Abstract
BACKGROUND
Despite the importance of identifying populations with multiple chronic conditions (MCC) for policy-makers, researchers, and clinicians, definitions of MCC vary considerably.
OBJECTIVES
To 1) determine the extent of agreement among four commonly used definitions of MCC, and 2) compare each definition's ability to predict 30-day hospital readmissions.
DESIGN
Retrospective cohort study.
SETTING
National Medicare claims data.
PARTICIPANTS
Random sample of Medicare beneficiaries experiencing hospital discharge from 2005-2009 (n=710,609).
MEASUREMENTS
We measured baseline chronic conditions for each participant using four definitions of MCC. The primary outcome was all-cause 30-day hospital readmission. We measured agreement between MCC definitions and calculated sensitivities and specificities for each definition's ability to identify patients experiencing a future readmission. We used logistic regression to assess the ability of each MCC definition to predict 30-day hospital readmission.
RESULTS
The sample prevalence of hospitalized Medicare beneficiaries with ≥2 chronic conditions ranged from 18.6% (ACG) to 92.9% (CCW) (n=710,609). There was slight to moderate agreement (kappa 0.03-0.44) between pair-wise combinations of MCC definitions. CCW-defined MCC was the most sensitive (Se 95.4%, Sp 7.4%) and ACG-defined MCC was the most specific (Se 32.7%, Sp 83.2%) predictor of having a hospital readmission. In the fully adjusted model, the risk of readmission was higher for those with c-SNP-defined MCC (OR 1.50, 95% CI 1.47-1.52), CCI-defined MCC (OR 1.45, 95% CI 1.42-1.47), ACG-defined MCC (OR 1.22, 95% CI 1.19-1.25), and CCW-defined MCC (OR 1.15, 95% CI 1.11-1.19) compared to those without MCC.
CONCLUSION
MCC definitions demonstrate poor agreement and should not be used interchangeably. The two definitions with the greatest agreement (CCI and c-SNP) were also the best predictors of 30-day hospital readmissions.
Keywords: Medicare, multimorbidity, multiple chronic conditions, readmissions, chronic care management
INTRODUCTION
Improving health care for patients with multiple chronic conditions (MCC) is a national priority because this patient population experiences disproportionately high rates of morbidity, mortality, hospitalizations, and hospital readmissions.1,2 Medicare estimates that two-thirds of its beneficiaries have 2 or more chronic conditions,2 and that the 14% of Medicare beneficiaries with 6 or more chronic conditions account for almost half of all Medicare spending.3 Despite the collective importance of this population, definitions and measures of MCC vary widely among researchers, policy-makers, and practitioners.4 The multitude of approaches used to define the chronic conditions that constitute MCC complicates clinical and policy efforts to target those at high risk for specific poor health outcomes. For example, Medicare created a new mechanism in January 2015 to reimburse health care teams for providing chronic care management services to Medicare beneficiaries with MCC defined as “two or more chronic conditions that are expected to last at least 12 months and that confer a significant risk of death, decompensation, or functional decline.”5 Without a widely accepted definition of MCC or established mechanisms for identifying individuals with MCC in medical records, providers may be unsure of whether a particular patient is eligible for chronic care management services. In addition, health systems striving to improve 30-day hospital readmission quality metrics need to understand the clinical implications of the MCC definitions they may be using to identify high-risk individuals for resource-intensive transitional care or care management interventions.6,7,8,9,10
Although the concept of comorbidity burden is a well-established risk factor for hospital readmission,11,12,13,14 it has been defined in a wide variety of ways. Half of established readmission risk prediction models11 incorporate a version of the Charlson Comorbidity Index15 or the Center for Medicare & Medicaid Services (CMS) Hierarchical Condition Categories.16 Medicare's Chronic Condition Warehouse (CCW) condition definitions are widely used in health services research,17,18,19 and clinicians have also received guidance that the CCW condition definitions could be used to identify patients eligible for enhanced chronic care management services.20 Medicare Advantage health insurance plans have been using a different strategy to target care coordination services toward high-need patients by selecting any of 15 “severe and disabling chronic conditions” to qualify patients at high risk of hospitalization or other adverse health outcomes for chronic condition Special Needs Plans (c-SNPs).21 These 15 c-SNP conditions were determined by a congressional panel of clinical advisors, including the Director of the Agency for Healthcare Research and Quality.22,23 The Johns Hopkins Adjusted Clinical Groups® (ACG) Case-Mix System software is used by health systems worldwide to predict future health care costs, and also contains its own algorithms for generating chronic condition counts, called Expanded Diagnosis Clusters™ (EDCs).24 Each of these methods for defining chronic conditions from diagnosis codes varies greatly. While there have been several direct comparisons of comorbidity measures’ abilities to predict mortality,25,26,27 there are few direct comparisons of comorbidity measures predicting health care expenditures28 or hospital readmissions,29,30 outcomes of considerable practical importance to policy-makers and health systems alike.
The purpose of this study was to compare the abilities of four chronic disease classification systems, commonly used in research and policy-making, to identify individuals with two or more chronic conditions at risk for hospital readmission. A threshold of two chronic conditions was chosen for consistency with the MCC criteria used by the U.S. Department of Health and Human Services1 and Medicare.2,5 We compared the Charlson Comorbidity Index (CCI), Medicare's CCW condition categories, Medicare Advantage c-SNP conditions, and the Johns Hopkins ACG® Case-Mix System EDCs.™ The specific objectives of these comparisons were to: 1) to determine the extent of agreement among four definitions of MCC in a national cohort of Medicare beneficiaries; and, 2) to compare each definition's ability to predict 30-day hospital readmissions. We hypothesized that the different MCC definitions would demonstrate moderate to poor agreement and that those MCC definitions including the greatest number of possible chronic conditions would be the most sensitive, but least specific, predictors of 30-day hospital readmissions.
