Abstract
Background
A lifestyle characterized by poor eating habits and physical inactivity is a risk factor for multiple lifestyle diseases in young adults. This study assessed the effects of implementing an intensive 10-day health promotion program combining diet and physical activities on body composition, physical fitness, and biochemical parameters of young adults.
Material/Methods
In this randomized pilot study, 30 female undergraduate students were randomly allocated to an intervention and a control group. The health promotion program consisted of unlimited amounts of vegetarian food; aerobic, flexibility, and strength exercises (3 hours/day); lectures on health (3 hours/day); massage practice (2 hours/day); and healthy cooking practice (1 hour/day). The effects of the intervention were analyzed using the Mann-Whitney U test and the Wilcoxon signed-rank test.
Results
The intensive 10-day health promotion program significantly reduced body weight, body mass index, triglyceride, total cholesterol, low-density lipoprotein cholesterol, blood glucose, and the homeostasis model assessment of insulin resistance. At the same time, participants demonstrated increased back muscle, leg muscle, and grip strength; waist and shoulder flexibility; balance; and cardiorespiratory endurance.
Conclusions
The intensive 10-day health promotion program is a viable intervention for improving body composition, physical fitness, glycemic control, and blood lipid levels in young adults.
MeSH Keywords: Advance Care Planning; Diet, Vegetarian; Sports Nutritional Sciences
Background
Lifestyle and health-related behaviors are strongly associated with morbidity and mortality in many chronic diseases worldwide [1,2]. Major factors include diet, physical activity, smoking, body mass index (BMI), and alcohol consumption [3–5].
Poor diet and physical inactivity are lifestyle behaviors common to young adults worldwide [6]. For example, university students experience significant changes in their diet due to busy class schedules and extracurricular activities, as well as the abundance of opportunities for eating out and drinking alcohol. In addition, excessive interest in appearance and poor health literacy even lead some to develop a habit of skipping meals [7]. Moreover, according to previous research, although most university campuses provide physical environments that promote physical activities, more than 54.8% of university students do not participate in sufficient physical activity and 25.8% do not participate in any physical activity at all [8,9].
These unhealthy behaviors have been reported to cause diseases such as obesity, cancer, cardiovascular disease, cerebrovascular disease, and osteoporosis [10,11]. In South Korea, the incidence of osteoporosis in young women and the prevalence of obese young adults have increased sharply over the last decade [12].
However, young adults have largely been neglected in health promotion programs. Young adulthood is a transitional period that bridges adolescence and adulthood, and the lifestyle of a person during this period not only reflects their past lifestyle, but may also predict their future lifestyle in adulthood and beyond. Failure to recognize the unhealthy lifestyles of young adults may therefore limit the success of childhood health promotion programs [13].
First line interventions for health promotion in young adults tend to target diet and physical activity [14–16]. However, only a few studies have investigated the effects of programs promoting healthy eating habits that also include physical activity [17,18]. Moreover, most relevant studies on the effects of a diet or physical activity program were long-term studies lasting more than 8 weeks [19,20]. However, in a preliminary study on the need for a health promotion program targeting young adults, we found that most respondents expected to experience a remarkable change after participating in a short-term intensive experience program.
Short-term programs have been shown to improve skeletal muscle strength, insulin sensitivity and serum lipids, as well as aid weight loss and changes in body composition. For example, a previous study reported that a 14-day diet and exercise intervention decreased body mass index (BMI), insulin sensitivity, triglycerides (TG) and total cholesterol (TC) in 21 overweight or obese children [21]. Similarly, a 6-day yoga and diet change program conducted in 47 obese adults reduced BMI, waist and hip circumference, fat-free mass and hand-grip strength [22].
Therefore, this study was conducted to assess the impact of an intensive 10-day health promotion program combining healthy diet and physical activity on body composition, physical fitness, and biochemical parameters of young adults.
Material and Methods
Participants
As college-based researchers often find it easier to recruit on campus, university students were chosen as participants of this health promotion study for young adults. The selection criteria were (1) no physical and/or psychological disease before study commencement and (2) no history of participation in any health promotion programs.
The G*Power 3.1 Program was used to calculate an appropriate sample size [23]. Each group required 17 subjects to detect an effect size of 0.80 with a power of 0.70 at a 0.05 level of significance. This number was based on a previous study, which suggested 10% of the project sample size (10 to 30 participants) to be appropriate for the pilot study [24].
Despite male students being eligible for inclusion, they were reluctant to participate in the program. Therefore, 34 female undergraduate students enrolled in the study, and were randomly assigned to the intervention group or the control group (17 in each group). Subjects’ family names were arranged according to the Korean alphabet, and then research randomization 4.0, a randomized computer program, was used to perform the randomization [25]. However, 3 students dropped out before the baseline examination because of scheduling conflicts and one dropped out before the follow-up examination because of a health condition (Figure 1). Finally, 30 participants (16 in the intervention group and 14 in the control group) were included in this study.
