Abstract
Purpose
To codify the use of multiparametric magnetic resonance imaging (mpMRI) for the interrogation of prostate neoplasia (PCa) in clinical practice and focal therapy (FT).
Methods
An international collaborative consensus project was undertaken using the Delphi method among experts in the field of PCa. An online questionnaire was presented in three consecutive rounds and modified each round based on the comments provided by the experts. Subsequently, a face-to-face meeting was held to discuss and finalize the consensus results.
Results
mpMRI should be performed in patients with prior negative biopsies if clinical suspicion remains, but not instead of the PSA test, nor as a stand-alone diagnostic tool or mpMRI-targeted biopsies only. It is not recommended to use a 1.5 Tesla MRI scanner without an endorectal or pelvic phased-array coil. mpMRI should be performed following standard biopsy-based PCa diagnosis in both the planning and follow-up of FT. If a lesion is seen, MRI-TRUS fusion biopsies should be performed for FT planning. Systematic biopsies are still required for FT planning in biopsy-naïve patients and for patients with residual PCa after FT. Standard repeat biopsies should be taken during the follow-up of FT. The final decision to perform FT should be based on histopathology. However, these consensus statements may differ for expert centers versus non-expert centers.
Conclusions
The mpMRI is an important tool for characterizing and targeting PCa in clinical practice and FT. Standardization of acquisition and reading should be the main priority to guarantee consistent mpMRI quality throughout the urological community.
Electronic supplementary material
The online version of this article (doi:10.1007/s00345-016-1932-1) contains supplementary material, which is available to authorized users.
Keywords: Focal therapy, Prostate cancer, Consensus, Magnetic resonance imaging, Delphi
Introduction
Recent technological advancements in multiparametric magnetic resonance imaging (mpMRI) have resulted in improved detection of clinically significant prostate cancer (PCa) and are increasingly used in urological practice and for focal therapy (FT). MpMRI most commonly includes T1-2-weighted imaging, dynamic contrast-enhanced (DCE) and diffusion-weighted imaging (DWI), providing clinicians with meaningful information regarding lesion volume, morphology, location and disease extent. Dynamic three-dimensional lesion characterization and risk assessment with mpMRI is key for adequate patient selection and treatment planning for FT. Clinical guidelines for standardized reporting and acquisition (e.g., PI-RADS v2 [1] or Likert scale) of prostate mpMRI are nowadays advised for both research and clinical practice. When comparing mpMRI and pathology following radical prostatectomy (sliced by use of a customized 3D mold), the positive predictive value (PPV) for the detection of PCa in the peripheral zone, central zone and overall prostate was 98, 100 and 98 %, respectively, whereas the negative predictive value (NPV) was 90 % for all mpMRI sequences [2]. In another series, the positive and negative predictive values were 86 and 85 % for lesions >0.2 mL and 77 and 95 % for lesions >0.5 mL [3]. Noteworthy, most excellent results on mpMRI PCa detection are published by expert centers where the quality of the mpMRI is assured by standardized acquisition, interpretation and image-pathology feedback. Hence, results may not be reflective to general urological practice (for an overview table on mpMRI PCa detection see [4, 5]). To illustrate, a recent systematic review of available literature on the detection of significant PCa by mpMRI showed that the NPV ranged from 63 to 98 % [6]; however, the majority of the included studies used prostate biopsies for histopathological validation.
Of interest for FT of the index lesion, the PPV of mpMRI was reported to be 82.6 % [7], whereas 80 % of all index tumors and 72 % of Gleason ≥7 tumors on whole mount pathology were identified by mpMRI [8]. Moreover, mpMRI-transrectal ultrasound (TRUS) fusion (cognitive and system-based) targeted biopsies (TB) has shown to decrease the detection of clinically insignificant PCa and increase de detection rate of clinically significant PCa with an absolute difference of 6.8 % between mpMRI-TRUS fusion TB versus TRUS-guided biopsies [9]. However, not all studies reached a statistically significant difference [9–15] (for systematic review see [9, 15]). Expert panels recommend to perform repeated mpMRI during surveillance following FT [4]. MpMRI-TRUS fusion TB has been shown to increase the detection of clinically significant PCa in the follow-up during active surveillance or during confirmatory biopsies of patients with previous negative TRUS-guided biopsies [16–18]. With increasing evidence, the position of mpMRI and MR-targeted biopsies to the accepted standard of PCa diagnostics needs to be re-evaluated. Therefore, an international multidisciplinary consensus project was initiated using the Delphi method, aiming to define the use of mpMRI and MR-targeted biopsies in clinical practice and focal therapy of PCa.
