Abstract
This study uses data from the 2009 Behavioral Risk Factors Surveillance System (BRFSS) to examine differences between male and female caregivers by demographics, health-related quality of life (HRQOL), and the effect of social support on HRQOL. Roughly two-thirds of caregivers were women, and demographic characteristics differed among men and women caregivers. Women caregivers reported significantly more mentally and physically unhealthy days than men, but there were no differences between men and women in general health or life satisfaction. Men were significantly more likely to report that they rarely or never received social support. Despite this, the effect of social support on HRQOL was stronger in men than in women. Implications of these findings for caregiver support programs are discussed.
Introduction
Current demographic trends reveal a growth in the numbers of adults aged 65 or older1 along with increased prevalence of multiple chronic conditions in the U.S2, underscoring the dramatically increasing need for long-term support services3. For example, in 2009, two-thirds of people age 65 or over who had one or more limitations in instrumental activities of daily living needed and received personal assistance1. As a result, more people are likely to find themselves being called upon to provide care to family and friends with increasingly complex needs. This care is often referred to as informal or family caregiving.
Traditionally, we know that caregiving has fallen to women as part of their role expectations in family and society4,5. It is expected that the proportion of men caregivers will increase substantially with the aging of the baby boomer generation, i.e. those born between 1946 and 19646,7. Prior studies have found that women caregivers generally fare worse than men caregivers on measures of physical and mental health8,9, including depression10, anxiety11,12 and physical complaints13,14. Although numerous studies have shown that women have larger and more complex social networks than men15,16, there is little information about whether these more developed networks confer a protective effect that would mitigate the differences in health outcomes between men and women caregivers. Furthermore, there is a dearth of information on gender differences that include large samples of caregivers despite significant progress in understanding the nature and effects of caregiving. Recent findings from the 2009 BRFSS17 found that roughly one-quarter (24.7%; 95% CI: 24.4%–25.0%) of respondents 18 years of age or older reported providing care to a friend or family member during the month preceding the survey.
The aims for this study are threefold. First, we estimate the proportion of men to women caregivers in the 2009 BRFSS and examine their demographic characteristics. Second, we examine gender differences in health-related quality of life (HRQOL) among caregivers. Finally, we explore how social support affects HRQL in men and women caregivers.
Methods
The BRFSS is the largest annual telephone health survey in the U.S., and uses random-digit dialed methodology and weighting to ensure that the results resemble the overall demographic characteristics of each state. A total of 421,215 participants from all 50 states, the District of Columbia, and 3 U.S. territories (Guam, Puerto Rico, and the Virgin Islands) were asked the following question in the 2009 BRFSS survey: “People may provide regular care or assistance to a friend or family member who has a health problem, long-term illness, or disability. During the past month, did you provide any such care or assistance to a friend or family member?” Persons who responded “Yes” to this inquiry were classified as caregivers (n=109,174). We used SPSS Version 2218 to analyze the data and account for the complex sampling design of the BRFSS.
We combined categories in several of the demographic variables. The race/ethnic groups were combined to yield four categories: “White Non-Hispanic,” “Black Non-Hispanic,” “Hispanic,” and “Other Non-Hispanic or Multi-Racial.” The “Other Non-Hispanic or Multi-Racial” category combined the Asian, Native Hawaiian or other Pacific Islander, Alaskan Native, and Multi-Racial categories. The marital status variable was reduced to three categories: “Married or Living with a Partner,” and “Never Married,” and “Separated/Divorced/Widowed. The education levels were combined into four categories: to “Less than High School” (i.e., “Never attended school or only kindergarten,” “Grades 1 through 9,” and “Grades 9 through 11”); “High School Graduate;” “Some College;” and “College Degree or Higher.” Respondents were classified into five age categories: 18–29, 30–39, 40–49, 50–59, and 60 years of age or older.
We then compared men and women caregivers on their responses to a set of HRQOL and Well-Being questions including the Centers for Disease Control’s (CDC) Healthy Days module19, and social/emotional support and life satisfaction items that appeared on the BRFSS. For these comparisons, we dichotomized the two CDC Healthy Days questions for physical and mental health by comparing those who reported 14 or more days of poor mental or physical health relative to those who reported fewer days (for more information on the validity of this measure see20. This coding scheme is frequently referred to as mental and physical distress in previous studies13. For life satisfaction, we compared the percentages of men and women caregivers who said they were “Very Satisfied” or “Satisfied” to those who answered “Dissatisfied” or “Very Dissatisfied.” For general health, we compared the percentages of “Excellent” and “Very Good” to “Fair” and “Poor” responses by gender. We measured social/emotional support from the question “How often do you get the social and emotional support you need?” and collapsed the response categories to yield three levels of support: “Always,” “Usually/Sometimes,” and “Rarely/Never.” We used the chi-square statistic to determine whether gender differences in these variables were significant at the .05 level.
