Abstract
Background
We addressed the impact of patient education followed by frequent visits on compliance with positive airway pressure (PAP) treatment in patients with obstructive sleep apnea (OSA) in a Turkish sleep clinic cohort.
Material/Methods
This single-center, randomized, controlled study was conducted in Istanbul, Turkey between June 2014 and April 2015. Among 115 eligible OSA patients (mean age 51.0±9.3 years; 75.5% men), 63 were randomized to standard support (SS) group (general information about OSA and PAP treatment at baseline), and 52 to educational support (ES) group (additional polysomnography chart viewing from both diagnostic and titration nights). All patients were scheduled to five PAP control visits between two weeks and six months after the PAP prescription. Primary outcome was the PAP compliance (4 hours/night for 70% of all the nights) at the last visit.
Results
Average PAP usage was 4.2±2.5 hours/night in the SS group, and 5.2±2.1 hours/night in the ES group (p=0.027). PAP compliance was achieved among 68.3% in the SS group, and 86.5% in the ES group (p=0.021). In a multivariate analysis, ES strategy followed by frequent visits predicted PAP compliance (odds ratio [OR] 3.6, 95% confidence interval [CI] 1.2–10.6; p=0.020). Other predictors were obesity (OR 3.4, 95% CI 1.2–9.7; p=0.019) and severe OSA (apnea-hypopnea index ≥30/hour) at baseline (OR 4.7, 95% CI 1.2–17.6; p=0.023). Primary school education level was inversely related with PAP compliance (OR 0.3, 95% CI 0.1–0.9; p=0.036).
Conclusions
Patient education with polysomnography chart view followed by frequent visits increased long-term compliance with PAP treatment.
MeSH Keywords: Compliance; Patient Education as Topic; Sleep Apnea, Obstructive
Background
Obstructive sleep apnea (OSA) is a common disorder with repetitive upper airway obstruction during sleep resulting in intermittent hypoxia and sleep fragmentation. When untreated, it may cause daytime sleepiness, fatigue, and poor quality of life [1]. OSA is also associated with increased risk for traffic accidents [2] and cardiovascular morbidity [3]. Positive airway pressure (PAP) is the first-line treatment for OSA; it reduces obstructive events, daytime sleepiness and improves quality of life, especially in those with excessive daytime sleepiness [4]. In literature and clinical practice, 4 hours of nightly PAP usage for 70% of the nights is considered adequate adherence to therapy, corresponding to an average PAP usage of 2.8 hours every night [5]. However, despite the benefits of PAP treatment, overall acceptance and adherence rates are not fully optimized as the estimated range has been reported to be between 46–80% [6,7]. It has been argued that some patients do not consider OSA as a serious health problem [8]. In this context, several educational [9,10] and intensive support strategies [11] have been proposed. For instance, a recent study reported that having patients view the polysomnography (PSG) charts as a part of an educational strategy may improve long-term PAP adherence [12]. Less is known regarding the PAP adherence rates in Turkey. A recent report demonstrated lower than expected adherence rates in OSA patients, of whom only 38% attended follow-up visits [13]. To date, there is no study addressing the impact of implementation of any of the suggested educational strategies in Turkey.
In our current study, we primarily addressed whether an intensified patient education strategy which included viewing PSG charts followed by frequent follow-up would improve the long-term compliance rate of patients with OSA in a Turkish sleep clinic cohort. We also addressed the predictors of adequate PAP adherence in this population.
Material and Methods
This single-center, prospective, randomized, controlled, parallel group study was approved by the institutional review board of the Department of Clinical Investigations at the Lütfi Kırdar Education and Research Hospital (approval nr 89513307/1009/309; June 03, 2014), and was carried out in accordance with the principles of the Helsinki Declaration. All participants gave written informed consent prior to participation in the study. The trial was registered retrospectively with ClinicalTrials.gov (NCT02756299).
