Abstract
Objectives
Hypertension prevalence is high among American Indians (AIs). AIs experience a substantial burden of interpersonal racial discrimination, which in other populations has been associated with higher blood pressure. The purpose of this study is to understand whether racial discrimination experiences are associated with higher blood pressure in AIs.
Materials and Methods
We used the Everyday Discrimination Scale to evaluate the relationship between discrimination and measured blood pressure among 77 AIs from two reservation communities in the Northern Plains. We used multivariate linear regression to evaluate the association of racial discrimination with systolic and diastolic blood pressure, respectively. Racial discrimination, systolic blood pressure, and diastolic blood pressure were analyzed as continuous variables. All analyses adjusted for sex, waist circumference, age, posttraumatic stress disorder status, and education.
Results
We found that 61% of participants experienced discrimination that they attributed to their race or ancestry. Racial discrimination was associated with significantly higher diastolic blood pressure (β = 0.22, SE = 0.09, P = 0.02), and with a similar non-significant trend toward higher systolic blood pressure (β = 0.25, SE = 0.15, P = 0.09).
Conclusion
The results of this analysis suggest that racial discrimination may contribute to higher diastolic blood pressure within Native communities. These findings highlight one pathway through which the social environment can shape patterns of biology and health in AI and other socially and politically marginalized groups.
Keywords: Indigenous, Native health, Racism, Stress physiology, Cardiovascular disease
INTRODUCTION
Although originally founded as the scientific discipline to document distinct racial types, anthropologists have since been among the most staunch advocates for the argument that race is a social, rather than biologically meaningful, construction (Montagu 1942). That said, there are substantial disparities in health, particularly with respect to chronic diseases, among racialized minorities in the US (Adler and Stewart 2010). When discussed, such findings often reify popular conceptions regarding the biological reality of race. In particular, there is a tendency to assume that there are substantial genetic differences between socially described racial groups, and that these in turn contribute to disparities in health among groups (Gravlee 2009; Madrigal et al. 2009). In response to these findings, many anthropologists now adopt a more nuanced approach to race; this involves acknowledging that race is a social construction, but that the social experience of race can have important impacts on biology and actually shape racialized inequalities in health (Gravlee 2009; Kuzawa and Sweet 2009; Thayer and Kuzawa 2011). Research is therefore needed to understand the biological processes through which the social experience of race can shape patterns of human biology and health.
One pathway through which the social experience of race can impact biology is through physiological responses to interpersonal racial discrimination. In particular, repeated racial discrimination can contribute to chronic and continued activation of stress physiology systems (Dressler et al. 2005; Jackson et al. 2010; Turner 2009). The impact of racial discrimination on blood pressure is frequently cited as an example of this pathophysiological process (Brondolo et al. 2011; Dolezsar et al. 2014), and has been well documented among African Americans and Hispanics (Beatty Moody et al. 2016; Dolezsar et al. 2014; Krieger and Sidney 1996). In this regard, a meta-analysis of 44 articles published between 1970 and 2012 found that perceived racial discrimination was associated with hypertensive status (Dolezsar et al. 2014). In sum, these findings suggest that health disparities among African Americans and Hispanics may be attributed, in part, to the experience of racial discrimination across the life course (Berger and Sarnyai 2014; Lewis et al. 2015).
Another population for whom interpersonal racial discrimination may impact health are American Indians (AIs). AIs, the subset of indigenous peoples living in the continental US, reflect diverse tribal backgrounds and cultures, but experience common social, political, and economic disadvantage (Kunitz et al. 2014; Schultz et al. 2016). These disadvantages are often manifested in the form of adverse health outcomes. Although data directly measuring blood pressure are limited for this group relative to others, prior research utilizing self-report data has found that the prevalence of hypertension among AIs is among the highest of all ethnic/racial groups in the US, in both men (Centers for Disease Control and Prevention 2003; Liao et al. 2011) and women (Liao et al. 2011). Although emerging research among AIs highlights the impact of socioeconomic disadvantage on health (Roh et al. 2015; Schell and Gallo 2012), this work has largely neglected the potential additional contribution of racial discrimination to the risk and course of chronic disease.