Methods
The Delphi method
This consensus project was executed following the Delphi method [19]. In short, a systematic literature search was conducted after which experts were selected and invited to participate. An online survey using online questionnaire software (www.SurveyMonkey.com) was constructed and presented to participants in three consecutive rounds. Only experts that completed all previous rounds were re-invited to participate in the subsequent round. After each round, the questionnaire was modified based on the comments provided by experts and aggregated results of the previous round were anonymously presented to allow the experts to re-evaluate their answers without peer-pressure. Subsequently, a face-to-face meeting was held to discuss the results of the online survey.
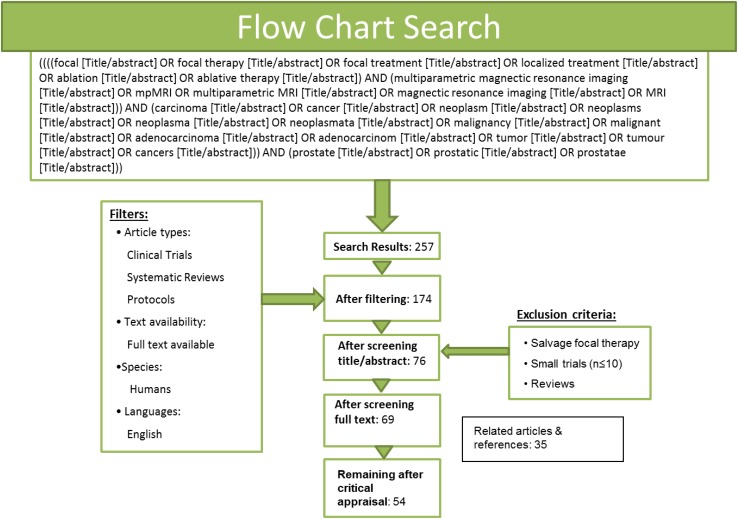
A systematic literature search of the PubMed database was performed on February 18, 2016 (see Fig. 1.), with filters: English language, full-text availability and human studies. Articles involving salvage therapy, reviews or small pilot-trials (n ≤ 10) were excluded. After reviewing the literature, 166 experts were invited to participate based on authorship or peer-recommendation. The online consensus process was performed between March 21 and May 27, 2016. The percentage of unanimity that should be reached to reach consensus was set at 80 %. A face-to-face panel meeting was organized on June 23, 2016, during the 9th International Symposium on Focal Therapy and Imaging in Prostate and Kidney Cancer (www.focaltherapy.org) and was attended by 17 participants (94 % completed all online rounds). Panelists discussed inconclusive results from the questionnaire in detail, as by definition results with online confirmed consensus cannot be changed. For an overview of the final results of the online questionnaire and face-to-face panel outcomes, see in ESM 1.
Fig. 1.
Systematic literature search
Results
Consensus process and background of participants
Ninety experts (90/166) accepted the invitation, and the response rate for the questionnaire was 100 % (90/90), 94 % (85/90), 88 % (79/90) for rounds 1, 2, and 3, respectively, and 87 % (78/90) completed all three rounds. In this group of experts 72 % were urologists, 16 % radiologists, 3 % pathologists, 3 % radiation oncologists and 6 % scientists. Average clinical experience in the field of PCa was 18.9 years (SD 9.6), 1567 years in total, and include experience with the following focal ablative modalities (primary and/or salvage); cryosurgery (n = 11), high-intensity focused ultrasound (n = 22), irreversible electroporation (n = 11), laser therapy (n = 5), vascular-targeted photodynamic therapy (n = 8), other (n = 4) and not specified/no FT (n = 29). Some participants had experience with more than one ablative modality for FT. A MRI-TRUS fusion system is used by 83 % (64/77) of clinicians in clinical practice to guide prostate biopsies or focal treatment procedures. A standardized mpMRI protocol (85 % PI-RADS, 7 % Likert, 2 % both PI-RADS/Likert, 2 % other) is used by 96 % (79/82) of clinicians. In conclusion, this group may provide a valid expert opinion due to the aforementioned experience of the participants with the utility of mpMRI and targeted biopsies in both clinical practice and focal therapy of PCa. For a list of all participants of the online survey and panel meeting, see in ESM 2.
