Abstract
Diabetic peripheral neuropathies (DPN) are a heterogeneous group of disorders caused by neuronal dysfunction in patients with diabetes. They have differing clinical courses, distributions, fiber involvement (large or small), and pathophysiology. These complications are associated with increased morbidity, distress, and healthcare costs. Approximately 50% of patients with diabetes develop peripheral neuropathy, and the projected rise in the global burden of diabetes is spurring an increase in neuropathy. Distal symmetrical polyneuropathy (DSPN) with painful diabetic neuropathy, occurring in around 20% of diabetes patients, and diabetic autonomic neuropathy (DAN) are the most common manifestations of DPN. Optimal glucose control represents the only broadly accepted therapeutic option though evidence of its benefit in type 2 diabetes is unclear. A number of symptomatic treatments are recommended in clinical guidelines for the management of painful DPN, including antidepressants such as amitriptyline and duloxetine, the γ-aminobutyric acid analogues gabapentin and pregabalin, opioids, and topical agents such as capsaicin. However, monotherapy is frequently not effective in achieving complete resolution of pain in DPN. There is a growing need for head-to-head studies of different single-drug and combination pharmacotherapies. Due to the ubiquity of autonomic innervation in the body, DAN causes a plethora of symptoms and signs affecting cardiovascular, urogenital, gastrointestinal, pupillomotor, thermoregulatory, and sudomotor systems. The current treatment of DAN is largely symptomatic, and does not correct the underlying autonomic nerve deficit. A number of novel potential candidates, including erythropoietin analogues, angiotensin II receptor type 2 antagonists, and sodium channel blockers are currently being evaluated in phase II clinical trials.
Keywords: diabetic peripheral neuropathy, small fiber, polyneuropathy, alpha-lipoic acid, nerve fiber density
Abbreviations: ACE – angiotensin-converting enzyme; ADA – American Diabetes Association; ALA – alpha-lipoic acid; ARI – aldose reductase inhibitor; CAN – cardiovascular autonomic neuropathy; CCM – corneal confocal microscopy; CVD - cardiovascular disease; DAN – diabetic autonomic neuropathy; DCCT – Diabetes Control and Complications Trial; DPN – diabetic peripheral neuropathy; DSPN – distal symmetrical polyneuropathy; EDIC – Epidemiology of Diabetes Interventions and Complications; EFNS – European Federation of Neurological Society; EPO – erythropoietin; IASP – International Association for the Study of Pain; IENFD – intraepidermal nerve fiber density; NCV – nerve conduction velocity; NICE – National Institute for Health and Care Excellence UK; pDPN – painful diabetic peripheral neuropathy; QST - quantitative sensory testing; SNRI – serotonin norepinephrine reuptake inhibitor; T1D – type 1 diabetes mellitus; T2D – type 2 diabetes mellitus; TCA – tricyclic antidepressant; UKPDS – United Kingdom Prospective Diabetes Study; VAS – visual analogue scale; VPT – vibration perception threshold
1. Introduction
Diabetes is associated with target-organ damage, including the microvascular triopathy of nephropathy, neuropathy, and retinopathy. These complications are associated with significant healthcare costs; the United States alone spends $245 billion in their management [1]. Recent estimates from the IDF show that the current worldwide prevalence of diabetes is 8.3%, with projections suggesting that by 2030 the number of adults with diabetes will increase by 69% [2]. This rising global burden of diabetes will clearly impact the prevalence and social burden of its complications. Diabetic neuropathy is one of the most common complications of diabetes, affecting at least 50% of patients with diabetes during their lifetime [3]. It has significant adverse consequences for patients, as it interferes with their everyday physical acting, leads to psychiatric comorbidities, and causes disability in patients with diabetes [4]. The human and economic burden of diabetic neuropathy is considerable for both patients and healthcare systems [5, 6].
Though diabetic neuropathy essentially involves damage or dysfunction affecting nerve fibers, its presentations are manifold. In about one fifth of patients, painful diabetic peripheral neuropathy (pDPN) predominates, and has a significant negative impact on health-related quality of life and general function [7]. Other manifestations include small-fiber neuropathy, autonomic neuropathy, diabetic amyotrophy, radiculopathy, mononeuritis multiplex, mononeuropathy, and treatment-induced neuropathy [8]. Diabetic autonomic neuropathy (DAN) can cause orthostatic hypotension, cardiac autonomic instability, and a range of debilitating manifestations, including gastroparesis, postural hypotension, urinary retention, and erectile dysfunction [9]. Furthermore, in the ACCORD trial, the risk of death in diabetic patients with DAN was 1.44-2.15 fold greater than in those without DAN [10].
Despite the significant individual and social burden associated with diabetic neuropathy, its treatment remains unsatisfactory. This is in part due to the innately unpredictable and complex nature of the disease, combined with limited systematic diagnostic testing, which differs from diabetic retinopathy and nephropathy, where the disease is more predictable and the diagnostic testing is widespread and systematically applied. Although the ADA recommends neuropathy testing annually after 5 years of type 1 diabetes and from the diagnosis of type 2 diabetes onwards, the testing advocated (monofilament/clinical examination) detects only advanced disease, and is rarely implemented [11]. Many therapies have been the subject of clinical trials for diabetic neuropathy and painful diabetic neuropathy. However, there are currently no FDA-approved therapies for diabetic neuropathy, and only three approved therapies for pDPN. Polypharmacy is associated with its own risks, especially since medications used for neuropathic pain are not specifically targeted on peripheral nociceptive pathways, and therefore demonstrate undesirable adverse effect profiles [12-14]. To address this unmet need, an unwieldy guideline jungle has emerged to build consensus on therapeutic approaches for diabetic neuropathy [15]. In the present review, we aim to provide a pragmatic guide on a range of treatments that have been evaluated in diabetic neuropathy.
2. Diagnosis and assessment
In 2010, the Toronto consensus panel on diabetic neuropathy subdivided the disease into typical and atypical diabetic neuropathy [8]. Typical DPN is "a symmetrical, length-dependent sensorimotor polyneuropathy attributable to metabolic and microvessel alterations as a result of chronic hyperglycemia exposure and cardiovascular risk covariates." Atypical variants of diabetic neuropathy differ in onset, course, manifestations, associations, and putative mechanisms, and are likely to be associated with pain and/or dysautonomia.
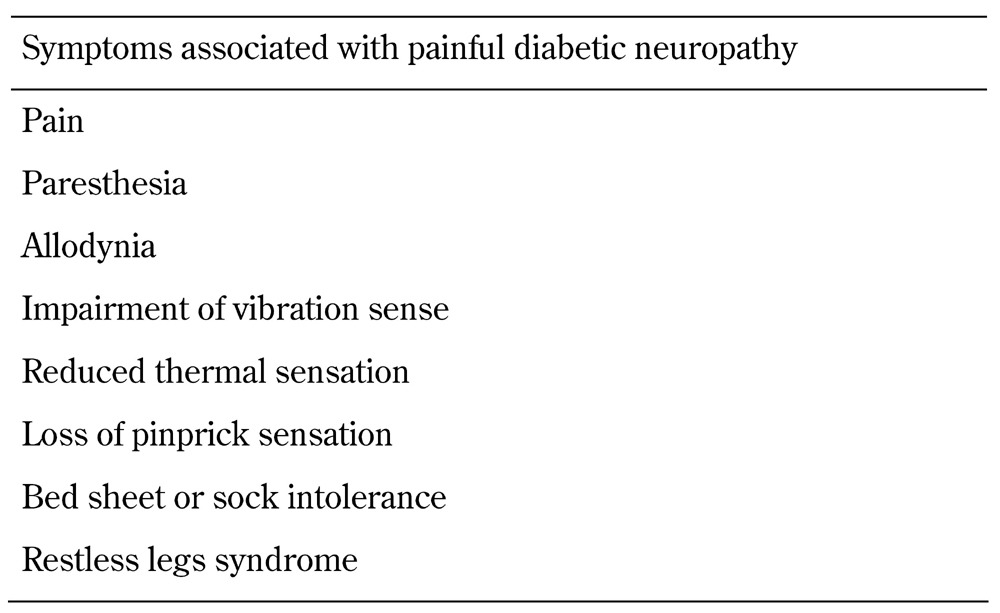
The presentation of diabetic neuropathy is variable, although the clinical picture is most frequently dominated by pain. Of note, pain is reported by approximately one third of patients with diabetes, regardless of associated neurological deficits [7]. The classical description is that of an unremitting burning pain that is characteristically worse at night, with a gradual distal-to-proximal progression of symptoms in a glove-and-stocking distribution [16]. A number of other features have been associated with the pain of diabetic neuropathy (Table 1). Motor symptoms occur less frequently, and typically appear as the disease progresses. Deficits in deep-tendon reflexes are similarly associated with advanced disease. It has been suggested that damage to small nerve fibers (carriers of nociceptive and thermal signals) may precede damage to large nerve fibers (that convey proprioception, innervate skeletal muscles, and mediate tendon reflex) [17]. Additionally, autonomic neuropathy can occur concurrently or independently of the somatic and motor dysfunction. The ubiquity of autonomic innervation in the body translates into a diverse clinical profile of DAN, which may occur in patients within two years of the diagnosis of diabetes, yet it remains an underdiagnosed entity in clinical practice [18].
Table 1. Symptoms associated with painful diabetic neuropathy.
In the clinic, painful diabetic neuropathy should be evaluated against a combination of typical symptoms of painful neuropathy, associated with neurological deficits [16]. A number of tools have evolved to aid the clinician in the diagnosis of diabetic neuropathy. The Toronto group highlighted the role of a multi-pronged approach that should consider signs or symptoms supported by neurophysiological studies and quantitative sensory testing [8]. Although nerve conduction studies are commonly advocated to confirm the diagnosis of DPN, and to assess its progression or regression in a clinical research setting, they may not detect the earliest nerve fiber damage, and only test a minority of nerve fibers, namely the large myelinated fibers [19, 20]. However, pain, temperature, autonomic function, and wound pathophysiology are largely dependent on small nerve fibers [21]. Newer techniques assess these small nerve fibers, and thus represent an intuitively attractive paradigm. Two such techniques include the visual quantification of intra-epidermal nerve fibers through skin biopsy and corneal confocal microscopy, which allows non-invasive in-vivo imaging of corneal nerves [19, 22].
Various tools have been validated to assess the neurological impairment in diabetic neuropathy. These include the Michigan Neuropathy Screening Instrument (MNSI) and Neuropathy Disability Score (NDS) [23, 24]. Pain-specific questionnaires have also been utilized to quantify painful symptoms. The available instruments include the Brief Pain Inventory [25], Neuropathic Pain Questionnaire (NPQ) [26], McGill Pain Questionnaire, and visual analogue scales (VAS) [27, 28]. Additionally, neuropathy-specific quality of life measures, such as the Europol [29] and the Norfolk Quality of Life Scale [30] may play a role in identifying patient-important factors in neuropathy.
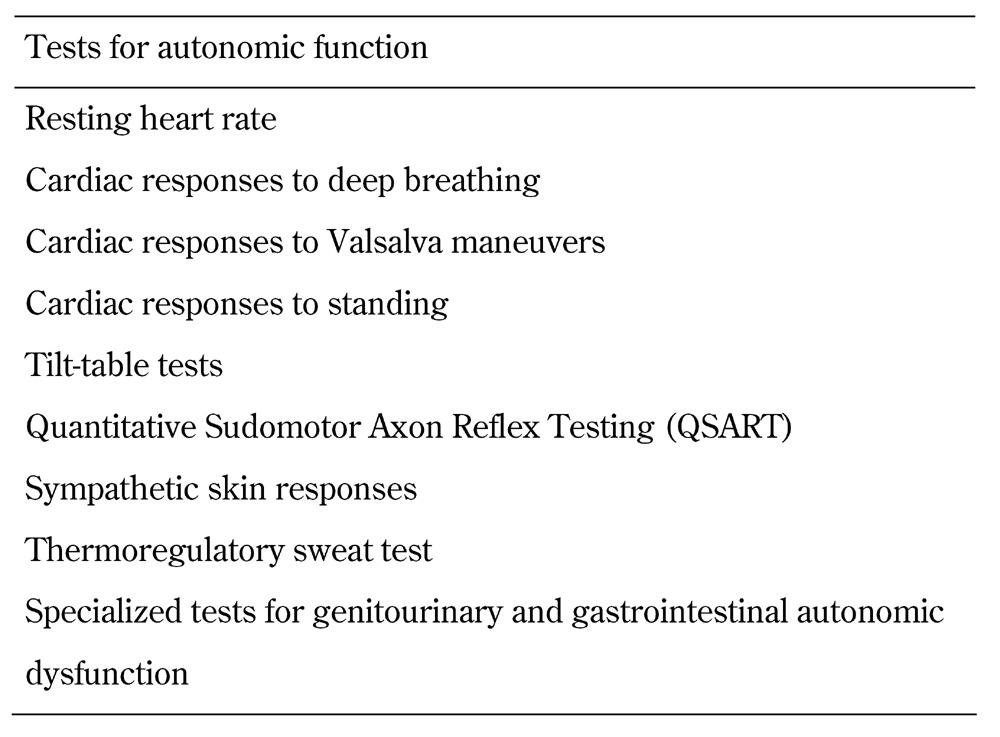
DAN is typically diagnosed through the assessment of the signs and symptoms attributable to the dysfunction of a particular organ system [8]. Cardiovascular autonomic neuropathy is perhaps the most prominent representative of the dysautonomic syndromes encountered in diabetes. Relatively simple tests, such as heart-rate variability, deep breathing, Valsalva maneuver, and blood pressure changes in response to posture can be used to assess CAN [31] (Table 2).
Table 2. Commonly used tests for autonomic function.
In the Rochester Diabetic Neuropathy Study, Dyck et al. found that in 10% of diabetic patients with neuropathy, the cause of neuropathic impairment was not attributable to diabetes [32]. This shows that it is always important to consider the differential diagnosis, which may help to identify potentially more serious or treatable causes (Table 3) in patients before reaching a firm diagnosis of diabetic neuropathy. We highlight a practical approach to the patient with diabetic neuropathy (Figure 1). Patients with diabetic neuropathy should be routinely counseled about their disease, in particular focusing on patient concerns and expectations, and the opportunity should be used to emphasize the role of satisfactory glycemic control. The lifetime risk of a patient with diabetes developing a foot lesion, including ulcers, Charcot foot abnormalities, injuries, infections, and lower-extremity amputation, has been estimated at 15-25% [33]. As neuropathy progresses, unsteadiness and gait abnormalities may be encountered, while motor dysfunction may predispose to inadvertent minor foot injuries. Thus, patients should be advised on the need for meticulous foot hygiene, appropriate footwear, and mobility support as needed.
