Abstract
Anti-angiogenic therapy has become an important component in the treatment of many solid tumors given the importance of adequate blood supply for tumor growth and metastasis. Despite promising preclinical data and early clinical trials, anti-angiogenic agents have failed to show a survival benefit in randomized controlled trials of patients with glioblastoma. In particular, agents targeting vascular endothelial growth factor (VEGF) appear to prolong progression free survival, possibly improve quality of life, and decrease steroid usage, yet the trials to date have demonstrated no extension of overall survival. In order to improve duration of response and convey a survival benefit, additional research is still needed to explore alternative pro-angiogenic pathways, mechanisms of resistance, combination strategies, and biomarkers to predict therapeutic response.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-016-0510-y) contains supplementary material, which is available to authorized users.
Keywords: Angiogenesis, Glioblastoma, Glioma, Bevacizumab, VEGF
Introduction
Angiogenesis is a hallmark of glioblastoma and remains an important therapeutic target in its treatment. Despite a multimodality approach consisting of surgery in addition to radiation therapy with concurrent and adjuvant temozolomide, the prognosis for glioblastoma remains poor with a median survival of 14−16 months [1, 2]. Because glioblastomas are histologically characterized by microvascular proliferation and express high levels of pro-angiogenic factors such as vascular endothelial growth factor (VEGF), agents that target the VEGF-pathway have been investigated in hopes of expanding currently limited treatment options (Table 1).
Table 1.
Landmark clinical trials of antiangiogenic agents for glioblastoma
| Trial | Phase | Disease type | Patients (n) | Arms | Median PFS (mo) | PFS-6 (%) | Median OS (mo) | Reference |
|---|---|---|---|---|---|---|---|---|
| BRAIN | 2 | rGBM | 167 | BEV | 4.2 | 42.6 | 9.2 | [3] |
| BEV + irinotecan | 5.6 | 50.3 | 8.7 | |||||
| NCI | 2 | rGBM | 48 | BEV | 4.0 | 29.0 | 7.8 | [4] |
| BELOB | 2 | rGBM | 153 | BEV | 3.0 | 16.0 | 8.0 | [5] |
| Lomustine | 1.0 | 13.0 | 8.0 | |||||
| BEV + lomustine | 4.0 | 42.0 | 12.0 | |||||
| EORTC 26101 | 3 | rGBM | 437 | BEV + lomustine | 4.2 | NR | 9.1 | [6] |
| Lomustine | 1.5 | NR | 8.6 | |||||
| REGAL | 3 | rGBM | 325 | Cediranib | 92 days | 16.0 | 8.0 | [7] |
| Cediranib + lomustine | 125 days | 35.0 | 9.4 | |||||
| Lomustine + placebo | 82 days | 25.0 | 9.8 | |||||
| Enzastaurin | 3 | rGBM | 266 | Enzastaurin | 1.5 | 11.1 | 6.6 | [8] |
| Lomustine | 1.6 | 19 | 7.1 | |||||
| RTOG 0825 | 3 | nGBM | 637 | BEV + TMZ/XRT | 10.7 | NR | 15.7 | [9] |
| TMZ/XRT | 7.3 | NR | 16.1 | |||||
| AVAGlio | 3 | nGBM | 921 | BEV + TMZ/XRT | 10.6 | NR | 16.9 | [10] |
| TMZ/XRT | 6.2 | NR | 16.8 | |||||
| GLARIUS | 2 | nGBM (MGMT unmethylated) | 170 | BEV + irinotecan/XRT | 9.7 | 71.1 | 16.6 | [11] |
| TMZ/XRT | 5.9 | 26.2 | 17.3 |
Abbreviations: rGBM recurrent glioblastoma, nGBM newly diagnosed glioblastoma, BEV bevacizumab, TMZ temozolomide, XRT radiation therapy, NR not reported
Bevacizumab is a recombinant, humanized, monoclonal antibody targeting the VEGF ligand A that was first approved for the treatment of metastatic colorectal cancer by the United States Food and Drug Administration (FDA) in 2004. It was subsequently approved for the treatment of non-small cell lung cancer in 2006, followed by renal cell carcinoma and recurrent glioblastoma in 2009 [12–15]. Despite its approval, multiple large phase 3 clinical trials have since failed to show survival benefit in patients with glioblastoma. This review will focus on the rationale behind anti-angiogenic therapy, data regarding the use of bevacizumab in newly diagnosed and recurrent glioblastoma, mechanisms of resistance to anti-VEGF therapy, and emerging areas of research to define optimal use and maximize clinical benefit.
Angiogenesis
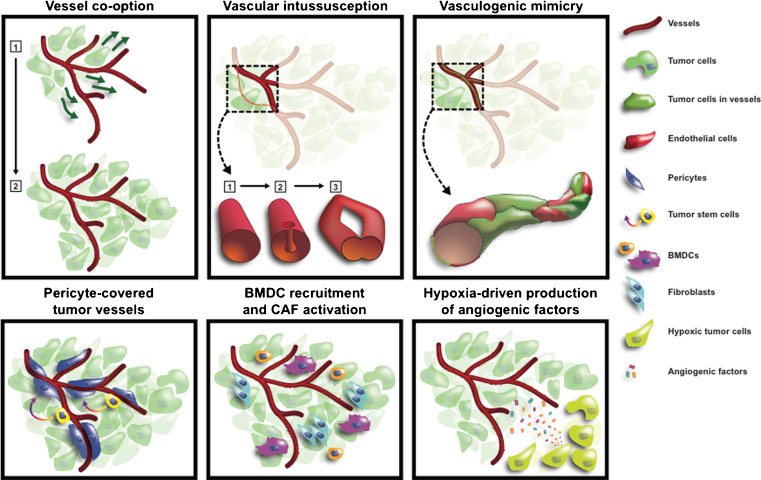
Tumors acquire blood supply through multiple mechanisms of vessel recruitment: (1) angiogenesis, where new vessels sprout from existing vessels; (2) migration and growth of tumor cells around pre-existing vessels through a process known as vessel co-option; (3) intussusception, or dilation and bifurcation of existing vessels; (4) vascular mimicry, whereby tumor cells incorporate into the endothelial lining; (5) recruitment of endothelial progenitor cells; and (6) differentiation of cancer stem-like cells into endothelial cells [16–18]. Nonsprouting mechanisms of vessel recruitment may be important for development of resistance to anti-angiogenic therapy (Fig. 1).
Fig. 1.
Mechanisms of angiogenesis and resistance to anti-VEGF therapy. Resistance to anti-VEGF therapy is thought to occur through the following mechanisms: (1) Vessel co-option: tumor cell migration and growth along native vasculature without new blood vessel formation. (2) Vascular intussusception: enlargement and bifurcation of existing vessels. (3) Vascular mimicry: incorporation of tumor cells into the endothelial lining, possibly through endothelial differentiation of tumor stem cells. (4) Peri-cyte covered vessels may be inherently more resistant to VEGF signaling. (5) Recruitment of bone marrow-derived cells and cancer associated fibroblasts which provide paracrine support. (6) Hypoxia-driven release of alternate angiogenic factors. Reprinted with permission from Lu-Emerson et al, J Clin Oncol 2015 [19]
Glioblastoma vasculature is functionally and structurally abnormal, characterized by uneven vessel diameter, permeability, tortuosity, and thickened basement membranes. This leads to hypoxic regions observed histopathologically as pseudopalisading necrosis, another hallmark of glioblastoma. Hypoxia and angiogenesis are intricately tied to tumor growth and invasion. Hypoxia results in upregulation of hypoxia-inducible factor-1α (HIF-1α), which subsequently leads to upregulation of VEGF [20]. It also promotes cancer cell invasion, genetic instability, stem-like phenotype, epithelial to mesenchymal transition, altered metabolism, and creation of an immunosuppressive environment [21]. In addition to VEGF, other pro-angiogenic factors upregulated in glioblastomas include hepatocyte growth factor (HGF), fibroblast growth factor (FGF), platelet-derived growth factor (PDGF), angiopoietins, and interleukin-8 [22–25]. Angiogenesis is also constitutively activated through non-hypoxia dependent pathways such as Ras/mitogen-activated protein kinase (MAPK) and phosphoinositide-3-kinase (PI3K) [26]. The many contributing pathways involved in angiogenesis create multiple opportunities for therapeutic targeting.
Targeting Angiogenesis and VEGF
Anti-angiogenic strategies have primarily focused on VEGF signaling by using antibodies to bind VEGF, blocking VEGF receptor (VEGFR) activation via small molecule tyrosine kinase inhibitors (TKIs), and directly blocking VEGF binding via engineered peptides or monoclonal antibodies. Many TKIs also have activity against other kinases involved in signaling in endothelial cells and pericytes, such as PDGFR, FGFR, EGFR, KIT, RAF, and RET, and even some types of cancer cells.
Early trials on anti-angiogenic agents in glioblastoma included thalidomide, a weak inhibitor of FGF and VEGF-mediated angiogenesis. It demonstrated modest activity when used alone or in combination with carmustine for recurrent glioblastoma, however there was no benefit observed when it was combined with the DNA alkylating agent temozolomide and radiation in the newly diagnosed setting [27–31]. Other potential angiogenesis inhibitors studied with no clear benefit included agents such as the thalidomide analogue lenalidomide, carboxyamidrotriazole, and penicillamine [32–35].
