Abstract
Background
Q fever is an endemic disease in different parts of Iran. This study aimed to investigate the prevalence of acute Q fever disease among at-risk individuals in northwestern Iran.
Methodology
An etiological study was carried out in 2013 in Tabriz County. A total of 116 individuals who were in contact with livestock and had a nonspecific febrile illness were enrolled in the study. IgG phase II antibodies against Coxiella burnetii were detected using ELISA.
Principal findings
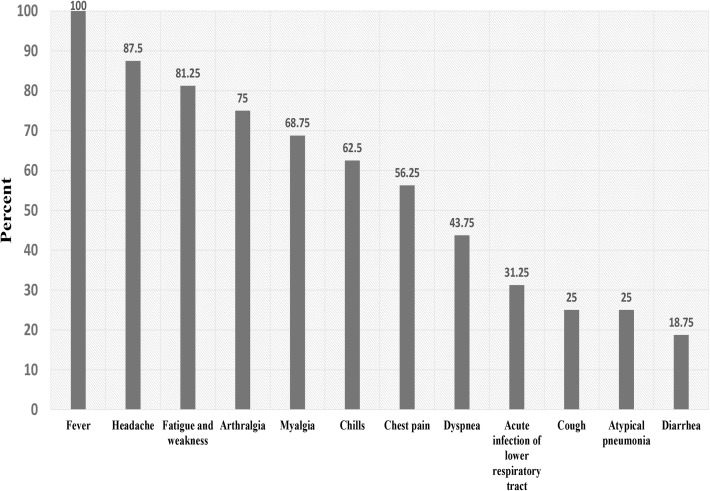
The prevalence of acute Q fever was 13.8% (95% confidence interval [CI]: 8.0, 21.0%). Headache (87.5%) and fatigue and weakness (81.3%) were the dominant clinical characteristics among patients whit acute Q fever. Acute lower respiratory tract infection and chills were poorly associated with acute Q fever. Furthermore, 32% (95% CI: 24, 41%) of participants had a history of previous exposure to Q fever agent (past infection). Consumption of unpasteurized dairy products was a weak risk factor for previous exposure to C. burnetii.
Conclusion
This study identified patients with acute Q fever in northwestern of Iran. The evidence from this study and previous studies conducted in different regions of Iran support this fact that Q fever is one of the important endemic zoonotic diseases in Iran and needs due attention by clinical physicians and health care system.
Author summary
Q fever is a zoonotic contagious disease caused by a bacterium called Coxiella burnetii. It is mostly asymptomatic in livestock and animals. Clinical manifestations of Q fever in humans includes asymptomatic, acute and chronic to fatigue syndrome. The most frequent clinical manifestation of acute Q fever is a flu-like and self-limited illness, and clinical presentations of these patients are highly variable and extensive. Chronic Q fever is accompanied by symptoms such as endocarditis, vasculitis, prosthetic joint arthritis, osteoarticular infection and lymphadenitis. Studies conducted in Iran emphasize that Q fever is an endemic disease in different parts of Iran. Since few studies have been conducted to identify acute Q fever patients with in Iran, the present study set to investigate the prevalence of acute Q fever among at-risk individuals in northwestern Iran. The prevalence of acute Q fever was 14.0% among 116 suspected febrile patients. It was also shown that 32% of the participants had serological evidence of previous infection (past infection) with Q fever. The findings showed that most clinical symptoms in patients with acute Q fever were fever, headache, fatigue and weakness, arthralgia, myalgia, chills, chest pain and dyspnea, respectively.
Introduction
Q fever is a zoonotic contagious disease caused by an intracellular gram-negative bacterium called Coxiella burnetii [1]. Q fever is mostly asymptomatic in livestock and animals, except in some cases, where it causes abortion or stillbirth. Infected animals shed this bacterium in their milk, faeces, urine and especially in birth products [2].
Inhalation of infectious aerosol particles constitutes the major route of acquiring the disease in humans, so inhalation of only one single C. burnetii can cause illness in humans [3]. Nevertheless, other routes of transmission of this infection to human are consumption of contaminated milks and dairy products, tick bites and transmission from a person to person [4]. Domestic ruminants (including cattle, sheep and goats) are the most important reservoirs of C. burnetii in the nature. However, transmission of the infection to human by dogs, cats, rabbits, birds, reptiles and arthropods, especially ticks and mites, has also been reported [5,6].
