Abstract
Patient: Female, 45
Final Diagnosis: Primary pituitary tuberculosis
Symptoms: Headache • vomiting • vomiting
Medication: —
Clinical Procedure: Pituitary biospy
Specialty: Endocrinology and Metabolic
Objective:
Rare disease
Background:
Primary pituitary tuberculosis (in absence of other organ involvement and constitutional symptoms) is an extremely rare disease with total reported cases in the literature fewer than a hundred. Misdiagnosis as pituitary adenoma is common and late diagnosis can result in a permanent endocrine dysfunction and/or long-term neurologic sequelae.
Case Report:
We report on the case of a middle-aged woman who presented with severe headache and left third cranial nerve palsy. Magnetic resonance imaging (MRI) revealed a large pituitary tumor invading the left cavernous sinus. The case was initially misdiagnosed as pituitary adenoma. A pituitary biopsy was performed and was suggestive of pituitary tuberculosis. Extensive radiologic investigations did not reveal any evidence of other organ involvement by tuberculosis. She was successfully treated with anti-tuberculous medications.
Conclusions:
In areas with a high pre-test probability of tuberculosis, pituitary tuberculosis should be included in the differential diagnosis of pituitary tumors in order to avoid unnecessary surgical interventions. Besides being the first histologically-proven primary pituitary tuberculosis case reported from Qatar, the current case is unique in that extensive radiologic investigations did not reveal any evidence of other systemic or pulmonary tuberculosis.
MeSH Keywords: Pituitary Neoplasms; Tuberculosis, Central Nervous System; Tuberculosis, Endocrine
Background
Despite being known to mankind for hundreds of years, tuberculosis (TB) remains a major global health problem. In 2015, TB was one of the top ten causes of death worldwide with 1.4 million TB deaths in the same year [1]. TB is a systemic disease that can affect any part of the human body. Pulmonary TB accounts for the majority of cases of TB in many countries and is the main transmissible form of the disease [2]. Interestingly, in Qatar, extra-pulmonary TB represents 53.6% of all TB cases. The most frequently reported forms of extra-pulmonary TB in Qatar are TB lymphadenitis (43.5%) and pleural TB (31.6%). Intracranial TB accounts for less than 5% of all TB cases in Qatar [3]. Isolated involvement of the pituitary gland by tuberculous process (in absence of other organ involvement) is an extremely rare occurrence and has not been previously reported from this part of the world. Since the post-mortem diagnosis of the first case by Letchworth in 1924 [4], only fewer than a hundred cases have been reported in the literature. In this paper, we report the first case of isolated pituitary TB diagnosed in Qatar. Extensive radiologic investigations did not reveal any evidence of other systemic or pulmonary TB.
Case Report
A 45 year-old Indian woman was admitted to Hamad General Hospital because of a two-week history of progressive bi-temporal headache that was associated with early morning vomiting and diplopia. She also reported drooping of her left eye lid with blurring of her vision. She denied any history of fever, cough, weight loss, or anorexia. There was no history of sick contact. Apart from long-standing essential hypertension and type 2 diabetes, she had no other chronic illnesses. Physical examination revealed an average-built woman with normal vital signs. Cranial nerve examination revealed complete left-sided third nerve palsy with dilated pupil. Fundoscopic examination did not show papilledema. The rest of physical examination was unremarkable. Laboratory investigations revealed a microcytic anemia (Hb of 8.4 gm/dL). Endocrine profile revealed anterior pituitary hormone deficiencies (Table 1). Erythrocyte sedimentation rate (ESR) was 33 mm/hour (0–20). QuantiFERON®-TB Gold was positive. Magnetic resonance imaging (MRI) of the brain revealed enlargement of the pituitary gland measuring about 12×15×14 cm with thickening of the pituitary stalk and left inter-cavernous extension compressing the left oculomotor nerve suggestive of pituitary macroadenoma (Figure 1). The patient underwent endoscopic transsphenoidal resection of the pituitary lesion. Histologic examination revealed heavily infiltrated pituitary gland by necrotizing granulomatous inflammation (Figure 2). Ziehl-Neeslen (ZN) stain for acid-fast bacilli and fungal studies were negative. Workup for disseminated TB, including CT scan of the chest and abdomen, was unremarkable and HIV testing was negative. Diagnosis of primary pituitary TB was made and four anti-tuberculous medications (isoniazid, rifampicin, ethambutol and pyrazinamide) were commenced (with the intention to treat for 9–12 months). The patient did not receive corticosteroid therapy. Follow-up appointment one month later revealed complete resolution of her symptoms and physical signs. Unfortunately, the patient lost further follow-up as she decided to travel to her home country.
Table 1.
