Abstract
Background We sought to evaluate the interobserver and intraobserver reliability of radiographs and magnetic resonance imaging (MRI) for grading of osteoarthritis in patients with scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC), and to determine whether MRI is more likely than radiographs to detect carpal osteoarthritis.
Methods Radiographs and MR studies of 46 patients with SLAC and SNAC arthritis were reviewed by two hand surgeons and two radiologists and were graded according to severity of osteoarthritis at seven carpal joints. Interobserver and intraobserver reliability was assessed using a weighted kappa analysis. Odds ratios were calculated to compare the likelihood of MRI versus radiographs in the determination of moderate or severe osteoarthritis.
Results Measures of reliability were higher for MRI than radiographs. For radiographic assessment of all patients combined, interobserver agreement was moderate and intraobserver agreement was also moderate. For MRI, interobserver agreement was substantial and intraobserver agreement was almost perfect. In all joints combined for patients with SLAC and SNAC, MRI was 2.42 times more likely to demonstrate moderate osteoarthritis compared with radiographs. In patients with SLAC, MRI was 11.73 times more likely than radiographs to show moderate osteoarthritis at the radiolunate joint. In patients with SNAC, there was no difference in demonstration of moderate osteoarthritis on MRI compared with radiographs.
Conclusion Carpal osteoarthritis can be more reliably assessed on MRI than radiographs. MRI is more sensitive at demonstrating moderate changes of osteoarthritis than radiographs, especially at the radiolunate joint in patients with SLAC arthritis. This has implications for surgical management of SLAC/SNAC arthritis and preoperative planning. MRI should be included in the diagnostic workup and evaluation of patients with SLAC and SNAC arthritis.
Level of Evidence Diagnostic III.
Keywords: scapholunate advanced collapse, scaphoid nonunion advanced collapse, magnetic resonance imaging, radiographs
Scapholunate advanced collapse (SLAC) is one of the more common forms of arthritis of the wrist and follows a predictable pattern of joint degeneration initiated by complete rupture of the scapholunate interosseous ligament.1 A similar pattern was subsequently identified in patients with chronic scaphoid nonunion, termed scaphoid nonunion advanced collapse (SNAC).2 Less common causes of wrist osteoarthritis (OA) include distal radius malunion, avascular necrosis of the scaphoid or lunate, Kienbock disease, and crystalline arthropathy.3 4
Nonsurgical treatment for SLAC and SNAC arthritis includes lifestyle modification, nonsteroidal anti-inflammatory medications, splints and casts, and intra-articular corticosteroid injections for symptomatic relief. Surgical treatment of SLAC or SNAC arthritis includes neurectomy, radial styloidectomy, four-corner arthrodesis, proximal row carpectomy (PRC), radiocarpal arthrodesis, or wrist arthoplasty.5 6 7 Four-corner arthrodesis, radiocarpal arthrodesis, and wrist arthroplasty are salvage procedures that can be considered when other treatment modalities fail. Radial styloidectomy, with or without denervation, can be performed in patients with early arthritis limited to the radial styloid.
PRC involves excision of the scaphoid, lunate, and triquetrum. Following the procedure, the capitate articulates with the lunate fossa of the radius. A major complication is subsequent development of radiocapitate OA. Chondral loss at the capitate head articular surface is the main contraindication to PRC, although the degree of chondral preservation required for a successful procedure is debated.8 9 Four-corner arthrodesis involves excision of the scaphoid and intercarpal arthrodesis of the capitate, lunate, hamate, and triquetrum. Typically, autologous bone graft is used in conjunction with internal fixation. The procedure is more likely to succeed when the radiolunate articular surface is pristine. The decision to perform PRC or four-corner fusion depends on the status of the capitate and lunate articular surface. Total wrist arthrodesis may be elected if both the capitolunate and radiolunate joints are compromised.
