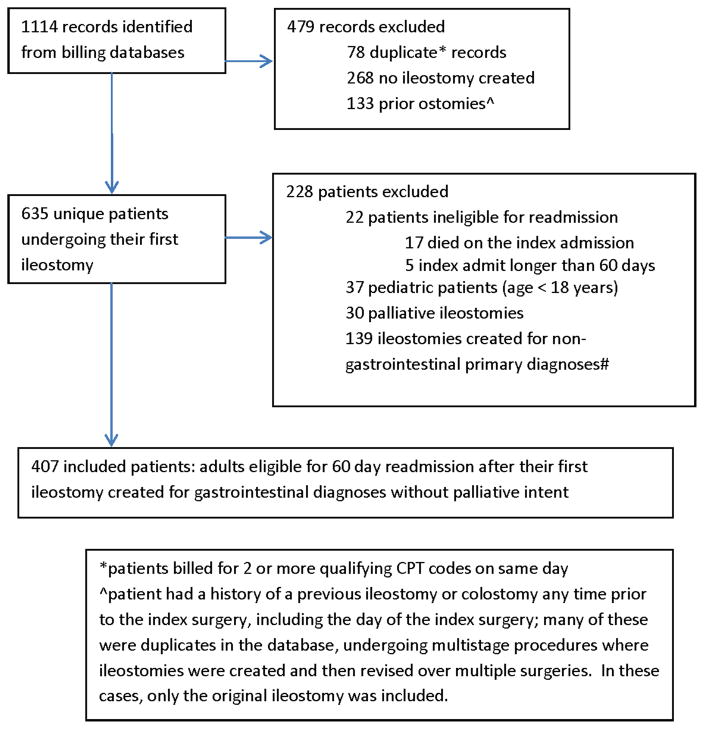
Over a 30-month period, 1114 records were identified from billing databases, of which 707 were excluded (Figure 1), yielding a cohort of 407 patients undergoing first ileostomy creation by a general or colorectal surgeon. Patient characteristics, operative factors, and post-operative sequela (Table 2) demonstrated that the mean age of the cohort was 53 years, 55% were male, and the most common reason for ileostomy creation was colorectal cancer (58%). Fifty-four percent of surgical procedures were open, 78% elective. Ninety-seven percent of patients had a WOCN visit, and 93% were discharged home (98% with nursing visits).
Figure 1.
Inclusion and Exclusion Flow Chart
Table 2.
Patient Demographics, Operative and Post-Operative Factors
| All patients (n=407) | Readmitted (n=113) | Not Readmitted (n=294) | Risk Ratio | 95% Conf. Int. | P value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean age (SD) | 53 | (16) | 53 | (16) | 53 | (17) | 1.0 | 1.0–1.0 | 0.89 | |
| Age groups | 18–39 | 23% | 95 | 20% | 23 | 24% | 72 | Ref | ||
| 40–59 | 39% | 157 | 44% | 50 | 36% | 107 | 1.3 | 0.9–2.0 | 0.20 | |
| 60–79 | 33% | 136 | 29% | 33 | 35% | 103 | 1.0 | 0.6–1.6 | 0.99 | |
| 80+ | 5% | 19 | 6% | 7 | 4% | 12 | 1.5 | 0.8–3.0 | 0.25 | |
| Age 65 or above | 25% | 101 | 24% | 27 | 29% | 86 | 1.0 | 0.7–1.4 | 0.79 | |
|
| ||||||||||
| Gender | F | 45% | 182 | 41% | 46 | 46% | 136 | Ref | ||
| M | 55% | 225 | 59% | 67 | 54% | 158 | 1.2 | 0.9–1.6 | 0.31 | |
|
| ||||||||||
| Institution | NYP-Cornell | 54% | 218 | 54% | 61 | 53% | 157 | Ref | ||
| MSKCC | 46% | 189 | 46% | 52 | 47% | 137 | 1.0 | 0.7–1.4 | 0.92 | |
|
| ||||||||||
| Lives alone | 21% | 86 | 25% | 28 | 19% | 58 | 1.2 | 0.9–1.8 | 0.26 | |
|
| ||||||||||
| Mean BMI (SD) | 26.1 | (5.4) | 25.9 | (5.5) | 26.1 | (5.4) | 1.0 | 1.0–1.0 | 0.71 | |
|
| ||||||||||
| Smoking | 16% | 64 | 22% | 25 | 13% | 39 | 1.5 | 1.1–2.2 | 0.02 | |
|
| ||||||||||
| Charlson | 0 | 67% | 274 | 57% | 65 | 71% | 209 | Ref | ||
| Comorbidity Index | 1–2 | 23% | 94 | 26% | 29 | 22% | 65 | 1.3 | 0.9–1.9 | 0.09 |
| 3+ | 10% | 39 | 17% | 19 | 7% | 20 | 2.1 | 1.4–3.0 | 0.001 | |
|
| ||||||||||
| Specific Comorbidity | ||||||||||
| Hypertension | 29% | 116 | 28% | 32 | 29% | 84 | 1.0 | 0.7–1.4 | 0.96 | |
| Cardiovascular Disease | 11% | 43 | 13% | 15 | 10% | 28 | 1.3 | 0.8–2.0 | 0.27 | |
| Diabetes | 9% | 37 | 14% | 16 | 7% | 21 | 1.7 | 1.1–2.5 | 0.03 | |
| Renal disease | 4% | 16 | 7% | 9 | 2% | 7 | 2.1 | 1.3–3.4 | 0.02 | |
|
| ||||||||||
| Medications | ||||||||||
| Diuretics | 8% | 33 | 5% | 6 | 9% | 27 | 0.6 | 0.3–1.3 | 0.20 | |
| Beta-blockers | 16% | 66 | 18% | 20 | 15% | 45 | 1.1 | 0.7–1.7 | 0.61 | |
| Other Anti-HTNs | 19% | 76 | 19% | 21 | 19% | 55 | 1.0 | 0.7–1.5 | 0.98 | |
| Anti-diarrheals | 6% | 23 | 7% | 8 | 5% | 15 | 1.3 | 0.7–2.3 | 0.44 | |
| Steroids | 17% | 68 | 20% | 23 | 15% | 45 | 1.3 | 0.9–1.9 | 0.22 | |
| Psych. Meds. | 23% | 95 | 23% | 26 | 23% | 69 | 1.0 | 0.7–1.4 | 0.92 | |
|
| ||||||||||
| Intestinal | None | 86% | 350 | 79% | 89 | 89% | 261 | Ref | ||
| Surgery | > 60d prior | 9% | 35 | 11% | 12 | 8% | 23 | 1.4 | 0.8–2.2 | 0.26 |
| History | < 60d prior | 5% | 22 | 11% | 12 | 3% | 10 | 2.2 | 1.4–3.3 | 0.003 |
|
| ||||||||||
| Diagnosis* | ||||||||||
