Abstract
Aims:
Proliferative diabetic retinopathy (PDR) is associated with microvascular complications that cause biochemical changes in the human retina and alter the proteome of vitreous humor and aqueous humor (AH).
Methods:
Human vitreous humor and AH of PDR subjects were collected. Subjects who had surgery for epiretinal membrane or macular hole served as controls. Protein profiles were obtained and analyzed after running the samples on a liquid chromatography-mass spectrometry/mass spectrometry.
Results:
In vitreous humor, 16 unique proteins were noted in PDR patients, but not in controls. Those were associated mainly with coagulation, complement, and kallikrein-kinin systems. Under coagulation, fibrinogen and prothrombin proteins were more evident and may emphasize the importance of angiogenesis in the development of PDR. Vitreous proteins showed replicative presence in AH too. As for AH samples, we detected 10 proteins found in PDR patients, which were related to transport, coagulation, and inflammatory responses.
Conclusions:
We found 57 proteins in human vitreous and 39 proteins in AH. Identification of these proteins that are involved in various pathways will be helpful to understand diabetic retinopathy pathogenesis and to develop proteome as a biomarker for PDR.
Keywords: Vitreous and aqueous proteome, proliferative diabetic retinopathy, humans
Introduction
Proliferative diabetic retinopathy (PDR), the most frequent cause of blindness in industrialized countries, affects 30% to 50% of the individuals with diabetes.1 Proliferative diabetic retinopathy is accompanied with chronic inflammation, microvascular injury, edema, increased vascular permeability, and breakdown of the blood-retinal barrier.2 Microvascular and biochemical changes that are involved in the development of diabetic retinopathy (DR) leak various inflammatory proteins into the retina that further increase vascular permeability and ischemia.3 The physiologic and pathologic conditions of the retina affect the protein components in the vitreous due to its contiguity. Vitreous humor (VH) and aqueous humor (AH) exchange substances continuously with the blood through the capillary wall and also with retinal tissues through direct and indirect contact. Thus, vitreous and aqueous provide an opportunity to indirectly explore the pathophysiologic events that take place in the retina.
Although hyperglycemia has been suggested to be a major catalyst for the cellular changes in retina, intraocular biochemical factors/proteins that potentially contribute to pathogenesis are not yet clearly identified.3 Thus, identification of these proteins in the intraocular fluids such as PDR VH and AH will be useful in understanding the pathophysiologic mechanisms that are involved in the disease process.
Advanced stages of PDR involve neovascularization on the retina or the optic disk. These new abnormal blood vessels erupt through the surface of the retina and proliferate into the vitreous cavity of the eye, leading to vitreous hemorrhage that result in loss of vision.4 Several markers and biochemical pathways involved in inflammation, oxidative stress, angiogenesis, and cellular proliferation have been proposed to contribute to the pathogenesis of DR and is still an active area of research to improve our understanding of the mechanisms responsible for the disease and identification of newer therapeutic targets for its effective management.5
In this study, we examined vitreous and aqueous proteome in PDR subjects and compared it with the proteome profile detected in normal subjects without PDR in the hope of identifying a better focused marker(s) with potential for personalized management.
Methods
Characteristics of subjects
This pilot study involves 10 subjects after the approval of the Institutional Review Board at the University of Florida, Jacksonville. Among the 10 subjects, 5 had PDR and 5 served as controls. Samples were collected after their consent during vitrectomy procedure either for PDR or for epimacular membrane or macular hole (controls). Exclusion criteria include the evidence of acute or chronic infection, evidence of ocular trauma, prior pan retinal photocoagulation (PRP) or intraocular surgery, and the use of antimetabolites or immunosuppressant. The mean age of PDR subjects was 53.2 ± 13.3 years compared with 66.0 ± 3.6 years in control subjects.
Collection of vitreous samples
Samples were collected as per our earlier protocol by Balaiya et al.1 In brief, after anesthesia, surgery eye was prepared with 5% povidine iodine solution in the usual sterile manner. A 25-gauge trochar was inserted for 3-port parsplana vitrectomy and the vitrector was introduced. Using active cutting, vitreous was aspirated into a 1-mL tuberculin syringe prior to initiation of infusion procedure. Samples were immediately cooled in ice and stored at −80°C in a freezer.
Collection aqueous humor
Aqueous humor was collected as per our earlier protocol by Balaiya et al.1 In brief, surgery eyes were applied with topical 1% Topicaine gel solution, and samples were collected using a 30-gauge needle and a 1-mL tuberculin syringe. It minimizes the iris damage and the anterior lens capsule and prevents protein contamination in the sample. Furthermore, the samples were centrifuged to remove any cells and immediately stored at −80°C in a freezer.
Liquid chromatography-mass spectrometry/mass spectrometry
Preparation of samples
All PDR vitreous samples and control vitreous samples were pooled and prepared for liquid chromatography-mass spectrometry/mass spectrometry (LC-MS/MS). Control vitreous samples were pooled and prepared for LC-MS/MS. Similarly, PDR and control aqueous samples were pooled separately and prepared. As per our earlier protocol,1 samples were desalted and buffer exchanged with 50 mM of ammonium bicarbonate (pH, 7.8; Promega, Madison, WI, USA) using 3-kDa cut-off spin column (Millipore, Billerica, MA, USA). Samples were reduced further using 5 µL of dithiothreitol (200 mM of DTT; Promega) at 95°C for 5 minutes. After turning off the heat, samples were maintained in the heating unit for another 35 minutes. The free sulfhydryl groups on the cysteine residues were then alkylated with 4 µL of iodoacetic acid (1 M; Promega) at 25°C/45 minutes in the dark to irreversibly prevent the free sulfhydryls from reforming disulfide bonds. This reaction was further stopped by incubating the samples at 20 µL of DTT at 25°C/45 minutes.
