Abstract
Introduction
In 2012, a total of 56 647 inguinal hernia repairs were performed in Poland. However, the absence of a uniform hernia repair register obscures the current herniology status in Poland, especially regarding laparoendoscopic procedures.
Aim
To determine the awareness of laparoendoscopic procedures among Polish surgeons and to ascertain their everyday clinical practice.
Material and methods
The data were collected at the national hernia conference in 2016, during an interactive session for surgeons with a special interest in herniology. They could respond to the survey items using the VoxVote application. All items and response options were displayed on participants’ smartphones. The questions were related to transabdominal preperitoneal/totally extraperitoneal (TAPP/TEP) hernia repair. The surgeons responded to 27 questions regarding routine inguinal hernia repair. One hundred and six surgeons from all regions of Poland participated in the survey.
Results
19.2% of respondents never inform patients about the possibility of performing laparoendoscopic repair. 45.2% admitted that they had referred a patient with a difficult inguinal hernia to another hospital or surgeon. Seventy-five percent stated they would be willing to perform TAPP/TEP if the reimbursement rates were more favourable. In bilateral hernias, 61.6% of the respondents perform a two-step open repair, while only 25% perform a single-stage laparoendoscopic repair of bilateral hernia. In women, only 13.3% perform laparoendoscopic hernia repairs, and 19.0% do not use mesh.
Conclusions
The skill level to perform TAPP/TEP repair is still inadequate among Polish surgeons. The absence of accurate data makes it impossible to verify whether the treatment methods used are compliant with the guidelines.
Keywords: groin hernia, inguinal hernia, laparoscopic repair, totally extraperitoneal, transabdominal preperitoneal, recommendations
Introduction
Although inguinal hernia repair is one of the most common surgical interventions, various procedures are used in different centres [1]. In 2012, a total of 56 647 inguinal hernia repairs reimbursed by the National Health Fund (NHF) were performed in Poland [2]. However, the absence of a uniform hernia repair register obscures the current herniology status in Poland. There are no data on the number of laparoendoscopic procedures done all over the country, which is a shameful exception in the whole of Europe. Out of 10 European countries using the Diagnosis Related Group (DRG) system, only in Poland is it impossible to determine the actual number of laparoendoscopic repairs performed annually. What is known, though, to discourage surgeons from performing laparoendoscopic hernia repair is the lack of additional reimbursement by the NHF for minimally invasive treatments. The unsatisfactory laparoendoscopy training system (i.e. the limited access to surgical training simulators, no formal requirement to train residents in transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP), and high training costs covered by surgeons themselves) additionally contributes to the existing situation [3].
Aim
The aim of the research was to determine the awareness of laparoendoscopic procedures among Polish surgeons and to ascertain their everyday clinical practice. The obtained data were intended to determine the uptake of TAPP and TEP repair, as well as to indicate the limitations of its widespread use in Poland.
Material and methods
The data were collected at the International Hernia Meeting in Zakopane, Poland, on December 10th, 2016, during an interactive session for surgeons with special interest in hernia surgery. They could respond to the survey items using the VoxVote smartphone application. All items and response options were displayed on participants’ smartphones. Some participants, who were unable to use the electronic survey system, completed the traditional questionnaire. Eventually, the results were summarised and a report was drafted.
The questions were related to TAPP and TEP hernia repair. The surgeons were requested to respond to 11 items addressing their usual practice and clinical decision-making in their hospitals as well as 16 questions assessing the contemporary guidelines on laparoendoscopic inguinal hernia repair.