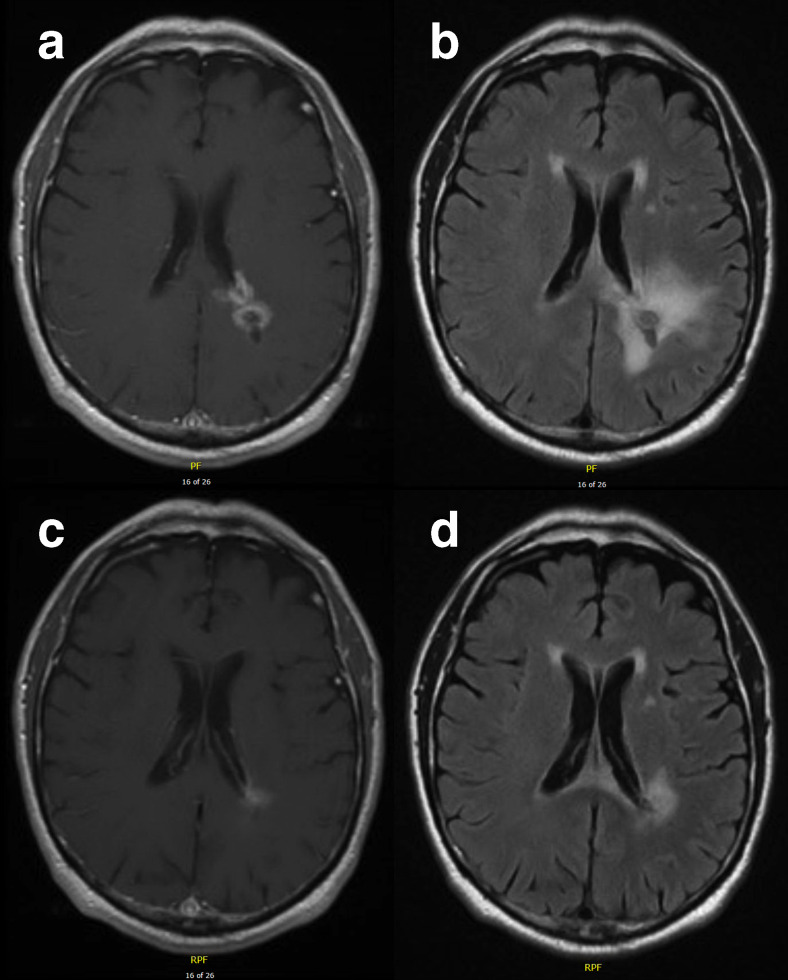
Recent clinical trials have focused on more potent inhibitors of angiogenesis, particularly bevacizumab, a humanized monoclonal antibody that binds VEGF-A with high affinity and specificity. Bevacizumab inhibits angiogenesis and tumor growth in preclinical models of glioblastoma [36–39]. The initial proposed mechanism of action is through decreased tumor perfusion, thereby depriving the tumor of nutrients and oxygen [40]. However, more recent studies have suggested that in the initial stages of treatment and at low doses, anti-angiogenic agents such as bevacizumab normalize tumor blood vessels, thereby improving vessel function and reducing tumor-associated edema [21]. Figure 2 demonstrates the frequently observed partial response with decrease in T2 hyperintensity and enhancement seen after bevacizumab initiation. Unfortunately, this usually transient phenomenon, known as pseudoresponse, does not confer a survival benefit [41, 42]. Increased perfusion is also observed in a subset of glioblastoma patients after bevacizumab and may sensitize the tumor to radiation and chemotherapy [43, 44].
Fig. 2.
Radiographic response to bevacizumab. Magnetic resonance imaging of a patient with left parietal glioblastoma before (A, B) and after (C, D) bevacizumab. There is decreased enhancement (A, C) and decreased T2/FLAIR hyperintensity (B, D) two months after initiating treatment
Numerous receptor tyrosine kinase inhibitors of VEGF and other pro-angiogenic pathways have been tested in clinical trials. However, with the exception of cediranib and enzastaurin, an oral serine/threonine kinase inhibitor, none have progressed beyond phase 2 clinical trials. Despite data showing promising radiographic response rates and progression free survival (PFS) at 6 months, a phase 3 trial demonstrated no difference in PFS or overall survival (OS) in recurrent glioblastoma patients treated with cediranib monotherapy or cediranib with lomustine, an alkylating nitrosourea, versus lomustine alone [45, ]. Enzastaurin, which targets the protein kinase C and PI3K/AKT pathways, showed an objective radiographic response rate of 22% when combined with bevacizumab in a phase 2 study in patients with recurrent glioblastoma [46]. However, a randomized, phase 3 trial of enzastaurin in recurrent glioblastoma showed no improvement in PFS and OS compared to lomustine [8].
In addition to VEGF, other proangiogenic targets include integrins [47–50], transforming growth factor beta (TGF-β) [51, 52], and matrix metalloproteinases (MMPs) [53–55]. MMPs are important for vascular remodeling, recruitment of bone marrow derived cells, and release of cytokines such as integrin [56, 57]. Integrins mediate cell adhesion, proliferation, migration, and invasion and also play a role in activation of TGF-β, which additionally is critical for tumor growth, invasion, and immune regulation [58]. The angiopoietin-2 (Ang-2)/TIE2 pathway has been targeted in systemic malignancies and preclinical models of glioblastoma given its interactions with VEGF and role in vessel stabilization as well as recruitment and reprograming of tumor-associated macrophages [59]. Other pathways under investigation include Delta-like ligand 4 (DLL4)/Notch, important for angiogenic sprouting [60, 61]; HGF/c-Met, important for tumor growth and angiogenesis [62, 63]; and Wnt/β -catenin, thought to promote glioblastoma stem cells, cell invasion and migration, and treatment resistance [64].
As bevacizumab has been the best-studied anti-angiogenic agent with the most promising results, the following sections will focus on the data regarding its use for recurrent and newly diagnosed glioblastoma.
Recurrent Glioblastoma
Two prospective, phase 2 studies led to accelerated FDA approval of bevacizumab as monotherapy for recurrent glioblastoma in 2009. The BRAIN study, completed in 2007, compared bevacizumab to bevacizumab plus irinotecan, an inhibitor of topoisomerase I. Radiographic response was assessed by the WHO Response Evaluation Criteria, which is based on the longest unidimensional measurement of a target enhancing lesion [65], although non-enhancing lesions and steroid dosage were also considered in the study. The overall response rates (ORR) were 28.2% and 37.8% with PFS-6 of 42.6% and 50.3%, respectively [66]. However, the trial was not designed as a superiority trial and allowed for crossover from single agent bevacizumab to the combination arm, potentially confounding the results. A second, single-arm study evaluated 48 recurrent glioblastoma patients treated with bevacizumab at the National Cancer Institute (NCI) and found an ORR of 35% and PFS-6 of 29% [67]. Both the Levin and the MacDonald criteria were used, with the Levin criteria qualitatively assessing enhancement, edema, and mass effect, and the MacDonald criteria focusing on objective bidimensional measurements of an enhancing target lesion [66, 67]. While the FDA approved the use of bevacizumab monotherapy in recurrent GBM based on these two trials, the European Medicines Agency declined approval due to the lack of a non-bevacizumab control arm, modest improvement in OS, and challenges with radiographic response assessment [68].
Multiple studies have also evaluated the use of bevacizumab in combination regimens. The BELOB trial was a randomized phase 2 study of 148 patients with recurrent glioblastoma randomized to lomustine, bevacizumab, or both. Combination therapy resulted in a PFS-6 of 41% compared to 11% and 18% with OS at 9 months of 59% compared to 43% and 38% for lomustine and bevacizumab alone, respectively [69]. Based on these results, a phase 3 study (EORTC 26101) was conducted to compare lomustine versus lomustine plus bevacizumab. There was no significant difference in OS for combination treatment versus lomustine alone, although median PFS was increased from 1.5 to 4.2 months for combination therapy [70].
Additional phase 2 trials have evaluated bevacizumab in combination with irinotecan, cetuximab, carboplatin, etoposide, fotemustine, sorafenib, temozolomide, erlotinib, panobinostat, and temsirolimus [66, 69–88]. There have also been trials evaluating bevacizumab and re-irradiation [89–91]. Unfortunately, none of these trials have demonstrated outcomes superior to historical controls treated with bevacizumab alone.
Newly Diagnosed Glioblastoma
Several early, single-arm phase 2 studies evaluating the use of bevacizumab with temozolomide and radiation showed near doubling of median PFS to 13−14 months compared to historical controls. However, only a modest improvement in median OS to 10−21 months was observed [92–94].
Two randomized, placebo-controlled, phase 3 trials investigated the addition of bevacizumab to standard temozolomide plus radiation (chemoradiation) in patients with newly diagnosed glioblastoma. The AVAglio study compared patients randomized to bevacizumab versus placebo in combination with standard chemoradiation. The PFS was significantly prolonged at 10.6 months in the bevacizumab group compared to 6.2 months in the standard therapy group [95]. The RTOG 0825 study also compared bevacizumab to placebo in combination with standard chemoradiation and demonstrated an improvement in PFS to 10.7 months versus 7.3 months with placebo, although this did not meet the predefined significance level of P = 0.004 [96]. Unfortunately, both studies failed to demonstrate a benefit in OS. Both studies also had crossover rates of 30 to 50%. Thus, the true impact on OS may have been obscured by a large number of patients in the placebo arm who subsequently were treated with bevacizumab at the time of disease progression.
The AVAglio and RTOG 0825 studies also differed in significant ways. While AVAglio used the revised Response Assessment in Neuro-oncology (RANO) criteria to assess disease progression, RTOG 0825 used the traditional Macdonald criteria [67, 95, 96]. Unlike the RANO criteria, the MacDonald criteria do not account for non-enhancing tumor volume, which may be important given the alteration of contrast permeability with bevacizumab. Both trials also attempted to assess other measures of clinical benefit such as performance status, corticosteroid requirement, and quality of life measures. Interestingly, the studies had some divergent findings. While the AVAglio trial showed that bevacizumab prolonged maintenance of performance status, decreased steroid utilization, and prolonged time to deterioration in pre-specified cognitive domains, RTOG 0825 found that bevacizumab led to worsened cognitive function. The cause of the differences is unclear, but possible explanations include different radiographic response criteria, substantial dropout in the RTOG trial, and differences in statistical modeling.