Traditionally, preoperative radiographs have been used to determine the likelihood of capitolunate and radiolunate OA when deciding between the various surgical alternatives. Radiographic evaluation relies on detection of joint space narrowing and the secondary osseous changes of subchondral sclerosis and osteophyte formation. Magnetic resonance imaging (MRI) has been shown to be reliable in evaluation of chondral defects in large joints such as the knee and hip when compared with arthroscopy as the gold standard.10 11 12 In addition to evaluation of ligaments, synovium, and bone marrow, the assessment of cartilage thickness and chondral defects on MRI is useful in the preoperative evaluation and surgical planning.
The purpose of this study was to, first, evaluate the interobserver and intraobserver reliability of radiographs and MRI for grading of OA in patients with SLAC and SNAC and, second, to determine whether MRI is more likely than radiographs to detect carpal OA in these patients. We hypothesized that MRI is at least as reliable as radiographs in evaluation of carpal OA and is more likely to demonstrate moderate arthritis compared with radiographs.
Methods
This retrospective study was approved by the Institutional Review Board. Patients over the age of 18 who had wrist radiographs and MRI from 2007 to 2014 at our institution with a diagnosis of SLAC or SNAC arthritis were included in the study. The patients were identified from a database containing reports of all MRI examinations performed at our institution. A search of MRI reports was made for the terms “SLAC,” “scapholunate advanced collapse,” “SNAC,” or “scaphoid non-union advanced collapse,” combined with a search of the study type “MRI wrist.” Patients who did not have posteroanterior (PA), lateral, and oblique radiographs of the ipsilateral wrist were excluded. Patients who had a known diagnosis of inflammatory arthritis or crystalline arthropathy were excluded.
A total of 23 patients with SLAC arthritis and 23 patients with SNAC arthritis met the inclusion criteria. Overall, the mean age was 50 years (range: 17–75), with 34 (74%) males and 12 (26%) females. Of them, 25 (54%) right hands included, and average time between radiograph and MRI was 44 days (range: 0–444). Patient demographics are given in Table 1.
Table 1. Patient demographics.
| All patients (n = 46) | SLAC (n = 23) | SNAC (n = 23) | |
|---|---|---|---|
| Age | Mean 50 (range 17–75) | Mean 60 (range 40–73) | Mean 39 (range 17–75) |
| Sex (M:F) | 34:12 | 15:8 | 20:3 |
| Hand involved (right:left) | 25:21 | 14:9 | 11:12 |
| Traditional radiographic SLAC1 or SNAC2 stage | 0: 3 I: 3 II: 7 III: 9 IV: 1 |
0: 4 I: 10 II: 1 III: 8 IV: 0 |
|
| Scaphoid fracture location | Proximal: 4 Middle: 18 Distal: 1 |
Abbreviations: SNAC, scaphoid nonunion advanced collapse; SLAC, scapholunate advanced collapse.
The wrist radiographs were evaluated by two board-certified hand surgeons independently, blinded to the MRI findings. Each surgeon read the radiographs twice, at least 3 weeks apart. The distal radioscaphoid, proximal radioscaphoid, capitolunate, radiolunate, scaphotrapeziotrapezoidal (STT), and hamatotriquetral joints were evaluated on PA, oblique, and lateral radiographs for joint space narrowing, osteophytes, subchondral sclerosis, and cysts on radiographs. Each joint was graded according to a modified Kellgren–Lawrence scale13 for OA as follows: grade 1, no evidence of OA; grade 2, minimal OA with definite osteophytes or joint space narrowing; grade 3, moderate OA with multiple osteophytes, definite joint space narrowing, some sclerosis, and possible changes in bone contour; grade 4, severe OA with large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity in bone contour. For patients with SNAC, the location of the fracture was documented as being in the distal, middle (waist), or proximal scaphoid.
