Abstract
Impaired rate-dependent depression (RDD) of the Hoffman reflex is associated with reduced dorsal spinal cord potassium chloride cotransporter expression and impaired spinal γ-aminobutyric acid type A receptor function, indicative of spinal inhibitory dysfunction. We have investigated the pathogenesis of impaired RDD in diabetic rodents exhibiting features of painful neuropathy and the translational potential of this marker of spinal inhibitory dysfunction in human painful diabetic neuropathy. Impaired RDD and allodynia were present in type 1 and type 2 diabetic rats but not in rats with type 1 diabetes receiving insulin supplementation that did not restore normoglycemia. Impaired RDD in diabetic rats was rapidly normalized by spinal delivery of duloxetine acting via 5-hydroxytryptamine type 2A receptors and temporally coincident with the alleviation of allodynia. Deficits in RDD and corneal nerve density were demonstrated in patients with painful diabetic neuropathy compared with healthy control subjects and patients with painless diabetic neuropathy. Spinal inhibitory dysfunction and peripheral small fiber pathology may contribute to the clinical phenotype in painful diabetic neuropathy. Deficits in RDD may help identify patients with spinally mediated painful diabetic neuropathy who may respond optimally to therapies such as duloxetine.
Introduction
Approximately 30% of patients with diabetes develop painful neuropathy (1). The efficacy of current therapies is highly variable (2,3), potentially reflecting diverse pain generator sites (4,5) and etiological mechanisms (6) in patients with diabetes with neuropathic pain. Phenotyping patients based on their symptom complex and putative mechanisms may enable more accurate prediction of treatment response (7). Although standard neurophysiology and quantitative sensory testing can differentiate patients with diabetes with and without neuropathy (8), recent Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) recommendations have emphasized a need for more detailed phenotyping of patients with painful neuropathy in order to improve both clinical care and success rates for putative analgesic drugs in clinical trials (9).
Rate-dependent depression (RDD), a measure of change in amplitude of the Hoffman (H) reflex over consecutive stimulations, can be recorded from electromyograms during standard electrophysiological procedures. RDD is impaired after disinhibition of spinal sensory processing caused by spinal cord injury in both awake humans (10,11) and anesthetized animals (12,13). In rats, RDD is driven by γ-aminobutyric acid (GABA) acting though GABA type A (GABAA) receptors and is attenuated when GABAA receptor–mediated inhibitory function is disrupted (14). We recently demonstrated that loss of RDD separated rats demonstrating impaired spinal GABAergic inhibitory function from rats with normal spinal GABAergic function, despite both showing a similar neuropathic pain phenotype (15). Measuring RDD may therefore allow assessment of the relative contribution of spinal inhibitory dysfunction and segregation of peripherally from spinally generated pain. While it is becoming apparent that only a minor fraction of patients with diabetes who experience pain exhibit the “irritable nociceptor” phenotype (5), it is not known whether RDD, and by implication spinal inhibitory systems, are impaired in any or all patients with painful diabetic neuropathy.
We investigated the pathogenic basis of RDD attenuation in diabetic rats and determined that modulation of RDD predicts the therapeutic efficacy of duloxetine, which alleviates neuropathic pain by enhancing spinal inhibitory systems (16,17). We also translated our experimental findings by assessing whether RDD and small-fiber pathology could segregate patients with painful compared with painless diabetic neuropathy.
Research Design and Methods
Animals and Induction of Diabetes
Studies were performed using adult female Sprague-Dawley or adult male Zucker Diabetic Fatty (ZDF) rats. Rats were housed two to three per cage with free access to food (Harlan 5001 diet) and water and maintained in an American Association for the Accreditation of Laboratory Animal Care–approved vivarium. Studies were performed according to protocols approved by the Institutional Animal Care and Use Committee of the University of California, San Diego. Insulin-deficient diabetes was induced after an overnight fast by injection of 50 mg/kg i.p. streptozotocin (STZ) (Sigma-Aldrich, St. Louis, MO), freshly dissolved in 0.9% sterile saline. Hyperglycemia was confirmed using a glucose meter (OneTouch Ultra; LifeScan, Milpitas, CA) from blood obtained by tail prick 4 days after STZ injection, and blood and cerebrospinal fluid were collected at study conclusion.