Study population
We recruited 490 consecutive adult patients (≥18 years old) with newly diagnosed OSA (apnea-hypopnea index ≥5 events/hour), who were free from upper airway obstructions (evaluated by the ear, nose and throat (ENT) specialist), and were offered PAP treatment at the Süreyyapaşa Chest Diseases and Thoracic Surgery Training and Research Hospital in Istanbul between June 12, 2014 and April 14, 2015 (Figure 1). Fifteen patients who were not interested in PAP treatment were excluded. Among the 475 patients undergoing a PAP titration night, 360 were further excluded (280 were living outside Istanbul, 15 were unable to come to follow-up, and 65 were not interested in the study). The remaining 115 patients were randomly 1: 1 assigned to standard support (SS) group (general information about OSA and PAP treatment at baseline), or to educational support (ES) group (additional polysomnography chart viewing from both diagnostic and titration nights). Participants were randomly assigned in order of appearance (random number table: SS/ES) with exception for patients scheduled for weekend treatment, who were included in the SS group.
Figure 1.
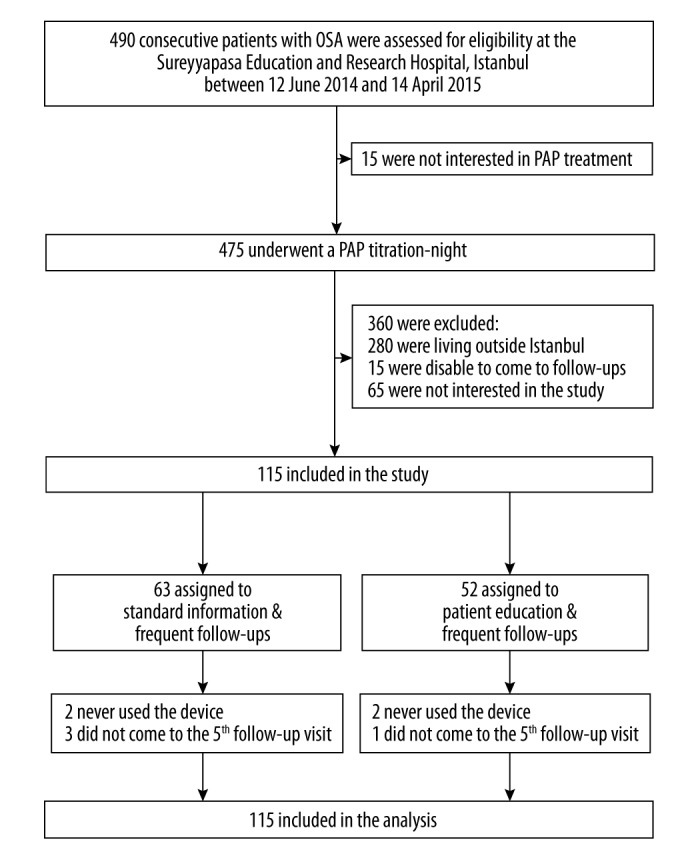
Consort flow diagram of patients through the study.
Baseline characteristics
The baseline anthropometrics and medical history in the study population were obtained from medical records. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2) and obesity was defined as a BMI ≥30 kg/m2) [2,14]. The educational status (primary school [basic level school education for 4–5 years], college, or high-school) was documented, and information regarding known concomitant diseases at baseline was based on the self-reported and/or physician diagnosed conditions. Epworth sleepiness scale (ESS) score was obtained for evaluation of the subjective daytime sleepiness, and categorized as non-sleepiness (ESS <8), mild sleepiness (ESS 8–10), moderate sleepiness (ESS 11–14), and severe sleepiness (ESS ≥15) at baseline [2].