Although the relationship between discrimination and blood pressure among AIs has not been investigated previously, there is some evidence to suggest that discrimination does influence other aspects of health among AIs. For example, among AI youth, discrimination, when combined with adolescent anger, has been related to early alcohol use (Les Whitbeck et al. 2004; Whitbeck et al. 2001) and depressive symptoms (Johansson et al. 2013; Whitbeck et al. 2002). Among gay, lesbian, and bisexual AIs – referred to as two-spirited persons in Native communities – racial discrimination has been linked to greater physical pain and impairment (Chae and Walters 2009). Lastly, AIs who experience discrimination in healthcare settings have been shown to receive substandard care (Burgess et al. 2008), such as less frequent monitoring of blood pressure (Gonzales et al. 2014). None of these studies examined the relationship between discrimination and blood pressure among AIs. That relationship, if any, is therefore unclear.
Given this background, the purpose of our study is to ascertain whether self-reported racial discrimination is associated with higher clinically measured blood pressure among a sample of AIs from the Northern Plains. This research can contribute to our understanding of how the social experience of race, a substantial source of stress for socially stigmatized groups, shapes patterns of human biology and health.
METHODS
Materials and Methods
Detailed sample characteristics can be found in a previous report (Thayer et al. 2016). Briefly, data for this analysis are derived from the Healing Hearts study of tribal individuals from two reservation communities in the Northern Plains. The purpose of Healing Hearts was to compare individuals with posttraumatic stress disorder (PTSD) to age, sex, and tribe matched non-PTSD participants to understand how PTSD may have shaped cardiovascular disease risk. Thus, within the Healing Hearts sample, approximately half of the participants had been diagnosed with lifetime PTSD. A primary exclusion criterion was overt cardiovascular disease. In addition, participants could not have a condition that would make it unsafe for them to travel to the clinical site in Aurora, Colorado, including unstable angina, myocardial infarction in the past week, severe obstructive lung disease, decompensated heart failure, severe coronary disease, or severe stroke. Although 197 individuals were recruited into the Healing Hearts study, discrimination data were only collected for 107 participants. Twenty-eight participants were then excluded from the analysis due to use of anti-hypertension medication, which would medically control blood pressure, and an additional two participants were missing one or more blood pressure measurements. This resulted in a final analysis sample of 77 individuals. Healing Hearts received approval from the Colorado Multiple Institutional Review Board and by the local tribal communities.
Study Measures
Discrimination
The Williams Everyday Discrimination Scale (EDS)(Williams et al. 1997) was used to assess racial discrimination. Nine questions asked about specific discrimination experiences. In response to the preamble, “In your day-to-day life, how often do the following things happen to you?”, participants indicated if they had been treated with less courtesy than other people; treated with less respect than others, etc. Response alternatives were presented on a 5-point Likert scale: never (0), less than once/year (1), a few times per year (2), a few times per month (3), at least once a week (4), or almost every day (5). An EDS score was calculated for each participant by summing scores across the 9 questions. Cronbach’s alpha for the EDS score in this sample was 0.89, indicating high reliability (Gonzales et al. 2014).
In response to “What do you think is the main reason for these experiences?”, participants answered “yes” or “no” with regard to ancestry, race, gender, height, weight, some other aspect of your appearance, sexual orientation, age, religion, education or income, or other. For the purposes of this study, racial discrimination was defined as checking “yes” to ancestry or race, alone or in combination with other causes. A racial EDS score was created, such that the continuous EDS score was used for participants who cited ancestry and/or race as a cause, and “0” was used for participants who said they were discriminated against for reasons not including ancestry and/or race, or who reported no discrimination at all. Values for the racial EDS score ranged from 0 to 35 out of a possible 45.
Blood pressure
Participants traveled to the University of Colorado Anschutz Medical Campus for a total of three days. Blood pressure was collected twice in the afternoon on two days using a standard mercury sphygmanometer according to the protocol developed by the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (Anonymous 1997). Systolic and diastolic values were collected at each time point, with measures averaged across the four collection points.
Covariates
Participant sex, age (years), and education (college graduate or not) were included as covariates based on a prior meta-analysis that found these factors to be significant covariates in a model using racial discrimination to predict blood pressure (Dolezsar et al. 2014). Since half of the sample had PTSD, and PTSD has been associated with elevated blood pressure (Kibler et al. 2009), we also adjusted for PTSD. Waist circumference was added as an additional covariate given the relationship between this variable and elevated blood pressure (Janssen et al. 2004).
Data Analysis
All continuous variables were initially assessed for normality. Multiple linear regression was used to evaluate the study hypothesis that racial discrimination, as indexed by racial EDS score, was predictive of elevated blood pressure. Racial discrimination was used to predict both diastolic and systolic blood pressure, respectively, with both blood pressure measurements analyzed as continuous variables. Both analyses adjusted for waist circumference, sex, age, PTSD, and college education.