| Colorectal cancer | 58% | 238 | 59% | 67 | 58% | 171 | Ref | |||
| IBD | 31% | 125 | 28% | 32 | 32% | 93 | 0.9 | 0.6–1.3 | 0.60 | |
| Other | 11% | 44 | 12% | 14 | 10% | 30 | 1.1 | 0.7–1.8 | 0.62 | |
|
| ||||||||||
| Colorectal Surgeon | 88% | 360 | 92% | 104 | 87% | 256 | 1.1 | 0.9–1.1 | 0.16 | |
|
| ||||||||||
| Procedure Urgency | ||||||||||
| Elective | 78% | 318 | 75% | 85 | 79% | 233 | Ref | |||
| Within 7 days | 11% | 46 | 15% | 17 | 10% | 29 | 1.4 | 0.9–2.1 | 0.15 | |
| Within 24 hours | 11% | 43 | 10% | 11 | 11% | 32 | 1.0 | 0.6–1.6 | 0.87 | |
|
| ||||||||||
| Ileostomy Procedure | ||||||||||
| +− SBR +− LOA | 11% | 44 | 16% | 18 | 9% | 26 | 1.7 | 1.1–2.5 | 0.03 | |
| + Colectomy | 27% | 110 | 23% | 26 | 29% | 84 | 1.0 | 0.6–1.4 | 0.81 | |
| +Proctocolectomy | 14% | 56 | 18% | 20 | 12% | 36 | 1.4 | 0.9–2.2 | 0.11 | |
| +Low Ant. Resection | 49% | 197 | 43% | 49 | 50% | 148 | Ref | |||
|
| ||||||||||
| Additional organ resected^ | 13% | 51 | 10% | 11 | 14% | 40 | 0.8 | 0.4–1.3 | 0.29 | |
|
| ||||||||||
| Contamination# | ||||||||||
| Mild | 67% | 273 | 63% | 71 | 69% | 202 | Ref | |||
| Moderate | 21% | 85 | 20% | 23 | 21% | 62 | 1.0 | 0.7–1.6 | 0.84 | |
| Heavy | 12% | 49 | 16% | 19 | 10% | 30 | 1.5 | 1.0–2.2 | 0.06 | |
|
| ||||||||||
| Stoma type | End | 25% | 103 | 21% | 24 | 27% | 79 | Ref | ||
| Loop | 75% | 304 | 79% | 89 | 73% | 215 | 1.3 | 0.9–1.9 | 0.24 | |
|
| ||||||||||
| Operative Approach$ | ||||||||||
| Minimally Invasive | 46% | 189 | 44% | 49 | 48% | 140 | Ref | |||
| Open | 54% | 218 | 57% | 64 | 52% | 154 | 1.1 | 0.8–1.6 | 0.44 | |
|
| ||||||||||
| Median OR time in min (Inter-Quartile Range) | 258 | (186–338) | 259 | (163–336) | 257 | (190–340) | 1.0 | 1.0–1.0 | 0.82 | |
|
| ||||||||||
| Median Estimated Blood Loss in ml (IQR) | 200 | (100–300) | 200 | (75–400) | 200 | (100–300) | 1.0 | 1.0–1.0 | 0.51 | |
|
| ||||||||||
| Intra-Op Blood transfusion | 6% | 26 | 9% | 10 | 5% | 16 | 1.4 | 0.9–2.4 | 0.21 | |
|
| ||||||||||
| Median Length of Stay in days (IQR) | 8 | (6–10) | 8 | (7–11) | 8 | (6–10) | 1.0 | 1.0–1.1 | 0.45 | |
| 1–5 days | 9% | 36 | 11% | 8% | 1.3 | 0.8–2.2 | 0.30 | |||
| 6–10 days | 66% | 270 | 60% | 12 | 69% | 24 | Ref | |||
| 11 days or more | 25% | 101 | 29% | 68 33 |
23% | 202 68 |
1.3 | 0.9–1.8 | 0.15 | |
|
| ||||||||||
| Median days until | ||||||||||
| Stoma output began*** | 2 | (2–3) | 2 | (2–3) | 3 | (2–3) | 0.9 | 0.8–1.1 | 0.32 | |
| Discharge after output | 5 | (4–7) | 6 | (4–8) | 5 | (4–7) | 1.0 | 1.0–1.1 | 0.23 | |
|
| ||||||||||
| Median ostomy output last 48 hrs recorded, liters | 1.4 (1.0–2.1) | 1.3 (0.9–2.2) | 1.4 (0.9–2.0) | 1.0 | 1.0–1.0 | 0.99 | ||||
|
| ||||||||||
| Mean Renal markers prior to discharge (SD) | ||||||||||
| Last BUN | 9.8 | (6.9) | 10 | (6.5) | 9.6 | (7.0) | 1.0 | 1.0–1.0 | 0.56 | |
| Last Creatinine | 0.9 | (0.7) | 1.0 | (1.0) | 0.8 | (0.5) | 1.3 | 0.9–1.7 | 0.14 | |
| Last Creatinine above 1.0 | 12% | 50 | 18% | 20 | 10% | 30 | 1.5 | 1.1–2.1 | 0.04 | |
|
| ||||||||||
| Clavien Dindo Inpatient Complication Grade^^ | ||||||||||
| 0 | 59% | 238 | 47% | 53 | 63% | 185 | Ref | |||
| 1–2 | 25% | 113 | 24% | 27 | 26% | 76 | 1.2 | 0.8–1.8 | 0.44 | |
| 3–4 | 17% | 66 | 30% | 33 | 11% | 33 | 2.3 | 1.6–3.2 | 0.0001 | |
|
| ||||||||||
