Abstract
Muscle-specific RING finger protein 1 (MuRF1) is a sarcomere-associated protein that is restricted to cardiac and skeletal muscle. In skeletal muscle, MuRF1 is up-regulated by conditions that provoke atrophy, but its function in the heart is not known. The presence of a RING finger in MuRF1 raises the possibility that it is a component of the ubiquitin–proteasome system of protein deg-radation. We performed a yeast two-hybrid screen to search for interaction partners of MuRF1 in the heart that might be targets of its putative ubiquitin ligase activity. This screen identified troponin I as a MuRF1 partner protein. MuRF1 and troponin I were found to associate both in vitro and in vivo in cultured cardiomyocytes. MuRF1 reduced steady-state troponin I levels when coexpressed in COS-7 cells and increased degradation of endogenous troponin I protein in cardiomyocytes. The degradation of troponin I in cardiomyocytes was associated with the accumulation of ubiquitylated intermediates of troponin I and was proteasome-dependent. In vitro, MuRF1 functioned as a ubiquitin ligase to catalyze ubiquitylation of troponin I through a RING finger-dependent mechanism. In isolated cardiomyocytes, MuRF1 reduced indices of contractility. In cardiomyocytes, these processes may determine the balance between hypertrophic and antihypertrophic signals and the regulation of myocyte contractile responses in the setting of heart failure.
Keywords: cardiomyocyte
Cardiac hypertrophy is characterized by an enlargement of the heart associated with an increase in cardiomyocyte cell volume and re-expression of certain fetal genes. Although cardiac hypertrophy is thought to benefit the heart initially by maintaining or augmenting pump function, prolongation of the hypertrophic state contributes to diastolic dysfunction and the development of arrhythmias, sudden death, and heart failure (1). In contrast, the reversal of hypertrophy is a powerful indicator of event-free survival in patients at otherwise high cardiovascular risk (2).
At the cellular level, cardiac hypertrophy is associated with increased protein synthesis leading to addition of contractile myofibers. It follows that the reversal of this process must include some mechanism to delete unnecessary proteins, particularly sarcomeric proteins that constitute the bulk of cardiomyocyte mass. In skeletal muscle systems, where this process has been characterized most carefully (3), atrophy, such as that induced by insulin deficiency, accelerates degradation of muscle proteins by activation of proteasome-dependent protein degradation along with the up-regulation of mRNA levels of genes that encode distinct components of the ubiquitin pathway (4). Although it was once commonly assumed that the primary role of the ubiquitin-proteasome pathway is to degrade abnormal and short-lived regulatory proteins (5, 6), studies conducted by using proteasome inhibitors (7) and ATP depletion (8, 9) indicate that this pathway also catalyzes the breakdown of most long-lived proteins, such as myosin, actin, troponin, and tropomyosin (3). However, the components of the ubiquitin-proteasome system that regulate degradation of sarcomeric proteins have remained elusive.
Recent screens for genes up-regulated in skeletal muscle atrophy have identified two proteins restricted to skeletal and cardiac muscle that may be components of the ubiquitin ligase family (members of which represent the rate-limiting enzymes for addition of polyubiquitin chains to proteins that are subsequently targeted to the proteasome for ATP-dependent degradation). MAFbx/atrogin-1 is an F-box-containing protein that binds to Skp1/cullin complexes (10) and induces atrophy in skeletal myotubes (11). Muscle-specific RING finger protein 1 (MuRF1) is one of a family of three MuRFs that contain a tripartite RING:B-box:coiled-coil domain, and deletion of MuRF1 in mice inhibits skeletal muscle atrophy (12). RING finger-containing proteins are the largest subset of ubiquitin ligases, although all proteins with RING fingers are not ubiquitin ligases. A number of questions remain unanswered about these proteins: What are the natural substrates for the ubiquitin ligase activities of atrogin-1 and MuRF1? Is there functional redundancy among MuRF1 family members? What are the roles of these proteins in cardiac muscle?
MuRF1 interacts with the myofibrillar giant spring protein titin at the M line (13, 14), resulting in disruption of the subdomain that binds MuRF1. This interaction suggests that MuRF1 regulates the stability of this large structural protein, although the functional consequences of this interaction remain to be explored, and titin does not appear to be a substrate for the ubiquitin ligase activity of MuRF1. We have therefore searched for additional MuRF1 interaction partners as a means of understanding how its ubiquitin ligase activity affects cardiomyocyte function.
Methods
Cell Culture and Transfection. COS-7 cells were transiently transfected by using FuGene (Roche). Neonatal rat ventricular myocytes (NRVM) were cultured in minimum essential medium containing Earle's salt with glutamine and 10% horse serum and 5% FBS. Recombinant adenoviruses were constructed with the Ad-Easy system, and cultures were infected for 24–48 h at a multiplicity of infection (moi) of 1–20 as indicated. The expression of proteins in the cells was routinely monitored by visualization of GFP fluorescence. In some experiments, adenovirus-infected cells were incubated with 40 μM MG132 or vehicle for 6 h before harvesting.