RESULTS
Eighty-eight percent of the sample reported having experienced some form of discrimination (all causes). The most common reported cause of discrimination was race/ancestry (61% of total sample; 68% of those reporting discrimination)(Figure 1). Sample characteristics, stratified by racial discrimination exposure, are summarized in Table 1. Among individuals reporting any racial discrimination experience, mean (SD) systolic blood pressure was 128.1 (15.4) mm Hg and diastolic blood pressure was 77.9 (10.4) mm Hg. Individuals not reporting racial discrimination had mean (SD) systolic and diastolic blood pressure values at 125.9 (11.7) mm Hg and 76.6 (7.4) mm Hg, respectively.
Figure 1.
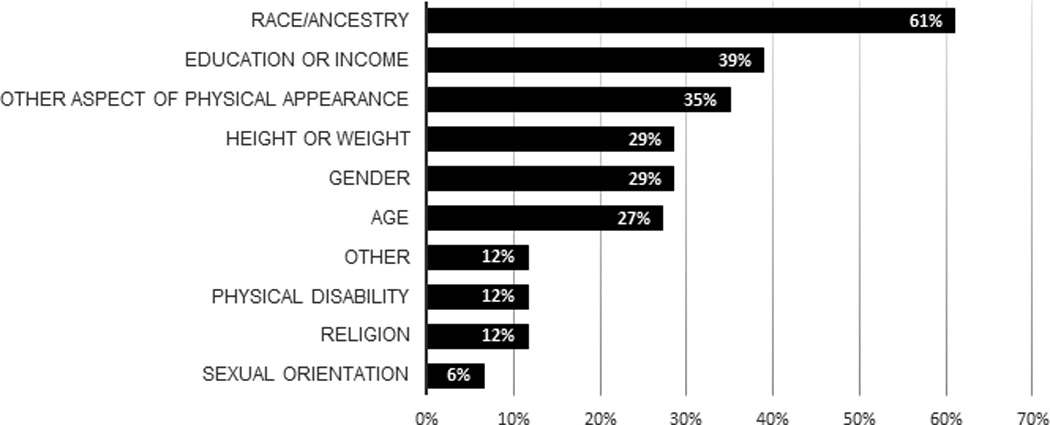
Percent of total sample reporting discrimination associated with each specific cause. Participants were allowed to select more than one cause.
Table 1.
Summary statistics of study sample stratified by racial discrimination experience.
| Total sample (N = 77) |
No Racial discrimination (N =30) |
Racial discrimination (N = 47) |
|
|---|---|---|---|
| Age, y | 41.3 (9.4) | 39.0 (8.3) | 42.7 (9.9) |
| Women, N (%) | 56 (71%) | 20 (67%) | 36 (73%) |
| Waist circumference (cm) | 101.0 (15.9) | 105.2 (16.8) | 98.4 (14.9) |
| BMI (Kg/M2) | 30.8 (7.9) | 32.0 (8.3) | 30.2 (7.6) |
| Systolic blood pressure (mm Hg) | 127.2 (14.0) | 125.9 (11.7) | 128.1 (15.4) |
| Diastolic blood pressure (mm Hg) | 77.4 (9.4) | 76.6 (7.4) | 77.9 (10.4) |
| Racial EDS score | 9.3 (10.4) | 0 | 15.0 (9.5) |
| College graduates, N (%) | 7 (9%) | 1 (3%) | 6 (13%) |
| Married, N (%) | 29 (38%) | 12 (40%) | 17 (36%) |
| PTSD, N (%) | 36 (47%) | 13 (43%) | 23 (49%) |
Mean and SD for continuous variables; count and percentage for categorical variables
In multivariate regression models, racial EDS score, a continuous measure of racial discrimination exposure, was significantly associated with higher mean diastolic blood pressure (β = 0.22 mm Hg, SE = 0.09, P = 0.02)(Table 2). Although it showed a similar effect size, mean systolic blood pressure was not significantly associated with racial EDS score (β = 0.25 mm Hg, SE = 0.15, P = 0.09).
Table 2.