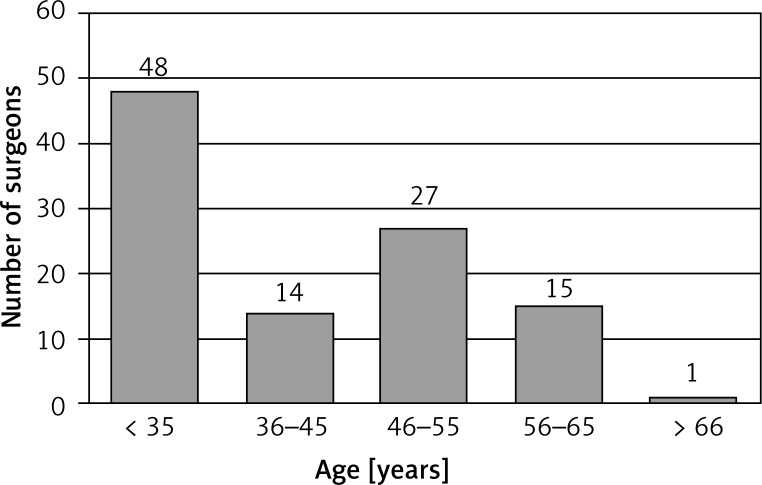
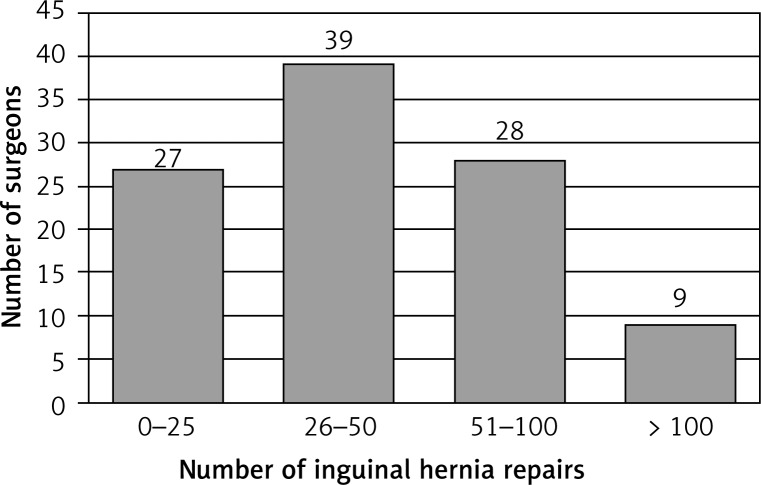
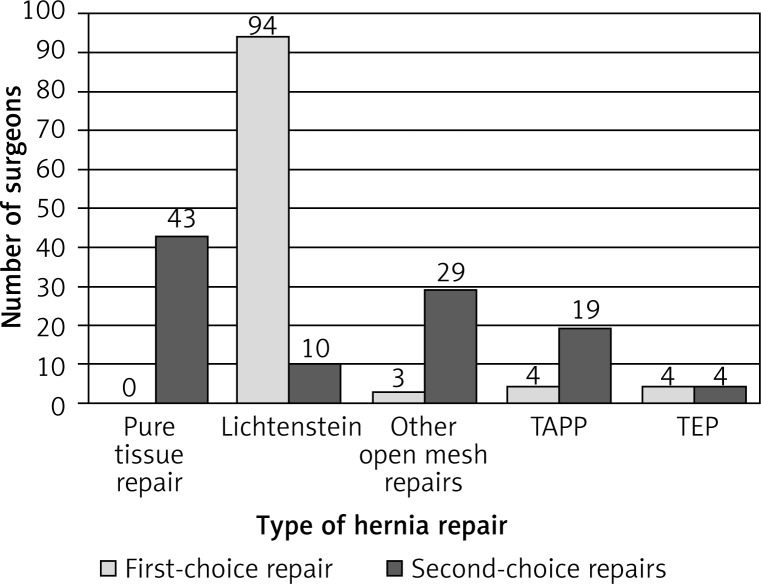
One hundred and six surgeons from all regions of Poland participated in the survey. The majority of respondents were either general surgery consultants (45.3%) or registrars (45.3%). Over half of them (58.7%) consider themselves experienced in inguinal hernia repair surgery, and one in five respondents (20.2%) consider themselves experts in hernia repair. Figures 1 and 2 show the age distribution of the respondents and the number of inguinal hernia repairs they perform annually. Twenty-one percent of the respondents perform TAPP or TEP repair, while one in three respondents work in a centre which offers laparoendoscopic hernia repair. At the same time, only 7.6% of the respondents selected TAPP and TEP repair as their preferred hernia repair method. In cases where the preferred procedure (Lichtenstein repair was selected as the preferred method by 89.6% of the respondents) could not be performed, 20.9% of surgeons would opt for TAPP or TEP repair (Figure 3). One in 4 respondents stated that their hospital did not offer a choice of different mesh implants depending on the surgical technique they intended to use.
Figure 1.
Voting surgeons’ population depending on their age (n = 105)
Figure 2.
Number of inguinal hernia repairs performed annually (n = 103)
Figure 3.
