Abstract
Background The purpose of this article was to review the anatomy, kinematics of the distal radioulnar joint (DRUJ), and to discuss definition, classification, and diagnosis of DRUJ instability.
Methods A biomechanical perspective on physical examination of DRUJ ballottement test was documented. Physiological dynamic DRUJ translation and differences of the translation following sequential ligament sectioning and changes in different forearm and wrist positions were demonstrated. The clinical significance of each ligament's contribution to joint stability in specific wrist positions was addressed.
Conclusion Each ligament stabilizing the DRUJ contributed to joint stability depending on the direction (palmer or dorsal) and different positions of the wrist and forearm. DRUJ ballottement test in each wrist and forearm position may detect tears of specific ligament stabilizing the DRUJ.
Keywords: DRUJ, TFCC, biomechanics, anatomy, function
The distal radioulnar joint (DRUJ) is inherently unstable, and the curvature of the sigmoid notch of the radius (radius of curvature: 18 mm) is twice as large as that of the ulnar head (8 mm).1 During forearm rotation, both dorsal–palmar and proximal–distal translation occurs between the joint surfaces. Although there is considerable variation between individuals, the osseous architecture of the sigmoid notch is a dorsally open wedge (10 degrees) and its dorsal length (10 mm) is greater than its volar length (6 mm).1 2 This architecture may explain the tendency of the ulnar head to lie in the dorsal aspect of the sigmoid notch and to subluxate dorsally when the forearm is pronated (piano key sign) following rupture of radioulnar ligament (RUL). The palmar osteocartilaginous lip of the sigmoid notch, which is the attachment site of the palmar RUL, plays an importance role in distal radioulnar stability. There are three types of sigmoid notch inclinations (obliquity) at the mid-coronal sequence: parallel, oblique (distally open wedge), or reverse oblique (proximally open wedge), relative to the long axis of the radius and ulna.3 A negative correlation has been demonstrated between the obliquity of the DRUJ and ulnar variance.1 4
The deep ligamentous portions of the triangular fibrocartilage complex (TFCC) provide the primary intrinsic stabilization of the DRUJ. These fibers, which attach at the ulnar fovea and lie on the axis of forearm rotation, are the most isometric and undergo the least length changes during pronosupination movement. The palmar deep fibers of the RULs may be taut in pronation to prevent dorsal ulnar head subluxation, and the dorsal deep fibers may be taut in supination to restrain the ulna from palmar migration relative to the radius.5 Supplemental stability is provided by superficial fibers of the RUL, which may have a checkrein effect during forearm rotation. The ulnocarpal ligament (UCL) complex and the floor of the extensor carpi ulnaris (ECU) tendon sheath, including the ulnar collateral ligament, are the other components of the TFCC and also stabilize the DRUJ in specific wrist positions. Other secondary stabilizers include the distal oblique bundle (DOB) of the distal interosseous membrane (DIOM), the ECU tendon, and the pronator quadratus muscle. The tendons of the ECU and pronator quadratus muscles serve as dynamic stabilizers.6 7
Definition of Distal Radioulnar Joint Instability
Linscheid et al and Cooney et al established radiological criteria for carpal instability based on the anatomical causes of carpal malalignment.8 9 Larsen et al proposed a standardized analysis of carpal instability using six categories that describe the chronicity, constancy, etiology, location, direction, and pattern of the instability.10 Although there are no standardized criteria for DRUJ instability, axial computed tomography (CT) may provide reliable assessment of both dynamic and static instabilities. Various evaluation methods on CT are available for quantifying DRUJ translation, and the reliability of reference DRUJ translation values has been demonstrated.11 12 13 14 CT images in neutral forearm rotation can detect static instability, and dynamic CT during maximum pronosupinations and stress CT can potentially identify dynamic instability.15 According to the Larsen's criteria discussed for carpal instability,10 it is important that CT-based criteria for dynamic and static DRUJ instabilities are defined; these are possible to establish by accumulating both normal and patient data drawn from multiple large populations.
Classification of Distal Radioulnar Joint Instability
An etiology-based classification system for DRUJ instability is described in Table 1. Traumatic DRUJ instability is most commonly encountered in a clinical hand surgery practice. Extra-articular fractures, including Essex-Lopresti fracture dislocation and Galeazzi fracture dislocation, involve dislocation of the DRUJ associated with complete RUL ruptures. DRUJ instability accompanying distal radial fractures is sometimes attributed to complete rupture of the RULs at the foveal insertion, which may occur as a purely soft tissue injury but is often identified by the presence of an ulnar styloid fracture.16 Extra-articular metaphyseal deformities such as radial shortening, dorsal and volar angulation, or radial translation also cause DRUJ instability.17 18 19 Moreover, displacement of intra-articular fractures involving the ulnar head or sigmoid notch may result in abnormal kinematics of the DRUJ, leading to DRUJ instability (Fig. 1). Other etiologic factors that may cause DRUJ instability include inflammatory, congenital, and neoplastic disease; the osteochondral deformities and arthritis associated with these factors are difficult to treat by interventions targeted at the ligamentous structures only.