Neuropathy
Peripheral nerve function was assessed by measuring sciatic motor and sensory nerve conduction velocity and paw thermal and tactile response thresholds as previously described in detail (18).
RDD of the H-Reflex
Under isoflurane anesthesia, one hind limb was secured and a transcutaneous needle electrode inserted at the ankle for tibial nerve stimulation. Two recording electrodes were inserted into hind paw interosseous muscles. Stimulus generation and recording of M and H waves from the resulting electromyogram were performed using a Powerlab 4/30 connected to a computer running Scope software (AD Instruments, Colorado Springs, CO). Tibial nerve stimulation used bursts of 5 × 200 μs duration square waves with 40-μs interpulse intervals. Each burst was repeated at 1 Hz stimulation frequency, which, in normal rats, causes an ∼40% decrease in H-wave amplitude between the first and subsequent bursts (15). Stimulation intensity was increased by 0.125-V increments until the stimulus that produced the maximum H-wave amplitude (Hmax) was found. RDD was calculated as percentage change in H-wave amplitude evoked by the second (H2) compared with the first (H1) stimulation burst. In rats, H2 is representative of all subsequent responses (14).
Pharmacological Interventions
3-O-methyl-glucose (3-OMG) (Sigma-Aldrich) was injected at 5 mmol/kg i.p. 1–2 min before STZ administration. Dose and timing were chosen to prevent hyperglycemia despite systemic presence of STZ (19). Continuous insulin treatment to prevent prolonged hyperglycemia was initiated in STZ-injected rats immediately after onset of hyperglycemia by subdermal implantation of insulin pellets that release 2 IU/24 h (Linshin Canada Inc.). Blood glucose levels were assessed weekly and additional pellets supplemented as necessary. The effects of short-term insulin treatment were assessed by implanting one subcutaneous insulin pellet or providing twice-daily subcutaneous insulin injections (4 IU, Humulin; Eli Lilly, Indianapolis, IN) to diabetic rats that were otherwise untreated for the previous 8 weeks. Blood glucose was assessed daily in the insulin pellet group and at 30-min intervals after acute insulin injection.
The 5-hydroxytryptamine type 2A/C (5-HT2A/C) receptor agonist 1-(2,5-dimethoxy-4-iodophenyl)-2-aminopropane hydrochloride (DOI) (20 µg; Sigma-Aldrich) was dissolved in water. Cymbalta (Eli Lilly, Indianapolis, IN) was used as a source of duloxetine hydrochloride (20 µg) and dissolved in saline. The 5-HT2A/1D receptor antagonist ketanserin (20 µg; Sigma-Aldrich) and selective 5-HT2A receptor antagonist pruvanserin (EMD 281014, provided by G. Bartoszyk, Merck KGaA, Darmstadt, Germany) were dissolved in saline. Drug formulations and doses were selected from previous studies (17).
Western Blotting
Spinal cords were obtained by hydraulic extrusion after decapitation of anesthetized rats. The lumbar enlargement was dissected on ice into dorsal and ventral portions that were collected into ice-cold homogenization buffer (50 mmol/L Tris-HCl, pH 7.4; 150 mmol/L NaCl; 1 mmol/L EDTA; 0.5% Triton X; and protease inhibitor cocktail) and homogenized before centrifugation (14,000g). Protein (7–15 µg) was prepared by incubation for 30 min in Laemmli sample buffer at 37°C before separation on 4–12% SDS-PAGE Bis-Tris gels (Novex; Invitrogen, Carlsbad, CA) and immunoblotted on nitrocellulose. Membranes were incubated with KCC2 (1:2,000; Millipore) and actin (1:2,000; Sigma-Aldrich) antibodies. Quantification of immunoreactivity was performed by densitometric analysis. For each animal, band intensities were normalized by calculating the ratio of intensity of the band of interest to the intensity of the actin (loading control) band. Normalized data were expressed as a percentage of group mean of values obtained for nondiabetic rats run on the same gel.