Types of hernia repair performed as the first- or the second-choice technique (n = 105)
Results
One in 5 (19.2%) respondents never informs their patients with inguinal hernia about the possibility to perform laparoendoscopic hernia repair. On the other hand, 57.7% of the respondents always inform their patients of such possibility, whereas 23.1% of them do it only in some cases. At the same time, almost a half of the respondents (45.2%) admitted that they had referred a patient with a difficult inguinal hernia to another hospital or more experienced surgeon.
Twenty-five percent of the surgeons stated that they had performed at least one TAPP or TEP repair within the three preceding months, whereas 75% of them stated they would be willing to perform them if the reimbursement rates within the NHF were more favourable. Only 8.7% of the survey respondents indicated that they would not be interested in performing laparoendoscopic hernia repair any time in the future.
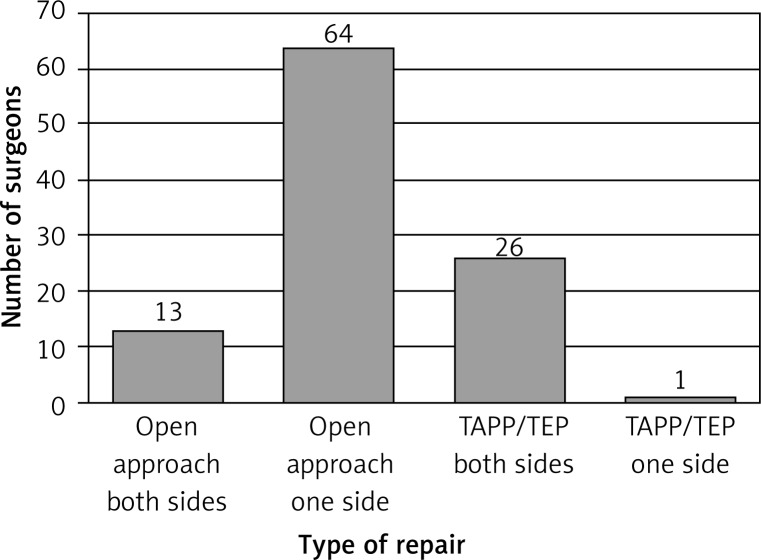
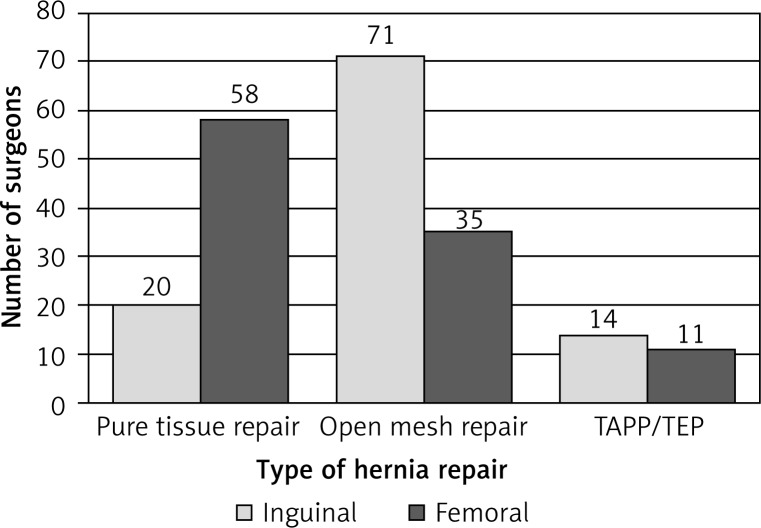
In cases of bilateral inguinal hernia, 61.6% of the respondents perform a two-step repair – the open anterior hernia repair on one side first, followed by hernia repair on the contralateral side some time later. Only 25% of the surveyed surgeons perform a single-stage laparoendoscopic repair of bilateral inguinal hernia as recommended by the international guidelines (Figure 4) [4]. A similar trend was observed in inguinal hernia repair in women: only 13.3% of the respondents perform laparoendoscopic hernia repairs, and as many as 19.0% do not use mesh implants, performing pure tissue repair. The percentage of surgeons who do not use mesh implants is even higher in cases of femoral hernia in women. As many as 55.8% of the respondents perform pure tissue repair in such cases (Figure 5).
Figure 4.
Types of repair for bilateral inguinal hernias (n = 104)
Figure 5.