Expression Constructs. All control plasmids, GAL4 DNA-BD bait vector (pGBKT7), and GAL4 AD prey vector (pACT2) used in the two-hybrid screen were from the Matchmaker two-hybrid system 3 (BD Biosciences). The C terminus (143–351) of MuRF1 was cloned in pGBKT7 (pGBKT7-CMuRF1). Adenovirus plasmids Ad.GFP, Ad.GFP-CHIP, and Ad.GFP-Myc-MuRF1 (expressing GFP and Myc-tagged MuRF1 bicistronically) were constructed in pADTrack-CMV. Full-length mouse MuRF1 was cloned in vectors pGEX-4AT-3 (GST-MuRF1), pGBKT7 (pGBKT7-MuRF1), and Myc-pCMV (Myc-MuRF1). The RING finger domain (amino acids 39–48) of the MuRF1 was deleted by PCR to obtain GST-MuRFΔRF. Plasmid hemagglutinin (HA)-troponin I was constructed by attaching an HA tag to the N terminus of troponin I by PCR and cloning it into pcDNA3. GST-p68RacGAP was described in ref. 15.
Yeast Two-Hybrid Screen. An activating domain fusion protein human heart library (catalog no. HL4042AH, Clontech) cloned into pACT2 (Marker: LEU2) was screened with pGBKT7-CMuRF1. After nutritional selection, candidate clones were rescued on medium-stringency medium (SD-His/Leu/Trip/X-α-gal) and screened on high-stringency medium (SD-Leu/Trip/His/Ade/X-α-gal) to eliminate false positives.
Pulse–Chase Experiments. NRVM were infected with Ad.GFP and Ad.GFP-Myc-MuRF1 at 0–20 moi for 8 h. Cells were labeled 48 h later with [35S]methionine and cysteine [100 μCi/ml (1 Ci = 37 GBq)] for 45 min, washed, and chased for 0, 4, 8, 12, 16, and 24 h. Troponin I immunoprecipitates were separated by SDS/PAGE, and dried gels were autoradiographed.
In Vitro Ubiquitylation Reactions. In vitro ubiquitylation was performed as described in ref. 16. In brief, bacterially expressed GST, GST-Myc-MuRF1, or GST-MuRF1ΔRF, 0.1 μM purified rabbit E1 (Calbiochem), 2.5 mg/ml ubiquitin (Sigma), and 1.6 μM UBCH5C were incubated in 20 mM Mops, pH 7.2/100 mM KCl/5 mM MgCl2/5mMATP/10 mM DTT/1 mM phenylmethylsulfonyl fluoride for 4 h at 30°C. Samples were analyzed by SDS/PAGE and immunoblotting.
Indirect Immunofluorescence Microscopy. Primary cultures of NRVM were treated with or without phenylephrine (PE) for 48 h, followed by infection with Ad.GFP or Ad.GFP-Myc-MuRF1 for 24 h. Cells were fixed in 3.7% formaldehyde-PBS for 10 min and permeabilized in 0.5% Triton X-100 and 1% BSA in PBS for 10 min. Cells were then incubated with mouse anti-troponin I (1:500) or rabbit anti-Myc (1:200) for 90 min, followed by incubation with anti-mouse Alexa 568 red (1:800) and anti-rabbit cascade blue conjugated (1:500) for 45 min.
Contractility Measurements. NRVM infected with Ad.GFP or Ad.GFP-Myc-MuRF1 for 48 h (moi 5) were field-stimulated at a frequency of 0.5 Hz for a pulse duration of 5 ms at a sampling rate of 240 Hz. Shortening was measured as movement of high-contrast, 5-μm microspheres (SPI Supplies, West Chester, PA) that were attached to the cell surface. Motion of the high-contrast edge along a selected rastor line segment was enhanced and processed with a video edge-detection system (Crescent Electronics, Sandy, UT) (17). Calibrated movement of the microsphere was converted from analog to digital online. For each cell, three consecutive field-stimulated contractions were averaged. Contractile parameters measured were micrometer of cell shortening, micrometer per millisecond cell shortening, and micrometer per millisecond cell relengthening. The rate constant of relengthening was calculated by normalizing the rate of relengthening by the amount of cell shortening (Ad.GFP cells, n = 14; Ad.GFP-Myc-MuRF1 cells, n = 15). Results are representative of three independent experiments.