Regression models predicting diastolic and systolic blood pressure, respectively, in response to racial discrimination, as indexed by EDS score (N = 77).
| Diastolic blood pressure | Systolic blood pressure | |||||
|---|---|---|---|---|---|---|
| β | SE | P | β | SE | P | |
| Racial EDS score | 0.22 | 0.09 | 0.02* | 0.25 | 0.15 | 0.09 |
| Female | −8.59 | 2.10 | <0.0001* | −9.80 | 3.40 | 0.005* |
| Waist circumference | 0.04 | 0.06 | 0.5 | 0.17 | 0.10 | 0.11 |
| Age | −0.18 | 0.11 | 0.12 | −0.006 | 0.18 | 0.97 |
| PTSD | 1.31 | 1.96 | 0.50 | 1.84 | 3.17 | 0.56 |
| College | 1.10 | 3.67 | 0.76 | 2.27 | 5.95 | 0.70 |
| Adjusted model R2 | 0.22 | 0.09 | ||||
P < 0.05
DISCUSSION
This is the first study to evaluate whether discrimination experience is related to blood pressure among a sample of AIs. We found that diastolic blood pressure was positively associated with racial discrimination experience. Although the magnitude of the relationship between racial discrimination and blood pressure was similar for both systolic and diastolic values, this relationship only reached statistical significance for diastolic blood pressure. Systolic blood pressure is often considered the better predictor of cardiovascular disease (Franklin 2007), but for individuals less than 50 years of age -- the average age of the current sample -- diastolic blood pressure has been found to be a stronger predictor of cardiovascular disease than systolic blood pressure (Franklin et al. 2001). The results of this analysis are therefore consistent with the hypothesis that racial discrimination may contribute to the high prevalence of cardiovascular disease observed in AIs (Harris et al. 2015).
AIs have the shortest life expectancy of any major racial or ethnic group in the US (Arias et al. 2014), and a high prevalence of hypertension and stroke (Harris et al. 2015). However, the causes underpinning these health inequities are much more poorly understood compared to other groups. Important research in other, non-AI minority groups has highlighted the biological pathways through which social inequalities, such as racial discrimination, can impact health (Brondolo et al. 2009; Dressler et al. 2005; Pascoe and Smart Richman 2009; Salomon and Jagusztyn 2008; Williams and Mohammed 2013). In addition to blood pressure, research has found that racial discrimination is associated with elevated stress hormones such as cortisol (Berger and Sarnyai 2014; Thayer and Kuzawa 2015), decreased heart rate variability (Wagner et al. 2015), and higher allostatic load (Brody et al. 2014). This study therefore represents a first step toward ascertaining one of the biological pathways through which discrimination experienced by Native peoples may impact health within these communities.
Prior research evaluating the relationship between racial discrimination and blood pressure in non-Native populations has yielded some inconsistent results. Some studies, such as the present one, reported the strongest associations with diastolic blood pressure; others noted impacts on systolic blood pressure; still others found neither or both (Brondolo et al. 2011; Couto et al. 2012). This inconsistency could be attributable to many things, such as differences in self-reported versus actually measured blood pressure, as well as differences in the use of specific discrimination scales (Lewis et al. 2015). There also appear to be differences in the relationship between discrimination and blood pressure across socially described racial groups. As an example, a meta-analysis found that the relationship between racial discrimination and diastolic blood pressure was positive for Blacks, but negative for Whites (Dolezsar et al. 2014). These results suggest that the experience of racial discrimination may have stronger and more negative impacts on blood pressure and other physiological systems (Zeiders et al. 2012) when experienced by racial minorities. This could reflect differences in anticipation of prejudice between minority and majority individuals (Sawyer et al. 2012), as well as greater exposure to racial discrimination across multiple domains, including housing, employment, and health care, among minorities (Krieger 2012).
Although not addressing the relationship between racial discrimination and blood pressure directly, prior anthropological research has addressed how the social experience of race influences blood pressure. Gravlee et al., working in Puerto Rico, demonstrated that social classification of race, which shapes inter-personal interactions, was more strongly predictive of blood pressure than either objectively measured skin color (Gravlee et al. 2005) or genetic ancestry markers (Gravlee et al. 2009). Sweet et al., working with a nationally representative sample of African Americans, found that individuals with darker skin and higher incomes had higher systolic blood pressure, while the relationship between incomes and systolic blood pressure was in the opposite direction for individuals with lighter skin (Sweet et al. 2007). The results of our analysis are consistent with these prior studies in suggesting that sociocultural pathways are important mediators of the relationship between the construct of race and blood pressure (Dressler et al. 2012). Interestingly, in our analysis, all-cause discrimination was not significantly associated with diastolic or systolic blood pressure (data not shown). These findings suggest that racial discrimination is a particularly salient stressor among AIs, potentially due to the compounded experiences of colonization and historical trauma that shape individual reaction to, and experience of, racial discrimination in this cultural context (Fast and Collin-Vézina 2010). Additional ethnographic research would be helpful for constructing culturally meaningful models of racial discrimination experience among Native communities.