Human Studies
Studies were approved by National Research Ethics Service Committee North West–Greater Manchester (09/H1006/38). All participants provided written informed consent. Study conduct adhered to the tenets of the declaration of Helsinki.
Twenty-seven patients with type 1 diabetes and 15 age-matched control subjects were recruited. Participants underwent the following assessments: Neuropathy Disability Score (NDS), Neuropathy Symptom Profile (NSP), vibration perception threshold (VPT), and thermal perception thresholds; sural sensory amplitude (SSamp) and conduction velocity (SSCV); and peroneal motor amplitude (PMamp) and conduction velocity (PMCV). For intraepidermal nerve fiber density (IENFD) assessment, 3-mm punch skin biopsy specimens were obtained from the dorsum of the foot and a bright-field immunohistochemistry protocol was used according to published guidelines (20). Linear IENFD (number of fibers/mm) was established in at least four sections of 50-μm thickness according to published counting rules (21). Corneal nerve fiber density (CNFD), nerve branch density (CNBD), and nerve fiber length (CNFL) were quantified according to established techniques (22).
A modified Toronto Diabetic Neuropathy Expert Group (8) recommendation was followed to define neuropathy, incorporating small-fiber neuropathy measures (2 SDs outside normal range for CNFD or IENFD) if PMCV was normal. Patients were stratified into painful (visual analog score [VAS] >3 of 10) (n = 13) and painless (VAS ≤3 of 10) (n = 14) groups.
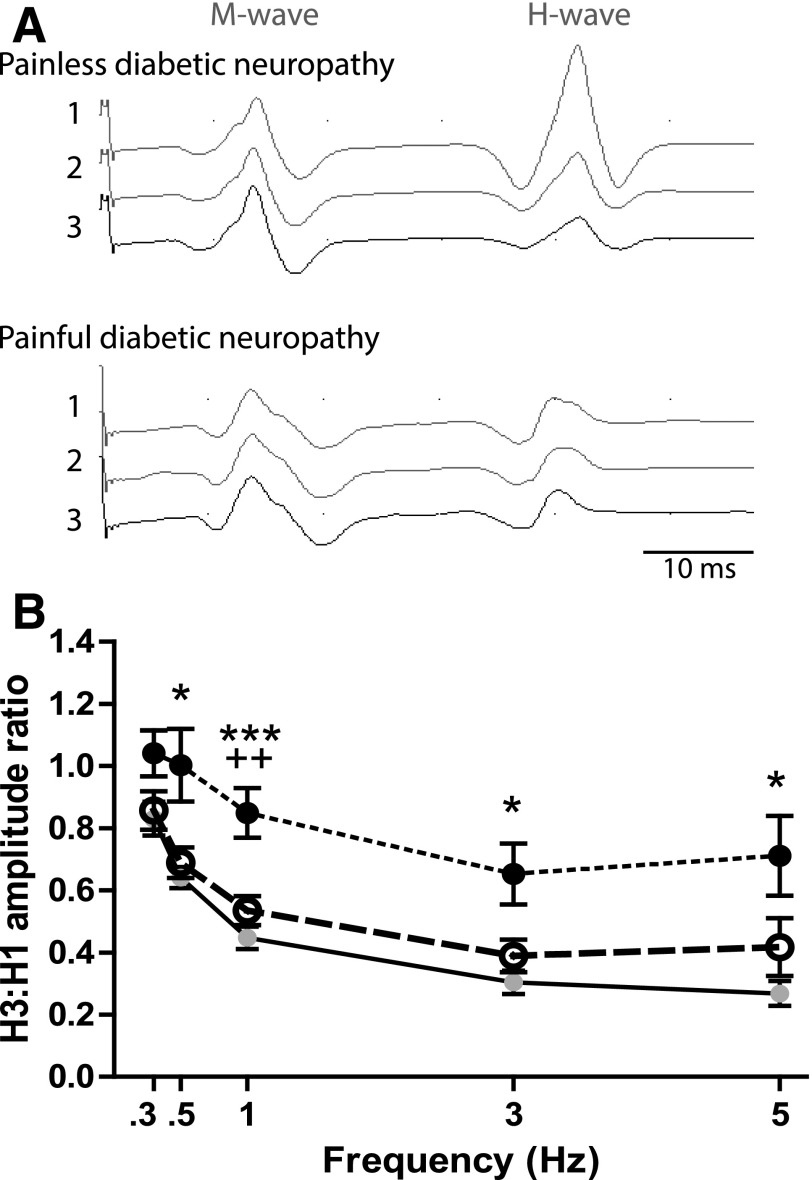
For H-reflex studies, a standardized protocol was adopted in which participants sat comfortably in a quiet room semirecumbent at 45° and facing forward with eyes open. Monophasic 1-ms duration square wave pulses were delivered using surface silver-silver chloride electrodes to the tibial nerve in the popliteal fossa (11). Surface 9-mm diameter silver-silver chloride recording electrodes