| NG tube placement | 18% | 73 | 17% | 19 | 18% | 54 | 0.9 | 0.6–1.4 | 0.71 | |
|
| ||||||||||
| Wound Ostomy Nurse | ||||||||||
| Pre-operative visit | 66% | 268 | 65% | 74 | 66% | 194 | 1.0 | 0.7–1.4 | 0.92 | |
| Inpatient visit | 96% | 389 | 96% | 109 | 95% | 280 | 1.3 | 0.5–3.0 | 0.62 | |
| Neither | 3% | 14 | 3% | 3 | 4% | 11 | 0.8 | 0.3–2.1 | 0.63 | |
|
| ||||||||||
| Discharged on anti-diarrheals | 13% | 53 | 16% | 18 | 12% | 35 | 1.3 | 0.8–2.6 | 0.28 | |
| Imodium only | 7% | 30 | 4% | 5 | 9% | 25 | Ref | |||
| Lomotil only | 4% | 16 | 8% | 9 | 2% | 7 | 3.3 | 1.4–8.4 | 0.009 | |
| Discharged on both | 2% | 7 | 4% | 4 | 1% | 3 | 3.4 | 1.2–9.6 | 0.05 | |
GI Cancer Includes dysplasia, high-risk syndromes, localized cancer, and metastatic cancer excised curatively; IBD includes Crohn’s, ulcerative colitis, and patients with IBD and coexisting cancers; Other includes diverticulitis, Clostridium difficile colitis, perforation, fistula in the absence of malignancy or inflammatory bowel disease, volvulus, ischemic colitis, gastrointestinal bleed, bowel obstruction, rectal prolapse, or intractable constipation
Time from decision to operate until operation
Most common were uterus, ovaries, salpinx, vagina, partial liver, or gallbladder
Contamination levels – Mild: cancer, mild IBD; Moderate: CDiff, ischemic colitis, or moderate-severe inflammatory bowel disease; Heavy: any pt with anastomotic leak, perforation, abscess, fistula
Minimally invasive includes robotic, laparoscopic, and hand-assisted laparoscopic surgery. Open surgery defined as a vertical midline incision > 8cm or placement of a Bookwalter or Balfour retractor
Output defined as >= 250cc in one day
Grade 1–2 complications include: NG tube placed, diuresis, blood transfusion, antibiotics, ARF, TPN given, pleural effusions, stomal swelling, wound opened at bedside, atrial fibrillation with RVR, DVT; Grade 3 complication is return to operating room, endoscopy suite or interventional radiology; Grade 4 complication is intensive care unit stay for any reason
Abbreviations: SD = standard deviation; NYP = New York Presbyterian; MSKCC = Memorial Sloan Kettering Cancer Center; BMI = body mass index; HTN = hypertension; IBD = inflammatory bowel disease; SBR = small bowel resection; LOA = lysis of adhesions; OR = operating room; IQR = inter-quartile range; BUN = Blood urea nitrogen; NG = nasogastric
Stratifying the cohort by institution, expected differences were observed. Compared to the general hospital, patients at the cancer center were more often males (64% vs. 48%) undergoing elective surgery (91% vs. 67%). At the cancer center, the most common diagnosis and operation was colorectal cancer (93%) and low anterior resection (74%), respectively; at the general hospital, inflammatory bowel disease (49%) and partial/total colectomy (42%), respectively. Despite these differences, readmission rates at the institutions were equal; age, complication rates, comorbidity burden, length-of-stay and other important population factors did not differ significantly. Given these similarities, both hospitals were deemed appropriate for analysis as a single cohort. Six surgeons at the cancer center and 14 surgeons at the general hospital created ileostomies during the study period, with an overall median of 19 per surgeon.