Conducting studies that evaluate the impact of environmental influences, such as racial discrimination, on blood pressure is important to challenge deterministic approaches that assume health disparities, including but not limited to differences in hypertension, reflect inherent genetic differences between groups. Although many deterministic models, such as the Slavery hypothesis (Wilson and Grim 1991), have been widely critiqued by anthropologists (e.g. (Madrigal et al. 2009), the idea that biological difference equates to genetic difference remains an attractively simple explanation for health disparities since it removes culpability from society (Kaufman and Hall 2003). Ideally, studies would incorporate both genetic and environmental information together, to understand the independent or combined influences of these factors on the outcome of interest. As an example of this type of study, Boulter et al. reported that there was a significant interaction between an Alu insertion polymorphism in the angiotensis-1-converting enzyme (ACE) gene with a measure of unfair treatment in predicting blood pressure among a sample of African Americans (Boulter et al. In press). Aside from interacting with genetic variation, discrimination and other environmental exposures may influence gene expression via changes in epigenetic regulation of genes (Thayer and Non 2015). Additional research is necessary to understand how environmental exposures, the genome, and the epigenome interactively influence complex biological outcomes such as blood pressure.
Racial discrimination has been previously associated with depressive symptoms, substance abuse, and physical pain and impairment among AIs, alluding to the broad mental and physical impacts of this form of discrimination (Chae and Walters 2009; Johansson et al. 2013; Whitbeck et al. 2001; Whitbeck et al. 2002). Importantly, enculturation, which refers to cultural embeddedness as measured by practicing traditional culture and self-reported cultural identity, as well as actualization, which refers to a dimension of racial identity attitude development, had protective influences in these prior studies. This suggests that strong cultural identities and/or engagement in cultural institutions could potentially help to buffer the negative impacts of racial discrimination on blood pressure reported in the present study, and should be investigated in future studies.
While this study is notable for using the gold standard measurement approaches for both discrimination (Quah 2016) and blood pressure (Tholl et al. 2004), there are nonetheless several limitations to this study that deserve acknowledgment. The data are cross-sectional, with discrimination experiences and blood pressure measured over the course of the same 3-day period. However, blood pressure was not collected immediately following the discrimination questionnaire, reducing the likelihood that recalling discrimination experiences may have elicited a stress response and elevated blood pressure in participants. That said, the experience of coming to the study site could be inherently stressful and may have therefore elevated blood pressure among all participants. In addition, other factors not adjusted for in the present analysis, including health behaviors such as physical activity, could also contribute to differences in blood pressure recorded here (Borrell et al. 2013). In addition, since the discrimination instrument was added after the study had already begun, discrimination data were missing for many participants in the larger Healing Hearts study. Finally, the use of a standardized discrimination scale, although useful for comparing the results of this study to those of prior studies in non-Native samples, is also limiting in that it may not capture locally salient models of social status and discrimination. Future research among AIs is needed to verify these reported relationships in larger samples, as well as those from different regions and both reservation and non-reservation communities.
CONCLUSION
Anthropologists have been documenting biological differences between socially described racial groups for many years. What makes contemporary work different from earlier approaches is an emphasis on how environmental exposures may shape patterns of variation, instead of the assumption that biological differences reflect inherent genetic differences between groups (Gravlee 2009; Madrigal 2009). This study contributes to growing inquiry into if and how racial inequalities in health may be mediated by interpersonal interactions, and whether social constructions of race shape biological differences (Berger and Sarnyai 2014; Dolezsar et al. 2014; Gravlee 2009; Lewis et al. 2015). The fact that racial discrimination was associated with diastolic blood pressure suggests that this is a particularly salient stressor among AIs. Unfortunately, indigenous peoples in the US and elsewhere have long experienced extreme poverty and social disenfranchisement, both of which contribute to continued experiences of racial discrimination (Gone and Trimble 2012). Given that the life experiences of Native people vary substantially across urban, rural, and reservation communities, there is a need to characterize the different forms that racial discrimination may take across these settings, as well as how such experiences may affect the risk and course of chronic diseases.
Acknowledgments
We thank the study participants and the participating tribes for their contribution to this research. Alanna Purdy assisted with the literature review. This project was funded by NHLBI R01 HL073824 and GCRC NIH grant M01 #RR00051. ZT analyzed the data for the analysis and drafted the manuscript. DB and SM designed the original study and led data collection. IB, DB, and SM provided critical comments on the manuscript.