Table 3. Important alternative causes of neuropathy to consider in the diabetic patient.
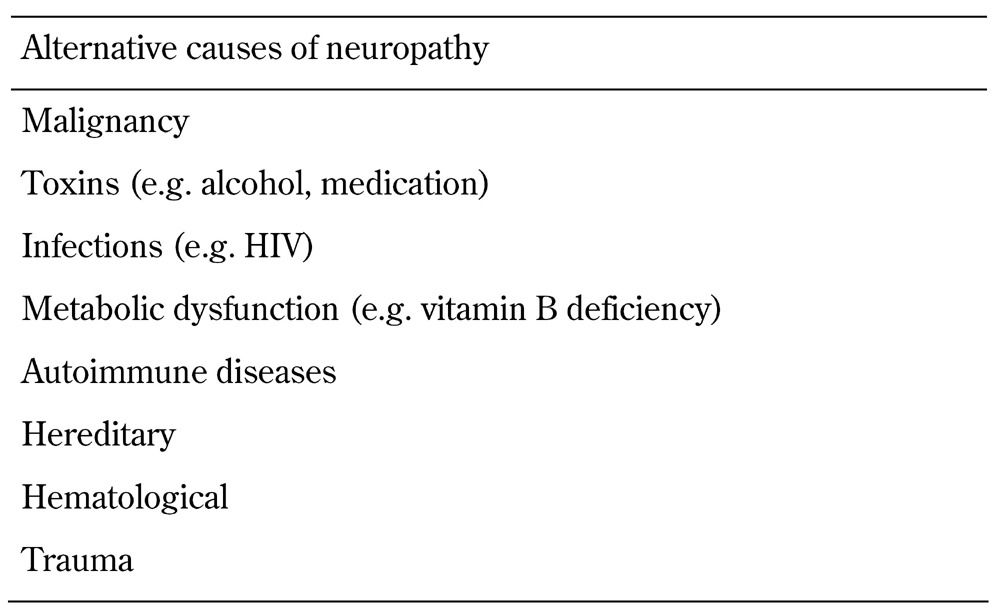
Figure 1.

Stepwise approach to diagnosis and management of diabetic peripheral neuropathy (DPN)
3. Pathogenetic treatments
A number of different therapeutic approaches that target the various pathogenetic mechanisms of diabetic neuropathy have been the subject of clinical trials (Figure 2). These treatments aim to impact favorably the underlying pathophysiological aberrations encountered in DPN by targeting different elements in the pathways leading to neurovascular dysfunction. Whilst numerous pathogenetic treatments have shown promise in experimental and early phase II studies, a recurring theme has been the lack of 'translation' into phase III clinical trials. Thus, at present there are no licensed medications in the US or UK for the treatment of diabetic neuropathy [34].
Figure 2.
Integrating pathophysiology of diabetic neuropathy and the sites of action of pathogenetic drugs. Abbreviations: ARI – aldose-reductase inhibitor, ACE – angiotensin-converting enzyme, AGE – advanced glycation end-product.
The obvious question is why no pathogenetic treatment for DPN has proved sufficiently efficacious to achieve regulatory approval. Ziegler and Luft suggested that, until the mid-1990s, trials were hampered by a generally poor design, short follow-up, and by being limited to patients with advanced DPN [35]. They suggested that trials, involving patients with early DPN, conducted over 3-5 years to establish a delay or arrest in the progression of neuropathy, rather than reversal, were more likely to be successful.
In 2007, Tesfaye et al. reported on the placebo-treated arms of two randomized controlled trials of ruboxistaurin in DPN, and found significant improvements in signs, symptoms, and quantitative vibration testing [36]. They concluded that studies of >12 months are needed to demonstrate deterioration in any placebo-treated DPN group. In the same year, Dyck et al. examined the challenges of selecting appropriate end-points for clinical trials by examining data from the placebo-treated groups of two large intervention trials and the Rochester Diabetic Neuropathy Study [37]. They concluded that there were three main reasons for the inability of these studies to demonstrate the continuous worsening of neuropathic end-points:
A strong placebo effect for symptoms and signs
Measurement noise
The fact that DPN may progress more gradually than previously thought
Commenting on the work by Dyck et al., Boulton further suggested a role for concomitant treatments (such as ACE inhibitors and lipid-lowering regimens) for cardiovascular comorbidities in people with diabetes [38]. These therapies might also positively impact peripheral nerve function, and therefore act as confounding factors in studies. Boulton reinforces the need for selecting robust end-points for future studies, which should not be prone to the variability that afflicts quantitative sensory testing and patient-reported outcome measures. This means that skin biopsy and corneal confocal microscopy may be suitable objective end-points in clinical intervention trials.
3.1 Glycemic control
Although no trial has suggested that strict glycemic control relieves pain in patients with painful DPN, erratic glucose control is associated with painful symptoms in diabetic neuropathy. Studies in type 1 diabetes (T1D) have suggested a role for optimal glycemic control in the management of diabetes. The Eurodiab Insulin-Dependent Diabetes Mellitus (IDDM) study found that suboptimal glycemic control was associated with the development of DPN in a large cohort of ~3,000 people with T1D. 1,172 patients with T1D were assessed for neuropathy at baseline (1989 to 1991) and at follow-up (1997 to 1999), with a mean follow-up period of 7.3 ± 0.6 years. A standardized protocol for the evaluation of DPN included clinical evaluation, quantitative sensory testing, and autonomic-function tests. A number of factors were independently associated with the incidence of neuropathy, including duration of diabetes, HbA1c status, and change in HbA1c value during follow-up [39]. Other than glycemic control, the incidence of neuropathy was associated with potentially modifiable cardiovascular risk factors, including body-mass index, smoking, hypertension, and raised triglyceride level [39]. Other observational studies since then have emphasized the link between poor glycemic control and DPN [40, 41].
Further evidence supporting the role of glycemic control in both primary and secondary prevention of DPN in patients with T1D comes from the Diabetic Control and Complications Trial (DCCT). This 10-year, 1,400-patient, multi-center study found that T1D patients, randomized to the intensive glucose control arm, had a 60% reduction in incidence of DPN and a 45% reduction in CAN with intensive treatment during the course of the trial. The Epidemiology of Diabetes Interventions and Complications (EDIC) was an observational study that followed up 90% of the DCCT cohort to determine the long-term impact of prior improvement in glycemic control on micro- and macrovascular outcomes [42, 43]. At the first EDIC study examination, HbA1c separation between the DCCT intensive and conventional groups narrowed substantially to 7.9% versus 8.3%. By the 5th year of the EDIC study, the difference in HbA1c between groups was no longer statistically significant (8.1% versus 8.2%; p = 0.099). Remarkably, despite no difference in glycemic control, the prevalence and incidence of DPN and CAN was significantly reduced in patients who received prior intensive insulin treatment compared with patients who received standard insulin therapy during the DCCT. This protective effect of prior intensive glycemic control (termed metabolic memory) persisted until 13 to 14 years after the end of the DCCT. For CAN, differences in glycated hemoglobin levels during the DCCT explained almost all of the protective effects of intensive versus standard therapy on the risk of incident CAN, supporting early commencement of intensive treatment in T1D. This highlights the importance of early diagnosis and timely intervention to reduce risk factors in the treatment of diabetic neuropathy.
In T2D, there is less evidence of benefits from intensive glycemic control. The United Kingdom Prospective Diabetes Study (UKPDS) emphasized the impact of glycemic control on microvascular complications in T2D, and reported a significant risk reduction for cardiovascular disease (CVD) and amputation for every 1% reduction in mean HbA1c [44]. A lower rate of impaired vibration perception threshold (VPT) with intensive therapy versus standard therapy was found, though this became significant after 15 years only (relative risk 0.60, 95% confidence interval 0.39-0.94), with no significant advantage observed at 3, 6, 9, and 12 years. The reduction in microvascular complications with intensive glycemic control in T2D was also suggested by a 6-year randomized, prospective study [45]. In 2011, Boussageon et al. conducted a meta-analysis of 7 trials involving over 34,000 patients, but they did not find a reduction in the incidence of DPN in patients managed through intensive glycemic control [46]. Furthermore, a Cochrane review of 17 randomized trials concluded that tight glycemic control prevented neuropathy in T1D, but a trend towards reduced incidence in T2D was not significant [47]. However, it should be noted that these meta-analyses have significant limitations as the targeted glucose levels, therapeutic strategies, outcome measures, trial design, and duration of follow-up differ between the separate studies. In particular, the majority of these studies utilized crude neuropathy end-points, including monofilament, foot exam, and vibration perception; these end-points cannot be expected to detect an improvement in underlying neuropathy.
The Veterans Affairs Cooperative Study reported no difference in the prevalence of autonomic neuropathy in T2D between the intensive and standard therapy arms at 2 years [48]. In contrast, the Steno-2 Trial reported that an intervention that integrated glucose control and multiple cardiovascular risk factor management reduced the prevalence of CAN, but not somatic neuropathy assessed using VPT, among patients with T2D and microalbuminuria [49].
Despite the conflicting evidence, optimization of glycemic control remains a broadly accepted first step and major aspect in the management of diabetic neuropathy, possibly with escalation to more intensive control in higher risk individuals. It should be noted that in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study, an intensive glucose-lowering regimen was associated with increased mortality (hazard ratio 1.22, 95% confidence interval 1.01 to 1.46, p = 0.04), suggesting that the harm associated with hypoglycemia and weight gain may offset the potential benefit of tight control [10]. Furthermore, three factors predicted the increased mortality in this study, namely poor glycemic control, aspirin use, and surprisingly, a history of diabetic neuropathy [50]. Therefore, the therapeutic escalation to more intensive glycemic control therapy should be considered with caution, especially in patients with diabetic neuropathy.
3.2 Pancreas transplantation
The only known therapy to restore insulin secretion in response to feedback mechanisms in patients with diabetes is pancreas transplantation [51, 52]. Differing lengths of time for improvement in DPN have been reported in patients treated with pancreas transplantation. Fioretto et al. found that the reversal of DPN is evident 10 years after transplantation [53]. Other observational studies have suggested that markers of DPN start recovering far earlier. Agudo et al. have reported an increase in action potential amplitude and conduction velocity at 3 months and 1 year after transplantation in a small study involving 26 patients [54]. In the controlled study by Kennedy et al., an improvement in sensory and motor function 12 months and 24 months after pancreas transplantation was reported in a cohort of 61 patients with T1D, although neurophysiological and autonomic function tests did not demonstrate recovery [55]. Navarro et al. reported similar findings in 115 T1D patients who underwent pancreas transplantation. These patients showed an improvement in composite scores assessing motor and sensory neuropathy, but only slight improvement in autonomic function after a longer 10-year follow-up [56].
Boucek et al. assessed intraepidermal nerve fiber density (IENFD), an objective test proposed as a gold standard for assessing the benefits of therapeutic intervention, in 18 subjects following pancreas and kidney transplantation [57]. They found that only 3 patients showed an improvement in IENFD, suggesting that some patients' DPN may have reached a non-reversible stage. However, it should be noted that all these studies used different outcome measures to assess DPN with variable follow-up periods. Hence, it is likely that the improvement in DPN reported in the literature depends entirely on the end-point used to assess DPN. Indeed, in a contemporary cohort of 15 patients, we found no significant changes in electrophysiology, quantitative sensory testing, and IENFD 6 months after transplantation, but corneal confocal microscopy, an objective test for assessing small nerve fiber damage, demonstrated significant improvement [58].
While pancreas transplantation therapy may represent the most effective method for restoring normoglycemia, its application is limited to patients with end-stage kidney disease or, less frequently, to patients with T1D and unpredictable hypoglycemia. This limitation is due to the restricted and unpredictable availability of suitable organs, complications of surgery, and the risks of long term immunosuppression. Recently, islet-cell transplantation has been considered as a less invasive alternative for suitable patients with diabetes. Del Carro and colleagues reported marked improvement in neurophysiology in a cohort of T1D patients, with no change in skin biopsy findings [59].
3.3 α-lipoic acid
Oxidative stress arises in the hyperglycemic state from an increased production of reactive oxygen species, which is due to the auto-oxidation of the excess glucose and a failure in antioxidant mechanisms [60]. These oxygen-free radicals mediate endothelial dysfunction by inhibiting nitric oxide, leading to ischemic nerve damage. Alpha-lipoic acid (ALA) is a free radical scavenger that alleviates this oxidative stress. It is used for the treatment of DPN in a number of countries, but currently does not have regulatory approval in the UK and US. ALA was found to be well-tolerated and efficacious in the management of painful DPN when administered parenterally. Indeed, Ziegler et al. reported a clinically significant improvement in the symptoms of DPN after administration of a 600 mg daily dose of ALA over 3 weeks in their meta-analysis of four placebo-controlled trials [61]. However, in the more recently published Neurological Assessment of Thioctic Acid in Diabetic Neuropathy (NATHAN) 1 study, a 4-year, multicenter, randomized controlled trial comparing ALA with placebo, Dyck et al. found no improvement in neurophysiology, quantitative sensory testing (QST), and composite neuropathy scores [37]. Importantly, the primary end-point did not deteriorate significantly in placebo-treated subjects, emphasizing the recurrent issue of a lack of placebo decline in trials of human DSPN [37].
3.4 Aldose reductase inhibitors
Aldose reductase is the rate-limiting enzyme in the polyol pathway for glucose metabolism [62]. Hyperglycemia increases the activity of aldose reductase, leading to reduced production of the vasodilator nitric oxide and eventually perpetuating ischemic nerve injury. Aldose reductase inhibitors (ARIs) have shown improvements in nerve conduction velocity, myelinated nerve fiber density, and regenerative clusters in sural nerve biopsies [63], but have consistently failed in phase III clinical trials [64]. There are also concerns about toxicity; given the limited efficacy, this has precluded their use in patients [65]. Epalrestat is the only ARI which is licensed in Japan and India based on randomized controlled trials [66]. However, a Cochrane collaboration review of 32 trials comprising 4,970 participants found no overall benefit of ARIs in DPN [67].
3.5 Benfotiamine
Benfotiamine is a fat-soluble derivative of thiamine, and has been shown in animal models to inhibit three major pathways implicated in oxidative stress and vascular dysfunction in diabetes: the advanced glycation end-product pathway, the hexosamine pathway, and the protein kinase-C-diacylglycerol pathway [68]. Although benfotiamine appears to be an appealing treatment option given its multimodal actions, clinical trials are inconclusive about its efficacy. One placebo-controlled phase III trial reported an improvement in patient-reported symptoms in the per-protocol arm of the study, although no improvement was noted in the intent-to-treat group compared with placebo [69]. Furthermore, the authors reported no difference in peripheral nerve function between the placebo and treatment arms of the study [69].