Lastly, we used multiple linear regression models to estimate physically and mentally unhealthy days among caregivers, accounting for the complex survey design. Social/emotional support, gender, and the social/emotional support by gender interaction were the variables of interest. Age (less than 50 years of age vs. 50 years of age or older), race, marital status, and education were included as covariates. Additionally, we controlled for current smoking status, disability status, and no leisure-time physical activity in the past 30 days, as these variables have previously been shown to be related to HRQOL outcomes21. Frequencies for these variables are included in Table 1.
Table 1.
Demographic Characteristics of Caregivers by Gender, 2009 BRFSSa.
| Category | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Weighted Estimate | 95% Confidence Interval
|
Unweighted Count | Weighted Estimate | 95% Confidence Interval
|
Unweighted Count | |||
| Lower | Upper | Lower | Upper | |||||
| Race* | ||||||||
| White Non-Hispanic | 66.3% | 65.0% | 67.6% | 27844 | 70.4% | 69.6% | 71.2% | 57197 |
| Black Non-Hispanic | 11.4% | 10.6% | 12.3% | 2707 | 12.2% | 11.7% | 12.8% | 7246 |
| Hispanic | 14.3% | 13.2% | 15.5% | 2132 | 11.9% | 11.2% | 12.5% | 4571 |
| Other or Multiracial, Non-Hispanic | 8.0% | 7.2% | 8.8% | 2390 | 5.5% | 5.2% | 5.9% | 3918 |
| Age Groups * | ||||||||
| 18–29 | 19.4% | 18.2% | 20.6% | 2331 | 14.1% | 13.4% | 14.9% | 3643 |
| 30–39 | 16.2% | 15.3% | 17.2% | 3324 | 16.4% | 15.8% | 17.0% | 7453 |
| 40–49 | 21.9% | 20.9% | 22.9% | 6423 | 21.7% | 21.1% | 22.3% | 13468 |
| 50–59 | 20.9% | 20.1% | 21.7% | 9443 | 23.5% | 23.0% | 24.1% | 20325 |
| 60+ | 21.7% | 21.0% | 22.4% | 13812 | 24.3% | 23.8% | 24.8% | 28043 |
| Education* | ||||||||
| Less than High School | 9.9% | 9.1% | 10.7% | 2873 | 8.0% | 7.5% | 8.5% | 5216 |
| High School Graduate | 29.5% | 28.4% | 30.6% | 9988 | 26.9% | 26.2% | 27.5% | 21048 |
| Some College | 26.6% | 25.6% | 27.6% | 9496 | 30.7% | 30.1% | 31.4% | 22843 |
| College Graduate | 34.0% | 32.9% | 35.1% | 13126 | 34.4% | 33.7% | 35.1% | 24421 |
| Marital Status* | ||||||||
| Married/Living with a Partner | 66.7% | 65.5% | 67.9% | 24574 | 65.1% | 64.3% | 65.8% | 43633 |
| Never Married | 21.6% | 20.5% | 22.8% | 4567 | 14.6% | 13.9% | 15.3% | 7187 |
| Separated/Divorced/Widowed | 11.7% | 10.9% | 12.4% | 6285 | 20.4% | 19.8% | 20.9% | 22532 |
| No Leisure Time Activity * | 19.2% | 18.4% | 20.1% | 7566 | 23.7% | 23.0% | 24.3% | 18147 |
| Current Cigarette Smoker * | 24.8% | 23.7% | 25.9% | 7329 | 19.9% | 19.3% | 20.5% | 13515 |
| Disabled | 24.0% | 23.0% | 25.0 | 10097 | 24.5 | 23.9 | 25.1 | 20144 |
Total unweighted cases = 109,174.
p <.0.05
Results
Approximately two-thirds of all caregivers were women (67.5%) and 32.5% were men. There were significantly more White and Black women caregivers compared to men of the same race and ethnicity (Table 1). The average age of caregivers was 47.1 years (95% CI = 46.9 – 47.3). Men were significantly younger than women caregivers (mean = 45.9, 95% CI= 45.5 – 46.3 versus mean = 48.0, 95% CI = 47.8 – 48.3). Education level varied significantly by gender, with men having a higher proportion of less than high school or high school graduates than women. Roughly two-thirds of both men and women caregivers were married or living with a partner (66.7% and 65.1% respectively), but men were significantly more likely to report never having been married than women (21.6% vs 14.6%), and women were more likely to report being divorced, separated, or widowed than men (20.4% vs 11.7%).