All-Cause and Specific Causes of Readmission
Thirty-seven percent of patients (150/407) returned to the ED; 28% were readmitted (113/407) within 60 days of surgery (Table 3), with 5% readmitted multiple times (21/407) and 3% readmitted to other institutions (14/407). After discharge, 12% received IV fluids as outpatients. Of the 12.5% (51/407) who came to the ED and were sent home, 27% (14/51) eventually returned and were readmitted. Receiving IV fluids did not prevent readmission in this group; readmission rates were equal whether or not IV fluids were given (28% vs. 27%, respectively, p=0.93).
Table 3.
Outcomes within 60 days post-operatively
| All Patients (n=407) | ||
|---|---|---|
| Returned to emergency department | 37% | 150 |
| Readmitted for any cause | 28% | 113 |
| Readmitted to an outside institution | 3% | 14 |
| Readmitted multiple times | 5% | 21 |
| Received IV fluids without readmission (in clinic, ED, or as outpatients) | 12% | 50 |
Sixty-five percent of readmitted patients had a single cause of readmission (73/113); 35% had multiple causes (40/113) (Table 4); 45% (51/113) required a major procedure during readmission (laparoscopy/laparotomy, endoscopy, or interventional radiology); and 2% died (2/113). The median time to first readmission was 19.5 days after surgery (IQR 13–31 days) or 10.5 days after discharge (IQR 5–18 days). The median length of first readmission was 5 days (IQR 2–7 days). Fifty-seven percent of readmitted patients had an office visit prior to readmission at a median of 6 days post-discharge, versus 11 days in patients who were not readmitted.
Table 4.
Causes of Readmission
| Readmitted patients (n=113) | Readmitted patients, age-stratified
|
||||||
|---|---|---|---|---|---|---|---|
| 18–64 years (n=86) | 65+ years (n=27) | p | |||||
| Causes of readmission (non-exclusive) | |||||||
| Dehydration | 42% | 47 | 32% | 28 | 70% | 19 | 0.0008 |
| Intra-peritoneal Infections | 31% | 35 | 36% | 31 | 15% | 4 | 0.04 |
| Extra-peritoneal infections | 29% | 33 | 19% | 16 | 41% | 11 | 0.001 |
| Urinary Tract Infection | 9% | 10 | |||||
| Wound infection | 9% | 10 | |||||
| Pouchitis | 4% | 4 | |||||
| C. Difficile Colitis | 3% | 3 | |||||
| Other | 6% | 7 | |||||
| Obstruction/Ileus | 13% | 15 | 15% | 13 | 7% | 2 | 0.33 |
| Stomal Complication | 12% | 14 | 13% | 11 | 11% | 3 | 0.87 |
| Major | 6% | 7 | |||||
| Miscellaneous causes* | 31% | 35 | 36% | 31 | 15% | 4 | 0.04 |
|
| |||||||
| Single cause of readmission | 65% | 73 | |||||
| Multiple causes | 35% | 40 | |||||
|
| |||||||
| Dehydration sole cause for readmission | 14% | 16 | |||||
|
| |||||||
| Procedures required during readmission | |||||||
| Any | 45% | 51 | |||||
| Laparotomy | 8% | 9 | |||||
| Stoma revision/early closure | 6% | 7 | |||||
| Transrectal procedure/Endoscopy | 14% | 16 | |||||
| Interventional Radiology | 27% | 30 | |||||
| In-room procedure^ | 29% | 33 | |||||
|
| |||||||
| Death during readmission | 2% | 2 | |||||
Miscellaneous causes were very diverse, including electrolyte abnormalities, acute renal failure, DVT, PE, portal vein thrombus, stomal obstruction by food particles, bleeding from rectum, peristomal dermatitis, failure to thrive, atrial fibrillation, leukopenia, CBD dilatation, angina, dysphagia, pleural effusion, CHF, gastroparesis, fever, post-chemotherapy enteritis, urinary retention, and partial SBO symptoms
In-room procedures included NG tube placement, wound exploration, wound VAC placement, or stomal intubation
The most common cause of readmission was dehydration (Table 4), occurring in 42% of readmissions (47/113); 35% (16/47) were readmitted for dehydration only. Dehydration conferred increased morbidity and 49% (23/47) were likely to have additional subsequent conditions: acute renal failure (23%, 11/47), significant electrolyte derangement (11%, 5/47), cardiac arrhythmia (15%, 7/47), and failure to thrive (6%, 3/47). Patients with dehydration were readmitted significantly later than those without (median 13 vs. 8.5 days after discharge, p=0.001), and length-of-stay during readmission was longer (median 5 vs. 4 days, p=0.001). Dehydration was also associated with repeat readmissions: 76% (16/21; p=0.0003) of multiple-readmits had at least one dehydration readmission and 24% (5/21) had multiple readmissions for dehydration.