All patients were scanned using the standardized protocol for MRI of the wrist at our institution. MRI was performed on either a 1.5 T (41/46 patients) or 3.0 T (5/46 patients) superconducting magnet with a surface coil without the use of intravenous contrast. For studies performed at 1.5 T, axial, coronal and sagittal fast spin-echo sequences were acquired with the following parameters—time to repetition (TR): 4,000 to 5,000 ms; echo time (TE): 24 ms; echo train length (ETL): 7 to 12; receiver bandwidth (RBW): 31.25 kHz; number of excitations (NEX): 2; matrix: 512 × 320 or 512 × 256; field of view (FOV): 8 to 9 cm, slice thickness: 3 to 4 mm; and no interslice gap. A volumetric coronal gradient recalled echo sequence was performed with the following parameters—TR 40 ms; TE 20 ms; flip angle: 10 degrees; RBW: 15.63 kHz; NEX: 2; matrix: 256 × 256; FOV: 8 cm; slice thickness: 1 mm; and no interslice gap. A coronal inversion recovery scan was obtained with the following parameters—TR: 4,000 ms; TE: 17 ms, inversion time (TI): 150 ms; ETL: 9; RBW: 31.25 kHz; NEX: 2; matrix: 256 × 192; FOV: 9 cm; slice thickness: 2.5 mm; and no interslice gap. Total imaging time was approximately 30 minutes. For studies performed at 3.0 T, axial, coronal, and sagittal fast spin-echo sequences were acquired with the following parameters—TR: 3,800 to 4,000 ms; TE: 29 ms; ETL: 10; RBW: 50 kHz; NEX: 2; matrix: 512 × 320 or 512 × 416; FOV: 8 cm; slice thickness: 2.0 to 2.5 mm; and no interslice gap. A volumetric coronal gradient recalled echo sequence was performed with the following parameters—TR: 35 ms; TE: 20 ms; flip angle: 10 degrees; RBW: 31.25 kHz; NEX: 2; matrix: 256 × 256; FOV: 8 cm; slice thickness: 1 mm; and no interslice gap. A coronal inversion recovery scan was obtained with the following parameters—TR: 5,900 ms; TE: 17 ms; TI: 170 ms; NEX: 2; matrix: 288 × 192; FOV: 9 to 10 cm; slice thickness: 2.5 to 3.0 mm; and no interslice gap. Total imaging time was approximately 30 minutes.
The MR studies were interpreted by two musculoskeletal radiologists independently, blinded to the radiograph findings. One radiologist read the MRI studies a second time, 2 months later. The distal radioscaphoid, proximal radioscaphoid, capitolunate, radiolunate, scaphocapitate, STT, pisotriquetral, and hamatotriquetral joints were assessed using the coronal, axial, and sagittal fast spin-echo images. For each joint component, a cartilage score was assigned based on the most advanced chondral lesion detected. The following grading system was used: grade 1, normal; grade 2, mild chondral wear (<50% of the cartilage thickness); grade 3, deep chondral wear (>50% of the thickness of cartilage) up to full thickness chondral loss involving less than 25% of the articular surface; grade 4, full thickness chondral loss involving greater than 25% of the articular surface.
Weighted Cohen's kappa (kw) analysis was performed to assess the interobserver and intraobserver reliability for radiographs, and the interobserver reliability for MRI. The interpretation of the kappa value was as follows—0.00 to 0.20: slight; 0.21 to 0.40: fair; 0.41 to 0.60: moderate; 0.61 to 0.80: substantial; and 0.81 to 1.00: almost perfect agreement.14 Odds ratios were performed to compare the likelihood of radiograph or MRI classifying a joint as moderately osteoarthritic (based on grade 3 on radiograph or MRI). The first reads of the senior surgeon and senior radiologist were used for the odds-ratio analysis.