Men caregivers were more likely to report being current smokers than women (24.8% vs. 19.9%). Men caregivers were less likely to report that they had no leisure time physical activity than women caregivers (19.2% vs. 23.7%). There were no gender differences in disability status.
There were no gender differences on self-reported general health or life satisfaction (Table 2). For the CDC Healthy Days questions, women caregivers were significantly more likely to report 14 or more physically unhealthy days (12.7% vs. 11.1%) and mentally unhealthy days (16.1% vs. 11.9%) relative to men. For the social and emotional support item, men were significantly more likely to report rarely or never receiving social/emotional support (9.9% vs. 7.4%).
Table 2.
Weighted Prevalence Estimates, Confidence Intervals, and Number of Respondents for HRQOL Outcomes by Gender, 2009 BRFSSa.
| Men | Women | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Weighted Prevalence | Confidence Interval | N | Weighted Prevalence | Confidence Interval | N | |
| HRQOL Outcome | ||||||
| Fair/Poor General Health | 16.7% | 15.8% – 17.5% | 6764 | 17.0% | 16.5% – 17.5% | 13338 |
| ≥14 Physically Unhealthy Days* | 11.1% | 10.4% – 11.8% | 4453 | 12.7% | 12.2% – 13.2% | 9775 |
| ≥14 Mentally Unhealthy Days* | 11.9% | 11.2% – 12.6% | 3850 | 16.1% | 15.6% – 16.7% | 10784 |
| Dissatisfied/Very Dissatisfied with Life | 7.1% | 6.6% – 7.8% | 2192 | 6.9% | 6.5% – 7.3% | 4609 |
| Rarely/Never Get Social Support* | 9.9% | 9.2% – 10.7% | 3205 | 7.4% | 7.0% 7.8% | 5243 |
Total unweighted cases = 109,174.
p < 0.05
We then modeled the effects of gender, social/emotional support and gender by social/emotional support interaction on physically and mentally unhealthy days, controlling for age, race, education, marital status, smoking status, disability status, and leisure-time physical activity using the Complex Samples General Linear Model option in SPSS v. 22. For mentally unhealthy days, there was a main effect for social/emotional support (F [2, 387281] = 998.3, p <0.0001), gender (F[1, 387281] = 333.3, p <0.0001), and a significant interaction between gender and social/emotional support (F [2, 387281] = 48.7, p < 0.0001). For physically unhealthy days, the main effects for social/emotional support and gender, were statistically significant at the .0001 level (F [2, 178820] = 154.78, [1, 178820] = 64.14, and [2, 178819] = 11.77 respectively), but the interaction of gender and social/emotional support failed to reach significance. The results of the stratified multiple regression results are presented in Table 3. Women reported significantly more physically unhealthy days (4.7 vs. 3.4) and mentally unhealthy days (11.9 vs. 7.6) than men. Among women, higher levels of social/emotional support were associated with fewer mentally unhealthy days; the effect was less strong among men (7.9 fewer days for “always” getting social/emotional support versus 4.6 fewer days, respectively). Nonetheless, women who reported high levels of social/emotional support reported significantly more mentally unhealthy days than men who reported similar levels of social and emotional support. (see Figure 1).
Table 3.
Multivariate Regression Models for Physically and Mentally Unhealthy Days, 2009 BRFSS
| Variables | Physically Unhealthy Days β |
Mentally Unhealthy Days β |
||
|---|---|---|---|---|
|
| ||||
| Men | Women | Men | Women | |
| Intercept | 3.4** | 4.7** | 7.6** | 11.9** |
| Social support | ||||
| Always/usually get social support needed | −1.4** | −2.6** | −4.6** | −7.9** |
| Sometimes get social support needed | −0.8** | −1.7** | −2.1** | −3.8** |
| Rarely/never get social support needed | .000a | .000a | .000a | .000a |
| Race/ethnicity | 0.06 | 0.3* | −0.2 | 0.3 |
| Education | −0.6** | −0.4** | −0.3* | −0.3* |
| Marital Status | 0.2 | −0.01 | 0.2 | 0.2 |
| Age > 50 yrs. | 1.0** | 1.0 | −1.8** | −2.1** |
| Disabled | 7.8 | 7.9** | 4.5** | 4.4** |
| Current cigarette smoker | −0.1 | 0.3* | 1.7** | 1.8** |
| No leisure time physical activity | −3.3** | 2.5** | 1.4** | 1.4** |
p <0.001
Set to zero because this parameter is redundant.
p <0.05
Figure 1.