Results
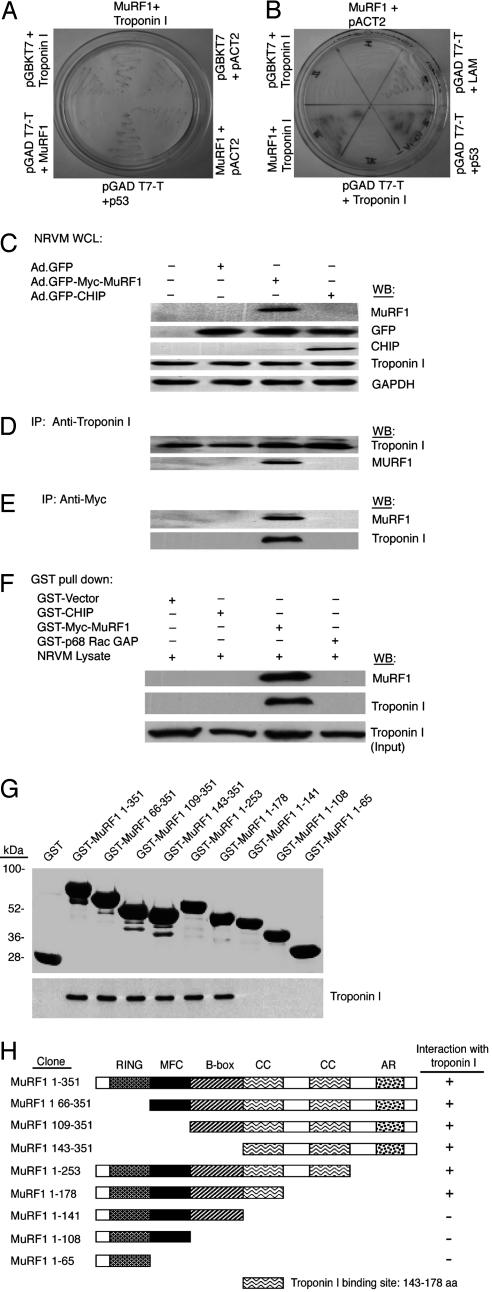
MuRF1 Interacts with the Sarcomeric Protein Troponin I. Titin, a megadalton-sized protein, has been shown to interact with a 144-residue segment of MuRF1 that contains the B-box and surrounding sequences of MuRF1 (13). We sought to ascertain whether other proteins bind to MuRF1 and to determine whether any of these proteins are substrates for its putative ubiquitin ligase activity. We performed a yeast two-hybrid screen by using residues 143–351 as a bait to screen an adult heart cDNA library. This region contains highly conserved coiled-coil domains that are similar to coiled-coil domains in sarcomeric proteins such as tropomyosin and myosin (13), which suggested to us that this region may play a regulatory role in sarcomere function. A total of 24 interacting clones were identified out of 2.4 × 106 screened clones. Four of the 22 clones could be confirmed by high-stringency screening and these encoded myosin-binding protein C (data not shown) and troponin I. We performed two-hybrid wheel assays to test the specificity of the interaction between MuRF1 and troponin I. By using either high-stringency nutritional selection (Fig. 1A) or LacZ expression (Fig. 1B), we found the interaction between MuRF1 and troponin I to be both potent (relative to the interaction of p53 with large T antigen) and highly selective.
Fig. 1.
MuRF1 interacts with cardiac troponin I in vivo and in vitro.(A and B) Troponin I was retrieved as one of the potential binding partners for MuRF1 in a two-hybrid screen. To reconfirm this binding, a wheel assay was performed by using medium-stringency β-gal filter assays (A) and high-stringency X-α-gal in-gel assays (B). (C–E) To confirm the above interaction in vivo, NRVM were infected with or without Ad.GFP, Ad.GFP-Myc-MuRF1, or Ad.GFP-CHIP at 2 moi. (C) After 24 h, cells were lysed and whole-cell lysates (WCL) were immunoblotted (WB) with anti-Myc (to detect MuRF1), anti-GFP, anti-CHIP, anti-troponin I, or anti-GAPDH as indicated. The cell lysates were immunoprecipitated with anti-troponin I (D) or anti-Myc (E) Abs followed by Western blotting with anti-Myc or anti-troponin I Abs. (F) To confirm the specificity of the interaction between MuRF1 and troponin I, GST-fusion proteins GST-Myc-MuRF1 and negative controls (GST alone, GST-CHIP, and GST-p68RacGAP) were incubated with NVRM lysates that express endogenous troponin I. The protein complexes were subjected to SDS/PAGE and immunoblotted with anti-Myc or anti-troponin I. (G) The region of MuRF1 involved in binding to troponin I was analyzed in pull-down assays. (Upper) GST-MuRF1 fusion proteins were analyzed by blotting with GST Ab. (Lower) The ability of the various MuRF1 fusion proteins to bind to HA-tagged troponin I was analyzed by blotting with HA Ab. (H) Schematic representations of MuRF1 residues that bind to troponin I are indicated. RING, RING domain; MFC, MuRF family conserved region; B-box, B-box domain domain; CC, coiled-coil domains; AR, acidic region.
We next examined whether MuRF1 associates in vivo with endogenous troponin I in cardiomyocytes. In these experiments, we also tested associations with related (ubiquitin ligase CHIP) and unrelated (p68RacGAP) proteins to exclude fortuitous interaction. Immunoblot analysis of NRVM lysates after adenoviral infection confirmed the presence of MuRF1, GFP, CHIP, and troponin I proteins (Fig. 1C), and microscopic analysis of GFP expression indicated >95% infection rates in all conditions. The association between MuRF1 and troponin I was tested by immunoprecipitating troponin I (Fig. 1D) and MuRF1 (Fig. 1E) from NRVM infected with Ad.GFP, Ad.GFP-Myc-MuRF1, or Ad.GFP-CHIP and measuring the levels of MuRF1 and endogenous troponin I in immunopellets. We found that troponin I and MuRF1 were indeed components of the immunocomplex precipitated by either troponin I or Myc (to detect MuRF1) Abs from lysate infected with Ad.GFP-Myc-MuRF1. Neither troponin I nor MuRF1 could be detected in immunopellets infected with control adenoviruses (Ad.GFP and Ad.GFP-CHIP).
To further confirm the interaction between MuRF1 and troponin I, we performed GST pull-down assays. Glutathione beads bound to fusion proteins GST-Myc-MuRF1 or controls (GST, GST-CHIP, or GST-p68RacGAP) were incubated with NRVM lysates. The presence of MuRF1 and troponin I complexes on glutathione-agarose beads was tested by immunoblot analysis of precipitated pellets with anti-Myc (to detect MuRF1) and anti-troponin I Abs. Troponin I was pulled down by GST-Myc-MuRF1 but not by control beads (Fig. 1F). Finally, we mapped the domains within MuRF1 that are responsible for interactions with troponin I by using GST pull-down assays and mapped the interaction domain to the first coiled-coil region located between amino acids 143 and 178 in MuRF1 (Fig. 1 G and H). These data confirm our observations by using the yeast two-hybrid system and indicate that MuRF1 interacts specifically with troponin I in vivo as well as in vitro.
