Abstract
Objective
This study aimed to evaluate a conceptual framework that assessed the effect of Hispanic residential isolation on Attention Deficit Hyperactivity Disorder (ADHD) health service utilization among 2.2 million publicly insured youth.
Design
Cross-sectional.
Setting
Medicaid administrative claims data for ambulatory care services from a US Pacific state linked with US census data.
Participants
Youth, aged 2-17 years, continuously enrolled in 2009
Main Outcome Measures
The percent annual prevalence and odds of ADHD diagnosis and stimulant use according to two measures of racial/ethnic residential isolation: 1) the county-level Hispanic isolation index (HI) defined as the population density of Hispanic residents in relation to other racial/ethnic groups in a county (<.5; .5-.64; ≥.65); and 2) the proportion of Hispanic residents in a ZIP code tabulation area (<25%; 25%-50%; >50%).
Results
Among the 47,364 youth with a clinician-reported ADHD diagnosis, 60% received a stimulant treatment (N = 28,334). As the county level HI increased, Hispanic residents of ethnically isolated locales were significantly less likely to receive an ADHD diagnosis (adjusted odds ratio [AOR]=.92 [95% CI=.88-.96]) and stimulant use (AOR=.61 [95% CI=.59-.64]) compared with Hispanic youth in less isolated areas. At the ZIP code level, a similar pattern of reduced ADHD diagnosis (AOR=.81 [95% CI=.77-.86]) and reduced stimulant use (AOR=.65 [95% CI=.61-.69]) was observed as Hispanic residential isolation increased from the least isolated to the most isolated ZIP code areas.
Conclusions
These findings highlight the opportunity for Big Data to advance mental health research on strategies to reduce racial/ethnic health disparities, particularly for poor and vulnerable youth. Further exploration of racial/ethnic residential isolation in other large data sources is needed to guide future policy development and to target culturally sensitive interventions.
Keywords: Medicaid, ADHD, Stimulants, Hispanic Youth, Racial/ethnic Disparities, Residential Segregation
Introduction
Variations in US health service utilization have been known and tracked in relation to geographic regions, subpopulations (eg, by age group, sex, race/ethnicity), insurance coverage, and other socioeconomic factors that influence utilization of health care services.1-4 Historically, the literature shows lower health care utilization among Hispanic youth compared with youth of other race/ethnicity.5-8 To advance the dialogue on the disparate use of mental health services by Hispanic youth compared with their racial/ethnic counterparts, our large population-based study focused on the diagnostic and medication treatment patterns of youth diagnosed with attention-deficit/hyperactivity disorder (ADHD) using administrative claims data from California, the state with the largest group of Hispanic youth with Medicaid insurance.
We examined ADHD diagnostic and treatment patterns because ADHD is the most common pediatric behavioral mental health disorder. In a 2011 national survey, approximately 6.4 million youth in the United States were diagnosed with ADHD.9 Furthermore, among youth aged 4-17 years, the population of ADHD diagnosed youth grew substantially from 7.8% in 2003 to approximately 11% in 2011, representing a 41% increase in 8 years. However, in 2011, there was a 44% lower ADHD diagnostic prevalence among Hispanic youth compared to their non-Hispanic counterparts.10 Analyzing different residential clusters of Hispanic to non-Hispanic persons may reveal practical differences in access and availability of services as well as cultural preferences that limit the use of medical care.11 Further, understanding the role of racial/ethnic geographic population density in the previously reported disparities in ADHD service utilization patterns will better address health disparities in underserved regions by including geographic population density in planning research and tailoring interventions more appropriately in the various Hispanic communities within regions of the United States.
For the past 25 years, numerous measures have been developed to assess residential segregation using geographic patterns of residential mix, eg, evenness, exposure, concentration, centralization and clustering.12 In our study, with data from a large statewide Medicaid youth population, we selected an exposure measure, namely isolation index, which assesses the population density of a minority group (ie, Hispanic) in relation to other racial/ethnic groups. We theorized that a similar racial/ethnic cultural background influences health care decisions that then lead to similar patterns of health service utilization.