METHODS
Design, Setting, and Participants
This retrospective cohort study used 2004-2009 Medicare claims data from a 5% random sample of Medicare beneficiaries in the Chronic Condition Data Warehouse.31 Medicare's provider of service file was used to obtain hospital characteristics. We focus on Medicare fee-for-service beneficiaries who were ages 65 and older, discharged from a hospitalization 1/1/2005-12/1/2009, enrolled in both Medicare Parts A and Part B for 12 months prior to the date of admission, enrolled in Medicare Parts A and B for 12 months after the date of discharge unless they died during the post-discharge period, and who experienced at least 1 inpatient or 2 outpatient (evaluation & management visit or emergency department visit) encounters in the 12 months prior to the index admission in order to ensure an adequate number of claims from which to obtain diagnostic codes during the baseline year. We excluded beneficiaries who experienced in-hospital deaths or who left against medical advice during their index admissions, consistent with Medicare's readmission metric approach. The University of Wisconsin-Madison Institutional Review Board determined that this study did not meet criteria for human subject research.
Measures
We measured the number of chronic conditions for each Medicare beneficiary using four separate approaches, including: 1) Medicare's CCW Conditions (CCW Original Version)32, 2) CCI conditions33, 3) Johns Hopkins ACG® Case-Mix System version 10 EDCs™ with stringent diagnostic certainty option enabled (version 11 is the most recent version available), and 4) the Medicare Advantage c-SNP conditions (Table 1). The c-SNPs were derived from Hierarchical Condition Categories (HCCs) (version 22) using a previously published strategy for deriving c-SNPs from version 12 HCCs.16 We used the approach developed by Taylor et al34 for identifying dementia because dementia is a c-SNP condition that does not have an equivalent HCC in the HCC community claims model. The 15 c-SNP conditions are currently being used by Medicare Advantage health insurance plans to identify beneficiaries eligible for enhanced care coordination services via physician verification of eligibility criteria rather than from claims data algorithms.21 All chronic condition definitions were derived from claims in the 12 months prior to index admission except for the 21 CCW conditions, which are included in the Chronic Condition Data Warehouse data file as “ever” variables, based on the first occurrence of a claim since beneficiary enrollment. We did not restrict the look-back period for CCW conditions to the baseline year alone because the ability to measure the cumulative prevalence of CCW conditions is a core feature of the CCW condition definition that is often considered an advantage, and cumulative prevalence of CCW conditions is used in Medicare's Chronic Condition Chartbook.2
Table 1.
Characteristics of Chronic Condition Classification Measures
| Chronic Condition Data Warehouse (CCW) | Charlson Comorbidity Index (CCI) | Johns Hopkins Adjusted Clinical Groups® (ACG®) Case-Mix Systema | Medicare Advantage Special Needs Plan Chronic Conditions (c-SNP) | |
|---|---|---|---|---|
| Total Possible Chronic Conditions (n) | 21 (19 for men, 20 for women) | 17 | 119 | 15 |
| Timeframe | Total years of Medicare enrollment | 1 year | 1 year | 1 year |
| Original Purpose | Prevalence/Cohort Identification for Research Purposes | Mortality Prediction | Prevalence/Cohort Identification for Research Purposesa | Select Medicare Advantage beneficiaries eligible for enhanced clinical services |
| Reference | Centers for Medicare and Medicaid Services (2005) | Klabunde et al (2000) | Johns Hopkins University (2009) | Pope et al (2011), Centers for Medicare and Medicaid Servicesb |
Expanded Diagnoses Clusters™ (EDCs™) are intended to be used for investigating the epidemiology of diseases within populations in contrast to the Johns Hopkins Adjusted Clinical Groups® Case-Mix System Aggregated Diagnosis Groups™ (ADGs®), which are actuarial cells designed for risk prediction modeling that include information about condition duration, severity, diagnostic certainty, etiology, and specialty care required.
The c-SNPs were derived from Hierarchical Condition Categories (HCCs) (version 22) using a previously published strategy for deriving c-SNPs from version 12 HCCs.16 We used the Taylor Flag34 for dementia since dementia is a c-SNP condition that does not have an equivalent HCC in the HCC community claims model. The 15 c-SNP conditions are currently being used by Medicare Advantage health insurance plans to identify beneficiaries eligible for enhanced care coordination services via physician verification of eligibility criteria rather than from claims data algorithms.21
The primary outcome was all-cause hospital readmission within 30 days of discharge from the first index admission each beneficiary experienced during the study period. Other beneficiary-level variables included age, sex, race, initial Medicare enrollment due to disability, index hospitalization length of stay, discharge to a skilled nursing facility, and baseline year utilization (hospitalizations, emergency department visits, and clinic visits), and death within 30 days of hospital discharge. Beneficiaries needed to survive until hospital discharge to be at risk for the primary outcome of 30-days hospital readmission and to be included in the study population. Hospital-level variables, obtained from Medicare's provider of service data file, included index hospital type (non-profit, for-profit, and public) and total beds.