Table 1. Etiology-based classification of DRUJ instability.
| Etiology | Cause of DRUJ instability |
|---|---|
| Traumatic | Osseous instability Extra-articular fracture Extra-articular fractureEssex-Lopresti fracture dislocation Galeazzi fracture dislocation Distal radius fracture  Intra-articular fracture Intra-articular fractureUlnar head fracture Sigmoid notch fracture Foveal avulsion fracture Ligamentous instability Radioulnar ligament tear |
| Inflammatory | Rheumatoid arthritis |
| Congenital | Madelung deformity |
| Neoplastic | Multiple osteochondromatosis |
Abbreviation: DRUJ, distal radioulnar joint.
Fig. 1.

(Left) Palmar plating for intra-articular distal radius fracture. (Center left) 3D CT indicating a displaced volar rim fragment. (Center right) Intra-articular fracture displacement of the sigmoid notch in the coronal plane. (Right) Dorsal subluxation of the ulnar head relative to the sigmoid notch malunion. CT, computed tomography; 3D, three-dimensional.
Diagnosis of Distal Radioulnar Joint Instability
Because the primary stabilizer of the DRUJ is the deep portion of the RULs, diagnosis of DRUJ instability should focus on identification of RUL ruptures at the fovea. Imaging studies, provocative tests, and arthroscopic findings associated with the diagnosis of DRUJ instability are described here.
Anatomy of the Ligamentous Portion of the Triangular Fibrocartilage Complex
There are a total of eight TFCC ligaments stabilizing the DRUJ, including four RULs, three ligaments in the UCL complex, and one ulnar collateral ligament.20 21 22 23 24 The four RULs consist of the deep and superficial limbs of the palmar and dorsal ligaments, which are triangular in shape and lie beneath the articular disc.23 The deep limbs of the RULs arise from the dorsal and palmar lips of the sigmoid notch and attach primarily to the fovea of the ulnar head, with additional attachments to the ulnar styloid base. The ligamentous fibers of the superficial limb are hardly separated from those of the deep limb and attach to the midportion of the ulnar styloid. The UCL complex consists of the ulnotriquetral, ulnolunate, and ulnocapitate ligaments, which originate together at the fovea of the ulnar head and from the palmar RULs.24 The ulnocapitate ligament runs more superficially than the other two ligaments. These three ligaments, along with the palmar RULs, extend distally to form a fan-like structure in the coronal plane and insert at the palmar aspects of the triquetrum, lunate, and capitate carpal bones. The floor of the ECU tendon sheath is part of the TFCC and connects the dorsal aspect of the ulnar styloid base to the dorsal surface of the triquetrum. The ECU floor includes fibers of the ulnar collateral ligament, which contribute to the ulnar collateral stability of the ulnocarpal joint. The DRUJ is stabilized in extension and radial deviation by tension in the ECU floor.25
Secondary Stabilizers
The DIOM is a secondary static stabilizer, and the dynamic stabilizers comprise the ECU and pronator quadratus muscles. There is considerable anatomical variation in the thickness of the DIOM; its DOB, which contains obvious thick fibers, exists in 40% of the forearm membrane.26 27 The DOB originates from the distal one-sixth of the ulnar shaft and runs distally to insert on the dorsal inferior rim of the sigmoid notch of the radius. The DOB reinforces the function of the deep limb of the dorsal RULs and acts as a static stabilizer of the DRUJ when the RULs of the TFCC are torn. ECU and pronator quadratus muscles play an important role in dynamically stabilizing the DRUJ. A biomechanical study demonstrated that there are substantial changes in the moment arm of the ECU after release of the TFCC from its ulnar attachment, leading to mechanical advantage of the ECU tendon.28 In one in vivo study, which investigated the function of the pronator quadratus by electromyographic analysis, the authors concluded that the deep head of the pronator quadratus muscle may act as a dynamic DRUJ stabilizer.7
Physical Examination
Patients with DRUJ instability often complain of a painful clunking (slack) sensation, which is noticeable when twisting the forearm or when they press both hands on a table with the forearm pronated and push themselves to standing from a seated position (press test).29 A positive ulnar fovea sign consists of exquisite tenderness in the ulnar fovea, which is the depression between the ulnar styloid base and flexor carpi ulnaris tendon, and comparisons are made with the contralateral side. The sensitivity of the fovea sign in detecting foveal disruptions and/or ulnotriquetral ligament injuries is 95%, and its specificity is 87%.30
Instability of the DRUJ has been assessed by manual stress tests such as the ballottement test and the piano key sign test. The DRUJ ballottement test is a passive mobility test that examines the dosopalmar laxity of the DRUJ with the forearm in neutral rotation.31 32 The sensitivity of the DRUJ ballottement test as a means of diagnosing a complete peripheral tear of the TFCC is 59%, and the specificity is 96%.33 Nakamura proposed criteria for assessing DRUJ instability using the DRUJ ballottement test.34 The instability is rated as grade 3 when there is gross instability without end point in both the palmar and dorsal directions. Grade 2 instability is when the examiner identifies instability with a lack of end point in either the palmar or dorsal direction, and grade 1 instability is when the instability of the affected side is greater than that of the contralateral side with solid end points.
