Abstract
Solitary bone metastasis to fibula in patients of lung carcinoma is a rare entity, with only four cases reported in literature. We, hereby, present a case of a 50 year-old-male who was given three cycles of chemotherapy for lung carcinoma with no distant metastasis but presented 2 months later with a fusiform, painful swelling around the knee that was clinically suspected to be inflammatory in nature but proved to be fibular metastasis on cytology. There was no evidence of skeletal metastasis on initial bone scan. He was given palliative radiotherapy for this with symptomatic relief.
Keywords: Fibular metastasis, lung carcinoma, solitary fibular metastasis
Introduction
Overall lung cancer is the most common cancer, in terms of both incidence as well as mortality.[1] Lung cancer can metastasise to multiple sites. Metastasis to liver, adrenals, bones, brain, and kidney have been reported.[2] Metastasis to bone commonly occurs in axial skeleton,[3] followed by femur and humerus. Metastasis distal to knee and elbow are rare and even rarer is solitary metastasis to fibula.[3] Till date, in the literature only 10 cases of solitary fibular metastasis have been reported,[3,4,5,6,7,8,9,10] out of which lung was the primary site of malignancy in only four cases.[3,4,5] The authors report a case of lung carcinoma undergoing chemotherapy that initially did not have any bony metastasis but presented with a painful swelling below the knee that turned out to be a solitary fibular metastasis on biopsy.
Case Report
A 50-year-old male came to outpatient department of our tertiary care center with complaints of left sided chest pain for 2 months, hoarseness of voice for 1 month, and cough with hemoptysis. There was history of chronic smoking. On examination, the patient was stable, nondyspnoeic with normal vitals. There was no icterus, pallor, or cyanosis. Karnofsky performance status was around 70%. A computed tomography (CT) scan of the chest was advised, which revealed a large, irregular, heterogeneous soft tissue density mass lesion in the left upper and lingular lobe of size ~6.3 cm × 5.6 cm × 11 cm (AP × T × CC). There were a few, well defined ground-glass nodules in bilateral lung fields suggestive of metastasis with left sided pleural effusion.
Histopathological examination from left lung mass was suggestive of poorly differentiated squamous cell carcinoma of the lung. Also, pleural fluid cytology examination was positive for malignancy. Contrast enhanced CT (CECT) abdomen and bone scan done as a part of metastatic work up revealed no distant metastasis. Chemoradiation was planned as the patient was surgically inoperable at the time of presentation. Taxane- and cisplatin-based chemotherapy was started at three weekly interval. During the course of treatment, after receiving the third cycle of chemotherapy, the patient developed severe pain in the right knee and proximal leg. On examination, a fusiform swelling with ill-defined margins was noted on the anterolateral aspect of the right knee joint [Figure 1a]. It was ~3 cm × 2.5 cm in size, hard, fixed, and tender. There was no history of fever or trauma. Initially it was considered as an inflammatory condition and treated accordingly. Later on, an X-ray of the knee joint was done that revealed an expansile lytic lesion of fibula [Figure 1b]. CECT knee showed an ill-defined, expansile, destructive lesion on the posterolateral aspect of the head of fibula with a large, heterogeneously enhancing soft tissue component. FNAC from the lesion in the fibula was performed that showed malignant squamous cells with evidence of keratinization suggesting the possibility of metastasis [Figure 1c]. Biopsy from the lesion confirmed metastatic squamous cell carcinoma to fibula [Figure 1d]. The patient was given palliative local radiotherapy 30 gray in 10 fractions for fibular metastasis. After 15 days of palliative irradiation the patient was evaluated, there was partial reduction in the size of the lesion but he got complete relief of pain. Patient was planned for second line chemotherapy but unfortunately he did not return and was lost to follow-up.
Figure 1.