3.6 Angiotensin-converting enzyme (ACE) inhibitors
The development and progression of nephropathy, retinopathy, and neuropathy are closely related. Angiotensin-converting enzyme (ACE) inhibitors delay progression of both nephropathy and retinopathy. Therefore, we have previously investigated the effect of ACE inhibition on diabetic neuropathy. We found an improvement in neurophysiology after 12 months of treatment with the ACE inhibitor trandolapril in 41 normotensive patients with DPN, although there was no difference in measures of autonomic function compared with placebo [70]. In a larger study, Ruggenenti et al. reported a reduction in the progression of neuropathy with the ACE inhibitor delapril [71].
3.7 Protein kinase C activation
Free radicals generated by the hyperglycemia-induced activation of protein kinase C (PKC) are thought to play a role in the pathogenesis of DPN by altering vascular permeability and causing vasoconstriction. The PKC inhibitor ruboxistaurin has been evaluated in clinical trials [72, 73]. A recent systematic review of six randomized controlled trials concluded that it offered no benefit in the treatment of DPN [74].
3.8 C-peptide
C-peptide deficiency is an important contributing factor to the characteristic functional and structural abnormalities of the peripheral nerves [75]. C-peptide binds to cell membranes, resulting in stimulation of endothelial nitric oxide synthase (eNOS) and Na+, K+-ATPase [76]. In the Joslin 50-Year Medallist Study, protection from diabetic complications (i.e. retinopathy, nephropathy, and neuropathy) was thought to be due to the presence of enriched protective factors against microvascular complications [77]. In two double-blind, placebo-controlled studies in T1D patients, C-peptide replacement or placebo was given with the patients' regular insulin therapy [78, 79]. Sensory nerve conduction velocity (NCV) assessed in the sural nerve showed a significant improvement. Whilst further detailed large randomized controlled trials of sufficient quality and length are required to assess the effectiveness of C-peptide as a therapeutic intervention, a large phase III trial reported no significant improvement in neurophysiology in 2015.
3.9 Actovegin
Actovegin is a deproteinized hemoderivative extracted from calf blood through ultrafiltration. It exerts an insulin-like effect by stimulating glucose transport, pyruvate dehydrogenase, and glucose oxidation [80]. In a multicenter, randomized, placebo-controlled, double-blind trial, actovegin was found to improve VPT and quality of life [80]. Despite the improvements seen in this trial, further, more comprehensive clinical trials are needed to confirm its benefits in the treatment of DPN [65].
3.10 Other pathogenetic treatments
Inconsistent blood glucose control has been particularly associated with DPN, and it has been hypothesized that stable glycemic control may play a role in the treatment and prevention of neuropathy. Near-normal glycemia can be achieved in people with diabetes treated with continuous subcutaneous insulin infusion (CSII). These patients show improvements in neurophysiology and painful symptoms [47]. Azmi et al. recently reported corneal nerve regeneration in a cohort of subjects managed by CSII compared with subjects managed by a multiple daily injection insulin regimen, despite no difference in HbA1c over 2 years of follow-up [81]. Interestingly, in this study, QST and neurophysiology showed no improvement.
A sural nerve biopsy study has reported an association between dyslipidemia and DPN; higher triglyceride levels were correlated with a reduction in myelinated fiber density [82]. Fried et al. suggested that lowering blood lipid levels may prevent or alleviate the symptoms of DPN [83]. Indeed, Smith et al. reported that a decrease in triglyceride levels in a cohort of patients with impaired glucose tolerance managed by lifestyle interventions was associated with an increase in IENFD [84]. Furthermore, a recent double-blind, placebo-controlled study of rosuvastatin showed an improvement in neurological deficits, symptoms, and nerve conduction parameters of DPN after 12 weeks [85]. The FIELD study reported a significant reduction in minor amputations in T2D patients receiving fenofibrate [86]. This result points to an important role for triglycerides or alternative mechanisms of benefit for PPARα agonists.
4. Symptomatic treatment
Symptomatic treatment of pain is a mainstay in the treatment of diabetic neuropathy. A number of agents have been evaluated in clinical trials [15]. These treatments aim to alleviate painful symptoms, but are not targeted at the underlying pathophysiology, nor do they redress impairments such as sensory deficits from neuropathy. Navigating through the pain management in DPN can be daunting given the limited efficacy and side-effect profiles of the various medications for pDPN. Various guidelines and a number of different algorithms have been proposed to simplify the approach to treatment (Table 4) [15]. Typically, neuropathic pain medications provide limited pain relief. It is therefore important for clinicians to discuss management options and expectations with patients, with the aim of providing clinically meaningful pain relief to patients, and improving their quality of life. Indeed, 30% pain relief or a 2-point reduction in pain on the 10-point Likert scale has been reported to be clinically meaningful to patients [87]. Additionally, careful consideration of patient factors is important before starting therapy as medical and psychiatric comorbidities may influence the choice of medication.
Table 4. Comparison of selected guideline recommendations for drugs used for pain in diabetic neuropathy.
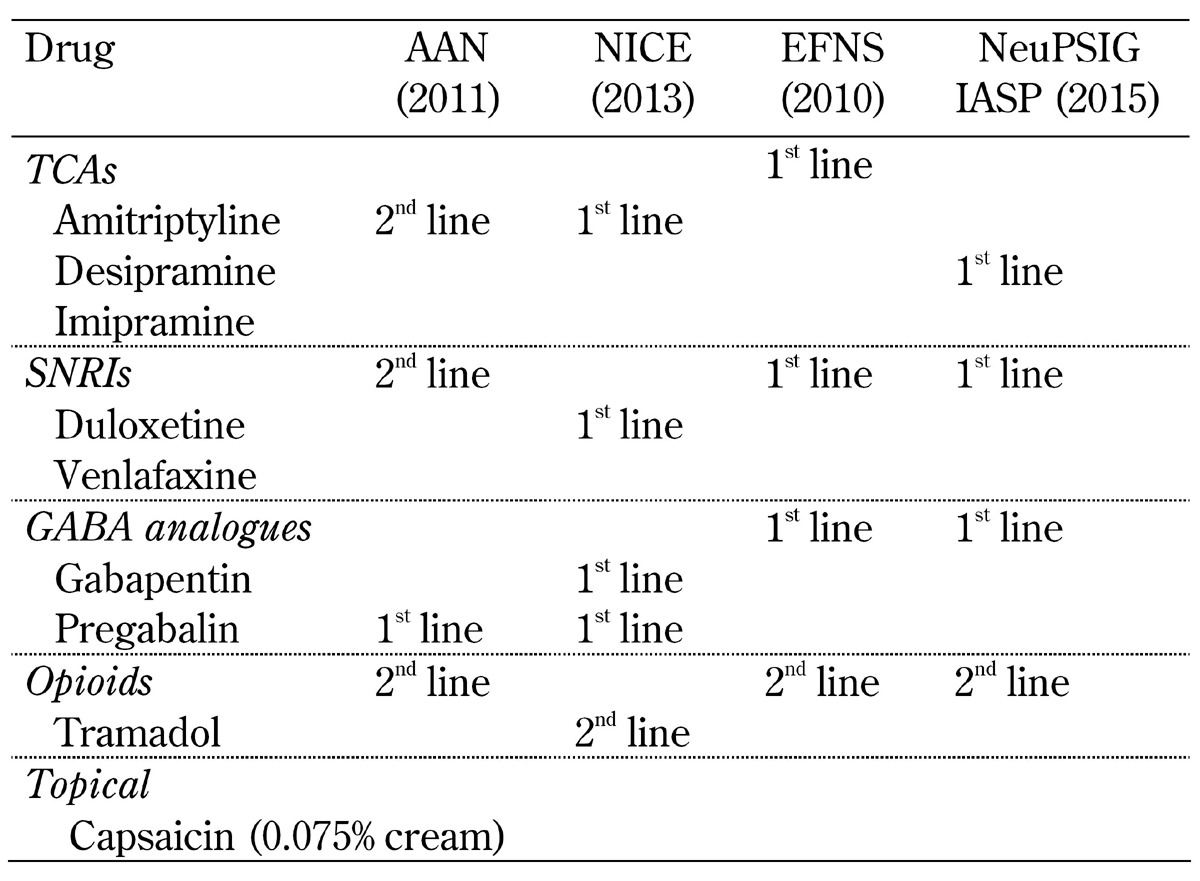
Legend: AAN – American Academy of Neurology, EFNS – European Federation of Neurological Societies, GABA – gamma aminobutyric acid, NeuPSIG IASP – Neuropathic Pain Special Interest Group of the International Association for the Study of Pain, NICE – National Institute for Health and Clinical Excellence, SNRI – serotonin norepinephrine reuptake inhibitor, TCA – tricyclic antidepressant.
Safety and effectiveness of analgesic medications for pDPN are usually compared on the basis of numbers needed to treat (NNT) or numbers needed to harm (NNH) to achieve 30% or 50% pain relief. Head-to-head trials are being conducted to compare efficacy and safety of different agents or combined regimens to improve the design of multi-drug therapy for DPN.
The use of non-steroidal anti-inflammatory drugs (NSAIDs) is not recommended in DPN because of their possible adverse properties to cause gastrointestinal hemorrhage and exacerbate pre-existing renal failure in diabetes. Despite these properties, they continue to be frequently prescribed. A study examined the general practice records of 16,690 patients with DPN and post-herpetic neuralgia, and found that 43% of patients were managed with NSAIDs [88]. In contrast, most published guidelines (Table 4) recommend tricyclic agents (TCAs), serotonin-norepinephrine reuptake inhibitors (SNRIs), or γ-aminobutyric acid (GABA) analogues (gabapentin or pregabalin) as first-line agents followed by opioids and topical treatments [15].
4.1 Tricyclic agents
Primarily based on cost considerations, TCAs have been the first-line treatment of choice for neuropathic pain for many years. In contemporary clinical care, they are less used because of the frequency and severity of their adverse effects [15]. Developed initially as antidepressants, TCAs exert a range of effects, including inhibition of serotonin and noradrenaline reuptake from synaptic clefts and acting as antagonists on N-methyl-D-aspartate (NMDA), 5-HT, histamine, muscarinic, and alpha-adrenergic receptors [89]. Some agents, such as amitriptyline, may have a role in sodium channel blockade. The exact mechanism by which they alleviate neuropathic pain remains unknown. Trials of TCAs in DPN are limited because of small sample sizes and inconsistent and inaccurate approaches to phenotyping neuropathy and assessing pain relief. Furthermore, the high doses used in clinical trials are rarely replicated in clinical practice because of the predictable anticholinergic side-effects of TCAs. Rudroju et al. reported that amitriptyline was the least safe and effective agent in a meta-analysis of six antidepressants and GABA analogues in the treatment of DPN [90]. However, two small crossover trials found evidence of benefits for active treatment with amitriptyline and desipramine over placebo in treating painful DPN [91, 92]. Additionally, evidence from randomized controlled trials indicates that imipramine is superior to placebo in managing diabetic neuropathic pain [93, 94].
4.2 Serotonin norepinephrine reuptake inhibitors (SNRIs)
SNRIs are selective inhibitors of serotonin and norepinephrine that exert their effects by disrupting the balance of neurotransmitters and stimulating descending inhibitory pathways to alleviate pain [95]. The SNRI duloxetine was the first drug to be approved by the FDA for the treatment of DPN [96]. In one of the early randomized, double-blind, placebo-controlled trials, Goldstein et al. compared doses of 20 mg, 60 mg, and 120 mg duloxetine with placebo in 457 patients [97]. 60 mg and 120 mg duloxetine were associated with a significant improvement in 24-hour average pain scores. Lunn et al. found that 60 mg and 120 mg daily doses were efficacious for the treatment of painful DPN in their analysis of data from eight studies (n = 2,728) [98]. Although the overall safety profile of duloxetine is superior to amitriptyline, with less prevalent anticholinergic side-effects [90], Goldstein et al. found that 20% and 14% of patients in their cohort treated with a daily dose of 60 mg duloxetine reported somnolence and constipation, respectively [97]. Furthermore, metabolic side-effects, including raised fasting glucose levels and weight gain, have also been described.
Venlafaxine is another SNRI that has been investigated in the context of DPN, and found to be efficacious, though it is not approved by the FDA, for this indication. Venlafaxine has been reported to be superior to placebo in alleviating the symptoms of pDPN at doses above 150 mg per day, though clinically significant electrocardiogram changes were reported in seven patients [99]. Two recent meta-analyses have suggested that venlafaxine is superior to duloxetine for treating pDPN and only sodium valproate was more efficacious when a numeric rating scale was used to assess pain relief [100, 101]. However, most trials evaluating venlafaxine in DPN are constrained by their small sample sizes and limited data about long-term safety. Thus, this option cannot be recommended ahead of duloxetine.
4.3 Anti-convulsants
Carbamazepine was among the first traditional anticonvulsants to be used for the management of painful neuropathy. Carbamazepine acts by inhibiting voltage-gated sodium channels, resulting in reduced peripheral nerve excitability. Early placebo-controlled trials suggested that carbamazepine may be useful in controlling neuropathic pain [102, 103]. Although a Cochrane review found limited evidence for its efficacy [100], In their meta-analysis, Griebeler et al. compared the effectiveness of agents used for managing painful DPN, and suggested that carbamazepine was effective in the treatment of DPN [100]. Carbamazepine is associated with myelosuppression and osteoporosis; its use has been largely superseded in clinical practice by other agents.
Oxcarbazepine, a keto-analogue of carbamazepine, caused a >50% improvement in the primary end-point of patient-reported pain scores in a multicenter trial [104]. However, two later studies found no improvement in the VAS score from baseline after treatment with oxcarbazepine [105, 106].
Gabapentin is a structural analogue of the neurotransmitter GABA that exerts its analgesic effect through inhibition of the α2δ unit of the presynaptic calcium channel [107]. In the first double-blind placebo-controlled trial, investigating gabapentin for treating painful DPN, Backonja et al. randomized 165 patients to either gabapentin or placebo [108]. They reported a significant improvement in pain scores and quality of life after 8 weeks of treatment. More recently, Mellegers et al. carried out a systematic review of 35 studies [109]. They reported that gabapentin was an effective agent for treating neuropathic pain. A Cochrane review supported the use of gabapentin for DPN with an NNT of 5.8 [110]. In a recent analysis, comparing six agents for treating painful DPN, Rudroju et al. reported that gabapentin offered the most favorable balance between safety and efficacy [90]. Therefore, gabapentin is frequently advised as a first-line treatment option in guidelines for the treatment of neuropathic pain [15].