Study design
All participants underwent a standard diagnostic overnight PSG (Comet Grass; Astro-Med, Inc., West Warwick, RI, USA). The PSG recordings included sleep monitoring through three-channel electroencephalography, two-channel electrooculography, one-channel submental electromyography, oxygen saturation via an oximeter probe, respiratory movements via chest and abdominal belts, nasal pressure via pressure sensor, thermistor, electrocardiography, and leg movements via tibial surface electrodes. Sleep stages as well as respiratory parameters were scored according to the criteria of American Academy of Sleep Medicine (AASM) from 2012 [15]; apnea was defined as a reduction in airflow of at least 90% for at least 10 seconds, and hypopnea was defined as a reduction in airflow of at least 30% accompanied by at least a 3% desaturation in the preceding 30 seconds, and a reduction in chest wall movement and/or arousal. The apnea-hypopnea index (AHI) referred to the average number of apneas and hypopneas per hour of sleep. OSA was defined as an AHI of at least 5 events/hour [15], and the severity of OSA was categorized as mild (AHI 5.0–14.9 events/hour); moderate (AHI 15.0–29.9 events/hour), or severe (AHI ≥30.0 events/hour). The diagnosis night was followed by a second full-night PSG with nasal PAP with manual titration by experienced sleep technicians manually according to the AASM guidelines [16]. The pressure was set at the minimum needed to abolish snoring, obstructive events and arousals, and to improve oxygenation. During titration, nasal or oronasal masks were used. Prior to PAP titration, the participants received education from the sleep technician regarding the PAP machine and mask, and a 10- to 15-minute period of PAP exposure with low pressure for PAP acclimatization. In the SS group, a sleep medicine physician (S.S. or G.C.A.) gave each participant a general explanation about OSA and PAP treatment in the morning following the diagnostic PSG night. This explanation required 10- to 15-minutes. In the ES group, all participants received education as in the SS group, and additionally viewed his/her own polysomnography chart in the morning following the PAP-titration night comparing the PSG from the diagnostic evaluation night, and the ES participants received explanations by a sleep medicine physician that emphasized the obstructive events and oxygen desaturations, and the disappearance of those signs on PAP treatment. This educational procedure, which took approximately 20 minutes, was performed by the same sleep medicine physician (S.S.). Following the PAP titration night, all participants were asked to rate how they felt in the morning on a 4-point scale (4, very good; 3, good; 2, no change; 1, worse).
In both groups, the decision on the type of PAP device was made by the sleep medicine physician according to the routine procedures of our clinic; continuous PAP (CPAP) was preferred as the first choice; auto-titrating PAP (APAP) was preferred for participants mainly with supine position or rapid eye movement (REM) dependent OSA; and bilevel PAP (BPAP) was chosen for participants requiring a high pressure (≥12 mbar). For CPAP titration and long-term use, the S9 series (ResMed, San Diego, CA, USA) was used; and for the BPAP titration and long-term use, the VPAP IV (ResMed, San Diego, CA, USA) were used.
In Turkey, the cost of PAP devices are covered by the State if the diagnostic procedures, as well as PAP titrations, are based on full PSG [17], and according to the current Turkish legislation, the patient is obliged to use the machine at least 1,200 hours/year to keep the device free of charge [17]. PAP usage monitoring is usually made by the Turkish Social Security Institution, and patients are asked to provide a report from their sleep physician. The patients in both groups were informed about this legislation requirement, although the follow-up period for the study was shorter than the one year State reporting period.
Follow-up procedures
All patients were invited for five appointments with the research coordinator, at 15, 30, 60, 90, and 180 days after the randomization. At the first and the last follow-up, ESS score was obtained. The objective PAP usage time (hours/night and percentage of PAP days/period) was recorded from the devices at each follow-up. Problems with the equipment and mask fitting were addressed at follow-up visits, and participants experiencing dryness were given moisturizers during the study period. Good PAP compliance was defined as the PAP usage for at least 4 hours/night on at least 70% of nights, corresponding 2.8 hours/night [5], and the short-term compliance was measured at the first follow-up, and the long-term compliance was measured at the last follow-up.