Other causes of readmission (Table 4) included intra-peritoneal infection (anastomotic leak or abscess requiring drainage (31%; 35/113), extra-peritoneal infection (primarily urinary and wound infections requiring antibiotics (29%; 33/113), and obstruction or ileus resulting in nasogastric drainage (13%; 15/113) (Table 4). Thirty-one percent had at least one “miscellaneous” reason for readmission (35/113). These varied widely in type and severity: idiopathic pain, nausea, anxiety, pulmonary embolism, new cancers, or mesenteric ischemia.
Univariate and Multivariate Associations: All-cause Readmission
Univariate analyses for all variables were performed (Table 2). Smoking, Charlson Comorbidity Index of 3 or more, diabetes, renal disease, intestinal surgery within 60 days prior, last inpatient creatinine greater than 1.0, Clavien-Dindo complication grade of 3–4, or discharge on diphenoxylate-atropine were significantly associated with all-cause readmission.
After assessment for univariate significance, clinical importance and multicollinearity, 17 predictor variables were included in initial multiple logistic regression model. Backward and forward stepwise regressions were applied to remove non-significant variables, and both processes separately converged on a single solution of seven variables demonstrating significant or near-significant association with all-cause readmission (Table 5). Clavien-Dindo complication grade 3–4 (OR 6.74, 95% CI 3.02–15.0, p<0.001), Charlson Comorbidity Index (OR 1.42 per point, 95% CI 1.17–1.71, p<0.001), and loop stoma (OR 2.18, 95% CI 1.21–3.93, p=0.01) were each predictive of readmission, while age 65 and older (OR 0.42, 95% CI 0.22–0.80, p=0.01) and longer length-of-stay (log transformed) were protective (OR 0.47, 95% CI 0.24–0.92, p=0.01). Discharge on diphenoxylate-atropine (p=0.07), and living alone (p=0.10), did not reach significance of 0.05, but remained in the model.
Table 5.
Multiple Logistic Regression Results
| All-Cause Readmission (n=113/407) | Age less than 65 (n=86/306) | Age 65 and over (n=27/101) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Age 65 or greater | 0.4 | 0.2–0.8 | 0.01 | ||||||
|
| |||||||||
| Lives alone | 1.6 | 0.9–2.8 | 0.10 | -- | 5.0 | 1.4–17 | 0.01 | ||
|
| |||||||||
| Charlson Cormorbidity Index |
1.4 per point |
1.2–1.7 | <0.001 | -- |
1.6 per point |
1.2–2.2 | 0.005 | ||
|
| |||||||||
| History of prior intestinal surgery | -- | -- |
5.8 11.6 if <=60 days ago |
1.4–24 | 0.02 | ||||
|
| |||||||||
| Loop stoma (vs end) | 2.2 | 1.2–3.9 | 0.01 | -- | 7.3 | 1.3–40 | 0.02 | ||
|
| |||||||||
| Clavien-Dindo Complication Grade 3–4 | 6.7 | 3.0–15 | <0.001 | 3.9 | 1.8–8.3 | <0.001 | 22 | 3.4–140 | 0.001 |
|
| |||||||||
| Length of stay (days; log transform) | 0.5 | 0.2–0.9 | 0.01 | -- | 0.1 | 0.01–0.6 | 0.01 | ||
|
| |||||||||
| Discharge on Lomotil | 2.4 | 0.9–6.1 | 0.07 | 3.6 | 1.2–11 | 0.02 | -- | ||
Secondary Analysis: Stratification by Age
The unexpected finding of a protective effect associated with older age was further explored. Because age appeared to have significant effects on other predictor variables, the cohort was stratified for further analysis by age greater or less than 65, chosen a priori as the Medicare eligibility age. Causes of readmission were found to differ significantly by age (Table 6). Older patients were most commonly readmitted for dehydration and extra-peritoneal infections--significantly more often than younger patients. Readmission for dehydration was more than twice as frequent in older patients (19% vs. 9%). Younger patients were most commonly readmitted for intra-peritoneal infections and miscellaneous causes.