We recommend that the carpal bones should be manually held against the radius during the ballottement test to improve accuracy and reliability. The DRUJ provocative test separately conducted during forearm pronation or supination can detect which limb of the palmar or dorsal RUL is disrupted.22 When abnormal translation of the ulnar head to the palmar side is positive during maximum forearm supination, a tear in the dorsal deep or palmar superficial limb of the RUL is suspected, and when dorsal translation during maximum pronation is positive, a palmar deep or dorsal superficial RUL tear is suspected.
Plain Radiographs
Radiographic findings that suggest DRUJ instability include dorsal subluxation of the ulnar head in the lateral view and DRUJ widening during forearm pronation in the clenched-fist posteroanterior (PA) view.35 36 Nakamura et al35 evaluated radiographic subluxation of the DRUJ in patients with unilateral wrist injury and reported that DRUJ dislocation was associated with greater than 5 mm dorsal shifts of the ulnar head on lateral wrist radiographs. These criteria can be used to evaluate static dorsal dislocation of the ulnar head in relation to the radius, but lateral radiographic views are not accurate for the diagnosis of DRUJ subluxation because as little as 10 degrees of rotation can make the joint appear reduced even when the joint is dislocated. Iida et al36 examined 30 patients with chronic RUL injury to determine the reliability and efficacy of clenched-fist stress radiographs in patients with RUL injury. The DRUJ gap distance observed in clenched-fist PA views of injured wrists was significantly greater than in the same views of the contralateral side. Moreover, the DRUJ gap distance significantly correlated with the magnitude of the radioulnar ratio in forearm pronation. The authors recommended that patients with a positive piano key sign, in whom dorsal subluxation of the ulnar head in forearm pronation is observed, would be good candidates for DRUJ gap distance measurement in clenched-fist PA views.
Computed Tomography
CT can be used to evaluate DRUJ congruency using several measurement methods. Mino et al proposed the use of the palmar and dorsal radioulnar lines and considered the location of the ulnar head outside of these lines' borders to be suggestive of instability.11 However, the radioulnar line method is unreliable for the diagnosis of subluxation of the DRUJ because of an unacceptably high rate of false-positive results. Wechsler et al described the epicenter and congruency methods as a solution to the limitations of using radioulnar lines; in their method, the center of rotation (epicenter) was defined as the halfway point between the center of the ulnar head and that of the ulnar styloid and was used as a reference point.14 Lo et al proposed the radioulnar ratio method, in which the center of the ulnar head was identified using a template of concentric circles, and the radioulnar ratio was measured on the basis of the location of the center of the ulnar head relative to the sigmoid notch.13 Lo et al demonstrated that the radioulnar ratio method more sensitively detected subtle instabilities in their laboratory-induced instability model.
Several studies have investigated the reliability and normal values of various CT methods for quantifying DRUJ translation. Park and Kim compared the intra- and inter-rater reliability among four measurement techniques, including their modification of Mino's subluxation ratio method.12 They suggested that the subluxation ratio method was the most reliable technique for measuring DRUJ translation and concluded that substantial variations in normal values should be considered when performing CT evaluations of symptomatic patients. Recently, Wijffels et al37 evaluated the reliability and normal ranges of CT-based measurement methods for determination of DRUJ translation in both posttraumatic and uninjured wrists. Although DRUJ instability measurements in pronosupination were reliable in both normal and posttraumatic wrists, the epicenter method seemed the most reliable for scoring DRUJ translation in the injured wrist. The authors concluded that scanning both wrists to compare the bilateral wrist may be helpful for preventing radiological overestimation of instability.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is useful to evaluate ligamentous tears of the TFCC; however, its sensitivity and specificity are variable. Reported diagnostic test sensitivities and specificities range from 17 to 94% and from 75 to 94%, respectively.38 39 40 41 Oneson et al38 reported a 25 to 50% correlation between ulnar-sided TFCC tears on MRIs and positive arthroscopic findings. Magnetic resonance arthrography, high-resolution images of 3-T MRI, and use of microscopy coils have improved accuracy over conventional MRI. A focal area of high signal intensity at the ulnar fovea is a useful MRI finding for detecting foveal avulsion injury of the TFCC in coronal plane T2* or fat-saturation T2-weighted images (Fig. 2). Although the reliability of MRI interpretation is relatively low (slight to substantial agreement), the absence of continuity of a low signal band between the radius and ulna may be a specific finding useful for distinguishing partial from complete TFCC ligament tears.
Fig. 2.

(Left) Preoperative MRI showing a focal high-intensity signal at the fovea, demonstrating complete avulsion of the radioulnar ligaments from the ulnar fovea. (Right) Postoperative MRI showing successful healing of the ligamentous attachment following open surgery. MRI, magnetic resonance imaging.