MuRF1 Colocalizes with Troponin I in Cardiac Myocytes. Previous studies have shown that MuRF1 is found in several niches within myocytes: the cytosol, nucleus, and along myofibrils (13, 18). We also observed similar localization of MuRF1 in cardiomyocytes treated with or without PE (Fig. 2, blue channel). Troponin I is mostly bound to the contractile apparatus in the myocardium along myofilaments, and ≈8% is found freely in the cytoplasm (19, 20). We observed that troponin I is located in a striated pattern throughout the breadth and length of NVRM untreated with PE (Fig. 2, red channel). In the absence of PE treatment, there was appreciable colocalization of MuRF1 and troponin I in NVRM, although not all foci of troponin I expression along the sarcomere contained dense foci of MuRF1 expression, which is consistent with previous reports that MuRF1 is concentrated at distinct sites that vary among individual sarcomeres (13). In NRVM treated with PE, cells were larger, and both MuRF1 and troponin I were colocalized along the myofibrils. In addition, after PE treatment both the proteins were present in globule-shaped structures that were present along the myofibrils and in the perinuclear region. Similar localization patterns were observed in NRVM treated with endothelin-1 and angiotensin II (data not shown). Given the results of our subsequent experiments, it is tempting to speculate that these globules may represent domains primed for protein degradation within cardiomyocytes.
Fig. 2.
MuRF1 colocalizes with troponin I in cultured cardiac myocytes. Primary cultures of NVRM were treated with or without PE (100 μM) for 48 h followed by incubation with Ad.GFP-Myc-MuRF1. After fixing the cells in formaldehyde, immunostaining was performed. Blue and red colors represent MuRF1 and troponin I, respectively.
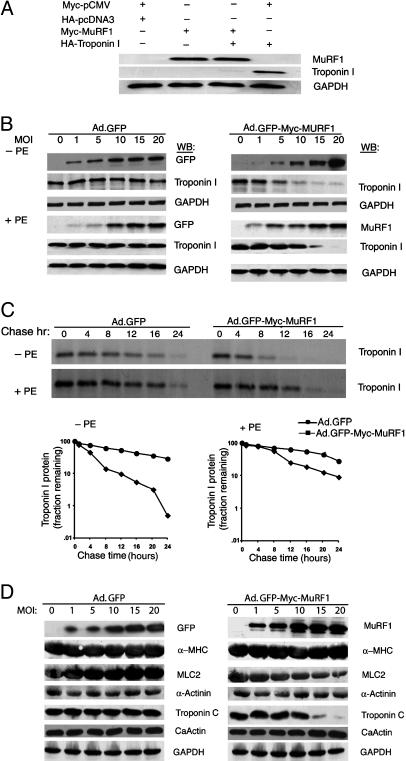
MuRF1 Decreases Steady-State Levels of Troponin I by Increasing Its Degradation. Based on the unusual colocalization pattern of MuRF1 and troponin I and the putative ubiquitin ligase activity of MuRF1, we next addressed whether increasing levels of MuRF1 would affect the stability of troponin I. To this end, we first monitored troponin I protein levels by Western blotting by using COS-7 cells cotransfected with plasmids expressing MuRF1 and troponin I. The transfection of MuRF1 together with troponin I markedly decreased the expression of troponin I compared with COS-7 cells expressing troponin I alone (Fig. 3A).
Fig. 3.
MuRF1 decreases troponin I protein expression by increasing its degradation. (A) COS-7 cells were cotransfected with plasmids and lysed 48 h later, and proteins from cell lysates were probed with Abs against Myc (to detect MuRF1), troponin I, and GAPDH. (B) NRVM were treated with or without PE for 48 h and then infected with Ad.GFP or Ad.GFP-Myc-MuRF1 at 0–20 moi for 8 h. Cell lysates were harvested 48 h after expression of GFP fluorescence in cells. Proteins in the lysates were separated by SDS/PAGE, and Western blotting (WB) was performed with Abs against troponin I, Myc, and GAPDH. (C) NRVM were treated with or without PE for 48 h, and they were infected with adenovirus for 8 h. After washing, cells were pulse-labeled with [35S]methionine and cysteine for 1 h and then chased for the indicated times. Troponin I protein was immunoprecipitated and separated by SDS/PAGE. Quantification of results are plotted as the percentage of troponin I protein at the 0-h value (in log scale) against time. A representative of three independent experiments is shown. (D) Western blot analysis of proteins from NRVM treated with the indicated adenoviruses. α-MHC, α-myosin heavy chain; MLC2, ventricular myosin light chain-2; CaActin, cardiac actin.
Although transient transfection experiments are informative, they do not always accurately reflect the steady-state association of two proteins in cells that constitutively express these proteins. Therefore, we next asked whether endogenous troponin I levels are affected by MuRF1 protein levels in NRVM treated with or without PE. For this purpose, we infected NRVM with Ad.GFP or Ad.GFP-Myc-MuRF1 at increasing titers and incubated the cells for 48 h after the onset of GFP expression. Under these conditions, an moi of between 1 and 5 results in near 100% infection efficiency for NRVM. In Ad.GFP-infected NRVM, the steady-state levels of troponin I were not appreciably altered, whereas the levels of troponin I declined progressively with increasing titers of MuRF1 adenovirus (Fig. 3B). Troponin I levels were 4-fold higher after PE treatment, and its stability was increased, whereas endogenous MuRF1 protein levels did not decrease (data not shown), suggesting that increased protein synthesis, adrenergic signaling, and/or sarcomere assembly may partially (but not completely) protect troponin I from destabilization.