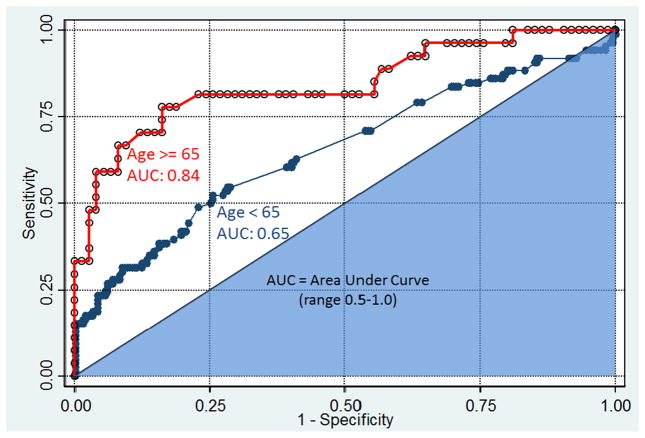
To further assess the effects of age, multivariable logistic regression for independent predictors of readmission was repeated with age stratification, yielding notable differences by age group (Table 5). In the older patients, all-cause readmission was independently predicted by five factors: Charlson Comorbidity Index (OR 1.58 per point, 95% CI 1.15–2.17, p=0.005), Clavien-Dindo Complication Grade 3–4 (OR 21.6, 95% CI 3.37–139, p=0.001), living alone (OR 4.98, 95% CI 1.42–17.4, p=0.01), loop ileostomy (7.26, 95% CI 1.33–39.5, p=0.02), or history of prior surgery (OR 5.80, 95% CI 1.41–23.9, p=0.02). In the younger patients, Clavien-Dindo Complication Grade 3–4 (OR 3.90, 95% CI 1.83–8.30, p<0.001) and discharge on diphenoxylate-atropine (OR 3.60, 95% CI 1.19–10.8, p=0.02) were the only independent predictors reaching significance. Moreover, the predictive capacity of the older patient model was much stronger. Models were evaluated using area under the ROC curve (AUC; Figure 2). The model for patients 65 years or older had an AUC of 0.84; the AUC for patients younger than 65 years was 0.65.
Figure 2.
Receiver Operator Characteristic (ROC) curves for age-stratified regression analyses of readmission with area under the curve statistic. Models include only variables with p<0.10; model results were converged upon by both forward and backward stepwise regression. Variables in older age model: living alone, Charlson Comorbidity Index, history of recent abdominal surgery, loop vs. end stoma, Clavien-Dindo complication grade, length of stay. For younger age model: Clavien-Dindo complication grade, discharge on Lomotil.
DISCUSSION
We rigorously examined a retrospective cohort of 407 new ileostomies from two affiliated hospitals, finding an all-cause readmission rate of 28% within 60 days of surgery. Dehydration was the most common cause; it was associated with longer, later, and multiple readmissions, as well as additional morbidity. Multiple logistic regressions revealed comorbidity burden, serious inpatient complications, loop stoma, shorter length-of-stay, and younger age as independent predictors of readmission. Stratification of the cohort by age demonstrated different patterns of readmission: older patient readmissions were primarily for dehydration or extra-peritoneal infections, and had more identifiable predictive factors. Readmissions in younger patients were largely due to intra-peritoneal infections or miscellaneous causes, and were mostly unpredictable by the factors studied.
Strengths and Limitations
This study is the largest cohort of readmitted ileostomy patients studied in detail to date, and has many strengths. From billing data, we comprehensively captured all ileostomies by 20 surgeons at two hospitals, representing current practices with minimal selection bias. Primary data from clinical records were meticulously collected with a priori selection and explicit definition of variables. Causes of readmission were also operationally defined, enhancing their reliability and reproducibility--especially for dehydration, which has rarely been formally defined in previous studies. Multiple causes of readmission were recorded when they existed concurrently, to minimize interpretation bias. Predictive variables studied were limited to those assessable at time of post-operative discharge, so that results can be used to identify high-risk patients for potential intervention prior to hospital discharge.
This study has limitations. The retrospective design relies on the accuracy and completeness of clinical charts. Readmission to outside institutions is particularly challenging to assess in any retrospective, institution-level study. However, unlike prior studies8,17, we made a significant effort to identify outside readmissions by reviewing the entire chart, including all follow-up notes by physicians and nurses. Some variables such as ethnicity, socioeconomic variables, or distance from hospital, were not collected. Patients with ileostomies created by gynecologists or urologists were excluded in order to enhance specificity to the practices of general and colorectal surgical communities; patients with prior ostomies were excluded to capture the experience of ostomy-naïve patients. Variation in surgeon-specific readmission rates existed, but the number of surgeons relative to the total sample prohibited analysis of readmission by surgeon.