Statistical Analysis
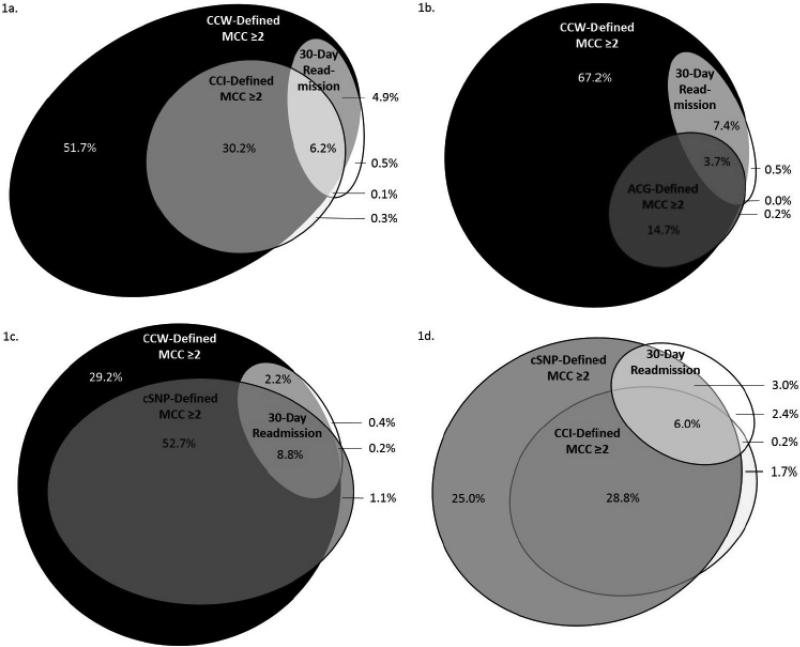
We first examined the prevalence of having two or more chronic conditions in the cohort, using the four different definitions of MCC, along with the baseline characteristics of Medicare beneficiaries and their index hospitalizations, stratified by MCC definition. We assessed agreement between each pair-wise combination of MCC definitions using Cohen's Kappa statistics.35 We created Area-Proportional elliptical Venn diagrams to illustrate the subsets of beneficiaries with MCC as defined by each measure in comparison with the subset of beneficiaries who experienced 30-day hospital readmissions. Venn diagrams were drawn using eulerAPE version 3 software36 and Microsoft PowerPoint. As a sensitivity analysis to further understand the implications of our choice to use a limited number of c-SNP-defined HCCs rather than all 79 HCCs, we also created a Venn diagram comparing the subset of beneficiaries with cSNP-defined MCC (≥2 of 15 conditions) with the subset of beneficiaries with MCC defined by total HCCs (≥2 of 79 conditions) in relation to 30-day hospital readmissions.
To determine the relationship between MCC category and 30-day hospital readmissions, we calculated the sensitivity, specificity, and likelihood ratio estimates for each MCC measure with respect to the primary outcome. Likelihood ratios were calculated from receiver operating curve analysis.37 Lastly, we used multivariable logistic regression to assess the ability of each MCC definition to predict 30-day hospital readmission, adjusting for baseline patient characteristics (age, sex, race, Medicaid status), index hospitalization characteristics (length of stay, discharge to skilled nursing facility, number of hospital beds, hospital type), and baseline year utilization (emergency department visits, hospitalizations, outpatient visits). After identifying the two MCC definitions most predictive of 30-day hospital readmission, we identified the individual chronic conditions within those definitions that had the highest positive likelihood ratios for predicting 30-day hospital readmission. We conducted sensitivity analyses to understand the ability of cutoffs other than ≥2 chronic conditions to predict 30-day hospital readmissions by using discrete chronic condition counts in receiver operating curve analyses, adjusted for the same variables as the logistic regression. Analyses were performed using SAS, version 9.4 (SAS Institute) and STATA, version 13.1 (StataCorp LP). There was less than 1% missing data (Table 2).
Table 2.
Baseline Characteristics of Medicare Beneficiaries and their Index Hospital Admissions by Varying Definitions of Multiple Chronic Conditions (MCC)
| Total Beneficiaries (n=710,609) | ≥2 CCW-Defined Conditionsa (n=660,358) | ≥2 CCI-Defined Conditionsa (n=261,168) | ≥2 ACG®-Defined Conditionsa (n=132,306) | ≥2 c-SNP-Defined Conditionsa (n=446,220) | |
|---|---|---|---|---|---|
| Total Medicare Beneficiaries (n, % total beneficiaries) | 710,609 (100.0) | 660,358 (92.9) | 261,168 (36.8) | 132,306 (18.6) | 446,220 (62.8) |
| Age (median years, IQR) | 78 (72-85) | 79 (73-85) | 79 (73-85) | 80 (74-86) | 79 (73-85) |
| Female (n, %) | 450,827 (63.4) | 424,435 (64.3) | 154,540 (59.2) | 81,245 (61.4) | 272,169 (61.0) |
| Race | |||||
| White (n, %) | 631,011 (88.8) | 586,157 (88.8) | 223,980 (85.8) | 114,197 (86.3) | 391,036 (87.6) |
| Black (n, %) | 52,592 (7.4) | 49,087 (7.4) | 26,073 (10.0) | 12,997 (9.8) | 37,327 (8.4) |
| Other (n, %) | 27,006 (3.8) | 25,114 (3.8) | 11,115 (4.3) | 5,112 (3.9) | 17,857 (4.0) |
| Enrolled in Medicaid (n, %) | 119,525 (16.8) | 114,807 (17.4) | 61,303 (23.5) | 30,918 (23.4) | 91,315 (20.5) |
| Hospital admissions in 12 months prior to index admission (median n, IQR) | 0 (0-1) | 0 (0-1) | 1 (0-2) | 2 (1-3) | 0 (0-1) |
| Emergency department visits in 12 months prior to index admission(median n, IQR) | 0 (0-1) | 0 (0-1) | 0 (0-1) | 1 (0-1) | 0 (0-1) |
| Clinic visits in 12 months prior to index admission (median n, IQR) | 9 (5-14) | 9 (6-15) | 12 (8-19) | 13 (8-20) | 11 (7-17) |
| Index Admission Length of Stay (median days, IQR) | 4 (2-6) | 4 (2-6) | 4 (3-7) | 4 (3-7) | 4 (2-7) |
| Index Admission Hospital Typeb,c | |||||
| Non-profit (n, %) | 520,770 (73.4) | 484,264 (73.5) | 192,035 (73.7) | 96,731 (73.3) | 326,898 (73.4) |
| For-profit (n, %) | 93,190 (13.1) | 86,723 (13.2) | 34,321 (13.2) | 17,738 (13.4) | 59,203 (13.3) |