Subluxation of the ulnar head can predict RUL tears using transaxial MRIs at the level of the DRUJ with the wrist in pronation. A retrospective study evaluating ulnar head subluxation in a total of 34 patients with intraoperatively confirmed tears of the foveal attachment of the TFCC revealed a mean dorsal ulnar subluxation measurement of 16 ± 4%, whereas the 11 controls had a mean subluxation measurement of 5 ± 4%.42
Computed Tomography Arthrography
A retrospective study of 33 patients with suspected TFCC foveal tears who had undergone wrist CT arthrography investigated the diagnostic accuracy of this technique for detecting tears.3 43 CT arthrography with a radial plane view exhibited enhanced specificity and positive predictive value when a type 3 or 4 lesion (type 3, a roundish defect at the fovea, and type 4, a large defect at the overall ulnar insertion) was identified in the detection of a TFCC foveal tear compared with historical controls.
Ultrasound
An ultrasonographic study tried to quantify DRUJ instability using 40 healthy volunteers and 17 patients with complete rupture of the TFCC.44 The authors investigated the dorsal translation ratio of the ulnar head while actively pressing the volar surface of the hand onto a brick. The translation ratios of the 17 patients with unilateral TFCC lesions were significantly different between the injured and uninjured wrists. There were no significant between side (right/left or dominant/nondominant) differences in the ratios of the 40 healthy volunteers. The authors reported that an absolute difference of more than 1 mm (injured vs. contralateral healthy side) using their method was highly suggestive of DRUJ instability.
Arthroscopy
Wrist arthroscopy provides a diagnostic and therapeutic modality in patients with symptomatic articular disc tears of the TFCC, as well as ligamentous tears causing DRUJ instability. Avulsion of the RULs at the ulnar fovea may result in DRUJ instability,16 and arthroscopy allows surgeons to diagnose the ligament tear by either indirect or direct techniques. Indirect techniques for the diagnosis include loss of the trampoline effect and the presence of a positive hook test,45 46 and direct DRUJ arthroscopy provides direct visualization of the foveal attachment of the ligaments.47 Recent advances in arthroscopic techniques have enabled minimally invasive ligament repair and arthroscopically assisted reconstruction of the TFCC ligaments.48 49
Biomechanical Perspectives on Distal Radioulnar Joint Instability
Physiological translation of the ulnar head relative to the radius may be influenced by loss of ligamentous support around the DRUJ, and the relative contributions of each ligament to joint stability have not been completely elucidated. We have conducted several experimental studies to determine the contribution of each ligament to DRUJ stability and to evaluate changes in joint stability in different forearm and wrist positions.6 50 51
Physiological Dynamic Translation of the Distal Radioulnar Joint
There is physiological translation of the DRUJ in the axial plane during active pronosupination of the forearm. In a normal wrist, the center of the ulnar head is located at the center of the sigmoid notch of the radius when the forearm is in neutral rotation. Based on the data derived from a study by Lo et al using a normal population, 10% dorsopalmar translation of the ulnar head occurs relative to the radius (10% of the dorsopalmar length of the sigmoid notch) during active pronosupination movements.13 Because the dorsopalmar length of the sigmoid notch is approximately 18 mm, the magnitude of dorsopalmar translation during active pronation and supination is 2 mm in each direction.
There is physiological laxity of the DRUJ in the axial plane when dorsoplamar forces are applied. This laxity varies depending on the forearm rotation. Based on the current authors' data using cadaver specimens without joint capsules, DRUJ laxity averaged 7 mm when 40 N of force was applied with the forearm in neutral rotation.6 The laxity decreased in pronation (6 mm) and supination (4 mm, p < 0.05) due to the checkrein effect of tightening of the superficial RUL as well as cam effect of osseous structure of the DRUJ (Table 2).
Table 2. Magnitude of DRUJ translation in specific wrist and forearm positions (mm) (average ± SD, n = 9).
| Neutral | Extension | Rad. deviation | Pronation | Supination | |
|---|---|---|---|---|---|
| Normal wrists | 7 ± 3 | – | – | 6 ± 5 | 4 ± 5a |
| Normal wrists | 7 ± 3 | 5 ± 2a | 5 ± 2 | – | – |
| UCL cut | 7 ± 3 | 7 ± 3 | 6 ± 3 | – | – |
| RUL cutb | 14 ± 4 | 12 ± 3 | 10 ± 4a | – | – |
| ECU-floor cutb | 20 ± 7 | 21 ± 7 | 21 ± 7 | – | – |
Abbreviations: DRUJ, distal radioulnar joint; ECU-floor, sheath floor of extensor carpi ulnaris tendon; RUL, radioulnar ligaments complex; SD, standard deviation; UCL, ulnocarpal ligaments complex.
Statistically significant difference from neutral position data in the same row.
Statistically significant difference from data in the upper column.
Changes in Translation after Sequential Ligament Sectioning
We investigated DRUJ stability in different wrist positions and examined the relative contribution of each ligamentous component of the TFCC to joint stability with applying 40 N of force of dorsopalmar translation of the ulna with respect to the radius.25 The magnitudes of displacement while in a neutral wrist position were compared with the intact wrists (7 mm of translation) and those at various stages of sequential ligament sectioning: UCL sectioned, RUL sectioned, and ECU floor sectioned (Table 2). UCL sectioning only had no significant influence on joint stability in a neutral position (7 mm). After sequential RUL sectioning, the displacement increased significantly (14 mm), and a more significant increase in joint instability was found following sectioning of the ECU floor (20 mm).