mpMRI in clinical urological practice
It is not recommended to use a 1.5 Tesla MRI scanner without an endorectal coil (ERC) or pelvic phased-array coil (81 % of whole group against, 92 % of radiologist against) and 83 % of the radiologists were also against the use of a 1.5T with a pelvic phased-array coil only. The panel emphasized that with older 1.5T systems, the use of an ERC is indispensable. When, however, newer generation 1.5T systems are used and/or if an experienced radiologist optimizes other acquisition parameters, good image quality can be obtained with 1.5T scanners without the use of an ERC. This is in line with the recommendations of the PI-RADS Steering Committee [1].
The use of mpMRI in the workup for patients suspected of PCa was codified, and consensus was reached that mpMRI should be performed after the first set of negative TRUS-guided biopsies if clinical suspicion remains (90 %), but not instead of the PSA test (96 %) nor as stand-alone diagnostic tool (95 %) or TB only (76 % with panel agreement). There was no agreement on whether or not mpMRI should be performed in the workup for all patients with suspicion of PCa, in combination with standard (10–12 core) prostate biopsies and mpMRI-TRUS fusion TB (if lesion is seen). The panel stated that only in expert centers, where the quality is assured and their own results are monitored, mpMRI may be performed in all patients suspected of PCa since it could increase the detection of clinically significant PCa, reduce the need for repeat biopsies and may avoid prostate biopsies in patients with a negative mpMRI [20]. Therefore, it could be economically justifiable, however, adequate cost-benefit studies per health care system are lacking and should be performed.
The experts were divided on whether the current NPV of mpMRI is acceptable in clinical practice to rule out significant PCa (47 % agree/49 % disagree). The panel refines that it may be applicable for expert centers with a known NPV of >90 % for clinically significant PCa, but not in community practice. In line, no consensus was reached that, after the first set of negative prostate biopsies, repeat prostate biopsies can be deferred if mpMRI does not show any suspect lesions. However, according to a recent AUA-SAR consensus statement, deferral of repeat biopsy may be considered in expert centers in case of a negative mpMRI (without a strong clinical suspicion) [21].
If prostate biopsies are performed before mpMRI, the majority recommended the minimum acceptable interval to wait before performing mpMRI to be 6 weeks (68 % with panel agreement), although it would still impair the imaging quality (97 %). Literature shows that post biopsy hemorrhage was prevalent (57 %) within 6 weeks following prostate biopsies, but did not have a detrimental effect on tumor detection or staging [22, 23].
Focal therapy planning
MpMRI should be performed for FT planning in patients with a TRUS-guided biopsy confirmed PCa (94 %), including T1-2-weighted imaging, DCE and DWI, but without magnetic resonance spectroscopic imaging (MRSI) (83 %). MRI-TRUS fusion (either system or cognitive) is the recommended technique to perform biopsies following mpMRI (93 %) if a radiographic lesion is seen and is deemed targetable. Transperineal template mapping biopsies (TTMB) (58 % in favor with panel agreement) can also be considered, whereas TRUS-guided and in bore MR-guided biopsies are the least favorable techniques (58 and 64 % against, respectively). The panel highlighted that all techniques can be considered, depending on availability and experience, but acknowledged MRI-TRUS fusion as the optimal approach. Stand-alone MRI-targeted prostate biopsies are only sufficient for FT planning without systematic (random) biopsies in patients with previous negative TTMB (86 %), but not in biopsy-naïve patients (93 %) or in patients undergoing repeat biopsies after primary FT for low- to intermediate-risk PCa (81 %). The final decision to perform FT should be based on (targeted) histopathology and should not be based on mpMRI results/PI-RADS score (86 %) alone. Histopathological confirmation remains crucial since a recent prospective evaluation of the PI-RADS v2 found a relatively low cancer detection rate of 16, 30 and 78 % for PI-RADS score 3, 4 and 5, respectively [24].