| Public (n, %) | 95,126 (13.4) | 87,960 (13.4) | 34,276 (13.2) | 17,549 (13.3) | 59,170 (13.3) |
| Index Hospital Total Beds (median n, IQR)c | 314 (168-497) | 314 (168-494) | 317 (173-502) | 316 (172-504) | 317 (172-502) |
| Discharged to Skilled Nursing Facility (SNF) from Index Admission (%) | 154,408 (21.7) | 149,680 (22.7) | 71,495 (27.4) | 40,112 (30.3) | 114,145 (25.6) |
| 30-Day Post-Discharge Mortality (%) | 60,402 (8.5) | 57,777 (8.8) | 34,479 (13.2) | 18,997 (14.4) | 49,730 (11.4) |
| 30-Day Hospital Readmission (%) | 82,504 (11.6) | 78,746 (11.9) | 44,245 (16.9) | 26,860 (20.3) | 63,886 (14.3) |
Chronic Condition Data Warehouse (CCW), Charlson Comorbidity Index (CCI), Johns Hopkins Adjusted Clinical Groups® (ACG®) Case-Mix System, Medicare Advantage Special Needs Plan Chronic Conditions (c-SNP)
Index Admission Hospital Type is based on the Provider of Service (POS) file 2 digit codes. Non-profit includes church (01), private (02), and other (03) voluntary non-profit hospitals. For-profit includes proprietary (04) hospitals. Public includes federal (05), state (06), local (07), and hospital district or authority (08) government hospitals.
Missing Data: There were 1,523 observations (0.21%) missing from the Provider of Service file for “Index Admission Hospital Type.” There were 1,518 (0.21%) observations missing from the POS file for “Index Hospital Total Beds.”
RESULTS
Degree of Agreement among MCC Definitions
The study sample included 710,609 Medicare beneficiaries who experienced at least one hospitalization from 1/1/2005 to 12/1/2009. Depending on MCC definition, the prevalence of MCC ranged from 18.6% (ACG) to 92.9% (CCW) (Table 2). Comparing of baseline beneficiary characteristics by MCC definition, patients with ACG-defined and CCI-defined MCC had slightly higher Medicaid enrollment, higher hospice enrollment, clinic visits in the 12 months prior to admission, and discharges to skilled nursing facilities. Overall, there was slight (0.03 between CCW and ACG) to moderate (0.44 between CCI and c-SNP) agreement between pair-wise combinations of MCC definitions in regard to which beneficiaries were categorized as having MCC or not having MCC (Supplemental Appendix 1).
Degree of Overlap between MCC and 30-Day Readmission by MCC Definition
The subsets of beneficiaries with MCC as defined by each measure in comparison with the subset of beneficiaries who experienced 30-day hospital readmissions are illustrated in Figure 1. CCW offered the most inclusive definition with CCI-defined, ACG-defined, and c-SNP-defined MCC forming population subsets almost entirely within CCW-defined MCC. CCW-defined, CCI-defined, ACG-defined, and c-SNP-defined MCC overlapped with 11.1%, 6.3%, 3.7%, and 8.6% of the 11.6% of total Medicare beneficiaries experiencing 30-day hospital readmission, respectively. While CCW-defined MCC identified the largest proportion of beneficiaries who experienced 30-day hospital readmissions, it also identified largest proportion of beneficiaries who did not experience a 30-day hospital readmission (81.9%).
Figure 1 (grayscale). Venn Diagrams Illustrating Intersections between Different Definitions of Baseline Multiple Chronic Conditions (MCC) and Future 30-Day Hospital Readmission.
Chronic Condition Data Warehouse (CCW); Charlson Comorbidity Index (CCI); Johns Hopkins Adjusted Clinical Groups® (ACG®) Case-Mix System; Medicare Advantage Special Needs Plan Chronic Conditions (c-SNP). Percentages are with respect to the total population (n=710,609).
1a. Venn diagram illustrating the intersection of Medicare beneficiaries with multiple chronic conditions, as defined by CCW (black) and CCI (gray), with beneficiaries who experienced 30-day hospital readmissions (white).
1b. Venn diagram illustrating the intersection of Medicare beneficiaries with multiple chronic conditions, as defined by CCW (black) and ACG (gray), with beneficiaries who experienced 30-day hospital readmissions (white).
1c. Venn diagram illustrating the intersection of Medicare beneficiaries with multiple chronic conditions, as defined by CCW (black) and c-SNP (gray), with beneficiaries who experienced 30-day hospital readmissions (white).
1d. Venn diagram illustrating the intersection of Medicare beneficiaries with multiple chronic conditions, as defined by c-SNP (dark gray) and CCI (light gray), with beneficiaries who experienced 30-day hospital readmissions (white).