To quantify the down-regulation of troponin I, we examined whether the overexpression MuRF1 reduces the half-life of endogenous troponin I by pulse–chase analysis of [35S]methionine plus cysteine-labeled NRVM. The half-life of troponin I in NRVM in the absence of PE stimulation was reduced from 17 h to 4 h after adenoviral expression of MuRF1 (Fig. 3C). Troponin I protein produced by NRVM treated with PE had a comparatively prolonged half-life, but increased MuRF1 levels similarly destabilized troponin I under these conditions. Finally, we tested the specificity of the effects of MuRF1 by examining its effects on other sarcomere-associated proteins. Among the proteins tested, we found that MuRF1 also decreased steady-state levels of troponin C and myosin light chain-2 (Fig. 3D). Taken together, these results indicate that MuRF1 down-regulates steady-state levels of troponin I by increasing its degradation in cardiomyocytes and may have similar activities on a select group of other contractile proteins as well.
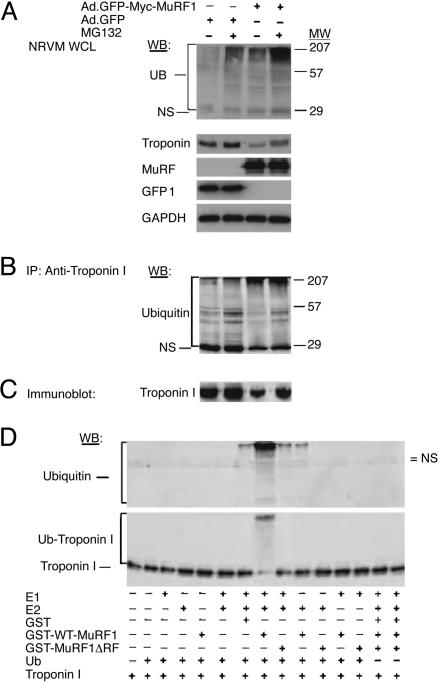
MuRF1 Is a RING Finger-Dependent Ubiquitin Ligase That Targets Troponin I for Proteasome-Dependent Degradation. Previous studies have suggested that MuRF1 has ubiquitin ligase activity, but definitive linkage of MuRF1 with ubiquitin-dependent degradation via the proteasome is lacking because substrates for such an activity have not been identified (11, 12). Based on our observations that MuRF1 specifically binds to and decreases the half-life of troponin I, we asked whether expression of MuRF1 mediates ubiquitylation of endogenous proteins. To this end, we infected NRVM with Ad.GFP-Myc-MuRF1 or Ad.GFP in the absence or presence of MG-132, a selective inhibitor of proteasome activity. A slowly migrating smear of high-molecular-weight proteins detectable by immunoblot analysis for ubiquitin was enhanced in cells infected with Ad.GFP-Myc-MuRF1, and the accumulation of these species was accentuated in the presence of the proteasome inhibitor (Fig. 4A), indicating that MuRF1 enhances the ubiquitylation of endogenous proteins, consistent with a ubiquitin ligase activity. The same lysates were also probed for the detection of troponin I, and the level of troponin I was markedly reduced by MuRF1. The proteasome inhibitor MG132 increased troponin I levels by 55% in NRVM infected with Ad.GFP and by 210% in cells infected with Ad.GFP-Myc-MuRF1, compared with untreated cells (Fig. 4A).
Fig. 4.
MuRF1 induces ubiquitylation of troponin I in vivo and in vitro. (A) NRVM were infected with Ad.GFP or Ad.GFP-Myc-MuRF1 and treated with MG-132 for 6 h. Ubiquitin (Ub) conjugates from lysates were separated by SDS/PAGE, and Western blotting (WB) was performed with an anti-ubiquitin Ab. Cell lysates were blotted simultaneously with anti-troponin I, anti-Myc, anti-GFP, and anti-GAPDH. NS, nonspecific; MW, molecular weight. (B and C) Lysates were subjected to immunoprecipitation with anti-troponin I followed by immunoblotting with anti-ubiquitin (B) or were directly probed with anti-troponin I (C) Abs to detect ubiquitylated species of troponin I. (D) In vitro ubiquitylation reactions were performed to test the ubiquitin ligase activity of MuRF1. Ubiquitin conjugates of troponin I were detected with anti-ubiquitin (Upper) and anti-troponin I (Lower) Abs. The ubiquitylation of troponin I is noticeable as the accumulation of slower-migrating species of troponin I with concomitant loss of the ubiquitylated protein.
To test the effects of MuRF1 on troponin I ubiquitylation with more sensitivity, we performed immunoprecipitations on NRVM lysates with a troponin I-specific Ab, followed by Western blotting with Abs specific for ubiquitin (to detect ubiquitylated species of troponin I). These experiments indicated that MuRF1 increases troponin I ubiquitylation, as detected by the accumulation of slowly migrating ubiquitin immunoreactivity in troponin I immunoprecipitates that was further augmented by MG132 treatment (Fig. 4B). Blotting of troponin I in these immunoprecipitates indicated that troponin I levels were decreased by MuRF1, and that these levels were rescued by MG132 treatment. These experiments indicate that MuRF1 serves as a ubiquitylation factor for endogenous proteins in cardiomyocytes, one of which is troponin I. Moreover, MuRF1 is a rate-limiting factor for these ubiquitylation events.
