Abstract
Suicidal and nonsuicidal self-injurious thoughts and behaviors (SITBs) among youth are major public health concerns. Although a growing body of research has focused on the complex association between nonsuicidal and suicidal self-injury, the temporal relationship between these two classes of behaviors is unclear. The current study addresses this empirical gap by examining the course of SITBs in adolescents receiving outpatient (N = 106; 82.1 % female) and inpatient (N = 174; 75.9 % female) treatment. SITBs (co-occurrence, age-of-onset, and time lag between SITBs) and major psychiatric disorders were assessed at a single time point with well-validated structured interviews. Adolescents in both clinical samples reported high co-occurrence of SITBs: most adolescents reported both lifetime nonsuicidal self-injury (NSSI) and suicidal thoughts. A similar temporal pattern of SITBs was reported in the two samples: thoughts of NSSI and suicide ideation had the earliest age-of-onset, followed by NSSI behaviors, suicide plans, and suicide attempts. However, the age-of-onset for each SITB was younger in the inpatient sample than in the outpatient sample. In terms of time lag between SITBs, suicide ideation occurred on average before initial engagement in NSSI, suggesting that pathways to NSSI and suicidal behavior may occur simultaneously rather than in succession from nonsuicidal to suicidal self-injury. Results also indicated that the time to transition between SITBs was relatively fast, and that a key period for intervention and prevention is within the first 6–12 months after the onset of suicidal thinking. Taken together, these findings have important implications for understanding the time-lagged relationship between nonsuicidal and suicidal self-injury.
Keywords: Self-injury, Nonsuicidal self-injury, Suicide, Suicide attempts, Adolescence
Self-injurious thoughts and behaviors (SITBs) refer to a broad class of cognitions and actions aimed at directly and deliberately injuring oneself. SITBs range from nonsuicidal self-injury (NSSI) performed without intent to die (e.g., cutting, burning) to suicidal behaviors in which an individual has at least some intent to die during the self-injurious act (e.g., suicide attempts; Nock 2010). In community samples, approximately one in five adolescents report engaging in NSSI (Muehlenkamp et al. 2012) and rates exceed 40 % in clinical studies of youth (Asarnow et al. 2011; Wilkinson et al. 2011). Prevalence estimates of suicidal thoughts and behaviors also are alarmingly high among adolescents. Each year, 16 % of high school students think about suicide and 8 % attempt to take their own lives (Centers for Disease Control and Prevention [CDC] 2015). In clinical samples of youth, rates of suicidal thoughts and behaviors are more than three times higher than community rates (Asarnow et al. 2011; Wilkinson et al. 2011). SITBs are associated with significant functional impairment for youth (Glenn and Klonsky 2013; Nock et al. 2006) as well as substantial burden for the health care system. Each year in the U.S., approximately 157,000 young people ages 10–24 years will present to the emergency department for self-injurious behaviors (CDC 2015), resulting in over 200 million dollars in annual medical costs (CDC 2010).
Associations between Nonsuicidal and Suicidal Self-Injury
The relationship between nonsuicidal and suicidal self-injury is complex. Substantial research indicates key differences between these two categories of self-injury, including the level of suicide intent (absent in NSSI), prevalence (NSSI is more prevalent than suicidal behavior), frequency (NSSI is engaged in more frequently than suicide attempts), and medical lethality (NSSI does not typically require medical intervention; Grandclerc et al. 2016; Hamza et al. 2012; Nock 2010). These distinctions led to the classification of NSSI and suicidal behavior as distinct clinical phenomena in the DSM-5 (see “Conditions for Further Study;” APA 2013). At the same time, there is significant overlap between these two behaviors. Nonsuicidal and suicidal self-injury often co-occur, especially in clinical samples (Klonsky et al. 2013; Nock et al. 2006). Most notably, growing evidence indicates that NSSI is one of the most robust prospective predictors of suicide attempts, above and beyond previous suicidal behavior (Asarnow et al. 2011; Guan et al. 2012; Scott et al. 2015; Wilkinson et al. 2011).
Although research has clarified some aspects of this complex relationship, the understanding of the temporal association between nonsuicidal and suicidal self-injury remains unclear. Two key ways to understand the timing among SITBs are to examine: (1) the age-of-onset of SITBs and (2) the time lag between SITBs. An important first step is to identify the age-of-onset of the full range of nonsuicidal and suicidal self-injurious thoughts and behaviors. Previous studies have primarily focused on the age-of-onset of self-injurious behaviors (i.e., NSSI and suicide attempts) in youth (e.g., Muehlenkamp and Gutierrez 2004; Tuisku et al. 2014). However, it is essential to know when individuals begin thinking about these behaviors to identify those at greatest risk before they take action. Another key issue is to clarify the time period in which individuals transition between SITBs (e.g., escalating from suicidal ideation to suicide attempts). Improving our understanding of the age-of-onset and time lag between SITBs will, ultimately, enhance identification of at-risk individuals, clarify optimal time periods for intervention, and thereby maximize prevention efforts. Below, we review extant research on the age-of-onset and transition time between SITBs as well as the key unanswered questions.
Ages-Of-Onset of Self-Injurious Thoughts and Behaviors
Though relatively rare in childhood, rates of all SITBs increase drastically during the transition to adolescence (Nock et al. 2008b; Nock et al. 2012; Nock et al. 2013). Cross-national research indicates that NSSI behaviors most often begin between ages 12–14 years (Jacobson and Gould 2007; Whitlock et al. 2011; Zetterqvist et al. 2013), whereas suicidal thoughts and behaviors appear to have a later age-of-onset (Kessler et al. 1999; Nock et al. 2012). Although there is an increase in the onset of suicidal thoughts and behaviors starting around age 12 (Nock et al. 2013), findings from large epidemiological studies in adults in the U.S. (Kessler et al. 1999) and cross-national research in adults from the WHO World Mental Health Surveys (Nock et al. 2012) indicate that the highest period of risk for the onset of suicide ideation, plans, and attempts occurs in late adolescence or early adulthood. Taken together, previous research suggests that NSSI typically begins in early adolescence, whereas suicidal thoughts and behaviors commonly emerge in later adolescence and early adulthood.
However, it is important to note that this previous research has been limited by the use of separate samples to compare the age-of-onset of nonsuicidal self-injury with that of suicidal self-injury (i.e., within-group versus between-groups analyses). As NSSI is a robust predictor of suicidal behavior (e.g., Guan et al. 2012; Scott et al. 2015), examining the age-of-onset for SITBs within the same sample may provide critical insights for prevention. In one of the first studies to address this issue, Bryan et al. (2015) examined the age-of-onset for both nonsuicidal and suicidal SITBs (i.e., NSSI, suicide ideation, and suicide attempts) in a large sample of veterans and military personnel. In this sample, the majority of adults (67 %) reported that suicide ideation emerged before the onset of NSSI, and NSSI most often (91 %) preceded first suicide attempts. Although prior research suggests that NSSI precedes suicidal thoughts and behaviors (e.g., Jacobson and Gould 2007; Kessler et al. 1999; Nock et al. 2012), Bryan and colleagues’ findings indicate that suicide ideation may actually begin before initial NSSI engagement. This research has important implications for understanding the pathways between nonsuicidal and suicidal self-injury and the mechanisms linking these behaviors (Grandclerc et al. 2016).