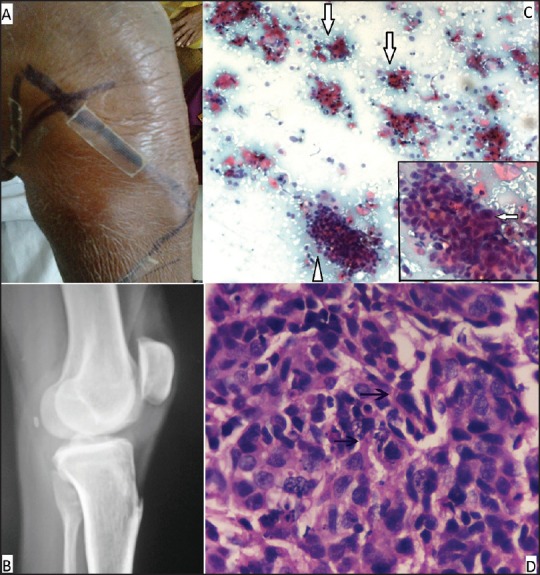
(a) Clinical photograph of the swelling (b) X-ray of knee joint (lateral view) shows lytic expansile lesion of the head of fibula (c) Fine needle aspiration cytology of the lesion shows clusters of malignant squamous cells (triangle) with evidence of keratinization (solid arrow) (100×) with evidence of intracytoplasmic keratinization (solid arrow, inset) (400×) (d) H and E stained section showing malignant squamous cells with hyperchromatic nuclei and dense eosinophilic cytoplasm (arrow) (H and E ×400)
Discussion
Fibula as the site of solitary metastasis from any primary tumour is extremely rare. Till date to the best of our knowledge, only 10 cases of solitary fibular metastasis have been reported.[3,4,5,6,7,8,9,10] Out of these 10 cases, in four cases the primary tumour was in lung as seen in our case.[3,4,5] Four cases of gynaecological malignancies have been reported with solitary metastasis to fibula.[6,7,8] And, one case of renal and gastric origin with solitary fibular metastasis has been reported.[9,10] In these 10 cases there was no sex predilection and male:female ratio was 1:1. The age range was mid-thirties to mid-seventies. The youngest patient was 36 years old with primary cervical cancer, whereas the oldest patient, who had lung carcinoma, was 76 years old. Among the 10 cases previously reported in literature, the right and the left fibula was involved with equal frequency. Three patients with primary lung cancer and one patient with vaginal cancer had solitary metastasis to fibula at the time of presentation, whereas one patient of lung cancer as well as the patient with gastric cancer developed fibular metastasis 6 months after detection of primary tumor. A female patient with carcinoma cervix developed fibular metastasis 9 months after treatment.[7] In patients with endometrial cancer and primary renal cell carcinoma, fibular metastasis was detected 5 years after the initial presentation.[8,9] In the present case, fibular metastasis was seen after 2 months from the initial diagnosis of primary lung cancer. In all these patients’ pain and swelling were the main symptoms when they developed fibular metastasis.
This type of presentation at unusual sites, initially suspected as nonmalignant inflammatory conditions, as seen in our case leads to delay in diagnosing these findings. Although bone scan is generally accepted as the initial method of choice for bone metastasis assessment, it is not performed as a routine clinical practice in our setup unless otherwise it is clinically indicated. In this patient, baseline bone scan was performed that was negative for bony metastasis. At the time of presentation of fibular disease, bone scan was not done as the clinical index of suspicion was more in favour of an infective or unrelated pathology, such as osteomyelitis. Moreover, there were no symptoms and signs suggestive of skeletal metastasis elsewhere in the patient. The unique features of this case are the involvement of long bone (fibula) as the sole metastatic site with no clinical feature indicative of metastasis throughout the rest of the skeleton and presentation as an inflammatory swelling.
Conclusion
This case report gives insight that any new complaint or/and finding in the patient developing during treatment should be evaluated carefully with high index of suspicion for metastasis so that active intervention could be done timely. Cytology from the new lesion can be helpful in making early diagnosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Lin HC, Yu CP, Lin HA, Lee HS. A case of lung cancer metastasized to the gastrointestinal anastomosis site where the primary gastric cancer was resected 17 years ago. Lung Cancer. 2011;72:255–7. doi: 10.1016/j.lungcan.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Hirano Y, Oda M, Tsunezuka Y, Ishikawa N, Watanabe G. Long-term survival cases of lung cancer presented as solitary bone metastasis. Ann Thorac Cardiovasc Surg. 2005;11:401–4. [PubMed] [Google Scholar]
- 4.Hsu CC, Chuang YW, Lin CY, Huang YF. Solitary fibular metastasis from lung cancer mimicking stress fracture. Clin Nucl Med. 2006;31:269–71. doi: 10.1097/01.rlu.0000210502.13622.50. [DOI] [PubMed] [Google Scholar]
- 5.Fanggiday JC, Uyterlinde W, van den Heuvel MM, Valdés Olmos RA. Solitary bone metastasis appearing outside the usual range of FDG PET/CT in stage III lung cancer: Is total body FDG PET/CT imaging mandatory? J Nucl Med Radiat Ther. 2012;3:135. [Google Scholar]
- 6.Tjalma WA, Somville J. Fibula metastasis as the presenting feature of vaginal cancer. Eur J Gynaecol Oncol. 2011;32:114–6. [PubMed] [Google Scholar]
- 7.Pasricha R, Tiwari A, Aggarwal T, Lal P. Carcinoma of uterine cervix with isolated metastasis to fibula and its unusual behavior: Report of a case and review of literature. J Cancer Res Ther. 2006;2:79–81. doi: 10.4103/0973-1482.25857. [DOI] [PubMed] [Google Scholar]
- 8.Vanecko RM, Yao ST, Schmitz RL. Metastasis to fibula from endometrial carcinoma. Report of 2 cases. Obstet Gynecol. 1967;29:803–5. [PubMed] [Google Scholar]
- 9.Rajan P, Warner A, Quick CR. Fibular metastasis from renal cell carcinoma masquerading as deep vein thrombosis. BJU Int. 1999;84:735–6. doi: 10.1046/j.1464-410x.1999.00295.x. [DOI] [PubMed] [Google Scholar]
- 10.Hekmat S, Ghaedian T, Barati H, Movahed M. Solitary metastasis of gastric cancer to fibula: A case report. Iran J Radiol. 2012;9:161–4. doi: 10.5812/iranjradiol.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]