Conceptual Framework
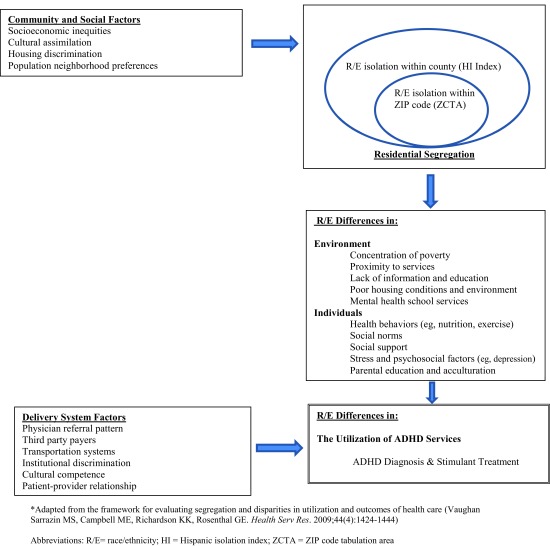
In researching disparities that affect minorities and youth in low-income families, it may be useful to view comparative diagnostic and treatment data in a conceptual framework of racial/ethnic residential segregation. Residential segregation research on health care utilization aims to link the population density of a minority group’s residential locale to its pattern of health service utilization and health outcomes. Racial/ethnic isolation (an exposure measure of residential segregation) is believed to indirectly influence health service utilization through individual and environmental factors such as poor housing conditions, detrimental communal health behaviors and beliefs, and low proximity to basic health services.13,14 Figure 1 depicts a conceptual framework for assessing the association between residential segregation and racial/ethnic disparities in the utilization of ADHD services. It highlights community and social factors that promote residential isolation, which in turn promotes disparities in health service utilization.
Figure 1. A conceptual framework for evaluating racial/ethnic (R/E) residential isolation and disparities in ADHD diagnosis and stimulant use.
Based on this conceptual mode, our study aimed to assess the impact of racial/ethnic geographic isolation on ADHD service utilization patterns among publicly insured youth. In this approach, the method capitalizes on both data volume (2.2 million youth Medicaid enrollees in California) and variety (ie, linkage of claims data to US census data). Specifically, we aimed to assess differences between Medicaid-insured Hispanic residents in high ethnic isolation areas and Hispanic residents in lower ethnic isolation areas in relation to clinician-reported ADHD diagnosis and stimulant use, the leading medication treatment for ADHD. These outcomes were assessed according to gradients of two measures of residential isolation: 1) county level Hispanic isolation indices (HI); and 2) ZIP code level proportion of Hispanic residents in the Medicaid enrollee’s ZIP code of residence. This ZIP code level measure of residential isolation is used as a proxy for census tract level measures to facilitate a more granular assessment of racial/ethnic composition in the Medicaid enrollees’ immediate locale since census tract information is not available in Medicaid data.
Methods
Data Source and Study Design
We analyzed computerized data from the 2009 Medicaid administrative claims of California. The data source included enrollment, outpatient hospital clinic and physician files, and prescription drug files. Medicaid enrollee data included enrollees’ ZIP code of residence which was linked to American Community Survey data at the county and ZIP code levels.15 These datasets were linked at the county level to calculate Hispanic Isolation Index and at the ZIP code level to calculate a proxy measure of isolation at a more granular level using ZIP code tabulation areas. A cross-sectional design was applied to the 2009 claims data restricting the dataset to continuously enrolled youth aged 2 through 17 years (N=2,221,010). The study population represented 83.7% of the state’s total Medicaid youth population and included all youth regardless of service utilization. The study was reviewed and approved by the University of Maryland Institutional Review Board. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Independent Variables and Hispanic Isolation Index
The main independent variables were county level Hispanic isolation index and ZIP code level Hispanic composition.
The Hispanic Isolation Index (HI) in each county was calculated as the Hispanic weighted average of the Hispanic proportion in each county.15 This index measures the extent to which minority members live in proximity to one another in a geographic area.12,16 The index ranges from 0 to 1.0. A score >.6 reflects a high level of isolation of Hispanic residents from members of other racial/ethnic groups.12 The range of county-level isolation indices in this study was categorized as <.50; .50 -.64; and ≥.65, which approximates tertiles in the distribution. HI was calculated using the following equation:16
n∑i-1 [(xi/X) (xi/ti)]
Where xi= Hispanic population of area i; n=total number of counties; X=sum of all xi; t=total population of area i
Zip Code Level - Hispanic Composition
Medicaid administrative claims data do not contain census tract information for each enrollee. However, data on the ZIP code of enrollees’ residence were available and were linked to the US Census Bureau’s ZIP code tabulation area (ZCTA) files for information on racial/ethnic composition per ZIP code area. Zip code level Hispanic composition was defined as the proportion of the Hispanic population living in the Medicaid enrollee’s ZIP code of residence, drawn from the US census ZCTA.15 Hispanic composition was categorized as < 25%; 25%-50%; and >50%, producing a gradient of Hispanic population density in the Medicaid enrollees’ immediate residential locale.