Although many post-operative management practices were shared between surgeons, neither hospital had instituted formal ERAS programs at the time of study, which have been recommended by the ASCRS for new ileostomy patients20. Nagle et al9 have demonstrated that early patient autonomy in ostomy care can potentially reduce readmissions, which was not described at time of our study. Most of our patients visited with WOCNs pre- and post-operatively and received stoma marking and education, although the details of those processes could not be captured with sufficient detail to evaluate their benefits. Incorporating our findings into ERAS programs for new ostomates is a priority. Despite these limitations, we believe that our results provide important findings for developing pathways for patients with new ileostomies.
Study Findings and Previous Literature
This large study strengthens the results of smaller studies. The 28% 60-day readmission rate after ileostomy, observed here, confirms the magnitude of the problem5,6,7,9,10. While the rate observed in this study and prior small studies was higher than the 17% observed by Messaris et al8, that study may lack applicability, as a single-institution cohort was assembled from records over 20-years. Using a reproducible, operational definition of dehydration, our study also concludes that dehydration is the most common cause of readmission after ileostomy7,8, and confirms that older age is a risk factor for dehydration7,8,17. As dehydration is the most common cause of readmission in patients 65 years and older, this suggests an opportunity for targeted efforts designed to reduce readmissions in this group.
Our study describes important and novel findings. It clarifies the magnitude of post-discharge morbidity incurred by dehydration, which was associated with both repeated and longer readmissions and by secondary morbidity in roughly 50% of cases. We used rigorous methods in a large cohort to demonstrate that serious inpatient complications, comorbidity burden, loop stoma, shorter length-of-stay, and younger age are factors independently predictive of readmission after ileostomy creation. Although rarely10,18,19 evaluated in prior studies, the most consistently significant independent predictor was serious pre-discharge complications, necessitating interventional procedures or intensive care management during the index admission. Complications can substantially exacerbate post-operative deconditioning, and have profound effects on patients’ coping strategies after discharge. Comorbidity burden was also strongly predictive of readmission. While comorbidity is routinely used to informally estimate patients’ capacity to recover after surgery, it has been measured inconsistently in the surgical literature including previous work on ileostomy readmission,7,8,10 and likely represents one of the best ways to identify those at risk. Half of all patients with a Charlson Comorbidity Index of three or more were readmitted—twice as often as those with an index of zero. Shorter length-of-stay predicted readmission, which is provocative in the context of tremendous interest in shortening length-of-stay. Loop stoma construction was also a predictor, likely demonstrating that more proximal stomas increase dehydration risk, and suggesting the need for more aggressive fluid management in outpatients.
The most compelling finding was that younger age independently predicted readmission, a surprising result that contradicted prior literature7,8,13. To understand this effect further, the cohort was stratified according to Medicare eligibility, revealing significant differences in causes and predictors of readmission. Patients older than 65 were most often readmitted with dehydration and extra-peritoneal infections (primarily wound and urinary tract), conditions that can often be safely treated without hospital admission if diagnosed early and treated appropriately. Furthermore, older patient readmissions were well-predicted by the variables measured (AUC 0.84). However, patients younger than 65 years had a significantly higher rate of readmission for intra-peritoneal infections, which are difficult to prevent and treat on an outpatient basis. Other causes of younger patient readmissions varied, and were relatively unpredictable overall (AUC 0.65). This study demonstrates, for the first time, that readmissions after ileostomy are more predictable and preventable in older patients.
Clinical and policy implications
This work has numerous implications. It demonstrates that ileostomy patients warrant special attention, and that dehydration represents an important opportunity for improved outcomes in this population. It establishes risk factors for ileostomy readmission that can be routinely identified prior to discharge, allowing targeted surveillance and interventions for patients at highest risk. Our work indicates that patients over 65 likely benefit most from risk-stratification. This suggests that more research on the relationship between older age and post-operative readmissions is warranted, and may facilitate further quality improvement.
Future Research
These risk factors for readmission of ileostomy patients, herein identified through detailed study of a large cohort, can be converted into a practical readmission risk-prediction tool that could be validated in another cohort. Such an instrument should allow for targeted, intensive, preventative interventions for at-risk patients. These interventions must be developed and could include more stringent discharge criteria to optimize patient’s status, discharge with more intensive outpatient services or reconsideration of discharge to a facility, and a more rigorous program of post-operative follow-up including additional telephone or electronic surveillance, earlier or more frequent appointments, routine laboratory investigation, or an electronic stoma output-reporting program. This study demonstrates that patients aged 65 and older might especially benefit from risk-stratification, enhanced discharge planning and post-discharge management, and that focus on prevention of dehydration and extra-peritoneal infections may be particularly effective strategies.