Clinical manifestations of Q fever in humans include asymptomatic, acute, and chronic to fatigue syndromes. Almost 60% of the infected people may not show any clinical symptoms. Acute Q fever is defined as a primary infection with C. burnetii [5,7]. The most frequent clinical manifestation of acute Q fever is a flu-like and self-limited illness, and the major clinical presentations of these patients are high and prolonged fever, severe headache, coughing, atypical pneumonia, hepatitis, myalgia, arthralgia, cardiac involvement, skin rash and neurologic signs [2,8]. The case fatality rate of acute Q fever is reported 1–2% [4,5]. Chronic Q fever is a disease occurring in less than 5% of acutely infected patients. It may occur several months, years, or even decades after the onset of the acute infection. This form of the disease can occur after infection with or without symptoms. Chronic Q fever is accompanied by symptoms such as endocarditis, vasculitis, prosthetic joint arthritis, osteoarticular infection and lymphadenitis.[7,9]. Endocarditis and vascular infection caused by Q fever are fatal if untreated [10].
Q fever is mainly diagnosed based on serological tests and antibody patterns that are different between acute, convalescent and chronic forms of the disease. There are two distinct antigenic phases to which humans develop antibody responses. Acute or chronic form of Q fever is diagnosed based on the dominant type of antibodies in response to antigens of phase I and II [11]. In acute Q fever infection, antibodies against phase II antigens are predominant, whereas phase I antibody titers are more prevalent in cases of chronic Q fever [10,12,13].
In Iran, the first clinical cases of acute Q fever were reported in 1952, including two patients with symptoms of severe fever and neurological signs in Abadan city, southwest Iran [14]. Furthermore, in 1970, four acute Q fever patients with pneumonic illness were reported from Shiraz, southern Iran [15]. Forty nine patients with acute Q fever were reported from Abadan city during 1970 to 1973 [16]. From 1972 to 1976, 80 patients with acute Q fever were diagnosed, among them three cases had pleuropericarditis lesions [17]. From 1976, the disease was neglected in Iran, and no human case was reported. In 2009, C. burnetii antibodies were reported in febrile patients in Kerman Province, southeastern Iran, and investigation on Q fever was resumed [18]. Afterwards, various seroepidemiological studies were conducted on animal and human population [19–23]. The first patient with Q fever endocarditis was reported in 2013 in Tehran [24]. Studies conducted in Iran emphasize that Q fever is an endemic disease in different parts of the Iran [25].
Since a few studies have been conducted to identify patients with acute Q fever in Iran, present study aimed to investigate the prevalence of acute Q fever among at-risk individuals in northwestern Iran.
Materials and methods
Study area
Tabriz is one of the major cities in Iran and the capital of East Azerbaijan Province located in northwestern Iran. This city, 237 square kilometers, is the third-largest city in Iran. The population of Tabriz and its suburb is approximately 1.8 million. East Azerbaijan Province is among the top five provinces in Iran in terms of production of dairy products with 10 million animal units. Tabriz has a semi-arid climate with hot summers and cold winters. Due to its mountainous climate, keeping and breeding livestock, especially sheep and goats are very common in this province. Dairy sheep and goats have an important role in dairy industry, and their milk is usually used to produce various traditional cheeses such as Lighvan cheese.
Study design
The study was carried out in 2013 in Tabriz County. Individuals (1) with high-risk occupation exposed to animals or livestock products or samples of human patients (veterinarians, farmers, butchers and laboratory personals), (2) people living in areas close to livestock whereabouts, or (3) people with a history of keeping animals (including livestock and pets) in the previous two months, were enrolled in the study provided that they had a nonspecific febrile illness (fever above 38°C accompanied by symptoms such as fatigue, myalgia, chills, headaches, atypical pneumonia and dyspnea). Sampling was done randomly among patients who referred to the Central Laboratory of East Azerbaijan Province (in Tabriz city) and had the above criteria.
Ethical considerations
The ethical committee of the Pasteur Institute of Iran approved the consent procedure, the proposal and the protocol of this study, covering all the samples (blood), questionnaire and verbal informed consent as most participants were either illiterate or had a primary education.
Sampling
After obtaining informed consent from participants, researcher-developed questionnaire including demographic characteristics and Q fever risk factors were collected from each person by a researcher-developed questionnaire. Then, 6-ml blood sample was taken from each patient, and a second blood sample was taken after 4 weeks. Blood samples were centrifuged for 10 minutes at 3000 rpm and were kept at -20°C after extraction of their sera. Sera samples were transferred to the national reference laboratory of Plague, Tularemia and Q fever (Research Centre for Emerging and Reemerging Infectious Diseases, Pasteur Institute of Iran).