Outcomes
ADHD Diagnosis
Clinician-reported ADHD diagnosis was assessed using International Classification of Diseases-9-Clinical Modification codes (ICD-9-CM code 314.xx) from outpatient treatment and physician files. At least 2 outpatient ADHD claims on separate days were required to qualify for the diagnosis of ADHD.17
Stimulant Use
The annual prevalence of stimulant use was defined as the proportion of total continuously enrolled youth with ≥1 stimulant dispensings in 2009. Only oral product forms of methylphenidate, dexmethylphenidate and amphetamine related salt products were identified as stimulants in this study. Stimulant use was ascertained from prescription drug files, which include national drug code, stimulant dispensing date and drug name.
Study Covariates
ZIP code tabulation area information was used to assess median annual household income in the Medicaid enrollee’s ZIP code of residence and was categorized as <$25,000; $25,000-$50,000; and >$50,000.18 ZCTA information was not available for 639 youth (1.35%) with an ADHD diagnosis. County level median income was imputed for these 639 youth.
Other study covariates included age groups (2–4, 5–9, 10–14, and 15–17 years), sex, and Medicaid eligibility category. Eligibility categories included foster care, youth with disabilities (ie, in families receiving Supplemental Security Income), and income eligible youth (ie, enrollees in the state Children’s Health Insurance Program or the Temporary Assistance for Needy Families program). Using a previously published algorithm,19 a hierarchical approach was applied for youth who were eligible in more than one category during 2009 in the following rank order: foster care, youth with disabilities, and income eligible youth.
Statistical Analysis
Statistical analyses were conducted using SAS version 9.3 (SAS Institute, Inc., Cary, NC). Demographic characteristics of continuously enrolled youth were assessed in terms of the total population and in relation to the county-level HI.
The annual prevalence of ADHD diagnosis per 100 youth was calculated as a proportion of the study participants, total and stratified by race/ethnicity. Furthermore, among youth diagnosed with ADHD, the annual percentage of stimulant use was calculated in total and stratified by race/ethnicity. Two sets of multivariable logistic regression models were conducted. Comparing youth of other races to White youth, the first set of regression examined: 1) the odds of an ADHD diagnosis; and 2) the odds of a stimulant dispensing among youth diagnosed with ADHD. Each of these two logistic regression models was adjusted for median household income, age group, sex and Medicaid eligibility category.
A second set of multivariable regression models was evaluated only among Hispanic youth. In the first models, we assessed the odds of an ADHD diagnosis by county-level HI index and by ZIP code level Hispanic proportion. In the second model, we assessed the odds of a stimulant dispensing among ADHD diagnosed youth by county-level HI index and by ZIP code level Hispanic proportion. The models were adjusted for covariates as described above.
Results
Population Characteristics
There were 2.2 million continuously enrolled Medicaid-insured youth aged 2-17 years in California in 2009. The majority were of Hispanic ethnicity (63.7%) and were <10 years of age (54.2%) (Table 1). Medicaid eligibility based on family income (TANF and CHIP) accounted for 90% of the enrolled youth, while the remainder was equally divided between foster care enrollees and youth with disabilities. More than half (53.7%) of the Medicaid eligible population lived in counties with a median household income less than $50,000/year.
Table 1. Population characteristics of continuously enrolled Medicaid-insured youth in total and according to Hispanic Isolation Index in California in 2009.