Figure 1.
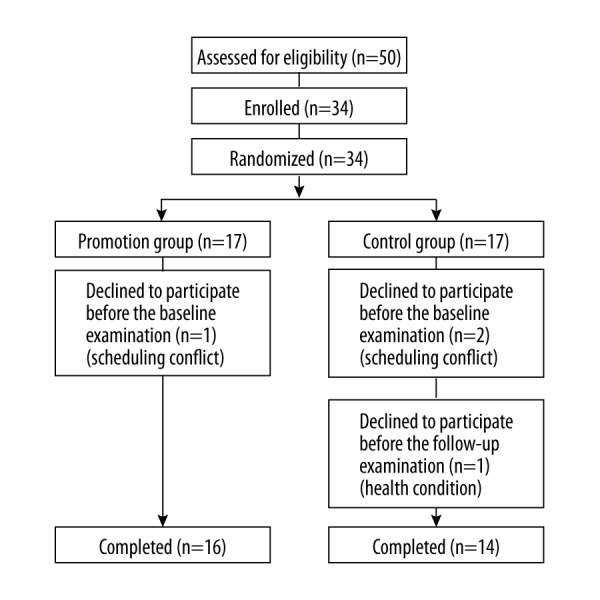
Flow diagram of participants.
This study was approved by the Ethical Committee of Sahmyook University and complied with the ethical standards of the Declaration of Helsinki. Witten informed consent was obtained from each participant.
The intensive 10-day health promotion program
The intensive 10-day health promotion program combining diet and physical activity (10-RHPDP) was designed and conducted by experts, professors, and researchers of nutrition, exercise, and lifestyle. All participants followed a planned 24-hour schedule during the program. After getting up at 6:00 a.m. and having breakfast, participants listened to health-related lectures on nutrition, exercise, and health for 3 hours in the morning and 1 hour after lunch for a total of 24 hours over the 10-day period. To ensure the long-lasting effects of the program, healthy diet, exercise, massage practice, cooking practice and various lectures relating to healthy lifestyle were also included.
In addition, participants exercised for a total of 23 hours over the 10-day period, which included taking a light walk for 1 hour every morning, and undertaking aerobic, flexibility, and strength exercises for 2 hours in the afternoon. Before lunch, participants engaged in healthy cooking sessions for a total of 8 hours over the 10-day period. After dinner, participants listened to a lecture on massage theory and practiced for a total of 16 hours over the course of the program. All participants had to drink water frequently throughout the day (a daily total of 1.5 L of water) and go to bed after the 10:00 p.m. roll call (no later than 10:30 p.m.).
With regard to the exercise program, participants ran 4–5 km a day at the track for aerobic exercise. They were instructed, encouraged, and supervised to run for 1 km at a low speed at which conversation was possible, for 2–3 km at a speed at which conversation was slightly uncomfortable, and for the last 1 km at the individual’s maximum speed. The total daily aerobic exercise time was approximately 45 minutes. After finishing the aerobic exercise, all the participants moved to an indoor gym and performed 10 different flexibility exercises and 6 different core exercises, maintaining each pose for 30 seconds and resting for 15 seconds between poses. In total, 3 sets of these exercises were performed over approximately 40 minutes.
Food was consumed at a scheduled time and place, and a vegetarian diet planned by a nutritionist was available for consumption in unlimited amounts. The diet comprised a variety of fruits and vegetables, whole grains, dairy products, eggs and legumes. Meat, poultry, and seafood were not included.
Participants assigned to the intervention group lived and engaged in activities as a group according to a 24-hour schedule. Dietary intake and physical activity outside the predetermined schedule were impossible because of strict supervision by the experiment assistants. The detailed 10-RHPDP schedules are shown in Table 1.
Table 1.
The 10-RHPDP schedule.