Serological tests
IgG phase II antibodies against C. burnetii were detected using a commercial quantitative enzyme-linked immunosorbent assay (ELISA) kit (Serion ELISA classic, Institut Virion/Serion GmbH, Würzburg, Germany) and according to the manufacturer's instructions. Paired sera samples of each patient were tested simultaneously. Dilution protocols were used according to the manufacturer's instructions, using a 1:500 dilution for the IgG phase II assay. The plates were read at 405 nm using a microplate reader (ELx808, BioTek Instruments Inc., USA). Obtained ODs were analyzed according to the Virion/Serion protocol and IgG phase II was quantitatively reported. IgG phase II extinctions were expressed in U/ml titer using a logistic-log-model calculation and were defined as positive when the titer was >30 U/ml, as borderline when the titer was 20–30 U/ml and as negative when the titer was < 20 U/ml. The laboratory diagnosis of acute infection by C. burnetii was made based on any of the following serological criteria: (1) seroconversion, defined as the appearance of specific antibodies against the phase II antigens of C. burnetii at a titer of at least 30 U/ml in the convalescent phase (whereas the serum antibody titer was negative at the initial acute phase), and (2) a fourfold increase in serum antibody titer between the acute phase and the convalescent phase (in two blood samples obtained 4 weeks apart). If the primary and the secondary serum titers were positive, and the fourfold rise was not observed in antibody titers, it was considered as a previous history of exposure to Q fever (past infection).
Statistical analysis
Statistical analysis was performed using the STATA software version 11. Descriptive data were reported in numbers (percentage). Chi-square test was used to assess the association among the categorical variables. P-values less than 0.05 were considered statistically significant, and P-values between 0.05 and 0.1 were considered as borderline significant.
Results
A total of 140 patients were initially enrolled; the second blood sample was taken from 116 patients (82.9%). Mean (SD) age of the patients was 39.3 (18.05) years; 61.4% of them were male. 28.6% were urban residents and 47% had high-risk occupations for Q fever infection; 81.2% of patients had a history of domestic animal keeping, and 93.2% lived near animal shelters. Histories of unpasteurized dairy product's consumption, abortion (among females), and tick bites were reported in 62.3%, 12.2%, and 4.7%, respectively.
The prevalence of acute Q fever was 13.8% (95% CI: 8.0, 21.0%). In terms of acute Q fever infection, there was no statistically significant difference between people were exposed to risk factors (including gender, age, living location, history of residence in nearby animal shelters, previous consumption of unpasteurized dairy products, history of abortion (in women) and history of ticks bites) and those were not (Table 1).
Table 1. Frequency (%) of risk factors in acute Q fever patient and a history of infection with Q fever.
| Variables | Total (% acute Q fever infection) n = 116 | P-value | Total (% history of infection with Q fever) n = 124 | P-value | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 72 (11.1) | 0.28 | 78 (32.1) | 0.94 | |
| Female | 44 (18.2) | 46 (31.6) | |||
| Age | |||||
| Under 20 | 25 (16) | 0.56 | 22 (31.8) | 0.97 | |
| 20–40 | 37 (16.2) | 38 (31.6) | |||
| 40–60 | 42 (14.2) | 49 (34.7) | |||
| Over 60 | 11 (0) | 14 (28.6) | |||
| Living location | |||||
| Urban | 33 (12.1) | 0.67 | 35 (28.6) | 0.55 | |
| Rural | 79 (15.2) | 85 (34.1) | |||
| High-risk occupations | |||||
| Yes | 53 (13.2) | 0.89 | 58 (31.1) | 0.74 | |
| No | 57 (14.1) | 59 (33.9) | |||
| Animals keeping | |||||
| Yes | 89 (14.6) | 0.97 | 95 (34.7) | 0.27 | |
| No | 21 (14.3) | 22 (22.8) | |||
| Living close to livestock shelters | |||||
| Yes | 103 (13.6) | 0.83 | 110 (34.5) | 0.20 | |
| No | 6 (16.7) | 8 (12.5) | |||
| Consumption of unpasteurized dairy products | |||||
| Yes | 67 (17.9) | 0.42 | 69 (40.6) | 0.07 | |
| No | 34 (11.7) | 39 (23.1) | |||
| Abortion | |||||
| Yes | 10 (10) | 0.53 | 11 (9.1) | 0.07 | |
| No | 33 (18.1) | 37 (37.8) | |||
| Tick bites | |||||
| Yes | 5 (40) | 0.06 | 4 (25) | 0.77 | |
| No | 102 (11.8) | 110 (31.8) | |||
| Contact with newborn animals | |||||
| Yes | 12 (8.3) | 0.58 | 13 (15.3) | 0.16 | |
| No | 92 (14.1) | 98 (34.7) | |||
Acute lower respiratory tract infection (26.3%) and chills (20.4%) were associated with acute Q fever (borderline significance: P = 0.08). There was no significant statistical association between acute Q fever infection and other clinical symptoms (headache in the past two weeks, cough, fatigue and weakness, diarrhea, myalgia, arthralgia, chest pain, atypical pneumonia, dyspnea and hepatitis) (Table 2). Headache (87.5%) and fatigue and weakness (81.3%) were the dominant clinical characteristics among the acute Q fever patients (Fig 1). The levels of IgG phase II antibody in patients with acute Q fever are shown in Table 3.