Results
Interobserver and intraobserver reliability were higher for MRI than radiographs. For all patients combined, interobserver and intraobserver agreement were 0.54 to 0.56 and 0.50 to 0.63, respectively, for radiographs, and 0.75 and 0.81, respectively, for MRI. Measures of agreement were generally higher for SNAC compared with SLAC. For SLAC, interobserver and intraobserver agreement were 0.34 to 0.52 and 0.50 to 0.63, respectively, for radiographs, and 0.62 and 0.67, respectively, for MRI. For SNAC, interobserver and intraobserver agreement were 0.57 to 0.66 and 0.54 to 0.60, respectively, for radiographs, and 0.76 and 0.83, respectively, for MRI. These kappa values are summarized in Tables 2 and 3.
Table 2. Measures of interobserver agreement for grading of osteoarthritis on MRI and radiographs.
| All patients | SLAC | SNAC | |||||
|---|---|---|---|---|---|---|---|
| Kappa (kw) | Interpretation | Kappa (kw) | Interpretation | Kappa (kw) | Interpretation | ||
| Radiographs | First read | 0.56 | Moderate | 0.52 | Moderate | 0.57 | Moderate |
| Second read | 0.54 | Moderate | 0.34 | Fair | 0.66 | Substantial | |
| MRI | First reads | 0.75 | Substantial | 0.62 | Substantial | 0.76 | Substantial |
Abbreviations: MRI, magnetic resonance imaging; SNAC, scaphoid nonunion advanced collapse; SLAC, scapholunate advanced collapse.
Table 3. Measures of intraobserver agreement for grading of osteoarthritis on MRI and radiographs.
| All patients | SLAC | SNAC | |||||
|---|---|---|---|---|---|---|---|
| Kappa (kw) | Interpretation | Kappa (kw) | Interpretation | Kappa (kw) | Interpretation | ||
| Radiographs | Reader A | 0.50 | Moderate | 0.43 | Moderate | 0.54 | Moderate |
| Reader B | 0.63 | Substantial | 0.63 | Substantial | 0.60 | Moderate | |
| MRI | Reader C | 0.81 | Almost perfect | 0.67 | Substantial | 0.83 | Almost perfect |
Abbreviations: MRI, magnetic resonance imaging; SNAC, scaphoid nonunion advanced collapse; SLAC, scapholunate advanced collapse.
MRI was 4.41 times more likely to demonstrate moderate OA at all joints combined compared with radiographs in the SLAC cohort (odds ratio [OR] = 4.41; 95% CI: 2.76–7.05; p < 0.005), but not in the SNAC cohort (OR = 1.31; 95% CI: 0.81–2.13, p = 0.3). In all patients combined, MRI was 2.42 times more likely to demonstrate moderate OA compared with radiographs (OR: 2.42; 95% CI: 1.75–3.36; p < 0.005).
For the individual joints, MRI was more likely to demonstrate moderate OA at several joints in the SLAC cohort but not in the SNAC cohort. In patients with SLAC, MRI was 11.73 times more likely than radiographs to show moderate OA at the radiolunate joint (OR = 11.73; 95% CI: 1.33–103.80; p = 0.009). MRI was more likely than radiographs to demonstrate OA at the distal radioscaphoid (p = 0.02), proximal radioscaphoid (OR = 9.63; 95% CI: 1.08–86.18; p = 0.02), scaphocapitate (OR = 24; 95% CI: 2.76–209.06; p < 0.005), hamatotriquetral (p < 0.005), and STT joints (OR = 29.75; 95% CI: 5.31–166.94; p < 0.005) in SLAC patients. There was no significant difference in demonstration of OA at the capitolunate joint on MRI or radiographs in SLAC patients (OR = 1.69; 95% CI: 0.53–5.42; p = 0.4). The ORs for all joints are given in Table 4.