Pregabalin is a GABA derivative with greater potency than gabapentin. It exerts its analgesic effect in a manner similar to gabapentin. Four double-blind placebo-controlled trials reported a significant improvement in pain scores following treatment with pregabalin [111-114]. This effect was found to be dose-dependent. The most beneficial effect in terms of pain relief, mood improvement, and sleep interference was reported with a dose of 600 mg. Snedecor and colleagues recently found in their meta-analysis of pharmacological agents for painful DPN that pregabalin resulted in the greatest pain relief when a VAS was used as outcome measure [101]. Based on the efficacy of pregabalin use in clinical trials, it remains one of the few agents licensed for treatment of neuropathic pain of DPN in both the USA and UK. Pregabalin use is associated with a number of adverse effects, including mood disturbance, peripheral edema, and sedation, even if there are minimal interactions with other medications. Abrupt discontinuation of pregabalin has been linked to cerebral edema and encephalopathy. Therefore, patients should be warned against abruptly stopping the therapy. Sicras et al. carried out a cost-comparative analysis of patients treated with either pregabalin or gabapentin [115]. They reported that pregabalin therapy resulted in reduced overall healthcare cost compared with gabapentin.
Raskin et al. found that topiramate alleviated neuropathic symptoms in a large placebo-controlled trial [116]. Similar results were reported in the subsequent open-label extension of this study [117]. However, three subsequent studies have reported no significant change in pain scores with topiramate therapy [118].
Lamotrigine, an antiepileptic agent with anti-nociceptive properties has also been evaluated. In two large placebo-controlled studies [119, 120], inconsistent pain relief was reported in diabetic patients randomized to the higher-dose lamotrigine group, while no significant effect was found in the low-dose lamotrigine group. Indeed, Wiffen et al. found no evidence for a benefit with lamotrigine in their Cochrane review [121].
4.4 Opioid analgesia
At analgesic doses, opioids modulate pain signals by activating spinal and supraspinal mechanisms via μ, δ, and κ type opioid receptors [89]. Tramadol is primarily a µ receptor agonist that also inhibits serotonin and norepinephrine reuptake. Harati et al. randomized 131 patients to either treatment with tramadol or placebo in a multicenter, outpatient, double-blind, parallel-group study [122]. They found that an average dose of 210 mg/day tramadol resulted in significant pain relief, as assessed through a Likert scale, and also improved social and physical functioning of subjects. These benefits persisted in the open-label extension of this 6-week trial. However, higher doses of tramadol were associated with frequent adverse effects, including nausea (23%), constipation (21%), and headache (17%).
In 2012, the extended-release (ER) formulation of tapentadol, a partial µ agonist with a norepinephrine reuptake inhibitory effect, received approval from the FDA for the relief of neuropathic pain. Schwartz and colleagues administered tapentadol ER in a 3-week open-label study with 588 patients [123]. 395 patients reported at least a one-point reduction in pain intensity on a numeric rating scale. These patients were subsequently randomized 1:1 to receive either placebo or a fixed optimal dose of tapentadol ER for a 12-week double-blind phase. Patients in the tapentadol arm of this trial reported a significant reduction in pain intensity compared with placebo. It has been proposed that tapentadol suppresses neuropathic pain through opioid spinal-supraspinal synergy in addition to the µ-opioid agonist and norepinephrine inhibitory effect [124].
Oxycodone, an opioid with greater bioavailability and potency than morphine, but with a diminished side-effect profile, has also been studied in pDPN. Gimbel et al. found that a 20 mg controlled-release dose reduced pain intensity in 159 patients [125]. In a smaller placebo-controlled crossover study of 36 patients, active treatment with oxycodone was associated with a significant improvement in average daily pain scores [126]. A recent meta-analysis by Snedecor and colleagues found that oxycodone was superior to tapentadol for pain relief in pDPN, although the data are limited by the small sample size and duration of clinical trials [101].
The use of long-term opioid therapy in DPN remains controversial because of the paucity of data on the risk-benefit ratio, considering that opioids are associated with significant long-term adverse effects, including nausea, constipation, itching, dizziness, suppression of the pituitary axis, immunological changes, and the potential for dependence and abuse. Opioids stimulate the mesolimbic reward center in the brain [127], leading to feelings of pleasure which can encourage craving and compulsive use. Indeed, opioids are among the most frequently misused prescription medication in the US [128], causing major concerns about their long-term use. This limits the wide use of opioids, and it is recommended that clinicians assess the risk of opioid misuse prior to prescribing opioids using a validated screening tool such as the Opioid Risk Tool (ORT) or the Diagnosis, Intractability, Risk, Efficacy (DIRE) score [128].
4.5 Topical therapies
Zhang et al. reported in a meta-analysis that topical application of capsaicin, an alkaloid derived from red chilli peppers, is effective in treating painful DPN [129]. The Capsaicin Study Group reported a significant reduction in pain intensity in a double-blind placebo-controlled trial involving 277 patients [130]. However, capsaicin therapy is associated with complete or nearly complete epidermal denervation in patients with subsequent impaired nerve regeneration [131]. Therefore, it cannot be recommended for DPN as it may result in an increased risk of foot ulceration due to denervation.
Campbell and colleagues assessed the role of topical 0.1% clonidine, an alpha-2 adrenergic receptor agonist with an established role in managing acute pain, in the treatment of DPN [132]. The integrity of nociceptive function was evaluated at baseline in 179 subjects by assessing the intensity of pain reported following the application of topical capsaicin. The patients were subsequently randomized either to the clonidine or the placebo arm of the trial. The authors reported a non-significant trend towards reduction in pain scores in patients receiving active treatment. Interestingly, when only patients with functional (and possibly sensitized) nociceptors in the affected skin, i.e. those with a positive capsaicin response, were considered, topical clonidine gel caused a significant reduction in pain intensity.
Topical nitrate has also been shown to benefit pDPN. Yuen and colleagues found that treatment with isosorbide dinatrate spray caused a significant reduction in pain intensity and burning discomfort in a double-blind crossover study of 22 patients [133].
Furthermore, 5% lidocaine plasters applied for 18 hours per day were shown to improve pain scores and quality of life ratings significantly in a small open-label 3-week study of 56 patients with pDPN [134]. In a recent comparative meta-analysis, Snedecor et al. reported that lidocaine plasters may be as efficacious as pregabalin [101].
Intradermal botulinum toxin type A (BTX-A) has been demonstrated to reduce pain and improve sleep quality in 18 patients with DPN in a double-blind crossover study [135]. Indeed, a recent meta-analysis of two studies in pDPN showed an improvement of 1.96 VAS points. The authors concluded that the tests for significance, low overall risk of bias, and minimal statistical heterogeneity suggested an impact of BTX-A on pain scores in pDPN with a need for further large-scale controlled trials [136].
5. Non-pharmacological approaches
As conventional medical therapies may be unsuitable or inadequate in some patients with painful neuropathy, a number of other non-conventional therapies have been proposed. Various forms of electrical stimulation have been used to manage pain in DPN, including transcutaneous electrical nerve stimulation, percutaneous electrical nerve stimulation, and frequency-modulated electromagnetic neural stimulation. In a review of eight studies, evaluating the role of electrical stimulation in DPN, Thakral and colleagues found that in six of these studies electrical stimulation was associated with an improvement in pain compared to sham treatment or placebo [137].
The role of acupuncture in managing chronic pain has been extensively investigated. Studies have recently examined its role in relieving the pain associated with DPN. In a recent single-blind trial in 45 subjects with painful DPN, Garrow et al. reported an improvement in pain in the acupuncture-treated group when compared with sham treatment [138]. However, Chen et al. suggest that it is difficult to draw conclusions from clinical trials evaluating acupuncture because these trials generally employ unconventional outcome measures of pain and have weak study designs [139].
Recently, Singleton and colleagues considered the impact of an exercise intervention on epidermal innervation, which is significantly reduced in DPN [140]. 100 patients with diabetes, but without peripheral neuropathy, were allocated to either a lifestyle counseling group or a weekly exercise intervention group. Interestingly, at the end of the one-year follow-up period, intraepidermal nerve fiber density was significantly higher in the exercise group, but unchanged in the lifestyle-counseling cohort. Similar results were reported in a cohort of patients with the metabolic syndrome [141]. While these studies suggest that regular exercise prevents DPN in diabetic patients, the significance of these findings needs to be validated in future trials to define better the type and duration of exercise and lifestyle modification required for potential benefits in patients with DPN.
6. Combination therapy for DPN
While guideline-creating organizations recommend a broad range of medications for DPN, there is increasing recognition among clinicians that monotherapy rarely provides adequate analgesia. Frequently, DPN management requires a combination of drugs to achieve adequate pain control. However, most studies only compare pharmacological therapies against placebo or sham treatment. Given the refractory nature of painful neuropathy to monotherapy, there is a growing need for comparative studies between different pharmacological agents.
Although data comparing drug combinations are sparse, some trials have compared monotherapy and combined therapy regimens. Gilron et al. conducted a small study in 56 patients with DPN or post-herpetic neuralgia who were randomized in a 1:1:1 ratio to receive one of three sequences of daily oral gabapentin, nortriptyline, or their combination [142]. Combination therapy was found to be superior in providing pain relief compared to gabapentin and nortriptyline alone, suggesting that dual therapy with these agents should be considered in patients who show only a partial response to one of these agents. Similarly, another study reported that combination therapy with morphine and gabapentin had superior efficacy with a similar adverse-effect profile compared with monotherapy with either agent at maximal tolerated doses [143].
Recent studies have also focused on head-to-head comparisons between individual pharmacological agents. Bansal et al. reported in a head-to-head comparison that pregabalin was more effective in providing pain relief in DPN than amitriptyline [144]. In a large multicenter, double-blind, parallel-group study in over 800 patients, Tesfaye and colleagues found that 60 mg/day duloxetine was more effective than 300 mg/day pregabalin (p < 0.001) in the initial 8-week phase [145]. Subsequently, a 50% response rate for pain relief was observed in 52.1% for combination and 39.3% for high-dose monotherapy (p = 0.068).
More recently, large meta-analyses have aimed to compare different therapies for painful neuropathy [100, 101]. Snedecor and colleagues evaluated data from 58 randomized controlled trials (n = 11,883), and evaluated the relative equivalence among the interventions studied [101]. Pregabalin (≥300 mg/day) was found to be the most effective agent when assessed by a 100-point VAS; topiramate was the least effective. A similar analysis was conducted by Griebeler et al. who considered 65 randomized controlled trials (n = 12,632) [100]. Comparing 27 different pharmacologic agents, Griebeler et al. reported that SNRIs showed greater pain reduction than anticonvulsants and TCAs. Although these studies may provide a convenient template for drawing relative comparisons between different drugs, the results of these studies should be interpreted with caution. It is difficult to assess and compensate for bias because of the well-documented dissonance in outcome measures, sample sizes, trial designs, and follow-up periods used in the clinical trials. This makes it challenging to draw meaningful conclusions when comparing effectiveness of different agents. Furthermore, in clinical practice, the choice of a pharmaceutical agent is also likely to be influenced by patient-specific factors, such as comorbid conditions and the potential for drug interaction and adverse effects.
7. Upcoming strategies for the treatment of painful neuropathy
Vincent and colleagues have proposed a number of cellular mechanisms as target sites for developing novel treatments of DPN [146]. The temperature-sensitive transient receptor potential channel (TRP) represents an attractive target in the pain pathway in DPN, especially as depression of TRPV1 response by capsaicin has been shown to be an effective treatment strategy [147].
Verheyen et al. have suggested that targeting the pathogenetic pathways implicated in DPN by utilizing vascular endothelial growth factor (VEGF) and VEGF-derived peptides may be an option for future therapies [148]. However, a recent clinical trial of VEGF in DPN was stopped due to lack of efficacy [149].
The angiotensin II type 2 receptor (AT2R) axis has been found to play a substantial role in promoting nociceptive signaling by stimulating hyperexcitability and persistent ectopic firing of first-order sensory neurons. Rice et al. have demonstrated that EMA401, a novel small molecule AT2R antagonist, provides significant pain relief in post-herpetic neuralgia in a novel, phase II randomized, placebo-controlled trial of 183 patients [150]. This drug remains in development as a therapeutic agent for neuropathic pain of different etiologies.
Intrathecal drug delivery systems have been used for intractable pain; they allow concentrated delivery of medication into the cerebrospinal fluid, and limit the risk of systemic adverse effects [151]. Morphine and ziconotide (a selective N-type voltage-gated calcium channel blocker) have been approved for intrathecal delivery, although their use has not been evaluated in DPN. However, implantation of intrathecal delivery systems must be undertaken with caution in patients with diabetes, given the risk of impaired wound healing and relative immunosuppression.
Erythropoietin (EPO), produced in situ by cells under stress, has been found to antagonize the production of pro-inflammatory molecules, and to promote tissue healing. While EPO has been found to ameliorate experimental DPN, its use is limited by serious adverse effects, in particular increased thrombotic risk [152]. ARA 290, a non-hematopoietic peptide designed from the structure of erythropoietin, selectively interacts with the EPO receptors that mediate tissue protection. In a recent phase-2 trial to evaluate the activity of ARA 290 in type 2 diabetes and pDPN, ARA 290 (4 mg) or placebo were self-administered subcutaneously daily for 28 days, and the subjects were followed up for an additional month without further treatment. Neuropathic symptoms were found to improve significantly in the ARA 290 group. Also, a significant improvement in corneal nerve morphology was found using corneal confocal microscopy, an objective test for DPN, in patients randomized to the ARA 290 arm of the trial relative to placebo. ARA 290 remains in development for DPN and type 2 diabetes [152].
8. Diabetic autonomic neuropathy (DAN)
The underlying pathological mechanisms of DAN can include metabolic damage to nerve fibers, neurovascular insufficiency, autoimmune damage, and neurohormonal growth factor deficiency. The manifestations of DAN are manifold (Table 5), and a number of autonomic function tests have been used for its assessment. These are outside the remit of this review and are discussed elsewhere [9]. Recently, corneal confocal microscopy has been shown to have an extremely high sensitivity and specificity for diagnosing DAN [153]. In general, the treatment of DAN seeks to alleviate the specific constellation of signs and symptoms affecting the cardiovascular, urogenital, gastrointestinal, pupillomotor, thermoregulatory, and sudomotor systems. Currently, no treatment results in complete resolution of the underlying pathophysiological abnormalities and treatment of DAN is an unmet need in clinical practice.
Table 5. Manifestations of diabetic autonomic neuropathy (DAN).