Trypsin digestion
Further samples were digested using sequencing grade trypsin (pH, 7-9; Promega) in ammonium bicarbonate solution in a ratio of 1:100 to 1:20 (based on trypsin to protein) at 37°C overnight. The amount of trypsin varied depending on the protein concentration and desired speed of digestion. In addition, samples were again digested using sequencing grade endoproteinase Lys-C (Promega), overnight at 37°C.
Electrospray ionization-mass spectrometry/mass spectrometry
To further purify the enzymatically digested samples, a capillary trap (PepMap; LC Packings, Thermofisher scientific, west palm beach, FL, USA) was used to desalt them for 5 minutes with a flow rate of 3 µL/min of 0.1% v/v acetic acid. Furthermore, residual buffers and detergents were removed from the samples by loading them onto an LC Packings C18 PepMap nanoflow high-performance liquid chromatography (HPLC) column. The HPLC column’s elution gradient began at 3% solvent A, 97% solvent B and ended at 60% solvent A, 40% solvent B for 60 minutes for protein identification (solvent A consists of 0.1% v/v acetic acid, 3% v/v acetonitrile (ACN), and 96.9% v/v H2O; solvent B consists of 0.1% v/v acetic acid, 96.9% v/v ACN, and 3% v/v H2O).
For LC-MS/MS analysis, the purified peptide samples were loaded onto LTQ Orbitrap XL mass spectrometer (ThermoFisher Scientific, West Palm Beach, FL, USA). The ion spray voltage was fixed at 2200 V, and full MS scans were collected with a resolution of 60 000 in the orbitrap from 300 to 2000 m/z. Collision-induced dissociation fragmented the 10 most intense ions. Dynamic exclusion was fixed at 60 seconds.
Protein Search Algorithm
Mascot (version 2.4.0; Matrix Science, London, UK) was used to analyze all MS/MS samples. Its main function was searching International Protein Index human database, assuming the digestion enzyme trypsin. The parameters used for the Mascot search were a fragment ion mass tolerance of 0.8 Da and a parent ion tolerance of 10 ppm. The following were specified as variable modifications in Mascot: iodoacetamide derivative of cysteine, deamidation of asparagine and glutamine, and oxidation of methionine.
Data Analysis
Scaffold (version Scaffold-4; Proteome Software Inc., Portland, OR, USA) was used to confirm the identities of MS/MS-based peptide and protein identifications. To be accepted, peptide identifications had to reach 80% or greater probability. Protein identifications were accepted at greater than 80% probability and contain at least 2 identified unique peptides. To further interrogate the data in the hope of finding more specific protein(s) linked to PDR, we searched in our profile for proteins which satisfy the following conditions: (1) found in the vitreous and (2) found in the PDR patients, but not in controls.
Results
Vitreous proteome
In this study, peptide false discovery rate (FDR) was 1.7% (prophet) and protein FDR was 0.2% (prophet). In vitreous, a total of 26 proteins were noted in both PDR and control groups using mass spectrometry analysis (supplement table 1; Figure 1). Of these, 16 proteins were unique to PDR patients and were not detected in controls. We categorize these proteins based on their major functions.
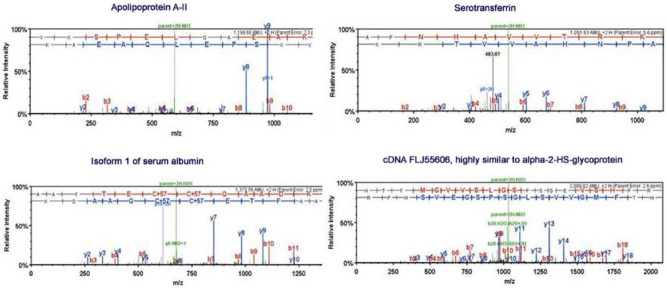
Figure 1.
Representative mass spectra of some of the identified proteins in this study.
Complement and coagulation cascade
We observed 15 proteins that are associated with coagulation, kinin-kallikrein, and complement system. Some proteins such as high-molecular-weight kininogen-1, isoform 1 of fibrinogen alpha chain, isoform gamma-B of fibrinogen gamma chain, fibrinogen beta chain, prothrombin, and histidine-rich glycoprotein were noted only in PDR vitreous. Kinins are responsible for dilating small blood vessels, triggering smooth muscle contraction, and increasing the permeability of vessel walls.6 Histidine-rich glycoprotein was found to be associated with antifibrinolytic activity. However, complement C4-A, complement C3, cDNA FLJ55673 highly similar to complement factor B, complement factor I, isoform 1 of clusterin, low molecular weight of kininogen-1, isoform 1 of alpha-1-antitrypsin (AAT), and alpha-2-macroglobulin were observed in both PDR and control vitreous. We found clusterin that functions as an integral component of the soluble C5b-9 complement complex assembled in the fluid phase of the complement proteins (C5b to C9) and vitronectin.7 Antithrombin III was noted in control vitreous, but not detected in PDR vitreous.