REFERENCES
- Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Annals of the New York Academy of Sciences. 2010;1186(1):5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- Anonymous. The sixth report of the National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Archives of Internal Medicine. 1997;157:2413–2446. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- Arias E, Xu J, Jim MA. Period life tables for the Non-Hispanic American Indian and Alaska Native population, 2007–2009. American Journal of Public Health. 2014;104(S3):S312–S319. doi: 10.2105/AJPH.2013.301635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatty Moody DL, Waldstein SR, Tobin JN, Cassells A, Schwartz JC, Brondolo E. Lifetime racial/ethnic discrimination and ambulatory blood pressure: The moderating effect of age. Health Psychology. 2016;35(4):333. doi: 10.1037/hea0000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger M, Sarnyai Z. 'More than skin deep': Stress neurobiology and mental health consequences of racial discrimination. Stress. 2014;(0):1–32. doi: 10.3109/10253890.2014.989204. [DOI] [PubMed] [Google Scholar]
- Borrell LN, Kiefe CI, Diez-Roux AV, Williams DR, Gordon-Larsen P. Racial discrimination, racial/ethnic segregation, and health behaviors in the CARDIA study. Ethnicity & Health. 2013;18(3):227–243. doi: 10.1080/13557858.2012.713092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulter AC, Quinlan J, Miró-Herrans AT, Pearson LN, Todd NL, Gravlee CC, Mulligan CJ. Interaction of Alu Polymorphisms and Novel Measures of Discrimination in Association with Blood Pressure in African Americans Living in Tallahassee. Human Biology. 87(4) doi: 10.13110/humanbiology.87.4.0295. In press. [DOI] [PubMed] [Google Scholar]
- Brody GH, Lei M-K, Chae DH, Yu T, Kogan SM, Beach SRH. Perceived discrimination among African American adolescents and allostatic load: A longitudinal analysis with buffering effects. Child Development. 2014 doi: 10.1111/cdev.12213. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E, Love EE, Pencille M, Schoenthaler A, Ogedegbe G. Racism and hypertension: a review of the empirical evidence and implications for clinical practice. American journal of hypertension. 2011;24(5):518–529. doi: 10.1038/ajh.2011.9. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Ver Halen NB, Pencille M, Beatty D, Contrada RJ. Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal of Behavioral Medicine. 2009;32(1):64–88. doi: 10.1007/s10865-008-9193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Ding Y, Hargreaves M, van Ryn M, Phelan S. The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. Journal of Health Care for the Poor and Underserved. 2008;19(3):894–911. doi: 10.1353/hpu.0.0063. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Health status of American Indians compared with other racial/ethnic minority populations--selected states, 2001–2002. MMWR Morbidity and mortality weekly report. 2003;52(47):1148. [PubMed] [Google Scholar]
- Chae DH, Walters KL. Racial discrimination and racial identity attitudes in relation to self-rated health and physical pain and impairment among two-spirit American Indians/Alaska Natives. American Journal of Public Health. 2009;99(Suppl 1):S144–S151. doi: 10.2105/AJPH.2007.126003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couto PF, Goto JB, Bastos JL. Blood pressure and interpersonal discrimination: systematic review of epidemiologic studies. Arquivos brasileiros de cardiologia. 2012;99(4):956–963. doi: 10.1590/s0066-782x2012005000090. [DOI] [PubMed] [Google Scholar]
- Dolezsar CM, McGrath JJ, Herzig AJ, Miller SB. Perceived racial discrimination and hypertension: A comprehensive systematic review. Health Psychology. 2014;33(1):20. doi: 10.1037/a0033718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler WW, Oths KS, Balieiro MC, Ribeiro RP, Dos Santos JE. How culture shapes the body: Cultural consonance and body mass in urban brazil. American Journal of Human Biology. 2012;24(3):325–331. doi: 10.1002/ajhb.22207. [DOI] [PubMed] [Google Scholar]
- Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: models to explain health disparities. Annu Rev Anthropol. 2005;34:231–252. [Google Scholar]
- Fast E, Collin-Vézina D. Historical trauma, race-based trauma and resilience of indigenous peoples: A literature review. First Peoples Child & Family Review. 2010;5(1):126–136. [Google Scholar]