Ability of MCC Definitions to Predict 30-Day Hospital Readmission
Having CCW-defined MCC was the most sensitive, but least specific predictor of having a 30-day hospital readmission (Table 3). Conversely, having ACG-defined MCC was the least sensitive and most specific predictor of having a 30-day hospital readmission. In the adjusted logistic regressions, having CCI-defined MCC and c-SNP-defined MCC were most closely associated with 30-day hospital readmission. The odds of having a 30-day hospital readmission increased 45% for beneficiaries with CCI-defined MCC and 50% for beneficiaries with c-SNP-defined MCC. In sensitivity analyses where the same multivariable logistic regression models were run with chronic condition counts, rather than dichotomous MCC status, the Receiver Operating Characteristic (ROC) Area under the Curve remained the highest for CCI-defined and c-SNP-defined chronic condition counts (Supplemental Appendix 2).
Table 3.
Sensitivity, Specificity, and Likelihood Ratios of Different Definitions of Multiple Chronic Condition (MCC) Identifying Patients who Experienced 30-Day Hospital Readmissions
| ≥2 CCW-Defined Conditionsa | ≥2 CCI-Defined Conditionsa | ≥2 ACG®-Defined Conditionsa | ≥2 c-SNP-Defined Conditionsa | |
|---|---|---|---|---|
| Sensitivity | 95.4% | 53.7% | 32.7% | 77.3% |
| Specificity | 7.4% | 65.5% | 83.2% | 39.2% |
| Positive Likelihood Ratio | 1.0 | 1.6 | 1.9 | 1.3 |
| Negative Likelihood Ratio | 0.6 | 0.7 | 0.8 | 0.6 |
Chronic Condition Data Warehouse (CCW), Charlson Comorbidity Index (CCI), Johns Hopkins Adjusted Clinical Groups® (ACG®) Case-Mix System, Medicare Advantage Special Needs Plan Chronic Conditions (c-SNP)
Most Predictive Chronic Conditions within MCC Definitions
Within the CCI measure, having moderate-severe liver disease (LR+ 2.86), renal disease (LR+ 2.06), or metastatic cancer (LR+ 2.00) as comorbidities had the highest positive likelihood ratios for predicting 30-day hospital readmission. Within the c-SNP measure, having end-stage renal disease (LR+ 2.83), end-stage liver disease (LR+ 2.40), substance abuse (LR+ 1.66), or a hematologic condition (LR+ 1.66) as comorbidities had the highest positive likelihood ratios for prediction 30-day hospital readmission. A complete list of the likelihood ratios for individual chronic conditions within the c-SNP, CCI, and CCW definitions of MCC is displayed in Supplemental Appendix 5.
DISCUSSION
Comparing four commonly used definitions of MCC within the same population of Medicare beneficiaries demonstrated fair to poor agreement for classifying individuals as having or not having MCC. While we expected low agreement, our hypothesis that the definitions including the greatest number of possible chronic conditions would be the most sensitive, but least specific predictors of 30-day hospital readmission was incorrect. CCW-defined MCC (≥2/21 conditions) was the most sensitive and ACG-defined MCC (≥2/119 Expanded Diagnosis Clusters) was the most specific. The two definitions with the greatest agreement, CCI conditions and c-SNP conditions, also demonstrated the greatest discriminatory power for differentiating individuals who would experience 30-day hospital readmissions from those who would not.
Even though all of the definitions intended to identify Medicare beneficiaries with ≥2 chronic conditions, there was a large disparity in the prevalence of MCC between different measures. Our results confirm that different MCC definitions cannot be used interchangeably. There are clinically relevant implications to methodological differences in how these definitions are operationalized that need to be taken into account when applying these definitions to case finding in clinical practice. For example, in the context of a hospital-based transitional care program attempting to identify individuals at highest risk of 30-day hospital readmission, the high specificity of the ACG EDCs and CCI conditions reflects more stringent selection criteria. The ACG stringent diagnostic certainty option required individuals to have more than one diagnosis code during the baseline year to be classified as having certain EDC conditions. Similarly, the CCI methodology required one inpatient or two outpatient diagnosis codes meeting criteria for a particular condition in order for an individual to be classified as having that condition. The high prevalence of CCW-defined MCC in this population is related to the broadly inclusive criteria inherent to this classification system, resulting in low ability to distinguish between individuals who would or would not experience 30-day hospital readmission. Therefore, using CCW-defined MCC in a hospital setting would be less likely to assist in identifying individuals at risk for 30-day readmission who could benefit from transitional care interventions. This finding is consistent with publicly available CMS reports, in which Medicare beneficiaries with MCC (as defined by CCW conditions) account for 98% of all hospital readmissions.2 A characteristic feature of the CCW classification system is its ability to identify individuals with any history of a single diagnosis code in their lifetime Medicare enrollment. In contrast, the other classification systems were only applied to Medicare claims from the baseline year. As a result, the MCC definitions identifying individuals with recent claims may have conditions requiring more active management while the CCW classification system may be more likely to identify inactive disease.
These finding further suggest that types of chronic conditions included in different MCC definitions may be important factors in their abilities to identify individuals who would experience 30-day hospital readmissions. Nine of the 15 conditions composing the highest-performing MCC definition (c-SNPs) are shared by the next best performing MCC definition (CCI). Different forms of liver disease and kidney disease are the individual conditions within each definition most predictive of readmission. The higher likelihood ratios associated with these conditions suggest that having either liver or kidney disease as a comorbidity increases the risk of 30-day readmission by 15-20% above one's initial “pre-test probability.” This finding is consistent with other research that found patients with chronic kidney disease as a comorbidity, rather than as the primary diagnosis for an index hospitalization, were at highest risk of potentially avoidable hospital readmissions.12 Decline in kidney or liver function are known risk factors for medication errors,38 and adverse drug events are common reasons for acute care encounters among older adults.39,40
These findings have important implications for clinicians and policy-makers. The unique features of the CCW “lifetime look-back” period may be most representative of a clinician's perspective of a patient's lifetime accumulation of chronic conditions. When clinicians are identifying patients with ≥2 chronic conditions “that confer a significant risk of death, decompensation, or functional decline” as required to be eligible for Medicare's chronic care management services, it will be important to consider the need for active management of those conditions in the prior year in order to identify patients who are at highest risk of poor health outcomes. Similarly, CCW conditions are analogous to past medical histories and problem lists that accumulate diagnosis codes in electronic medical records (EMRs). If EMRs are designed to identify patients with MCC in the future, it will be important to consider the EMR's ability to distinguish between active and inactive chronic conditions. Identifying patients with actively managed chronic conditions who have had claims related to that condition in the prior 12 months may be a better strategy for identifying individuals at risk of 30-day readmission than identifying patients with a lifetime accumulation of certain conditions.