Endocrine profile of the patient.
| Hormone | Value | Reference range |
|---|---|---|
| TSH | 0.3 mIU/L | 0.45–4.5 |
| FT4 | 7.74 pmol/L | 9–20 |
| FSH | 4.0 IU/L | 4–9 |
| LH | 1.52 IU/L | 2–11 |
| Prolactin | 564 mIU/L | 109–557 |
| IGF1 | 74.2 mcg/L | 92.7–244.6 |
| Morning cortisol | 217 nmol/L | 138–580 |
Figure 1.
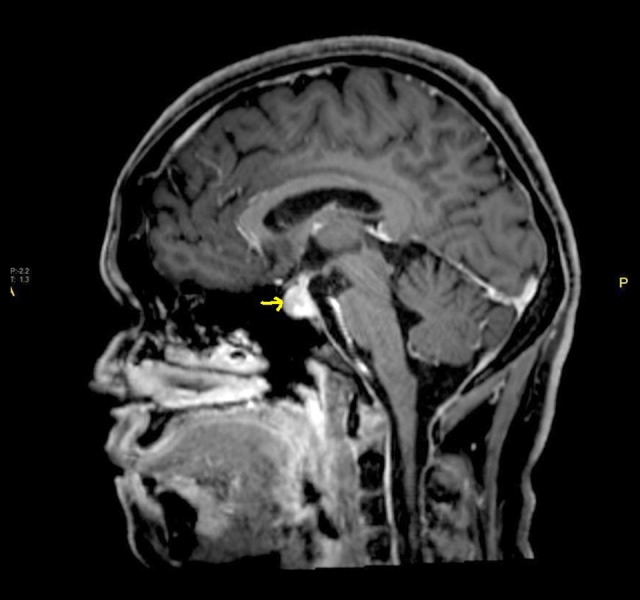
MRI of the pituitary gland demonstrating homogeneous enhancement of pituitary tuberculoma with left intercavernous extension and thickening of the pituitary stalk.
Figure 2.
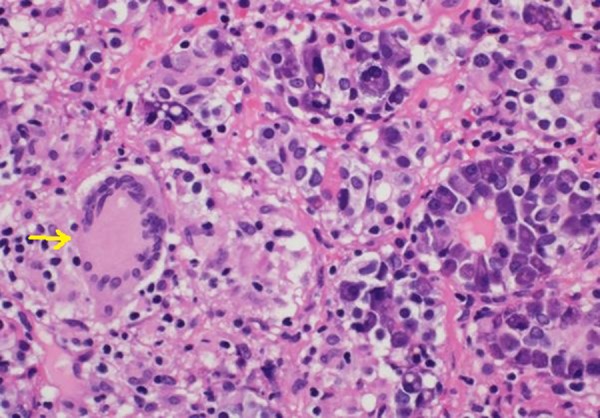
Pituitary biopsy showing necrotizing epithelioid granulomas.
Discussion
The mechanism by which TB bacilli spread to the pituitary gland without apparent involvement of other body organs remains unclear. Hematogenous spread and extension from a tuberculous infection of the paranasal sinuses have been suggested in previous reports [5,6]. The diagnosis of primary pituitary TB is usually very challenging and differentiation from pituitary adenoma on clinical and radiologic basis is often difficult. About 70% of pituitary TB cases reported in the literature were from the Indian subcontinent which can be attributed to the high prevalence of TB in this part of the world [7]. In a very recent comprehensive review of 81 previously published cases of pituitary tuberculomas, Srisukh et al. [8] found that young people were the most commonly affected by the disease and almost 73% of affected cases were females. Headache and visual disturbances were the most common presenting symptoms and absence of constitutional symptoms of TB, such as fever, was characteristic. Hypofunction of the anterior pituitary gland and hyperprolactinemia were seen in about 24% of cases. Interestingly, it has been suggested that the presence of central diabetes insipidus is one of the key features in distinguishing pituitary tuberculoma from pituitary adenoma [8]. Pituitary apoplexy has been reported in three cases of pituitary tuberculomas [8]. In the majority of cases reported in the literature, misdiagnosis as pituitary adenoma was common and histologic examination of the pituitary lesion was the main diagnostic modality. MRI is considered the best radiological modality to diagnose pituitary lesions; however, differentiation between pituitary tuberculoma and adenoma on the basis of MRI findings can be very difficult. Previous reports have suggested that thickening of pituitary stalk can be useful to differentiate pituitary tuberculoma from an adenoma [9]. However, this sign is non-specific and can be seen in a variety of other inflammatory and neoplastic lesions of the pituitary gland such as sarcoidosis, syphilis, lymphomas, and Wegner’s granulomatosis. Other reports suggested the pattern of enhancement as a useful tool in differentiating tuberculomas from other pituitary lesions [6]. Nevertheless, a high index of clinical suspicion remains crucial to avoid unnecessary invasive procedures in such a critical part of the body. Typical finding on histologic examination of pituitary tuberculoma is the demonstration of caseating granuloma. Ziehl-Neelsen stain for TB bacilli is usually negative [10]. The prognosis of pituitary TB depends on the timing of diagnosis and initiation of proper anti-tuberculous medications. Early diagnosis and prompt use of these medications can result in complete recovery of endocrine and neurologic function. However, late diagnosis and treatment may result in permanent endocrine dysfunction. There are no prior studies that have determined the optimal duration of anti-tuberculous medications. A prolonged course (9–12 months), such as that used for meningeal and central nervous system TB, may be a reasonable approach. Surgical intervention is usually reserved for diagnostic or decompressive purposes [8,11]. Hormone replacement therapy may be needed if pituitary functions are affected. In our patient, final diagnosis of primary pituitary TB was made based on typical histologic findings, positive QuantiFERON®-TB Gold and the ethnic origin of the patient (Indian subcontinent). Unfortunately, polymerase chain reaction (PCR) for rapid identification of Mycobacterium tuberculosis DNA was not performed on the pituitary tissue due to the lack of initial suspicion of TB. PCR is being increasingly used as a suitable method for sensitive and fast detection of M. tuberculosis complex DNA in histological material including formalin-fixed tissues and dried scraped material [12]. There was no evidence of other systemic or pulmonary TB in the current case after extensive radiologic investigations. Despite the high prevalence of TB in expatriates living in Qatar, to the best of our knowledge this is the first case of primary pituitary TB to be reported from this part of the world.