| Time | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 | Day 9 | Day 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 6:30–7:30 | CME | CME | CME | CME | CME | CME | CME | |||
| 7:30–8:45 | Breakfast | Breakfast | Breakfast | Breakfast | Breakfast | Breakfast | Breakfast | |||
| 8:45–9:00 | Recreation | Recreation | Recreation | Recreation | Recreation | Recreation | Recreation | |||
| 9:00–9:50 | Various tests | L: Food and health 1 | L: Exercise and health 1 | L: Digestion and health | L: Exercise and health 2 | L: RH 1 | L: Aquatic therapy | L: Exercise and health 3 | Various tests | |
| 10:00–10:50 | L: Food and health 2 | L: Drinking and health | L: Breathing and health | L: Smoking and health | L: RH 2 | L: Water and health 3 | L: Habit and health | |||
| 11:00–12:00 | CP 1 | CP 2 | CP 3 | CP 4 | CP 5 | CP 6 | CP 7 | CP 8 | EM | |
| 12:00–2:00 | Lunch | Lunch | Lunch | Lunch | Lunch | Lunch | Lunch | Lunch | ||
| 2:00–2:50 | Program orientation | L: Water and health 2 | L: Mind and health | L: BVH | L: Stress and health | L: EH | L: Nature and health | L: Rest and health | L: Health planner | |
| 3:00–5:00 | L: IL | CAE | CAE | CAE | CAE | CAE | CAE | CAE | CAE | |
| 5:00–6:30 | Dinner | Dinner | Dinner | Dinner | Dinner | Dinner | Dinner | Dinner | Dinner | |
| 6:30–8:30 | L: Water and health 1 | Aquatic therapy | Foot/hand massage | Ice/Salt Massage | Antistress massage | Russian bath massage | Russian bath massage | Face/neck massage | Natural healing |
L – lecture; IL – introduction to lifestyle; CME – customized morning exercise; CAE – customized afternoon exercise; RH – relationship and health; CP – cooking practice; BVH – blood vessel and health; EH – environment and health; EM – evaluation meeting.
Participants assigned to the control group spent 10 days consuming their normal diets and refraining from any formal exercise, as per their usual custom.
Data collection and outcome measurement
All subjects attended a baseline assessment at Sahmyook University prior to study commencement. A 12-hour fasting blood sample (approximately 10 mL) was taken, and height (cm) was measured using a Martin anthropometer. Weight (kg), BMI, body fat (percent), and muscle mass (kg) were measured with a bioelectrical impedance analysis instrument (Biospace Co., Seoul, South Korea) after resting for approximately 20 minutes. To assess physical fitness, muscle strength (grip and leg and back extension), flexibility (sit and reach, shoulder), balance (single-leg standing), and cardiorespiratory capacity (12-minute run) were measured using a grip dynamometer (DS Total Sports, Incheon, South Korea), dynamometer (TAKEI Scientific Instruments Co., Tokyo, Japan), and sit and reach box (DS Total Sports, Incheon, South Korea).
Serum levels of TG, TC, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) were measured using the enzymatic colorimetric assay method (Model; P, Roche Co, Mannheim, Germany). Glucose levels were measured with enzymatic kinetic assays (Hexokinase) (Model; P, Roche Co, Mannheim, Germany). Insulin levels were measured with electrochemiluminescence immunoassays (ECLIA) (Model; E, Roche Co, Mannheim, Germany). The biochemical parameters were then analyzed using modular analytics. Homeostasis model assessment of insulin resistance index (HOMA-IR), the index value of the indicator representing the insulin resistance, was calculated using the following formula: HOMA-IR=[fasting plasma insulin (μIU/mL) × fasting plasma glucose (mmol/L)] [26].
Statistical analysis
Statistical analysis was performed using the IBM SPSS program for Windows version 20.0 (IBM Corp., Armonk, NY, USA). All data are expressed as mean ± standard deviation. The Mann–Whitney U test for intergroup comparisons and Wilcoxon signed-rank test for intragroup comparisons were used. P<0.05 was considered statistically significant.
Results
Demographic and clinical characteristics at baseline
The mean age of the subjects was 20.0±1.1 years, the mean height was 161.7±5.1 cm, and the mean weight was 56.2±8.7 kg. Before the intervention, there were no statistically significant differences in any variables between the intervention and control groups, thus ensuring homogeneity between the groups (Table 2).
Table 2.
Basic characteristics of the participants.