| Total | County-level Hispanic Isolation Index | |||||||
| <.50 | .50–.64 | ≥.65 | ||||||
| N=2,221,010 | % | n=627,029 | % | n=722,794 | % | n=871,187 | % | |
| Overall HI % | 28.2 | 32.5 | 39.2 | |||||
| Race/ethnicity | ||||||||
| White | 330,386 | 14.9 | 139,878 | 22.3 | 120,630 | 16.7 | 69,878 | 8.0 |
| Hispanic | 1,414,221 | 63.7 | 277,512 | 44.3 | 478,792 | 66.2 | 657,917 | 75.5 |
| Black | 234,164 | 10.5 | 91,086 | 14.5 | 58,132 | 8.0 | 84,946 | 9.8 |
| Othera | 242,239 | 10.9 | 118,553 | 18.9 | 65,240 | 9.0 | 58,446 | 6.7 |
| Age group, yrs | ||||||||
| 2–4 | 510,034 | 23.0 | 143,084 | 22.8 | 173,128 | 23.9 | 193,824 | 22.3 |
| 5–9 | 691,902 | 31.2 | 191,992 | 30.6 | 229,206 | 31.7 | 270,704 | 31.1 |
| 10–14 | 633,454 | 28.5 | 176,685 | 28.2 | 203,110 | 28.1 | 253,659 | 29.1 |
| 15–17 | 385,620 | 17.4 | 115,268 | 18.4 | 117,352 | 16.2 | 153,000 | 17.6 |
| Sex | ||||||||
| Female | 1,100,184 | 49.5 | 311,575 | 49.7 | 358,230 | 49.6 | 430,379 | 49.4 |
| Male | 1,120,826 | 50.5 | 315,454 | 50.3 | 364,564 | 50.4 | 440,808 | 50.6 |
| Medicaid eligibility group | ||||||||
| Income (TANF & CHIP) | 1,980,322 | 89.9 | 544,235 | 86.8 | 648,469 | 89.7 | 787,618 | 90.4 |
| Disability (SSI) | 122,603 | 5.5 | 39,902 | 6.4 | 39,338 | 5.4 | 43,363 | 5.0 |
| Foster Care | 118,085 | 4.6 | 42,892 | 6.8 | 34,987 | 4.8 | 40,206 | 4.6 |
| Median household income, county-level | ||||||||
| <$35,000 | 321,002 | 14.5 | 37,976 | 6.1 | 113,071 | 15.6 | 169,955 | 19.5 |
| $35,000-$50,000 | 870,838 | 39.2 | 216,251 | 34.5 | 246,994 | 34.2 | 407,593 | 46.8 |
| >$50,000 | 1,029,170 | 46.3 | 372,802 | 59.5 | 362,729 | 50.2 | 787,618 | 33.7 |
a. Alaskan Native, Asian, Pacific Islander or unknown race.
TANF, Temporary Assistance for Needy Families; CHIP, Children’s Health Insurance Program; SSI, Supplemental Security Income.
Residential Distribution Patterns
The county-level distribution of the 2.2 million youth enrollees according to the HI index ranged from 28.2% in counties with an HI index <.5, to 39.2% in counties with an HI index >.65 (Table 1). Compared with the 44.3% of Hispanic youth living in counties with an HI index <.5, 75.5% of the residents of counties with HI index ≥ .65 were Hispanic youth. At the ZIP code level, the majority of enrollees (53.9%) resided in ZIP code areas with >50% Hispanic population (data not shown).
The gradient effect of increasing geographic isolation is further observed in ZIP code level median household income differences. Of the residents of counties with an HI index ≥0.65, 19.5% had median household income less than $35,000/year. By comparison, in the least isolated counties (HI index <.5), only 6.1% of the Medicaid enrollees had a median household income less than $35,000 (Table 1).
ADHD Diagnosis and Stimulant Use by Race/Ethnicity
There were 47,364 Medicaid-insured youth with a clinician-reported ADHD diagnosis in 2009, resulting in an annual clinician-reported diagnostic prevalence of 2.1%. The prevalence of ADHD diagnosis by race/ethnicity ranged from a high of 5.0% among White enrollees to a low of 1.2% among Hispanic enrollees (Table 2). Overall, the odds of receiving an ADHD diagnosis were significantly lower among Hispanic compared with White youth (AOR=.35; 95% CI=.34–.36). Among total youth with a clinician-reported ADHD diagnosis (N=47,364), 59.8% received one or more stimulant dispensings during the study year. Across racial/ethnic groups, stimulant use among ADHD diagnosed youth ranged from 65.7% among White enrollees to 54.9% among Hispanic enrollees. Overall, the odds of receiving a stimulant dispensing was significantly lower among Hispanic compared with White youth (AOR=.69; 95% CI=.66–.73).
Table 2. Prevalence and adjusted odds ratios (AOR) of clinician-reported ADHD diagnosis and percentage of stimulant use among 2.2 million continuously enrolled Medicaid-insured youth in California in 2009.
| N | % Prevalence | AORb | 95% CI | |
| ADHD diagnosis, N=47,364 | 2.1 | |||
| Race/ethnicity | ||||
| White | 16,560 | 5.0 | 1.00 | Reference |
| Hispanic | 17,281 | 1.2 | .35 | .34–.36 |
| Black | 7,849 | 3.4 | .64 | .63–.66 |
| Otherc | 5,674 | 2.3 | .38 | .37–.40 |
| Stimulant use, n=28,334a | 59.8 | |||
| Race/ethnicity | ||||
| White | 10,887 | 65.7 | 1.00 | Reference |
| Hispanic | 9,488 | 54.9 | .69 | .66–.73 |
| Black | 4,458 | 56.8 | .67 | .63–.70 |
| Other | 3,501 | 61.7 | .76 | .71–.81 |
a. Among ADHD diagnosed youth.
b. Adjusting for age-group, sex, and Medicaid eligibility group.
c. Alaskan Native, Asian, Pacific Islander or unknown race.