Presently, little is known about the age-of-onset of both nonsuicidal and suicidal SITBs in the same sample of adolescents—the developmental period when these thoughts and behaviors typically emerge (Nock et al. 2008b; Nock et al. 2013). Moreover, even less is known about differences between outpatients and more clinically acute psychiatric inpatients. Given that the age-of-onset of psychiatric disorders and clinically relevant behaviors is typically younger in more clinically severe samples (Carter et al. 2003; Moor et al. 2012; Zisook et al. 2007), it is likely that these patterns will emerge at younger ages as psychiatric symptomatology becomes more severe.
Time Lag between Self-Injurious Thoughts and Behaviors
The majority of previous research has focused on clarifying the time lag between suicidal thoughts and behaviors (e.g., suicide ideation to attempt). Results indicate that one-third of adolescents (Nock et al. 2013) and adults (Nock et al. 2008a) who think about suicide will go on to make a suicide plan, and approximately one-third of individuals who think about suicide will make a suicide attempt. Most adolescents and adults who make the transition from suicidal thinking to suicidal action will do so within one year after suicide ideation onset (Kessler et al. 1999; Nock et al. 2013). Bryan et al. (2015) conducted one of the first examinations of the time lag between the onset of NSSI and suicidal thoughts and behaviors. Using a one-time, retrospective assessment, they found that, among adults, the transition from suicide ideation to NSSI, on average, occurred within one year, and from NSSI to suicide attempts within approximately 4.5 years. However, results from this study should be interpreted with caution due to the small sample sizes (e.g., NSSI to suicide attempts, n = 10), and, critically, it is unclear how these results would generalize to adolescents.
Current Study
The purpose of the current study was to improve our understanding of the age-of-onset and time lag between nonsuicidal and suicidal SITBs in adolescents. For this study, adolescents who had engaged in at least one SITB were assessed at a single time point about their SITB history. To examine the generalizability of these findings across the continuum of care, the study included two samples of youth receiving mental health treatment: community-based outpatients and clinically acute inpatients. First, we predicted higher rates—both occurrence and co-occurrence—of all SITBs in adolescent inpatients. Second, we examined the age-of-onset for both nonsuicidal and suicidal SITBs. Consistent with prior research (e.g., Jacobson and Gould 2007; Kessler et al. 1999; Nock et al. 2012), we hypothesized that NSSI would have an earlier age-of-onset than suicide attempts. Moreover, in line with recent research (Bryan et al. 2015), we predicted that suicide ideation would have an earlier age-of-onset than NSSI. In terms of clinical severity, we hypothesized that the pattern of SITBs would be the same in both samples (i.e., same order of onset), however, inpatients would have an earlier age-of-onset for all SITBs relative to the outpatients. Third, we examined the time lag between each of the SITBs—that is, the average length of time to transition from one self-injurious thought or behavior to the next. Consistent with prior research (Nock et al. 2008a; Nock et al. 2013), we predicted that adolescents would report approximately one year between: (a) the onset of suicide ideation and suicide plans and (b) suicide plans and first suicide attempts. Further, we predicted that adolescents would report less than a year between the onset of suicide ideation and NSSI.1
Method
Sample 1. Adolescents Receiving Outpatient Mental Health Treatment
Participants and Procedure
Participants were recruited in the northeastern United States from a large, ongoing study focused on identifying objective risk markers of suicidal behaviors in youth. Eligible participants were aged 12–19 years old, fluent in English, and were either diagnosed with a current mood or anxiety disorder or were currently receiving mental health treatment. Exclusion criteria included inability to provide informed assent or consent, cognitive impairment, pervasive developmental disorder or major neurological disorder, extreme agitation, acute psychosis, risk of violence, or imminent risk for suicide. Based on these criteria, 158 adolescents were enrolled in the study between December 2012 and June 2015. Given our focus on the relationships among SITBs, participants were only included in the current analyses if they had a history of any SITB (see Measures section for list of SITBs and definitions). Of the total sample, 52 participants were excluded from the study analyses for the following reasons: significant cognitive impairment not apparent during initial screening (n = 6), incomplete study measures (n = 2), absence of a major psychiatric disorder or mental health treatment history (n = 5), no history of SITBs (n = 25), or inconsistent reporting of lifetime SITBs during the 6-month or 12-month follow-up interview (e.g., initially reported no previous suicide attempt but reported a lifetime attempt during one of the follow-up interviews; n = 14).
The final outpatient sample for the current study consisted of 106 adolescents: 82.1 % female. The average age of the sample was 17.60 years (SD = 1.65), and the ethnic composition was 70.8 % Caucasian, 7.5 % Asian, 5.7 % Hispanic, 2.8 % African American, 0.9 % American Indian, and 12.3 % mixed ethnicity/other ethnic group. In terms of yearly household income, 19.8 % reported $40,000 or less, 30.2 % reported $40–80,000, and 48.1 % reported $80,000 or more (one participant did not report). Excluded individuals were slightly younger (M = 16.63, SD = 2.08) than the participants included in the sample (Mann-Whitney U = 1984.00, z = −2.94, p = .003). However, there were no differences between included and excluded participants in terms of gender, χ2(2, N = 158) = 3.26, p = .196, ethnicity (minority vs. non-minority), χ2(1, N = 158) = 0.003, p = .959, or household income, χ2(3, N = 157) = 1.04, p = .792. Major DSM-IV psychiatric disorders in the sample are summarized in Table 1.
Table 1.
Axis I disorder diagnoses1 in the psychiatric outpatient and inpatient adolescent samples
| Outpatients (N = 106) | Inpatients (N = 174) | Group comparison2
|
|||
|---|---|---|---|---|---|
| % (n) | % (n) | Chi square (χ2) | p | ES (Φ) | |
| Anxiety Disorder | 68.9 % (73) | 66.1 % (115) | 0.23 | 0.631 | 0.029 |
| ADHD | 10.4 % (11) | 14.4 % (25) | 2.53 | 0.283 | 0.095 |
| Bipolar Disorder | 0.0 % (0) | 4.6 % (8) | 4.97 | 0.026 | 0.133 |
| Depressive Disorder | 44.3 % (47) | 50.6 % (88) | 1.03 | 0.311 | 0.061 |
| DBD | 19.8 % (21) | 1.7 % (3) | 27.50 | <0.001 | 0.313 |
| Eating Disorder | 9.4 % (10) | 4.0 % (7) | 5.10 | 0.078 | 0.135 |
| OCD | 6.6 % (7) | 8.0 % (14) | 0.20 | 0.657 | 0.027 |
| PTSD | 20.8 % (22) | 20.1 % (35) | 0.02 | 0.897 | 0.008 |
| Psychotic Disorder | 0.9 % (1) | 0.0 % (0) | 3.31 | 0.191 | 0.109 |
| SUD | 34.0 % (36) | 11.5 % (20) | 22.80 | <0.001 | 0.285 |
Anxiety disorder includes any of the following current disorders: panic disorder, agoraphobia, social phobia, specific phobia, or generalized anxiety disorder; ADHD = Attention-Deficit Hyperactivity Disorder includes any of the following current subtypes: combined, inattentive, or hyperactive/impulsive; Bipolar Disorder includes current bipolar I or II disorder; Depressive Disorder includes current major depressive disorder or dysthymia; DBD = Disruptive Behavior Disorder includes current conduct disorder or oppositional defiant disorder; Eating Disorder includes current anorexia nervosa or bulimia nervosa; OCD = Obsessive Compulsive Disorder; PTSD = Posttraumatic Stress Disorder; SUD = Substance Use Disorder includes current alcohol abuse/dependence or substance (drug) abuse/dependence
Categorical group differences were examined using Pearson chi-square (χ2 ) tests (n = 280) and Cramer’s phi coefficients (Φ) for effect size
All study procedures were approved by the University’s Institutional Review Board (IRB). Consent was obtained from parent/legal guardians and youth 18–19 years of age, and assent was received from adolescents aged 13–17 years. Participants completed all Time 1 study measures described in this paper in one laboratory visit and were remunerated at the end of lab session. Adolescents also completed 6- and 12-month follow-up assessments. For the current project, these follow-up assessments were used to confirm the SITBs reported at baseline.