Table 2. Frequency of acute respiratory infection symptoms in persons with acute Q fever infection.
| Variables | Number of patients (% having acute Q fever patients) | P-value | |
|---|---|---|---|
| Headache | |||
| Yes | 108 (13) | 0.34 | |
| NO | 8 (25) | ||
| Chill | |||
| Yes | 49 (20.4) | 0.08 | |
| NO | 67 (9) | ||
| Chest pain | |||
| Yes | 64 (14.1) | 0.92 | |
| NO | 52 (13.4) | ||
| Cough | |||
| Yes | 34 (11.7) | 0.68 | |
| NO | 82 (14.6) | ||
| Fatigue and weakness | |||
| Yes | 97 (13.4) | 0.78 | |
| NO | 19 (15.7) | ||
| Diarrhea | |||
| Yes | 10 (30) | 0.12 | |
| NO | 106 (12.3) | ||
| Acute lower respiratory tract infection | |||
| Yes | 19 (26.3) | 0.08 | |
| NO | 97 (11.3) | ||
| Arthralgia | |||
| Yes | 88 (12.5) | 0.47 | |
| NO | 28 (17.9) | ||
| Myalgia | |||
| Yes | 96 (12.5) | 0.37 | |
| NO | 20 (20) | ||
| Atypical pneumonia | |||
| Yes | 49 (8.1) | 0.13 | |
| NO | 67 (18) | ||
| Dyspnea | |||
| Yes | 45 (15.5) | 0.67 | |
| NO | 71 (12.7) | ||
| Hepatitis | |||
| Yes | 1 (0) | 0.68 | |
| NO | 115 (14) | ||
Fig 1. Clinical characteristics of patients with acute Q fever.
Table 3. Levels of IgG phase II antibody titers in patients with acute Q fever.
| No. | Concentration of IgG Phase II (U/ml) in first sample | Concentration of IgG Phase II (U/ml) in the second sample |
|---|---|---|
| 1 | 5 | 38 |
| 2 | 24 | 50 |
| 3 | 26 | 95 |
| 4 | 16 | 50 |
| 5 | 5 | 30 |
| 6 | 6 | 50 |
| 7 | 12 | 30 |
| 8 | 13 | 50 |
| 9 | 11 | 150 |
| 10 | 15 | 42 |
| 11 | <5 | 26 |
| 12 | 8 | 26 |
| 13 | 10 | 24 |
| 14 | 14 | 38 |
| 15 | 12 | 27 |
| 16 | <5 | 500< |
After excluding acute cases from all participants, 32% (95% CI: 24, 41%) of participants had a history of previous exposure to Q fever (past infection). Consumption of unpasteurized dairy products (40.6%) was a risk factor for previous exposure to C. burnetii (borderline significance: P = 0.07). None of other risk factors were associated with previous exposure to C. burnetii (Table 1).
Discussion
This study was conducted to identify patients with acute Q fever in northwestern Iran. One hundred and forty suspected patients were enrolled in the study, 116 of whom were assessed for acute Q fever. The prevalence of acute Q fever was 13.9% among the suspected febrile patients. It was also shown that 32% of the participants had serological evidence of previous infection (past infection) to Q fever. In a similar study in Zahedan city (southeastern Iran) in 2011, 35.2% of 105 suspected feverish patients were diagnosed acute Q fever [26], which is much higher than the current report. Furthermore, in another study conducted among febrile patients suspected to have brucellosis in Kerman Province (southern Iran), 36% had phase II IgG antibody of Q fever [18]. In a study conducted in 2012 in Ardebil Province (northwestern Iran neighboring East Azerbaijan Province), remarkable seroprevalence of Q fever (33.6%) was observed among sheep [19]. The evidences from this study and previous studies conducted in different regions of Iran support the fact that Q fever is a prominent endemic zoonotic disease in Iran and needs more attention by physicians and health care system.
In similar studies conducted in France, Denmark, Mali and Croatia 2.1% (of 179794), 2.3% (of 1613), 3.9% (of 165) and 5.8% (of 552) of febrile suspected patients were diagnosed to have acute Q fever, respectively [27–30]. The rate of infection in this study was reported much higher than the so-called as in the current study, patients with epidemiological risk factors (having high-risk occupation or living in areas close to livestock or having a history of keeping animals) and clinical risk factors (having a nonspecific febrile illness) were enrolled as the cases and which increased the chance of finding acute Q fever patients. In one study, 1985 to 2009 in France, 3723 (2.1%) of 179,794 suspected patients with Q fever were diagnosed with acute Q fever, and the number of diagnosed Q fever patients was ascending over the years [28]. It could be due to the thereby improvement and development of diagnostic tests of Q fever as well as increasing attention of the physicians and the health care system to Q fever in France.