ADHD Diagnosis and Hispanic Residential Locale
When analyzed according to county-level HI, the prevalence of ADHD diagnosis among Hispanic youth decreased modestly from 1.32% to 1.16% (AOR=0.92; 95% CI=0.88-0.96), as HI increased from <.5 to ≥.65 (Table 3). However, when assessed at the ZIP code level, the prevalence of ADHD diagnosis among Hispanic youth decreased from 1.72% to 1.12% (AOR=.81; 95% CI=.77–.86) as the Hispanic population in enrollees’ ZIP code of residence increased from <25% to ≥50%. The decrease in the percent prevalence of ADHD diagnosis was considerably greater at the ZIP code level of residential isolation than at the county level of residential isolation (Table 3).
Table 3. Prevalence and adjusted odds ratios (AOR) of clinician-reported ADHD diagnosis among Medicaid-insured Hispanic youth in California by county-level Hispanic isolation index and ZIP code level proportion of Hispanics.
| County-level Hispanic isolation index | % | AORa | 95% CI |
| <.5 | 1.32 | 1.00 | Reference |
| .5–.64 | 1.26 | .99 | .94–1.03 |
| ≥.65 | 1.16 | .92 | .88–.96 |
| ZIP code level of Hispanic proportion | |||
| <25% | 1.72 | 1.00 | Reference |
| 25%-50% | 1.35 | .89 | .84–.94 |
| >50% | 1.12 | .81 | .77–.86 |
a. Adjusting for age-group, sex, median household income (county level), and Medicaid eligibility group.
Stimulant Use and Hispanic Residential Locale
Among Hispanic youth diagnosed with ADHD, the percent stimulant use decreased substantially from 61.37% to 48.28% (AOR=.61; 95% CI=.59-.64) as county level HI index increased from <.5 to ≥.65 (Table 4).
Table 4. Percentage and adjusted odds ratios (AOR) of stimulant use among ADHD diagnosed Medicaid-insured Hispanic youth in California by county-level Hispanic isolation index and ZIP code level proportion of Hispanics.
| County-level Hispanic isolation index | % | AORa | 95% CI |
| <.5 | 61.37 | 1.00 | Reference |
| .5 – .64 | 59.35 | .85 | .82 – .89 |
| ≥.65 | 48.28 | .61 | .59 – .64 |
| ZIP code level Hispanic proportion | |||
| < 25% | 61.37 | 1.00 | Reference |
| 25% - 50% | 56.74 | .81 | .77 – .86 |
| > 50% | 53.02 | .65 | .61 – .69 |
a. Adjusting for age-group, sex, median household income (county level) and Medicaid eligibility group.
Similar findings were observed when stimulant use was assessed across the range of Hispanic composition at the ZIP code level. The percent stimulant use among Hispanic youth diagnosed with ADHD decreased from 61.37% to 53.02% as the proportion of Hispanic residents in enrollees’ ZIP code of residence increased from <25% to ≥50% (AOR=.65; 95% CI=.61–.69) (Table 4).
Discussion
This study of Hispanic residential locale and pediatric ADHD service utilization supports findings from adult studies of health care utilization in that fewer health care services are delivered with increasing racial/ethnic residential isolation.20-23 Compared with youth of other racial/ethnic groups, Hispanic youth had a lower prevalence of ADHD diagnosis and stimulant treatment. The situation worsened with respect to residential locale. The major findings from this population-based study of Medicaid enrolled youth are: 1) The annual percent prevalence and the odds of an ADHD diagnosis were significantly lower for the most isolated Hispanic youth compared with their least isolated Hispanic counterparts regardless of the measure of racial/ethnic residential isolation; and 2) Similarly, among ADHD-diagnosed Hispanic youth, regardless of the measure of population density of Hispanic residents, stimulant use decreased significantly as Hispanic residential isolation intensified.
Collectively, these findings support the role of geographic population density as a factor in accounting for racial/ethnic differences in mental health services for ADHD, the leading pediatric mental health condition and for the use of stimulants, the main evidence-based ADHD treatment. In the following sections, we try to set these findings in the broader context of prior research and future research priorities.