Inflammatory mediators and oxidative stress modulators
We noted acute phase inflammatory proteins such as alpha-1-acid glycoprotein1 and alpha-1-acid glycoprotein 2 in control vitreous. Clusterin, a participant in complement system, also participates in cell signaling, apoptosis, and cell proliferation; it can interfere with nuclear factor kappa B (NF-kB), PI3 kinase, or mitogen-activated protein (MAP) kinase signaling.8 Certain antioxidant proteins were found in PDR vitreous, which includes vitronectin and ceruloplasmin.
Visual cycle mediators
We found proteins that are associated with visual cycle and perception. Retinol-binding proteins (RBPs) are important in fatty acid transport and are essential for the maintenance of photoreceptors.9 Retinol-binding protein 3 (RBP3) was found exclusively in control vitreous. RBP3 is a soluble single-subunit glycoprotein that is synthesized and secreted by rod photoreceptor cells into the interphotoreceptor matrix.10 It is believed to transport all trans-retinol to the retinal pigment epithelium (RPE) and 11-cis-retinal from the RPE to the bleached photoreceptors, thus playing an important role in the visual cycle. A mutation in RBP3 gene (Asp1080Asn) has been linked to autosomal recessive retinitis pigmentosa.11 We also found RBP4 which is a specific carrier for retinol in blood. It inhibits insulin signaling in muscle and adipose tissues and causes systemic insulin resistance.12 We noted that isoform 1 of endothelial growth factor containing fibulin-like extracellular matrix (ECM) protein 1 is involved in visual perception and is also associated with age-related macular degeneration.13 We noted the presence of photoreceptor-specific protein retbindin (isoform 2) in PDR vitreous.
Transporter proteins
Many of the transporter proteins were detected in both control and PDR vitreous, including serotransferrin, apolipoprotein A-1, apolipoprotein A-II, apolipoprotein A-IV, hemopexin, and vitamin D–binding protein. Serotransferrin participates in iron transport and apolipoproteins participate in the transport of cholesterol.13 Hemopexin, a primary carrier of plasma heme, was expressed in neuroretina, RPE, and glial cells.14 Transthyretin was found only in control vitreous but not in PDR vitreous. It transports thyroxine and retinol through its association with RBP in the blood and cerebrospinal fluid (Table 2).15
Table 2.
Vitreous proteins that participate in complement, coagulation, and kinin-kallikrein system.
| S. no. | Name of the protein | International Protein Index (IPI) | Sequence coverage—control (%) | Sequence coverage—PDR (%) |
|---|---|---|---|---|
| 1 | Complement C4-A | IPI00032258 | 7.2 | 7.3 |
| 2 | Complement C3 | IPI00783987 | 5.1 | 4.1 |
| 3 | cDNA FLJ55673, highly similar to complement factor B | IPI00019591 | 4 | 8.5 |
| 4 | Complement factor I | IPI00291867 | 0 | 6.9 |
| 5 | Clusterin | IPI00291262 | 39 | 26 |
| Coagulation system | ||||
| 6 | Isoform 1 of alpha-1-antitrypsin | IPI00553177 | 48 | 5.7 |
| 7 | Isoform 1 of fibrinogen alpha chain | IPI00021885 | 0 | 29 |
| 8 | Fibrinogen beta chain | IPI00298497 | 0 | 18 |
| 9 | Alpha-2-macroglobulin | IPI00478003 | 3 | 1.6 |
| 10 | Prothrombin | IPI00019568 | 0 | 8.5 |
| 11 | Isoform gamma-B of fibrinogen gamma chain | IPI00021891 | 0 | 12 |
| 12 | Antithrombin III | IPI00032179 | 6.2 | 0 |
| 13 | Histidine-rich glycoprotein | IPI00022371 | 0 | 9.9 |
| Kinin-kallikrein system | ||||
| 14 | Isoform LMW of kininogen-1 | IPI00215894 | 6.1 | 14 |
| 15 | Isoform HMW of kininogen-1 | IPI00032328 | 0 | 4.7 |
Abbreviations: HMW, high molecular weight; LMW, low molecular weight; PDR, proliferative diabetic retinopathy.
Aqueous proteome—known proteins in the aqueous
A total of 39 proteins were observed in aqueous (Table 3). All of these proteins were reported in earlier literature except putative uncharacterized proteins and retinol-binding protein 4. Among them, 10 proteins were noted in PDR aqueous, but not in control aqueous: apolipoprotein A-1, apolipoprotein A-II, apolipoprotein A-IV, isoform 1 of fibrinogen alpha chain, fibrinogen beta chain, cluster of alpha-1-acid glycoprotein 1, alpha-1-acid glycoprotein 1, ceruloplasmin, alpha-2-macroglobulin, and similar to Ig kappa chain V-III region variable (VG) precursor. However, 4 proteins were present in control aqueous only, such as zinc-alpha-2-glycoprotein, histidine-rich glycoprotein, insulin-like growth factor–binding protein 7, and protein AMBP.