Changes in Translation at Specific Wrist Positions
DRUJ stability was compared at different wrist positions. The magnitude of dorsopalmar translation of the radiocarpal unit relative to the ulna in the various wrist positions at different stages of sectioning of the soft tissue was compared with the intact in the neutral position. Wrist position significantly influenced the displacement (Table 2). In intact wrists, the displacement in wrist extension was significantly lower than when the wrist was in a neutral position. However, after UCL sectioning, there were no longer any significant differences. After sequential RUL sectioning, the displacement in radial deviation was also significantly lower than when the wrist was in a neutral position. Following sequential ECU floor sectioning, there were no longer any significant differences. Thus, in intact wrists, DRUJ stability during wrist extension is likely due to tightening of the UCL. After complete RUL sectioning, the DRUJ is stabilized in radial deviation due to tightening of the ECU floor.
Contributions of the TFCC and DIOM to Dorsopalmar DRUJ Dislocation
Palmar and dorsal DRUJ dislocation was observed either in dorsal and palmar displacement (Fig. 3). Compared with the dorsal (3 mm) and palmar (4 mm) translation of the DRUJ in the intact wrists, dorsal dislocation of the ulnar head was observed following complete TFCC sectioning (10 mm translation), but there were no significant differences in palmar translation of the ulnar head (5 mm). After additional sectioning of the DIOM, significant differences in both dorsal (23 mm) and palmar (17 mm) translation were found, and bidirectional dislocation of the DRUJ was observed (Table 3). As the DOB, which is a thickened fiber of the DIOM, originates from the distal one-sixth of the ulnar shaft and runs distally to insert on the dorsal inferior rim of the sigmoid notch of the radius, the DIOM may reinforce the function of the deep limb of the dorsal RULs. The DIOM may act as a static stabilizer of the DRUJ when the RULs of the TFCC are torn.
Fig. 3.
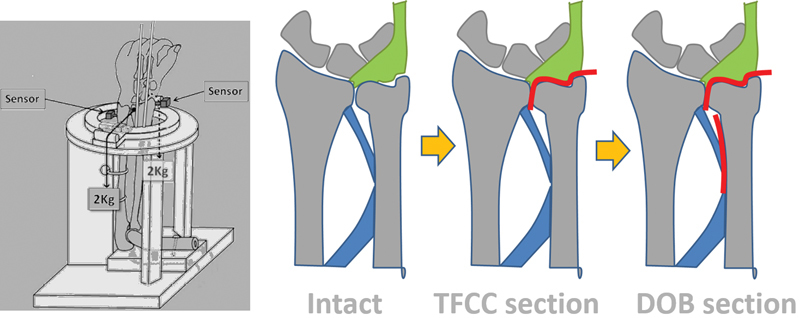
(Left) Schematic drawing of the experimental setup. (Right) Schematic drawing of sequential sectioning of the TFCC, followed by DOB sectioning. DOB, distal oblique bundle; TFCC, triangular fibrocartilage complex.
Table 3. Magnitude of dorsal and palmer translation of DRUJ (mm) (average ± SD, n = 10).
Abbreviations: DOB, distal oblique bundle of interosseous membrane; DRUJ, distal radioulnar joint; SD, standard deviation; TFCC, triangular fibrocartilage complex.
Statistically significant difference from normal wrist data in the same column.
Technique and Biomechanics of the DRUJ Ballottement Test
Technique
A previous biomechanical study using cadaver wrists demonstrated that, compared with other manual stress tests, the DRUJ ballottement test was the most accurate for evaluating instability.50 The DRUJ ballottement test is usually conducted with the forearm in neutral rotation and is interpreted as positive if the examiner identifies noticeable displacement of the radius relative to the ulnar head or a lack of end-point resistance. Examiners may recognize DRUJ instability depending on the magnitude of movement of the examiner's fingernail grasping the ulnar head and the radius. When the fingernail movement is larger than the bony movement, examiners may overestimate the extent of DRUJ instability.
There is no established maneuver for the DRUJ ballottement test, although two have been described: holding the carpal bones with the radius (holding technique) or without (nonholding technique) during the ballottement testing.31 52 The reliability and accuracy of the DRUJ ballottement test was examined with the intact TFCC and with TFCC sectioned at the fovea.50 Before TFCC sectioning, the DRUJ movement during the holding and nonholding techniques averaged 9.8 and 10.8 mm, respectively (p < 0.05). The increase in DRUJ movement after TFCC sectioning was greater with the holding technique (average 2.3 mm) than with the nonholding technique (average 1.6 mm). The DRUJ ballottement test with magnetic markers is relatively accurate and reliable for detecting unstable joints. The holding technique should be used in assessing DRUJ instability in clinical practice (Fig. 4).
Fig. 4.

(Left) Schematic drawing of the holding technique used during the DRUJ ballottement test, demonstrating accurate testing for tears of the TFCC ligament complex. (Right) Schematic drawing of the nonholding technique used during the DRUJ ballottement test, demonstrating the possibility of assessing not only the TFCC ligaments but also the radiocarpal ligament complex. DRUJ, distal radioulnar joint; TFCC, triangular fibrocartilage complex.