Precise Lesion size and extension cannot be adequately assessed based with the current mpMRI quality according to the available scientific data for focal treatment planning (82 %). In a small cohort (n = 33), it was shown that mpMRI underestimated lesion size and boundaries. This underestimation was larger for high suspicion on imaging or higher Gleason score, however, if a simulated safety margin of 9 mm was applied, all lesions would have been treated completely [25]. The panel agreed that more data are needed to optimize treatment boundaries for FT planning.
mpMRI during and in the follow-up of focal therapy
MRI-TRUS system fusion is considered to be the best and most practical imaging modality to guide FT procedures (e.g., needle-placement) (86 % agreement). However, the panel remarked that cognitive fusion or other modalities might be acceptable, depending on availability and experience. MpMRI should be part of the follow-up (standardized care) following focal therapy (91 %), excluding MRSI (79 %, with panel agreement). MRI-TRUS fusion biopsies should be performed following mpMRI if a lesion is seen (78 %, with panel agreement). To illustrate: in 59 patients suspected of recurrent PCa following HIFU, the likelihood of finding PCa was greater with TB on lesions seen with T2-weighted and DCE-MRI compared with systematic random biopsies [26]. However, mpMRI with MRI-TRUS fusion TB cannot serve as stand-alone follow-up modality following FT and standard repeat (random) biopsies should be taken (78 %, with panel agreement). In a paper by Shah et al. on the histological outcomes after focal HIFU and focal cryosurgery, standard repeat biopsies were positive in 25 % (98/391) and 22 % (39/175) for focal cryosurgery and focal HIFU, respectively [27]. The majority of these positive post-treatment biopsies were clinically insignificant PCa, and whether these lesions would have been identified by mpMRI remains unknown. To the best of our knowledge, there are no large series comparing MR-guided TB with standard systematic repeat biopsies on their ability to detect clinically significant PCa following FT.
Discussion
This Delphi consensus project represents the opinion of 90 FT experts, experienced with mpMRI and MRI-TRUS fusion (TB), for all recommendations see Table 1. Despite experience, it should still be regarded as expert opinion, considered level 5 evidence, may be biased by personal enthusiasm and is potentially not reflective for community-based urologists. Nonetheless, these statements can provide clinicians guidance in areas where high-level evidence is sparse and provide a basis for standardization for clinical utilization of mpMRI and/or focal therapy that could result in improved interpretation of reported series.
Table 1.
Overview of consensus recommendations
| Recommendation | Online or panel agreement |
|---|---|
| mpMRI should be performed in patients with prior negative biopsies if clinical suspicion remains | Online |
| mpMRI should not be performed as stand-alone diagnostic tool or with mpMRI-targeted biopsies only | Online |
| mpMRI should be performed following standard biopsy-based PCa diagnosis in both the planning and follow-up of FT | Online |
| MRI-TRUS fusion is the recommended technique to perform biopsies following mpMRI | Online |
| Systematic biopsies are still required for FT planning in biopsy-naïve patients and patients with residual PCa after FT | Online |
| Repeat biopsies should be taken during the follow-up of FT | Online |
| The final decision to perform FT should be based on histopathology and not be based on mpMRI results alone | Online |
| Only in expert centers, where the quality is assured and own results are monitored, mpMRI may be performed in all patients suspected of PCa | Panel |
| Only in expert centers, deferral of repeat biopsy may be considered in case of a negative mpMRI | Panel |
| It should be our goal to guarantee high-quality mpMRI throughout the urological community before implementing it as standard of care | Panel |
The main challenge that was repeatedly encountered was the discrepancy regarding the consensus statements that can be made for expert centers versus non-expert centers. For experienced centers, where high-quality mpMRI is obtained by standardized reporting and acquisition, experience by radiologists, and where the own data are known, some excellent results have been published, establishing the mpMRI as a reliable diagnostic tool [2, 3, 6]. In community practice, this process may be less optimal, causing heterogeneous mpMRI quality with decreased sensitivity and specificity, resulting in clinically significant PCa being missed, understaging and a high number needed to image impairing the potential cost-effectiveness [20]. The panel argued that it should be our goal to guarantee high-quality mpMRI throughout the urological community before implementing it as standard of care. Important elements to achieve this are expert training, imaging-pathology feedback and/or certification. Moreover, cost-benefit studies must be performed per health care system and the availability of MRI scanners and logistics should improve [28]. Furthermore, it may be inevitable that FT can only be performed in centers where the mpMRI quality is guaranteed, since mpMRI and MRI-TRUS fusion biopsies should be performed in both the planning and follow-up of FT.