Table 3.
Proteins identified from aqueous of control and PDR subjects.
| S. no. | Name of the protein | Accession number—International Protein Index (IPI) | Biological functions | Sequence coverage (%) | |
|---|---|---|---|---|---|
| Control | PDR | ||||
| 1 | Isoform 1 of serum albumin | IPI00745872 | Transport | 77 | 91 |
| 2 | Serotransferrin | IPI00022463 | Transport | 54 | 71 |
| 3 | Isoform 1 of clusterin | IPI00291262 | Immune response | 6.90 | 17 |
| 4 | Cluster of FLJ00385 protein (fragment) | IPI00168728 | 24 | 43 | |
| 5 | Putative uncharacterized protein DKFZp686P15220 | IPI00645363 | 24 | 43 | |
| 6 | Similar to hepatitis B virus receptor-binding protein | IPI00977788 | 0 | 26 | |
| 7 | Isoform 1 of alpha-1-antitrypsin | IPI00553177 | Coagulation | 12 | 18 |
| 8 | cDNA FLJ55606, highly similar to alpha-2-HS-glycoprotein | IPI00022431 | Binding, intercellular | 11 | 16 |
| 9 | Haptoglobin | IPI00641737 | Binding | 18 | 39 |
| 10 | Prostaglandin-H2 d-isomerase | IPI00013179 | Biosynthesis, transport | 38 | 34 |
| 11 | Vitamin D–binding protein isoform 1 precursor | IPI00555812 | Transport and cargo protein | 15 | 30 |
| 12 | Apolipoprotein A-I | IPI00021841 | Transport | 0 | 21 |
| 13 | Isoform 1 of fibrinogen alpha chain | IPI00021885 | Coagulation | 0 | 2.20 |
| 14 | Beta-2-glycoprotein 1 | IPI00298828 | 11 | 22 | |
| 15 | Apolipoprotein A-II | IPI00021854 | Transport | 0 | 72 |
| 16 | Isoform 1 of alpha-1B-glycoprotein | IPI00022895 | 22 | 36 | |
| 17 | Cluster of cDNA FLJ52545, highly similar to Dickkopf-related protein 3 (IPI00002714) | IPI00002714 | Signaling | 12 | 9.10 |
| 18 | Uncharacterized protein | IPI00971192 | 12 | 9.10 | |
| 19 | Pigment epithelium–derived factor | IPI00006114 | Cell proliferation, antiangiogenic | 5.00 | 11 |
| 20 | Cystatin-C | IPI00032293 | Protease inhibitor, binding | 40 | 25 |
| 21 | Complement C4-A | IPI00032258 | Immune response | 2.50 | 5.70 |
| 22 | Hemopexin | IPI00022488 | Transport | 13 | 19 |
| 23 | Complement C3 (fragment) | IPI00783987 | Immune response | 1.9 | 4.7 |
| 24 | cDNA FLJ55673, highly similar to complement factor B | IPI00019591 | Immune response | 3.3 | 3.50 |
| 25 | Fibrinogen beta chain | IPI00298497 | Coagulation | 0 | 5.30 |
| 26 | Apolipoprotein A-IV | IPI00304273 | Transport | 0 | 6.60 |
| 27 | Zinc-alpha-2-glycoprotein | IPI00166729 | Fatty acid binding, ribonuclease activity | 9.70 | 0 |
| 28 | Alpha-1-acid glycoprotein 1 | IPI00022429 | Inflammatory protein | 0 | 12 |
| 29 | Isoform LMW of kininogen-1 | IPI00215894 | Kinin-kallikrein system | 9.10 | 12 |
| 30 | Ceruloplasmin | IPI00017601 | Transport, binding | 0 | 6.30 |
| 31 | Histidine-rich glycoprotein | IPI00022371 | Antifibrinolytic activity | 9.70 | 0 |
| 32 | Transthyretin | IPI00022432 | Transport | 14 | 41 |
| 33 | Alpha-2-macroglobulin | IPI00478003 | Coagulation | 0 | 1.60 |
| 34 | Retinol-binding protein 4 | IPI00022420 | Visual cycle | 9.50 | 9.50 |
| 35 | Ig kappa chain V-III region WOL | IPI00387118 | Binding | 22 | 25 |
| 36 | Insulin-like growth factor–binding protein 7 | IPI00016915 | Cell adhesion | 17 | 0 |
| 37 | Similar to Ig kappa chain V-III region VG precursor | IPI00977405 | 0 | 30 | |
| 38 | Protein AMBP | IPI00022426 | Protease inhibitor, binding | 7.70 | 0 |
| 39 | Myosin-reactive immunoglobulin kappa chain variable region (fragment) | IPI00384401 | 25 | 31 | |
Abbreviations: AMBP, alpha-1-microglobulin/bikunin precursor; LMW, low molecular weight; PDR, proliferative diabetic retinopathy; PEDF, pigment epithelium–derived factor.