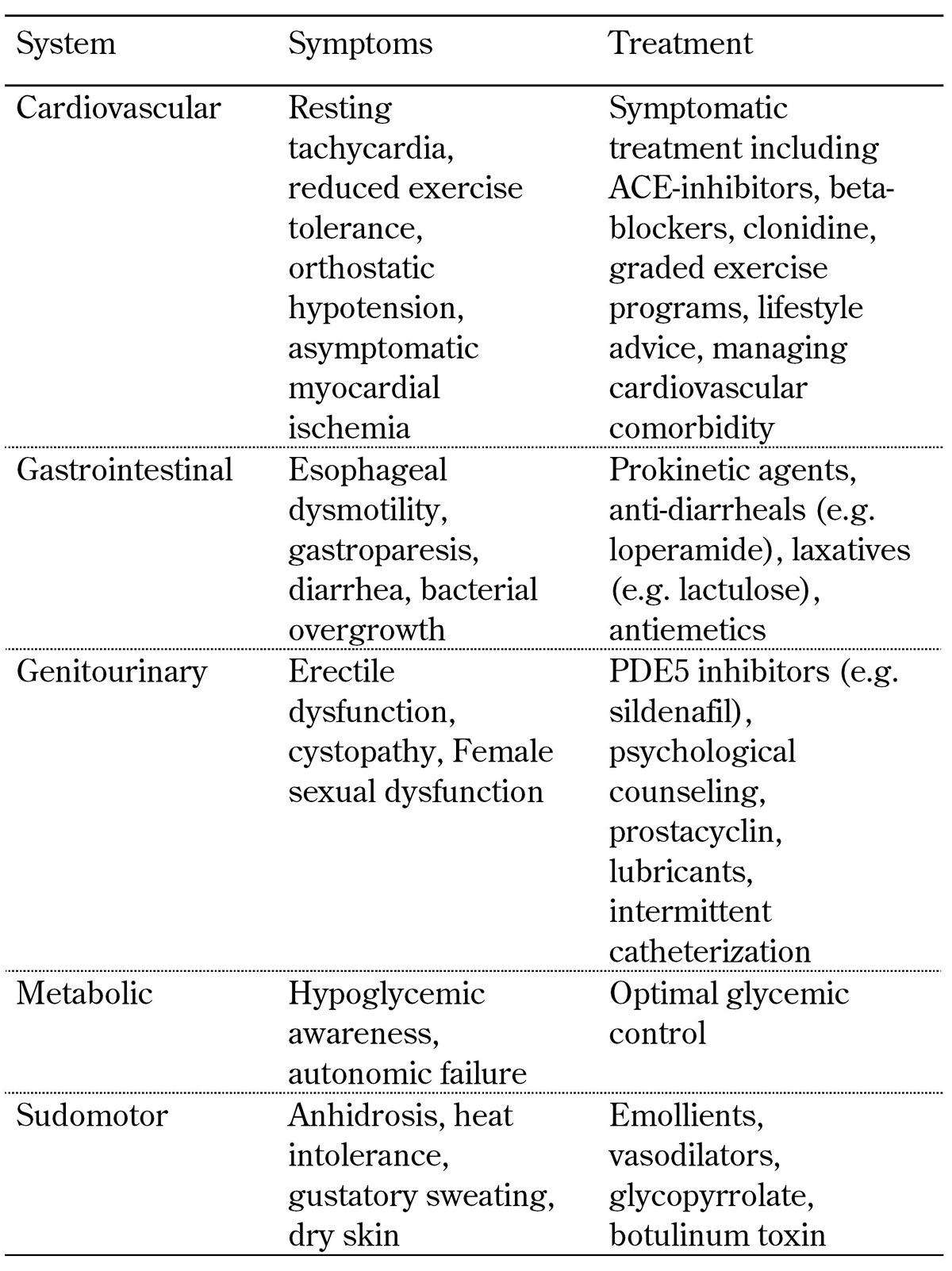
Legend: ACE – angiotensin-converting enzyme, PDE5 – phosphodiesterase 5.
8.1 Cardiac autonomic neuropathy
Cardiovascular autonomic neuropathy (CAN) is characterized by aberrant autonomic function of the cardiovascular system. It is the most prevalent and commonly studied form of DAN [18]. The prevalence of CAN ranges from 2.5% to 50% in different cohorts. CAN has been shown to negatively impact mortality due to its relationship with serious comorbidities (including silent myocardial ischemia, coronary artery disease, stroke, diabetic nephropathy, and increased perioperative morbidity). Thus, the management of CAN has important implications for prognosis in diabetes.
Data from the DCCT has demonstrated that intensive glycemic control can delay or prevent the onset of DAN in patients with type 1 diabetes, with a reduction in the prevalence of CAN by 53% in the intensive glycemic therapy group [154]. The benefits of early intensive glucose control persisted during EDIC, with a slower decline in cardiac autonomic function in patients in the intensive therapy group of the DCCT [42].
However, the situation in patients with type 2 diabetes is less clear. The VA Cooperative Study showed that strict glucose control and intensive insulin therapy did not affect the prevalence of CAN [48]. In contrast, the Steno-2 trial reported that a multifactorial cardiovascular risk intervention appeared to lower autonomic dysfunction by 63% [155]. However, glucose-lowering therapy appeared to have the least impact in preventing DAN compared with antihypertensive drugs, lipid-lowering agents, antiplatelet therapy, and vitamin-mineral supplementation.
Another drug class that has been studied in the context of DAN is ARI. In a recent meta-analysis, Hu et al. evaluated the efficacy and safety of ARIs for the treatment of CAN in diabetes, based on cardiac autonomic function tests [156]. From their analysis of ten studies, the authors concluded that ARIs improved cardiac autonomic function, with an acceptable safety profile for all agents except tolrestat. Other treatment strategies that have been suggested for CAN are shown in Table 5.
8.2 Gastrointestinal autonomic neuropathy
Gastrointestinal secretions and motility are controlled by interactions between the autonomic and enteric nervous systems [157]. Therefore, DAN can affect the gastrointestinal system at any level, and patients report a wide range of symptoms. Also, the diagnosis is frequently based on exclusion. Although esophageal dysmotility has been reported in patients with diabetes, it remains an uncommon manifestation of DAN [18]. In some cases, especially if accompanied by gastroparesis or delayed gastric emptying, esophageal dysmotility in diabetes can predispose to or worsen gastroesophageal reflux disease. It has been suggested that this should be managed conservatively using protein pump inhibitors [158].
Gastroparesis appears to occur frequently in patients with diabetes, but is asymptomatic in most cases. One study reported that impaired gastric emptying was present in as many as 50% of patients with type 2 diabetes. In symptomatic cases, high-fiber diets are advocated, although these are often empirical recommendations and require further investigation. Prokinetic agents, including erythromycin, metoclopramide, and domperidone, remain the treatments of choice [159]. In severe cases, a jejunostomy may be indicated.
The management of other gastrointestinal complications of DAN, such as diarrhea or constipation that affect 20% and 25% of patients respectively, is largely symptomatic [18]. The management of diarrhea should rely on correcting deficiencies in fluid and electrolyte balance [160]. Antidiarrheal medications such as loperamide may help to control the number of stools. Clonidine has also been shown to play a role in improving diabetic diarrhea. Constipation is usually managed conservatively with lifestyle advice focused on diet and exercise, but some patients may require the use of laxatives which should be prescribed in line with local guidelines for constipation [18].
8.3 Genitourinary autonomic neuropathy
MuCulloch and colleagues have reported the prevalence of erectile dysfunction (ED) in males with diabetes to be around 35-75% [161]. It is closely related to endothelial dysfunction; thus it is important to screen the patient for cardiovascular disease [162]. ED is managed through a multifactorial strategy. Patients should be advised to abstain from smoking or alcohol and, where possible, medications known to cause ED should be discontinued to eliminate other risk factors. Phosphodiesterase type 5 (PDE5) inhibitors such as sildenafil and tadalafil form the mainstay of the treatment [162, 163]. These agents exert their effects by stimulating the accumulation of cGMP and increasing blood flow through the corpus cavernosum. They have been shown to have little effectiveness in diabetic subjects compared with subjects without diabetes. Therefore, diabetic patients often require higher doses of these oral agents. PDE5 inhibitors may be contraindicated in cardiovascular disease or for patients on nitrate-containing drugs. In these men, prostacyclin injected directly into the corpus callosum may be considered [164].
Bladder dysfunction has been commonly reported in patients with type 1 and type 2 diabetes, although its prevalence and manifestations vary greatly between cohorts [165]. A comprehensive history and autonomic function testing may aid the clinician in diagnosing bladder dysfunction due to diabetes, which may be clinically silent, initially. The treatment aims to prevent urinary retention and infection. In a meta-analysis of 56 randomized controlled trials, Chapple et al. showed that antimuscarinic agents are generally safe and effective in patients with diabetes and overactive bladder [166]. Behavioral modalities such as pelvic-floor exercises have also been found to be effective in patients with stress, urge, and mixed incontinence [165]. Treatment of detrusor areflexia varies according to severity, and can involve exercises to encourage micturition, alpha-blocking agents such as doxazosin to encourage external sphincter relaxation, intermittent catheterization, or surgical interventions such as sacral neuromodulation or vesical neck resection.
9. Conclusions
Diabetic neuropathy is a highly prevalent and disabling condition associated with significant healthcare costs. Although diabetic neuropathies differ in clinical course, distribution, fiber involvement, and pathophysiology, two major categories include painful neuropathy and autonomic neuropathy. At present, there are no pathogenetic treatments for DPN apart from improved glycemic control.
Painful DPN is common, difficult to manage, and therefore distressing. A plethora of agents has been the subject of formal clinical trials, but achieving adequate pain relief is difficult. At present, there are only two FDA-approved medications for painful diabetic neuropathy, but a number of other agents have shown some efficacy in clinical trials. Therefore, selection of the appropriate therapy depends on the medical and psychiatric co-morbidities, potential adverse effects, and drug interactions in an individual patient.
Autonomic neuropathy has diverse clinical manifestations depending on the autonomic pathways affected by diabetes. These autonomic manifestations are responsible for the most troublesome features of DPN, and result in significant mortality and morbidity. The treatment of autonomic neuropathy depends largely on the clinical features of the disease, and is affected by the inability to resolve successfully the underlying pathophysiological deficit. Given the limitations of current therapies for DPN, further studies are necessary for identifying the best combinations of treatments for diabetic neuropathy.
Acknowledgments
Disclosures
The authors report no conflict of interests.
References
- 1.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia. 1993;36(2):150–154. doi: 10.1007/BF00400697. [DOI] [PubMed] [Google Scholar]
- 4.Oliveira AF, Valente JG, Leite IC, Schramm JM, Azevedo AS, Gadelha AM. Global burden of disease attributable to diabetes mellitus in Brazil. Cad Saude Publica. 2009;25(6):1234–1244. doi: 10.1590/s0102-311x2009000600006. [DOI] [PubMed] [Google Scholar]
- 5.Alleman CJ, Westerhout KY, Hensen M, Chambers C, Stoker M, Long S, van Nooten FE. Humanistic and economic burden of painful diabetic peripheral neuropathy in Europe: A review of the literature. Diabetes Res Clin Pract. 2015;109(2):215–225. doi: 10.1016/j.diabres.2015.04.031. [DOI] [PubMed] [Google Scholar]
- 6.Vinik A, Emir B, Cheung R, Whalen E. Relationship between pain relief and improvements in patient function/quality of life in patients with painful diabetic peripheral neuropathy or postherpetic neuralgia treated with pregabalin. Clin Ther. 2013;35(5):612–623. doi: 10.1016/j.clinthera.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Abbott CA, Malik RA, van Ross ER, Kulkarni J, Boulton AJ. Prevalence and characteristics of painful diabetic neuropathy in a large community-based diabetic population in the U.K. Diabetes Care. 2011;34(10):2220–2224. doi: 10.2337/dc11-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, Lauria G, Malik RA, Spallone V, Vinik A. et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285–2293. doi: 10.2337/dc10-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003;26(5):1553–1579. doi: 10.2337/diacare.26.5.1553. [DOI] [PubMed] [Google Scholar]
- 10.Pop-Busui R, Evans GW, Gerstein HC, Fonseca V, Fleg JL, Hoogwerf BJ, Genuth S, Grimm RH, Corson MA, Prineas R Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of cardiac autonomic dysfunction on mortality risk in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care. 2010;33(7):1578–1584. doi: 10.2337/dc10-0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boulton AJ, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, Malik RA, Maser RE, Sosenko JM, Ziegler D American Diabetes Association. Diabetic neuropathies: a statement by the American Diabetes Association. Diabetes Care. 2005;28(4):956–962. doi: 10.2337/diacare.28.4.956. [DOI] [PubMed] [Google Scholar]
- 12.Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65. doi: 10.1517/14740338.2013.827660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Black JA, Simmons RK, Boothby CE, Davies MJ, Webb D, Khunti K, Long GH, Griffin SJ. Medication burden in the first 5 years following diagnosis of type 2 diabetes: findings from the ADDITION-UK trial cohort. BMJ Open Diabetes Res Care. 2015;3(1):e000075. doi: 10.1136/bmjdrc-2014-000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sindrup SH, Jensen TS. Efficacy of pharmacological treatments of neuropathic pain: an update and effect related to mechanism of drug action. Pain. 1999;83(3):389–400. doi: 10.1016/S0304-3959(99)00154-2. [DOI] [PubMed] [Google Scholar]
- 15.Spallone V. Management of painful diabetic neuropathy: guideline guidance or jungle? Curr Diab Rep. 2012;12(4):403–413. doi: 10.1007/s11892-012-0287-2. [DOI] [PubMed] [Google Scholar]
- 16.Javed S, Petropoulos IN, Tavakoli M, Malik RA. Clinical and diagnostic features of small fiber damage in diabetic polyneuropathy. Handb Clin Neurol. 2014;126:275–290. doi: 10.1016/B978-0-444-53480-4.00019-9. [DOI] [PubMed] [Google Scholar]
- 17.Breiner A, Lovblom LE, Perkins BA, Bril V. Does the prevailing hypothesis that small-fiber dysfunction precedes large-fiber dysfunction apply to type 1 diabetic patients? Diabetes Care. 2014;37(5):1418–1424. doi: 10.2337/dc13-2005. [DOI] [PubMed] [Google Scholar]
- 18.Vinik AI, Erbas T. Diabetic autonomic neuropathy. Handb Clin Neurol. 2013;117:279–294. doi: 10.1016/B978-0-444-53491-0.00022-5. [DOI] [PubMed] [Google Scholar]
- 19.Tavakoli M, Petropoulos IN, Malik RA. Corneal confocal microscopy to assess diabetic neuropathy: an eye on the foot. J Diabetes Sci Technol. 2013;7(5):1179–1189. doi: 10.1177/193229681300700509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quattrini C, Tavakoli M, Jeziorska M, Kallinikos P, Tesfaye S, Finnigan J, Marshall A, Boulton AJ, Efron N, Malik RA. Surrogate markers of small fiber damage in human diabetic neuropathy. Diabetes. 2007;56(8):2148–2154. doi: 10.2337/db07-0285. [DOI] [PubMed] [Google Scholar]
- 21.Laverdet B, Danigo A, Girard D, Magy L, Demiot C, Desmouliere A. Skin innervation: important roles during normal and pathological cutaneous repair. Histol Histopathol. 2015;30(8):875–892. doi: 10.14670/HH-11-610. [DOI] [PubMed] [Google Scholar]