Types of hernia repair in women: inguinal (n = 105) and femoral (n = 104)
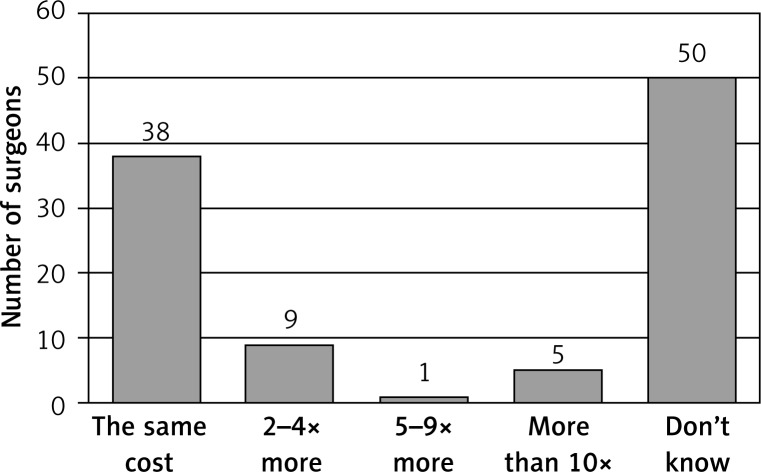
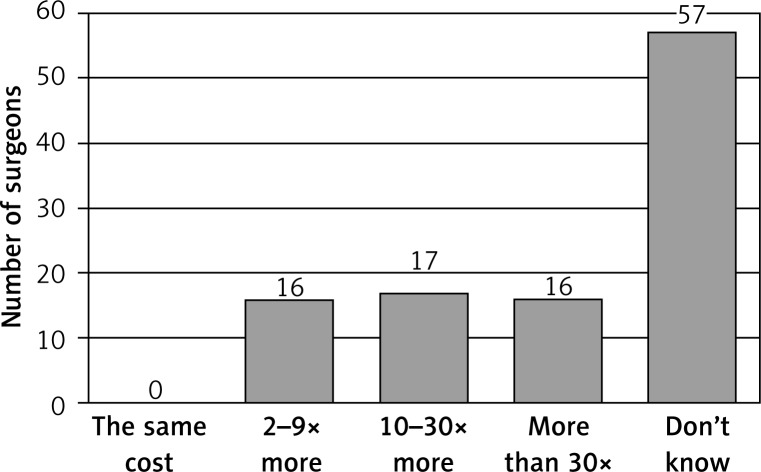
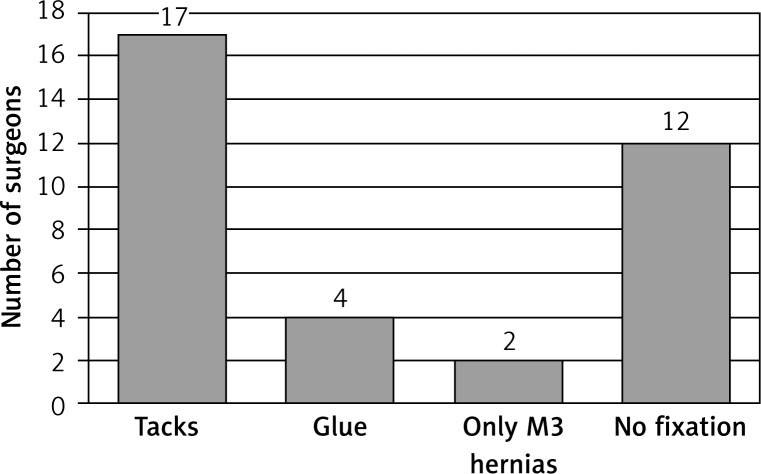
The respondents demonstrated varying degrees of knowledge relative to the costs of medical devices and disposable materials used for TAPP and TEP (should the need be determined intraoperatively). Responding to the question addressing the cost of the flat mesh implant used for TAPP or TEP as compared to the mesh implant with identical parameters used for open approach surgery, a half of the respondents stated they did not know the difference in prices, and only 36.9% of them indicated correctly that the costs of both materials were equal (Figure 6). Similar discrepancies in surgeons’ view were noted in a question related to the cost of the mesh fixation device. As many as 53.8% of the respondents stated they did not know the difference between the cost of the absorbable tack fixation device in laparoendoscopic repair and sutures used for mesh fixation during an open anterior hernia repair. Only 15.1% of the surgeons were able to correctly estimate the cost of absorbable tack fixation devices (Figure 7). At the same time, almost half of the surveyed surgeons (48.6%) use tacks for mesh fixation during laparoendoscopic hernia repair as compared to 11.4% using tissue glue (Figure 8).