CONCLUSIONS
Readmission is a prevalent and morbid problem for patients with new ileostomies, occurring in 28% within 60 days of surgery. Causes are heterogeneous, but dehydration is the most common. The strongest predictors of readmission at time of discharge are comorbidity burden and serious inpatient complications. Readmissions in younger patients are more frequently for intra-peritoneal infections; these are difficult to predict, and are primarily associated with serious impatient complications. Readmission in patients over 65 years, however, are more frequently for potentially preventable conditions such as dehydration and UTI; for this cohort readmission is more easily predictable, and is associated with comorbidity, serious complications, living alone, prior intestinal surgery, loop stoma, and short length-of-stay. Patients should be risk-stratified prior to discharge—especially the elderly—and those at risk should be targeted for preventative interventions.
Acknowledgments
Source of Funding: Daniel R. Fish, MD was supported by the Agency for Healthcare Research and Quality training grant T32HS000066.
This study was funded in part through the NIH/NCI Support Grant P30 CA008748.
Footnotes
Conflicts of Interest: None declared
This study was presented at the Annual Meeting of the American Society of Colon and Rectal Surgeons, May 17 – May 21, 2014, Hollywood, FL
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009 Apr 2;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Hendren S, Morris AM, Zhang W, et al. Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum. 2011 Nov;54(11):1362–7. doi: 10.1097/DCR.0b013e31822b72d3. [DOI] [PubMed] [Google Scholar]
- 3.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012 Apr;214(4):390–8. doi: 10.1016/j.jamcollsurg.2011.12.025. discussion 398–9. [DOI] [PubMed] [Google Scholar]
- 4.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011 Dec;54(12):1475–9. doi: 10.1097/DCR.0b013e31822ff8f0. [DOI] [PubMed] [Google Scholar]
- 5.Poritz, et al. Ostomy creation significantly increases er visits and hospital readmission after colorectal resection (2012) Gastroenterology. 2012;142(5 Suppl 1):S1029–S1030. [Google Scholar]
- 6.Alves-Ferriera PC, de Campos-Lobato L, Vogel J. What are the risk factors for readmission in patients with an ileostomy? Dis Colon Rectum. 2011;54:e179. [Google Scholar]
- 7.Hayden DM, Pinzon MCM, Francescatti AB, et al. Hospital readmission for fluid and electrolyte abnormalities following ileostomy construction: preventable or unpredictable? J Gastrointest Surg. 2013;17:298–303. doi: 10.1007/s11605-012-2073-5. [DOI] [PubMed] [Google Scholar]
- 8.Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum. 2012 Feb;55(2):175–80. doi: 10.1097/DCR.0b013e31823d0ec5. [DOI] [PubMed] [Google Scholar]
- 9.Nagle D, Pare T, Keenan E, et al. Ileostomy pathway virtually eliminates readmissions for dehydration in new ostomates. Dis Colon Rectum. 2012;55:1266–1272. doi: 10.1097/DCR.0b013e31827080c1. [DOI] [PubMed] [Google Scholar]
- 10.Tyler JA, Fox JP, Dharmarajan S, et al. Acute health care resource utilization for ileostomy patients is higher than expected. Dis Colon Rectum. 2014;57:1412–20. doi: 10.1097/DCR.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 11.Husain SG, Cataldo TE. Stomas and wound management. Clin Colon Rectal Surg. 2008 Feb;21(1):31–40. doi: 10.1055/s-2008-1055319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beck-Kaltenbach N, Voigt K, Rumstadt B. Renal impairment caused by temporary loop ileostomy. Int J Colorectal Dis. 2011;26:623–626. doi: 10.1007/s00384-010-1086-3. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Ales KA, Pompei P, et al. A new method of classification of prognostic comorbidity for longitudinal studies: development and validation. J Chron Disease. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004 Aug;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson VanVoorhis CR, Morgan BL. Understanding power and rules of thumb for determining sample sizes. Tutorial in Quantitative Methods for Psychology. 2007;3(2):43–50. [Google Scholar]
- 16.Green SB. How many subjects does it take to do a regression analysis? Multivariate Behavioral Research. 1991;26(3):499–510. doi: 10.1207/s15327906mbr2603_7. [DOI] [PubMed] [Google Scholar]
- 17.Paquette IM, Solan P, Rafferty JF, et al. Readmission for dehydration or renal failure after ileostomy creation. Dis Colon Rectum. 2012;56:974–9. doi: 10.1097/DCR.0b013e31828d02ba. [DOI] [PubMed] [Google Scholar]
- 18.Bartlett EK, Hoffman RL, Mahmoud NN, et al. Post-discharge occurrences after colorectal surgery happen early and are associated with dramatically increased rates of readmission. Dis Colon Rectum. 2014;57(11):1309–16. doi: 10.1097/DCR.0000000000000212. [DOI] [PubMed] [Google Scholar]
- 19.Tevis SE, Weber SM, Kent C, et al. Nomogram to predict postoperative readmission in patients who undergo general surgery. JAMA Surg. 2015;150(6):505–510. doi: 10.1001/jamasurg.2014.4043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hendren S, Hammond K, Glasgow S, et al. Clinical Practice Guidelines for ostomy surgery. Dis Colon Rectum. 2015;58(4):375–87. doi: 10.1097/DCR.0000000000000347. [DOI] [PubMed] [Google Scholar]