Regional and Racial/Ethnic Variations in the Medicaid-Insured Population
Nationally, regional population health studies have documented lower use of mental health services in states within the western region.10,24,25 These states have very large proportions of Hispanic residents. For example, Hispanic youth in California represent 38.9% of the US Hispanic youth population.26 In the pediatric Medicaid population analyzed in this study, Hispanic youth constituted more than 60% of total Medicaid enrollees, yet their use of services was substantially lower than their White counterparts, and less than their African American and other racial/ethnic counterparts. When assessing health outcomes in community settings, a focus on racial/ethnic residential isolation can enrich our understanding of the deeply lower utilization of mental health services in minority Hispanic populations, particularly among those with low socioeconomic status. Refining the model as was done in the study broadens the context for additional research and targets future interventions on such health disparities.
Expanding the Framework for Health Disparities Research with Big Data
Experts in the field of health disparities have called for expanding the framework of health disparity research to address quality of care27and to bring the social determinants of health inequalities into sharper focus.28 This study sought to respond to the need to further understand the long-standing lower use of health services by Hispanic youth compared with youth of other racial/ethnic groups.
Our study suggests a novel approach that uses Big Data (linking statewide Medicaid claims to US census data) to identify increased Hispanic population density as a determinant of ADHD diagnosis and stimulant treatment among publicly insured Hispanic youth. This approach helps to generate evidence for policy makers to address health disparities in underserved regions. These low service patterns of minority youth may be attributable to differences in health status, access, language barriers and cultural or personal preference,29-31 as well as to institutional racism (ie, structural aspects of the health care delivery system due to perceived or real discrimination).32 Future studies along the Hispanic geographic population density ‘gradient’ could offer critical insight. To address the reasons individuals do not seek care at all, new research methods from patient- and caregiver-centered health care33 could include geographic population density in planning, conducting and disseminating research in the various Hispanic communities within regions of the United States.34
Until a greater research effort is made to establish outcomes of community care across the range of critical factors (namely, socioeconomic, race/ethnicity and small and large area variations), health services research will continue to report discrepant patterns, but with little additional insight to meet the needs of families and youth. Innovative approaches to add the missing critical factors (eg, satisfaction, medication adverse events and reasons for discontinuation), can be embedded in the usual practice setting through the electronic health record so that brief reporting of benefits (improvement in symptoms and functioning, eg, social relationships and academic performance),35 risks (adverse events requiring discontinuation of medication or other therapy) and satisfaction with care can be recorded, even in today’s brief medical visits.36
Our findings suggest that further work should be targeted according to the gradient of Hispanic geographic population density so that social determinants of health can be more fully assessed in accounting for regional and racial/ethnic differences in service use. Focus groups can be used to help assess the quality of services, particularly where perceived discrimination may play a part. Given the substantial growth in Hispanic immigrant communities over the past decades, more attention to the length of acculturation within subgroups of Latinos, eg, Floridians of Cuban vs Californians of Mexican vs New Yorkers of Puerto Rican descent37 could identify preferences related to generational experience and contribute to greater sensitivity to the ethnic background of immigrants. Also, there are opportunities provided by the Affordable Care Act to expand the reach of health care to include many undocumented families.38,39
National survey data often lead to clinically focused discussions of ‘unmet need’ in minority groups related to the long-term goal of ADHD medication treatment. In this narrow clinical view, the social, cultural and economic aspects of child development are easily lost. Thus, we propose that a broader discussion of ‘unmet need’ by minority youth is needed in view of the lack of long-term stimulant outcomes to assure effectiveness and safety of drug therapy in community-treated populations. In this broader approach, the growth of an underclass in the U.S. will be better addressed because health and health care suffer when poverty, family and neighborhood instability are not addressed.28 Without a broader discourse, we cannot expect to address concerns about medicalization of the poor as a malignant endeavor.40
Limitations
Several limitations should be noted: 1) The data source may not generalize to other state Medicaid programs, although the California program includes 38.9% of all US Medicaid-insured Hispanic youth.26 Also, we were not able to subgroup the enrollees into Latinos from particular origins, but presume most enrollees were of Mexican or Mexican American ethnicity;18 2) The diagnostic data in this study represent clinician-reported diagnoses that often are not commensurate with research-level data. Yet, such data provide information on how mental health conditions/problems are identified and treated in community populations; 3) The study outcomes on diagnosis and stimulant treatment provided in this study do not address the continuity of care or duration of stimulant use but provide support for pursuing such aspects of preference and adherence in the future; 4) While census tract data were not available in the Medicaid administrative claims data, our study assessed both county-level and ZIP code level characteristics that were consistent in suggesting that Hispanic population density is an important factor in the utilization of pediatric mental health services; and 5) Finally, this study assessed only stimulant use in the ADHD diagnosed population regardless of other possible medication treatment. However, stimulant users accounted for 93.1% of all ADHD diagnosed youth who received any form of ADHD medication treatment.