Sample 2. Adolescents Receiving Inpatient Mental Health Treatment
Participants and Procedure
Participants were recruited in the northeastern United States from a larger quality assurance study focused on identifying mechanisms leading to nonsuicidal and suicidal SITBs. Participants were adolescents, 13–18 years old, admitted to the adolescent inpatient treatment program between June 2012 and December 2013. Based on these criteria, 195 adolescents were enrolled in the study. Similar to Sample 1, participants only were included in the current analyses if they had a history of any SITB. Of the total sample, 21 participants were excluded from the study analyses for the following reasons: no history of SITBs (n = 11), missing SITB information (n = 7), inconsistent reporting of lifetime SITBs during the clinical interview (n = 2), or a psychiatric condition due to a medical disorder or organic cause (n = 1).
The final inpatient sample for the current study consisted of 174 adolescents: 75.9 % female. The average age of the sample was 15.54 years (SD = 1.32) and the ethnic composition was 78.2 % Caucasian, 9.2 % Asian, 2.9 % African American, 0.6 % American Indian, 0.6 % Native Hawaiian/Pacific Islander, and 8.0 % mixed ethnic background (one person did not report their ethnic background). In terms of yearly household income, 7.5 % reported $25,000 or less, 21.8 % reported $25–75,000, and 32.2 % reported $100,000 or more. Income information was missing for 38.5 % of the sample. Therefore, we also examined parental education as a measure of socioeconomic status. In this sample, 5.7 % of mothers/female guardians had not finished high school, 20.1 % finished high school/GED, had some type of vocational or trade schooling, or some college, and 70.7 % had a 4-year degree or higher (six participants did not report mother’s educational background). There were no differences between included and excluded participants in terms of age, t(193) = 0.21, p = .837, gender, χ2(1, N = 195) = 1.92, p = .166, ethnicity (minority vs. non-minority), χ2(1, N = 194) = 1.52, p = .217, household income, χ2(1, N = 120) = 0.18, p = .915, or mother’s educational background, χ2(1, N = 188) = 0.44, p = .803. Major DSM-IV psychiatric disorders in the sample are summarized in Table 1.
Study procedures were approved by the appropriate hospital’s IRB. Consent was obtained from parent/legal guardians and youth 18 years of age and older, and assent was received from adolescents aged 13–17 years. Participants completed assessments included in the current study within 48 h of admission to treatment.
Measures
The same interview measures were used in both samples. In the outpatient sample, the interview measures were administered by a clinical psychologist (Ph.D.). In the inpatient sample, the interviews were administered by post-baccalaureate research assistants, masters-level graduate students, or doctoral-level graduate students, who all completed 40 h of didactic and practical training with a board-certified, licensed clinical psychologist.
Self-Injurious and Suicidal Thoughts and Behaviors
The Self-Injurious Thoughts and Behaviors Interview (SITBI; Nock et al. 2007) is a structured interview used to measure the presence, frequency, and age-of-onset (in years) of nonsuicidal and suicidal self-injurious thoughts and behaviors including: (a) nonsuicidal (NSSI) thoughts: “Have you had thoughts of purposely hurting yourself without wanting to die?” (e.g., by cutting or burning), (b) NSSI behaviors: “Have you actually purposely hurt yourself without wanting to die? “, (c) suicide ideation: “Have you had thoughts of killing yourself? “, (d) suicide plans: “Have you actually made a plan to kill yourself? “, (e) aborted attempts: “Have you been close to killing yourself and at the last minute decided not to? “, (f) interrupted attempts: “Have you been very close to killing yourself and at the last minute someone or something else stopped you? “, (g) suicide attempts: “Have you made an actual attempt to kill yourself in which you had at least some intent to die? “, and (h) suicide gestures: “Have you done something to make someone believe that you wanted to kill yourself when you actually did not want to? “ The SITBI has demonstrated sound psychometric properties, including excellent interrater reliability (average κ = .99), strong test-retest reliability across a 6-month period (average κ = .70), strong parent-adolescent agreement on the presence of suicide ideation, suicide plans, suicide attempts, and NSSI, and construct validity with respect to other measures of suicide ideation (average κ = .54), suicide attempts (κ = .65), and NSSI (average κ = .87; Nock et al. 2007). The SITBI has been used in a number of previous studies to assess SITBs among inpatient (Auerbach et al. 2015; van Alphen et al. in press) and community/outpatient adolescent samples (Barrocas et al. 2012; Nock et al. 2009). Notably, examination of SITBs using a structured interview allowed for follow-up questions and resolution of misunderstandings that commonly occur using brief self-report methodologies (Millner et al. 2015; Nock and Kessler 2006).
Psychiatric Disorders
Major DSM-IV psychiatric disorders were assessed with the Mini-International Neuropsychiatric Interview for Children and Adolescents, Child Version (MINI-Kid; Sheehan et al. 2009) in both samples. The MINI-Kid is a brief structured diagnostic interview that assesses the main clinical conditions diagnosed during childhood and adolescence. The MINI-Kid has demonstrated good to excellent test-retest and interrater reliability, as well as good to excellent concordance with longer semi-structured clinical interviews, such as the Schedule for Affective Disorders and Schizophrenia for School-Age Children (Sheehan et al. 2010). Moreover, the MINI-Kid has been utilized in previous studies to assess major psychiatric disorders in both inpatient (Glenn and Klonsky 2013; Stewart et al. 2015) and community/outpatient samples of children and adolescents (Kar and Bastia 2006; Wilkinson et al. 2008). In the outpatient sample, the MINI-Kid was conducted with the adolescent and parent/legal guardian separately, whereas only the adolescent completed the MINI-Kid in the inpatient sample. For consistency across samples, only adolescent reports were compared across samples (see Table 1).
Data Analytic Plan
Occurrence (i.e., presence/absence) and co-occurrence of SITBs were examined within the two samples separately and compared across samples using Pearson chi-square tests and Cramer’s phi coefficients for effect size. The age-of-onset of SITBs was reported for each sample separately and compared across samples using Mann-Whitney U tests and rank-biserial correlation for effect size. Time lag between SITBs was examined by computing difference scores using the reported age-of-onset for each SITB. For instance, to calculate the transition from NSSI to suicide ideation, we subtracted the age-of-onset for NSSI from the age-of-onset for suicide ideation. Positive values would indicate that, on average, suicide ideation had its onset after NSSI, whereas negative values would indicate that, on average, suicide ideation had its onset before NSSI. The time lag between SITBs was examined in each sample separately and then compared across samples using independent samples t-tests and Cohen’s d for effect size.