Table 4. Likelihood of MRI compared with radiographs for the detection of moderate osteoarthritis.
| Joints | SLAC | SNAC | All patients | |||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) |
p-Value | Odds ratio (95% CI) |
p-Value | Odds ratio (95% CI) |
p-Value | |
| All joints |
4.41
(2.76–7.05) |
<0.005 | 1.31 (0.81–2.13) |
0.268 |
2.42
(1.75–3.36) |
<0.005 |
| Distal radioscaphoid | NA a | 0.018 | 0.76 (0.18–3.23) |
0.710 | 1.62 (0.53–5.00) |
0.400 |
| Proximal radioscaphoid |
9.63
(1.08–86.18) |
0.020 | 0.50 (0.10–2.47) |
0.381 | 2.21 (0.96–5.09) |
0.061 |
| Scaphocapitate |
24.00
(2.76–209.06) |
<0.005 | 1.82 (0.52–6.37) |
0.345 |
4.68
(1.74–12.62) |
0.002 |
| Capitolunate | 1.69 (0.53–5.42) |
0.376 | 0.82 (0.24–2.82) |
0.753 | 1.20 (0.52–2.75) |
0.672 |
| Radiolunate |
11.73
(1.33–103.80) |
0.009 | NAb | 0.148 |
12.50
(1.53–102.26) |
0.004 |
| Hamatotriquetral | NA c | <0.005 | 1.00 (0.77–1.30) |
0.999 | 4.59 (1.38–15.29) |
0.009 |
| STT |
29.75
(5.31–166.94) |
<0.005 | 2.92 (0.65–13.12) |
0.153 |
8.95
(3.00–26.71) |
<0.005 |
Abbreviations: CI, confidence interval; MRI, magnetic resonance imaging; NA, not applicable; SNAC, scaphoid nonunion advanced collapse; SLAC, scapholunate advanced collapse; STT, scaphotrapeziotrapezoidal.
Note: p-Values <0.09 are significant.
Unable to calculate odds ratio as MRI demonstrated grade ≥ 3 chondral wear at the distal radioscaphoid joint in all patients with SLAC.
Unable to calculate odds ratio as radiographs demonstrated grade ≤2 osteoarthritis or less at the radiolunate joint in all patients with SNAC.
Unable to calculate odds ratio as radiographs demonstrated grade ≤2 osteoarthritis or less at the hamatotriquetral joint in all patients with SLAC.
Discussion
Preoperative assessment of carpal OA has been traditionally performed with radiographs by evaluating the secondary osseous changes of OA. Conversely, MRI allows assessment of articular cartilage, which may help guide preoperative planning. Although MRI was not more likely than radiographs to demonstrate arthritic changes at the capitolunate joint in our study, its sensitivity in better demonstrating radiolunate wear may influence the decision to perform four corner arthrodesis or total arthrodesis. These procedures differ greatly in functional outcome, and providing an accurate expectation to patients of postoperative ability to return to former active daily lifestyles warrants preoperative discussion and consent.
Evaluation of OA of the wrist on MRI is challenging as the hyaline cartilage is thin. A study of patients with lunate chondromalacia showed MRI had a sensitivity of 77% and specificity of 86% for the detection of lunate chondral defects with arthroscopy as the gold standard.15 A cadaveric study demonstrated MRI had sensitivity of 52% and specificity of 83% for the detection of moderate chondral defects in the proximal and distal carpal row.16 The lower sensitivities reported in the cadaveric study may be due to the limited MRI sequences, as only coronal sequences were acquired instead of three plane MRI sequences.
A few studies have reported variable interobserver reliability for evaluation of OA in SLAC and SNAC patients. One study showed moderate interobserver and substantial intraobserver reliability for SLAC, with kappa of 0.59 and 0.65, respectively.17 For SNAC measures of reliability were lower with slight interobserver and fair moderate interobserver agreement (kappa: 0.20 and 0.29, respectively).17 Another study demonstrated low interobserver agreement with kappa < 0.5 among five different readers, with the level of agreement being unrelated to the level of expertise of the reader.18 The authors suggested that a more reliable method than radiographic staging is required to assess OA in these patients when planning treatment. Our study differed in that we assessed measures of reliability for individual joints rather than for the SLAC or SNAC stage.