This consensus project recommended that mpMRI should be performed in patients with prior negative biopsies if clinical suspicion for PCa remains, which is stated more firmly than the EAU guideline recommendation that mpMRI may be used to evaluate the need to perform repeat biopsies [28]. Ahmed et al. presented during the 9th International Symposium on Focal Therapy and Imaging in Prostate and Kidney Cancer the first level 1 evidence that using mpMRI as a triage test, in all patients suspected of PCa (n = 576), can avoid unnecessary prostate biopsies and detected more clinically significant PCa (≥Gleason 4 + 3) than systematic (random) TRUS-guided biopsies. Based on their results, these authors calculated that in the United Kingdom it was cost-effective to perform mpMRI in all patients suspected of PCa (unpublished data, [20]). This underlines the panel statement that in expert centers mpMRI may be performed in all patients suspected of PCa. The outcomes regarding mpMRI acquisition and reporting are following the recommendations by the PI-RADS Steering Committee [1] that shows the potential that the PI-RADS recommendations have to effectuate uniform mpMRI.
Previous consensus meetings differed on the need for systematic biopsies when MRI-TRUS fusion TB were performed in biopsy-naïve patients [29, 30]. Since mpMRI quality is not constant throughout the field, abandoning systematic biopsies after MRI-TRUS fusion TB for FT planning in biopsy-naïve patients is not recommended by this consensus group. In line, systematic prostate biopsies should be taken during the follow-up after FT.
Conclusions
In expert centers mpMRI evaluation of the prostate is an established component in PCa diagnostics and this consensus project aimed to define the use of mpMRI in clinical care, especially in relation to FT. In FT, mpMRI should be used for patient selection, treatment planning or guidance, and post-treatment monitoring. Newly developed MRI-TRUS (system or cognitive) fusion is increasingly being used either during prostate biopsy procedures or during treatment planning or guidance. This consensus project was conducted during the turning point whether or not mpMRI of the prostate should be standard of care in all patients with or suspected of PCa. Standardization of acquisition and reading should be the main priority to guarantee consistent mpMRI quality throughout the field to substantiate the discrepancy between what you want to recommend and what you actually can recommend.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
All participants listed in ESM 2 that greatly helped the conduct of this study by completing the online questionnaires. This consensus project was supported by a Grant of the Cure for Cancer foundation. No commercial funding was received for the conduct of this consensus project.
Author contributions
M.J. Scheltema, J. Kay, A.W. Postema, D.M. de Bruin, T.J. Polascik and J.J. De la Rosette were involved in project development, data collection, data analysis, and manuscript writing/editing; T.M. de Reijke and M.P. Laguna were involved in project development and manuscript writing/editing; and J. Feller, J. Futterer, A.K. George, R.T. Gupta, F. Kahmann, C. Kastner, S. Natarajan, S. Rais-Bahrami, A.R. Rastinehad, G. Salomon, N. Stone, R. van Velthoven, R. Villani, A. Villers and J. Walz were involved in data collection, data analysis and manuscript editing.
Compliance with ethical standards
This consensus was conducted according to the Declaration of Helsinki and does not involve human subjects.
Conflict of interest
The following authors declare no conflict of interest: Scheltema, Tay, Postema, de Bruin, Feller, Futterer, George, Gupta, Kahmann, Kastner, Laguna, Natarajan, Rastinehad, de Reijke, Salomon, van Velthoven, Villani, Villers, Walz, Polascik, De la Rosette. Stone is owner of 3D Biopsy, Rais-Bahrami is consultant for Philips/Invivo and Gupta is consultant for Invivo.