Conclusions
ADHD service utilization for Medicaid-insured Hispanic youth decreased significantly as Hispanic residential isolation increased. These findings support residential segregation as a moderator in population mental health research to identify strategies to overcome racial/ethnic health disparities, particularly for poor and vulnerable youth. The findings also highlight the opportunity for Big Data to identify underserved regions and to target these areas for interventions to improve services to minority youth populations, particularly where language and cultural isolation may be major barriers.
Acknowledgments
This project was funded by the Food and Drug Administration, Centers of Excellence in Regulatory Science and Innovation, Minority Health Award (1U01FD004320).
References
- 1.Wennberg JE. In Health Care, Geography is Destiny. Tracking Medicine: A Researcher’s Quest to Understand Health Care. New York: Oxford University Press; 2010:3-13. [Google Scholar]
- 2.CDC The National Ambulatory Medical Care Survey (NAMCS). 2015; http://www.cdc.gov/nchs/ahcd/about_ahcd.htm#NAMCS. Accessed May 9, 2016.
- 3.Cox ER, Motheral BR, Henderson RR, Mager D. Geographic variation in the prevalence of stimulant medication use among children 5 to 14 years old: results from a commercially insured US sample. Pediatrics. 2003;111(2):237-243. 10.1542/peds.111.2.237 [DOI] [PubMed] [Google Scholar]
- 4.Sturm R, Ringel JS, Andreyeva T. Geographic disparities in children’s mental health care. Pediatrics. 2003;112(4):e308-e315. 10.1542/peds.112.4.e308 [DOI] [PubMed] [Google Scholar]
- 5.Branner CM, Koyama T, Jensen GL. Racial and ethnic differences in pediatric obesity-prevention counseling: national prevalence of clinician practices. Obesity (Silver Spring). 2008;16(3):690-694. 10.1038/oby.2007.78 [DOI] [PubMed] [Google Scholar]
- 6.Ferris TG, Kuhlthau K, Ausiello J, Perrin J, Kahn R. Are minority children the last to benefit from a new technology? Technology diffusion and inhaled corticosteriods for asthma. Med Care. 2006;44(1):81-86. 10.1097/01.mlr.0000188914.47033.cd [DOI] [PubMed] [Google Scholar]
- 7.Olfson M, Druss BG, Marcus SC. Trends in mental health care among children and adolescents. N Engl J Med. 2015;372(21):2029-2038. 10.1056/NEJMsa1413512 [DOI] [PubMed] [Google Scholar]
- 8.Zenlea IS, Milliren CE, Mednick L, Rhodes ET. Depression screening in adolescents in the United States: a national study of ambulatory office-based practice. Acad Pediatr. 2014;14(2):186-191. 10.1016/j.acap.2013.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC Attention-Deficit/Hyperactivity DIsorder: Data and Statistics 2016; http://www.cdc.gov/ncbddd/adhd/data.html.
- 10.Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53(1): 34-46. e32. [DOI] [PMC free article] [PubMed]
- 11.Schulz AJ, Kannan S, Dvonch JT, et al. . Social and physical environments and disparities in risk for cardiovascular disease: the healthy environments partnership conceptual model. Environ Health Perspect. 2005;113(12):1817-1825. 10.1289/ehp.7913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Payne-Sturges D, Gee GC, Crowder K, et al. . Workshop summary: connecting social and environmental factors to measure and track environmental health disparities. Environ Res. 2006;102(2):146-153. 10.1016/j.envres.2005.11.001 [DOI] [PubMed] [Google Scholar]
- 13.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404-416. 10.1016/S0033-3549(04)50068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Massey DS, Denton NA. The dimensions of residential segregation. Soc Forces. 1988;67(2):281-315. 10.2307/2579183 [DOI] [Google Scholar]
- 15.Census US. ZIP Code Tabulation Areas (ZCTAs) https://www.census.gov/geo/reference/zctas.html. Accessed May 19, 2016.
- 16.Census US. Measures of Residential Segregation. https://www.census.gov/hhes/www/housing/resseg/pdf/app_b.pdf Accessed May 19, 2016.
- 17.Lurie N, Popkin M, Dysken M, Moscovice I, Finch M. Accuracy of diagnoses of schizophrenia in Medicaid claims. Hosp Community Psychiatry. 1992;43(1):69-71. [DOI] [PubMed] [Google Scholar]
- 18.Census US. California Demographic Statistics http://www.census.gov/quickfacts/table/POP010210/06,00 Accessed May 19, 2016.