Combination therapies with bevacizumab in newly diagnosed glioblastoma have also been assessed. The randomized, phase 2 GLAIRUS study compared standard of care chemoradiation with temozolomide versus radiation with bevacizumab and irinotecan in patients whose tumors expressed the DNA repair enzyme O6-methyl guanine DNA methyltransferase (MGMT). Loss of MGMT function through gene promoter methylation has been shown to confer increased sensitivity to therapy with temozolomide in glioblastoma [97]. The GLARIUS trial found that PFS was significantly prolonged at 9.7 months in the bevacizumab plus irinotecan arm compared to 5.99 months in the control arm. However, the OS did not significantly differ with OS of 17.5 months in the control arm compared to 16.6 months in the experimental arm. Neither therapy regimen was superior in delaying the time to deterioration in pre-specified dimensions of quality of life [11].
Mechanisms of Resistance
Despite impressive radiographic responses and improved PFS, response to anti-angiogenic therapy is unfortunately not durable. Alternative mechanisms of vessel recruitment are ultimately utilized (Fig. 1). Local hypoxia may trigger alternative pro-angiogenic factors such as HGF, FGF, Ang-2, SDF1α, and interleukin-8 [98–102]. Preclinical studies have shown that dual targeting of VEGF and Ang-2 may overcome this form of resistance to anti-VEGF monotherapy [103–105]. Vessel co-option, the process whereby tumors utilize native brain vessels to recruit blood supply, is also under investigation as an escape mechanism to anti-angiogenic therapy [21]. The molecular mechanisms of vessel co-option are poorly understood and may yield novel therapeutic approaches once the pathways are identified.
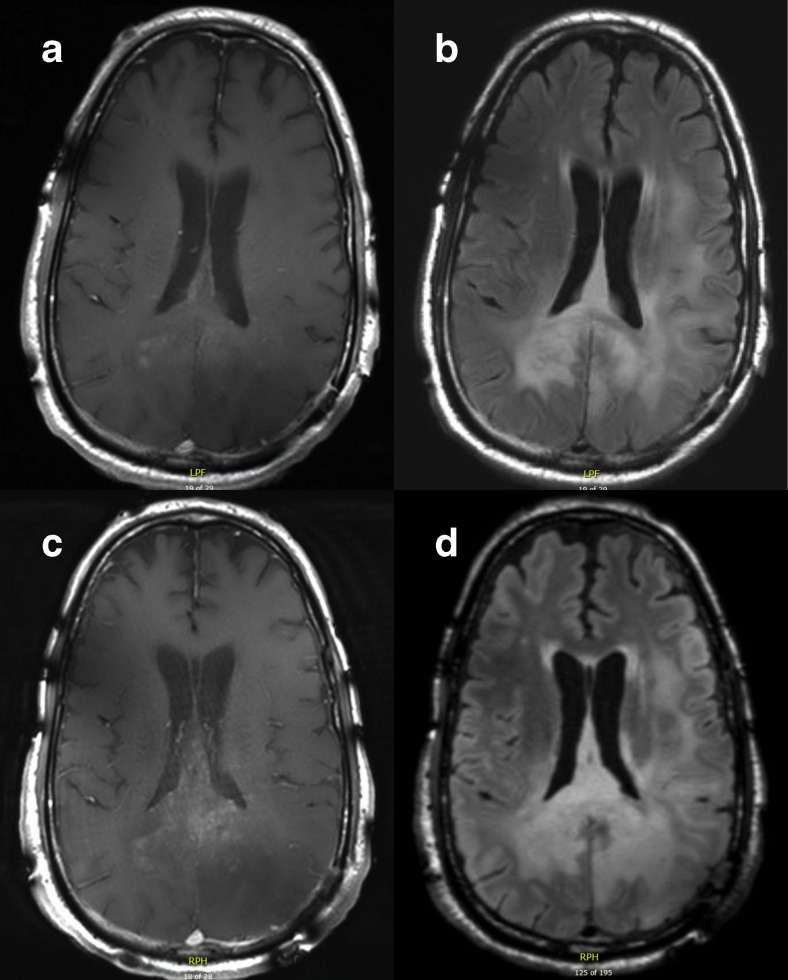
Some tumor vessel subtypes are thought to have inherent insensitivity to VEGF inhibition due to decreased sensitivity of pericytes [106, 107]. There is also preclinical data that anti-angiogenic therapy induces transformation from a proneural to a more invasive mesenchymal phenotype, including upregulation and increased phosphorylation of the receptor tyrosine kinase c-Met [108–110]. Increased invasion may also be mediated by MMPs [111]. Retrospective data in patients found that treatment with bevacizumab was associated with non-enhancing, diffuse or distant recurrence (Fig. 3) [70].
Fig 3.
Disease progression on bevacizumab. Magnetic resonance imaging from a patient with glioblastoma who progressed on bevacizumab. Panels A and B show T1 post-contrast and T2/FLAIR sequences, respectively, of a patient with glioblastoma involving the splenium of the corpus callosum. Panels C and D show post-contrast and T2/FLAIR sequences after one month with notable increase in patchy enhancement and corresponding increase in T2 hyperintensity
Given the potential disease progression via non-enhancing, infiltrative or invasive disease with anti-angiogenic therapy, combination therapy with an agent that targets invasion may also be a promising strategy to overcome resistance. For example, inhibition and knockdown of c-Met inhibit tumor growth and prolong survival in GBM mouse models [108–110]. Interim analysis from a completed phase 2 trial of the monovalent MET inhibitor onartuzumab or placebo with bevacizumab showed no difference in PFS, OS, or ORR, however a phase 1 trial of another c-Met inhibitor INC280 is ongoing (NCT02386826).
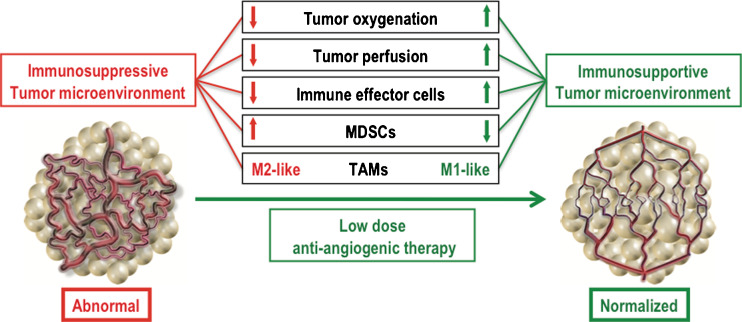
Anti-angiogenesis and the Immune System
Angiogenesis plays an important role in tumor immunity, and the immune composition of the tumor microenvironment changes with vascular normalization and decreased local hypoxia. Preclinical data in extracranial tumors suggest that anti-angiogenic therapies increase tumor delivery of activated T cells, rendering the tumor more susceptible to immune attack [112]. Anti-angiogenic therapy also facilitates the recruitment of bone marrow-derived cells and polarization of tumor associated macrophages to immune stimulatory M1-skewed macrophages (Fig. 4) [20, 113, 114]. Furthermore, increased circulating levels of VEGF inhibit T cell immune response by suppressing maturation of dendritic cell precursors and promoting proliferation of regulatory T cells [112]. However, studies have also suggested that immune activation may play a role in resistance to anti-angiogenic therapy. Peripheral mobilization of myeloid cells via granulocyte colony stimulating factor (G-CSF) has been associated with refractoriness to anti-angiogenic therapy [114, 115]. Pro-angiogenic M2-polarized macrophages may also be important, and strategies to reprogram or inhibit the M2 phenotype, such as through inhibition of Ang-2 or proinflammatory cytokines, have been shown to augment anti-angiogenic therapy in animal models [103, 116, 117].
Fig. 4.
Anti-angiogenic therapy and the immune microenvironment. Abnormal tumor vasculature creates a hypoxic tumor microenvironment, thereby decreasing tumor oxygenation, tumor perfusion, reducing the number of immune effector cells in the microenvironment, increasing myeloid-derived stem cells, and polarizing tumor associated macrophages to the immune inhibitory M2-like phenotype. Low dose anti-VEGF therapy is thought to normalize blood vessels and have the opposite effect. Reprinted with permission from Huang et al, Cancer Res [112]
Despite the conventional notion that the central nervous system is immune-privileged due to the blood brain barrier, the immunomodulatory effect of anti-VEGF has led to recent clinical trials combining bevacizumab with immunotherapy in hopes of a synergistic effect in facilitating anti-tumor immunity. Preliminary results from a phase 2 trial of standard of care chemoradiation versus standard of care plus the dendritic cell vaccine AV0113 in patients with newly diagnosed glioblastoma showed no difference in PFS or OS; however, in the subgroup of 22 patients that received the vaccine as second-line therapy with bevacizumab, there was an improvement in OS compared to the control arm (535 ± 155 days versus 406 ± 224 days) [118]. Preliminary results from the phase 2 study of patients with EGFRvIII mutant recurrent glioblastomas (approximately 20−30% of all primary glioblastomas) demonstrate that the combination of rindopepimut, a peptide vaccine against EGFRvIII, with bevacizumab prolonged median OS from 8.8 months in the control arm (bevacizumab plus keyhole limpet hemocyanin) to 12 months in the experimental arm [54]. PFS-6 was also significantly increased from 11% to 27%. However, the phase 3 ACT IV trial of standard of care with temozolomide versus temozolomide plus rindopepimut was recently stopped after interim analysis showed no difference in median OS (20.4 months in the rindopepimut group versus 21.1 months in the control group, HR 0.99) [119]. The question remains whether rindopepimut may have a more robust effect on survival when combined with an anti-angiogenic therapy such as bevacizumab. In addition to vaccine strategies, adoptive cell transfer (ACT) combined with anti-angiogenic therapy in a mouse model of B16 melanoma showed a synergistic effect with increased infiltration of transferred cells and prolonged survival compared to ACT alone [120].