Additionally, more detailed classification that accounts for disease severity, rather than just presence or absence of a condition, may facilitate identification of individuals with MCC who are at risk of poor health outcomes. The 15 c-SNP conditions were specifically selected to represent “severe and disabling chronic conditions,” and several CCI conditions are distinguished by severity. In contrast, our study suggests that CCW-defined conditions, which do not account for disease severity, have low specificity for identifying patients at high risk for poor health outcomes. By focusing on individuals with MCC who have conditions likely to result in 30-day readmissions, health systems may be able to better manage their high-cost populations by offering upstream interventions to prevent poor outcomes. As new quality metrics are applied to patient populations with MCC, such as the “risk-standardized acute admissions rates for patients with MCC” that was applied to Accountable Care Organizations (ACOs) starting in 2015, it will be increasingly important to use a consistent definition of MCC. Eight CCW conditions (with a range of 1-3 years of “lookback” for eligible diagnosis codes) are currently used to define the patient population with MCC for this ACO quality metric.41 However, the current MCC definition omits liver disease, which was found to be an important component of MCC definitions in this study. With increasing services and quality metrics targeted toward patients with MCC, it may be advantageous for clinicians and policy-makers to use MCC measures that account for both active management and disease severity, such as c-SNP or CCI, in order to match interventions with patients at highest risk of poor health outcomes.
While CCW-defined MCC was the most sensitive MCC measure and ACG-defined MCC was the most specific measure, CCI-defined and c-SNP-defined MCC measures performed better at distinguishing between individuals who would have 30-day hospital readmission and those who would not. A balance between sensitivity and specificity is necessary to identify “high-risk” individuals for health service interventions, and that balance may need to be optimized in the context of the specific health outcomes that a program is trying to impact.
Limitations
While this study used a nationally representative cohort of Medicare beneficiaries, there are limitations inherent in the retrospective design. Baseline data on chronic conditions were originally collected for billing rather than research purposes, a common limitation to health services research. Access to and utilization of the health care system is required to receive medical diagnoses. Those with more inpatient and outpatient visits in the baseline year have more opportunity to acquire diagnoses and are at higher risk for future health care utilization, including our primary outcome of 30-day hospital readmissions. In addition to adjusting the analytic models for baseline utilization, we mitigated this limitation by ensuring that all patients included in the cohort had at least one inpatient or two outpatient or emergency department visits in the baseline year so that every patient had a similar minimum threshold of opportunities to acquire diagnoses. However, this inclusion criteria limits the generalizability of the study to Medicare beneficiaries with lower levels of baseline health care utilization. In addition, there are other chronic condition classification systems beyond the four examined in this paper that are worthy of further study.4 Finally, while this study focused on 30-day hospital readmissions, future studies are needed to investigate the comparative abilities of these MCC definitions in predicting other important outcomes such as morbidity, mortality, post-acute care utilization, and overall cost of care.
Conclusion
In conclusion, common definitions for identifying individuals with MCC demonstrate major differences and poor agreement. If seeking reliable approaches for identifying patients with MCC at high risk for 30-day hospital readmission, the c-SNP conditions and CCI conditions demonstrate the most discriminatory power among the classification systems we tested. Further research is needed to incorporate more discriminatory comorbidity measures into full readmission risk prediction models that contain multiple risk factors for hospitalization including functional status.42 Currently, c-SNP conditions are rarely used outside of Medicare Advantage health plans43 and they warrant further study as a means for identifying individuals for readmissions reductions programs or other care coordination services.
Supplementary Material
Table 4.
Odds of 30-Day Readmission Risk for Medicare Beneficiaries with Multiple Chronic Conditions (MCC) Compared to Beneficiares without MCC, by Different Definitions of Multiple Chronic Conditions (MCC)
| ≥2 CCW-Defined Conditionsa | ≥2 CCI-Defined Conditionsa | ≥2 ACG®-Defined Conditionsa | ≥2 c-SNP-Defined Conditionsa | |
|---|---|---|---|---|
| Unadjusted OR (95% CI) | 1.68 (1.62 - 1.73) | 2.19 (2.16 - 2.22) | 2.39 (2.35 - 2.43) | 2.21 (2.17 - 2.24) |
| Adjusted OR (95% CI) for baseline patient and index hospital characteristicsb | 1.45 (1.40 - 1.50) | 1.95 (1.92 - 1.98) | 2.17 (2.13 - 2.20) | 1.92 (1.89 - 1.96) |
| Adjusted OR (95% CI) for baseline patient characteristics, index hospital characteristics, and and baseline year utilizationc | 1.15 (1.11 - 1.19) | 1.45 (1.42 - 1.47) | 1.22 (1.19 - 1.25) | 1.50 (1.47 - 1.52) |
Chronic Condition Data Warehouse (CCW), Charlson Comorbidity Index (CCI), Johns Hopkins Adjusted Clinical Groups® (ACG®) Case-Mix System, Medicare Advantage Special Needs Plan Chronic Conditions (c-SNP)
Adjusted for age, sex, race, Medicaid status, index hospitalization length of stay, discharge to Skilled Nursing Facility (SNF), number of hospital beds, hospital type
Adjusted for age, sex, race, Medicaid status, index hospitalization length of stay, discharge to Skilled Nursing Facility (SNF), number of hospital beds, hospital type, baseline year hospital admissions, baseline year emergency department visits, and baseline year outpatient visits.
