Abstract
Introduction:
One of the problems that the delivery of continuous positive airway pressure (CPAP) via a helmet poses is the generation of noise. The objective of our study was to assess the effect that the use of filter has on sound pressure levels generated by the delivery of positive airway pressure at different gas flow rates.
Materials and Methods:
Sound pressure levels generated by neonatal helmet CPAP delivery were measured at different gas flows (20, 30, and 40 l/min) with and without a breathing filter. Noise intensity was measured by installing microphones in the inner ear of dummy heads wearing helmets.
Results:
The sound pressure level increased by 38% at a gas flow of 40 l/min, as compared to a gas flow of 20 l/min {74 dBA [interquartile range (IQR) 2,2] vs 52 dBA (IQR 5,9), respectively}. Using the breathing filter as a diffuser has a variety of effects on sound pressure levels according to the gas flow rate.
Conclusion:
The intensity of the noise generated by helmet delivery of positive airway pressure depends on the type of helmet used, gas flow, and use or not of a diffuser filter. Breathing filters with gas flows over 30 l/min might not be recommended since they would not attenuate but will rather amplify sound pressure.
Keywords: Continuous positive airway pressure, filter, helmet, neonatal intensive care units, noise exposure
Introduction
One of the factors that have contributed to the increase of survival rates in very-low weight neonates is the improvement of mechanical ventilation systems.[1] The use of noninvasive ventilation systems − which include, among others, the administration of continuous positive airway pressure via nasal interface (nCPAP) − has been associated with lower reintubation rates and a lower incidence of bronchopulmonary dysplasia, as compared to invasive mechanical ventilation. The drawbacks of using nasal continuous positive airway pressure (CPAP) interfaces in neonates have been overcome with the use of cephalic interfaces (helmet).[2,3] However, tolerability improves, CPAP interruptions decrease, and skin lesions and air leaks through the mouth are prevented with helmet CPAP interfaces.
One of the problems associated with the use of nasal CPAP interfaces is the noise generated by this type of ventilation systems.[4,5] There is evidence that sound pressure levels are higher for helmets, as compared to facial masks[6] or prongs.[7]
Conversely, neonatal exposure to high sound pressure levels has been proven to have a negative impact in the short- and the long-term (cardiovascular, respiratory, and neurological alterations).[8,9,10,11] Therefore, the American Academy of Pediatrics has established that sound pressure levels in neonatal intensive care units (NICUs) should not exceed 45 dBA.[12] Yet, a mean exposure of 49 ± 1.4 dB(A) has been reported.[13]
A variety of measures have been proposed to reduce the negative impact that noise exposure has on NICU patients.[14] It has been demonstrated that when noise reduction measures are implemented, very-low weight neonates improve their weight gain.[8] It has been suggested that their neurological development might improve too.[15]
One of the aspects to consider when using a helmet is CO2 rebreathing. To overcome this complication, using different gas flow rates has been proposed.[16]
Our aim was to assess the effect that different gas flow rates and the use of a filter have on the sound pressure levels to which neonates are exposed when receiving ventilation support via two different helmet CPAP systems.
Materials and Methods
Two neonatal helmet CPAP delivery systems were compared: Starmed Castar (Mirandola, Italy) and Dimar (Mirandola, Italy). To measure sound pressure levels, the two helmet CPAP device models were sequentially placed in a dummy head (Types 4100 de Brüel & Kjær). Sound pressure levels were measured using a sound calibrator (Model 4231 de Brüel) to check the measuring chain at the beginning and at the end of each measurement, a pulse analyzer model 3560C (“Brüel & Kjær”) with microphones installed in the inner ears of the dummy, and another microphone to measure background noise. A VelociCalc plus (TSI) was used to measure background noise.[17] This way, loud external noises such as alarms or other common noises at a NICU were excluded from analysis. The dummy head with the helmet was placed in the center of a switched-off incubator with the doors closed (Caleo, Drager Medical AG & Co., Moislinger Allee, Lubek, Germany). Non-humidified cold air was used to avoid the additional noise generated by condensation drops in the tubing system.