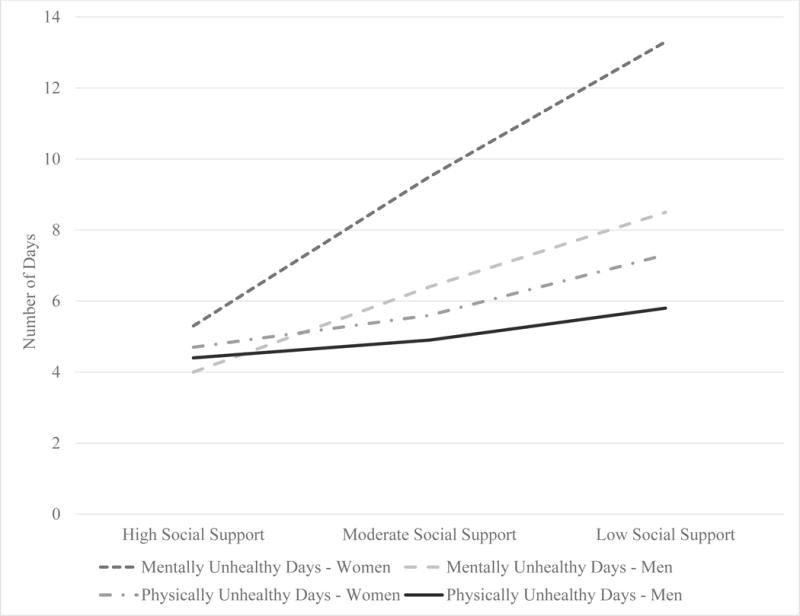
Mean Physically and Mentally Unhealthy Days by Gender at Different Levels of Social Support.
As shown in Table 3, being 50 or older was associated with a lower number of mentally unhealthy days for both men and women. Men and women over 50 years of age reported more physically unhealthy days than those younger than 50 years of age. Marital status was not significant in any model. Higher levels of education were associated with fewer physically and mentally unhealthy days among both men and women. Race was not significantly related to physically and mentally unhealthy days in men. However, race was significantly related to mentally unhealthy days for women. Cigarette smoking was associated with significantly more mentally unhealthy days for both men and women, but was not associated with physically unhealthy days for either gender. Leisure time activity was related to a reduction in mentally and physically unhealthy days for both men and women by roughly one day.
Discussion
These findings are consistent with earlier research that found higher levels of depression, social support, and a stronger relationship between the two among women than men caregivers22, 23. In our study, men caregivers reported substantially fewer mentally and physically unhealthy days than women and the buffering effects of social support were stronger in women. Nevertheless, women reporting high levels of social and emotional support still reported more physically and mentally unhealthy days than men reporting low levels of social and emotional support. So despite the higher proportion of men reporting that they rarely or never received the social/emotional support they needed, this did not have as strong an effect on the number of physically and mentally unhealthy days as low social/emotional support had on women. This may be due to the different role that social support plays in the mental health of men and women24. Because women tend to have larger social networks than men15, and men may tend to rely on their spouses and family members for their main source of social support, women caretakers may be more sensitized to the presence or absence of social support However, social/emotional support did provide some buffer against more unhealthy days for both men and women.
Intriguingly, marital status was unrelated to HRQOL for either men or women in our models. It is possible that social support, rather than the presence or absence of a partner, may be more important to caregivers’ health, as we had no way of measuring the quality of the marital relationship. Future research on this topic in greater depth may yield a better understanding of the role of marriage in supporting caregiver health.