Acknowledgments
Conflict of Interest Checklist
| Elements of Financial/Personal Conflicts | MD | ED | KR | KAK | AG-B | AJK | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | X | X | ||||||
| Grants/Funds | X | X | X | X | X | X | ||||||
| Honoraria | X | X | X | X | X | X | ||||||
| Speaker Forum | X | X | X | X | X | X | ||||||
| Consultant | X | X | X | X | X | X | ||||||
| Stocks | X | X | X | X | X | X | ||||||
| Royalties | X | X | X | X | X | X | ||||||
| Expert Testimony | X | X | X | X | X | X | ||||||
| Board Member | X | X | X | X | X | X | ||||||
| Patents | X | X | X | X | X | X | ||||||
| Personal Relationship | X | X | X | X | X | X | ||||||
For “yes”, provide a brief explanation here:
This project was supported by and all authors were affiliated with the Health Innovation Program, the UW School of Medicine and Public Health from The Wisconsin Partnership Program, and the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research (UW ICTR) through the National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. Dr. Dattalo is supported with resources and use of facilities at the Geriatric Research, Education and Clinical Center of the William S. Middleton Memorial VA Hospital in addition to American Federation for Aging Research Hartford Center of Excellence National Center of Excellence Award [PI Asthana]. Dr. DuGoff has received grant support from AcademyHealth New Investigator award and the National Institutes of Health Loan Repayment Program. Dr. Kennelty has received institutional grant support from the Department of Veterans Affairs and has served as a consultant for the Gerontological Society of America. Dr. Kind is supported by the University of Wisconsin Hospitals and Clinics; a National Institute on Aging Beeson Career Development Award (K23AG034551 [PI Kind], National Institute on Aging, The American Federation for Aging Research, The John A. Hartford Foundation, The Atlantic Philanthropies and The Starr Foundation); National Institute on Aging Award Number 2P50AG033514-06; National Institute on Minority Health and Health Disparities Research Award Number R01MD010243; National Institute on Aging Grant R01AG050504; CMS Special Innovation Project (SIP 1) Contract Number HHSM-500-2014-QIN010I-T0004; and by the Madison VA Geriatrics Research, Education and Clinical Center. Dr. Kind's time was also partially supported by the University of Wisconsin School of Medicine and Public Health from the Wisconsin Partnership Program. The contents do not represent views of the Dept. of Veterans Affairs or the United States Government.
Sponsor's Role: None.
Additional acknowledgements: We would additionally like to acknowledge Julia Loosen, our undergraduate research assistant, for assistance with reference management and manuscript formatting.
Footnotes
Related Paper Presentations: An abstract using the same data was submitted and accepted for Presidential Poster Presentation at the 2016 Annual Scientific Meeting of the American Geriatrics Society conference in Long Beach, CA.
REFERENCES
- 1.Multiple Chronic Conditions- A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions. U.S. Department of Health and Human Services; Washington, DC: 2010. [Google Scholar]
- 2.Chronic Conditions among Medicare Beneficiaries, Chartbook. Centers for Medicare and Medicaid Services; Baltimore, MD: 2012. [Google Scholar]
- 3.Lochner KA, Goodman RA, Posner S, Parekh A. Multiple Chronic Conditions Among Medicare Beneficiaries: State-level Variations in Prevalence, Untilization, and Cost, 2011. Medicare Medicaid Res Rev. 2013;3:E1–E19. doi: 10.5600/mmrr.003.03.b02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and Measuring Chronic Conditions: Imperatives for Research, Policy, Program, and Practice. Preventing Chronic Disease. 2013;10:E66. doi: 10.5888/pcd10.120239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards ST, Landon BE. Medicare's Chronic Care Management Payment — Payment Reform for Primary Care. New England Journal of Medicine. 2014;371:2049–2051. doi: 10.1056/NEJMp1410790. [DOI] [PubMed] [Google Scholar]
- 6.Kind AJ, Jensen L, Barczi S, et al. Low-cost transitional care with nurse managers making mostly phone contact with patients cut rehospitalization at a VA hospital. Health Aff (Millwood) 2012;31:2659–2668. doi: 10.1377/hlthaff.2012.0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Annals of internal medicine. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 9.Bixby MB, Naylor MD. The transitional care model (TCM): hospital discharge screening criteria for high risk older adults. Medsurg Nurs. 2010;196:62–63. [PubMed] [Google Scholar]
- 10.Goodell S, Bodenheimer TS, Berry-Millett R. Care Management of Patients with Complex Health Care Needs. Princeton, NJ: 2009. [PubMed] [Google Scholar]
- 11.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. Jama. 2011;306:1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donze J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ. 2013;347:f7171. doi: 10.1136/bmj.f7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berkowitz SA, Anderson GF. Medicare beneficiaries most likely to be readmitted. J Hosp Med. 2013;8:639–641. doi: 10.1002/jhm.2074. [DOI] [PubMed] [Google Scholar]
- 14.Billings J, Dixon J, Mijanovich T, Wennberg D. Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients. BMJ (Clinical research ed) 2006;333:327. doi: 10.1136/bmj.38870.657917.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Pope GC, Kautter J, Ingber MJ, Freeman S, Sekar R, Newhart C. Evaluation of the CMSHCC Risk Adjustment Model: Final Report. RTI International. 2011 [Google Scholar]
- 17.DuGoff EH, Canudas-Romo V, Buttorff C, Leff B, Anderson GF. Multiple chronic conditions and life expectancy: a life table analysis. Medical care. 2014;52:688–694. doi: 10.1097/MLR.0000000000000166. [DOI] [PubMed] [Google Scholar]
- 18.Master Beneficiary Summary File. Volume 2016. Research Data Assistance Center; Minneapolis, MN: 2010. [Google Scholar]
- 19.Condition Categories. Chronic Conditions Data Warehouse, Volume 2016: NewWave-GDIT, LLC. 2016 [Google Scholar]
- 20.Providing and Billing Medicare for Chronic Care Management Chronic Care Management. 2015. pp. 1–13.