Discussion
The pathogenesis of diabetes is multifactorial and comprises a complex network of pathophysiologic events with metabolic and hemodynamic alterations.16
Prolonged hyperglycemia, in association with co-existing dyslipidemia, hypertension and hyperinsulinemia, is the key determinant in the pathophysiology of diabetic complications. Sustained hyperglycemia may induce several biochemical changes including, but not limited to, increased nonenzymatic glycation, oxidation toxicity, protein kinase C (PKC) activation, induction of prothrombotic status, activation of cytokine-mediated inflammation, and activation of sympathoadrenal system.17
These biochemical changes ultimately lead to vascular structural changes, including capillary basement membrane thickening, interstitial fibrosis, and myocyte hypertrophy and necrosis.18 However, the molecular pathogenesis of DR is relatively limited. The proteomic analysis of human vitreous and aqueous samples is difficult due to the minimal amount of proteins present. This difficulty was overcome by subjecting the samples to multiple fractionation techniques, including in solution digestion. Vitreous and aqueous protein profiles of PDR subjects were completely different from those of control subjects without DR.19,20 In this study, we detected 16 proteins exclusively in the vitreous of PDR subjects but not in vitreous of controls, whereas in the aqueous we detected 10 proteins exclusively in the PDR subjects but not in aqueous of controls.
Among proteins unique to PDR patients, 7 (4 in the vitreous and 3 in the aqueous) were directly related to coagulation. Diabetes is considered to be a hypercoagulable state, and many clotting factors are elevated in diabetic patients, including prothrombin activation fragment, factor VII, factor VIII, factor XI, and factor XII.21 Activation of these cascades can initiate thrombosis, leukostasis, and inflammation that are involved in vascular lesions. We also detected various isoforms of fibrinogen molecules, as well as alpha-2 macroglobulin in PDR vitreous. The involvement of fibrinogen is of particular importance. Previous studies found that plasma fibrinogen levels were significantly higher in diabetics with retinopathy. High plasma fibrinogen levels contribute significantly and independently to the development of DR.22 The structure of fibrin is an important determinant of angiogenesis which in turn plays a major role in the development of PDR.23 In addition, we found that antithrombin III (inhibitor of coagulation) was detected in control vitreous, but not in PDR vitreous, consistent with a hypercoagulable environment for PDR vitreous. Interestingly, these findings were in discrepancy with other studies showing that antithrombin III had higher expression in PDR versus control vitreous.19 We believe that the underlying cause for this discrepancy could be related to sample collection at different clinical stages of PDR (vasoproliferative vs fibrotic), which warrants further evaluation.
In addition to coagulation proteins, we detected proteins related to inflammation and inflammatory responses. Inflammation is an important pathophysiologic mechanism in the development and progression of diabetes mellitus (DM). Activation of proinflammatory modulators NF-kB and PKC is well documented in diabetic patients in several studies,18,24 and inflammatory mediators have been suggested as therapeutic targets for DM. In this study, proinflammatory proteins (complement factors and various isoforms of glycoproteins) were exclusively expressed in PDR vitreous. The presence of kininogen in PDR group explains its role in proinflammatory plasma kallikrein pathway in the pathogenesis of DR. However, the inhibition of this system in rodent models reduces retinal leakage induced by diabetes and hypertension.25 Clusterin is another inflammatory regulator of interest. It is a heterodimeric glycoprotein found in most human tissues and was previously reported as an antipermeability factor.26 Its expression was reported to be elevated in the inner nuclear and ganglion cell layers of retinas in streptozotocin-induced diabetic rats.27 In a mouse model of DR, clusterin reduced the leakage from vessels in the diabetic retina, which was accompanied by the restoration of the expression of tight junction proteins.8 These suggest that clusterin may play an important role in the prevention of diabetes-induced blood-retinal barrier breakdown. Moreover, antisense oligonucleotides to clusterin were found to have an antiangiogenic effect in vitro.27 But in our study, we detected the presence of clusterin in both PDR and control samples. Another protein found in this study that has anti-inflammatory effect was isoform 1 of AAT level. Alpha-1-antitrypsin is currently evaluated in clinical trials for type 1 diabetes because it was reported to exert anti-inflammatory and tissue-protective effects independent of protease inhibition, which was believed to be protective in diabetic pathogenesis.28
Interestingly, we detected RBP in control vitreous, but not in PDR vitreous. Downregulation of interstitial retinol-binding protein (IRBP) was reported to compromise the neuroprotection against neurotoxic factors involved in neurodegeneration.29 The absence of RBP3 protein in PDR vitreous may represent the neurodegeneration and dysfunction of this protein in visual cycle.
Pigment epithelium–derived factor (PEDF) is a secreted glycoprotein belonging to a group of serine protease inhibitors with antiangiogenic activities.30 Pigment epithelium–derived factor is a multifunctional protein, which may target multiple pathways exerting neurotropic, neuroprotective, antiangiogenic, antivasopermeability, anti-inflammation, antithrombogenic, and antioxidative effects in DR.30 Pigment epithelium–derived factor concentration was found to be significantly lower in the vitreous fluids of subjects with PDR.31 In concordance with these studies, we observed PEDF exclusively in control vitreous, but not in PDR vitreous. In contrast, Gao et al19 reported that PEDF protein level was higher in PDR vitreous compared with no PDR or normal vitreous samples.