There were some additional interesting findings in this study. Roughly one-quarter of caregivers self-identified as disabled, confirming earlier research7. Disability status was more strongly related to physically unhealthy days in men and women, but social/emotional support was almost twice as strong a predictor of mentally unhealthy days as disability status for both genders. Nonetheless, caregiving by members in this group most likely poses additional difficulties, and further research.is needed to assess the effects of disability on caregivers and recipients of that care. In addition, we found that the overall smoking prevalence for this sample of caregivers was slightly above the 2010 estimate of 19.5% for the entire US population,25 suggesting that caregivers may be more likely to have more unhealthy behaviors than non-caregivers.
Clearly, there are other factors besides gender that may have an impact on caregiver quality of life, such as length of caregiving, intensity of caregiving, interference from other roles, and financial concerns, to name a few. Future research with more detailed information about caregiving activities is needed to understand the relative contributions of each of these factors to caregiver quality of life.
These results must be interpreted with regard to several potential limitations. First, the BRFSS caregiving question only pertains to the previous thirty days; persons who provided assistance outside of that timeframe would be classified as non-caregivers. However, this time frame has been used extensively by other researchers26. Second, the BRFSS reaches only those US citizens who have a land-line telephone; this may result in under-representation of younger adults, who tend to rely upon cell phone service exclusively, as well as those without the financial means to afford a telephone line. How these biases would affect our results is unquantifiable. Our measure of social/emotional support was a single item, which is a less precise measure than could be obtained by using a social support scale.
Despite the limitations, our findings that women caregivers reported poorer health related quality of life is consistent with earlier findings. A more novel finding was the lower social support level that men report receiving. Given that less is known about men caregivers on a population level, we hope that future studies will examine these gender differences more thoroughly.
Implications for Practice and/or Policy
These findings may be useful to inform the study of caregiver interventions and strategies. Interventions for caregivers may include social and emotional support, skills training, education, activity planning, environmental redesign, and may be tested either singly or in combination26. Moreover, in many of the intervention studies reviewed here, the majority of the samples were comprised of women caregivers. As a result, it may be helpful to examine how gender influences the success of caregiving interventions and whether messages about programs need to be more gender-specific. This may be particularly important when the strategies are designed to address support issues. Further, it will be important to consider the various types of relationships (e.g., husband/wife, father/son) in which men may serve as the caregiver as a moderator of intervention effectiveness.
Acknowledgments
The findings and conclusions in this presentation are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.U.S. Department of Health and Human Services AoA. A Profile of Older Americans: 2012. http://www.aoa.gov/AoARoot/Aging_Statistics/Profile/2012/docs/2012profile.pdf2012.
- 2.Ward BW, Schiller JS. Prevalence of Multiple Chronic Conditions among Us Adults: Estimates from the National Health Interview Survey, 2010. Prev Chronic Dis. 2013;10:E65. doi: 10.5888/pcd10.120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stone RA, Benson WF. Financing and Organizing Health and Long-Term Care Services for Older Populations. In: Prohaska T, Anderson LA, Binstock RH, editors. Public Health for an Aging Society. Baltimore: Johns Hopkins University Press; 2012. pp. 53–73. [Google Scholar]
- 4.Gilligan C. In a Different Voice. Cambridge, MA: Harvard University Press; 1982. [Google Scholar]
- 5.McGuire LC, Anderson LA, Talley RC, Crews JE. Supportive Care Needs of Americans: A Major Issue for Women as Both Recipients and Providers of Such Care. J Womens Health. 2007;16(6):784–789. doi: 10.1089/jwh.2007.CDC6. [DOI] [PubMed] [Google Scholar]
- 6.Swanberg JE, Kanatzar T, Mendiondo M, McCoskey M. Caring for Our Elders: A Contemporary Conundrum for Working People. Families in Society-the Journal of Contemporary Social Services. 2006;87(3):417–426. [Google Scholar]