- 21.Wieland D, Boland R, Baskins J, Kinosian B. Five-year survival in a Program of All-inclusive Care for Elderly compared with alternative institutional and home- and community-based care. J Gerontol A Biol Sci Med Sci. 2010;65:721–726. doi: 10.1093/gerona/glq040. [DOI] [PubMed] [Google Scholar]
- 22.2008 Special Needs Plan Chronic Condition Panel: Final Report. 2008.
- 23.Medicare Improvements for Patients and Providers Act (MIPPA) of 2008. P L 110-275. United States: 2008. [Google Scholar]
- 24.Weiner J, editor. The Johns Hopkins ACG® System. Technical Reference Guide Version 9.0. The Johns Hopkins Univeristy; Baltimore, MD: 2009. [Google Scholar]
- 25.Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Medical care. 2012;50:1109–1118. doi: 10.1097/MLR.0b013e31825f64d0. [DOI] [PubMed] [Google Scholar]
- 26.Yurkovich M, Avina-Zubieta JA, Thomas J, Gorenchtein M, Lacaille D. A systematic review identifies valid comorbidity indices derived from administrative health data. J Clin Epidemiol. 2015;68:3–14. doi: 10.1016/j.jclinepi.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 27.Boeckxstaens P, Vaes B, Van Pottelbergh G, et al. Multimorbidity measures were poor predictors of adverse events in patients aged ≥80 years: a prospective cohort study. Journal of Clinical Epidemiology. 2015;68:220–227. doi: 10.1016/j.jclinepi.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 28.Farley JF, Harley CR, Devine JW. A comparison of comorbidity measurements to predict healthcare expenditures. The American journal of managed care. 2006;12:110–119. [PubMed] [Google Scholar]
- 29.Holman CD, Preen DB, Baynham NJ, Finn JC, Semmens JB. A multipurpose comorbidity scoring system performed better than the Charlson index. J Clin Epidemiol. 2005;58:1006–1014. doi: 10.1016/j.jclinepi.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 30.Zekry D, Loures Valle BH, Graf C, et al. Prospective comparison of 6 comorbidity indices as predictors of 1-year post-hospital discharge institutionalization, readmission, and mortality in elderly individuals. J Am Med Dir Assoc. 2012;13:272–278. doi: 10.1016/j.jamda.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 31.Service BCSa . Chronic Condition Data Warehouse. Centers for Medicare & Medicaid Services; West Des Moines, IA: 2009. [Google Scholar]
- 32.Chronic Condition Reference List Chronic Conditions Data Warehouse. 2006.
- 33.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 34.Taylor DH, Østbye T, Langa KM, Weir D, Plassman BL. The Accuracy of Medicare Claims as an Epidemiological Tool: The Case of Dementia Revisited. Journal of Alzheimer's disease : JAD. 2009;17:807–815. doi: 10.3233/JAD-2009-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen J. A coefficient of agreement for nominal scales. Educational and Psychological Measurement. 1960;20:37–34. [Google Scholar]
- 36.Micallef L, Rodgers P. eulerAPE: Drawing Area-Proportional 3-Venn Diagrams Using Ellipses. PLoS ONE. 2014:9. doi: 10.1371/journal.pone.0101717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choi B. Slopes of a receiver operating characteristic curve and likelihood ratios for a diagnostic test. Am J Epidemiol. 1998;148:1127–1132. doi: 10.1093/oxfordjournals.aje.a009592. [DOI] [PubMed] [Google Scholar]
- 38.Preventing Medication Errors: Quality Chasm Series. The National Academies Press; Washington, DC: 2007. [Google Scholar]
- 39.Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Annals of emergency medicine. 2001;38:666–671. doi: 10.1067/mem.2001.119456. [DOI] [PubMed] [Google Scholar]
- 40.Hafner JW, Jr., Belknap SM, Squillante MD, Bucheit KA. Adverse drug events in emergency department patients. Annals of emergency medicine. 2002;39:258–267. doi: 10.1067/mem.2002.121401. [DOI] [PubMed] [Google Scholar]
- 41.Services CfMM, editor. A Blueprint for the CMS Measures Management System, Version 9. Health Services Advisory Group, Inc; 2015. ACO #38 Risk-Standardized Acute Admission Rates for Patients with Multiple Chronic Conditions. Measure Information Form (MIF). [Google Scholar]
- 42.Shih SL, Gerrard P, Goldstein R, et al. Functional Status Outperforms Comorbidities in Predicting Acute Care Readmissions in Medically Complex Patients. J Gen Intern Med. 2015;30:1688–1695. doi: 10.1007/s11606-015-3350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cohen R, Lemieux J, Schoenborn J, Mulligan T. Medicare Advantage Chronic Special Needs Plan boosted primary care, reduced hospital use among diabetes patients. Health affairs (Project Hope) 2012;31:110–119. doi: 10.1377/hlthaff.2011.0998. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.