We observed several ECM proteins and adhesion proteins in the vitreous. We detected transthyrectin, isoform 1 of collagen alpha-1(II) chain, collagen alpha-2(IX) chain, collagen alpha-3(IX) chain, isoform B of collagen alpha-1(XI) chain, and matrix-binding proteins such as opticin only in control vitreous. Expression of transthyrectin was low in the vitreous of diabetic macular edema patient,14 suggesting a protective role of this transport protein in DR. Opticin, a member of the small leucine-rich repeat protein family, is expressed in the retina, iris, VH, non-pigmented epithelium of the ciliary body, sclera, optic nerve, choroid, uveal tract, and lens.10 It is associated with age-related macular degeneration and retinitis pigmentosa,20 but their role in DR is not yet known.
Most of the proteins in vitreous were simultaneously observed in our aqueous proteome. This observation was similar to earlier reports.32,33 The abnormal protein expression profiles in AH of PDR patients were likely secondary to leakage of proteins from the damaged retina and retinal blood vessels to aqueous through the VH to AH barrier. In addition to this VH-AH pathway, retinal proteins can also leak into cilia-retina circulation through the disturbed blood-retinal and blood-aqueous barrier.34 In our earlier study,35 we analyzed the aqueous proteome in subjects who had bevacizumab injection for various ocular disorders before and after injection using Luminex xMap. Postinjection samples showed increased levels of isoform 1 of AAT and complement C3 proteins, whereas haptoglobin (hemoglobin-binding protein) and apolipoprotein A-1 protein (transporter) levels were decreased. These observations suggest that bevacizumab, a combinational therapy along with a laser treatment in PDR, not only neutralizes vascular endothelial growth factor but also normalizes the intraocular pathologic environment. Thus, AH proteins that represent the pathophysiologic environment of the retina can also serve as biomarkers for disease conditions such as PDR and recognize them as biotargets for clinical research.36 However, there are certain limitations associated with this study. The observation of less number of proteins in this study compared with previous published literature may be due to the collection of a small volume of samples and the collection at different clinical stages of PDR. Less sample size and lack of quantitative information need to be eliminated by the further detailed study.
Conclusions
In conclusion, we identified 57 proteins in human vitreous and 39 proteins in aqueous that were present exclusively either in PDR or in control groups. Many of the proteins participate in multiple cascades, including coagulation, complement, and kinin-kallikrein systems. Some of the proteins participate in biological processes that include intracellular proteins and ECM proteins. Our findings suggest that both vitreous and aqueous proteome can serve as biomarkers for PDR conditions, and further understanding of each protein at molecular level may provide better insights for DR pathogenesis and novel therapeutic targets for DR (Table 1).
Table 1.
Proteins identified from vitreous of control and PDR subjects.
| Accession number—International Protein Index (IPI) | Name of the proteins in PDR vitreous only | Biological functions |
|---|---|---|
| IPI00021885 | Isoform 1 of fibrinogen alpha chain | Coagulation |
| IPI00298497 | Fibrinogen beta chain | Coagulation |
| IPI00166729 | Zinc-alpha-2-glycoprotein | Associated with insulin resistance, lipid metabolism |
| IPI00032328 | Isoform high molecular weight of kininogen-1 | Kinin-kallikrein system, inflammation, angiogenesis |
| IPI00022371 | Histidine-rich glycoprotein | Antifibrinolytic activity |
| IPI00654755 | Hemoglobin subunit beta | Binding |
| IPI00291867 | Complement factor I | Complement system |
| IPI00410714 | Hemoglobin subunit alpha | Transport |
| IPI00014048 | Ribonuclease pancreatic | Enzyme, involved in binding |
| IPI00029658 | Isoform 1 of EGF-containing fibulin-like extracellular matrix | Involved in visual perception, binding, signaling |
| IPI00019568 | Prothrombin | Coagulation (thrombotic risk) |
| IPI00022426 | Protein AMBP | Protease inhibitor, binding activity |
| IPI00298971 | Vitronectin | Coagulation cascade |
| IPI00027765 | Isoform 2 of retbindin | Photoreceptor-specific protein |
| IPI00021891 | Isoform gamma-B of fibrinogen gamma chain | Coagulation, transport, signaling |
| IPI00006608 | Isoform APP770 of amyloid beta A4 protein | Cytoskeleton, binding, transport |
| Accession number—IPI | Name of proteins in control vitreous only | Biological functions |
| IPI00006114 | PEDF | Antiangiogenic, cell proliferation |
| IPI00022337 | Retinol-binding protein 3 | Fatty acid transport, Visual cycle |
| IPI00022429 | Alpha-1-acid glycoprotein 1 | Acute phase inflammatory reactant |
| IPI00020091 | Alpha-1-acid glycoprotein 2 | Acute phase inflammatory reactant |
| IPI00002678 | Opticin | Receptor, adhesion, signaling |
| IPI00022432 | Transthyretin | Transport, signaling |
| IPI00289999 | Collagen alpha-3(IX) chain | Peptide hormone, transport, binding, signaling, intercellular |