Although there are few studies reporting the interobserver reliability of MRI for evaluation of wrist cartilage in OA, the use of MRI to assess chondral thickness in rheumatoid arthritis (RA) has been reported. One study of 22 patients with RA and 22 controls reported high reliability with interobserver and intraobserver intraclass correlations of 0.91 and 0.94, respectively, for the degree of joint space narrowing on MRI.19 Our study differs in the grading system used (based on the most severe chondral lesion rather than joint space narrowing), which may account for the lower intraobserver and intraobserver reliability. Furthermore, MRI assessment of overall joint space narrowing does not imply that the cartilage is eroded or takes into account focal chondral defects, which is important in influencing the need for surgical preservation of the joint.
Use of joint space narrowing on radiographs provides an indirect assessment of cartilage thickness. On the other hand, MRI provides direct visualization and assessment of cartilage thickness and “bone-on-bone” focal chondral defects (Fig. 1). Use of MRI for the evaluation of OA of the wrist has not yet been well established, although it is well known that MRI is more sensitive compared with radiography for detection of OA in the knee.20 Radiographic changes of OA often occur later in degenerative joint disease. One longitudinal study of 224 patients reported 80 patients who developed chondral defects on MRI over a 30-month period, but did not demonstrate radiographic progression of OA.21 In this study, radiographic changes had high specificity (91%) but low sensitivity (23%) for chondral loss detected on MRI.21 The Framingham Osteoarthritis Study showed that 492 out of 710 patients with no radiographic evidence of femorotibial OA (Kellgren–Lawrence grade 0) had either focal chondral defects or areas of diffuse partial or full thickness chondral loss on MRI.22
Fig. 1.
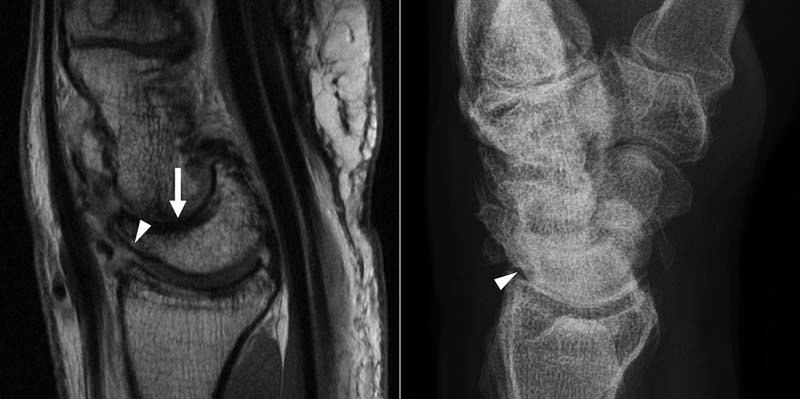
A 71-year-old man with SLAC arthritis. (A) Sagittal fast spin-echo magnetic resonance imaging demonstrates high grade to full thickness chondral loss at the dorsal margin of the radiolunate joint (arrowhead). Full thickness chondral loss is also seen at the capitolunate joint (arrow). (B) Corresponding radiograph demonstrates a normal radiolunate joint.
Chan et al showed that MRI more frequently detects tricompartmental OA of the knee whereas radiographs and computed tomography (CT) only showed bicompartmental changes, mainly because of lateral compartment chondral loss that was not detected on radiographs or CT.23 The authors proposed that this was due to coexistent medial compartment OA, which causes weight to be shifted medially, opening the lateral joint space. Thus, joint space narrowing on radiographs is influenced by the biomechanics of the joint and is not always a reliable indicator of chondral thickness. MRI has the advantage over radiographs of being able to provide three-dimensional assessment of the chondral surfaces. Radiographic assessment of carpal joints is influenced by the projection and can be limited by overlapping structures. Prior studies, for example, have noted agreement between radiographic and open assessment in only 33 to 39%24 25 of STT joints, 33%26 of capitolunate joints, and 12%26 of radiolunate joints inspected.