Statistics
Statistical analysis was performed using the Statistical Package for Social Sciences, version 20.0 for Windows system (SPSS Inc., Chicago, IL, USA). Descriptive statistics are given as mean ±SD, and when appropriate, as median with interquartile ranges (IQR), and categorical variables as numbers (percentages). The analyses were on an intention-to-treat basis. Differences between the groups were analyzed with the Student t test for independent samples, and the chi-square test or Fisher’s exact test was used to compare proportions between the groups. A multivariable regression analysis was performed for all baseline characteristics as the independent predictors and with the long-term PAP compliance as the dependent variable in a stepwise backwards model (variables with p>0.10 removed). Corrected odds ratios (OR) were calculated from the regression coefficients, and all ORs are presented with their 95% confidence intervals (CI). Separately, the short-term CPAP hours/night was compared with the long-term CPAP hours/night using paired t-test within the groups, and the Pearson’s correlation for the whole cohort. All statistical tests were two-sided, and a p-value less than 0.05 was considered significant.
Results
Among 115 eligible OSA patients (mean age 51.0±9.3 years; 75.5% men), 63 were randomized to the SS group and 52 to the ES group (Figure 1). Baseline anthropometrics, educational status, and clinical characteristics did not differ significantly between the groups (Table 1). As shown in Table 2, there were no significant differences with regard to PSG findings at baseline or on PAP titration. Following the PAP titration night, 57.1% in the SS group, and 80.8% in the ES group were satisfied (good/very good) with the PAP titration (p=0.007). Distribution of CPAP, APAP, and BPAP devices was 71.4%, 4.8%, and 23.8%, respectively, in the SS group, and 71.2%, 7.7%, and 21.2%, respectively, in the ES group (p=0.65). Two patients in the SS group, and two patients in the ES group never used their devices, and their CPAP usage hours/night was included in the final analysis as 0. The agreement with exact timing of appointments with time of scheduled follow-up appointments was poor in both groups (data not shown). Three patients in the SS group, and one patient in the ES group did not come to their fifth appointments, and the data from their fourth follow-ups were entered in the final evaluation. In spite of the poor agreement with the scheduled appointments, 58 out of 63 patients in the SS group, and 49 out of 52 patients in the ES group completed the five follow-up appointments during the study period. The median time from randomization to first follow-up was 20 days for both groups with an IQR 17–27 days for the SS group, and 16–26 days for the ES group (p=0.89). The median time to last follow-up was 187 days (IQR 170–202 days) in the SS group, and 184 days (IQR 173–198 days) in the ES group (p=0.16). Mean PAP levels in patients on CPAP, and mean inspiratory and expiratory PAP levels in patients on BPAP did not differ significantly between the groups (data not shown).
Table 1.
Demographic and clinical characteristics of study patients at baseline.
| SS group (n=63) | ES group (n=52) | p Value | |
|---|---|---|---|
| Age, years | 50.3 (9.3) | 51.8 (9.4) | 0.394 |
| AHI, events/hours | 41.2 (23.8) | 41.6 (25.0) | 0.933 |
| ODI, events/hours | 41.3 (24.0) | 40.0 (24.1) | 0.780 |
| ESS score | 10.4 (5.9) | 9.5 (4.3) | 0.354 |
| BMI, kg/m2 | 32.7 (5.5) | 32.2 (6.1) | 0.652 |
| Obesity, % | 66.7 | 57.7 | 0322 |
| Female, % | 23.8 | 25.0 | 0.882 |
| Primary school education, % | 58.7 | 48.1 | 0.254 |
| Pulmonary disease, % | 9.5 | 5.8 | 0.509 |
| Hypertension, % | 41.3 | 34.6 | 0.465 |
| Diabetes mellitus, % | 20.6 | 9.6 | 0.106 |
| Cardiac disease, % | 6.3 | 3.8 | 0.688 |
Values are mean (standard deviation) or percent patients. ES – educational support; SS – standard support; AHI – apnea hypopnea index; ODI – oxygen desaturation index; ESS – Epworth Sleepiness Scale; BMI – body mass index.
Table 2.