Results
Occurrence and Co-Occurrence of Self-Injurious Thoughts and Behaviors
Participants in both samples were only included if they had any lifetime history of SITBs. Therefore, estimates should not be considered prevalence rates of SITBs, but instead rates of specific SITBs in self-injuring samples. The most commonly reported SITBs in both samples were suicide ideation (outpatients: 88.7 %; inpatients: 96.6 %), followed by NSSI thoughts (outpatients: 85.8 %; inpatients: 90.2 %), and NSSI behaviors (outpatients: 79.2 %; inpatients: 83.9 %; Table 2). Almost all SITBs (except for suicide gestures) were more prevalent among adolescents receiving inpatient treatment, but only suicide ideation and suicide plans were significantly higher in the inpatient group.
Table 2.
Lifetime prevalence and age-of-onset of self-injurious thoughts and behaviors (SITBs) in the two adolescent samples
| Lifetime SITBs | Outpatients (N = 106) | Inpatients (N = 174) | Group comparison1
|
||
|---|---|---|---|---|---|
| % (n) | % (n) | Statistical Test (χ2) | p | ES (Φ) | |
| NSSI Thoughts | 85.8 % (91) | 90.2 % (157) | 1.25 | 0.264 | 0.067 |
| NSSI | 79.2 % (84) | 83.9 % (146) | 0.98 | 0.323 | 0.059 |
| Suicide Gesture | 15.1 % (16) | 9.8 % (17) | 1.80 | 0.180 | 0.080 |
| Suicide Ideation | 88.7 % (94) | 96.6 % (168) | 6.79 | 0.009 | 0.156 |
| Suicide Plan | 52.8 % (56) | 71.3 % (124) | 9.75 | 0.002 | 0.187 |
| Aborted Attempt | 34.9 % (37) | 40.8 % (71) | 0.97 | 0.325 | 0.059 |
| Interrupted Attempt | 14.2 % (15) | 22.4 % (39) | 2.89 | 0.089 | 0.102 |
| Suicide Attempt | 39.6 % (42) | 39.1 % (68) | 0.01 | 0.928 | 0.005 |
| Age-of-Onset (Years) | M(SD); Mdn (Range) | M(SD); Mdn (Range) | Statistical Test (U) | p | ES (r) |
| NSSI Thoughts | 13.44 (2.45); 13 (6–19) | 12.70 (2.11); 13 (5–17) | 6096.00 | 0.051 | 0.12 |
| NSSI | 13.96 (2.46); 14 (6–19) | 13.21 (2.06); 13 (5–17) | 5175.50 | 0.046 | 0.13 |
| Suicide Gesture | 14.53 (2.10); 14 (11–18) | 14.24 (2.33); 15 (7–17) | 126.00 | 0.954 | 0.01 |
| Suicide Ideation | 13.37 (2.88); 14 (5–19) | 12.66 (2.43); 13 (4–17) | 6600.50 | 0.037 | 0.13 |
| Suicide Plan | 14.27 (2.82); 14.50 (7–19) | 13.77 (2.20); 14 (5–18) | 2958.50 | 0.109 | 0.12 |
| Suicide Attempt | 15.20 (2.56); 16 (8–19) | 14.31 (1.93); 14 (7–18) | 1025.50 | 0.016 | 0.23 |
NSSI = nonsuicidal self-injury
Categorical group differences were examined using Pearson chi-square tests (χ2 ) and Cramer’s phi coefficients (Φ) for effect size. Dimensional group differences were examined using Mann-Whitney U tests and rank-biserial correlation (r) for effect size
Most adolescents reported multiple SITBs in their lifetime and rates of co-occurrence among SITBs were relatively similar across the samples (Table 3). There was a high co-occurrence of NSSI and suicide ideation (outpatients: 67.9 %; inpatients: 80.5 %), and over one third of adolescents in both samples reported engaging in both NSSI and suicide attempts (outpatients: 35.8 %; inpatients: 35.1 %) in their lifetime. Notably, of adolescents who attempted suicide, almost all reported lifetime engagement in NSSI (outpatients: 90.5 %; inpatients: 89.7 %). We also examined co-occurrence of suicide ideation with lifetime histories of aborted and interrupted suicide attempts, which have been less frequently examined in adolescent samples. Over one third of adolescents (outpatients: 34.9 %; inpatients: 40.8 %) reported suicide ideation and an aborted suicide attempt. Co-occurrence of interrupted attempts and suicide ideation was less common (outpatients: 14.2 %; inpatients: 22.4 %).
Table 3.
Co-occurrence of self-injurious thoughts and behaviors (SITBs) in adolescent outpatients (N = 106) (above the diagonal) and adolescent inpatients (N = 174) (below the diagonal)
| % (n) | NSSI Thoughts (n = 91) | NSSI (n = 84) | Suicide Gestures (n = 16) | Suicide Ideation (n = 94) | Suicide Plans (n = 56) | Aborted Attempts (n = 37) | Interrupted Attempts (n = 15) | Suicide Attempts (n = 42) |
|---|---|---|---|---|---|---|---|---|
| NSSI Thoughts (n = 157) | ——— | 78.3 % (83) | 14.2 % (15) | 74.5 % (79) | 45.3 % (48) | 33.0 % (35) | 13.2 % (14) | 35.8 % (38) |
| NSSI (n = 146) | 83.3 % (145) | ——— | 14.2 % (15) | 67.9 % (72) | 43.4 % (46) | 30.2 % (32) | 12.3 % (13) | 35.8 % (38) |
| Suicide Gestures (n = 17) | 9.2 % (16) | 8.0 % (14) | ——— | 11.3 % (12) | 6.6 % (7) | 3.8 % (4) | 4.7 % (5) | 4.7 % (5) |
| Suicide Ideation (n = 168) | 86.8 % (151) | 80.5 % (140) | 9.2 % (16) | ——— | 52.8 % (56) | 34.9 % (37) | 14.2 % (15) | 39.6 % (42) |
| Suicide Plans n = 124) | 64.4 % (112) | 61.5 % (107) | 5.2 % (9) | 71.3 % (124) | ——— | 28.3 % (30) | 13.2 % (14) | 32.1 % (34) |
| Aborted Attempts (n = 71) | 37.9 % (66) | 36.2 % (63) | 2.9 % (5) | 40.8 % (71) | 37.9 % (66) | ——— | 7.5 % (8) | 21.7 % (23) |
| Interrupted Attempts (n = 39) | 22.4 % (39) | 20.7 % (36) | 2.3 % (4) | 22.4 % (39) | 19.5 % (34) | 12.1 % (21) | ——— | 11.3 % (12) |
| Suicide Attempts (n = 68) | 36.2 % (63) | 35.1 % (61) | 2.9 % (5) | 39.1 % (68) | 33.3 % (58) | 20.7 % (36) | 12.6 % (22) | ——— |
NSSI = nonsuicidal self-injury
In addition to co-occurrence rates in the total sample, we also examined the co-occurrence of suicidal behaviors among only adolescents reporting suicide ideation (i.e., among adolescents who think about suicide, what percentage also engage in a range of suicidal behaviors?). Among adolescents reporting suicide ideation (outpatients: n = 94; inpatients: n = 168), the following suicidal behaviors were also reported: (a) suicide planning (outpatients: 59.6 %; inpatients: 73.8 %), (b) aborted attempts (outpatients: 39.4 %; inpatients: 42.3 %), (c) interrupted attempts (outpatients: 16.0 %; inpatients: 23.2 %), and (d) suicide attempts (outpatients: 44.7 %; inpatients: 40.5 %).