We concede several limitations to this study. There may have been inclusion bias as patients were selected based on findings of SLAC or SNAC arthritis on the original MRI reports, and a control group of patients was not included. Furthermore, all radiograph and MRI readers were aware that the patients had a diagnosis of either SNAC or SLAC arthritis. The number of patients in our study was relatively small, as reflected in the wide confidence intervals for the ORs. Our study also did not include arthroscopic or pathological correlation to confirm radiographic or MRI findings. Importantly, radiographic and MRI assessment of arthritic change was performed by separate observers, and thus our results may have differed if both modalities were evaluated by the same reviewer.
In conclusion, these findings, in addition to only moderate inter- and intraobserver reliability, suggest that radiographs should not be the diagnostic modality of choice when evaluating carpal OA. Given that MRI can more reliably assess articular cartilage loss than radiographs and is more likely to detect osteoarthritic changes, we recommend MRI be performed in the diagnostic workup and evaluation of patients with SLAC and SNAC arthritis.
Footnotes
Conflict of Interest None.
References
- 1.Watson H K, Ballet F L. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9(3):358–365. doi: 10.1016/s0363-5023(84)80223-3. [DOI] [PubMed] [Google Scholar]
- 2.Vender M I, Watson H K, Wiener B D, Black D M. Degenerative change in symptomatic scaphoid nonunion. J Hand Surg Am. 1987;12(4):514–519. doi: 10.1016/s0363-5023(87)80198-3. [DOI] [PubMed] [Google Scholar]
- 3.Cayci C, Carlsen B T. Osteoarthritis of the wrist. Plast Reconstr Surg. 2014;133(3):605–615. doi: 10.1097/01.prs.0000438463.90968.d6. [DOI] [PubMed] [Google Scholar]
- 4.Trehan S K, Lee S K, Wolfe S W. Scapholunate advanced collapse: nomenclature and differential diagnosis. J Hand Surg Am. 2015;40(10):2085–2089. doi: 10.1016/j.jhsa.2015.06.110. [DOI] [PubMed] [Google Scholar]
- 5.Kitay A, Wolfe S W. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2012;37(10):2175–2196. doi: 10.1016/j.jhsa.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 6.Shah C M, Stern P J. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med. 2013;6(1):9–17. doi: 10.1007/s12178-012-9149-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiss K E, Rodner C M. Osteoarthritis of the wrist. J Hand Surg Am. 2007;32(5):725–746. doi: 10.1016/j.jhsa.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Strauch R J. Scapholunate advanced collapse and scaphoid nonunion advanced collapse arthritis—update on evaluation and treatment. J Hand Surg Am. 2011;36(4):729–735. doi: 10.1016/j.jhsa.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 9.Kiefhaber T R. Management of scapholunate advanced collapse pattern of degenerative arthritis of the wrist. J Hand Surg Am. 2009;34(8):1527–1530. doi: 10.1016/j.jhsa.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 10.Bredella M A, Tirman P F, Peterfy C G. et al. Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol. 1999;172(4):1073–1080. doi: 10.2214/ajr.172.4.10587150. [DOI] [PubMed] [Google Scholar]
- 11.Mintz D N, Hooper T, Connell D, Buly R, Padgett D E, Potter H G. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy. 2005;21(4):385–393. doi: 10.1016/j.arthro.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Disler D G, McCauley T R, Wirth C R, Fuchs M D. Detection of knee hyaline cartilage defects using fat-suppressed three-dimensional spoiled gradient-echo MR imaging: comparison with standard MR imaging and correlation with arthroscopy. Am J Roentgenol. 1995;165(2):377–382. doi: 10.2214/ajr.165.2.7618561. [DOI] [PubMed] [Google Scholar]