Polysomnography findings of study patients.
| SS group (n=63) | ES group (n=52) | p Value | |
|---|---|---|---|
| TST at baseline, minutes | 379 (59) | 392 (52) | 0.221 |
| TST on PAP, minutes | 389 (58) | 404 (53) | 0.150 |
| SE at baseline, % | 82.4 (13.1) | 84.9 (11.1) | 0.291 |
| SE on PAP, % | 83.6 (10.4) | 81.9 (14.7) | 0.473 |
| SWS at baseline, % | 16.5 (9.3) | 16.2 (11.6) | 0.886 |
| SWS on PAP, % | 25.6 (11.6) | 22.5 (11.2) | 0.147 |
| REM sleep at baseline, % | 14.9 (5.7) | 14.9 (7.1) | 0.998 |
| REM sleep on PAP, % | 23.6 (7.7) | 23.6 (8.6) | 0.955 |
Values are mean (standard deviation). ES – educational support; SS – standard support; TST – total sleep time; PAP – positive airway pressure; SE – sleep efficiency; SWS – slow-wave-sleep; REM – rapid eye movement.
At short-term follow-up, the average PAP usage was 3.6±2.3 hours/night in the SS group, and 4.1±2.3 hours/night in the ES group (p=0.62). However, PAP compliance, defined as the minimum usage of 2.8 hours/night, was achieved in 58.7% of patient’s in the SS group, and 76.9% of patients in the ES group (p=0.039). ESS scores decreased significantly in both groups (from 10.4±5.9 to 2.3±2.9 in the SS group; p<0.001 and from 9.5±4.2 to 2.5±3.2 in the ES group; p<0.001).
At long-term follow-up, the average PAP usage was 4.2±2.5 hours/night in the SS group, and 5.2±2.1 hours/night in the ES group (p=0.027). PAP compliance was achieved among 68.3% in the SS group, and 86.5% in the ES group (p=0.021). The increase in PAP usage (hours/night) was significant in both groups (p=0.025 in the SS group, and p<0.001 in the ES group, [paired t-test]), and there was a significant linear relationship (r=0.53; p<0.001) between short-term PAP hours/night and long-term PAP hours/night (Figure 2).
Figure 2.
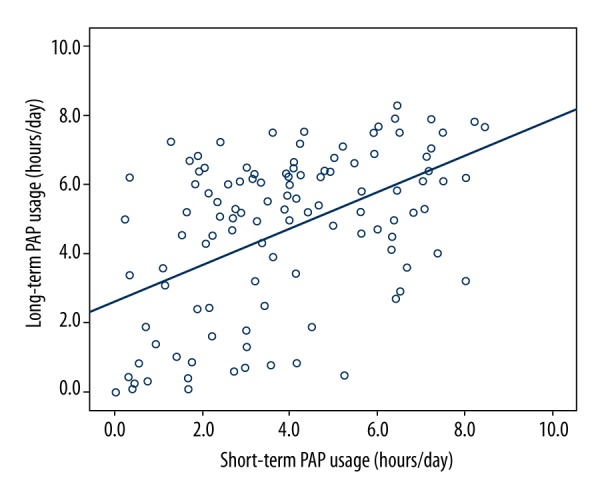
Short-long term compliance.
As shown in Table 3, the ES strategy followed by frequent visits predicted the PAP compliance in the multivariate analysis (OR 3.6, 95% CI 1.2–10.6; p=0.020). Other predictors were obesity (OR 3.4, 95% CI 1.2–9.7; p=0.019) and severe OSA at baseline (OR 4.7, 95% CI 1.2–17.6; p=0.023). Primary school education level was inversely correlated with the PAP compliance.
Table 3.
Variables associated with PAP compliance in multivariate logistic regression analysis.
| OR | 95% CI | p Value | |
|---|---|---|---|
| Educational support | 3.6 | 1.2–10.6 | 0.020 |
| Obesity | 3.4 | 1.2–9.7 | 0.019 |
| Severe OSA (AHI ≥30/h) | 4.7 | 1.2–17.6 | 0.023 |
| Primary school education | 0.3 | 0.1–0.9 | 0.036 |
| Female sex | 2.6 | 0.8–8.3 | 0.116 |
| Age | 1.0 | 0.9–1.1 | 0.352 |
| ESS score ≥15 | 4.1 | 0.7–25.6 | 0.130 |
PAP – positive airway pressure; OR – odds ratio; CI – confidence interval; OSA – obstructive sleep apnea; ESS – Epworth Sleepiness Scale.