Figure 6.
How many times the cost of a flat mesh for open repair exceeds the cost of a mesh with the same technical parameters used for TAPP/TEP repair (n = 103)
Figure 7.
How many times the cost of disposable absorbable tacks exceeds the cost of sutures used for mesh fixation (n = 106)
Figure 8.
Types of mesh fixation in TAPP/TEP (n = 35)
Discussion
In 2009, the European Hernia Society (EHS) published the EHS Guidelines for the Treatment of Inguinal Hernia in Adult Patients [4]. In subsequent years, literature reviews and treatment guidelines were also published by other medical societies, i.e. the International Endohernia Society and the European Association for Endoscopic Surgery [5, 6]. All the above guidelines confirm that laparoendoscopic treatment constitutes an essential part of a treatment algorithm in inguinal hernia. Unfortunately, laparoendoscopic procedures in Poland are named with the same clinical codes as in open surgery. For that reason, the actual number of TAPP and TEP procedures performed annually cannot be determined. This, in turn, makes it impossible to determine whether and to what extent the treatment guidelines are followed, as well as which treatment aspects should still be addressed and improved by e.g. surgical training. Such a meeting of surgeons with a special interest in herniology was an excellent opportunity to collect data on their current clinical practice of managing inguinal hernias.
Laparoscopic surgical techniques and endoscopic hernia repair are a part of surgical training offered to registrars in many countries [7]. The outcomes of intensive training based on interactive techniques, surgical simulators and video recording analysis show a lack of differences between the skill level of experienced surgeons, and registrars reveal that the learning curve has been completed [8]. As a result, a surgeon is able to choose the most appropriate technique for each case. Unfortunately, an opinion that laparoendoscopic hernia repair should only be performed by surgeons with advanced skills in minimally invasive surgery is still commonplace in Poland. As a result, the number of surgeons capable of performing these procedures is still insufficient. Although a third of the respondents stated that laparoendoscopic hernia repair was offered by their hospitals, only a fifth of them actually perform these procedures. Therefore, the number of TAPP and TEP procedures performed in these hospitals is low, which can impact the treatment outcomes, which are more likely to be worse than in the high-volume centres [9]. Additionally, the cost of laparoendoscopic hernia repair with the absence of adequate reimbursement made TAPP and TEP repair neither the first choice (3.8% and 3.8%, respectively) nor the second choice (18.1% and 3.8%, respectively) procedure for most of them. As a result, the number of laparoendoscopic hernia repairs performed annually by a single surgeon is not high. It does not facilitate a quick overcoming of the learning curve and gaining surgical excellence, which may have been reflected in the recurrence rates and complication rates [10]. Hernia treatment is not centralised in Poland. Furthermore, too many surgeons perform too few procedures annually. Two thirds of the surveyed surgeons perform fewer than 50 inguinal hernia repairs (open approach and/or laparoendoscopic) a year, which together with the absence of commonly implemented training schemes makes the learning curve far too long. The above remains an issue, although most of the respondents (91.3%) already use laparoendoscopic techniques in their practice or declare their willingness to use them in future.
Due to the lack of experience in laparoendoscopic hernia repair, only just over a half of the respondents inform their patients of possible TAPP or TEP repair. An equally high percentage of the surveyed surgeons never referred their patients to another surgeon or hospital, although they themselves were unable to perform both the anterior and posterior repair. The above is inconsistent with the guidelines of the European Hernia Society, which suggest providing patients with different treatment methods in a recommended treatment algorithm.
Performing a single step hernia repair of bilateral inguinal hernia was strongly recommended in the discussed document. Unfortunately, in Poland the reimbursement rates for hernia repair are identical for unilateral and bilateral hernia cases. As a result, two thirds of the surveyed surgeons opt for a two-stage approach, managing one side at a time. The available literature confirms improved cost-effectiveness of a single-stage bilateral inguinal hernia repair [11]. This improved cost-effectiveness was demonstrated even in cases of intraoperative finding of an asymptomatic hernia on the contralateral side, which should be repaired at the same time, provided that the patient has given their informed consent to such intervention [12].