Following pretest, the equipment was set at a dynamic range of 0–140 dB and a bandwidth of 20 Hz–20 kHz for A-weighting and “linear” frequency weighting. Since the human ear does not perceive all frequencies equally and it is much more sensitive to frequencies within the 1–4 kHz range, and high-frequency sounds are prevalent at NICUs (monitor alarms),[18] sound pressure levels were measured in third-octave bands.
Sound pressure levels were measured in one-third octave bands using A-weighting, which splits the spectrum of frequencies into narrow bands that are differently weighted according to the sensitivity of the human ear to the particular frequency. In an A-weighted scale, the low frequencies were attenuated, just as in the human auditory system.
Sound measurements were taken at different gas flow rates: 20, 30, and 40 l/min (Clear Therm-Micro modelo 1441, Tyco, Mirandola, Italy) with and without a heat moisture exchange (HMEF) placed at the junction of the inspiratory branch of the respiratory circuit with the helmet. The flow generator used was a Dräger CF800 O2/Air Mixer (Malmesbury, Wiltshire, UK) device. All experimental series were repeated five times. During the study, sound pressure levels remained constant within the helmet in all conditions at 5 cm H2O. The level of CPAP was maintained at 5 cm H2O by an exhalation valve system (SPV 20 Starmed Spa, Mirandola, Modena, Italy). Room conditions were as follows: mean room temperature: 22.1 ± 1°C, and relative humidity was concentrated within the 52.9 ± 5% range.
The study was approved by the Ethical Committee of our institution (Hospital Puerta del Mar Investigation Subcommittee) following international ethic recommendations (Helsinki Declaration) and based on current Spanish legislation (Oviedo Apostille Convention).
Data were expressed as medians [interquartile range (IQR)]. As normal distribution was not appropriate in our samples, sound pressure levels at different gas flow rates in the two groups were compared using the non-parametrical test Kruskal–Wallis and the Wilcoxon test with Bonferroni correction. Matched samples were compared using the Wilcoxon test.
Results
A total of 4968 sound level measurements − with a duration of 5 s each − were obtained, 216 of which were background sounds.
Figure 1 displays sound pressure levels registered at flow rates of 20, 30, and 40 l/min without filter for StarMed helmet. Sound pressure levels were 38% higher at a gas flow of 40 l/min, as compared to a gas flow of 20 l/min [52 dBA (IQR 5,9) vs 74 dBA (IQR 2,2), respectively]. These results were similar when we tested the Dimar helmet.
Figure 1.
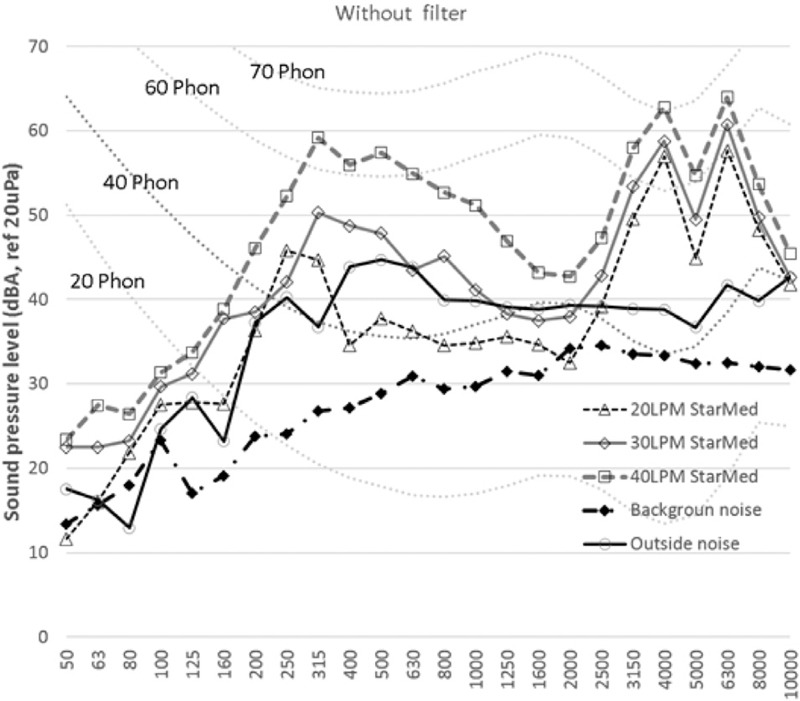
Sound pressure levels. The levels are registered at flow rates of 20, 30, and 40 l/min without filter STARMED helmet
The diffuser filter was found to attenuate sound pressure at a gas flow rate of 20 l/min in both helmet models. However, when the flow rate was set at 40 l/min, the diffuser filter increased sound pressure levels rather than attenuating it. When the flow rate was set at an intermediate value of 30 l/min, opposite results were obtained. Thus, the filter amplified noise in the ear closest to the air entry, while it attenuated noise in the opposite ear [Figure 2].