Discussion
In the current study, the intensified patient education strategy with PSG charts view followed by frequent follow-up appointments improved the PAP compliance in OSA patients in this sleep clinic cohort. Other significant predictors of PAP compliance were obesity and OSA severity at baseline, while primary school education level was inversely correlated with the PAP compliance.
To our knowledge, this is the first study to report the impact of an educational strategy including PSG chart view at baseline and after the titration night followed by five PAP control appointments during a median follow-up of six months in a sleep clinic cohort.
The strengths of the study include the randomized controlled design with similar baseline characteristics of the groups, the frequent follow-up visits, as well as a low dropout rate during the study period. The ES strategy seemed to increase the awareness of OSA and its risks especially in obese and severe OSA patients, and the outcomes were significantly better in the ES group, even after adjustment for the baseline educational status of the participants. Though the patients did not follow the exact scheduled appointment times, almost all participants returned for five follow-ups during the study period. There was a significant increase in PAP usage in hours/night in both groups over time, suggesting the importance of the frequent follow-ups as continuous support in order to increase awareness and PAP compliance.
In some previous studies, the importance of education on PAP adherence was addressed [9–12]. A similar design as ours was recently reported by Falcone and colleagues [12], demonstrating that 93% the participants who viewed their PSG charts returned for follow-up at one month and 76% returned at 12 months. At one-month follow-up, 94% of the ES group and 69% of the SS group achieved PAP usage of at least four hours during 70% of the time period, and these rates were almost similar at one year follow-up [12]. The CPAP usage in hours/night was also reported to be higher in the ES group already at one month with no further increase at one year follow-up. However, in our study, the initial adherence rates were lower, probably due to the educational level of the patients, but the compliance rates were improved significantly at six-month follow-up, suggesting that the follow-up visits were important for increasing awareness of the disease and improvement of PAP compliance, especially in patients with a lower educational level. Another previous study by Nadeem and colleagues demonstrated that OSA patients who viewed their PSG charts at baseline without viewing the PSG charts on PAP titration did not improve their PAP adherences [18], which might reflect the importance of PSG chart view of PAP titration in the educational strategy. However, in that study, there were no frequent follow-ups and the educational level of the participants was not considered.
Other educational studies regarding PAP adherence have often included multiple simultaneous interventions. In one study, OSA patients received home nursing, a 3-night CPAP trial, and educational support [11]. In another study, the intensive support included optimizing the equipment with humidifiers and mask fit, together with counseling and educational support [19]. In trials with telephone support, one study reported that the patients who were called by phone regularly for two months had increased adherence ratios [20]. Another study reported that there was no difference between sending standardized messages and additional phone calls [21].
Less is known regarding the PAP adherence rates in OSA patients in Turkey. Salepci and colleagues followed a larger cohort of 648 patients in the same region of Istanbul as our hospital, during 2005 to 2011, and reported that only 38% of patients attended the clinical follow-ups, and the required adherence rate was achieved among 65% of the patients attending the follow-ups [13]. The low socio-economic status of the study population and unawareness of the seriousness of the disease were possible explanations of those study results [13]. This suggests that educational support is even more important in cohorts with a low educational level. It should also be emphasized that the current Turkish legislation regarding the minimum requirement of PAP usage in order to keep the device free of charge as a kind of “reinforcement” might have influenced our results with better follow-up attendance rates and increased PAP compliance over time compared to the results in the study of the Salepci and colleagues [13]. However, this information was given to both groups, and the “additional” benefit of the ES strategy seemed to be an effective method in this context.
In our study, short-term PAP adherence was associated with long-term PAP adherence, as was previously suggested [22,23]. Obesity and severe OSA (AHI ≥30 events/hour) were also significant predictors of better PAP adherence, which is in line with previous reports [5]. The inverse relationship between educational level of the patients and PAP adherence was also reported previously [24]. The patient satisfaction with the PAP titration night seems to be important regardless of the ES or SS intervention allocation. All patients demonstrated a markedly reduced subjective sleepiness at the short-term follow-up, and we found no relationship between ESS severity at baseline and the PAP compliance at long-term follow-up in contrast to some of the other studies [5,25]. Neither did we find a relationship between patient sex and PAP compliance, as suggested in another recent report [26].