- Franklin SS. The importance of diastolic blood pressure in predicting cardiovascular risk. Journal of the American Society of Hypertension. 2007;1(1):82–93. doi: 10.1016/j.jash.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, Levy D. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103(9):1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- Gone JP, Trimble JE. American Indian and Alaska Native mental health: Diverse perspectives on enduring disparities. Annual Review of Clinical Psychology. 2012;8(1):131–160. doi: 10.1146/annurev-clinpsy-032511-143127. [DOI] [PubMed] [Google Scholar]
- Gonzales KL, Lambert WE, Fu R, Jacob M, Harding AK. Perceived racial discrimination in health care, completion of standard diabetes services, and diabetes control among a sample of American Indian women. The Diabetes Educator. 2014;40(6):747–755. doi: 10.1177/0145721714551422. [DOI] [PubMed] [Google Scholar]
- Gravlee CC. How race becomes biology: Embodiment of social inequality. American Journal of Physical Anthropology. 2009;139(1):47–57. doi: 10.1002/ajpa.20983. [DOI] [PubMed] [Google Scholar]
- Gravlee CC, Dressler WW, Bernard HR. Skin Color, Social Classification, and Blood Pressure in Southeastern Puerto Rico. American Journal of Public Health. 2005;95(12):2191–2197. doi: 10.2105/AJPH.2005.065615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravlee CC, Non AL, Mulligan CJ. Genetic Ancestry, Social Classification, and Racial Inequalities in Blood Pressure in Southeastern Puerto Rico. PLoS ONE. 2009;4(9):e6821. doi: 10.1371/journal.pone.0006821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris R, Nelson LA, Muller C, Buchwald D. Stroke in American Indians and Alaska Natives: A systematic review. American Journal of Public Health. 2015;105(8):e16–e26. doi: 10.2105/AJPH.2015.302698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. American journal of public health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. The American Journal of Clinical Nutrition. 2004;79(3):379–384. doi: 10.1093/ajcn/79.3.379. [DOI] [PubMed] [Google Scholar]
- Johansson P, Muller CJ, Samos MW, Goldberg J. The influence of perceived discrimination on health-related quality of life in an East Coast American Indian tribe. Journal of Health Care for the Poor and Underserved. 2013;24(4):1531–1541. doi: 10.1353/hpu.2013.0183. [DOI] [PubMed] [Google Scholar]
- Kaufman JS, Hall SA. The slavery hypertension hypothesis: dissemination and appeal of a modern race theory. Epidemiology. 2003;14(1):111–118. doi: 10.1097/00001648-200301000-00027. [DOI] [PubMed] [Google Scholar]
- Kibler JL, Joshi K, Ma M. Hypertension in relation to posttraumatic stress disorder and depression in the US National Comorbidity Survey. Behavioral Medicine. 2009;34(4):125–132. doi: 10.3200/BMED.34.4.125-132. [DOI] [PubMed] [Google Scholar]
- Krieger N. Methods for the Scientific Study of Discrimination and Health: An Ecosocial Approach. American Journal of Public Health. 2012;102(5):936–944. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. American Journal of Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunitz SJ, Veazie M, Henderson JA. Historical trends and regional differences in all-Cause and amenable mortality among American Indians and Alaska Natives since 1950. American Journal of Public Health. 2014;104(S3):S268–S277. doi: 10.2105/AJPH.2013.301684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: Developmental origins of US racial disparities in cardiovascular health. American Journal Of Human Biology. 2009;21(1):2–15. doi: 10.1002/ajhb.20822. [DOI] [PubMed] [Google Scholar]
- Les Whitbeck B, Chen X, Hoyt DR, Adams GW. Discrimination, historical loss and enculturation: culturally specific risk and resiliency factors for alcohol abuse among American Indians. Journal of studies on alcohol. 2004;65(4):409–418. doi: 10.15288/jsa.2004.65.409. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology. 2015;11(1) doi: 10.1146/annurev-clinpsy-032814-112728. null. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Y, Bang D, Cosgrove S, Dulin R, Harris Z, Taylor A, White S, Yatabe G, Liburd L, Giles W. Surveillance of health status in minority communities-Racial and Ethnic approaches to community health across the US (REACH US) Risk Factor Survey, United States, 2009. MMWR Surveillance summaries: Morbidity and mortality weekly report Surveillance summaries/CDC. 2011;60(6):1–44. [PubMed] [Google Scholar]
- Madrigal L, Blell M, Ruiz E Ot, xe, rola D, xe, and n F. Health, Risk, and Adversity. NED - New edition, 1 ed. Berghahn Books; 2009. The Slavery Hypothesis An Evaluation of a Genetic-Deterministic Explanation for Hypertension Prevalence Rate Inequalities; pp. 236–255. [Google Scholar]