Figure 2.
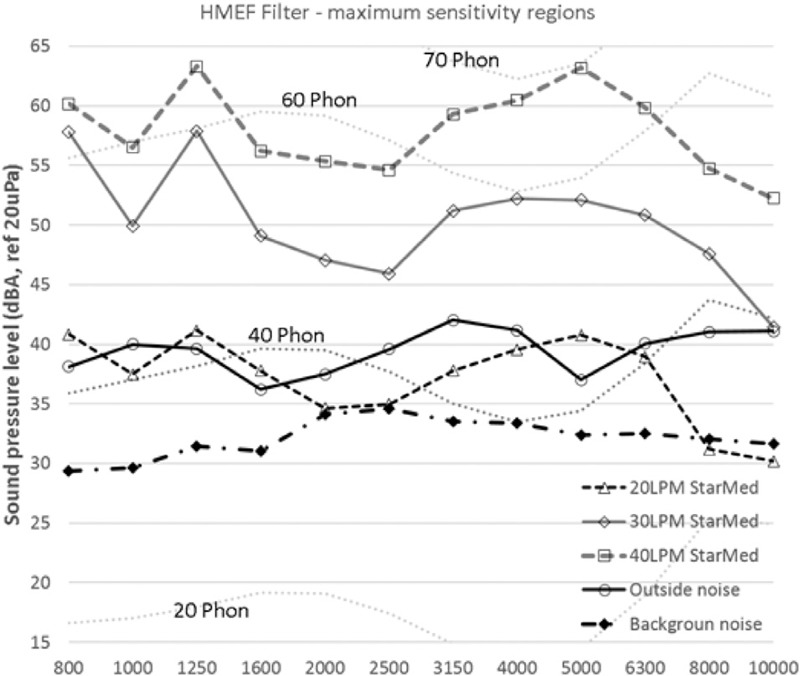
Sound pressure levels. The levels are registered at flow rates of 20, 30, and 40 l/min with filter STARMED helmet
Regardless of the gas flow rate, the noise generated by the neonatal helmet CPAP devices and HMEF filters exceeded 45 dB.
At 30 and 40 l/min flow rates, sound levels exceeded the 40 phons isophonic curve in most of the spectrum.
Discussion
Our results show that using the breathing filter as a diffuser has a variety of effects on sound pressure levels according to the gas flow rate. While they attenuate sound pressure, the noise, with gas flow rate of 20 l/min, when used with gas flow rates over 30 l/min, has shown an amplification effect.
At 24–28 weeks of gestation, the auditory system is developed enough to perceive sounds that change the neonatal heart rate. In preterm infants, the protection provided by the amniotic fluid against noise disappears.[19] Overexposure to noise may have deleterious effects on the neurological development of the neonate;[11] therefore, unnecessary neonatal exposure to noise should be avoided at NICUs.