- 7.Laditka JN, Laditka SB. Aging Children and Their Older Parents: The Coming Generation of Caregiving. J Women Aging. 2000;12(1–2):189–204. doi: 10.1300/J074v12n01_12. [DOI] [PubMed] [Google Scholar]
- 8.Pinquart M, Sorensen S. Gender Differences in Caregiver Stressors, Social Resources, and Health: An Updated Meta-Analysis. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):33–45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- 9.Yee JL, Schulz R. Gender Differences in Psychiatric Morbidity among Family Caregivers: A Review and Analysis. Gerontologist. 2000;40(2):147–164. doi: 10.1093/geront/40.2.147. [DOI] [PubMed] [Google Scholar]
- 10.Cuijpers P. Depressive Disorders in Caregivers of Dementia Patients: A Systematic Review. Aging & Mental Health. 2005;9(4):325–330. doi: 10.1080/13607860500090078. [DOI] [PubMed] [Google Scholar]
- 11.Judge KS, Yarry SJ, Looman WJ, Bass DM. Improved Strain and Psychosocial Outcomes for Caregivers of Individuals with Dementia: Findings from Project Answers. The Gerontologist. 2013;53(2):280–292. doi: 10.1093/geront/gns076. [DOI] [PubMed] [Google Scholar]
- 12.Mahoney R, Regan C, Katona C, Livingston G. Anxiety and Depression in Family Caregivers of People with Alzheimer Disease – the Laser-Ad Study. Am J Geriatr Psychiatry. 2005;13(9):795–801. doi: 10.1176/appi.ajgp.13.9.795. [DOI] [PubMed] [Google Scholar]
- 13.Alexander T, Wilz G. Family Caregivers: Gender Differences in Adjustment to Stroke Survivors’ Mental Changes. Rehabil Psychol. 2010;55(2):159–169. doi: 10.1037/a0019253. [DOI] [PubMed] [Google Scholar]
- 14.Vitaliano PP, Zhang JP, Scanlan JM. Is Caregiving Hazardous to One’s Physical Health? A Meta-Analysis. Psychol Bull. 2003;129(6):946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 15.Antonucci TC, Akiyama H. An Examination of Sex-Differences in Social Support among Older Men and Women. Sex Roles. 1987;17(11–12):737–749. [Google Scholar]
- 16.Shumaker SA, Hill DR. Gender Differences in Social Support and Physical Health. Health Psychol. 1991;10(2):102–111. doi: 10.1037//0278-6133.10.2.102. [DOI] [PubMed] [Google Scholar]
- 17.Anderson LA, Edwards VJ, Pearson WS, Talley RC, McGuire LC, Andresen EM. Adult Caregivers in the United States: Characteristics and Differences in Well-Being, by Caregiver Age and Caregiving Status. Prev Chronic Dis. 2013;10:E135. doi: 10.5888/pcd10.130090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spss Statistics for Windows [computer program] Armonk, NY: IBM Corp; 2012. Version Version 21.0. [Google Scholar]
- 19.Barile JP, Reeve BB, Smith AW, et al. Monitoring Population Health for Healthy People 2020: Evaluation of the Nih Promis(R) Global Health, Cdc Healthy Days, and Satisfaction with Life Instruments. Qual Life Res. 2013;22(6):1201–1211. doi: 10.1007/s11136-012-0246-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bann CM, Kobau R, Lewis MA, Zack MM, Luncheon C, Thompson WW. Development and Psychometric Evaluation of the Public Health Surveillance Well-Being Scale. Qual Life Res. 2012;21(6):1031–1043. doi: 10.1007/s11136-011-0002-9. [DOI] [PubMed] [Google Scholar]
- 21.Thompson WW, Zack MM, Krahn GL, Andresen EM, Barile JP. Health-Related Quality of Life among Older Adults with and without Functional Limitations. Am J Public Health. 2012;102(3):496–502. doi: 10.2105/AJPH.2011.300500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kendler KS, Myers J, Prescott CA. Sex Differences in the Relationship between Social Support and Risk for Major Depression: A Longitudinal Study of Opposite-Sex Twin Pairs. Am J Psychiatry. 2005;162(2):250–256. doi: 10.1176/appi.ajp.162.2.250. [DOI] [PubMed] [Google Scholar]
- 23.Schraedley PK, Gotlib IH, Hayward C. Gender Differences in Correlates of Depressive Symptoms in Adolescents. J Adolesc Health. 1999;25(2):98–108. doi: 10.1016/s1054-139x(99)00038-5. [DOI] [PubMed] [Google Scholar]
- 24.Belle D. Gender Differences the Social Moderators of Stress. In: Barnett RC, Biener L, Baruch GK, editors. Gender and Stress. New York, NY: Free Press; 1987. pp. 257–277. [Google Scholar]
- 25.King BA, Dube SR, Tynan MA. Current Tobacco Use among Adults in the United States: Findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102(11):e93–e100. doi: 10.2105/AJPH.2012.301002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gitlin LN, Schulz R. Family Caregiving of Older Adults. In: Prohaska T, Anderson LA, Binstock RH, editors. Public Health for an Aging Society. Baltimore, MD: Johns Hopkins University Press; 2012. pp. 181–204. [Google Scholar]