Wrist and Forearm Position during the Ballottement Test
Forearm pronosupination: Kleinman22 proposed a DRUJ provocative test to detect RUL tears in either the palmar or dorsal limb of the RUL separately. When abnormal and painful translation of the ulnar head to the palmar side is positive during maximum forearm supination, rupture of the dorsal deep fibers of the RUL is suspected, and when dorsal translation is positive during maximum pronation, either palmar deep limb rupture of the RUL is suspected.
Wrist extension and radial deviation: Our previous biomechanical study revealed that wrist position significantly influenced DRUJ laxity,25 DRUJ was more stable in wrist extension than neutral position before the UCL sectioning. After the UCL sectioning, there were no longer any significant differences in laxity. These results suggest that the ballottement test in wrist extension may detect UCL tears. After sectioning of the RULs, the DRUJ laxity in radial deviation was significantly lower than when in a neutral position. After sectioning of the ECU floor, there were no longer any significant differences. The DRUJ is stabilized in radial deviation due to tightening of the ECU floor. Thus, the ballottement test with the wrist in radial deviation may detect disruption of the ECU floor. When an examiner identifies DRUJ laxity and the patient complains of ulnodorsal wrist pain during the testing conducted with the wrist in radial deviation, a tear of the ECU floor should be suspected.
Acknowledgments
The authors would like to acknowledge Dr. Mitsuhiro Aoki, Dr. Pasuk Mahakkanukrauh, and Dr. Mineko Fujimiya for providing their cadaver specimens and for helping the authors' experimental works related to wrist biomechanics.
Footnotes
Conflict of Interest None.
References
- 1.Daneshvar P, Willing R, Pahuta M, Grewal R, King G J. Osseous anatomy of the distal radioulnar joint: an assessment using 3-dimensional modeling and clinical implications. J Hand Surg Am. 2016;41(11):1071–1079. doi: 10.1016/j.jhsa.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 2.De Smet L, Fabry G. Orientation of the sigmoid notch of the distal radius: determination of different types of the distal radioulnar joint. Acta Orthop Belg. 1993;59(3):269–272. [PubMed] [Google Scholar]
- 3.Tolat A R, Stanley J K, Trail I A. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg [Br] 1996;21(5):587–594. doi: 10.1016/s0266-7681(96)80136-7. [DOI] [PubMed] [Google Scholar]
- 4.Huang J I, Hanel D P. Anatomy and biomechanics of the distal radioulnar joint. Hand Clin. 2012;28(2):157–163. doi: 10.1016/j.hcl.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Hagert E, Hagert C G. Understanding stability of the distal radioulnar joint through an understanding of its anatomy. Hand Clin. 2010;26(4):459–466. doi: 10.1016/j.hcl.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Iida A, Omokawa S, Moritomo H. et al. Biomechanical study of the extensor carpi ulnaris as a dynamic wrist stabilizer. J Hand Surg Am. 2012;37(12):2456–2461. doi: 10.1016/j.jhsa.2012.07.042. [DOI] [PubMed] [Google Scholar]
- 7.Gordon K D, Dunning C E, Johnson J A, King G J. Influence of the pronator quadratus and supinator muscle load on DRUJ stability. J Hand Surg Am. 2003;28(6):943–950. doi: 10.1016/s0363-5023(03)00487-8. [DOI] [PubMed] [Google Scholar]
- 8.Linscheid R L Dobyns J H Beckenbaugh R D Cooney W P III Wood M B Instability patterns of the wrist J Hand Surg Am 19838(5 Pt 2):682–686. [DOI] [PubMed] [Google Scholar]
- 9.Cooney W P III, Linscheid R L, Dobyns J H. Carpal instability: treatment of ligament injuries of the wrist. Instr Course Lect. 1992;41:33–44. [PubMed] [Google Scholar]
- 10.Larsen C F, Amadio P C, Gilula L A, Hodge J C. Analysis of carpal instability: I. Description of the scheme. J Hand Surg Am. 1995;20(5):757–764. doi: 10.1016/S0363-5023(05)80426-5. [DOI] [PubMed] [Google Scholar]
- 11.Mino D E, Palmer A K, Levinsohn E M. Radiography and computerized tomography in the diagnosis of incongruity of the distal radio-ulnar joint. A prospective study. J Bone Joint Surg Am. 1985;67(2):247–252. [PubMed] [Google Scholar]
- 12.Park M J, Kim J P. Reliability and normal values of various computed tomography methods for quantifying distal radioulnar joint translation. J Bone Joint Surg Am. 2008;90(1):145–153. doi: 10.2106/JBJS.F.01603. [DOI] [PubMed] [Google Scholar]
- 13.Lo I K, MacDermid J C, Bennett J D, Bogoch E, King G J. The radioulnar ratio: a new method of quantifying distal radioulnar joint subluxation. J Hand Surg Am. 2001;26(2):236–243. doi: 10.1053/jhsu.2001.22908. [DOI] [PubMed] [Google Scholar]