Sound pressure levels are high at NICUs,[20] and the noise generated by ventilation devices used by many neonates contributes to such high levels. According to Karam et al., the use of different CPAP devices with different types of prongs in preterm infants generates sound levels of >45 dBA. In addition, the sound levels generated by the different nCPAP devices are not generally related to the device model or the pressure produced.[4] Studies comparing sound pressure levels generated by different nCPAP interfaces concluded that helmets generated higher sound levels, as compared to face masks[6] or prongs.[7] The results obtained in our study show that the sound pressure levels generated by the DimAir and the StarMed helmet model at 20 l/min without a diffuser were 65.13 ± 1.15 and 61.40 ± 1.40 dBA, respectively. These sound pressure levels are significantly lower than those reported by other authors, ranging between 81 (77–94)[21] and 94.4 ± 1.6 dBA.[6] Differences might be explained by the helmet design used in each study.
A concern associated with the use of helmets as a CPAP interface is the increase of CO2 inspired during rebreathing, although this possibility decreases when the gas flow increases.[22] To avoid rebreathing, flows of 40,[2,16] >30,[23] or 25 l/min[21] have been recommended, although some authors consider that a flow of 8–10 l/min is enough for neonates.[3]
It is known that the noise generated by high flow nasal cannula (HFNC)[24] and nCPAP[4] rises with the increase of the gas flow. This direct relationship between gas flow rate and sound pressure level has also been observed for helmets.[6] The results obtained in our study also demonstrate that there is a relationship between sound pressure levels and gas flow rate. Thus, when the gas flow was raised from 20 to 40 l/min, sound pressure levels increased from 52 to 74 dBA. Other studies have also observed this relationship, reporting that when sound pressure levels were increased from 8 to 12 l/min, sound levels rose from 70 dBA (IQR 69.9–70.4) to 73.5 dBA (IQR 73.3–73.8).[7] These sound pressure levels are slightly higher than those registered in our study, even though we used lower flow rates. This might be due to the use of different helmet models − which have a different volume and are made of different materials − and to the use of a dummy head instead of a real human head.
Contradictory results have been obtained on the efficacy of using a filter to reduce the noise generated by the use of helmets. On the one hand, Trevisanuto et al. [7] observed that the use of HMEF placed between the inspiratory circuit and the helmet reduced the intensity of the noise generated at different gas flow rates. On the other hand, other authors[25] have not found any relationship between the use of HMEF and sound pressure levels; nevertheless, it is worthy of note that the gas flow was administered through a mask instead of a high flow device, and the microphone was placed in the ear closest to the air entry of the helmet. Regarding our study, we found that the effect of filters placed at the junction of the inspiratory branch with the helmet on sound pressure levels depends on the gas flow rate. The diffuser filter was observed to attenuate sound pressure at a gas flow rate of 20 l/min in both helmet models. However, when the flow rate was set at 40 l/min, the diffuser filter increased sound pressure rather than attenuating it. At an intermediate gas flow rate of 30 l/min, opposite results were obtained for each ear.
The results obtained in our study suggest that even using a filter, sound pressure levels exceed the recommended threshold (45 dBA),[12] regardless of the gas flow rate. At 30 and 40 l/min flow rates, sound levels exceeded the 40 phons isophonic curve in most of the spectrum. Thus, 40 phons is the threshold for healthy individuals; when sound levels exceed this limit, they cause pain, especially when their duration is long. However, this threshold might be different for neonates. This finding is consistent with the results obtained by Cavaliere et al.,[6] who reported that sound levels increased with the use of the helmet. Conversely, another study on infants[26] found that no additional discomfort (measured using the COMFORT scale) was caused by the use of helmets, which generate a 51–75 dBA sound pressure level. However, this study was performed only on 27 neonates, interobserver reliability in the use of the COMFORT scale was not assessed, and a potential relationship between the score on the COMFORT scale with sound pressure levels was not assessed.
A limitation to this study is that it is an in vitro study. Thus, we measured sound intensity within the helmet, but not the intensity as perceived in the inner ear, and we are aware that bone conduction reduces the sound intensity perceived in the inner ear.[5] In addition, although two different helmet models were used in this study (StarMed and DimAir), we do not know whether the results obtained can be projected to devices made of other materials and of different sizes.