Age-Of-Onset of Self-Injurious Thoughts and Behaviors
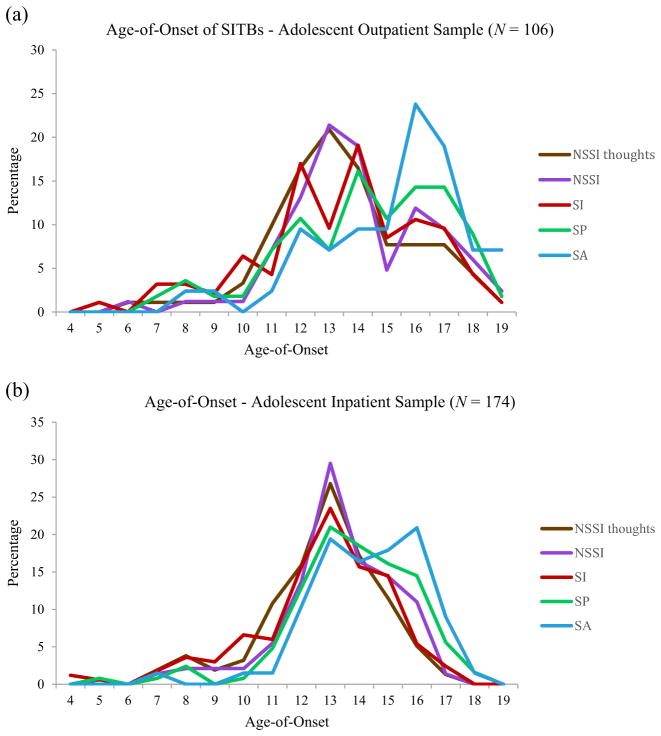
Age-of-onset of SITBs are summarized in Table 2. Results indicated a similar pattern in both samples, which was shifted slightly younger in the inpatient sample (see Fig. 1a and b). Adolescents reported that all SITBs began, on average, between 12 and 16 years of age. Thoughts of NSSI and thoughts of suicide had the earliest age-of-onset, followed by NSSI behaviors, suicide plans, and finally suicide attempts. Overall, adolescents receiving inpatient treatment had a significantly earlier age-of-onset for NSSI thoughts, NSSI, suicide ideation, and suicide attempts.2
Fig. 1.
Age-of-onset of self-injurious thoughts and behaviors (SITBs) in the adolescent outpatient sample (a) and adolescent inpatient sample (b). NSSI thoughts = thoughts of nonsuicidal self-injury; NSSI = nonsuicidal self-injury behavior; SI = suicide ideation; SP = suicide plan; SA = suicide attempt
Time Lag between Self-Injurious Thoughts and Behaviors
As noted in the data analytic plan, we computed transition variables between SITBs of interest based on the reported age-of-onset. Transition variables were computed both with and without outliers (M ± 3 SD). Results indicated a similar pattern in both samples of adolescents (see Table 4 and Fig. 2). On average, thoughts of NSSI and suicide ideation started around the same age. Thoughts of NSSI started 4–6 months before adolescents engaged in NSSI behaviors for the first time. Thoughts of suicide also started 4–6 months before adolescents first started engaging in NSSI. NSSI started approximately 3–6 months before the onset of suicide planning and 1–2 years before first suicide attempts. As anticipated, suicide ideation preceded both suicide plans and suicide attempts, and suicide plans preceded suicide attempts. On average, adolescents reported thinking about suicide for 9–12 months before they started thinking about a suicide plan, and thinking about suicide for approximately 18–24 months before making a suicide attempt. The transition between suicide planning and suicide attempts was about 8–15 months. The time lag between SITBs was not significantly different across the two samples (ps > .05).
Table 4.
Transition (in years) between self-injurious thoughts and behaviors (SITBs) in adolescent outpatient and adolescent inpatient samples
| Transition between SITBs1 | Adolescent Outpatient (N = 106)
|
Adolescent Inpatient (N = 174)
|
Group Comparison2
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | M (SD) | Range (years) | n | M (SD) | Range (years) | t | df | p | d | |
| NSSI thoughts to NSSI | ||||||||||
| Including outliers | 83 | 0.47 (1.11) | 0 to 6 | 145 | 0.52 (.84) | 0 to 4 | −0.36 | 226 | 0.717 | 0.05 |
| Excluding outliers | 80 | 0.30 (.66) | 0 to 3 | 143 | 0.47 (.74) | 0 to 3 | −1.69 | 221 | 0.092 | 0.24 |
| NSSI thoughts to SI | ||||||||||
| Including outliers | 79 | −0.10 (1.88) | −8 to 4 | 149 | −0.03 (1.84) | −7 to 5 | −0.29 | 226 | 0.717 | 0.04 |
| Excluding outliers | 78 | 0.00 (1.66) | −5 to 4 | 147 | 0.06 (1.69) | −5 to 5 | −0.26 | 223 | 0.795 | 0.04 |
| NSSI thoughts to SP | ||||||||||
| Including outliers | 48 | .96 (2.65) | −6 to 10 | 112 | 1.12 (1.92) | −5 to 7 | −0.42 | 158 | 0.673 | 0.07 |
| Excluding outliers | 47 | 0.77 (2.32) | −6 to 7 | 110 | 1.12 (1.76) | −4 to 6 | −1.04 | 155 | 0.299 | 0.17 |
| NSSI thoughts to SA | ||||||||||
| Including outliers | 38 | 2.16 (2.66) | −1 to 13 | 62 | 1.69 (2.30) | −6 to 8 | 0.93 | 98 | 0.357 | 0.19 |
| Excluding outliers | 37 | 1.86 (1.97) | −1 to 7 | 61 | 1.82 (2.09) | −5 to 8 | 0.11 | 96 | .916 | .02 |
| NSSI to SI | ||||||||||
| Including outliers | 72 | −.61 (2.13) | −8 to 4 | 139 | −0.48 (1.92) | −6 to 5 | −0.45 | 209 | 0.656 | .06 |
| Excluding outliers | 70 | −.41 (1.80) | −5 to 4 | 139 | −0.48 (1.92) | −6 to 5 | 0.25 | 207 | 0.806 | 0.04 |
| NSSI to SP | ||||||||||
| Including outliers | 46 | 0.41 (2.60) | −6 to 10 | 107 | 0.57 (1.95) | −6 to 7 | −0.41 | 151 | .682 | .07 |
| Excluding outliers | 45 | 0.20 (2.19) | −6 to 4 | 105 | 0.57 (1.75) | −5 to 6 | −1.10 | 148 | 0.273 | 0.19 |
| NSSI to SA | ||||||||||
| Including outliers | 38 | 1.89 (2.85) | −3 to 13 | 60 | 1.28 (2.23) | −6 to 8 | 1.19 | 96 | 0.238 | 0.24 |
| Excluding outliers | 37 | 1.59 (2.19) | −3 to 7 | 58 | 1.29 (1.85) | −5 to 7 | 0.72 | 93 | 0.472 | 0.15 |
| SI to SA | ||||||||||
| Including outliers | 42 | 2.07 (2.96) | 0 to 12 | 66 | 1.74 (2.16) | 0 to 9 | 0.67 | 106 | 0.506 | 0.13 |
| Excluding outliers | 40 | 1.58 (1.97) | 0 to 7 | 65 | 1.63 (1.97) | 0 to 8 | −0.14 | 103 | 0.888 | 0.03 |
| SI to SP | ||||||||||
| Including outliers | 56 | 0.89 (1.59) | 0 to 9 | 122 | 1.08 (1.75) | −6 to 8 | −0.69 | 176 | .492 | .11 |
| Excluding outliers | 55 | 0.75 (1.16) | 0 to 5 | 118 | 0.97 (1.27) | −2 to 6 | −1.14 | 171 | .258 | .18 |
| SP to SA | ||||||||||
| Including outliers | 34 | 1.26 (2.40) | −3 to 10 | 57 | 0.91 (1.68) | −1 to 8 | 0.82 | 89 | 0.414 | 0.17 |
| Excluding outliers | 33 | 1.00 (1.87) | −3 to 6 | 55 | 0.69 (1.22) | −1 to 5 | 0.94 | 86 | 0.350 | 0.20 |
NSSI = nonsuicidal self-injury, SA = suicide attempt, SI = suicide ideation, SP = suicide planning
Transitions were calculated by subtracting the age-of-onset of the first SITB from the age-of-onset of the second SITB (e.g., age-of-onset SI minus age-of-onset NSSI). Negative values indicate that the second SITB had an earlier age-of-onset than the first SITB. Outliers defined as M ± 3 SD
Group differences were examined using independent-samples t-tests. Effect sizes reported as Cohen’s d
Fig. 2.