| IPI00186460 | Isoform 1 of collagen alpha-1(II) chain | Peptide hormone, transport, binding, signaling, intercellular |
| IPI00019088 | Collagen alpha-2(IX) chain | Peptide hormone, transport, binding, signaling, intercellular |
| IPI00218539 | Isoform B of collagen alpha-1(XI) chain | Peptide hormone, transport, binding, signaling, intercellular |
| IPI00031030 | Isoform 1 of amyloid-like protein 2 | Involved in binding and signaling |
| IPI00021000 | Isoform A of osteopontin | Immunomodulation, angiogenesis |
| IPI00387118 | Ig kappa chain V-III region WOL | Binding |
| IPI00011229 | Cathepsin D | Signaling, proteases |
| IPI00032179 | Antithrombin III | Coagulation system |
| Accession number—IPI | Proteins present in both PDR and control vitreous | Biological functions |
| IPI00745872 | Isoform 1 of serum albumin | Transport |
| IPI00022463 | Serotransferrin | Transport |
| IPI00291262 | Isoform 1 of clusterin | Immune response |
| IPI00168728 | Cluster of FLJ00385 protein | |
| IPI00553177 | Isoform1 of alpha-1-antitrypsin | Coagulation |
| IPI00645363 | Putative uncharacterized protein DKFZp686P15220 | |
| IPI00022431 | cDNA FLJ55606, highly similar to alpha-2-HS-glycoprotein | Intercellular, binding |
| IPI00641737 | Haptoglobin | Binding |
| IPI00013179 | Prostaglandin-H2 d-isomerase | Biosynthesis, transport |
| IPI00555812 | Vitamin D–binding protein isoform 1 precursor | Transport and cargo |
| IPI00021841 | Apolipoprotein A-I | Transport |
| IPI00298828 | Beta-2-glycoprotein 1 | |
| IPI00021854 | Apolipoprotein A-II | Transport |
| IPI00022895 | Isoform 1 of alpha-1B-glycoprotein | Receptor, signaling |
| IPI00002714 | cDNA FLJ52545, highly similar to Dickkopf-related protein 3 | Signaling |
| IPI00304273 | Apolipoprotein A-IV | Transport |
| IPI00021842 | Apolipoprotein E | Transport |
| IPI00032293 | Cystatin-C | Protease inhibitor, binding |
| IPI00032258 | Complement C4-A | Immune response |
| IPI00022488 | Hemopexin | Transport |
| IPI00783987 | Complement C3 | Immune response |
| IPI00019591 | cDNA FLJ55673, highly similar to complement factor B | Immune response |
| IPI00215894 | Isoform LMW of kininogen-1 | Kallikrein-kinin system |
| IPI00017601 | Ceruloplasmin | Transport, binding |
| IPI00478003 | Alpha-2-macroglobulin | Coagulation |
| IPI00026314 | Isoform 1 of gelsolin | Cytoskeleton, binding, intercellular |
Abbreviations: AMBP, alpha-1-microglobulin/bikunin precursor; EGF, epidermal growth factor; LMW, low molecular weight; PDR, proliferative diabetic retinopathy; PEDF, pigment epithelium–derived factor.
Supplementary Material
Footnotes
Peer Review:Nine peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1818 words, excluding any confidential comments to the academic editor.
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: SB was supported in part by a grant from NIH/NCATS-CTSI to University of Florida (UL1 TR000064) for this work.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: SB participated in technical lab work and manuscript writing, ZZ wrote the clinical part of the manuscript, and KVC participated in revision and final approval of the manuscript.
References
- 1. Balaiya S, Grant MB, Priluck J, Chalam KV. Growth factors/chemokines in diabetic vitreous and aqueous alter the function of bone marrow-derived progenitor (CD34+) cells in humans. Am J Physiol Endocrinol Metab. 2014;307:E695–E702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tomic M, Ljubic S, Kastelan S. The role of inflammation and endothelial dysfunction in the pathogenesis of diabetic retinopathy. Coll Antropol. 2013;37(suppl. 1):51–57. [PubMed] [Google Scholar]
- 3. El-Asrar AM. Role of inflammation in the pathogenesis of diabetic retinopathy. Middle East Afr J Ophthalmol. 2012;19:70–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Frank RN. Treating diabetic retinopathy by inhibiting growth factor pathways. Curr Opin Investig Drugs. 2009;10:327–335. [PubMed] [Google Scholar]
- 5. Tarr JM, Kaul K, Chopra M, Kohner EM, Chibber R. Pathophysiology of diabetic retinopathy. ISRN Ophthalmol. 2013;2013:Article ID 343560 (13 pp.). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eisen V. Kinins in physiology and pathology. Trends Pharmacol Sci. 1979-1980;1:212–215. [Google Scholar]
- 7. French LE, Wohlwend A, Sappino AP, Tschopp J, Schifferli JA. Human clusterin gene expression is confined to surviving cells during in vitro programmed cell death. J Clin Invest. 1994;93:877–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kim JH, Jun HO, Yu YS, et al. Protective effect of clusterin from oxidative stress-induced apoptosis in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 2010;51:561–566. [DOI] [PubMed] [Google Scholar]
- 9. Gonzalez-Fernandez F. Interphotoreceptor retinoid-binding protein—an old gene for new eyes. Vision Res. 2003;43:3021–3036. [DOI] [PubMed] [Google Scholar]