| Intervention group (n=16) | Control group (n=14) | P-value | |
|---|---|---|---|
| Age (years) | 19.9±1.2 | 20.1±1.1 | 0.643 |
| Height (cm) | 162.7±4.4 | 160.5±5.8 | 0.251 |
| Weight (kg) | 57.1±8.5 | 55.1±9.1 | 0.527 |
| BMI (kg/m2) | 21.5±2.4 | 21.5±4.0 | 0.972 |
| Fat free mass (kg) | 39.1±4.7 | 38.1±4.0 | 0.499 |
| Muscle mass (kg) | 36.8±4.4 | 35.7±3.7 | 0.495 |
| Skeletal muscle mass (kg) | 21.0±2.8 | 20.4±2.4 | 0.539 |
| Fat mass (kg) | 18.0±4.9 | 17.0±6.3 | 0.643 |
| Percent body fat (%) | 31.1±5.0 | 30.2±6.4 | 0.674 |
| Back muscle strength (kg) | 56.3±13.5 | 62.1±11.7 | 0.226 |
| Right leg muscle strength (kg) | 27.5±4.3 | 28.5±4.4 | 0.518 |
| Left leg muscle strength (kg) | 27.0±4.5 | 28.2±4.6 | 0.481 |
| Right Grip strength (kg) | 22.6±4.4 | 24.4±3.9 | 0.242 |
| Left grip strength (kg) | 21.3±4.8 | 24.5±3.8 | 0.048 |
| Waist flexibility (cm) | 12.9±11.4 | 14.0±12.2 | 0.798 |
| Right shoulder flexibility (cm) | 7.9±5.6 | 5.7±5.1 | 0.267 |
| Left shoulder flexibility (cm) | 1.5±8.1 | 3.0±7.9 | 0.623 |
| Right single leg stance (sec) | 13.7±7.7 | 19.7±13.3 | 0.154 |
| Left single leg stance (sec) | 15.0±9.0 | 16.1±11.1 | 0.770 |
| 12 minute run (m) | 1697.5±125.1 | 1631.1±214.6 | 0.302 |
| Triglycerides (mg/dL) | 79.3±40.3 | 76.7±36.3 | 0.859 |
| Total cholesterol (mg/dL) | 171.3±38.0 | 181.1±23.9 | 0.412 |
| HDL-C (mg/dL) | 64.9±12.7 | 66.4±12.7 | 0.751 |
| LDL-C (mg/dL) | 96.4±31.8 | 104.6±24.4 | 0.440 |
| Glucose (mg/dL) | 90.9±8.0 | 87.1±5.4 | 0.137 |
| Insulin (μIU/mL) | 8.8±8.6 | 8.3±3.6 | 0.835 |
| HOMA-IR | 2.0±2.0 | 1.8±0.8 | 0.674 |
BMI – body mass index; HDL-C – high-density lipoprotein cholesterol; LDL-C – low-density lipoprotein cholesterol: HOMA-IR – homeostatic model assessment of insulin resistance.
Body composition
Body weight and BMI decreased significantly in the intervention group compared with that in the control group (P<0.001). There were no statistically significant differences in fat-free mass, muscle mass, skeletal muscle mass, fat mass, or body fat percentage between the 2 groups (Table 3).
Table 3.
Changes in body composition.
| Intervention group | Control group | P-value | |||||
|---|---|---|---|---|---|---|---|
| Pre-program | Post-program | Change | Pre-program | Post-program | Change | ||
| Weight (kg) | 57.1±8.5 | 56.1±8.5 | −1.1±0.7& | 55.1±9.1 | 55.4±9.1 | 0.3±0.5 | <0.001 |
| BMI (kg/m2) | 21.5±2.4 | 21.1±2.4 | −0.4±0.3& | 21.5±4.0 | 21.6±4.0 | 0.1±0.2 | <0.001 |
| Muscle mass (kg) | 36.8±4.4 | 37.1±4.4 | 0.3±0.7 | 35.7±3.7 | 36.1±3.8 | 0.4±0.8# | 0.733 |
| Fat mass (kg) | 18.0±4.9 | 17.2±4.9 | −0.8±0.6& | 17.0±6.3 | 16.4±6.1 | −0.7±0.6* | 0.642 |
| Percent body fat (%) | 31.1±5.0 | 30.5±5.1 | −0.6±1.0& | 30.2±6.4 | 29.8±6.2 | −0.4±1.1* | 0.179 |
P<0.05;
P<0.01;
P<0.001 calculated from the Wilcoxon signed ranks test.
BMI – body mass index.
Physical fitness
Back and leg strength, bilateral grip strength, waist flexibility, bilateral shoulder flexibility, balance, and cardiorespiratory endurance increased significantly in the intervention group compared to that in the control group (P<0.01 to P<0.001) (Table 4).
Table 4.
Changes in physical fitness.