References
- 1.Barentsz JO, Weinreb JC, Verma S, Thoeny HC, Tempany CM, Shtern F, et al. Synopsis of the PI-RADS v2 guidelines for multiparametric prostate magnetic resonance imaging and recommendations for use. Eur Urol. 2016;69(1):41–49. doi: 10.1016/j.eururo.2015.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turkbey B, Mani H, Shah V, Rastinehad AR, Bernardo M, Pohida T, et al. Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol. 2011;186(5):1818–1824. doi: 10.1016/j.juro.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Villers A, Puech P, Mouton D, Leroy X, Ballereau C, Lemaitre L. Dynamic contrast enhanced, pelvic phased array magnetic resonance imaging of localized prostate cancer for predicting tumor volume: correlation with radical prostatectomy findings. J Urol. 2006;176(6):2432–2437. doi: 10.1016/j.juro.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Muller BG, Futterer JJ, Gupta RT, Katz A, Kirkham A, Kurhanewicz J, et al. The role of magnetic resonance imaging (MRI) in focal therapy for prostate cancer: recommendations from a consensus panel. BJU Int. 2014;113(2):218–227. doi: 10.1111/bju.12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mendez MH, Joh DY, Gupta R, Polascik TJ. Current trends and new frontiers in focal therapy for localized prostate cancer. Curr Urol Rep. 2015;16(6):1–11. doi: 10.1007/s11934-015-0513-y. [DOI] [PubMed] [Google Scholar]
- 6.Futterer JJ, Briganti A, De Visschere P, Emberton M, Giannarini G, Kirkham A, et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol. 2015;68(6):1045–1053. doi: 10.1016/j.eururo.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 7.Rosenkrantz AB, Deng FM, Kim S, Lim RP, Hindman N, Mussi TC, et al. Prostate cancer: multiparametric mri for index lesion localization—a multiple-reader study. Am J Roentgenol. 2012;199(4):830–837. doi: 10.2214/AJR.11.8446. [DOI] [PubMed] [Google Scholar]
- 8.Le JD, Tan N, Shkolyar E, Lu DY, Kwan L, Marks LS et al (2014) Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol [Internet]. European Association of Urology 67(3):1–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25257029 [DOI] [PubMed]
- 9.Valerio M, Donaldson I, Emberton M, Ehdaie B, Hadaschik BA, Marks LS, et al. Detection of clinically significant prostate cancer using magnetic resonance imaging-ultrasound fusion targeted biopsy: a systematic review. Eur Urol. 2015;68(1):8–19. doi: 10.1016/j.eururo.2014.10.026. [DOI] [PubMed] [Google Scholar]
- 10.Baco E, Ukimura O, Rud E, Vlatkovic L, Svindland A, Aron M, et al. Magnetic resonance imaging-transrectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol. 2015;67(4):787–794. doi: 10.1016/j.eururo.2014.08.077. [DOI] [PubMed] [Google Scholar]
- 11.Arsov C, Becker N, Rabenalt R, Hiester A, Quentin M, Dietzel F, et al. The use of targeted MR-guided prostate biopsy reduces the risk of Gleason upgrading on radical prostatectomy. J Cancer Res Clin Oncol. 2015;141(11):2061–2068. doi: 10.1007/s00432-015-1991-5. [DOI] [PubMed] [Google Scholar]
- 12.Pokorny MR, De Rooij M, Duncan E, Schröder FH, Parkinson R, Barentsz JO, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol. 2014;66(1):22–29. doi: 10.1016/j.eururo.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Wysock JS, Rosenkrantz AB, Huang WC, Stifelman MD, Lepor H, Deng FM, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the profus trial. Eur Urol. 2014;66(2):343–351. doi: 10.1016/j.eururo.2013.10.048. [DOI] [PubMed] [Google Scholar]
- 14.Puech P, Rouvière O, Renard-Penna R. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US—MR fusion guidance versus systematic biopsy. Radiology. 2013;268(2):461–469. doi: 10.1148/radiol.13121501. [DOI] [PubMed] [Google Scholar]
- 15.Haider MA, Yao X, Loblaw A, Finelli A (2014) Multiparametric magnetic resonance imaging in the diagnosis of prostate cancer: a systematic review. Clin Oncol [Internet]. Elsevier Ltd. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0936655516300991 [DOI] [PubMed]
- 16.Da Rosa MR, Milot L, Sugar L, Vesprini D, Chung H, Loblaw A, et al. A prospective comparison of MRI-US fused targeted biopsy versus systematic ultrasound-guided biopsy for detecting clinically significant prostate cancer in patients on active surveillance. J Magn Reson Imaging. 2015;41(1):220–225. doi: 10.1002/jmri.24710. [DOI] [PubMed] [Google Scholar]