Acute Q fever was not found significantly associated with any of the studied risk factors. In a study in southeastern Iran, contacts with domestic animals and consumption of unpasteurized dairy products were identified as risk factors [26]. In two studies conducted in Australia, France and Croatia, age and gender were reported as risk factors for acute Q fever [28,30,31]. In Mali, gender, consumptions of unpasteurized dairy products and contact with newborn animals were risk factors [29]. Probably small number of patients and small number of diagnosed acute Q fever cases compared with other study are the causes for lack of finding risk factors. A larger number of suspected patients are recommended to be evaluated in future studies. Furthermore, if there had been a data bank of patients with Q fever, it would have contributed to the achievement of risk factors of Q fever infections as well as the incidence of the disease in Iran.
In this study, chills and acute lower respiratory tract infection were poorly associated with acute Q fever infection. In a study from 1983 to 1999 in Spain and in a study from 2004 to 2007 in Taiwan, the most frequent clinical pictures of Q fever patients were fever with chills [32,33]. During an outbreak of acute Q fever in the Netherlands, acute lower respiratory tract infection was the most frequent symptoms among the patients [34].
The findings showed that headache (87.5%), fatigue and weakness (81.3%), arthralgia (75%), myalgia (68.8%), chills (62%), chest pain (56.3%) and dyspnea (43.8%) were the most prevalent clinical symptoms in patients with acute Q fever. In the similar study in southeastern Iran, major clinical symptoms in patients with acute Q fever were fever (100%), myalgia (59.4%), headaches (43.2%), and arthralgia (37.8) [26]. Fever (69%) and headaches (52%) were the most prevalent clinical symptoms in patients with acute Q fever in Mali [29]. In Portugal, the major clinical symptoms were fever (100%), myalgia (68.8%), headache (62.5%), weakness (56.3%), sweating (53.1%) and chills (43.8%) [35]. In South Korea, fever (89.3%), myalgia (67.9%), weakness (53.6%) and chills (50%) were reported as the most prevalent symptoms [36]. In Spain, the most common symptoms of acute Q fever were headache (58.5%), hepatitis (49.2%), arthromyalgia (37.7%), fever (31.7%) and pneumonia (19.1%) [37]. In Taiwan, fever (99%), relative bradycardia (73%), chills (69%) and headaches (45%) were the most common clinical symptoms [33]. In Tunisia, the highest clinical signs and symptoms in patients with acute Q fever were fever (100%), fatigue (76%), hepatitis (71.5%), chills (47.5%), headache (42.8%) and sweating (33.3%) [38]. Comparing the clinical symptoms obtained in the present study with the so-called studies, the most non-specific symptoms for acute Q fever include fever, headache, chills, myalgia, arthralgia, weakness and fatigue and there are little differences in clinical symptoms. Although, some clinical signs such as hepatitis have a highlighted role in some countries[37,38], they were not observed in the current our study and some other studies. If this disease is a part of the health surveillance system in Iran and also if more clinical cases of Q fever are diagnosed and recorded, a much better view of clinical symptoms of Q fever can be obtained patients data.
In this study, 32% of participants showed evidence of previous infection (past infection) to Q fever; this rate was less than one in Zahedan city (34.3%) [26] and Kerman Province (36%) [18]. In similar studies, 35.5% in Mali [29], 21.74% in Croatia [30] and 8.7% [27] in Denmark were previously infected with Q fever. In a systematic review conducted in Africa, human seroprevalence was <8% with the exception of studies among children and in Egypt, it was 10–32% [39]. In the seroepidemiological studies of Q fever among various populations in Iran, different rates have been also reported; seroprevalence of Q fever was reported 22.5% in the Sistan va Baluchestan Province among butchers and slaughterhouse workers [40], 27.8% in the Kurdistan Province (western Iran) among butchers, slaughterhouse workers, hunters, health care workers, and patients who referred to medical laboratory [21] and 68% in Kerman Province among slaughterhouse workers [22]. Seroprevalence of Q fever was reported 12.8% in Northern Ireland [41] and 3.1% in USA [42], compared with the lower compared with the studies carried out in Iran.
The consumption of unpasteurized dairy products was a weak risk factor for previous exposure to C. burnetii. C. burnetii were isolated from livestock milks (bovine, ovine, caprine, and camel) in the different parts of Iran [43–46]. Therefore, the risk factors must be considered seriously.