Ongoing clinical trials for glioblastoma patients are evaluating the use of anti-angiogenic therapy in combination with immune checkpoint inhibitors (pembrolizumab NCT02337491 and durvalumab NCT02336165) and vaccines (SL-701 NCT02078648 and heat shock protein peptide complexes NCT01814813).
Searching for Biomarkers
Unlike other targeted therapies, no established biomarkers currently exist to help predict response to anti-angiogenic therapy. Tissue, serologic, and imaging markers are all under active investigation, although none have yet been validated for use in clinical practice.
Tumor Tissue
Tumor tissue biomarkers have been evaluated mostly in the setting of bevacizumab. In the RTOG-0825 randomized trial, a 10-gene panel assessed the degree of mesenchymal gene enrichment and was significantly associated with worse PFS and OS in response to bevacizumab [121]. Other tissue markers include levels of VEGF, carbonic anhydrase 9 (a marker of hypoxia), and the number of CD68+, CD11+ tumor-associated macrophages [122, 123]. Markers that have not been found to predict response include MGMT methylation status, IDH1, EGFR, PDGFR-α, and c-KIT [124–126].
Blood Biomarkers
Circulating blood biomarkers are particularly important for glioblastomas as repeat surgery for tissue sampling is often not feasible. Candidate biomarkers include VEGF and sVEGFR2, SDF-1α, PIGF, and MMPs [95, 113, 127–129]. Some studies have shown associations between changes in biomarker levels and outcomes. For example, elevated levels of MMP-9, sVEGFR-1 (a negative regulator of VEGF), and SDF-1α have been associated with decreased survival in patients receiving anti-angiogenic agents such as cediranib and aflibercept [45, 130]. On the other hand, increased collagen IV levels have been associated with improved PFS in recurrent glioblastoma [131]. The identification of validated serum biomarkers will aid in drug development as well as noninvasive monitoring and treatment selection in patients.
Imaging Biomarkers
In 2010, the Response Assessment in Neuro-Oncology Working Group proposed the RANO criteria to account for rapid reduction of contrast enhancement after anti-angiogenic therapy as well as transient increase in tumor enhancement shortly after chemoradiation (pseudoprogression) [95]. The criteria include the assessment of non-enhancing lesions and also offers guidelines for distinguishing pseudoprogression from progression. Quantifiable radiographic changes after treatment have led to investigation of various imaging markers to help predict tumor response, including apparent diffusion coefficient [132], restriction spectrum imaging [133], dynamic contrast enhanced (DCE) and dynamic susceptibility-contrast (DSC) techniques [134, 135], vessel architectural imaging [136], and dopamine and positron emission tomography [137, 138]. Consistent with the vascular normalization hypothesis, data suggest that improved perfusion is correlated with increased OS in both newly-diagnosed and recurrent glioblastoma patients treated with the pan-VEGF inhibitor cediranib. In one study, patients with recurrent glioblastoma treated with cediranib, an oral pan-VEGF inhibitor, who had sustained increase in perfusion longer than one month had increased OS of 348 days compared to patients with decreased or stable tumor perfusion (213 days and 169 days, respectively, P < 0.01) [139]. Another study of cediranib in newly diagnosed glioblastoma patients found that patients with durably increased perfusion had a mean OS of 26.3 months compared to 17 months in those with stable or decreased perfusion (P < 0.05) [126]. Thus, early imaging changes in response to anti-angiogenic therapy may help identify patients more likely to benefit from anti-VEGF therapy.
Future Directions
While bevacizumab continues to be a mainstay in the treatment of recurrent glioblastoma, the lack of survival benefit in clinical trials has prompted investigation of biomarkers that can help determine the optimum patient population and predict radiographic response. Although the RANO criteria does account for nonenhancing disease and decreased enhancement after anti-angiogenic therapy, more research is needed to distinguish treatment effect from disease progression and further clarify radiographic response patterns in the setting of altered vascular permeability.
The lack of survival benefit despite increase in progression free survival also highlights the potential importance of secondary endpoints such as quality of life measures and steroid usage. Given the vital location, slight radiographic progression of a glioblastoma or increased edema can translate into a disproportionate impact on functional status. While clinical trials and new therapies should continue to focus on prolonging survival, there remains a need to better characterize the impact on day-to-day challenges patients face.
Another area of investigation includes optimal dosing and timing of bevacizumab or other anti-angiogenic therapies. Retrospective data suggest that the treatment of patients with high-grade glioma with low doses of bevacizumab (5 mg/kg per week or 7.5 mg/kg every 3−4 weeks) may be superior to standard dosing, potentially due to vascular normalization at lower doses [140, 141]. A recent randomized phase 2 trial comparing low dose bevacizumab plus lomustine to standard dose bevacizumab monotherapy in recurrent GBM showed no difference in the primary endpoint of PFS (4.34 months for the combination arm versus 4.11 months for bevacizumab monotherapy, p = 0.19) [142]. However, there was a trend toward improved median PFS in patients with first recurrence. Due to the potential of rebound cerebral edema after discontinuation of bevacizumab, salvage therapy has been difficult, leading many patients and oncologists to delay bevacizumab as long as possible. However, it is unclear to what extent this delay is warranted as additional retrospective data in systemic malignancies indicate that there may be benefit to continuing anti-angiogenic therapy past progression [143–146].
While optimizing bevacizumab administration is important, the multiple, complex pathways that promote angiogenesis also support the use of combination strategies. Improved orthotopic animal models from patient-derived tumors will play an important role in the evaluation of new therapies, treatment combinations, and resistance mechanisms, although these models will have limited utility in the evaluation of immunotherapies. It is notable that the only randomized clinical trial that appeared to confer some improvement in survival was in patients with recurrent glioblastoma treated with bevacizumab and chemotherapy. Thus, targeting several pathways or combining anti-angiogenic agents with other classes of drugs such as immunotherapy may prevent the development of treatment resistance and maximize survival benefit.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 932 kb)
Acknowledgments
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert MR, Wang M, Aldape KD, et al. Dose-dense temozolomide for newly diagnosed glioblastoma: a randomized phase III clinical trial. J Clin Oncol. 2013;31:4085–91. doi: 10.1200/JCO.2013.49.6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman HS, Prados MD, Wen PY, et al (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27:4733–4740 [DOI] [PubMed]
- 4.Kreisl TN, Kim L, Moore K, et al (2009) Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 27:740–745 [DOI] [PMC free article] [PubMed]
- 5.Taal W, Oosterkamp HM, Walenkamp AME, et al (2014) Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): A randomised controlled phase 2 trial. Lancet Oncol 15:943–953 [DOI] [PubMed]
- 6.Wick W, Brandes A, Gorlia T, et al (2015) Phase III trial exploring the combination of bevacizumab and lomustine in patients with first recurrence of a glioblastoma: the EORTC 26101 trial. Neuro Oncol 17:v1.5-v1
- 7.Batchelor TT, Mulholland P, Neyns B, et al (2013) Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J Clin Oncol 31:3212–3218 [DOI] [PMC free article] [PubMed]
- 8.Wick W, Puduvalli VK, Chamberlain MC, et al (2010) Phase III study of enzastaurin compared with lomustine in the treatment of recurrent intracranial glioblastoma. J Clin Oncol 28:1168–1174 [DOI] [PMC free article] [PubMed]
- 9.Gilbert MR, Dignam JJ, Armstrong TS, et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370:699–708 [DOI] [PMC free article] [PubMed]
- 10.Chinot OL, Wick W, Mason W, et al (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370:709–722 [DOI] [PubMed]
- 11.Herrlinger U, Schäfer N, Steinbach JP, et al (2016) Bevacizumab plus irinotecan versus temozolomide in newly diagnosed O6-methylguanine-DNA methyltransferase nonmethylated glioblastoma: the randomized GLARIUS trial. J Clin Oncol. doi: 10.1200/JCO.2015.63.4691 [DOI] [PubMed]
- 12.Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–42. doi: 10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 13.Cohen MH, Gootenberg J, Keegan P, Pazdur R. FDA drug approval summary: bevacizumab (Avastin(R)) plus carboplatin and paclitaxel as first-line treatment of advanced/metastatic recurrent nonsquamous non-small cell lung cancer. Oncologist. 2007;12:713–718. doi: 10.1634/theoncologist.12-6-713. [DOI] [PubMed] [Google Scholar]