| Intervention group | Control group | P-value | |||||
|---|---|---|---|---|---|---|---|
| Pre-program | Post-program | Change | Pre-program | Post-program | Change | ||
| Back muscular strength (kg) | 56.3±13.5 | 65.8±11.7 | 9.7±6.1& | 62.1±11.7 | 59.6±10.6 | −2.6±6.2 | <0.001 |
| Right leg muscular strength (kg) | 27.5±4.3 | 32.5±5.1 | 5.1±4.7& | 28.5±4.4 | 24.9±3.7 | −3.7±4.7* | <0.001 |
| Left leg muscular strength (kg) | 27.0±4.5 | 32.5±4.8 | 5.6±5.4# | 28.2±4.6 | 25.0±3.6 | −3.2±4.1* | <0.001 |
| Right grip strength (kg) | 22.6±4.4 | 25.7±4.1 | 3.1±3.3# | 24.4±3.9 | 24.1±3.6 | −0.3±2.5 | 0.004 |
| Left grip strength (kg) | 21.3±4.8 | 24.3±3.5 | 3.1±3.5# | 24.5±3.8 | 22.4±3.5 | −2.2±2.0# | <0.001 |
| Waist flexibility (cm) | 12.9±11.4 | 18.5±8.7 | 5.6±4.6& | 14.0±12.2 | 14.7±10.7 | 0.7±3.3 | 0.003 |
| Right shoulder flexibility (cm) | 7.9±5.6 | 15.3±4.3 | 7.4±4.4& | 5.7±5.1 | 7.6±5.8 | 1.9±4.1 | 0.001 |
| Left shoulder flexibility (cm) | 1.5±8.1 | 10.9±5.7 | 9.3±4.8& | 3.0±7.9 | 4.8±6.0 | 1.9±5.4 | <0.001 |
| Right single leg stance (sec) | 13.7±7.7 | 46.0±46.6 | 32.3±42.4# | 19.7±3.3 | 15.4±13.3 | −4.3±13.1 | 0.004 |
| Left single leg stance (sec) | 15.0±9.0 | 52.4±55.8 | 37.5±53.1* | 16.1±11.1 | 13.7±12.9 | −2.3±15.9 | 0.011 |
| 12 minute run (m) | 1697.5± 125.1 | 2017.4± 90.0 | 319.9± 110.4& | 1631.1± 214.6 | 1610.0± 323.0 | −21.1±34.6 | 0.001 |
P<0.05;
P<0.01;
P<0.001 calculated from the Wilcoxon signed ranks test.
Blood factors
TG, TC, LDL-C, glucose levels and HOMA-IR decreased significantly in the intervention group compared to those in the control group (P<0.05 to P<0.001), but there were no statistically significant differences for HDL-C and insulin. Detailed results are presented in Table 5.
Table 5.
Changes in blood factors.
| Intervention group | Control group | P-value | |||||
|---|---|---|---|---|---|---|---|
| Pre-program | Post-program | Change | Pre-program | Post-program | Change | ||
| TG (mg/dL) | 79.3±40.3 | 52.8±13.0 | −26.5±29.2# | 76.7±36.3 | 84.7±35.9 | 8.0±27.9 | 0.003 |
| TC (mg/dL) | 171.3±38.0 | 157.8±25.7 | −13.5±17.8# | 181.1±23.9 | 180.6±25.7 | −0.5±14.2 | 0.037 |
| HDL-C (mg/dL) | 96.4±31.8 | 80.8±21.9 | −15.6±15.2 | 104.6±24.4 | 102.9±25.6 | −1.7±11.6 | 0.289 |
| LDL-C (mg/dL) | 64.9±12.7 | 66.4±13.0 | 1.4±5.7# | 66.4±12.7 | 65.3±9.4 | −1.1±7.4 | 0.010 |
| Glucose (mg/dL) | 90.9±8.0 | 84.4±8.8 | −6.5±6.8# | 87.1±5.4 | 90.0±6.3 | 2.9±3.7* | <0.001 |
| Insulin (μIU/mL) | 8.8±8.6 | 4.3±2.4 | −4.5±8.5 | 8.3±3.6 | 8.2±3.5 | −0.1±2.7 | 0.075 |
| HOMA-IR | 2.0±2.0 | 0.9±0.6 | −1.1±1.9* | 1.8±0.8 | 1.8±0.8 | 0.0±0.6 | 0.047 |
P<0.05;
P<0.01;
P<0.001 calculated from the Wilcoxon signed ranks test.
TG – triglyceride; TC – total cholesterol; HDL-C – high-density lipoprotein cholesterol; LDL-C – low-density lipoprotein cholesterol: HOMA-IR – homeostatic model assessment of insulin resistance.
Discussion
This study was performed to determine the effects of the 10-RHPDP on body composition, physical fitness, and blood factors of young adults.