This study also had a number of limitations. First, it was a single-center study, which limits generalizability of results across geographic regions in Turkey. Second, only PAP adherence rates and PAP hours/night were considered as primary outcomes, and the reduction in daytime sleepiness was based on the ESS scores. It is possible that there were significant differences in other symptoms, quality of life, and cognitive function. Third, the patients not coming to the scheduled follow-up visit were contacted by phone by the sleep physician, which might have reinforced the patients participation. This might be considered a bias. However, the phone calls were done for all participants regardless of the group allocation.
The current study did not either include a cost-benefit analysis. This educational procedure with PSG chart view does not entail any additional cost except for adding 5 to 10 minutes, twice, to the standard protocol, and thus, it may be easily reproduced in any sleep medicine center. However, the frequent follow-ups are not a routine procedure in Turkey, and this should be evaluated in a larger cohort addressing the cost-benefit aspects of the management of OSA patients. Given the high adherence rates in severe OSA patients as shown in our study, new national educational strategies should be developed, especially with more focus on OSA patients with a low educational level. In order to overcome the potential limit of the sleep centers with full PSGs, the current international guidelines of the management of OSA patients with home-monitoring diagnostic and PAP-titration procedures [27] should be implemented.
Conclusions
Patient education with PSG chart view, both from the diagnostic and PAP titration night, followed by frequent visits increased the long-term compliance with PAP treatment. Other significant predictors of PAP compliance were obesity and OSA severity at baseline while primary school education level was inversely correlated with the PAP compliance. These findings urge the implementation of the recent guidelines for management of OSA patients with home-monitoring systems in Turkey in order to reduce the clinical overload. This would allow the clinicians to have more time for the educational support strategies, especially for the patients with a low educational level. These strategies may also have important health economic implications.
Acknowledgment
We would like to thank our sleep technicians Durmuş Koyuncu, Rıza Denizhan, and Cem Bingöl for skillful management of the PSG and PAP titration procedures, and the research nurse Birsen Tarim for the administrative support for the follow-up appointments.
Footnotes
Conflict of interests
Authors report no conflict of interests related to the current study. Dr Peker reports institutional grants in Sweden from ResMed Foundation outside the current work.
Source of support: Departmental sources
Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. New Engl J Med. 1993;328(17):1230–35. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 2.Howard ME, Desai AV, Grunstein RR, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170(9):1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 3.Celen YT, Peker Y. Cardiovascular consequences of sleep apnea – II: Cardiovascular mechanisms. Anadolu Kardiyol Derg. 2010;10(1):168–75. doi: 10.5152/akd.2010.017. [DOI] [PubMed] [Google Scholar]
- 4.Engleman HM, Martin SE, Kingshott RN, et al. Randomised placebo controlled trial of daytime function after continuous positive airway pressure (CPAP) therapy for the sleep apnea/hypopnea syndrome. Thorax. 1998;53(5):341–45. doi: 10.1136/thx.53.5.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sawyer AM, Gooneratne NS, Marcus CL, et al. A systematic review of CPAP adherence across age groups: Clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15(6):343–56. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147(4):887–95. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 7.Reeves-Hoche MK, Meck R, Zwillich CW. Nasal CPAP: An objective evaluation of patient compliance. Am J Respir Crit Care Med. 1994;149(1):149–54. doi: 10.1164/ajrccm.149.1.8111574. [DOI] [PubMed] [Google Scholar]