- Montagu A. Man's Most Dangerous Myth: The Fallacy of Race. New York: Columbia University Press; 1942. [Google Scholar]
- Pascoe E, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quah SR. International Encyclopedia of Public Health. Elsevier Science; 2016. [Google Scholar]
- Roh S, Brown-Rice KA, Lee KH, Lee Y-S, Lawler MJ, Martin JI. Stressors, coping resources, and depressive symptoms among rural American Indian older adults. Social Work in Public Health. 2015:1–15. doi: 10.1080/19371918.2015.1019174. [DOI] [PubMed] [Google Scholar]
- Salomon K, Jagusztyn NE. Resting cardiovascular levels and reactivity to interpersonal incivility among Black, Latina/o, and White individuals: the moderating role of ethnic discrimination. Health Psychology. 2008;27(4):473. doi: 10.1037/0278-6133.27.4.473. [DOI] [PubMed] [Google Scholar]
- Sawyer PJ, Major B, Casad BJ, Townsend SSM, Mendes WB. Discrimination and the stress response: Psychological and physiological consequences of anticipating prejudice in interethnic interactions. American Journal of Public Health. 2012;102(5):1020–1026. doi: 10.2105/AJPH.2011.300620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell LM, Gallo MV. Overweight and obesity among North American Indian infants, children, and youth. American Journal of Human Biology. 2012;24(3):302–313. doi: 10.1002/ajhb.22257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz K, Walters KL, Beltran R, Stroud S, Johnson-Jennings M. “I'm stronger than I thought”: Native women reconnecting to body, health, and place. Health & Place. 2016;40:21–28. doi: 10.1016/j.healthplace.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet E, McDade TW, Kiefe CI, Liu K. Relationships Between Skin Color, Income, and Blood Pressure Among African Americans in the CARDIA Study. American Journal of Public Health. 2007;97(12):2253–2259. doi: 10.2105/AJPH.2006.088799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer Z, Barbosa-Leiker C, McDonell M, Nelson L, Buchwald D, Manson S. Early life trauma, post-traumatic stress disorder, and allostatic load in a sample of American Indian adults. American Journal of Human Biology. 2016 doi: 10.1002/ajhb.22943. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer ZM, Kuzawa CW. Biological memories of past environments: epigenetic pathways to health disparities. Epigenetics. 2011;6(7):798–803. doi: 10.4161/epi.6.7.16222. [DOI] [PubMed] [Google Scholar]
- Thayer ZM, Kuzawa CW. Ethnic discrimination predicts poor self-rated health and cortisol in pregnancy: Insights from New Zealand. Social Science & Medicine. 2015;128(0):36–42. doi: 10.1016/j.socscimed.2015.01.003. [DOI] [PubMed] [Google Scholar]
- Thayer ZM, Non AL. Anthropology Meets Epigenetics: Current and Future Directions. American Anthropologist. 2015;117(4):722–735. [Google Scholar]
- Tholl U, Forstner K, Anlauf M. Measuring blood pressure: pitfalls and recommendations. Nephrology Dialysis Transplantation. 2004;19(4):766–770. doi: 10.1093/ndt/gfg602. [DOI] [PubMed] [Google Scholar]
- Turner RJ. Advances in the Conceptualization of the Stress Process. Springer; 2009. Understanding health disparities: The promise of the stress process model; pp. 3–21. [Google Scholar]
- Wagner J, Lampert R, Tennen H, Feinn R. Exposure to discrimination and heart rate variability reactivity to acute stress among women with diabetes. Stress and Health. 2015;31(3):255–262. doi: 10.1002/smi.2542. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Hoyt DR, McMorris BJ, Chen X, Stubben JD. Perceived discrimination and early substance abuse among American Indian children. Journal of Health and Social Behavior. 2001;42(4):405–424. [PubMed] [Google Scholar]
- Whitbeck LB, McMorris BJ, Hoyt DR, Stubben JD, LaFromboise T. Perceived discrimination, traditional practices, and depressive symptoms among American Indians in the Upper Midwest. Journal of Health and Social Behavior. 2002;43(4):400–418. [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Racism and health I: Pathways and scientific evidence. American Behavioral Scientist. 2013 doi: 10.1177/0002764213487340. 0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Wilson TW, Grim CE. Biohistory of slavery and blood pressure differences in blacks today. A hypothesis. Hypertension. 1991;17(1 Suppl):I122. doi: 10.1161/01.hyp.17.1_suppl.i122. [DOI] [PubMed] [Google Scholar]
- Zeiders KH, Doane LD, Roosa MW. Perceived discrimination and diurnal cortisol: Examining relations among Mexican American adolescents. Hormones and Behavior. 2012;61(4):541–548. doi: 10.1016/j.yhbeh.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]