The analysis of a question addressing the treatment of inguinal hernia in women demonstrated a similar discrepancy between the EHS/IHS/EAES guidelines and the actual clinical practice. Despite clear guidelines recommending the use of mesh implants in both women and men, too many of the surveyed surgeons perform pure tissue repair in inguinal and femoral hernia in female patients (19.0% and 55.8% of the respondents, respectively). According to Henrikson, concomitant femoral hernia was unexpectedly revealed in 38.1% of recurrent inguinal hernia repair procedures [13]. The chance of revealing an asymptomatic femoral hernia when performing a repair surgery is much greater with laparoendoscopic procedures. Furthermore, TAPP and TEP repair in women reduce the risk of reoperation – including reoperation due to recurrence – three-fold as compared to Lichtenstein repair (odds ratio (OR) of 0.31 and 0.41, respectively vs. OR of 1.0) [14]. This was confirmed by Schouten et al., who reported the recurrence rate of 3.0% after TEP repair, as compared to 12.5% after the open anterior mesh repair [15]. However, only 11.9% of the respondents perform TAPP or TEP repair in women.
Another commonly held belief is that the laparoendoscopic repair of inguinal hernia is excessively expensive and not cost-effective for NHF-funded centres. It appears, though, that the discussed misconception can be attributed to a lack of knowledge of technical aspects of such repair. In line with the above, 14.6% of the respondents thought that the flat mesh used for TAPP/TEP repair was more expensive than the mesh implant of identical parameters used for Lichtenstein repair, and almost half of the respondents (48.5%) replied that they did not know the difference in pricing. At the same time, the literature review suggests that the results of TAPP and TEP repair using flat mesh implants are comparable to those using the 3D or self-gripping mesh implants intended for laparoendoscopic repairs [16, 17]. The knowledge of costs of absorbable tack fixation devices used for mesh fixation was even lower. Only one in 7 (15.1%) respondents correctly estimated the price of the absorbable tack fixation device as over 30 times higher as compared to standard sutures. At the same time, 65.7% of the surveyed surgeons who perform TAPP or TEP repair use different methods of routine mesh fixation. Research confirmed that lack of routine mesh fixation in these procedures does not increase the risk of recurrence, while decreasing pain [18]. It is more important to ensure the appropriate overlap over the hernia defect, which is why the use of larger mesh implants (sized 12 × 18 cm vs. 10 × 15 cm) was recommended in TAPP and TEP repair in patients with large direct inguinal hernias (M3-EHS). Following this guideline in daily clinical practice significantly reduces treatment costs and may promote the use of laparoendoscopic inguinal hernia repair [19].
The limitation of the research was the study cohort, a group of surgeons with particular interest in hernia repair surgery. Undoubtedly, the uptake of laparoendoscopic hernia repair procedures is higher in this group as compared to the nationwide statistics. Additionally, the knowledge of contemporary surgical techniques and their familiarity with current treatment guidelines may result in more accurate responses given by this cohort as compared to surgeons with no special interest in hernia repair surgery, who perform a low number of hernia repairs annually. Hence, it seems that the availability of laparoendoscopic hernia repair to patients all over Poland is significantly lower than presented in this report.
Conclusions
The skill level to perform laparoendoscopic inguinal hernia repair is still inadequate among Polish surgeons. The absence of accurate statistics regarding TAPP and TEP repair makes it impossible to verify whether the treatment methods used in Poland (e.g. in bilateral inguinal hernia or hernia in women) are compliant with the guidelines of the respective medical societies. Improved knowledge of surgical techniques and costs of laparoendoscopic hernia repair along with access to well-planned training may result in a better uptake of TAPP and TEP repair in Polish hospitals.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003;362:1561–71. doi: 10.1016/S0140-6736(03)14746-0. [DOI] [PubMed] [Google Scholar]