- 22.Lauria G, Cornblath DR, Johansson O, McArthur JC, Mellgren SI, Nolano M, Rosenberg N, Sommer C European Federation of Neurological Societies. EFNS guidelines on the use of skin biopsy in the diagnosis of peripheral neuropathy. Eur J Neurol. 2005;12(10):747–758. doi: 10.1111/j.1468-1331.2005.01260.x. [DOI] [PubMed] [Google Scholar]
- 23.Feldman EL, Stevens MJ, Thomas PK, Brown MB, Canal N, Greene DA. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care. 1994;17(11):1281–1289. doi: 10.2337/diacare.17.11.1281. [DOI] [PubMed] [Google Scholar]
- 24.Weintrob N, Amitay I, Lilos P, Shalitin S, Lazar L, Josefsberg Z. Bedside neuropathy disability score compared to quantitative sensory testing for measurement of diabetic neuropathy in children, adolescents, and young adults with type 1 diabetes. J Diabetes Complications. 2007;21(1):13–19. doi: 10.1016/j.jdiacomp.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 26.Krause SJ, Backonja MM. Development of a neuropathic pain questionnaire. Clin J Pain. 2003;19(5):306–314. doi: 10.1097/00002508-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 28.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 29.Vileikyte L, Peyrot M, Bundy C, Rubin RR, Leventhal H, Mora P, Shaw JE, Baker P, Boulton AJ. The development and validation of a neuropathy- and foot ulcer-specific quality of life instrument. Diabetes Care. 2003;26(9):2549–2555. doi: 10.2337/diacare.26.9.2549. [DOI] [PubMed] [Google Scholar]
- 30.Vinik EJ, Hayes RP, Oglesby A, Bastyr E, Barlow P, Ford-Molvik SL, Vinik AI. The development and validation of the Norfolk QOL-DN, a new measure of patients' perception of the effects of diabetes and diabetic neuropathy. Diabetes Technol Ther. 2005;7(3):497–508. doi: 10.1089/dia.2005.7.497. [DOI] [PubMed] [Google Scholar]
- 31.Freeman R. Assessment of cardiovascular autonomic function. Clin Neurophysiol. 2006;117(4):716–730. doi: 10.1016/j.clinph.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 32.Dyck PJ, Kratz KM, Karnes JL, Litchy WJ, Klein R, Pach JM, Wilson DM, O'Brien PC, Melton LJ, Service FJ. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy Study. Neurology. 1993;43(4):817–824. doi: 10.1212/wnl.43.4.817. [DOI] [PubMed] [Google Scholar]
- 33.Wu SC, Driver VR, Wrobel JS, Armstrong DG. Foot ulcers in the diabetic patient, prevention and treatment. Vasc Health Risk Manag. 2007;3(1):65–76. [PMC free article] [PubMed] [Google Scholar]
- 34.Malik RA. Why are there no good treatments for diabetic neuropathy? Lancet Diabetes Endocrinol. 2014;2(8):607–609. doi: 10.1016/S2213-8587(14)70067-1. [DOI] [PubMed] [Google Scholar]
- 35.Ziegler D, Luft D. Clinical trials for drugs against diabetic neuropathy: can we combine scientific needs with clinical practicalities? Int Rev Neurobiol. 2002;50:431–463. doi: 10.1016/s0074-7742(02)50085-4. [DOI] [PubMed] [Google Scholar]
- 36.Tesfaye S, Tandan R, Bastyr EJ, Kles KA, Skljarevski V, Price KL Ruboxistaurin Study Group. Factors that impact symptomatic diabetic peripheral neuropathy in placebo-administered patients from two 1-year clinical trials. Diabetes Care. 2007;30(10):2626–2632. doi: 10.2337/dc07-0608. [DOI] [PubMed] [Google Scholar]
- 37.Dyck PJ, Norell JE, Tritschler H, Schuette K, Samigullin R, Ziegler D, Bastyr EJ, Litchy WJ, O'Brien PC. Challenges in design of multicenter trials: end points assessed longitudinally for change and monotonicity. Diabetes Care. 2007;30(10):2619–2625. doi: 10.2337/dc06-2479. [DOI] [PubMed] [Google Scholar]
- 38.Boulton AJ. Whither clinical research in diabetic sensorimotor peripheral neuropathy? Problems of end point selection for clinical trials. Diabetes Care. 2007;30(10):2752–2753. doi: 10.2337/dc07-1374. [DOI] [PubMed] [Google Scholar]
- 39.Tesfaye S, Chaturvedi N, Eaton SE, Ward JD, Manes C, Ionescu-Tirgoviste C, Witte DR, Fuller JH. Vascular risk factors and diabetic neuropathy. N Engl J Med. 2005;352(4):341–350. doi: 10.1056/NEJMoa032782. [DOI] [PubMed] [Google Scholar]
- 40.Oyibo SO, Prasad YD, Jackson NJ, Jude EB, Boulton AJ. The relationship between blood glucose excursions and painful diabetic peripheral neuropathy: a pilot study. Diabet Med. 2002;19(10):870–873. doi: 10.1046/j.1464-5491.2002.00801.x. [DOI] [PubMed] [Google Scholar]
- 41.Herman WH, Aubert RE, Engelgau MM, Thompson TJ, Ali MA, Sous ES, Hegazy M, Badran A, Kenny SJ, Gunter EW. et al. Diabetes mellitus in Egypt: glycaemic control and microvascular and neuropathic complications. Diabet Med. 1998;15(12):1045–1051. doi: 10.1002/(SICI)1096-9136(1998120)15:12<1045::AID-DIA696>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 42.Pop-Busui R, Herman WH, Feldman EL, Low PA, Martin CL, Cleary PA, Waberski BH, Lachin JM, Albers JW DCCT/EDIC Research Group. DCCT and EDIC studies in type 1 diabetes: lessons for diabetic neuropathy regarding metabolic memory and natural history. Curr Diab Rep. 2010;10(4):276–282. doi: 10.1007/s11892-010-0120-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martin CL, Albers JW, Pop-Busui R DCCT/EDIC Research Group. Neuropathy and related findings in the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care. 2014;37(1):31–38. doi: 10.2337/dc13-2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, Kojima Y, Furuyoshi N, Shichiri M. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract. 1995;28(2):103–117. doi: 10.1016/0168-8227(95)01064-k. [DOI] [PubMed] [Google Scholar]
- 46.Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassai B, Erpeldinger S, Wright JM, Gueyffier F, Cornu C. Effect of intensive glucose lowering treatment on all-cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 2011;343:d4169. doi: 10.1136/bmj.d4169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Callaghan BC, Little AA, Feldman EL, Hughes RA. Enhanced glucose control for preventing and treating diabetic neuropathy. Cochrane Database Syst Rev. 2012;6:CD007543. doi: 10.1002/14651858.CD007543.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Azad N, Emanuele NV, Abraira C, Henderson WG, Colwell J, Levin SR, Nuttall FQ, Comstock JP, Sawin CT, Silbert C, Rubino FA. The effects of intensive glycemic control on neuropathy in the VA cooperative study on type II diabetes mellitus (VA CSDM) J Diabetes Complications. 1999;13(5-6):307–313. doi: 10.1016/s1056-8727(99)00062-8. [DOI] [PubMed] [Google Scholar]
- 49.Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–591. doi: 10.1056/NEJMoa0706245. [DOI] [PubMed] [Google Scholar]
- 50.Calles-Escandon J, Lovato LC, Simons-Morton DG, Kendall DM, Pop-Busui R, Cohen RM, Bonds DE, Fonseca VA, Ismail-Beigi F, Banerji MA. et al. Effect of intensive compared with standard glycemia treatment strategies on mortality by baseline subgroup characteristics: the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care. 2010;33(4):721–727. doi: 10.2337/dc09-1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tavakoli A, Liong S. Pancreatic transplant in diabetes. Adv Exp Med Biol. 2012;771:420–437. doi: 10.1007/978-1-4614-5441-0_30. [DOI] [PubMed] [Google Scholar]
- 52.Fiorina P, Secchi A. Pancreatic islet cell transplant for treatment of diabetes. Endocrinol Metab Clin North Am. 2007;36(4):999–1013. doi: 10.1016/j.ecl.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 53.Fioretto P, Steffes MW, Sutherland DE, Goetz FC, Mauer M. Reversal of lesions of diabetic nephropathy after pancreas transplantation. N Engl J Med. 1998;339(2):69–75. doi: 10.1056/NEJM199807093390202. [DOI] [PubMed] [Google Scholar]
- 54.Agudo R, Valls-Sole J, Recasens M, Fabregat N, Ricart MJ, Esmatjes E. [Effects of kidney and pancreas transplantation on neurophysiological rates of polyneuropathy and autonomous cardiac function in diabetic patients with end-stage renal disease] Med Clin (Barc) 2002;118(14):534–538. doi: 10.1016/s0025-7753(02)72442-1. [DOI] [PubMed] [Google Scholar]
- 55.Kennedy WR, Navarro X, Goetz FC, Sutherland DE, Najarian JS. Effects of pancreatic transplantation on diabetic neuropathy. N Engl J Med. 1990;322(15):1031–1037. doi: 10.1056/NEJM199004123221503. [DOI] [PubMed] [Google Scholar]
- 56.Navarro X, Sutherland DE, Kennedy WR. Long-term effects of pancreatic transplantation on diabetic neuropathy. Ann Neurol. 1997;42(5):727–736. doi: 10.1002/ana.410420509. [DOI] [PubMed] [Google Scholar]
- 57.Boucek P, Havrdova T, Voska L, Lodererova A, He L, Saudek F, Lipar K, Adamec M, Sommer C. Epidermal innervation in type 1 diabetic patients: a 2.5-year prospective study after simultaneous pancreas/kidney transplantation. Diabetes Care. 2008;31(8):1611–1612. doi: 10.2337/dc07-2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mehra S, Tavakoli M, Kallinikos PA, Efron N, Boulton AJ, Augustine T, Malik RA. Corneal confocal microscopy detects early nerve regeneration after pancreas transplantation in patients with type 1 diabetes. Diabetes Care. 2007;30(10):2608–2612. doi: 10.2337/dc07-0870. [DOI] [PubMed] [Google Scholar]
- 59.Del Carro U, Fiorina P, Amadio S, De Toni Franceschini L, Petrelli A, Menini S, Martinelli Boneschi F, Ferrari S, Pugliese G, Maffi P. et al. Evaluation of polyneuropathy markers in type 1 diabetic kidney transplant patients and effects of islet transplantation: neurophysiological and skin biopsy longitudinal analysis. Diabetes Care. 2007;30(12):3063–3069. doi: 10.2337/dc07-0206. [DOI] [PubMed] [Google Scholar]
- 60.Kaur S, Pandhi P, Dutta P. Painful diabetic neuropathy: an update. Ann Neurosci. 2011;18(4):168–175. doi: 10.5214/ans.0972-7531.1118409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ziegler D, Nowak H, Kempler P, Vargha P, Low PA. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a meta-analysis. Diabet Med. 2004;21(2):114–121. doi: 10.1111/j.1464-5491.2004.01109.x. [DOI] [PubMed] [Google Scholar]
- 62.Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol. 2012;11(6):521–534. doi: 10.1016/S1474-4422(12)70065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tomlinson DR, Moriarty RJ, Mayer JH. Prevention and reversal of defective axonal transport and motor nerve conduction velocity in rats with experimental diabetes by treatment with the aldose reductase inhibitor Sorbinil. Diabetes. 1984;33(5):470–476. doi: 10.2337/diab.33.5.470. [DOI] [PubMed] [Google Scholar]
- 64.Boulton AJ, Malik RA, Arezzo JC, Sosenko JM. Diabetic Somatic Neuropathies. Diabetes Care. 2004;27(6):1458–1486. doi: 10.2337/diacare.27.6.1458. [DOI] [PubMed] [Google Scholar]
- 65.Boulton AJ, Kempler P, Ametov A, Ziegler D. Whither pathogenetic treatments for diabetic polyneuropathy? Diabetes Metab Res Rev. 2013;29(5):327–333. doi: 10.1002/dmrr.2397. [DOI] [PubMed] [Google Scholar]
- 66.Goto Y, Hotta N, Shigeta Y, Sakamoto N, Kikkawa R. Effects of an aldose reductase inhibitor, epalrestat, on diabetic neuropathy. Clinical benefit and indication for the drug assessed from the results of a placebo-controlled double-blind study. Biomed Pharmacother. 1995;49(6):269–277. doi: 10.1016/0753-3322(96)82642-4. [DOI] [PubMed] [Google Scholar]
- 67.Chalk C, Benstead TJ, Moore F. Aldose reductase inhibitors for the treatment of diabetic polyneuropathy. Cochrane Database Syst Rev. 2007;4:CD004572. doi: 10.1002/14651858.CD004572.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hammes HP, Du X, Edelstein D, Taguchi T, Matsumura T, Ju Q, Lin J, Bierhaus A, Nawroth P, Hannak D. et al. Benfotiamine blocks three major pathways of hyperglycemic damage and prevents experimental diabetic retinopathy. Nat Med. 2003;9(3):294–299. doi: 10.1038/nm834. [DOI] [PubMed] [Google Scholar]
- 69.Stracke H, Gaus W, Achenbach U, Federlin K, Bretzel RG. Benfotiamine in diabetic polyneuropathy (BENDIP): results of a randomised, double blind, placebo-controlled clinical study. Exp Clin Endocrinol Diabetes. 2008;116(10):600–605. doi: 10.1055/s-2008-1065351. [DOI] [PubMed] [Google Scholar]
- 70.Malik RA, Williamson S, Abbott C, Carrington AL, Iqbal J, Schady W, Boulton AJ. Effect of angiotensin-converting-enzyme (ACE) inhibitor trandolapril on human diabetic neuropathy: randomised double-blind controlled trial. Lancet. 1998;352(9145):1978–1981. doi: 10.1016/S0140-6736(98)02478-7. [DOI] [PubMed] [Google Scholar]
- 71.Ruggenenti P, Lauria G, Iliev IP, Fassi A, Ilieva AP, Rota S, Chiurchiu C, Barlovic DP, Sghirlanzoni A, Lombardi R. et al. Effects of manidipine and delapril in hypertensive patients with type 2 diabetes mellitus: the delapril and manidipine for nephroprotection in diabetes (DEMAND) randomized clinical trial. Hypertension. 2011;58(5):776–783. doi: 10.1161/HYPERTENSIONAHA.111.174474. [DOI] [PubMed] [Google Scholar]