The program was effective in reducing weight and BMI, and in increasing back muscle strength, leg muscle strength, grip strength, waist and shoulder flexibility, balance, and cardiorespiratory endurance of young adult females aged 18–22 years. Few studies worldwide have investigated the effects of a short-term intensive health promotion program that combines diet and physical activity in healthy young adults. Therefore, direct comparison of study results is difficult. A study performed in adults aged 18–50 years, however, reported a decrease in body weight and total fat mass after the implementation of a program combining a hypocaloric diet and exercise training [27]. In a study of women aged 19–50 years, a program combining a 1500±2000 calories/day diet, 30–60 minutes/day of moderate-intensity physical activity, and behavioral modification consultations was found to reduce BMI and body fat percentage [28]. In another study investigating the effects of diet and exercise, alone or combined, on weight and body composition in obese menopausal women [29], there was a statistically significant weight loss in the low-fat diet and moderate-intensity aerobic exercise groups, but the greatest change was observed in the group where a combination of both interventions was applied. A randomized controlled trial conducted by Christensen et al. [30] designed a workplace intervention to achieve an energy deficit of 1200 kcal/day including strengthening exercise (15 minutes/hour), aerobic fitness (2 hours/week), and cognitive behavioral training (1 hour/week). This resulted in a reduction in weight, BMI, and body fat percentage, and increased back muscle strength and hand grip strength. Similarly, Rigamonti et al. [31] reported that a 3-week multidisciplinary body weight reduction program combining an energy-restricted diet, 90 min/daily aerobic physical activity, psychological counseling, and nutritional education, improved BMI and percent fat mass in 7 obese male adolescents. These results provide important evidence on the benefit of a health promotion program for healthy young adults, as well as the feasibility of adhering to the program for at least 10 days for overweight or obese young adults. As with the previous studies, the findings of this study suggest that undergoing a short-term lifestyle program can enhance the physique and physical fitness of healthy adults. Therefore, to achieve successful health promotion, it is important to help participants recognize the importance of a healthy lifestyle by providing training on healthy eating habits and adequate physical activity. It is believed that encouraging young adults to participate in a health program, albeit a short-term one, is important.
Although the control group in this study had spent 10 days maintaining their normal lifestyle, there was a decrease in leg strength after 10 days. This could be because the participants may have been unmotivated to perform the leg strength measurements. In addition, the Korean culture views demonstrations of physical strength as unfeminine, which may have contributed to the subjects’ reluctance to engage in the assessment.
Another important finding was the discovery that the 10-RHPDP was effective in reducing serum lipid and glucose levels as well as insulin resistance in our subjects. The program also increased HDL-C and reduced insulin levels, although these findings were not statistically significant. A study investigating the effects of diet and physical activity in young adults aged 18–35 years showed similar results – Jakicic et al. [32] reported that a 6-month diet and physical activity program decreased participants’ TC, TG, and glucose levels and increased their fitness levels. Although other studies demonstrated biochemical parameters levels comparable to those found in our study, they varied widely with respect to duration, size, population, and types of diet and exercise interventions used. Besnier et al. [33] demonstrated a reduction in insulin levels and HOMA-IR after individualized exercise training combined with a fruit- and vegetable-rich diet in overweight or obese women, and Otten et al. [34] reported improved glycemic control and HOMA-IR after a Paleolithic diet with 1 hour of supervised exercise (aerobic exercise and resistance training) 3 times per week among 32 patients with type 2 diabetes. Similarly, Brekke et al. [35] showed that TC, LDL-C, and insulin levels were decreased and HDL-C levels increased after a 12-week behavior modification intervention with diet and exercise among overweight and obese lactating women. Furthermore, a meta-analysis by Kelley et al. [36] found that TG, TC, and LDL-C levels were reduced but HDL-C levels were not significantly changed by diet and aerobic exercise intervention in 6 studies, which may help explain the improvements seen in this study. Thus, the 10-RHPDP may be efficacious in improving the glycemic control and blood lipid levels of young adults. Finally, combining diet and physical activity interventions can reduce the risk of developing multiple lifestyle diseases such as obesity, diabetes, hypertension, and cardiovascular diseases in young adults. There were no statistically significant changes, however, in fat-free mass, muscle mass, skeletal muscle mass, fat mass, or body fat percentage. This may be because (1) most of the results of the variables fell within the normal ranges, (2) it is difficult to produce a change during a 10-day period, or (3) the subjects had vegetarian diets that did not provide sufficient protein.
This study was the first randomized pilot trial of a short-term lifestyle modification program in healthy South Korean young adults. The aim of the study was to improve several health-related parameters by combining diet and physical activity interventions. One of the strengths of the 10-RHPDP is its multidisciplinary approach. Experts, professors, and researchers of nutrition, exercise, and lifestyle designed and facilitated the program. Additionally, compared with previous trials that took place over a longer period and took a less intensive approach (including biweekly or triweekly meetings), this study used an intensive program over a short period of time, which is likely the reason for the high compliance among our study participants
However, the study had several limitations. First, changes in psychological variables were not measured. It is important to assess psychological variables that could be affected by physical changes. Second, all of the participants were females, as it was difficult to recruit male participants for the diet intervention. Therefore, the possibility that the effect of the 10-RHPDP may differ according to sex cannot be excluded. Third, the study only targeted the students of a single university; therefore, generalization of the results should be done carefully. In the future, further research should be conducted with a larger sample size. Despite the study’s limitations, its findings suggest that the 10-RHPDP can improve not only the physique and physical fitness, but also the glycemic control and blood lipid levels of young adults.