Transition (in years) between self-injurious thoughts and behaviors (SITBs) in the adolescent outpatient sample (a) and adolescent inpatient sample (b). Means displayed include outliers
Discussion
Findings from the current study extend knowledge about the course of nonsuicidal and suicidal self-injurious thoughts and behaviors in youth. Hypotheses about higher SITB rates (occurrence and co-occurrence) among inpatient versus out-patient youth were partially supported. Predictions about the age-of-onset patterns among SITBs, time lag between SITBs, and differences across the continuum of care were supported. Each finding is discussed in turn below.
Occurrence and Co-Occurrence of Self-Injurious Thoughts and Behaviors
In line with previous studies (Klonsky et al. 2013; Muehlenkamp et al. 2011; Nock et al. 2006), there was a high co-occurrence of SITBs in both clinical samples of youth. The majority of adolescents reported a history of both NSSI and suicide ideation, and one-third reported both NSSI and suicide attempts in their lifetime. Though we hypothesized a higher occurrence and co-occurrence of all SITBs in the inpatient, compared to the outpatient, sample, only some SITBs were significantly more common (i.e., suicide ideation and suicide plans), and more likely to co-occur (e.g., NSSI and suicide ideation; NSSI and suicide plans) among inpatients. One explanation for this finding is that lifetime SITBs were examined within the context of adolescents’ current level of treatment—not the most severe level of care received in their lifetime (i.e., some adolescents in current outpatient treatment may have received inpatient treatment in the past). Despite this limitation, current findings indicate a high co-occurrence of nonsuicidal and suicidal SITBs among adolescents receiving both inpatient and outpatient mental health treatment.
In addition to the major SITB categories, this study also extends previous research by examining aborted and interrupted suicide attempts, which have received much less attention. Among adolescents who reported a lifetime history of suicide ideation, approximately 33 % made an aborted suicide attempt and roughly 20 % made an interrupted attempt. These suicide-related behaviors may be useful for distinguishing more severe individuals among the large and heterogeneous group who think about suicide (Rueter et al. 2008). Future research is needed to understand how aborted and interrupted attempts may be related to risk for future suicide attempts in youth.
Taken together, these findings add to the growing research literature indicating that, although nonsuicidal and suicidal self-injury are distinct in terms of suicide intent, prevalence, and frequency (Grandclerc et al. 2016; Hamza et al. 2012; Nock 2010), they significantly overlap both cross-sectionally (Klonsky et al. 2013; Nock et al. 2006) and in their longitudinal course (Giletta et al. 2015). NSSI and suicide ideation may exhibit strong overlap to the degree that they share genetic risk factors (Maciejewski et al. 2014) and are common manifestations of the same underlying cause that precedes suicidal behavior (e.g., emotional distress; Victor and Klonsky 2014). Future research is needed to clarify why some adolescents transition to engagement in suicidal behavior while others do not.
Age-Of-Onset of Self-Injurious Thoughts and Behaviors
The temporal course of SITBs was examined with the age-of-onset and time lag between SITBs. In terms of age-of-onset, outpatient and inpatient adolescents reported that, on average, all SITBs began between the ages of 12 and 16. Across both groups, thoughts of NSSI and thoughts of suicide had the earliest age-of-onset, followed by NSSI behaviors, suicide plans, and finally suicide attempts. Adolescent inpatients had a significantly earlier age-of-onset for all SITBs than adolescents receiving outpatient treatment, which is perhaps not surprising given the younger age-of-onset for psychiatric disorders and clinically relevant behaviors found in more clinically severe samples (Carter et al. 2003; Moor et al. 2012; Zisook et al. 2007). Although the age-of-onset of suicidal behaviors in the general population occurs in late adolescence or early adulthood (Kessler et al. 1999), suicide attempts appear to begin significantly earlier in more clinically acute youth, with peaks between the ages of 15–18 years.
The age-of-onset of SITBs in early- to mid-adolescence coincides with increased rates of psychiatric disorders during this developmental period, such as major depression (Avenevoli et al. 2015) and substance use disorders (Merikangas et al. 2010). However, the increase in psychiatric symptoms can only partially account for the age-of-onset of SITBs during adolescence, as not all youth engaging in SITBs have psychiatric disorders (Glenn and Klonsky 2013; Nock et al. 2006). The majority of previous research on SITBs has examined individuals who have already started thinking about or engaging in self-injurious or suicidal behaviors (Nock 2010). Future prospective research is needed in younger samples, before the onset of SITBs, to identify other, and ideally SITB-specific, vulnerability factors that may contribute to the increased incidence of SITBs during this developmental period.
Time Lag between Self-Injurious Thoughts and Behaviors
In terms of the time lag between SITBs, both outpatients and inpatients reported that thoughts of suicide started 4–6 months before initial engagement in NSSI. However, NSSI started approximately 3–6 months before the onset of suicide planning and 1–2 years before suicide attempts. Consistent with previous research in nationally representative samples of adolescents and adults (Nock et al. 2008a; Nock et al. 2013), adolescents reported thinking about suicide for 9–12 months before they started developing a suicide plan, thinking about suicide for 18–24 months before making their first attempt, and transitioning from suicide planning to suicide attempts over the course of one year. Notably, the time lag between SITBs was not significantly different between the inpatient and outpatient samples. Taken together with the age-of-onset findings, SITBs have an overall earlier age-of-onset in more clinically severe youth, but the time to transition from one SITB to the next is relatively similar across the continuum of care.
These results have a number of implications for understanding the trajectory between nonsuicidal and suicidal self-injurious thoughts and behaviors. First, given findings indicating that the onset of NSSI thoughts and suicide ideation may occur at the same time, and predate initial engagement in NSSI, pathways to NSSI and suicidal behavior may occur simultaneously rather than in succession from nonsuicidal to suicidal self-injury. This is consistent with research indicating that NSSI and suicide ideation may share underlying vulnerability factors (Maciejewski et al. 2014; Victor and Klonsky 2014), which may manifest around the same time developmentally. Moreover, if suicide ideation precedes NSSI behavior, NSSI may increase risk for suicidal behavior among adolescents who have already started thinking about suicide. This finding may be particularly important for research aimed at understanding the mechanisms linking nonsuicidal to suicidal self-injury (Grandclerc et al. 2016). Moreover, it is important for allied health professionals to know that youth engaging in NSSI may have already started thinking about suicide.