In conclusion, we observed that sound pressure levels during the administration of helmet CPAP exceed the limits currently recommended (45 dBA). In addition, we found that sound pressure levels are related to the type of helmet, the gas flow rate, and the use or not of a diffuser at the junction of the inspiratory branch of the helmet. When administering helmet CPAP to neonates, a gas flow rate as low as possible should be administered and diffuser filters should be used only with flow rates lower than 30 l/min.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26. doi: 10.1542/peds.2011-3028. [DOI] [PubMed] [Google Scholar]
- 2.Chidini G, Calderini E, Cesana BM, Gandini C, Prandi E, Pelosi P. Noninvasive continuous positive airway pressure in acute respiratory failure: Helmet versus facial mask. Pediatrics. 2010;126:e330–6. doi: 10.1542/peds.2009-3357. [DOI] [PubMed] [Google Scholar]
- 3.Trevisanuto D, Grazzina N, Doglioni N, Ferrarese P, Marzari F, Zanardo V. A new device for administration of continuous positive airway pressure in preterm infants: Comparison with a standard nasal CPAP continuous positive airway pressure system. Intensive Care Med. 2005;31:859–64. doi: 10.1007/s00134-005-2638-9. [DOI] [PubMed] [Google Scholar]
- 4.Karam O, Donatiello C, Van Lancker E, Chritin V, Pfister RE, Rimensberger PC. Noise levels during nCPAP are flow-dependent but not device-dependent. Arch Dis Child Fetal Neonatal Ed. 2008;93:F132–4. doi: 10.1136/adc.2007.129098. [DOI] [PubMed] [Google Scholar]
- 5.Surenthiran SS, Wilbraham K, May J, Chant T, Emmerson AJ, Newton VE. Noise levels within the ear and post-nasal space in neonates in intensive care. Arch Dis Child Fetal Neonatal Ed. 2003;88:F315–8. doi: 10.1136/fn.88.4.F315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cavaliere F, Conti G, Costa R, Proietti R, Sciuto A, Masieri S. Noise exposure during noninvasive ventilation with a helmet, a nasal mask, and a facial mask. Intensive Care Med. 2004;30:1755–60. doi: 10.1007/s00134-004-2347-9. [DOI] [PubMed] [Google Scholar]
- 7.Trevisanuto D, Camiletti L, Doglioni N, Cavallin F, Udilano A, Zanardo V. Noise exposure is increased with neonatal helmet CPAP in comparison with conventional nasal CPAP. Acta Anaesthesiol Scand. 2011;55:35–8. doi: 10.1111/j.1399-6576.2010.02356.x. [DOI] [PubMed] [Google Scholar]
- 8.Abou Turk C, Williams AL, Lasky RE. A randomized clinical trial evaluating silicone earplugs for very low birth weight newborns in intensive care. J Perinatol. 2009;29:358–63. doi: 10.1038/jp.2008.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang EF, Merzenich MM. Environmental noise retards auditory cortical development. Science. 2003;300:498–502. doi: 10.1126/science.1082163. [DOI] [PubMed] [Google Scholar]
- 10.Trapanotto M, Benini F, Farina M, Gobber D, Magnavita V, Zacchello F. Behavioural and physiological reactivity to noise in the newborn. J Paediatr Child Health. 2004;40:275–81. doi: 10.1111/j.1440-1754.2004.00363.x. [DOI] [PubMed] [Google Scholar]
- 11.Wachman EM, Lahav A. The effects of noise on preterm infants in the NICU. Arch Dis Child Fetal Neonatal Ed. 2011;96:F305–9. doi: 10.1136/adc.2009.182014. [DOI] [PubMed] [Google Scholar]
- 12.Noise: A hazard for the fetus and newborn. American Academy of Pediatrics. Committee on Environmental Health. Pediatrics. 1997;100:724–7. [PubMed] [Google Scholar]