In vitro ubiquitylation assays were performed with recombinant proteins to directly test the ubiquitin ligase activity of MuRF1. We used an approach similar to that used to characterize the ubiquitin ligase activity of the RING finger protein c-Cbl, in which ubiquitylation in the absence of a specific substrate is tested as an indication of multiubiquitin chain assembly that occurs either freely, on co-purifying proteins, or on the ubiquitin ligase itself (21). Bacterially expressed MuRF1 (as a GST fusion) and UBCH5c, an E2 ubiquitin-conjugating enzyme, were incubated in a reaction containing ubiquitin, E1 and troponin I, and these reaction mixtures were probed simultaneously by Western blotting with an anti-ubiquitin or anti-troponin I Ab. Ubiquitylation activities, as assessed by the detection of high-molecular-weight multiubiquitin chains of ubiquitin and ubiquitylated troponin I, were detected only in reactions containing E1, UBCH5c, and MuRF1 in the presence of ubiquitin (Fig. 4C). Deletion of any single component in this reaction abolished troponin I ubiquitylation.
MuRF1 contains an amino-terminal RING finger, and the family of RING finger proteins is linked with ubiquitin ligase activity in many cases. If the ability of MuRF1 to down-regulate troponin I is truly due to ubiquitin ligase activity, then disruption of the RING finger domain should abrogate its ubiquitin ligase activity. To test this hypothesis, we deleted the RING finger and examined the ubiquitin ligase activity of this mutant in the reconstituted ubiquitylation assay. Deletion of the RING finger totally abolished ubiquitylation of troponin I (Fig. 4C). Taken together, our data indicate that MuRF1 is the ubiquitin ligase responsible for catalyzing proteasome-dependent degradation of troponin I and that the RING finger domain of MuRF1 is required for its ubiquitin ligase activity.
Effects of MuRF1 on Cardiomyocyte Contractility. We examined contractility in neonatal cardiomyocytes to test the effects of MuRF1 on sarcomere function. Cell shortening and rate of shortening during field-stimulated contractions were measured in isolated cardiomyocytes infected with Ad.GFP or Ad.GFP-Myc-MuRF1 for 48 h. Increasing MuRF1 levels in cardiomyocytes decreased both maximal shortening and the rate of shortening (–dL/dt) by 25%. In contrast, the relaxation rate constant (rate of relaxation normalized to total shortening) was unchanged by MuRF1. In addition, we noted that MuRF1 dose-dependently decreased the frequency of spontaneous cardiomyocyte contractions by 70% at an moi of 1 without affecting viability. Although we do not know whether these effects are entirely dependent on the ubiquitin ligase activity of MuRF1, these observations indicate that MuRF1 impairs both contractile responses and beating frequencies in NRVM, which underscores the functional consequences of MuRF1-dependent perturbations in the sarcomere.
Discussion
MuRF1 was originally identified by searching for genes up-regulated in models of skeletal muscle atrophy (11). The restriction of its expression to skeletal and cardiac muscle suggests that it may be part of the general program to regulate cell size in myocytes. To explore this possibility, and to identify potential targets for the ubiquitin ligase activity of MuRF1, we performed a yeast two-hybrid screen that identified troponin I as a MuRF1 interaction partner. In this report, we demonstrate that MuRF1–troponin I interactions can be detected in cardiomyocytes. MuRF1 decreases steady-state levels of troponin I by inducing its ubiquitylation and proteasome-dependent degradation. By using in vitro reconstitution assays, we show that MuRF1 is a bona fide RING finger-dependent ubiquitin ligase that catalyzes a rate-limiting step in troponin I degradation. Although degradation of troponin I via the proteasome has previously been described, the identity of the protein(s) responsible has until now been elusive.
Interaction of titin with MuRF1 in sarcomeres has previously been reported (13, 18). Our data and that of other groups indicate that MuRF1 exists in multiple locations within the cell, including the cytosol, along the sarcomere, and within the nucleus. In the cytosol, MuRF1 is the only MuRF family member that binds to titin (13). The present studies extend the list of sarcomeric proteins that bind MuRF1 to include troponin I. It is important to note that MuRF1 does not appear to target titin for degradation (13), whereas for troponin I it does. Interestingly, in cardiomyocytes treated with PE, both MuRF1 and troponin I colocalize along myofibrils and are also present in small globule-shaped structures along the myofibrils and in the perinuclear region (Fig. 2). It is tempting to speculate that these globules may represent domains of ubiquitin-dependent protein degradation within cardiomyocytes that are analogous to so-called aggresomes (22, 23). These globules may serve as nucleation sites for the degradation of sarcomeric proteins by ubiquitin ligases such as MuRF1 when rates of protein turnover are high.
Protein degradation in striated muscle proceeds via three proteolytic systems. Lysosomal proteases are responsible for degradation of endocytosed proteins including membrane proteins (24–26). The cytosolic proteases μ-calpain and m-calpain trigger proteolytic cleavage of target proteins (frequently in response to phosphorylation events) (27); calpain-dependent cleavage may either clear the target protein or, on occasion, lead to the generation of stable proteolytic intermediates with gain-of-function activity. The ubiquitin-proteasome system is a major ATP-dependent pathway for protein degradation in muscle, particularly for myofibrillar proteins that comprise the majority of muscle proteins. In skeletal muscle, the rapid degradation of muscle proteins in response to fasting, disuse, or aging takes place because of activation of ubiquitin-proteosome pathways (11, 12). Much more is known about pathways of protein degradation in skeletal muscle than in cardiomyocytes, although it is generally assumed that the processes are similar.