- 14.Wechsler R J, Wehbe M A, Rifkin M D, Edeiken J, Branch H M. Computed tomography diagnosis of distal radioulnar subluxation. Skeletal Radiol. 1987;16(1):1–5. doi: 10.1007/BF00349919. [DOI] [PubMed] [Google Scholar]
- 15.Pirela-Cruz M A, Goll S R, Klug M, Windler D. Stress computed tomography analysis of the distal radioulnar joint: a diagnostic tool for determining translational motion. J Hand Surg Am. 1991;16(1):75–82. doi: 10.1016/s0363-5023(10)80017-6. [DOI] [PubMed] [Google Scholar]
- 16.Fujitani R, Omokawa S, Akahane M, Iida A, Ono H, Tanaka Y. Predictors of distal radioulnar joint instability in distal radius fractures. J Hand Surg Am. 2011;36(12):1919–1925. doi: 10.1016/j.jhsa.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Saito T, Nakamura T, Nagura T, Nishiwaki M, Sato K, Toyama Y. The effects of dorsally angulated distal radius fractures on distal radioulnar joint stability: a biomechanical study. J Hand Surg Eur Vol. 2013;38(7):739–745. doi: 10.1177/1753193412473036. [DOI] [PubMed] [Google Scholar]
- 18.Nishiwaki M, Welsh M, Gammon B, Ferreira L M, Johnson J A, King G J. Volar subluxation of the ulnar head in dorsal translation deformities of distal radius fractures: an in vitro biomechanical study. J Orthop Trauma. 2015;29(6):295–300. doi: 10.1097/BOT.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 19.Dy C J, Jang E, Taylor S A, Meyers K N, Wolfe S W. The impact of coronal alignment on distal radioulnar joint stability following distal radius fracture. J Hand Surg Am. 2014;39(7):1264–1272. doi: 10.1016/j.jhsa.2014.03.041. [DOI] [PubMed] [Google Scholar]
- 20.Nakamura T, Yabe Y, Horiuchi Y. Functional anatomy of the triangular fibrocartilage complex. J Hand Surg [Br] 1996;21(5):581–586. doi: 10.1016/s0266-7681(96)80135-5. [DOI] [PubMed] [Google Scholar]
- 21.Nakamura T, Yabe Y. Histological anatomy of the triangular fibrocartilage complex of the human wrist. Ann Anat. 2000;182(6):567–572. doi: 10.1016/S0940-9602(00)80106-5. [DOI] [PubMed] [Google Scholar]
- 22.Kleinman W B. Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am. 2007;32(7):1086–1106. doi: 10.1016/j.jhsa.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 23.Benjamin M, Evans E J, Pemberton D J. Histological studies on the triangular fibrocartilage complex of the wrist. J Anat. 1990;172:59–67. [PMC free article] [PubMed] [Google Scholar]
- 24.Moritomo H. Anatomy and clinical relevance of the ulnocarpal ligament. J Wrist Surg. 2013;2(2):186–189. doi: 10.1055/s-0033-1345023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iida A, Omokawa S, Moritomo H. et al. Effect of wrist position on distal radioulnar joint stability: a biomechanical study. J Orthop Res. 2014;32(10):1247–1251. doi: 10.1002/jor.22669. [DOI] [PubMed] [Google Scholar]
- 26.Moritomo H. The distal interosseous membrane: current concepts in wrist anatomy and biomechanics. J Hand Surg Am. 2012;37(7):1501–1507. doi: 10.1016/j.jhsa.2012.04.037. [DOI] [PubMed] [Google Scholar]
- 27.Moritomo H. The distal oblique bundle of the distal interosseous membrane of the forearm. J Wrist Surg. 2013;2(1):93–94. doi: 10.1055/s-0032-1333428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang J B, Ryu J, Kish V. The triangular fibrocartilage complex: an important component of the pulley for the ulnar wrist extensor. J Hand Surg Am. 1998;23(6):986–991. doi: 10.1016/S0363-5023(98)80004-X. [DOI] [PubMed] [Google Scholar]
- 29.Lester B, Halbrecht J, Levy I M, Gaudinez R. “Press test” for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg. 1995;35(1):41–45. doi: 10.1097/00000637-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Tay S C, Tomita K, Berger R A. The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg Am. 2007;32(4):438–444. doi: 10.1016/j.jhsa.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 31.King G J, McMurtry R Y. Philadelphia: WB Saunders; 1996. Physical examination of the wrist and hand; pp. 5–18. [Google Scholar]
- 32.Cooney W P, Bishop A T, Linscheid R L. Philadelphia: Lippincott Williams and Wilkins; 1998. Physical examination of the wrist; pp. 236–261. [Google Scholar]
- 33.Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am. 2000;25(3):464–468. doi: 10.1053/jhsu.2000.6467. [DOI] [PubMed] [Google Scholar]
- 34.Nakamura T. Pathology, diagnosis and treatment of distal radioulnar ligament instability [in Japanese] J Jpn Orthop Assoc. 2008;82(2):90–90. [Google Scholar]
- 35.Nakamura R, Horii E, Imaeda T, Tsunoda K, Nakao E. Distal radioulnar joint subluxation and dislocation diagnosed by standard roentgenography. Skeletal Radiol. 1995;24(2):91–94. doi: 10.1007/BF00198067. [DOI] [PubMed] [Google Scholar]