A second implication is that the transition between SITBs is relatively fast. Consistent with findings in normative samples of youth (Nock et al. 2013), the longest transition was from suicide ideation to suicide attempts, which was 1–2 years on average. Thus, a key period for intervention and prevention of suicidal behavior is within the first 6 to 12 months after the onset of suicidal thinking or engagement in NSSI. At the same time, the mechanisms that facilitate this transition from thinking about suicide to NSSI engagement remain unclear. Research on risk and protective factors will be key for identifying potentially modifiable treatment targets. In addition, future studies are needed to examine potential moderators of these transitions and for whom this time lag may be faster or slower.
Strengths and Limitations
The current study extends prior research in at least four important ways. First, this study assessed the full range of SITBs and not just behavioral outcomes (i.e., NSSI and suicide attempts). By assessing thoughts, this study found that suicide ideation started, on average, before the onset of NSSI, enhancing understanding of the time-lagged relationship between these two classes of self-injury. Second, the inclusion of two clinical samples (outpatient and inpatient) allowed us to examine how SITB patterns differed based on clinical severity. Results indicated similar patterns of SITBs that were shifted slightly younger in adolescents receiving more acute clinical care. Third, given that SITBs were assessed in adolescents around the age-of-onset of these thoughts and behaviors, this study was less limited by retrospective biases than similar studies in adults. Finally, this study benefited from assessment of SITBs using validated clinical interviews, which are the gold standard measurement tools because clarifications can be made and misunderstandings can be resolved in person.
There are also several limitations of this research that warrant discussion. First, adolescents in our sample were predominantly female, Caucasian, and from higher socioeconomic backgrounds. Although many of these characteristics are common among SITB (CDC 2015; Muehlenkamp and Gutierrez 2004) and treatment-seeking samples (Oliver et al. 2005), they limit generalizability to other populations. Replication in more diverse clinical samples is needed. Second, although this study examined SITBs closer to the initial onset of these clinical phenomena, the reporting of SITBs’ age-of-onset was still retrospective using a single time point assessment, and thus susceptible to reporting biases. Future research could address this limitation by using a repeated measures, prospective design to examine the transition across different forms of SITBs. Third, adolescents reported the age-of-onset of SITBs in years, rather than in months, which decreased specificity of the time lag between SITB variables. Future studies could use a more detailed calendar method for assessing the course of SITBs. Fourth, the interview utilized for this study did not assess the age-of-onset of all suicidal behaviors (e.g., aborted attempts, interrupted attempts), and therefore, we were not able to include these behaviors in our examination of SITB transitions. Fifth, this study assessed SITB prevalence up to that point in adolescence rather than full lifetime prevalence (e.g., including later adolescence and adulthood). It is probable that some adolescents who have yet to experience the assessed SITBs, particularly suicide attempts, will go on to engage in these behaviors in later adolescence. The field would benefit from longitudinal assessments that follow youth from late childhood (before the onset of any SITBs) through adulthood to capture the full course of these thoughts and behaviors. Finally, the current study focused on the descriptive course of SITBs in youth rather than factors predicting the transition between SITBs. It will be important for future research to examine specific mechanisms that may facilitate the escalation between SITBs (Grandclerc et al. 2016), which may ultimately suggest direct targets for intervention and prevention.
Acknowledgments
Funding The research was partially supported by grants from the National Institute of Mental Health (F32MH097354 [CRG]; K23MH097786 [RPA]), the Rolfe Fund (RPA), the Tommy Fuss Fund (RPA), the Simches Fund (RPA), and with support from the John D. and Catherine T. MacArthur Foundation (MKN).
Footnotes
In line with Bryan et al. (2015), we aimed to examine differences in the transition from suicidal thinking to suicidal action among those with and without a history of NSSI. However, in our two large clinical samples, the number of adolescents who had attempted suicide but not engaged in NSSI was very small (SA only: n = 11 across both samples), as compared to adolescents who had engaged in both NSSI and attempted suicide (NSSI + SA: n = 102 across both samples). Therefore, we did not have sufficient power for the proposed analyses.
Gender differences in the age-of-onset of SITBs were examined. Across both samples, females had slightly earlier ages of onset than males, but this difference was only significant for the onset of: (a) suicide ideation in the outpatient sample: male (n = 16, M = 14.69, SD = 2.39); female (n = 78, M = 13.10, SD = 2.91), t(92) = 2.04, p = .044, Cohen’s d = 0.60, and (b) suicide attempts in the inpatient sample: male (n = 12, M = 15.42, SD = 1.83); female (n = 55, M = 14.07, SD = 1.88), t(65) = 2.25, p = .028, Cohen’s d = 0.73. However, these results should be interpreted with caution as both samples were predominantly female.
Compliance with Ethical Standards
Conflict of Interest The authors declare that they have no conflicts of interest.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD, et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: findings from the TORDIA study. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:772–781. doi: 10.1016/j.jaac.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Millner AJ, Stewart JG, Esposito EC. Identifying differences between depressed adolescent suicide ideators and attempters. Journal of Affective Disorders. 2015;186:127–133. doi: 10.1016/j.jad.2015.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the National Comorbidity Survey–Adolescent Supplement: prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54:37–44. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrocas AL, Hankin BL, Young JF, Abela JR. Rates of nonsuicidal self-injury in youth: age, sex, and behavioral methods in a community sample. Pediatrics. 2012;130:39–45. doi: 10.1542/peds.2011-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, Bryan AO, May AM, Klonsky ED. Trajectories of suicide ideation, nonsuicidal self-injury, and suicide attempts in a nonclinical sample of military personnel and veterans. Suicide and Life-threatening Behavior. 2015;45:315–325. doi: 10.1111/sltb.12127. [DOI] [PubMed] [Google Scholar]
- Carter TDC, Mundo E, Parikh SV, Kennedy JL. Early age at onset as a risk factor for poor outcome of bipolar disorder. Journal of Psychiatric Research. 2003;37:297–303. doi: 10.1016/s0022-3956(03)00052-9. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Web-based Injury Statistics Query and Reporting System (WISQARS) National Center for Injury Prevention and Control, CDC; 2010. Available from www.cdc.gov/injury/wisqars/index.html. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Injury Center: Violence prevention—suicide prevention: Youth suicide. 2015 Retrieved from www.cdc.gov/violenceprevention/suicide/youth_suicide.html.