- 14.Summers J, Cohen MH, Keegan P, Pazdur R. FDA drug approval summary: bevacizumab plus interferon for advanced renal cell carcinoma. Oncologist. 2010;15:104–111. doi: 10.1634/theoncologist.2009-0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen MH, Shen YL, Keegan P, Pazdur R. FDA drug approval summary: bevacizumab (Avastin) as treatment of recurrent glioblastoma multiforme. Oncologist. 2009;14:1131–1138. doi: 10.1634/theoncologist.2009-0121. [DOI] [PubMed] [Google Scholar]
- 16.Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang R, Chadalavada K, Wilshire J, Kowalik U, Hovinga KE, Geber A, Fligelman B, Leversha M, Brennan C, Tabar V. Glioblastoma stem-like cells give rise to tumour endothelium. Nature. 2010;468:829–833. doi: 10.1038/nature09624. [DOI] [PubMed] [Google Scholar]
- 18.Ricci-Vitiani L, Pallini R, Biffoni M, et al. Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature. 2010;468:824–8. doi: 10.1038/nature09557. [DOI] [PubMed] [Google Scholar]
- 19.Lu-Emerson C, Duda DG, Emblem KE, Taylor JW, Gerstner ER, Loeffler JS, Batchelor TT, Jain RK. Lessons from anti-vascular endothelial growth factor and anti-vascular endothelial growth factor receptor trials in patients with glioblastoma. J Clin Oncol. 2015;33:1197–1213. doi: 10.1200/JCO.2014.55.9575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du R, Lu KV, Petritsch C, et al. HIF1alpha induces the recruitment of bone marrow-derived vascular modulatory cells to regulate tumor angiogenesis and invasion. Cancer Cell. 2008;13:206–20. doi: 10.1016/j.ccr.2008.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jain RK. Antiangiogenesis strategies revisited: from starving tumors to alleviating hypoxia. Cancer Cell. 2014;26:605–622. doi: 10.1016/j.ccell.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shih AH, Holland EC. Platelet-derived growth factor (PDGF) and glial tumorigenesis. Cancer Lett. 2006;232:139–147. doi: 10.1016/j.canlet.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Reiss Y, Machein MR, Plate KH. The role of angiopoietins during angiogenesis in gliomas. Brain Pathol. 2005;15:311–317. doi: 10.1111/j.1750-3639.2005.tb00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brat DJ, Bellail AC, Van Meir EG. The role of interleukin-8 and its receptors in gliomagenesis and tumoral angiogenesis. Neuro Oncol. 2005;7:122–33. doi: 10.1215/S1152851704001061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmidt NO, Westphal M, Hagel C, Ergün S, Stavrou D, Rosen EM, Lamszus K. Levels of vascular endothelial growth factor, hepatocyte growth factor/scatter factor and basic fibroblast growth factor in human gliomas and their relation to angiogenesis. Int J Cancer. 1999;84:10–8. doi: 10.1002/(sici)1097-0215(19990219)84:1<10::aid-ijc3>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 26.Jayson GC, Kerbel R, Ellis LM, Harris AL (2016) Antiangiogenic therapy in oncology: current status and future directions. Lancet (London, England) 70:6171–80 [DOI] [PubMed]
- 27.Fine HA, Figg WD, Jaeckle K, et al. Phase II trial of the antiangiogenic agent thalidomide in patients with recurrent high-grade gliomas. J Clin Oncol. 2000;18:708–15. doi: 10.1200/JCO.2000.18.4.708. [DOI] [PubMed] [Google Scholar]
- 28.Marx GM, Pavlakis N, McCowatt S, Boyle FM, Levi JA, Bell DR, Cook R, Biggs M, Little N, Wheeler HR. Phase II study of thalidomide in the treatment of recurrent glioblastoma multiforme. J Neurooncol. 2001;54:31–8. doi: 10.1023/a:1012554328801. [DOI] [PubMed] [Google Scholar]
- 29.Chang SM, Lamborn KR, Malec M, Larson D, Wara W, Sneed P, Rabbitt J, Page M, Nicholas MK, Prados MD. Phase II study of temozolomide and thalidomide with radiation therapy for newly diagnosed glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2004;60:353–357. doi: 10.1016/j.ijrobp.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 30.Fine HA, Wen PY, Maher EA, Viscosi E, Batchelor T, Lakhani N, Figg WD, Purow BW, Borkowf CB. Phase II trial of thalidomide and carmustine for patients with recurrent high-grade gliomas. J Clin Oncol. 2003;21:2299–2304. doi: 10.1200/JCO.2003.08.045. [DOI] [PubMed] [Google Scholar]
- 31.Kesari S, Schiff D, Henson JW, et al. Phase II study of temozolomide, thalidomide, and celecoxib for newly diagnosed glioblastoma in adults. Neuro Oncol. 2008;10:300–308. doi: 10.1215/15228517-2008-005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Drappatz J, Wong ET, Schiff D, et al. A pilot safety study of lenalidomide and radiotherapy for patients with newly diagnosed glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2009;73:222–227. doi: 10.1016/j.ijrobp.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 33.Fine HA, Kim L, Albert PS, Duic JP, Ma H, Zhang W, Tohnya T, Figg WD, Royce C. A phase I trial of lenalidomide in patients with recurrent primary central nervous system tumors. Clin Cancer Res. 2007;13:7101–6. doi: 10.1158/1078-0432.CCR-07-1546. [DOI] [PubMed] [Google Scholar]
- 34.Mikkelsen T, Lush R, Grossman SA, Carson KA, Fisher JD, Alavi JB, Rosenfeld S. Phase II clinical and pharmacologic study of radiation therapy and carboxyamido-triazole (CAI) in adults with newly diagnosed glioblastoma multiforme. Invest New Drugs. 2007;25:259–63. doi: 10.1007/s10637-006-9023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brem S, Grossman S a, Carson K a, New P, Phuphanich S, Alavi JB, Mikkelsen T, Fisher JD (2005) Phase 2 trial of copper depletion and penicillamine as antiangiogenesis therapy of glioblastoma. Neuro Oncol 7:246–253 [DOI] [PMC free article] [PubMed]
- 36.Kim KJ, Li B, Winer J, Armanini M, Gillett N, Phillips HS, Ferrara N. Inhibition of vascular endothelial growth factor-induced angiogenesis suppresses tumour growth in vivo. Nature. 1993;362:841–4. doi: 10.1038/362841a0. [DOI] [PubMed] [Google Scholar]
- 37.Rubenstein JL, Kim J, Ozawa T, Zhang M, Westphal M, Deen DF, Shuman MA. Anti-VEGF antibody treatment of glioblastoma prolongs survival but results in increased vascular cooption. Neoplasia. 2000;2:306–14. doi: 10.1038/sj.neo.7900102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jahnke K, Muldoon LL, Varallyay CG, Lewin SJ, Kraemer DF, Neuwelt EA. Bevacizumab and carboplatin increase survival and asymptomatic tumor volume in a glioma model. Neuro Oncol. 2009;11:142–150. doi: 10.1215/15228517-2008-077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee CG, Heijn M, di Tomaso E, et al. Anti-vascular endothelial growth factor treatment augments tumor radiation response under normoxic or hypoxic conditions. Cancer Res. 2000;60:5565–5570. [PubMed] [Google Scholar]
- 40.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285:1182–6. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 41.Ellingson BM, Cloughesy TF, Lai A, Nghiemphu PL, Mischel PS, Pope WB. Quantitative volumetric analysis of conventional MRI response in recurrent glioblastoma treated with bevacizumab. Neuro Oncol. 2011;13:401–409. doi: 10.1093/neuonc/noq206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gorlia T, Stupp R, Brandes AA, et al. New prognostic factors and calculators for outcome prediction in patients with recurrent glioblastoma: A pooled analysis of EORTC Brain Tumour Group phase i and II clinical trials. Eur J Cancer. 2012;48:1176–1184. doi: 10.1016/j.ejca.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 43.Winkler F, Kozin SV, Tong RT, et al. Kinetics of vascular normalization by VEGFR2 blockade governs brain tumor response to radiation: Role of oxygenation, angiopoietin-1, and matrix metalloproteinases. Cancer Cell. 2004;6:553–563. doi: 10.1016/j.ccr.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 44.Batchelor TT, Sorensen AG, di Tomaso E, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007;11:83–95. doi: 10.1016/j.ccr.2006.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Batchelor TT, Duda DG, Di Tomaso E, et al. Phase II study of cediranib, an oral pan-vascular endothelial growth factor receptor tyrosine kinase inhibitor, in patients with recurrent glioblastoma. J Clin Oncol. 2010;28:2817–2823. doi: 10.1200/JCO.2009.26.3988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Odia Y, Iwamoto FM, Moustakas A, Fraum TJ, Salgado CA, Li A, Kreisl TN, Sul J, Butman JA, Fine HA. A phase II trial of enzastaurin (LY317615) in combination with bevacizumab in adults with recurrent malignant gliomas. J Neurooncol. 2016;127:127–135. doi: 10.1007/s11060-015-2020-x. [DOI] [PubMed] [Google Scholar]
- 47.Nabors LB, Mikkelsen T, Rosenfeld SS, et al. Phase I and correlative biology study of cilengitide in patients with recurrent malignant glioma. J Clin Oncol. 2007;25:1651–7. doi: 10.1200/JCO.2006.06.6514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reardon DA, Fink KL, Mikkelsen T, et al. Randomized phase II study of cilengitide, an integrin-targeting arginine-glycine-aspartic acid peptide, in recurrent glioblastoma multiforme. J Clin Oncol. 2008;26:5610–5617. doi: 10.1200/JCO.2008.16.7510. [DOI] [PubMed] [Google Scholar]