- 36.Iida A, Omokawa S, Akahane M, Kawamura K, Takayama K, Tanaka Y. Distal radioulnar joint stress radiography for detecting radioulnar ligament injury. J Hand Surg Am. 2012;37(5):968–974. doi: 10.1016/j.jhsa.2012.01.041. [DOI] [PubMed] [Google Scholar]
- 37.Wijffels M, Stomp W, Krijnen P, Reijnierse M, Schipper I. Computed tomography for the detection of distal radioulnar joint instability: normal variation and reliability of four CT scoring systems in 46 patients. Skeletal Radiol. 2016;45(11):1487–1493. doi: 10.1007/s00256-016-2455-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oneson S R, Timins M E, Scales L M, Erickson S J, Chamoy L. MR imaging diagnosis of triangular fibrocartilage pathology with arthroscopic correlation. Am J Roentgenol. 1997;168(6):1513–1518. doi: 10.2214/ajr.168.6.9168716. [DOI] [PubMed] [Google Scholar]
- 39.Haims A H, Schweitzer M E, Morrison W B. et al. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. Am J Roentgenol. 2002;178(2):419–422. doi: 10.2214/ajr.178.2.1780419. [DOI] [PubMed] [Google Scholar]
- 40.Blazar P E, Chan P S, Kneeland J B, Leatherwood D, Bozentka D J, Kowalchick R. The effect of observer experience on magnetic resonance imaging interpretation and localization of triangular fibrocartilage complex lesions. J Hand Surg Am. 2001;26(4):742–748. doi: 10.1053/jhsu.2001.24966. [DOI] [PubMed] [Google Scholar]
- 41.Anderson M L, Skinner J A, Felmlee J P, Berger R A, Amrami K K. Diagnostic comparison of 1.5 tesla and 3.0 tesla preoperative MRI of the wrist in patients with ulnar-sided wrist pain. J Hand Surg Am. 2008;33(7):1153–1159. doi: 10.1016/j.jhsa.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 42.Ehman E C, Hayes M L, Berger R A, Felmlee J P, Amrami K K. Subluxation of the distal radioulnar joint as a predictor of foveal triangular fibrocartilage complex tears. J Hand Surg Am. 2011;36(11):1780–1784. doi: 10.1016/j.jhsa.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 43.Moritomo H, Arimitsu S, Kubo N, Masatomi T, Yukioka M. Computed tomography arthrography using a radial plane view for the detection of triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2015;40(2):245–251. doi: 10.1016/j.jhsa.2014.10.051. [DOI] [PubMed] [Google Scholar]
- 44.Hess F, Farshad M, Sutter R, Nagy L, Schweizer A. A novel technique for detecting instability of the distal radioulnar joint in complete triangular fibrocartilage complex lesions. J Wrist Surg. 2012;1(2):153–158. doi: 10.1055/s-0032-1312046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hermansdorfer J D, Kleinman W B. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg Am. 1991;16(2):340–346. doi: 10.1016/s0363-5023(10)80123-6. [DOI] [PubMed] [Google Scholar]
- 46.Ruch D S, Yang C C, Smith B P. Results of acute arthroscopically repaired triangular fibrocartilage complex injuries associated with intra-articular distal radius fractures. Arthroscopy. 2003;19(5):511–516. doi: 10.1053/jars.2003.50154. [DOI] [PubMed] [Google Scholar]
- 47.Nakamura T, Iwamoto T, Matsumura N, Sato K, Toyama Y. Radiographic and arthroscopic assessment of DRUJ instability due to foveal avulsion of the radioulnar ligament in distal radius fractures. J Wrist Surg. 2014;3(1):12–17. doi: 10.1055/s-0033-1364175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Atzei A, Rizzo A, Luchetti R, Fairplay T. Arthroscopic foveal repair of triangular fibrocartilage complex peripheral lesion with distal radioulnar joint instability. Tech Hand Up Extrem Surg. 2008;12(4):226–235. doi: 10.1097/BTH.0b013e3181901b1. [DOI] [PubMed] [Google Scholar]
- 49.Tse W L, Lau S W, Wong W Y. et al. Arthroscopic reconstruction of triangular fibrocartilage complex (TFCC) with tendon graft for chronic DRUJ instability. Injury. 2013;44(3):386–390. doi: 10.1016/j.injury.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 50.Onishi T, Omokawa S, Iida A. et al. Biomechanical study of distal radioulnar joint ballottement test. J Orthop Res. 2016 doi: 10.1002/jor.23355. [DOI] [PubMed] [Google Scholar]
- 51.Moriya T, Aoki M, Iba K, Ozasa Y, Wada T, Yamashita T. Effect of triangular ligament tears on distal radioulnar joint instability and evaluation of three clinical tests: a biomechanical study. J Hand Surg Eur Vol. 2009;34(2):219–223. doi: 10.1177/1753193408098482. [DOI] [PubMed] [Google Scholar]
- 52.Szabo R M. Distal radioulnar joint instability. J Bone Joint Surg Am. 2006;88(4):884–894. doi: 10.2106/00004623-200604000-00027. [DOI] [PubMed] [Google Scholar]