- 72.Brooks B, Delaney-Robinson C, Molyneaux L, Yue DK. Endothelial and neural regulation of skin microvascular blood flow in patients with diabetic peripheral neuropathy: effect of treatment with the isoform-specific protein kinase C beta inhibitor, ruboxistaurin. J Diabetes Complications. 2008;22(2):88–95. doi: 10.1016/j.jdiacomp.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 73.Vinik AI, Bril V, Kempler P, Litchy WJ, Tesfaye S, Price KL, Bastyr EJ 3rd MBBQ Study Group. Treatment of symptomatic diabetic peripheral neuropathy with the protein kinase C beta-inhibitor ruboxistaurin mesylate during a 1-year, randomized, placebo-controlled, double-blind clinical trial. Clin Ther. 2005;27(8):1164–1180. doi: 10.1016/j.clinthera.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 74.Bansal D, Badhan Y, Gudala K, Schifano F. Ruboxistaurin for the treatment of diabetic peripheral neuropathy: a systematic review of randomized clinical trials. Diabetes Metab J. 2013;37(5):375–384. doi: 10.4093/dmj.2013.37.5.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sima AA. New insights into the metabolic and molecular basis for diabetic neuropathy. Cell Mol Life Sci. 2003;60(11):2445–2464. doi: 10.1007/s00018-003-3084-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wahren J, Ekberg K, Jornvall H. C-peptide is a bioactive peptide. Diabetologia. 2007;50(3):503–509. doi: 10.1007/s00125-006-0559-y. [DOI] [PubMed] [Google Scholar]
- 77.Sun JK, Keenan HA, Cavallerano JD, Asztalos BF, Schaefer EJ, Sell DR, Strauch CM, Monnier VM, Doria A, Aiello LP, King GL. Protection from retinopathy and other complications in patients with type 1 diabetes of extreme duration: The Joslin 50-Year Medalist Study. Diabetes Care. 2011;34(4):968–974. doi: 10.2337/dc10-1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ekberg K, Brismar T, Johansson BL, Jonsson B, Lindstrom P, Wahren J. Amelioration of sensory nerve dysfunction by C-peptide in patients with type 1 diabetes. Diabetes. 2003;52(2):536–541. doi: 10.2337/diabetes.52.2.536. [DOI] [PubMed] [Google Scholar]
- 79.Ekberg K, Brismar T, Johansson BL, Lindstrom P, Juntti-Berggren L, Norrby A, Berne C, Arnqvist HJ, Bolinder J, Wahren J. C-peptide replacement therapy and sensory nerve function in type 1 diabetic neuropathy. Diabetes Care. 2007;30(1):71–76. doi: 10.2337/dc06-1274. [DOI] [PubMed] [Google Scholar]
- 80.Ziegler D, Movsesyan L, Mankovsky B, Gurieva I, Abylaiuly Z, Strokov I. Treatment of symptomatic polyneuropathy with actovegin in type 2 diabetic patients. Diabetes Care. 2009;32(8):1479–1484. doi: 10.2337/dc09-0545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Azmi S, Ferdousi M, Petropoulos IN, Ponirakis G, Fadavi H, Tavakoli M, Alam U, Jones W, Marshall A, Jeziorska M. et al. Corneal confocal microscopy shows an improvement in small-fiber neuropathy in subjects with type 1 diabetes on continuous subcutaneous insulin infusion compared with multiple daily injection. Diabetes Care. 2015;38(1):E3–E4. doi: 10.2337/dc14-1698. [DOI] [PubMed] [Google Scholar]
- 82.Wiggin TD, Sullivan KA, Pop-Busui R, Amato A, Sima AA, Feldman EL. Elevated triglycerides correlate with progression of diabetic neuropathy. Diabetes. 2009;58(7):1634–1640. doi: 10.2337/db08-1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fried LF, Forrest KY, Ellis D, Chang Y, Silvers N, Orchard TJ. Lipid modulation in insulin-dependent diabetes mellitus: effect on microvascular outcomes. J Diabetes Complications. 2001;15(3):113–119. doi: 10.1016/s1056-8727(01)00140-4. [DOI] [PubMed] [Google Scholar]
- 84.Smith AG, Russell J, Feldman EL, Goldstein J, Peltier A, Smith S, Hamwi J, Pollari D, Bixby B, Howard J, Singleton JR. Lifestyle intervention for pre-diabetic neuropathy. Diabetes Care. 2006;29(6):1294–1299. doi: 10.2337/dc06-0224. [DOI] [PubMed] [Google Scholar]
- 85.Hernandez-Ojeda J, Roman-Pintos LM, Rodriguez-Carrizalez AD, Troyo-Sanroman R, Cardona-Munoz EG, Alatorre-Carranza MD, Miranda-Diaz AG. Effect of rosuvastatin on diabetic polyneuropathy: a randomized, double-blind, placebo-controlled Phase IIa study. Diabetes Metab Syndr Obes. 2014;7:401–407. doi: 10.2147/DMSO.S65500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rajamani K, Colman PG, Li LP, Best JD, Voysey M, D'Emden MC, Laakso M, Baker JR, Keech AC FIELD study investigators. Effect of fenofibrate on amputation events in people with type 2 diabetes mellitus (FIELD study): a prespecified analysis of a randomised controlled trial. Lancet. 2009;373(9677):1780–1788. doi: 10.1016/S0140-6736(09)60698-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 88.Gore M, Dukes E, Rowbotham DJ, Tai KS, Leslie D. Clinical characteristics and pain management among patients with painful peripheral neuropathic disorders in general practice settings. Eur J Pain. 2007;11(6):652–664. doi: 10.1016/j.ejpain.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 89.Chong MS, Hester J. Diabetic painful neuropathy: current and future treatment options. Drugs. 2007;67(4):569–585. doi: 10.2165/00003495-200767040-00006. [DOI] [PubMed] [Google Scholar]
- 90.Rudroju N, Bansal D, Talakokkula ST, Gudala K, Hota D, Bhansali A, Ghai B. Comparative efficacy and safety of six antidepressants and anticonvulsants in painful diabetic neuropathy: a network meta-analysis. Pain Physician. 2013;16(6):E705–E714. [PubMed] [Google Scholar]
- 91.Max MB, Kishore-Kumar R, Schafer SC, Meister B, Gracely RH, Smoller B, Dubner R. Efficacy of desipramine in painful diabetic neuropathy: a placebo-controlled trial. Pain. 1991;45(1):3–9. doi: 10.1016/0304-3959(91)90157-S. [DOI] [PubMed] [Google Scholar]
- 92.Max MB, Lynch SA, Muir J, Shoaf SE, Smoller B, Dubner R. Effects of desipramine, amitriptyline, and fluoxetine on pain in diabetic neuropathy. N Engl J Med. 1992;326(19):1250–1256. doi: 10.1056/NEJM199205073261904. [DOI] [PubMed] [Google Scholar]
- 93.Sindrup SH, Gram LF, Skjold T, Grodum E, Brøsen K, Beck-Nielsen H. Clomipramine vs desipramine vs placebo in the treatment of diabetic neuropathy symptoms. A double-blind cross-over study. Br J Clin Pharmacol. 1990;30(5):683–691. doi: 10.1111/j.1365-2125.1990.tb03836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kvinesdal B, Molin J, Froland A, Gram LF. Imipramine treatment of painful diabetic neuropathy. JAMA. 1984;251(13):1727–1730. [PubMed] [Google Scholar]
- 95.Marks DM, Shah MJ, Patkar AA, Masand PS, Park GY, Pae CU. Serotonin-norepinephrine reuptake inhibitors for pain control: premise and promise. Curr Neuropharmacol. 2009;7(4):331–336. doi: 10.2174/157015909790031201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wernicke JF, Wang F, Pritchett YL, Smith TR, Raskin J, D'Souza DN, Iyengar S, Chappell AS. An open-label 52-week clinical extension comparing duloxetine with routine care in patients with diabetic peripheral neuropathic pain. Pain Med. 2007;8(6):503–513. doi: 10.1111/j.1526-4637.2006.00258.x. [DOI] [PubMed] [Google Scholar]
- 97.Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005;116(1-2):109–118. doi: 10.1016/j.pain.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 98.Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev. 2014;1:CD007115. doi: 10.1002/14651858.CD007115.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rowbotham MC, Goli V, Kunz NR, Lei D. Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. Pain. 2004;110(3):697–706. doi: 10.1016/j.pain.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 100.Griebeler ML, Morey-Vargas OL, Brito JP, Tsapas A, Wang Z, Carranza Leon BG, Phung OJ, Montori VM, Murad MH. Pharmacologic interventions for painful diabetic neuropathy: an umbrella systematic review and comparative effectiveness network meta-analysis. Ann Intern Med. 2014;161(9):639–649. doi: 10.7326/M14-0511. [DOI] [PubMed] [Google Scholar]
- 101.Snedecor SJ, Sudharshan L, Cappelleri JC, Sadosky A, Mehta S, Botteman M. Systematic review and meta-analysis of pharmacological therapies for painful diabetic peripheral neuropathy. Pain Pract. 2014;14(2):167–184. doi: 10.1111/papr.12054. [DOI] [PubMed] [Google Scholar]
- 102.Rull JA, Quibrera R, Gonzalez-Millan H, Lozano Castaneda O. Symptomatic treatment of peripheral diabetic neuropathy with carbamazepine (Tegretol): double blind crossover trial. Diabetologia. 1969;5(4):215–218. doi: 10.1007/BF01212087. [DOI] [PubMed] [Google Scholar]
- 103.Wilton TD. Tegretol in the treatment of diabetic neuropathy. S Afr Med J. 1974;48(20):869–872. [PubMed] [Google Scholar]
- 104.Dogra S, Beydoun S, Mazzola J, Hopwood M, Wan Y. Oxcarbazepine in painful diabetic neuropathy: a randomized, placebo-controlled study. Eur J Pain. 2005;9(5):543–554. doi: 10.1016/j.ejpain.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 105.Beydoun A, Shaibani A, Hopwood M, Wan Y. Oxcarbazepine in painful diabetic neuropathy: results of a dose-ranging study. Acta Neurol Scand. 2006;113(6):395–404. doi: 10.1111/j.1600-0404.2006.00631.x. [DOI] [PubMed] [Google Scholar]
- 106.Grosskopf J, Mazzola J, Wan Y, Hopwood M. A randomized, placebo-controlled study of oxcarbazepine in painful diabetic neuropathy. Acta Neurol Scand. 2006;114(3):177–180. doi: 10.1111/j.1600-0404.2005.00559.x. [DOI] [PubMed] [Google Scholar]
- 107.Rose MA, Kam PC. Gabapentin: pharmacology and its use in pain management. Anaesthesia. 2002;57(5):451–462. doi: 10.1046/j.0003-2409.2001.02399.x. [DOI] [PubMed] [Google Scholar]
- 108.Backonja M, Beydoun A, Edwards KR, Schwartz SL, Fonseca V, Hes M, LaMoreaux L, Garofalo E. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA. 1998;280(21):1831–1836. doi: 10.1001/jama.280.21.1831. [DOI] [PubMed] [Google Scholar]
- 109.Mellegers MA, Furlan AD, Mailis A. Gabapentin for neuropathic pain: systematic review of controlled and uncontrolled literature. Clin J Pain. 2001;17(4):284–295. doi: 10.1097/00002508-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 110.Moore RA, Wiffen PJ, Derry S, Toelle T, Rice AS. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2014;4:CD007938. doi: 10.1002/14651858.CD007938.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lesser H, Sharma U, LaMoreaux L, Poole RM. Pregabalin relieves symptoms of painful diabetic neuropathy: a randomized controlled trial. Neurology. 2004;63(11):2104–2110. doi: 10.1212/01.wnl.0000145767.36287.a1. [DOI] [PubMed] [Google Scholar]
- 112.Arezzo JC, Rosenstock J, Lamoreaux L, Pauer L. Efficacy and safety of pregabalin 600 mg/d for treating painful diabetic peripheral neuropathy: a double-blind placebo-controlled trial. BMC Neurol. 2008;8:33. doi: 10.1186/1471-2377-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Richter RW, Portenoy R, Sharma U, Lamoreaux L, Bockbrader H, Knapp LE. Relief of painful diabetic peripheral neuropathy with pregabalin: a randomized, placebo-controlled trial. J Pain. 2005;6(4):253–260. doi: 10.1016/j.jpain.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 114.Rosenstock J, Tuchman M, LaMoreaux L, Sharma U. Pregabalin for the treatment of painful diabetic peripheral neuropathy: a double-blind, placebo-controlled trial. Pain. 2004;110(3):628–638. doi: 10.1016/j.pain.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 115.Sicras A, Rejas J, Navarro R, Planas A. Adding pregabalin or gabapentin for the management of community-treated patients with painful diabetic peripheral neuropathy: a comparative cost analysis. Clin Drug Investig. 2013;33(11):825–835. doi: 10.1007/s40261-013-0131-8. [DOI] [PubMed] [Google Scholar]
- 116.Raskin P, Donofrio PD, Rosenthal NR, Hewitt DJ, Jordan DM, Xiang J, Vinik AI CAPSS-141 Study Group. Topiramate vs placebo in painful diabetic neuropathy: analgesic and metabolic effects. Neurology. 2004;63(5):865–873. doi: 10.1212/01.wnl.0000137341.89781.14. [DOI] [PubMed] [Google Scholar]
- 117.Donofrio PD, Raskin P, Rosenthal NR, Hewitt DJ, Jordan DM, Xiang J, Vinik AI CAPSS-141 Study Group. Safety and effectiveness of topiramate for the management of painful diabetic peripheral neuropathy in an open-label extension study. Clin Ther. 2005;27(9):1420–1431. doi: 10.1016/j.clinthera.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 118.Thienel U, Neto W, Schwabe SK, Vijapurkar U Topiramate Diabetic Neuropathic Pain Study Group. Topiramate in painful diabetic polyneuropathy: findings from three double-blind placebo-controlled trials. Acta Neurol Scand. 2004;110(4):221–231. doi: 10.1111/j.1600-0404.2004.00338.x. [DOI] [PubMed] [Google Scholar]
- 119.Eisenberg E, Lurie Y, Braker C, Daoud D, Ishay A. Lamotrigine reduces painful diabetic neuropathy: a randomized, controlled study. Neurology. 2001;57(3):505–509. doi: 10.1212/wnl.57.3.505. [DOI] [PubMed] [Google Scholar]