- 17.Pepe P, Garufi A, Priolo G, Pennisi M. Can MRI/TRUS fusion targeted biopsy replace saturation prostate biopsy in the re-evaluation of men in active surveillance? World J Urol. 2015 doi: 10.1007/s00345-015-1749-3. [DOI] [PubMed] [Google Scholar]
- 18.Sonn GA, Chang E, Natarajan S, Margolis DJ, MacAiran M, Lieu P, et al. Value of targeted prostate biopsy using magnetic resonance-ultrasound fusion in men with prior negative biopsy and elevated prostate-specific antigen. Eur Urol. 2014;65(4):809–815. doi: 10.1016/j.eururo.2013.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Linstone HA, Turoff M (2002) The Delphi method—techniques and applications. Delphi Method—Tech Appl [Internet]. 1–616. Available from: http://www.millennium-project.org/FRMv3_0/04-Delphi.pdf
- 20.Ahmed HU, El-Shater Bosaily A, Brown LC, Kaplan RS, Colaco-Moraes Y, Ward K et al (2016) The PROMIS study: a paired-cohort, blinded confirmatory study evaluating the accuracy of multi-parametric MRI and TRUS biopsy in men with an elevated PSA. ASCO Meet Abstr [Internet]. 34(15_suppl):5000. Available from: http://meeting.ascopubs.org/cgi/content/abstract/34/15_suppl/5000
- 21.Rosenkrantz AB, Verma S, Choyke P, Eberhardt SC, Eggener SE, Gaitonde K et al (2016) Prostate MRI and MRI-targeted biopsy in patients with a prior negative biopsy: a consensus statement of the American Urological Association and the Society of Abdominal Radiology’s Prostate Cancer Disease-Focused Panel. J Urol [Internet]. Elsevier Ltd. Epub ahead. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0022534716306590
- 22.Tamada T, Sone T, Jo Y, Yamamoto A, Yamashita T, Egashira N et al (2008) Prostate cancer: relationships between postbiopsy hemorrhage and tumor detectability at MR diagnosis. Radiology [Internet]. 248(2):531–539. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18539890 [DOI] [PubMed]
- 23.Feng T, Koopman S, Kim HL. Impact of post prostate biopsy hemorrhage on multiparametric magnetic resonance imaging. Can J Urol. 2015;22:5. [PubMed] [Google Scholar]
- 24.Mertan FV, Greer MD, Shih JH, George AK, Kongnyuy M, Muthigi A et al (2016) Prospective evaluation of the prostate imaging reporting and data system version 2 (PI-RADSv2) for prostate cancer detection. J Urol [Internet]. Elsevier Ltd 2. Available from: http://www.sciencedirect.com/science/article/pii/S0022534716301999 [DOI] [PubMed]
- 25.Le Nobin J, Rosenkrantz AB, Villers A, Orczyk C, Deng FM, Melamed J, et al. Image guided focal therapy for magnetic resonance imaging visible prostate cancer: defining a 3-Dimensional treatment margin based on magnetic resonance imaging histology co-registration analysis. J Urol. 2015;194(2):364–370. doi: 10.1016/j.juro.2015.02.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rouvière O, Girouin N, Glas L, Ben Cheikh A, Gelet A, Mège-Lechevallier F, et al. Prostate cancer transrectal HIFU ablation: detection of local recurrences using T2-weighted and dynamic contrast-enhanced MRI. Eur Radiol. 2010;20(1):48–55. doi: 10.1007/s00330-009-1520-5. [DOI] [PubMed] [Google Scholar]
- 27.Shah TT, Kasivisvanathan V, Jameson C, Freeman A, Emberton M, Ahmed HU. Histological outcomes after focal high-intensity focused ultrasound and cryotherapy. World J Urol. 2015 doi: 10.1007/s00345-015-1561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mottet N, Bellmunt J, Briers E, van den Bergh RCN, Bolla M, van Casteren NJ et al (2015) Guidelines on prostate cancer. Eur Assoc Urol Guidel [Internet] 1–156. Available from: www.uroweb.org/gls/pockets/english/07_Prostate_Cancer.pdf
- 29.Donaldson IA, Alonzi R, Barratt D, Barret E, Berge V, Bott S et al (2014) Focal therapy: patients, interventions, and outcomes—a report from a consensus meeting. Eur Urol [Internet]. European Association of Urology 67–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25281389 [DOI] [PMC free article] [PubMed]
- 30.Muller BG, van den Bos W, Brausi M, Fütterer JJ, Ghai S, Pinto PA et al (2015) Follow-up modalities in focal therapy for prostate cancer: results from a Delphi consensus project. World J Urol [Internet]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25559111 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.