- 13.Kellgren J H, Lawrence J S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landis J R, Koch G G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 15.Bordalo-Rodrigues M, Schweitzer M, Bergin D, Culp R, Barakat M S. Lunate chondromalacia: evaluation of routine MRI sequences. AJR Am J Roentgenol. 2005;184(5):1464–1469. doi: 10.2214/ajr.184.5.01841464. [DOI] [PubMed] [Google Scholar]
- 16.Saupe N, Pfirrmann C W, Schmid M R, Schertler T, Manestar M, Weishaupt D. MR imaging of cartilage in cadaveric wrists: comparison between imaging at 1.5 and 3.0 T and gross pathologic inspection. Radiology. 2007;243(1):180–187. doi: 10.1148/radiol.2431060294. [DOI] [PubMed] [Google Scholar]
- 17.Vishwanathan K, Hearnden A, Talwalkar S, Hayton M, Murali S R, Trail I A. Reproducibility of radiographic classification of scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist. J Hand Surg Eur Vol. 2013;38(7):780–787. doi: 10.1177/1753193413484629. [DOI] [PubMed] [Google Scholar]
- 18.Penteado F T, Dos Santos J B, Caporrino F A, de Moraes V Y, Belloti J C, Faloppa F. Scaphoid nonunion advanced collapse classifications: a reliability study. J Hand Microsurg. 2012;4(1):12–15. doi: 10.1007/s12593-012-0062-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McQueen F, Clarke A, McHaffie A. et al. Assessment of cartilage loss at the wrist in rheumatoid arthritis using a new MRI scoring system. Ann Rheum Dis. 2010;69(11):1971–1975. doi: 10.1136/ard.2009.127324. [DOI] [PubMed] [Google Scholar]
- 20.Ding C, Cicuttini F, Jones G. How important is MRI for detecting early osteoarthritis? Nat Clin Pract Rheumatol. 2008;4(1):4–5. doi: 10.1038/ncprheum0676. [DOI] [PubMed] [Google Scholar]
- 21.Amin S, LaValley M P, Guermazi A. et al. The relationship between cartilage loss on magnetic resonance imaging and radiographic progression in men and women with knee osteoarthritis. Arthritis Rheum. 2005;52(10):3152–3159. doi: 10.1002/art.21296. [DOI] [PubMed] [Google Scholar]
- 22.Guermazi A Niu J Hayashi D et al. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study) BMJ 2012345e5339. Doi: 10.1136/bmj.e5339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan W P, Lang P, Stevens M P. et al. Osteoarthritis of the knee: comparison of radiography, CT, and MR imaging to assess extent and severity. Am J Roentgenol. 1991;157(4):799–806. doi: 10.2214/ajr.157.4.1892040. [DOI] [PubMed] [Google Scholar]
- 24.Brown G D III, Roh M S, Strauch R J, Rosenwasser M P, Ateshian G A, Mow V C. Radiography and visual pathology of the osteoarthritic scaphotrapezio-trapezoidal joint, and its relationship to trapeziometacarpal osteoarthritis. J Hand Surg Am. 2003;28(5):739–743. doi: 10.1016/s0363-5023(03)00258-2. [DOI] [PubMed] [Google Scholar]
- 25.North E R, Eaton R G. Degenerative joint disease of the trapezium: a comparative radiographic and anatomic study. J Hand Surg Am. 1983;8(2):160–166. doi: 10.1016/s0363-5023(83)80008-2. [DOI] [PubMed] [Google Scholar]
- 26.Zinberg E M, Chi Y. Proximal row carpectomy versus scaphoid excision and intercarpal arthrodesis: intraoperative assessment and procedure selection. J Hand Surg Am. 2014;39(6):1055–1062. doi: 10.1016/j.jhsa.2014.03.032. [DOI] [PubMed] [Google Scholar]