- Giletta M, Prinstein MJ, Abela JR, Gibb BE, Barrocas AL, Hankin BL. Trajectories of suicide ideation and nonsuicidal self-injury among adolescents in mainland China: peer predictors, joint development, and risk for suicide attempts. Journal of Consulting and Clinical Psychology. 2015;83:265–279. doi: 10.1037/a0038652. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Klonsky ED. Nonsuicidal self-injury disorder: an empirical investigation in adolescent psychiatric patients. Journal of Clinical Child & Adolescent Psychology. 2013;42:496–507. doi: 10.1080/15374416.2013.794699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandclerc S, De Labrouhe D, Spodenkiewicz M, Lachal J, Moro MR. Relations between nonsuicidal self-injury and suicidal behavior in adolescence: a systematic review. PloS One. 2016;11:e0153760. doi: 10.1371/journal.pone.0153760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan K, Fox KR, Prinstein MJ. Nonsuicidal self-injury as a time-invariant predictor of adolescent suicide ideation and attempts in a diverse community sample. Journal of Consulting and Clinical Psychology. 2012;80:842–849. doi: 10.1037/a0029429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza CA, Stewart SL, Willoughby T. Examining the link between nonsuicidal self-injury and suicidal behavior: a review of the literature and an integrated model. Clinical Psychology Review. 2012;32:482–495. doi: 10.1016/j.cpr.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Jacobson CM, Gould M. The epidemiology and phenomenology of non-suicidal self-injurious behavior among adolescents: a critical review of the literature. Archives of Suicide Research. 2007;11:129–147. doi: 10.1080/13811110701247602. [DOI] [PubMed] [Google Scholar]
- Kar N, Bastia BK. Post-traumatic stress disorder, depression and generalized anxiety disorder in adolescents after a natural disaster: a study of comorbidity. Clinical Practice and Epidemiology in Mental Health. 2006;2:17–23. doi: 10.1186/1745-0179-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. Journal of Abnormal Psychology. 2013;122:231–237. doi: 10.1037/a0030278. [DOI] [PubMed] [Google Scholar]
- Maciejewski DF, Creemers HE, Lynskey MT, Madden PA, Heath AC, Statham DJ, et al. Overlapping genetic and environmental influences on nonsuicidal self-injury and suicidal ideation: different outcomes, same etiology? JAMA Psychiatry. 2014;71:699–705. doi: 10.1001/jamapsychiatry.2014.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millner AJ, Lee MD, Nock MK. Single-item measurement of suicidal behaviors: validity and consequences of misclassi-fication. PloS One. 2015;10:e0141606. doi: 10.1371/journal.pone.0141606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moor S, Crowe M, Luty S, Carter J, Joyce PR. Effects of comorbidity and early age of onset in young people with bipolar disorder on self-harming behaviour and suicide attempts. Journal of Affective Disorders. 2012;136:1212–1215. doi: 10.1016/j.jad.2011.10.018. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Gutierrez PM. An investigation of differences between self- injurious behavior and suicide attempts in a sample of adolescents. Suicide and Life-threatening Behavior. 2004;34:12–23. doi: 10.1521/suli.34.1.12.27769. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Ertelt TW, Miller AL, Claes L. Borderline personality symptoms differentiate non-suicidal and suicidal self-injury in ethnically diverse adolescent outpatients. Journal of Child Psychology and Psychiatry. 2011;52:148–155. doi: 10.1111/j.1469-7610.2010.02305.x. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child and Adolescent Psychiatry and Mental Health. 2012;6:1–9. doi: 10.1186/1753-2000-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK. Self-injury. Annual Review of Clinical Psychology. 2010;6:339–363. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. Journal of Abnormal Psychology. 2006;115:616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Nonsuicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Research. 2006;144:65–72. doi: 10.1016/j.psychres.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, Michel BD. Self-injurious thoughts and behaviors interview: development, reliability, and validity in an adolescent sample. Psychological Assessment. 2007;19:309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, et al. Cross-national prevalence and risk factors for suicidal ideation, plans, and attempts. British Journal of Psychiatry. 2008a;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008b;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ, Sterba SK. Revealing the form and function of self-injurious thoughts and behaviors: a real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology. 2009;118:816–827. doi: 10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Ono Y. Suicide: global perspectives from the WHO world mental health surveys. New York, NY: Cambridge University Press; 2012. [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70:300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver MI, Pearson N, Coe N, Gunnell D. Help-seeking behaviour in men and women with common mental health problems: cross-sectional study. The British Journal of Psychiatry. 2005;186:297–301. doi: 10.1192/bjp.186.4.297. [DOI] [PubMed] [Google Scholar]
- Rueter MA, Holm KE, McGeorge CR, Conger RD. Adolescent suicidal ideation subgroups and their association with suicidal plans and attempts in young adulthood. Suicide and Life-threatening Behavior. 2008;38:564–575. doi: 10.1521/suli.2008.38.5.564. [DOI] [PubMed] [Google Scholar]
- Scott LN, Pilkonis PA, Hipwell AE, Keenan K, Stepp SD. Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: a multi-wave prospective study. Comprehensive Psychiatry. 2015;58:1–10. doi: 10.1016/j.comppsych.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D, Shytle D, Milo K, Janavs J, Lecrubier Y. Mini international neuropsychiatric interview for children and adolescents (M.I.N.I. Kid), English version 6.0. Tampa, FL: University of South Florida College of Medicine; 2009. [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, et al. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID) Journal of Clinical Psychiatry. 2010;71:313–326. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- Stewart JG, Kim JC, Esposito EC, Gold J, Nock MK, Auerbach RP. Predicting suicide attempts in depressed adolescents: clarifying the role of disinhibition and child sexual abuse. Journal of Affective Disorders. 2015;187:27–34. doi: 10.1016/j.jad.2015.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuisku V, Kiviruusu O, Pelkonen M, Karlsson L, Strandholm T, Marttunen M. Depressed adolescents as young adults–predictors of suicide attempt and non-suicidal self-injury during an 8-year follow-up. Journal of Affective Disorders. 2014;152:313–319. doi: 10.1016/j.jad.2013.09.031. [DOI] [PubMed] [Google Scholar]
- van Alphen NR, Stewart JG, Esposito EC, Pridgen B, Gold J, Auerbach RP. Predictors of rehospitalization for depressed adolescents admitted to acute psychiatric treatment. The Journal of Clinical Psychiatry. doi: 10.4088/JCP.15m10326. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor SE, Klonsky ED. Correlates of suicide attempts among self-injurers: a meta-analysis. Clinical Psychology Review. 2014;34:282–297. doi: 10.1016/j.cpr.2014.03.005. [DOI] [PubMed] [Google Scholar]
- Whitlock J, Muehlenkamp J, Purington A, Eckenrode J, Barreira P, Baral Abrams G, et al. Nonsuicidal self-injury in a college population: general trends and sex differences. Journal of American College Health. 2011;59:691–698. doi: 10.1080/07448481.2010.529626. [DOI] [PubMed] [Google Scholar]
- Wilkinson BJ, Marshall RM, Curtwright B. Impact of Tourette’s disorder on parent reported stress. Journal of Child and Family Studies. 2008;17:582–598. [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the adolescent depression antidepressants and psychotherapy trial (ADAPT) American Journal of Psychiatry. 2011;168:495–501. doi: 10.1176/appi.ajp.2010.10050718. [DOI] [PubMed] [Google Scholar]
- Zetterqvist M, Lundh LG, Dahlström Ö, Svedin CG. Prevalence and function of non-suicidal self-injury (NSSI) in a community sample of adolescents, using suggested DSM-5 criteria for a potential NSSI disorder. Journal of Abnormal Child Psychology. 2013;41:759–773. doi: 10.1007/s10802-013-9712-5. [DOI] [PubMed] [Google Scholar]
- Zisook S, Lesser I, Stewart JW, Wisniewski SR, Balasubramani GK, Fava M, et al. Effect of age at onset on the course of major depressive disorder. American Journal of Psychiatry. 2007;164:1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]