- 49.Stupp R, Hegi ME, Neyns B, et al. Phase I/IIa study of cilengitide and temozolomide with concomitant radiotherapy followed by cilengitide and temozolomide maintenance therapy in patients with newly diagnosed glioblastoma. J Clin Oncol. 2010;28:2712–2718. doi: 10.1200/JCO.2009.26.6650. [DOI] [PubMed] [Google Scholar]
- 50.Stupp R, Hegi ME, Gorlia T, et al. Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071-22072 study): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15:1100–1108. doi: 10.1016/S1470-2045(14)70379-1. [DOI] [PubMed] [Google Scholar]
- 51.Bogdahn U, Hau P, Stockhammer G, et al. Targeted therapy for high-grade glioma with the TGF-beta2 inhibitor trabedersen: Results of a randomized and controlled phase IIb study. Neuro Oncol. 2011;13:132–142. doi: 10.1093/neuonc/noq142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schlingensiepen KH, Schlingensiepen R, Steinbrecher A, Hau P, Bogdahn U, Fischer-Blass B, Jachimczak P. Targeted tumor therapy with the TGF-beta 2 antisense compound AP 12009. Cytokine Growth Factor Rev. 2006;17:129–139. doi: 10.1016/j.cytogfr.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 53.Groves MD, Puduvalli VK, Hess KR, Jaeckle KA, Peterson P, Yung WKA, Levin VA. Phase II trial of temozolomide plus the matrix metalloproteinase inhibitor, marimastat, in recurrent and progressive glioblastoma multiforme. J Clin Oncol. 2002;20:1383–8. doi: 10.1200/JCO.2002.20.5.1383. [DOI] [PubMed] [Google Scholar]
- 54.Levin VA, Phuphanich S, Glantz MJ, et al (2002) Randomized phase II study of temozolomide (TMZ) with and without the matrix metalloprotease (MMP) inhibitor prinomastat in patients (pts) with glioblastoma multiforme (GBM) following best surgery and radiation therapy. Proc Am Soc Clin Oncol 21:26a
- 55.Levin VA, Phuphanich S, Yung WKA, Forsyth PA, Del Maestro R, Perry JR, Fuller GN, Baillet M. Randomized, double-blind, placebo-controlled trial of marimastat in glioblastoma multiforme patients following surgery and irradiation. J Neurooncol. 2006;78:295–302. doi: 10.1007/s11060-005-9098-5. [DOI] [PubMed] [Google Scholar]
- 56.Heissig B, Hattori K, Dias S, et al. Recruitment of stem and progenitor cells from the bone marrow niche requires MMP-9 mediated release of kit-ligand. Cell. 2002;109:625–37. doi: 10.1016/s0092-8674(02)00754-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rundhaug JE. Matrix metalloproteinases and angiogenesis. Angiogenesis Review Series. J Cell Mol Med. 2005;9:267–285. doi: 10.1111/j.1582-4934.2005.tb00355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Massagué J. TGFb in cancer. Cell. 2008;134:215–230. doi: 10.1016/j.cell.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gerald D, Chintharlapalli S, Augustin HG, Benjamin LE. Angiopoietin-2: An attractive target for improved antiangiogenic tumor therapy. Cancer Res. 2013;73:1649–1657. doi: 10.1158/0008-5472.CAN-12-4697. [DOI] [PubMed] [Google Scholar]
- 60.Kangsamaksin T, Murtomaki A, Kofler NM, Cuervo H, Chaudhri RA, Tattersall IW, Rosenstiel PE, Shawber CJ, Kitajewski J. NOTCH decoys that selectively block DLL/NOTCH or JAG/NOTCH disrupt angiogenesis by unique mechanisms to inhibit tumor growth. Cancer Discov. 2015;5:182–97. doi: 10.1158/2159-8290.CD-14-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Smith DC, Eisenberg PD, Manikhas G, Chugh R, Gubens MA, Stagg RJ, Kapoun AM, Xu L, Dupont J, Sikic B. A phase I dose escalation and expansion study of the anticancer stem cell agent demcizumab (Anti-DLL4) in patients with previously treated solid tumors. Clin Cancer Res. 2014;20:6295–6303. doi: 10.1158/1078-0432.CCR-14-1373. [DOI] [PubMed] [Google Scholar]
- 62.Wen PY, Schiff D, Cloughesy TF, et al. A phase II study evaluating the efficacy and safety of AMG 102 (rilotumumab) in patients with recurrent glioblastoma. Neuro Oncol. 2011;13:437–446. doi: 10.1093/neuonc/noq198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cloughesy TF, Finocchiaro G, Belda C, Recht L, Brandes AA, Weller M, Liu B, Bruey J, Verret W (2015) Onartuzumab plus bevacizumab versus placebo plus bevacizumab in recurrent glioblastoma (GBM): HGF and MGMT biomarker data. J Clin Oncol 33:abstr 2015
- 64.Lee Y, Lee J-K, Ahn SH, Lee J, Nam D-H. WNT signaling in glioblastoma and therapeutic opportunities. Lab Investig. 2015;0:1–14. doi: 10.1038/labinvest.2015.140. [DOI] [PubMed] [Google Scholar]
- 65.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 66.Levin VA, Crafts DC, Norman DM, Hoffer PB, Spire J-P, Wilson CB. Criteria for evaluating patients undergoing chemotherapy for malignant brain tumors. J Neurosurg. 1977;47:329–335. doi: 10.3171/jns.1977.47.3.0329. [DOI] [PubMed] [Google Scholar]
- 67.Macdonald DR, Cascino TL, Schold SC, Cairncross JG. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol. 1990;8:1277–80. doi: 10.1200/JCO.1990.8.7.1277. [DOI] [PubMed] [Google Scholar]
- 68.Wick W, Weller M, Van Den Bent M, Stupp R. Bevacizumab and recurrent malignant gliomas: A European perspective. J Clin Oncol. 2010;28:188–189. doi: 10.1200/JCO.2009.26.9027. [DOI] [PubMed] [Google Scholar]
- 69.Lee EQ, Reardon DA, Schiff D, et al. Phase II study of panobinostat in combination with bevacizumab for recurrent glioblastoma and anaplastic glioma. Neuro Oncol. 2015;17:862–867. doi: 10.1093/neuonc/nou350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Norden AD, Young GS, Setayesh K, et al. Bevacizumab for recurrent malignant gliomas: efficacy, toxicity, and patterns of recurrence. Neurology. 2008;70:779–87. doi: 10.1212/01.wnl.0000304121.57857.38. [DOI] [PubMed] [Google Scholar]
- 71.Francesconi AB, Dupre S, Matos M, Martin D, Hughes BG, Wyld DK, Lickliter JD. Carboplatin and etoposide combined with bevacizumab for the treatment of recurrent glioblastoma multiforme. J Clin Neurosci. 2010;17:970–4. doi: 10.1016/j.jocn.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 72.Reardon DA, Desjardins A, Peters KB, et al. Phase II study of carboplatin, irinotecan, and bevacizumab for bevacizumab naïve, recurrent glioblastoma. J Neurooncol. 2012;107:155–64. doi: 10.1007/s11060-011-0722-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reardon DA, Desjardins A, Vredenburgh JJ, et al. Metronomic chemotherapy with daily, oral etoposide plus bevacizumab for recurrent malignant glioma: a phase II study. Br J Cancer. 2009;101:1986–94. doi: 10.1038/sj.bjc.6605412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ali SA, McHayleh WM, Ahmad A, Sehgal R, Braffet M, Rahman M, Bejjani G, Friedland DM. Bevacizumab and irinotecan therapy in glioblastoma multiforme: a series of 13 cases. J Neurosurg. 2008;109:268–72. doi: 10.3171/JNS/2008/109/8/0268. [DOI] [PubMed] [Google Scholar]
- 75.Bokstein F, Shpigel S, Blumenthal DT. Treatment with bevacizumab and irinotecan for recurrent high-grade glial tumors. Cancer. 2008;112:2267–2273. doi: 10.1002/cncr.23401. [DOI] [PubMed] [Google Scholar]
- 76.Kang TY, Jin T, Elinzano H, Peereboom D. Irinotecan and bevacizumab in progressive primary brain tumors, an evaluation of efficacy and safety. J Neurooncol. 2008;89:113–118. doi: 10.1007/s11060-008-9599-0. [DOI] [PubMed] [Google Scholar]
- 77.Zuniga RM, Torcuator R, Jain R, Anderson J, Doyle T, Ellika S, Schultz L, Mikkelsen T. Efficacy, safety and patterns of response and recurrence in patients with recurrent high-grade gliomas treated with bevacizumab plus irinotecan. J Neurooncol. 2009;91:329–336. doi: 10.1007/s11060-008-9718-y. [DOI] [PubMed] [Google Scholar]
- 78.Nghiemphu PL, Liu W, Lee Y, et al. Bevacizumab and chemotherapy for recurrent glioblastoma: A single-institution experience. Neurology. 2009;72:1217–1222. doi: 10.1212/01.wnl.0000345668.03039.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Desjardins A, Reardon DA, Coan A, Marcello J, Herndon JE, Bailey L, Peters KB, Friedman HS, Vredenburgh JJ. Bevacizumab and daily temozolomide for recurrent glioblastoma. Cancer. 2012;118:1302–1312. doi: 10.1002/cncr.26381. [DOI] [PubMed] [Google Scholar]
- 80.Sathornsumetee S, Desjardins A, Vredenburgh JJ, et al. Phase II trial of bevacizumab and erlotinib in patients with recurrent malignant glioma. Neuro Oncol. 2010;12:1300–1310. doi: 10.1093/neuonc/noq099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Galanis E, Anderson SK, Lafky JM, et al. Phase II study of bevacizumab in combination with sorafenib in recurrent glioblastoma (N0776): a north central cancer treatment group trial. Clin Cancer Res. 2013;19:4816–23. doi: 10.1158/1078-0432.CCR-13-0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Drappatz J, Lee EQ, Hammond S, et al. Phase I study of panobinostat in combination with bevacizumab for recurrent high-grade glioma. J Neurooncol. 2012;107:133–8. doi: 10.1007/s11060-011-0717-z. [DOI] [PubMed] [Google Scholar]
- 83.Lassen U, Sorensen M, Gaziel TB, Hasselbalch B, Poulsen HS. Phase II study of bevacizumab and temsirolimus combination therapy for recurrent glioblastoma multiforme. Anticancer Res. 2013;33:1657–1660. [PubMed] [Google Scholar]