were placed on the long axis of the soleus. Peak-peak Hmax was determined by incrementing stimulation current by 1 mA at 0.3 Hz. Only patients with an Hmax of >400 µV were included, with five patients excluded because of absent or low voltage waveforms—four without and one with a pain VAS >3. For RDD, trains of three stimuli were delivered at 0.3, 0.5, 1, 3, and 5 Hz. Stimulation order was randomized with a minimum of 10 s allowed between each run. Submaximal stimulation producing an H-reflex 50–75% of Hmax was used. Consecutive H-reflex recordings within trains were termed H1–H3, respectively. RDD, defined as H3-to-H1 amplitude ratio, was calculated for each stimulation frequency (11), as H2 did not identify the maximal change from H1 (A.G.M., unpublished observations).
Statistics
Statistical analyses were performed with Prism statistical software (GraphPad Software, Inc., La Jolla, CA). Parametric data were analyzed using unpaired two-tailed t test, one-way ANOVA followed by Tukey or Dunnett post hoc test for multiple comparisons, or two-way ANOVA followed by Bonferroni post hoc test as indicated. Nonparametric data were analyzed using the Kruskal-Wallis test followed by Dunn post hoc test for multiple comparisons as indicated. Pairwise comparisons were made using the Mann-Whitney U test (post hoc Bonferroni-corrected P < 0.05). Correlations were performed using Spearman rank test and expressed as a coefficient (r) with significance level.
Results
3-OMG or Insulin Treatment Prevents Impaired RDD and Indices of Painful Neuropathy After STZ Administration
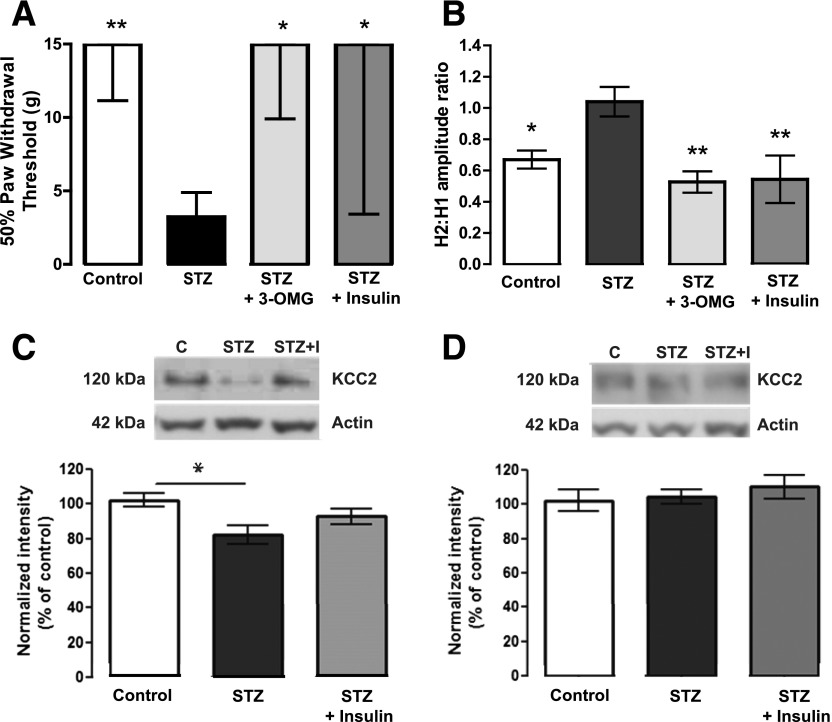
STZ-injected rats showed weight loss, hyperglycemia, increased HbA1c, and elevated cerebrospinal fluid glucose at the end of the study (Table 1). Continuous insulin therapy and 3-OMG pretreatment, to impede pancreatic β-cell STZ uptake and subsequent apoptosis (23), both prevented all systemic physiological consequences of STZ injection. STZ diabetic