- 120.Vinik AI, Tuchman M, Safirstein B, Corder C, Kirby L, Wilks K, Quessy S, Blum D, Grainger J, White J, Silver M. Lamotrigine for treatment of pain associated with diabetic neuropathy: results of two randomized, double-blind, placebo-controlled studies. Pain. 2007;128(1-2):169–179. doi: 10.1016/j.pain.2006.09.040. [DOI] [PubMed] [Google Scholar]
- 121.Wiffen PJ, Derry S, Moore RA. Lamotrigine for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2013;12:CD006044. doi: 10.1002/14651858.CD006044.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Harati Y, Gooch C, Swenson M, Edelman S, Greene D, Raskin P, Donofrio P, Cornblath D, Sachdeo R, Siu CO, Kamin M. Double-blind randomized trial of tramadol for the treatment of the pain of diabetic neuropathy. Neurology. 1998;50(6):1842–1846. doi: 10.1212/wnl.50.6.1842. [DOI] [PubMed] [Google Scholar]
- 123.Schwartz S, Etropolski M, Shapiro DY, Okamoto A, Lange R, Haeussler J, Rauschkolb C. Safety and efficacy of tapentadol ER in patients with painful diabetic peripheral neuropathy: results of a randomized-withdrawal, placebo-controlled trial. Curr Med Res Opin. 2011;27(1):151–162. doi: 10.1185/03007995.2010.537589. [DOI] [PubMed] [Google Scholar]
- 124.Christoph T, Schröder W, Tallarida RJ, De Vry J, Tzschentke TM. Spinal-supraspinal and intrinsic μ-opioid receptor agonist-norepinephrine reuptake inhibitor (MOR-NRI) synergy of tapentadol in diabetic heat hyperalgesia in mice. J Pharmacol Exp Ther. 2013;347(3):794–801. doi: 10.1124/jpet.113.207704. [DOI] [PubMed] [Google Scholar]
- 125.Gimbel JS, Richards P, Portenoy RK. Controlled-release oxycodone for pain in diabetic neuropathy: a randomized controlled trial. Neurology. 2003;60(6):927–934. doi: 10.1212/01.wnl.0000057720.36503.2c. [DOI] [PubMed] [Google Scholar]
- 126.Watson CP, Moulin D, Watt-Watson J, Gordon A, Eisenhoffer J. Controlled-release oxycodone relieves neuropathic pain: a randomized controlled trial in painful diabetic neuropathy. Pain. 2003;105(1-2):71–78. doi: 10.1016/s0304-3959(03)00160-x. [DOI] [PubMed] [Google Scholar]
- 127.Kosten TR, George TP. The neurobiology of opioid dependence: implications for treatment. Sci Pract Perspect. 2002;1(1):13–20. doi: 10.1151/spp021113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Manubay JM, Muchow C, Sullivan MA. Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics. Prim Care. 2011;38(1):71–90. doi: 10.1016/j.pop.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhang WY, Li Wan Po A. The effectiveness of topically applied capsaicin. A meta-analysis. Eur J Clin Pharmacol. 1994;46(6):517–522. doi: 10.1007/BF00196108. [DOI] [PubMed] [Google Scholar]
- 130.Treatment of painful diabetic neuropathy with topical capsaicin. A multicenter, double-blind, vehicle-controlled study. The Capsaicin Study Group. Arch Intern Med. 1991;151(11):2225–2229. doi: 10.1001/archinte.151.11.2225. [DOI] [PubMed] [Google Scholar]
- 131.Polydefkis M, Hauer P, Sheth S, Sirdofsky M, Griffin JW, McArthur JC. The time course of epidermal nerve fibre regeneration: studies in normal controls and in people with diabetes, with and without neuropathy. Brain. 2004;127(Pt 7):1606–1615. doi: 10.1093/brain/awh175. [DOI] [PubMed] [Google Scholar]
- 132.Campbell CM, Kipnes MS, Stouch BC, Brady KL, Kelly M, Schmidt WK, Petersen KL, Rowbotham MC, Campbell JN. Randomized control trial of topical clonidine for treatment of painful diabetic neuropathy. Pain. 2012;153(9):1815–1823. doi: 10.1016/j.pain.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Yuen KC, Baker NR, Rayman G. Treatment of chronic painful diabetic neuropathy with isosorbide dinitrate spray: a double-blind placebo-controlled cross-over study. Diabetes Care. 2002;25(10):1699–1703. doi: 10.2337/diacare.25.10.1699. [DOI] [PubMed] [Google Scholar]
- 134.Barbano RL, Herrmann DN, Hart-Gouleau S, Pennella-Vaughan J, Lodewick PA, Dworkin RH. Effectiveness, tolerability, and impact on quality of life of the 5% lidocaine patch in diabetic polyneuropathy. Arch Neurol. 2004;61(6):914–918. doi: 10.1001/archneur.61.6.914. [DOI] [PubMed] [Google Scholar]
- 135.Yuan RY, Sheu JJ, Yu JM, Chen WT, Tseng IJ, Chang HH, Hu CJ. Botulinum toxin for diabetic neuropathic pain: a randomized double-blind crossover trial. Neurology. 2009;72(17):1473–1478. doi: 10.1212/01.wnl.0000345968.05959.cf. [DOI] [PubMed] [Google Scholar]
- 136.Lakhan SE, Velasco DN, Tepper D. Botulinum toxin-A for painful diabetic neuropathy: a meta-analysis. Pain Med. 2015;16(9):1773–1780. doi: 10.1111/pme.12728. [DOI] [PubMed] [Google Scholar]
- 137.Thakral G, Kim PJ, LaFontaine J, Menzies R, Najafi B, Lavery LA. Electrical stimulation as an adjunctive treatment of painful and sensory diabetic neuropathy. J Diabetes Sci Technol. 2013;7(5):1202–1209. doi: 10.1177/193229681300700510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Garrow AP, Xing M, Vere J, Verrall B, Wang L, Jude EB. Role of acupuncture in the management of diabetic painful neuropathy (DPN): a pilot RCT. Acupunct Med. 2014;32(3):242–249. doi: 10.1136/acupmed-2013-010495. [DOI] [PubMed] [Google Scholar]
- 139.Chen W, Yang GY, Liu B, Manheimer E, Liu JP. Manual acupuncture for treatment of diabetic peripheral neuropathy: a systematic review of randomized controlled trials. Plos One. 2013;8(9):e73764. doi: 10.1371/journal.pone.0073764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Singleton JR, Marcus RL, Jackson JE, K Lessard M, Graham TE, Smith AG. Exercise increases cutaneous nerve density in diabetic patients without neuropathy. Ann Clin Transl Neurol. 2014;1(10):844–849. doi: 10.1002/acn3.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Singleton JR, Marcus RL, Lessard MK, Jackson JE, Smith AG. Supervised exercise improves cutaneous reinnervation capacity in metabolic syndrome patients. Ann Neurol. 2015;77(1):146–153. doi: 10.1002/ana.24310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gilron I, Bailey JM, Tu D, Holden RR, Jackson AC, Houlden RL. Nortriptyline and gabapentin, alone and in combination for neuropathic pain: a double-blind, randomised controlled crossover trial. Lancet. 2009;374(9697):1252–1261. doi: 10.1016/S0140-6736(09)61081-3. [DOI] [PubMed] [Google Scholar]
- 143.Gilron I, Bailey JM, Tu D, Holden RR, Weaver DF, Houlden RL. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med. 2005;352(13):1324–1334. doi: 10.1056/NEJMoa042580. [DOI] [PubMed] [Google Scholar]
- 144.Bansal D, Bhansali A, Hota D, Chakrabarti A, Dutta P. Amitriptyline vs. pregabalin in painful diabetic neuropathy: a randomized double blind clinical trial. Diabet Med. 2009;26(10):1019–1026. doi: 10.1111/j.1464-5491.2009.02806.x. [DOI] [PubMed] [Google Scholar]
- 145.Tesfaye S, Wilhelm S, Lledo A, Schacht A, Tölle T, Bouhassira D, Cruccu G, Skljarevski V, Freynhagen R. Duloxetine and pregabalin: high-dose monotherapy or their combination? The "COMBO-DN study" - a multinational, randomized, double-blind, parallel-group study in patients with diabetic peripheral neuropathic pain. Pain. 2013;154(12):2616–2625. doi: 10.1016/j.pain.2013.05.043. [DOI] [PubMed] [Google Scholar]
- 146.Vincent AM, Callaghan BC, Smith AL, Feldman EL. Diabetic neuropathy: cellular mechanisms as therapeutic targets. Nat Rev Neurol. 2011;7(10):573–583. doi: 10.1038/nrneurol.2011.137. [DOI] [PubMed] [Google Scholar]
- 147.Brederson JD, Kym PR, Szallasi A. Targeting TRP channels for pain relief. Eur J Pharmacol. 2013;716(1-3):61–76. doi: 10.1016/j.ejphar.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 148.Verheyen A, Peeraer E, Lambrechts D, Poesen K, Carmeliet P, Shibuya M, Pintelon I, Timmermans JP, Nuydens R, Meert T. Therapeutic potential of VEGF and VEGF-derived peptide in peripheral neuropathies. Neuroscience. 2013;244:77–89. doi: 10.1016/j.neuroscience.2013.03.050. [DOI] [PubMed] [Google Scholar]
- 149.Ropper AH, Gorson KC, Gooch CL, Weinberg DH, Pieczek A, Ware JH, Kershen J, Rogers A, Simovic D, Schratzberger P. et al. Vascular endothelial growth factor gene transfer for diabetic polyneuropathy: a randomized, double-blinded trial. Ann Neurol. 2009;65(4):386–393. doi: 10.1002/ana.21675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rice AS, Dworkin RH, McCarthy TD, Anand P, Bountra C, McCloud PI, Hill J, Cutter G, Kitson G, Desem N. et al. EMA401, an orally administered highly selective angiotensin II type 2 receptor antagonist, as a novel treatment for postherpetic neuralgia: a randomised, double-blind, placebo-controlled phase 2 clinical trial. Lancet. 2014;383(9929):1637–1647. doi: 10.1016/S0140-6736(13)62337-5. [DOI] [PubMed] [Google Scholar]
- 151.Deer TR, Smith HS, Cousins M, Doleys DM, Levy RM, Rathmell JP, Staats PS, Wallace M, Webster LR. Consensus guidelines for the selection and implantation of patients with noncancer pain for intrathecal drug delivery. Pain Physician. 2010;13(3):E175–E213. [PubMed] [Google Scholar]
- 152.Brines M, Dunne AN, Van Velzen M, Proto PL, Ostenson CG, Kirk RI, Petropoulos I, Javed S, Malik RA, Cerami A, Dahan A. ARA 290, a non-erythropoietic peptide engineered from erythropoietin, improves metabolic control and neuropathic symptoms in patients with type 2 diabetes. Mol Med. 2015;20:658–666. doi: 10.2119/molmed.2014.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Tavakoli M, Begum P, McLaughlin J, Malik RA. Corneal confocal microscopy for the diagnosis of diabetic autonomic neuropathy. Muscle Nerve. 2015;52(3):363–370. doi: 10.1002/mus.24553. [DOI] [PubMed] [Google Scholar]
- 154.The effect of intensive diabetes therapy on the development and progression of neuropathy. The Diabetes Control and Complications Trial Research Group. Ann Intern Med. 1995;122(8):561–568. doi: 10.7326/0003-4819-122-8-199504150-00001. [DOI] [PubMed] [Google Scholar]
- 155.Gaede P, Vedel P, Parving HH, Pedersen O. Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the Steno type 2 randomised study. Lancet. 1999;353(9153):617–622. doi: 10.1016/S0140-6736(98)07368-1. [DOI] [PubMed] [Google Scholar]
- 156.Hu X, Li S, Yang G, Liu H, Boden G, Li L. Efficacy and safety of aldose reductase inhibitor for the treatment of diabetic cardiovascular autonomic neuropathy: systematic review and meta-analysis. Plos One. 2014;9(2):e87096. doi: 10.1371/journal.pone.0087096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gatopoulou A, Papanas N, Maltezos E. Diabetic gastrointestinal autonomic neuropathy: current status and new achievements for everyday clinical practice. Eur J Intern Med. 2012;23(6):499–505. doi: 10.1016/j.ejim.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 158.Promberger R, Lenglinger J, Riedl O, Seebacher G, Eilenberg W, Ott J, Riegler F, Gadenstätter M, Neumayer C. Gastro-oesophageal reflux disease in type 2 diabetics: symptom load and pathophysiologic aspects - a retro-pro study. BMC Gastroenterol. 2013;13:132. doi: 10.1186/1471-230X-13-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Ma J, Rayner CK, Jones KL, Horowitz M. Diabetic gastroparesis: diagnosis and management. Drugs. 2009;69(8):971–986. doi: 10.2165/00003495-200969080-00003. [DOI] [PubMed] [Google Scholar]
- 160.Gould M, Sellin JH. Diabetic diarrhea. Curr Gastroenterol Rep. 2009;11(5):354–359. doi: 10.1007/s11894-009-0054-y. [DOI] [PubMed] [Google Scholar]
- 161.McCulloch DK, Campbell IW, Wu FC, Prescott RJ, Clarke BF. The prevalence of diabetic impotence. Diabetologia. 1980;18(4):279–283. doi: 10.1007/BF00251005. [DOI] [PubMed] [Google Scholar]
- 162.Phe V, Roupret M. Erectile dysfunction and diabetes: a review of the current evidence-based medicine and a synthesis of the main available therapies. Diabetes Metab. 2012;38(1):1–13. doi: 10.1016/j.diabet.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 163.Rendell MS, Rajfer J, Wicker PA, Smith MD. Sildenafil for treatment of erectile dysfunction in men with diabetes: a randomized controlled trial. Sildenafil Diabetes Study Group. JAMA. 1999;281(5):421–426. doi: 10.1001/jama.281.5.421. [DOI] [PubMed] [Google Scholar]
- 164.Basu A, Ryder RE. New treatment options for erectile dysfunction in patients with diabetes mellitus. Drugs. 2004;64(23):2667–2688. doi: 10.2165/00003495-200464230-00004. [DOI] [PubMed] [Google Scholar]
- 165.Golbidi S, Laher I. Bladder dysfunction in diabetes mellitus. Front Pharmacol. 2010;1:136. doi: 10.3389/fphar.2010.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chapple CR, Khullar V, Gabriel Z, Muston D, Bitoun CE, Weinstein D. The effects of antimuscarinic treatments in overactive bladder: an update of a systematic review and meta-analysis. Eur Urol. 2008;54(3):543–562. doi: 10.1016/j.eururo.2008.06.047. [DOI] [PubMed] [Google Scholar]