- 2.O’Reilly J, Serdén L. Performance of 10 European DRG systems in explaining variation in resource utilisation in inguinal hernia repair. Health Econ. 2012;21(Suppl. 2):89–101. doi: 10.1002/hec.2839. [DOI] [PubMed] [Google Scholar]
- 3.Matyja A, Pasternak A, Solecki R, et al. Association of Polish Surgeons. Practical approach to inguinal hernia treatment – guidelines of the Association of Polish Surgeons. Pol Przegl Chir. 2015;86:552–4. doi: 10.2478/pjs-2014-0098. [DOI] [PubMed] [Google Scholar]
- 4.Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:343–403. doi: 10.1007/s10029-009-0529-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bittner R, Arregui ME, Bisgaard T, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)] Surg Endosc. 2011;25:2773–843. doi: 10.1007/s00464-011-1799-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poelman MM, van den Heuvel B, Deelder JD, et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc. 2013;27:3505–19. doi: 10.1007/s00464-013-3001-9. [DOI] [PubMed] [Google Scholar]
- 7.Bökeler U, Schwarz J, Bittner R, et al. Teaching and training in laparoscopic inguinal hernia repair (TAPP): impact of the learning curve on patient outcome. Surg Endosc. 2013;27:2886–93. doi: 10.1007/s00464-013-2849-z. [DOI] [PubMed] [Google Scholar]
- 8.Feliu-Palà X, Martín-Gómez M, Morales-Conde S, et al. The impact of the surgeon’s experience on the results of laparoscopic hernia repair. Surg Endosc. 2001;15:1467–70. doi: 10.1007/s00464-001-9017-6. [DOI] [PubMed] [Google Scholar]
- 9.Andresen K, Friis-Andersen H, Rosenberg J. Laparoscopic repair of primary inguinal hernia performed in public hospitals or low-volume centers have increased risk of reoperation for recurrence. Surg Innov. 2016;23:142–7. doi: 10.1177/1553350615596636. [DOI] [PubMed] [Google Scholar]
- 10.Köckerling F, Bittner R, Kraft B, et al. Does surgeon volume matter in the outcome of endoscopic inguinal hernia repair? Surg Endosc. 2017;31:573–85. doi: 10.1007/s00464-016-5001-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pawanindra Lal, Philips P, Chander J, et al. Is unilateral laparoscopic TEP inguinal hernia repair a job half done? The case for bilateral repair. Surg Endosc. 2010;24:1737–45. doi: 10.1007/s00464-009-0841-4. [DOI] [PubMed] [Google Scholar]
- 12.Bochkarev V, Ringley C, Vitamvas M, et al. Bilateral laparoscopic inguinal hernia repair in patients with occult contralateral inguinal defects. Surg Endosc. 2007;21:734–6. doi: 10.1007/s00464-007-9196-x. [DOI] [PubMed] [Google Scholar]
- 13.Henriksen NA, Thorup J, Jorgensen LN. Unsuspected femoral hernia in patients with a preoperative diagnosis of recurrent inguinal hernia. Hernia. 2012;16:381–5. doi: 10.1007/s10029-012-0924-3. [DOI] [PubMed] [Google Scholar]
- 14.Koch A, Edwards A, Haapaniemi S, et al. Prospective evaluation of 6895 groin hernia repairs in women. Br J Surg. 2005;92:1553–8. doi: 10.1002/bjs.5156. [DOI] [PubMed] [Google Scholar]
- 15.Schouten N, Burgmans JP, van Dalen T, et al. Female ‘groin’ hernia: totally extraperitoneal (TEP) endoscopic repair seems the most appropriate treatment modality. Hernia. 2012;16:387–92. doi: 10.1007/s10029-012-0904-7. [DOI] [PubMed] [Google Scholar]
- 16.Bell RC, Price JG. Laparoscopic inguinal hernia repair using an anatomically contoured three-dimensional mesh. Surg Endosc. 2003;17:1784–8. doi: 10.1007/s00464-002-8763-4. [DOI] [PubMed] [Google Scholar]
- 17.Klobusicky P, Hoskovec D. Reduction of chronic post-herniotomy pain and recurrence rate. Use of the anatomical self-gripping ProGrip laparoscopic mesh in TAPP hernia repair. Preliminary results of a prospective study. Videosurgery Miniinv. 2015;10:373–81. doi: 10.5114/wiitm.2015.54222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tam KW, Liang HH, Chai CY. Outcomes of staple fixation of mesh versus nonfixation in laparoscopic total extraperitoneal inguinal repair: a meta-analysis of randomized controlled trials. World J Surg. 2010;34:3065–74. doi: 10.1007/s00268-010-0760-5. [DOI] [PubMed] [Google Scholar]
- 19.Khajanchee YS, Kenyon TA, Hansen PD, et al. Economic evaluation of laparoscopic and open inguinal herniorrhaphies: the effect of cost-containment measures and internal hospital policy decisions on costs and charges. Hernia. 2004;8:196–202. doi: 10.1007/s10029-004-0212-y. [DOI] [PubMed] [Google Scholar]