Conclusions
The diagnosis of primary pituitary TB can be very difficult even with the availability of sophisticated radiologic imaging. A high index of clinical suspicion, (particularly in countries with high TB prevalence) is thus of paramount importance to minimize unnecessary invasive procedures and surgical interventions. Although non-specific, the presence of thickened pituitary stalk on MRI scan should raise the possibility of pituitary TB as a differential diagnosis of pituitary pathology.
Acknowledgments
The authors are indebted to Dr. Muna Al-maslamani for her continuous support during the preparation of this manuscript. Special thanks to Dr. Khalid Salem from radiology department, Hamad General Hospital for providing and commenting on the pituitary MRI image.
Footnotes
Conflict of interest
None.
References:
- 1.World Health Organization (WHO) Global Tuberculosis Report 2016. Available from: URL: http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1. Accessed Dec.19, 2016.
- 2.Kulchavenya E. Extrapulmonary tuberculosis: Are statistical reports accurate? Ther Adv Infect Dis. 2014;2:61–70. doi: 10.1177/2049936114528173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khattab M, Khan F, Maslamani M, et al. Pulmonary and extra pulmonary tuberculosis in Qatar: A first retrospective population-based study. Advances in Infectious Diseases. 2015;5:148–53. [Google Scholar]
- 4.Letchworth TW. Tuberculoma of the pituitary body. Br Med J. 1924;1:1127. doi: 10.1136/bmj.1.3313.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rich AR, McCordock HA. The pathogenesis of tuberculous meningitis. Bulletin of the Johns Hopkins Hospital. 1933;52:5–37. [Google Scholar]
- 6.Bonifacio-Delgadillo D, Aburto-Murrieta Y, Salinas-Lara C, et al. Clinical presentation and magnetic resonance findings in sellar tuberculomas. Case Rep Med. 2014;2014:961913. doi: 10.1155/2014/961913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sunil K, Menon R, Goel N, et al. Pituitary tuberculosis. J Assoc Physicians India. 2007;55:453–56. [PubMed] [Google Scholar]
- 8.Srisukh S, Tanpaibule T, Kiertiburanakul S, et al. Pituitary tuberculoma: A consideration in the differential diagnosis in a patient manifesting with pituitary apoplexy-like syndrome. ID Cases. 2016;5:63–66. doi: 10.1016/j.idcr.2016.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pereira J, Vaz R, Carvalho D, Cruz C. Thickening of the pituitary stalk: A finding suggestive of intrasellar tuberculoma? Case report. Neurosurgery. 1995;36:1013–15. doi: 10.1227/00006123-199505000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Petrossians P, Delvenne P, Flandroy P, et al. An unusual pituitary pathology. J Clin Endocrinol Metab. 1998;83(10):3454–58. doi: 10.1210/jcem.83.10.5159. [DOI] [PubMed] [Google Scholar]
- 11.Dutta P, Pinaki, Bhansali A, et al. Suprasellar tubercular abscess presenting as panhypopituitarism: A common lesion in an uncommon site with a brief review of literature. Pituitary. 2006;9:73–77. doi: 10.1007/s11102-006-5420-2. [DOI] [PubMed] [Google Scholar]
- 12.Purohit M, Mustafa T. Laboratory diagnosis of extra-pulmonary tuberculosis (EPTB) in resource-constrained setting: State of the art, challenges and the need. J Clin Diagn Res. 2015;9:EE01–6. doi: 10.7860/JCDR/2015/12422.5792. [DOI] [PMC free article] [PubMed] [Google Scholar]