Troponin I undergoes degradation via two mechanisms. Troponin I is proteolytically cleaved by calpains after ischemia-reperfusion injury. This generates a 193-aa cleavage product that accumulates in the stunned myocardium (28–31). Overexpression of this troponin I fragment causes cardiac dysfunction in mice (32), indicating that calpain-dependent proteolysis of troponin I leads to a toxic gain-of-function intermediate. In addition, purified troponins (as well as myosin, actin, and tropomyosin) are readily degraded via the ubiquitin-proteasome pathway in muscle extracts (3). Our data indicate that MuRF1 is a key component of the ubiquitin ligase complex that is required for troponin I ubiquitylation and degradation, whereas we do not see the typical cleavage products of troponin I that are induced by calpains; in other words, MuRF1-dependent ubiquitylation and calpain-dependent proteolysis appear to be distinct cellular processes. The ability of MuRF1 to induce complete proteolysis of troponin I bypasses the possibility of accumulation of the types of toxic proteolytic intermediates that appear after calpain-dependent cleavage, thus providing a biological rationale for the existence of two independent proteolytic mechanisms for troponin I degradation.
Interestingly, troponins are resistant to degradation by the ubiquitin-proteasome pathway when present in myofibrils or in soluble actomyosin complexes (3). This observation indicates that specific linkages in the contractile apparatus protect troponins from ubiquitylation and suggests that the dissociation of free myosin, troponin, and other myofibrillar proteins from contractile filaments is the rate-limiting step in their degradation. These observations may be relevant to the role played by MuRF1 in the sarcomere. MuRF1 binds to titin and disrupts its interactions with the M-line without inducing the degradation of titin, thus partially disrupting sarcomere assembly (18). We hypothesize that MuRF1 may destabilize sarcomeres by binding to titin, which would in turn provide MuRF1 with access to its substrate troponin I. Troponin I could then be targeted for ubiquitylation and proteasome-dependent degradation by MuRF1. This activity of MuRF1 may be generalized to other sarcomere accessory proteins (Fig. 3D).
Functionally, we found that MuRF1 reduces cardiomyocyte contractility and beating frequencies. These effects most likely reflect the summation of the effects of MuRF1 on sarcomeric proteins, which emphasizes the need to characterize the full range of substrates that are recognized for degradation by MuRF1. Nevertheless, the effects of MuRF1 on contractility are consistent with the reported effects of loss of troponin I function. Deletion of troponin I results in decreased contractility and cardiac dysfunction in mice (33), and a recessive mutation in troponin I that disrupts assembly of the troponin complex also results in a contractility defect in humans (34). It is tempting to speculate that disassembly of sarcomeres by molecules such as MuRF1 may be a maladaptive response that contributes to wall thinning and contractile dysfunction in dilated cardiomyopathies.
Acknowledgments
We thank Kristine Porter for excellent technical assistance. This work was supported by National Institutes of Health Grants HL65619 and GM61728 (to C.P.) and HL56687 (to H.A.R.). C.P. is an Established Investigator of the American Heart Association and a Burroughs Wellcome Fund Clinical Scientist in Translational Research.
Author contributions: V.K., H.M., H.A.R., and C.P. designed research; V.K., H.M., R.A., and H.-H.L. performed research; V.K. and H.-H.L. contributed new reagents/analytic tools; V.K., H.M., R.A., H.-H.L., H.A.R., and C.P. analyzed data; and V.K. and C.P. wrote the paper.
This paper was submitted directly (Track II) to the PNAS office.
Abbreviations: MuRF1, muscle-specific RING finger protein 1; HA, hemagglutinin; NRVM, neonatal rat ventricular myocytes; PE, phenylephrine; moi, multiplicity of infection.