- 8.Tyrrell J, Poulet C, Pe Pin JL, Veale D. A preliminary study of psychological factors affecting patients’ acceptance of CPAP therapy for sleep apnea syndrome. Sleep Med. 2006;7(4):375–79. doi: 10.1016/j.sleep.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machine in adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2014;(1):CD007736. doi: 10.1002/14651858.CD007736.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Golay A, Girard A, Grandin S, et al. A new educational program for patients suffering from sleep apnea syndrome. Patient Education and Counseling. 2006;60(2):220–27. doi: 10.1016/j.pec.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Hoy CJ, Vennelle M, Kingshott RN, et al. Can intensive support improve continous positive airway pressure use in patients with the sleep apnea/hypopne syndrome? Am J Respir Crit Care Med. 1999;159(4 Pt 1):1096–100. doi: 10.1164/ajrccm.159.4.9808008. [DOI] [PubMed] [Google Scholar]
- 12.Falcone VT, Damiani MF, Quaranta VN, et al. Polysomnograph chart view by patients: A new educational strategy to improve CPAP adherence in sleep apnea therapy. Respir Care. 2014;59(2):193–98. doi: 10.4187/respcare.02491. [DOI] [PubMed] [Google Scholar]
- 13.Salepci B, Caglayan B, Kiral N, et al. CPAP adherence of patients with obstructive sleep apnea. Respir Care. 2013;58(9):1467–73. doi: 10.4187/respcare.02139. [DOI] [PubMed] [Google Scholar]
- 14.Khosla T, Lowe FR. Indices of obesity derived from body weight and height. Br J Prev Soc Med. 1967;21(3):122–28. doi: 10.1136/jech.21.3.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157–71. [PMC free article] [PubMed] [Google Scholar]
- 17.Official Register in Turkey with 24.03.2013 date and item no: 28597. Available from URL: http://www.saglikaktuel.com/d/file/2013_sut_metin_www.saglikaktuelcom.pdf.
- 18.Nadeem R, Rishi MA, Srinivasan L, et al. Effect of visualization of raw graphic polysomnography data by sleep apnea patients on adherence to CPAP therapy. Respir Care. 2013;58(4):607–13. doi: 10.4187/respcare.01539. [DOI] [PubMed] [Google Scholar]
- 19.Damjonovic D, Fluck A, Bremer H, et al. Compliance in sleep apnea therapy: Influence of home care support and pressure mode. Eur Respir J. 2009;33(4):804–11. doi: 10.1183/09031936.00023408. [DOI] [PubMed] [Google Scholar]
- 20.De Molles DA, Sparrow D, Gottlieb DJ, Friedman R. A pilot trial of a telecommunications system in sleep apnea management. Med Care. 2004;42(8):764–69. doi: 10.1097/01.mlr.0000132353.99209.fe. [DOI] [PubMed] [Google Scholar]
- 21.Munafo D, Hevener W, Crocker M, et al. A telehealth program for CPAP adherence reduces labor and yields similar adherence and efficacy when compared to standard of care. Sleep Breath. 2016;20(2):777–85. doi: 10.1007/s11325-015-1298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aloia MS, Arnedt JT, Stanchina M, Millman RP. How early in treatment is PAP adherence established? Revisiting night-to-night variability. Behav Sleep Med. 2007;5(3):229–40. doi: 10.1080/15402000701264005. [DOI] [PubMed] [Google Scholar]
- 23.Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30(3):320–24. [PubMed] [Google Scholar]
- 24.Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics aspredictors of CPAP adherence. Sleep. 2011;34(12):1653–58. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: A population-based study. Chest. 2002;121(2):430–35. doi: 10.1378/chest.121.2.430. [DOI] [PubMed] [Google Scholar]
- 26.Turnbull CD, Bratton DJ, Craig SE, et al. In patients with minimally symptomatic OSA can baseline charasteristics and early patterns of CPAP usage predict those who are likely to be longer-term users of CPAP. J Thorac Dis. 2016;8(2):276–81. doi: 10.3978/j.issn.2072-1439.2016.01.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuna ST, Badr MS, Kimoff RJ, et al. An official ATS/AASM/ACCP/ERS workshop report: Research priorities in ambulatory management of adults with obstructive sleep apnea. Proc Am Thorac Soc. 2011;8(1):1–16. doi: 10.1513/pats.2009-042WS. [DOI] [PubMed] [Google Scholar]