Among various diagnostic methods of Q fever, serological methods are the gold standard method for diagnosis. There are a variety of serological methods for the detection of C. burnetii antibodies such as complement fixation assay (CFA), ELISA and indirect immunofluorescence assay (IFA). Although the reference method for serological diagnosis of Q fever is IFA, ELISA was used for serological diagnosis of Q fever due to lack of access to IFA. In a very comprehensive recent study, different serological methods and commercial kits were assessed in 10 different laboratories in the Netherlands and three international reference laboratories in three countries (USA, France and Australia). It was shown that IFA, ELISA, and CFA are all suitable serodiagnostic assays to diagnose acute Q fever. Sensitivity and specificity of the ELISA methods in the detection and diagnosis of IgG phase II antibody compared with reference method (IFA) were 100 and 100, respectively. Therefore, ELISA can be used as an alternative method for the diagnosis and screening of Q fever particularly in cases of acute Q fever [47].
A larger number of patients are recommended to be studied for better understanding of Q-fever risk factors. Also, molecular diagnostic techniques are recommended to be used along with serological methods.
Supporting information
(DOCX)
Acknowledgments
We would like to express our gratitude to staffs of Central Laboratory from Tabriz University of Medical Sciences for their support in sampling.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Pasteur Institute of Iran and Center for Disease Control of the Iranian Ministry of Health and Medical Education had financial support to this project (Grant No. 810). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Dijkstra F, Hoek W, Wijers N, Schimmer B, Rietveld A, et al. (2012) The 2007–2010 Q fever epidemic in the Netherlands: characteristics of notified acute Q fever patients and the association with dairy goat farming. FEMS Immunology & Medical Microbiology 64: 3–12. [DOI] [PubMed] [Google Scholar]
- 2.Parker NR, Barralet JH, Bell AM (2006) Q fever. The Lancet 367: 679–688. [DOI] [PubMed] [Google Scholar]
- 3.Raoult D, Marrie T, Mege J (2005) Natural history and pathophysiology of Q fever. The Lancet infectious diseases 5: 219–226. doi: 10.1016/S1473-3099(05)70052-9 [DOI] [PubMed] [Google Scholar]
- 4.Angelakis E, Raoult D (2011) Emergence of Q fever. Iranian Journal of Public Health 40: 1–18. [PMC free article] [PubMed] [Google Scholar]
- 5.Angelakis E, Raoult D (2010) Q fever. Veterinary microbiology 140: 297–309. doi: 10.1016/j.vetmic.2009.07.016 [DOI] [PubMed] [Google Scholar]
- 6.Knobel DL, Maina AN, Cutler SJ, Ogola E, Feikin DR, et al. (2013) Coxiella burnetii in humans, domestic ruminants, and ticks in rural western Kenya. The American journal of tropical medicine and hygiene 88: 513–518. doi: 10.4269/ajtmh.12-0169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maurin M, Raoult Df (1999) Q fever. Clinical microbiology reviews 12: 518–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marrie TJ (2010) Q fever pneumonia. Infectious disease clinics of North America 24: 27–41. doi: 10.1016/j.idc.2009.10.004 [DOI] [PubMed] [Google Scholar]
- 9.Raoult D (2012) Chronic Q fever: expert opinion versus literature analysis and consensus. Journal of Infection 65: 102–108. doi: 10.1016/j.jinf.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 10.Anderson A (2013) Diagnosis and Management of Q Fever—United States, 2013: Recommendations from CDC and the Q Fever Working Group: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention. [Google Scholar]
- 11.Fournier P-E, Marrie TJ, Raoult D (1998) Diagnosis of Q fever. Journal of clinical microbiology 36: 1823–1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wielders CC, Boerman AW, Schimmer B, van den Brom R, Notermans DW, et al. (2015) Persistent high IgG phase I antibody levels against Coxiella burnetii among veterinarians compared to patients previously diagnosed with acute Q fever after three years of follow-up. PLoS One 10: e0116937 doi: 10.1371/journal.pone.0116937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wielders CL, Kampschreur LL, Schneeberger PP, Jager MM, Hoepelman IA, et al. (2012) Early diagnosis and treatment of symptomatic acute Q fever patients does not prohibit IgG antibody responses to Coxiella burnetii. Clinical and Vaccine Immunology: CVI. 00322–00312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Courdurier J, Bück G, Quesnel J (1952) Investigation into Q Fever in Madagascar. Bulletin de la Société de Pathologie Exotique 45: 602–604. [PubMed] [Google Scholar]