References
- 1.Lorell, B. H. & Carabello, B. A. (2000) Circulation 102, 470–479. [DOI] [PubMed] [Google Scholar]
- 2.Verdecchia, P., Schillaci, G., Borgioni, C., Ciucci, A., Gattobigio, R., Zampi, I., Reboldi, G. & Porcellati, C. (1998) Circulation 97, 48–54. [DOI] [PubMed] [Google Scholar]
- 3.Solomon, V. & Goldberg, A. L. (1996) J. Biol. Chem. 271, 26690–26697. [DOI] [PubMed] [Google Scholar]
- 4.Lecker, S. H., Solomon, V., Price, S. R., Kwon, Y. T., Mitch, W. E. & Goldberg, A. L. (1999) J. Clin. Invest. 104, 1411–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Etlinger, J. D. & Goldberg, A. L. (1977) Proc. Natl. Acad. Sci. USA 74, 54–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hershko, A., Eytan, E., Ciechanover, A. & Haas, A. L. (1982) J. Biol. Chem. 257, 13964–13970. [PubMed] [Google Scholar]
- 7.Rock, K. L., Gramm, C., Rothstein, L., Clark, K., Stein, R., Dick, L., Hwang, D. & Goldberg, A. L. (1994) Cell 78, 761–771. [DOI] [PubMed] [Google Scholar]
- 8.Gronostajski, R. M., Pardee, A. B. & Goldberg, A. L. (1985) J. Biol. Chem. 260, 3344–3349. [PubMed] [Google Scholar]
- 9.Levy, D., Garrison, R. J., Savage, D. D., Kannel, W. B. & Castelli, W. P. (1990) N. Engl. J. Med. 322, 1561–1566. [DOI] [PubMed] [Google Scholar]
- 10.Gomes, M. D., Lecker, S. H., Jagoe, R. T., Navon, A. & Goldberg, A. L. (2001) Proc. Natl. Acad. Sci. USA 98, 14440–14445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodine, S. C., Latres, E., Baumhueter, S., Lai, V. K., Nunez, L., Clarke, B. A., Poueymirou, W. T., Panaro, F. J., Na, E., Dharmarajan, K., et al. (2001) Science 294, 1704–1708. [DOI] [PubMed] [Google Scholar]
- 12.Glass, D. J. (2003) Trends Mol. Med. 9, 344–350. [DOI] [PubMed] [Google Scholar]
- 13.Centner, T., Yano, J., Kimura, E., McElhinny, A. S., Pelin, K., Witt, C. C., Bang, M. L., Trombitas, K., Granzier, H., Gregorio, C. C., et al. (2001) J. Mol. Biol. 306, 717–726. [DOI] [PubMed] [Google Scholar]
- 14.Pizon, V., Iakovenko, A., Van Der Ven, P. F., Kelly, R., Fatu, C., Furst, D. O., Karsenti, E. & Gautel, M. (2002) J. Cell Sci. 115, 4469–4482. [DOI] [PubMed] [Google Scholar]
- 15.Aitsebaomo, J., Wennerberg, K., Der, C. J., Zhang, C., Kedar, V., Moser, M., Kingsley-Kallesen, M. L., Zeng, G.-Q. & Patterson, C. (2004) J. Biol. Chem. 17963–17972. [DOI] [PubMed]
- 16.Jiang, J., Ballinger, C., Wu, Y., Dai, Q., Cyr, D., Höhfeld, J. & Patterson, C. (2001) J. Biol. Chem. 276, 42938–42944. [DOI] [PubMed] [Google Scholar]
- 17.Hajjar, R. J., Schmidt, U., Kang, J. X., Matsui, T. & Rosenzweig, A. (1997) Circ. Res. 81, 145–153. [DOI] [PubMed] [Google Scholar]
- 18.McElhinny, A. S., Kakinuma, K., Sorimachi, H., Labeit, S. & Gregorio, C. C. (2002) J. Cell Biol. 157, 125–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bleier, J., Vorderwinkler, K.-P., Falkensammer, J., Mair, P., Dapunt, O., Puschendorf, B. & Mair, J. (1998) Clin. Chem. 44, 1912–1918. [PubMed] [Google Scholar]
- 20.Westfall, M. V., Borton, A. R., Albayya, F. P. & Metzger, J. M. (2002) Circ. Res. 91, 525–531. [DOI] [PubMed] [Google Scholar]
- 21.Joazeiro, C. A., Wing, S. S., Huang, H., Leverson, J. D., Hunter, T. & Liu, Y. C. (1999) Science 286, 309–312. [DOI] [PubMed] [Google Scholar]
- 22.Johnston, J. A., Ward, C. L. & Kopito, R. R. (1998) J. Cell Biol. 143, 1883–1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lelouard, H., Gatti, E., Cappello, F., Gresser, O., Camosseto, V. & Pierre, P. (2002) Nature 417, 177–182. [DOI] [PubMed] [Google Scholar]
- 24.Furuno, K. & Goldberg, A. L. (1986) Biochem. J. 237, 859–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dice, J. F. (1987) FASEB J. 1, 349–357. [DOI] [PubMed] [Google Scholar]
- 26.Lardeux, B. R. & Mortimore, G. E. (1987) J. Biol. Chem. 262, 14514–14519. [PubMed] [Google Scholar]
- 27.DeMartino, G. N. & Goldberg, A. L. (1981) Enzyme 26, 1–7. [DOI] [PubMed] [Google Scholar]
- 28.Gao, W. D., Atar, D., Liu, Y., Perez, N. G., Murphy, A. M. & Marban, E. (1997) Circ. Res. 80, 393–399. [PubMed] [Google Scholar]
- 29.McDonough, J. L., Arrell, D. K. & Van Eyk, J. E. (1999) Circ. Res. 84, 9–20. [DOI] [PubMed] [Google Scholar]
- 30.Granzier, H., Labeit, D., Wu, Y. & Labeit, S. (2002) J. Muscle Res. Cell Motil. 23, 457–471. [DOI] [PubMed] [Google Scholar]
- 31.Granzier, H. & Labeit, S. (2002) J. Physiol. (London) 541, 335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murphy, A. M., Kogler, H., Georgakopoulos, D., McDonough, J. L., Kass, D. A., Van Eyk, J. E. & Marban, E. (2000) Science 287, 488–491. [DOI] [PubMed] [Google Scholar]
- 33.Huang, X., Pi, Y., Lee, K. J., Henkel, A. S., Gregg, R. G., Powers, P. A. & Walker, J. W. (1999) Circ. Res. 84, 1–8. [DOI] [PubMed] [Google Scholar]
- 34.Murphy, R. T., Mogensen, J., Shaw, A., Kubo, T., Hughes, S. & McKenna, W. J. (2004) Lancet 363, 371–372. [DOI] [PubMed] [Google Scholar]