Conclusions
The results of this study showed that an intensive 10-day health promotion program improved weight, BMI, muscle strength, muscle flexibility, balance, cardiorespiratory endurance, HOMA-IR, and TG, TC, LDL-C, and glucose levels in a group of young women. It is easy to administer and may be an effective way to improve body composition, physical fitness, glycemic control, and blood lipid levels in this population.
Footnotes
Source of support: This study was supported by 2014 Research Grant from Kangwon National University
References
- 1.Ford ES, Zhao G, Tsai J, Li C. Low-risk lifestyle behaviors, and all-cause mortality: Findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health. 2011;101:1922–29. doi: 10.2105/AJPH.2011.300167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ford ES, Croft JB, Posner SF, et al. Co-occurrence of leading lifestyle-related chronic conditions among adults in the United States, 2002–2009. Prev Chronic Dis. 2013;10:E60. doi: 10.5888/pcd10.120316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wikström K, Lindström J, Harald K, et al. Clinical and lifestyle-related risk factors for incident multimorbidity: 10-year follow-up of Finnish population-based cohorts 1982–2012. Eur J Intern Med. 2015;3:211–16. doi: 10.1016/j.ejim.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Bonevski B, Guillaumier A, Paul C, Walsh R. The vocational education setting for health promotion: A survey of students’ health risk behaviours and preferences for help. Health Promot J Austr. 2013;24:185–91. doi: 10.1071/HE13047. [DOI] [PubMed] [Google Scholar]
- 5.Burtscher M, Bodner T, Burtscher J, et al. Life-style characteristics and cardiovascular risk factors in regular downhill skiers: An observational study. BMC Public Health. 2013;13:788. doi: 10.1186/1471-2458-13-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allman-Farinelli MA. Nutrition promotion to prevent obesity in young adults. Healthcare (Basel) 2015;3(3):809–21. doi: 10.3390/healthcare3030809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HY, Kim JH, Jung HG. A comparison of health related habits, nutrition knowledge, dietary habits, and blood composition according to gender and weight status of college students in Ulsan. J Nutr. 2012;45:336–46. [Google Scholar]
- 8.García Puello F, Herazo Beltrán Y, Tuesca Molina R. Levels of physical activity among colombian university students. Rev Med Chil. 2015;143(11):1411–18. doi: 10.4067/S0034-98872015001100006. [DOI] [PubMed] [Google Scholar]
- 9.Teleman AA, de Waure C, Soffiani V, et al. Physical activity and health promotion in Italian university students. Ann Ist Super Sanità. 2015;51:106–10. doi: 10.4415/ANN_15_02_06. [DOI] [PubMed] [Google Scholar]
- 10.Plotnikoff RC, Costigan SA, Williams RL, et al. Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: A systematic review and meta-analysis. Int J Behav Nut Phys Act. 2015;12:1–10. doi: 10.1186/s12966-015-0203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mynarski W, Cholewa J, Rozpara M, et al. Recommendations for health-enhancing physical activities in type 2 diabetes patients. J Phys Ther Sci. 2015;27:2419–22. doi: 10.1589/jpts.27.2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Health Insurance Service. Health insurance statistics yearbook: 8th annual publication. [cited May 3, 2015]. Availabe from http://www.hira.or.kr/dummy.do?pgmid=HIRAA020045010000&cmsurl=/cms/medi_info/07/03/01/1337460_27398.html&subject=2014%eb%85%84+%ea%b1%b4%ea%b0%95%eb%b3%b4%ed%97%98%ed%86%b5%ea%b3%84%ec%97%b0%eb%b3%b4#none.