- 15.Eghtedari A, Kohout JCE, Path M (1970) Q fever in Iran A report of clinical cases and serological studies in Shiraz. Pahlavi Med J 1: 66–73. [Google Scholar]
- 16.Caughey J, Harootunian S (1976) Q fever in Iran. The Lancet 308: 638. [DOI] [PubMed] [Google Scholar]
- 17.Caughey J (1977) Pleuropericardial lesion in Q fever. British medical journal 1: 1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khalili M, Shahabi-Nejad N, Golchin M (2010) Q fever serology in febrile patients in southeast Iran. Transactions of the Royal Society of Tropical Medicine and Hygiene 104: 623–624. doi: 10.1016/j.trstmh.2010.04.002 [DOI] [PubMed] [Google Scholar]
- 19.Esmaeili S, Bagheri Amiri F, Mostafavi E (2014) Seroprevalence survey of Q fever among sheep in northwestern Iran. Vector-Borne and Zoonotic Diseases 14: 189–192. doi: 10.1089/vbz.2013.1382 [DOI] [PubMed] [Google Scholar]
- 20.Esmaeili S, Mostafavi E, Shahdordizadeh M, Mahmoudi H (2013) A seroepidemiological survey of Q fever among sheep in Mazandaran province, northern Iran. Annals of Agricultural and Environmental Medicine 20: 708–710. [PubMed] [Google Scholar]
- 21.Esmaeili S, Pourhossein B, Gouya MM, Amiri FB, Mostafavi E (2014) Seroepidemiological survey of Q fever and brucellosis in Kurdistan Province, western Iran. Vector-Borne and Zoonotic Diseases 14: 41–45. doi: 10.1089/vbz.2013.1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khalili M, Mosavi M, Diali HG, Mirza HN (2014) Serologic survey for Coxiella burnetii phase II antibodies among slaughterhouse workers in Kerman, southeast of Iran. Asian Pacific journal of tropical biomedicine 4: S209–S212. doi: 10.12980/APJTB.4.2014C1268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khalili M, Sakhaee E (2009) An update on a serologic survey of Q fever in domestic animals in Iran. The American journal of tropical medicine and hygiene 80: 1031–1032. [PubMed] [Google Scholar]
- 24.Yaghmaie F, Esmaeili S, Francis SA, Mostafavi E (2015) Q fever endocarditis in Iran: A case report. Journal of infection and public health 8: 498–501. doi: 10.1016/j.jiph.2014.12.004 [DOI] [PubMed] [Google Scholar]
- 25.Mostafavi E, Rastad H, Khalili M (2012) Q Fever: An emerging public health concern in Iran. Asian Journal of Epidemiology 5: 66–74. [Google Scholar]
- 26.Metanat M, RAD NS, Alavi-Naini R, Shahreki S, Sharifi-Mood B, et al. (2014) Acute Q fever among febrile patients in Zahedan, southeastern Iran. Turk J Med Sci 44: 99–103. [DOI] [PubMed] [Google Scholar]
- 27.Bacci S, Villumsen S, Valentiner‐Branth P, Smith B, Krogfelt K, et al. (2012) Epidemiology and clinical features of human infection with Coxiella burnetii in Denmark during 2006–07. Zoonoses and public health 59: 61–68. doi: 10.1111/j.1863-2378.2011.01419.x [DOI] [PubMed] [Google Scholar]
- 28.Frankel D, Richet H, Renvoisé A, Raoult D (2011) Q fever in France, 1985–2009. Emerging infectious diseases 17: 350 doi: 10.3201/eid1703.100882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steinmann P, Bonfoh B, Peter O, Schelling E, Traore M, et al. (2005) Seroprevalence of Q‐fever in febrile individuals in Mali. Tropical Medicine & International Health 10: 612–617. [DOI] [PubMed] [Google Scholar]
- 30.Vilibic-Cavlek T, Kucinar J, Ljubin-Sternak S, Kolaric B, Kaic B, et al. (2012) Prevalence of Coxiella burnetii Antibodies Among Febrile Patients in Croatia, 2008–2010. Vector-Borne and Zoonotic Diseases 12: 293–296. doi: 10.1089/vbz.2011.0681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karki S, Gidding H, Newall A, McIntyre P, Liu B (2015) Risk factors and burden of acute Q fever in older adults in New South Wales: a prospective cohort study. The Medical journal of Australia 203: 438–438. [DOI] [PubMed] [Google Scholar]