- 13.Wang D, Aubertin C, Barrowman N, Moreau K, Dunn S, Harrold J. Examining the effects of a targeted noise reduction program in a neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2014;99:F203–8. doi: 10.1136/archdischild-2013-304928. [DOI] [PubMed] [Google Scholar]
- 14.Walsh-Sukys M, Reitenbach A, Hudson-Barr D, DePompei P. Reducing light and sound in the neonatal intensive care unit: An evaluation of patient safety, staff satisfaction and costs. J Perinatol. 2001;21:230–5. doi: 10.1038/sj.jp.7200534. [DOI] [PubMed] [Google Scholar]
- 15.Almadhoob A, Ohlsson A. Sound reduction management in the neonatal intensive care unit for preterm or very low birth weight infants. Cochrane Database Syst Rev. 2015;1:CD010333. doi: 10.1002/14651858.CD010333.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Taccone P, Hess D, Caironi P, Bigatello LM. Continuous positive airway pressure delivered with a “helmet”: Effects on carbon dioxide rebreathing. Crit Care Med. 2004;32:2090–6. doi: 10.1097/01.ccm.0000142577.63316.c0. [DOI] [PubMed] [Google Scholar]
- 17.Fernández-Hernández F, Ricardo-Cueto JL, Lubián-López SP, Alonso-Ojembarrena A. Influence of air-oxygen flow in infants with CPAP in a NICU. Prague: Paper presented at Euronoise; 2012. [Google Scholar]
- 18.Livera MD, Priya B, Ramesh A, Suman Rao PN, Srilakshmi V, Nagapoornima M, et al. Spectral analysis of noise in the neonatal intensive care unit. Indian J Pediatr. 2008;75:217–22. doi: 10.1007/s12098-008-0048-z. [DOI] [PubMed] [Google Scholar]
- 19.Gerhardt KJ, Abrams RM. Fetal exposures to sound and vibroacoustic stimulation. J Perinatol. 2000;20:S21–30. doi: 10.1038/sj.jp.7200446. [DOI] [PubMed] [Google Scholar]
- 20.Lasky RE, Williams AL. Noise and light exposures for extremely low birth weight newborns during their stay in the neonatal intensive care unit. Pediatrics. 2009;123:540–6. doi: 10.1542/peds.2007-3418. [DOI] [PubMed] [Google Scholar]
- 21.Milési C, Ferragu F, Jaber S, Rideau A, Combes C, Matecki S, et al. Continuous positive airway pressure ventilation with helmet in infants under 1 year. Intensive Care Med. 2010;36:1592–6. doi: 10.1007/s00134-010-1940-3. [DOI] [PubMed] [Google Scholar]
- 22.Patroniti N, Foti G, Manfio A, Coppo A, Bellani G, Pesenti A. Head helmet versus face mask for non-invasive continuous positive airway pressure: A physiological study. Intensive Care Med. 2003;29:1680–7. doi: 10.1007/s00134-003-1931-8. [DOI] [PubMed] [Google Scholar]
- 23.Racca F, Appendini L, Gregoretti C, Stra E, Patessio A, Donner CF, et al. Effectiveness of mask and helmet interfaces to deliver noninvasive ventilation in a human model of resistive breathing. J Appl Physiol. 2005;99:1262–71. doi: 10.1152/japplphysiol.01363.2004. [DOI] [PubMed] [Google Scholar]
- 24.Roberts CT, Dawson JA, Alquoka E, Carew PJ, Donath SM, Davis PG, et al. Are high flow nasal cannulae noisier than bubble CPAP for preterm infants? Arch Dis Child Fetal Neonatal Ed. 2014;99:F291–5. doi: 10.1136/archdischild-2013-305033. [DOI] [PubMed] [Google Scholar]
- 25.Cavaliere F, Conti G, Costa R, Spinazzola G, Proietti R, Sciuto A, et al. Exposure to noise during continuous positive airway pressure: Influence of interfaces and delivery systems. Acta Anaesthesiol Scand. 2008;52:52–6. doi: 10.1111/j.1399-6576.2007.01474.x. [DOI] [PubMed] [Google Scholar]
- 26.Medina A, Alvarez Fernández P, Rey Galán C, Álvarez Mendiola P, Álvarez Blanco S, Vivanco Allende A. Comfort and noise level in infants with helmet interface. An Pediatr (Barc) 2015;83:272–6. doi: 10.1016/j.anpedi.2015.02.010. [DOI] [PubMed] [Google Scholar]