- 84.Møller S, Grunnet K, Hansen S, Schultz H, Holmberg M, Sorensen M, Poulsen HS, Lassen U. A phase II trial with bevacizumab and irinotecan for patients with primary brain tumors and progression after standard therapy. Acta Oncol (Madr) 2012;51:797–804. doi: 10.3109/0284186X.2012.681063. [DOI] [PubMed] [Google Scholar]
- 85.Soffietti R, Trevisan E, Bertero L, et al. Bevacizumab and fotemustine for recurrent glioblastoma: A phase II study of AINO (Italian Association of Neuro-Oncology) J Neurooncol. 2014;116:533–541. doi: 10.1007/s11060-013-1317-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Reardon DA, Desjardins A, Peters KB, et al. Phase 2 study of carboplatin, irinotecan, and bevacizumab for recurrent glioblastoma after progression on bevacizumab therapy. Cancer. 2011;117:5351–8. doi: 10.1002/cncr.26188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Raizer JJ, Giglio P, Hu J, et al. A phase II study of bevacizumab and erlotinib after radiation and temozolomide in MGMT unmethylated GBM patients. J Neurooncol. 2016;126:185–192. doi: 10.1007/s11060-015-1958-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Field KM, Simes J, Nowak AK, et al. Randomized phase 2 study of carboplatin and bevacizumab in recurrent glioblastoma. Neuro Oncol. 2015;17:1504–1513. doi: 10.1093/neuonc/nov104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cuneo KC, Vredenburgh JJ, Sampson JH, Reardon DA, Desjardins A, Peters KB, Friedman HS, Willett CG, Kirkpatrick JP. Safety and efficacy of stereotactic radiosurgery and adjuvant bevacizumab in patients with recurrent malignant gliomas. Int J Radiat Oncol Biol Phys. 2013;82:2018–2024. doi: 10.1016/j.ijrobp.2010.12.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cabrera AR, Cuneo KC, Vredenburgh JJ, Sampson JH, Kirkpatrick JP. Stereotactic radiosurgery and bevacizumab for recurrent glioblastoma multiforme. J Natl Compr Canc Netw. 2012;10:695–699. doi: 10.6004/jnccn.2012.0072. [DOI] [PubMed] [Google Scholar]
- 91.Gutin PH, Iwamoto FM, Beal K, Mohile NA, Karimi S, Hou BL, Lymberis S, Yamada Y, Chang J, Abrey LE. Safety and efficacy of bevacizumab with hypofractionated stereotactic irradiation for recurrent malignant gliomas. Int J Radiat Oncol Biol Phys. 2009;75:156–63. doi: 10.1016/j.ijrobp.2008.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lai A, Tran A, Nghiemphu PL, et al. Phase II study of bevacizumab plus temozolomide during and after radiation therapy for patients with newly diagnosed glioblastoma multiforme. J Clin Oncol. 2011;29:142–148. doi: 10.1200/JCO.2010.30.2729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vredenburgh JJ, Desjardins A, Kirkpatrick JP, et al. Addition of bevacizumab to standard radiation therapy and daily temozolomide is associated with minimal toxicity in newly diagnosed glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2012;82:58–66. doi: 10.1016/j.ijrobp.2010.08.058. [DOI] [PubMed] [Google Scholar]
- 94.Vredenburgh JJ, Desjardins A, Reardon DA, et al. The addition of bevacizumab to standard radiation therapy and temozolomide followed by bevacizumab, temozolomide, and irinotecan for newly diagnosed glioblastoma. Clin Cancer Res. 2011;17:4119–24. doi: 10.1158/1078-0432.CCR-11-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wen PY, Macdonald DR, Reardon DA, et al. Updated response assessment criteria for high-grade gliomas: Response assessment in neuro-oncology working group. J Clin Oncol. 2010;28:1963–1972. doi: 10.1200/JCO.2009.26.3541. [DOI] [PubMed] [Google Scholar]
- 96.Chinot OL, Macdonald DR, Abrey LE, Zahlmann G, Kerloeguen Y, Cloughesy TF. Response assessment criteria for glioblastoma: practical adaptation and implementation in clinical trials of antiangiogenic therapy. Curr Neurol Neurosci Rep. 2013;13:347. doi: 10.1007/s11910-013-0347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hegi ME, Diserens A-C, Gorlia T, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352:997–1003. doi: 10.1056/NEJMoa043331. [DOI] [PubMed] [Google Scholar]
- 98.DeLay M, Jahangiri A, Carbonell WS, Hu Y-L, Tsao S, Tom MW, Paquette J, Tokuyasu TA, Aghi MK. Microarray analysis verifies two distinct phenotypes of glioblastomas resistant to antiangiogenic therapy. Clin Cancer Res. 2012;18:2930–42. doi: 10.1158/1078-0432.CCR-11-2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lu KV, Bergers G. Mechanisms of evasive resistance to anti-VEGF therapy in glioblastoma. CNS Oncol. 2013;2:49–65. doi: 10.2217/cns.12.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Casanovas O, Hicklin DJ, Bergers G, Hanahan D. Drug resistance by evasion of antiangiogenic targeting of VEGF signaling in late-stage pancreatic islet tumors. Cancer Cell. 2005;8:299–309. doi: 10.1016/j.ccr.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 101.Rigamonti N, Kadioglu E, Keklikoglou I, Rmili CW, Leow CC, de Palma M. Role of angiopoietin-2 in adaptive tumor resistance to VEGF signaling blockade. Cell Rep. 2014;8:696–706. doi: 10.1016/j.celrep.2014.06.059. [DOI] [PubMed] [Google Scholar]
- 102.Huang D, Ding Y, Zhou M, Rini BI, Petillo D, Qian C, Kahnoski R, Futreal PA, Furge KA, Teh BT. Interleukin-8 mediates resistance to antiangiogenic agent sunitinib in renal cell carcinoma. Cancer Res. 2010;70:1063–71. doi: 10.1158/0008-5472.CAN-09-3965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kloepper J, Riedemann L, Amoozgar Z, et al. Ang-2/VEGF bispecific antibody reprograms macrophages and resident microglia to anti-tumor phenotype and prolongs glioblastoma survival. Proc Natl Acad Sci USA. 2016;113:4476–4481. doi: 10.1073/pnas.1525360113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Peterson TE, Kirkpatrick ND, Huang Y, et al. Dual inhibition of Ang-2 and VEGF receptors normalizes tumor vasculature and prolongs survival in glioblastoma by altering macrophages. Proc Natl Acad Sci USA. 2016;113(16):440–5. doi: 10.1073/pnas.1525349113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Park J-S, Kim I-K, Han S, et al. Normalization of tumor vessels by Tie2 activation and Ang2 inhibition enhances drug delivery and produces a favorable tumor microenvironment. Cancer Cell. 2016;30:953–967. doi: 10.1016/j.ccell.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 106.Sitohy B, Nagy JA, Jaminet SCS, Dvorak HF. Tumor-surrogate blood vessel subtypes exhibit differential susceptibility to anti-VEGF therapy. Cancer Res. 2011;71:7021–7028. doi: 10.1158/0008-5472.CAN-11-1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Benjamin LE, Golijanin D, Itin A, Pode D, Keshet E. Selective ablation of immature blood vessels in established human tumors follows vascular endothelial growth factor withdrawal. J Clin Invest. 1999;103:159–165. doi: 10.1172/JCI5028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Piao Y, Liang J, Holmes L, Henry V, Sulman E, De Groot JF. Acquired resistance to anti-VEGF therapy in glioblastoma is associated with a mesenchymal transition. Clin Cancer Res. 2013;19:4392–4403. doi: 10.1158/1078-0432.CCR-12-1557. [DOI] [PubMed] [Google Scholar]
- 109.Lu KV, Chang JP, Parachoniak CA, et al. VEGF inhibits tumor cell invasion and mesenchymal transition through a MET/VEGFR2 complex. Cancer Cell. 2012;22:21–35. doi: 10.1016/j.ccr.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jahangiri A, De Lay M, Miller LM, et al. Gene expression profile identifies tyrosine kinase c-Met as a targetable mediator of antiangiogenic therapy resistance. Clin Cancer Res. 2013;19:1773–83. doi: 10.1158/1078-0432.CCR-12-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lucio-Eterovic AK, Piao Y, De Groot JF. Mediators of glioblastoma resistance and invasion during antivascular endothelial growth factor therapy. Clin Cancer Res. 2009;15:4589–4599. doi: 10.1158/1078-0432.CCR-09-0575. [DOI] [PubMed] [Google Scholar]
- 112.Huang Y, Goel S, Duda DG, Fukumura D, Jain RK. Vascular normalization as an emerging strategy to enhance cancer immunotherapy. Cancer Res. 2013;73:2943–2948. doi: 10.1158/0008-5472.CAN-12-4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.De Groot JF, Piao Y, Tran H, et al. Myeloid biomarkers associated with glioblastoma response to anti-VEGF therapy with aflibercept. Clin Cancer Res. 2011;17:4872–4881. doi: 10.1158/1078-0432.CCR-11-0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shojaei F, Wu X, Qu X, Kowanetz M, Yu L, Tan M, Meng YG, Ferrara N. G-CSF-initiated myeloid cell mobilization and angiogenesis mediate tumor refractoriness to anti-VEGF therapy in mouse models. Proc Natl Acad Sci USA. 2009;106:6742–6747. doi: 10.1073/pnas.0902280106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chung AS, Wu X, Zhuang G, et al. An interleukin-17-mediated paracrine network promotes tumor resistance to anti-angiogenic therapy. Nat Med. 2013;19:1114–1123. doi: 10.1038/nm.3291. [DOI] [PubMed] [Google Scholar]