- 32.de Alarcón A, Villanueva JL, Viciana P, López-Cortés L, Torronteras R, et al. (2003) Q fever: epidemiology, clinical features and prognosis. A study from 1983 to 1999 in the South of Spain. Journal of Infection 47: 110–116. [DOI] [PubMed] [Google Scholar]
- 33.Chang K, Lee N-Y, Chen Y-H, Lee H-C, Lu P-L, et al. (2008) Acute Q fever in southern Taiwan: atypical manifestations of hyperbilirubinemia and prolonged fever. Diagnostic microbiology and infectious disease 60: 211–216. doi: 10.1016/j.diagmicrobio.2007.09.008 [DOI] [PubMed] [Google Scholar]
- 34.Van Steenbergen J, Morroy G, Groot C, Ruikes F, Marcelis J, et al. (2007) [An outbreak of Q fever in The Netherlands—possible link to goats]. Nederlands tijdschrift voor geneeskunde 151: 1998–2003. [PubMed] [Google Scholar]
- 35.Palmela C, Badura R, Valadas E (2012) Acute Q fever in Portugal. Epidemiological and clinical features of 32 hospitalized patients. Germs 2: 43–59. doi: 10.11599/germs.2012.1013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kwak W, Chu H, Hwang S, Park J-H, Hwang KJ, et al. (2013) Epidemiological characteristics of serologically confirmed q Fever cases in South Korea, 2006–2011. Osong public health and research perspectives 4: 34–38. doi: 10.1016/j.phrp.2012.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Espejo E, Gil-Díaz A, Oteo JA, Castillo-Rueda R, García-Alvarez L, et al. (2014) Clinical presentation of acute Q fever in Spain: seasonal and geographical differences. International Journal of Infectious Diseases 26: 162–164. doi: 10.1016/j.ijid.2014.06.016 [DOI] [PubMed] [Google Scholar]
- 38.Bellazreg F, Kaabia N, Hachfi W, Khalifa M, Jazia EB, et al. (2009) Acute Q fever in hospitalised patients in Central Tunisia: report of 21 cases. Clinical Microbiology and Infection 15: 138–139. doi: 10.1111/j.1469-0691.2008.02138.x [DOI] [PubMed] [Google Scholar]
- 39.Vanderburg S, Rubach MP, Halliday JE, Cleaveland S, Reddy EA, et al. (2014) Epidemiology of Coxiella burnetii infection in Africa: a OneHealth systematic review. PLoS Negl Trop Dis 8: e2787 doi: 10.1371/journal.pntd.0002787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Esmaeili S, Naddaf SR, Pourhossein B, Shahraki AH, Amiri FB, et al. (2016) Seroprevalence of Brucellosis, Leptospirosis, and Q Fever among Butchers and Slaughterhouse Workers in South-Eastern Iran. PloS one 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCaughey C, McKenna J, McKenna C, Coyle P, O’Neill H, et al. (2008) Human seroprevalence to Coxiella burnetii (Q fever) in Northern Ireland. Zoonoses and public health 55: 189–194. doi: 10.1111/j.1863-2378.2008.01109.x [DOI] [PubMed] [Google Scholar]
- 42.Anderson AD, Kruszon-Moran D, Loftis AD, McQuillan G, Nicholson WL, et al. (2009) Seroprevalence of Q fever in the United States, 2003–2004. The American journal of tropical medicine and hygiene 81: 691–694. doi: 10.4269/ajtmh.2009.09-0168 [DOI] [PubMed] [Google Scholar]
- 43.Khalili M, Diali HG, Mirza HN, Mosavi SM (2015) Detection of Coxiella burnetii by PCR in bulk tank milk samples from dairy caprine herds in southeast of Iran. Asian Pacific Journal of Tropical Disease 5: 119–122. [Google Scholar]
- 44.Nasehfar A, Bonyadian M, Boroujeni RK, Esfahani MM, Kazemeini H, et al. (2015) Prevalence of Coxiella Burnetii by Nested PCR in Bovine Bulk Milk Samples in Central Zone of Iran. American Advances Journal of Biological Sciences 1: 10–13. [Google Scholar]
- 45.Ghalyanchi Langeroudi A, Babkhani N, Zolfaghari MR, Majidzadeh Arbadili K, Morovvati A, et al. (2013) Detection of Coxeilla brunetii in bulk tank milk samples from dairy bovine farms using nested-PCR in Qom, Iran, 2011. Iranian Journal of Veterinary Medicine 7: 207–211. [Google Scholar]
- 46.Rahimi E, Ameri M, Karim G, Doosti A (2011) Prevalence of Coxiella burnetii in bulk milk samples from dairy bovine, ovine, caprine, and camel herds in Iran as determined by polymerase chain reaction. Foodborne pathogens and disease 8: 307–310. doi: 10.1089/fpd.2010.0684 [DOI] [PubMed] [Google Scholar]
- 47.Herremans T, Hogema BM, Nabuurs M, Peeters M, Wegdam-Blans M, et al. (2013) Comparison of the performance of IFA, CFA, and ELISA assays for the serodiagnosis of acute Q fever by quality assessment. Diagnostic microbiology and infectious disease 75: 16–21. doi: 10.1016/j.diagmicrobio.2012.09.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.