- 19.Burcu M, Zito JM, Ibe A, Safer DJ. Atypical antipsychotic use among Medicaid-insured children and adolescents: duration, safety, and monitoring implications. J Child Adolesc Psychopharmacol. 2014;24(3):112-119. 10.1089/cap.2013.0094 [DOI] [PubMed] [Google Scholar]
- 20.Gaskin DJ, Dinwiddie GY, Chan KS, McCleary R. Residential segregation and disparities in health care services utilization. Med Care Res Rev. 2012;69(2):158-175. 10.1177/1077558711420263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chan KS, Gaskin DJ, Dinwiddie GY, McCleary R. Do diabetic patients living in racially segregated neighborhoods experience different access and quality of care? Med Care. 2012;50(8):692-699. 10.1097/MLR.0b013e318254a43c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and black-white disparities in hypertension. Am J Epidemiol. 2011;174(5):537-545. 10.1093/aje/kwr116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dinwiddie GY, Gaskin DJ, Chan KS, Norrington J, McCleary R. Residential segregation, geographic proximity and type of services used: evidence for racial/ethnic disparities in mental health. Soc Sci Med. 2013;80:67-75. 10.1016/j.socscimed.2012.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ExpressScripts Turning Attention to ADHD. 2014; http://lab.express-scripts.com/insights/industry-updates/report-turning-attention-to-adhd
- 25.McDonald DC, Jalbert SK. Geographic variation and disparity in stimulant treatment of adults and children in the United States in 2008. Psychiatr Serv. 2013;64(11):1079-1086. 10.1176/appi.ps.004442012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Th The Kaiser Family Foundation Medicaid enrollment by race/ethnicity. http://kff.org/medicaid/state-indicator/medicaid-enrollment-by-raceethnicity/ Accessed May 19, 2016.
- 27.White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Serv Res. 2012;47(3 Pt 2):1278-1299. 10.1111/j.1475-6773.2012.01410.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099-1104. 10.1016/S0140-6736(05)74234-3 [DOI] [PubMed] [Google Scholar]
- 29.Alegria M, Hasnain-Wynia R, Ayanian JZ. Taking the measure of health care disparities. Health Serv Res. 2012;47(3 Pt 2):1225-1231. 10.1111/j.1475-6773.2012.01424.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 31.Chi JT, Handcock MS. Identifying Sources of Health Care Underutilization Among California’s Immigrants. J Racial Ethn Health Disparities. 2014;1(3):207-218. 10.1007/s40615-014-0028-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57(8):1-22. 10.1177/0002764213487340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.AHRQ Key Themes and Highlights from the National Healthcare Disparities Report. 2008 http://archive.ahrq.gov/research/findings/nhqrdr/nhdr08/Key.html
- 34.Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Aff (Millwood). 2008;27(2):321-333. 10.1377/hlthaff.27.2.321 [DOI] [PubMed] [Google Scholar]
- 35.López L, Green AR, Tan-McGrory A, King R, Betancourt JR. Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. Jt Comm J Qual Patient Saf. 2011;37(10):437-445. 10.1016/S1553-7250(11)37055-9 [DOI] [PubMed] [Google Scholar]
- 36.Zito JM, Derivan AT, Kratochvil CJ, Safer DJ, Fegert JM, Greenhill LL. Off-label psychopharmacologic prescribing for children: history supports close clinical monitoring. Child Adolesc Psychiatry Ment Health. 2008;2(1):24. 10.1186/1753-2000-2-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu SM, Huang ZJ, Kogan MD. State-level health care access and use among children in US immigrant families. Am J Public Health. 2008;98(11):1996-2003. 10.2105/AJPH.2007.117911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.The Economist. Migration to the United States: Under-age and on the move. Jun 28, 2014; http://www.economist.com/news/briefing/21605886-wave-unaccompanied-children-swamps-debate-over-immigration-under-age-and-move. Accessed February 2, 2017.
- 39.Gee ER. Eligible uninsured Latinos: 8 in 10 could receive health insurance marketplace tax credits, Medicaid or CHIP 2014; https://aspe.hhs.gov/sites/default/files/pdf/76756/rb_uninsuredLatinos.pdf. Accessed February 2, 2017.
- 40.Conrad P. The Medicalization of Society: On the Transformation of Human Conditions into Treatable Disorders. Baltimore: JHU Press; 2008. [Google Scholar]