- 13.Allman-Farinelli M, Partridge SR, McGeechan K, et al. A mobile health lifestyle program for prevention of weight gain in young adults (TXT2BFiT): Nine-month outcomes of a randomized controlled trial. JMIR Mhealth Uhealth. 2016;4(2):e78. doi: 10.2196/mhealth.5768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Floegel A, Wientzek A, Bachlechner U, et al. Linking diet, physical activity, cardiorespiratory fitness and obesity to serum metabolite networks: Findings from a population-based study. Int J Obes (Lond) 2014;38:1388–96. doi: 10.1038/ijo.2014.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fleig L, Küper C, Lippke S, et al. Cross-behavior associations and multiple health behavior change: A longitudinal study on physical activity and fruit and vegetable intake. J Health Psychol. 2015;20(5):525–34. doi: 10.1177/1359105315574951. [DOI] [PubMed] [Google Scholar]
- 16.Brown T, Smith S, Bhopal R, et al. Diet and physical activity interventions to prevent or treat obesity in South Asian children and adults: A systematic review and meta-analysis. Int J Environ Res Public Health. 2015;12(1):566–94. doi: 10.3390/ijerph120100566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pronk NP, Remington PL Community Preventive Services Task Force. Combined diet and physical activity promotion programs for prevention of diabetes: Community preventive services task force recommendation statement. Ann Intern Med. 2015;163:465–368. doi: 10.7326/M15-1029. [DOI] [PubMed] [Google Scholar]
- 18.Kattelmann KK, Bredbenner CB, White AA, et al. The effects of young adults eating and active for health (YEAH): A theory-based web-delivered intervention. J Nutr Educ Behav. 2014;46(6):S27–41. doi: 10.1016/j.jneb.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 19.Han GS, Kang MH. The effects of between 14-weeks of pilates and dance sports exercise program and female college students soft lean mass, body fat, BMI, waist-hip ratio and physical strength factor. KSSS. 2013;22:1051–65. [Google Scholar]
- 20.Jakicic JM, King WC, Marcus MD, et al. Short-term weight loss with diet and physical activity in young adults: The IDEA study. Obesity (Silver Spring) 2015;23(12):2385–97. doi: 10.1002/oby.21241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Izadpanah A, Barnard RJ, Almeda AJ, et al. A short-term diet and exercise intervention ameliorates inflammation and markers of metabolic health in overweight/obese children. Am J Physiol Endocrinol Metab. 2012;303(4):E542–50. doi: 10.1152/ajpendo.00190.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Telles S, Naveen VK, Balkrishna A, Kumar S. Short term health impact of a yoga and diet change program on obesity. Med Sci Monit. 2010;16(1):CR35–40. [PubMed] [Google Scholar]
- 23.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 24.Connelly LM. Pilot studies. Medsurg Nurs. 2008;17(6):411–12. [PubMed] [Google Scholar]
- 25.Urbaniak GC, Plous S. Research Randomizer Version 4.0 [Computer software] Retrieved on May 22, 2015, from http://www.randomizer.org/
- 26.Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–19. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 27.Benito PJ, Bermejo LM, Peinado AB, et al. Change in weight and body composition in obese subjects following a hypocaloric diet plus different training programs or physical activity recommendations. J Appl Physiol (1985) 2015;118(8):1006–13. doi: 10.1152/japplphysiol.00928.2014. [DOI] [PubMed] [Google Scholar]
- 28.Andreou E, Philippou C, Papandreou D. Effects of an intervention and maintenance weight loss diet with and without exercise on anthropometric indices in overweight and obese healthy women. Ann Nutr Metab. 2011;59:187–92. doi: 10.1159/000334755. [DOI] [PubMed] [Google Scholar]
- 29.Foster-Schubert KE, Alfano CM, Duggan CR, et al. Effect of diet and exercise, alone or combined, on weight and body composition in overweight-to-obese post-menopausal women. Obesity. 2012;20:1628–38. doi: 10.1038/oby.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Christensen JR, Faber A, Ekner D, et al. Diet, physical exercise and cognitive behavioral training as a combined workplace based intervention to reduce body weight and increase physical capacity in health care workers – a randomized controlled trial. BMC Public Health. 2011;11:671. doi: 10.1186/1471-2458-11-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rigamonti AE, Agosti F, Patrizi A, et al. GH responsiveness before and after a 3-week multidisciplinary body weight reduction program associated with an incremental respiratory muscle endurance training in obese adolescents. Horm Metab Res. 2014;46(1):59–64. doi: 10.1055/s-0033-1354403. [DOI] [PubMed] [Google Scholar]
- 32.Jakicic JM, King WC, Marcus MD, et al. Short-term weight loss with diet and physical activity in young adults: the IDEA study. Obesity. 2015;23:2385–97. doi: 10.1002/oby.21241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Besnier F, Lenclume V, Gérardin P, et al. Individualized exercise training at maximal fat oxidation combined with fruit and vegetable-rich diet in overweight or obese women: the LIPOXmax-Réunion randomized controlled trial. PLoS One. 2015;10:e0139246. doi: 10.1371/journal.pone.0139246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Otten J, Stomby A, Waling M, et al. Effects of a Paleolithic diet with and without supervised exercise on fat mass, insulin sensitivity, and glycemic control: A randomized controlled trial in individuals with type 2 diabetes. Diabetes Metab Res Rev. 2016 doi: 10.1002/dmrr.2828. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brekke HK, Bertz F, Rasmussen KM, et al. Diet and exercise interventions among overweight and obese lactating women: Randomized trial of effects on cardiovascular risk factors. PLoS One. 2014;9:e88250. doi: 10.1371/journal.pone.0088250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kelley GA, Kelley KS, Roberts S, Haskell W. Comparison of aerobic exercise, diet or both on lipids and lipoproteins in adults: A meta-analysis of randomized controlled trials. Clin Nutr. 2012;31:156–67. doi: 10.1016/j.clnu.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