- 116.Tripathi C, Tewari BN, Kanchan RK, Baghel KS, Nautiyal N, Shrivastava R, Kaur H, Bhatt MLB, Bhadauria S. Macrophages are recruited to hypoxic tumor areas and acquire a pro-angiogenic M2-polarized phenotype via hypoxic cancer cell derived cytokines Oncostatin M and Eotaxin. Oncotarget. 2014;5:5350–68. doi: 10.18632/oncotarget.2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Scholz A, Harter PN, Cremer S, et al. Endothelial cell-derived angiopoietin- 2 is a therapeutic target in treatment-naive and bevacizumab-resistant glioblastoma. EMBO Mol Med. 2015;8(1):39–57. doi: 10.15252/emmm.201505505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Buchroithner J, Pichler J, Marosi C, et al. Vascular endothelia growth factor targeted therapy may improve the effect of dendritic cell-based cancer immune therapy. Int J Clin Pharmacol Ther. 2014;52:76–7. doi: 10.5414/CPXCES13EA02. [DOI] [PubMed] [Google Scholar]
- 119.Reardon DA, Schuster J, Tran DD, et al (2015) ReACT: Long-term survival from a randomized phase II study of rindopepimut (CDX-110) plus bevacizumab in relapsed glioblastoma. J Clin Oncol 33:abstr 2009
- 120.Shrimali RK, Yu Z, Theoret MR, Chinnasamy D, Restifo NP, Rosenberg SA. Antiangiogenic agents can increase lymphocyte infiltration into tumor and enhance the effectiveness of adoptive immunotherapy of cancer. Cancer Res. 2010;70:6171–80. doi: 10.1158/0008-5472.CAN-10-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sulman EP, Won M, Blumenthal DT, et al. Molecular predictors of outcome and response to bevacizumab (BEV) based on analysis of RTOG 0825, a phase III trial comparing chemoradiation (CRT) with and without BEV in patients with newly diagnosed glioblastoma (GBM) J Clin Oncol. 2013;31:LBA2010. [Google Scholar]
- 122.Sathornsumetee S, Cao Y, Marcello JE, Herndon JE, McLendon RE, Desjardins A, Friedman HS, Dewhirst MW, Vredenburgh JJ, Rich JN. Tumor angiogenic and hypoxic profiles predict radiographic response and survival in malignant astrocytoma patients treated with bevacizumab and irinotecan. J Clin Oncol. 2008;26:271–8. doi: 10.1200/JCO.2007.13.3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lu-Emerson C, Snuderl M, Kirkpatrick ND, et al. Increase in tumor-associated macrophages after antiangiogenic therapy is associated with poor survival among patients with recurrent glioblastoma. Neuro Oncol. 2013;15:1079–1087. doi: 10.1093/neuonc/not082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen C, Huang R, MacLean A, Muzikansky A, Mukundan S, Wen PY, Norden AD. Recurrent high-grade glioma treated with bevacizumab: Prognostic value of MGMT methylation, EGFR status and pretreatment MRI in determining response and survival. J Neurooncol. 2013;115:267–276. doi: 10.1007/s11060-013-1225-0. [DOI] [PubMed] [Google Scholar]
- 125.Lv S, Teugels E, Sadones J, et al. Correlation between IDH1 gene mutation status and survival of patients treated for recurrent glioma. Anticancer Res. 2011;31:4457–4463. [PubMed] [Google Scholar]
- 126.Batchelor TT, Gerstner ER, Emblem KE, et al. Improved tumor oxygenation and survival in glioblastoma patients who show increased blood perfusion after cediranib and chemoradiation. Proc Natl Acad Sci USA. 2013;110:19059–64. doi: 10.1073/pnas.1318022110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Duda DG, Willett CG, Ancukiewicz M, et al. Plasma soluble VEGFR-1 is a potential dual biomarker of response and toxicity for bevacizumab with chemoradiation in locally advanced rectal cancer. Oncologist. 2010;15:577–583. doi: 10.1634/theoncologist.2010-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Duda DG, Kozin SV, Kirkpatrick ND, Xu L, Fukumura D, Jain RK. CXCL12 (SDF1α)-CXCR4/CXCR7 pathway inhibition: An emerging sensitizer for anticancer therapies? Clin Cancer Res. 2011;17:2074–2080. doi: 10.1158/1078-0432.CCR-10-2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tabouret E, Boudouresque F, Barrie M, et al. Association of matrix metalloproteinase 2 plasma level with response and survival in patients treated with bevacizumab for recurrent high-grade glioma. Neuro Oncol. 2014;16:392–399. doi: 10.1093/neuonc/not226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.De Groot JF, Lamborn KR, Chang SM, et al. Phase II study of aflibercept in recurrent malignant glioma: A North American brain tumor consortium study. J Clin Oncol. 2011;29:2689–2695. doi: 10.1200/JCO.2010.34.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sorensen AG, Batchelor TT, Zhang W-T, et al. A “vascular normalization index” as potential mechanistic biomarker to predict survival after a single dose of cediranib in recurrent glioblastoma patients. Cancer Res. 2009;69:5296–5300. doi: 10.1158/0008-5472.CAN-09-0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Pope WB, Kim HJ, Huo J, et al. Recurrent glioblastoma multiforme: ADC histogram analysis predicts response to bevacizumab treatment. Radiology. 2009;252:182–189. doi: 10.1148/radiol.2521081534. [DOI] [PubMed] [Google Scholar]
- 133.Kothari PD, White NS, Farid N, Chung R, Kuperman JM, Girard HM, Shankaranarayanan A, Kesari S, McDonald CR, Dale AM. Longitudinal restriction spectrum imaging is resistant to pseudoresponse in patients with high-grade gliomas treated with bevacizumab. AJNR Am J Neuroradiol. 2013;34:1752–7. doi: 10.3174/ajnr.A3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Piludu F, Marzi S, Pace A, Villani V, Fabi A, Carapella CM, Terrenato I, Antenucci A, Vidiri A. Early biomarkers from dynamic contrast-enhanced magnetic resonance imaging to predict the response to antiangiogenic therapy in high-grade gliomas. Neuroradiology. 2015;57:1269–1280. doi: 10.1007/s00234-015-1582-9. [DOI] [PubMed] [Google Scholar]
- 135.O’Connor JPB, Jackson A, Parker GJM, Roberts C, Jayson GC. Dynamic contrast-enhanced MRI in clinical trials of antivascular therapies. Nat Rev Clin Oncol. 2012;9:167–177. doi: 10.1038/nrclinonc.2012.2. [DOI] [PubMed] [Google Scholar]
- 136.Emblem KE, Mouridsen K, Bjornerud A, et al. Vessel architectural imaging identifies cancer patient responders to anti-angiogenic therapy. Nat Med. 2013;19:1178–83. doi: 10.1038/nm.3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chen W, Delaloye S, Silverman DHS, et al. Predicting treatment response of malignant gliomas to bevacizumab and irinotecan by imaging proliferation with [18F] fluorothymidine positron emission tomography: A pilot study. J Clin Oncol. 2007;25:4714–4721. doi: 10.1200/JCO.2006.10.5825. [DOI] [PubMed] [Google Scholar]
- 138.Harris RJ, Cloughesy TF, Pope WB, Nghiemphu PL, Lai A, Zaw T, Czernin J, Phelps ME, Chen W, Ellingson BM. 18F-FDOPA and 18F-FLT positron emission tomography parametric response maps predict response in recurrent malignant gliomas treated with bevacizumab. Neuro Oncol. 2012;14:1079–1089. doi: 10.1093/neuonc/nos141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sorensen AG, Emblem KE, Polaskova P, et al. Increased survival of glioblastoma patients who respond to antiangiogenic therapy with elevated blood perfusion. Cancer Res. 2012;72:402–407. doi: 10.1158/0008-5472.CAN-11-2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lorgis V, Maura G, Coppa G, Hassani K, Taillandier L, Chauffert B, Apetoh L, Ladoire S, Ghiringhelli F. Relation between bevacizumab dose intensity and high-grade glioma survival: A retrospective study in two large cohorts. J Neurooncol. 2012;107:351–358. doi: 10.1007/s11060-011-0748-5. [DOI] [PubMed] [Google Scholar]
- 141.Levin VA, Mendelssohn ND, Chan J, Stovall MC, Peak SJ, Yee JL, Hui RL, Chen DM. Impact of bevacizumab administered dose on overall survival of patients with progressive glioblastoma. J Neurooncol. 2015;122:145–150. doi: 10.1007/s11060-014-1693-x. [DOI] [PubMed] [Google Scholar]
- 142.Weathers S-P, Han X, Liu DD, et al (2016) A randomized phase II trial of standard dose bevacizumab versus low dose bevacizumab plus lomustine (CCNU) in adults with recurrent glioblastoma. J Neurooncol 129:487–494 [DOI] [PMC free article] [PubMed]
- 143.Reardon DA, Herndon JE, Peters KB, et al. Bevacizumab continuation beyond initial bevacizumab progression among recurrent glioblastoma patients. Br J Cancer. 2012;107:1481–7. doi: 10.1038/bjc.2012.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tang TC, Man S, Xu P, Francia G, Hashimoto K, Emmenegger U, Kerbel RS. Development of a resistance-like phenotype to sorafenib by human hepatocellular carcinoma cells is reversible and can be delayed by metronomic UFT chemotherapy. Neoplasia. 2010;12:928–940. doi: 10.1593/neo.10804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bennouna J, Sastre J, Arnold D, et al. Continuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147): A randomised phase 3 trial. Lancet Oncol. 2013;14:29–37. doi: 10.1016/S1470-2045(12)70477-1. [DOI] [PubMed] [Google Scholar]
- 146.von Minckwitz G, Puglisi F, Cortes J, et al. Bevacizumab plus chemotherapy versus chemotherapy alone as second-line treatment for patients with HER2-negative locally recurrent or metastatic breast cancer after first-line treatment with bevacizumab plus chemotherapy (TANIA): an open-label, randomised. Lancet Oncol. 2014;15:1269–78. doi: 10.1016/S1470-2045(14)70439-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 932 kb)