- 10. Ramesh S, Bonshek RE, Bishop PN. Immunolocalisation of opticin in the human eye. Br J Ophthalmol. 2004;88:697–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. den Hollander AI, McGee TL, Ziviello C, et al. A homozygous missense mutation in the IRBP gene (RBP3) associated with autosomal recessive retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2009;50:1864–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Farjo KM, Farjo RA, Halsey S, Moiseyev G, Ma JX. Retinol-binding protein 4 induces inflammation in human endothelial cells by an NADPH oxidase- and nuclear factor kappa B-dependent and retinol-independent mechanism. Mol Cell Biol. 2012;32:5103–5115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Skeie JM, Brown EN, Martinez HD, et al. Proteomic analysis of vitreous biopsy techniques. Retina. 2012;32:2141–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hernandez C, Garcia-Ramirez M, Simo R. Overexpression of hemopexin in the diabetic eye: a new pathogenic candidate for diabetic macular edema. Diabetes Care. 2013;36:2815–2821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zheng W, Lu YM, Lu GY, Zhao Q, Cheung O, Blaner WS. Transthyretin, thyroxine, and retinol-binding protein in human cerebrospinal fluid: effect of lead exposure. Toxicol Sci. 2001;61:107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cade WT. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther. 2008;88:1322–1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Goldstein DS. Adrenal responses to stress. Cell Mol Neurobiol. 2010;30:1433–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Farhangkhoee H, Khan ZA, Kaur H, Xin X, Chen S, Chakrabarti S. Vascular endothelial dysfunction in diabetic cardiomyopathy: pathogenesis and potential treatment targets. Pharmacol Ther. 2006;111:384–399. [DOI] [PubMed] [Google Scholar]
- 19. Gao BB, Chen X, Timothy N, Aiello LP, Feener EP. Characterization of the vitreous proteome in diabetes without diabetic retinopathy and diabetes with proliferative diabetic retinopathy. J Proteome Res. 2008;7:2516–2525. [DOI] [PubMed] [Google Scholar]
- 20. Murthy KR, Goel R, Subbannayya Y, et al. Proteomic analysis of human vitreous humor. Clin Proteomics. 2014;11:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Carr ME, Jr, Muller CT. Treatment of massive pulmonary embolism in a soldier in Kosovo: the potential value of cardiopulmonary resuscitation and fibrinolytic therapy. Mil Med. 2011;176:1453–1456. [DOI] [PubMed] [Google Scholar]
- 22. Azad N, Agrawal L, Emanuele NV, et al. Association of PAI-1 and fibrinogen with diabetic retinopathy in the Veterans Affairs Diabetes Trial (VADT). Diabetes Care. 2014;37:501–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kolodziejczyk J, Ponczek MB. The role of fibrinogen, fibrin and fibrin(ogen) degradation products (FDPS) in tumor progression. Contemp Oncol (Pozn). 2013;17:113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Krentz AJ, Clough G, Byrne CD. Interactions between microvascular and macrovascular disease in diabetes: pathophysiology and therapeutic implications. Diabetes Obes Metab. 2007;9:781–791. [DOI] [PubMed] [Google Scholar]
- 25. Feener EP. Plasma kallikrein and diabetic macular edema. Curr Diab Rep. 2010;10:270–275. [DOI] [PubMed] [Google Scholar]
- 26. Kim JH, Yu YS, Min BH, Kim KW. Protective effect of clusterin on blood-retinal barrier breakdown in diabetic retinopathy. Invest Ophthalmol Vis Sci. 2010;51:1659–1665. [DOI] [PubMed] [Google Scholar]
- 27. Jackson JK, Gleave ME, Gleave J, Burt HM. The inhibition of angiogenesis by antisense oligonucleotides to clusterin. Angiogenesis. 2005;8:229–238. [DOI] [PubMed] [Google Scholar]
- 28. Lewis EC. Expanding the clinical indications for α(1)-antitrypsin therapy. Mol Med. 2012;18:957–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Simo R, Hernandez C. Neurodegeneration in the diabetic eye: new insights and therapeutic perspectives. Trends Endocrinol Metab. 2014;25:23–33. [DOI] [PubMed] [Google Scholar]
- 30. Marciniak K, Butwicka A, Nowak JZ. [PEDF: an endogenous factor displaying potent neuroprotective, neurotrophic, and antiangiogenic activity]. Postepy Hig Med Dosw (Online). 2006;60:387–396. [PubMed] [Google Scholar]
- 31. Al-Latayfeh M, Silva PS, Sun JK, Aiello LP. Antiangiogenic therapy for ischemic retinopathies. Cold Spring Harb Perspect Med. 2012;2:a006411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Funatsu H, Yamashita H, Nakanishi Y, Hori S. Angiotensin II and vascular endothelial growth factor in the vitreous fluid of patients with proliferative diabetic retinopathy. Br J Ophthalmol. 2002;86:311–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jonas JB. Intravitreal triamcinolone acetonide for diabetic retinopathy. Dev Ophthalmol. 2007;39:96–110. [DOI] [PubMed] [Google Scholar]
- 34. Freddo TF. A contemporary concept of the blood-aqueous barrier. Prog Retin Eye Res. 2013;32:181–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sharma RK, Chalam KV. In vitro evaluation of bevacizumab toxicity on a retinal ganglion cell line. Acta Ophthalmol. 2009;87:618–622. [DOI] [PubMed] [Google Scholar]
- 36. Rocha AS, Santos FM, Monteiro JP, et al. Trends in proteomic analysis of human vitreous humor samples. Electrophoresis. 2014;35:2495–2508. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.