rats showed expected indices of loss-of-function neuropathy such as slowing of nerve conduction velocity and thermal hypoalgesia (Table 1) while concurrently exhibiting tactile allodynia and impaired RDD (Fig. 1A–B). Pretreatment with 3-OMG or prolonged insulin treatment prevented all manifestations of neuropathy. STZ diabetes also caused a selective reduction of spinal KCC2 protein expression in the dorsal (P < 0.05 vs. control) (Fig. 1C), but not ventral (Fig. 1D), horn that was prevented by insulin supplementation.
Table 1.
Indices of diabetes and neuropathy at death in rat models of type 1 (STZ) and type 2 (ZDF) diabetes
| N | Body weight (g) | Blood glucose (mmol/L) | Blood HbA1c (%) | CSF glucose (mmol/L) | Sciatic MNCV (m/s) | Sciatic SNCV (m/s) | Thermal latency (s) | Tactile threshold (g) | |
|---|---|---|---|---|---|---|---|---|---|
| Control | 9 | 279 ± 3*** | 5.4 ± 0.1*** | 4.3 ± 0.1*** | 2.7 ± 0.2*** | 54.6 ± 1.2*** | 58.3 ± 1.6*** | 8.3 ± 0.4* | 15.0*** |
| STZ | 10 | 201 ± 4 | 27.4 ± 2.1 | 7.6 ± 0.2 | 17.1 ± 1.5 | 45.6 ± 0.9 | 47.9 ± 1.8 | 10.8 ± 0.8 | 3.1 |
| STZ + 3-OMG | 7 | 274 ± 3*** | 6.3 ± 0.3*** | 4.3 ± 0.1*** | nd | 54.3 ± 0.8*** | 55.2 ± 1.5* | 7.6 ± 0.4*** | 15.0*** |
| STZ + insulin | 6 | 259 ± 7*** | 11.9 ± 4.9** | 4.2 ± 0.3*** | 4.9 ± 1.4*** | 48.2 ± 1.0 | 55.7 ± 2.5* | 8.1 ± 0.8* | 15.0*** |
| Lean | 12 | 429 ± 4* | 9.0 ± 0.3*** | nd | nd | 56.2 ± 0.9* | 57.4 ± 2.3* | 7.1 ± 0.5** | 10.8** |
| ZDF | 9 | 380 ± 19 | 29.0 ± 1.1 | nd | nd | 53.7 ± 0.5 | 50.7 ± 1.9 | 9.9 ± 1.0 | 3.4 |
Parametric data are group mean ± SEM with statistical analysis by unpaired t test or one-way ANOVA with Dunnett post hoc test. Nonparametric data are group median with Mann-Whitney U test or Kruskal-Wallis with Dunn post hoc test. CSF, cerebrospinal fluid; MNCV, motor nerve conduction velocity; nd, not determined; SNCV, sensory nerve conduction velocity.
*P < 0.05,
**P < 0.01, and
***P < 0.001 vs. STZ or ZDF as appropriate.
Figure 1.
Fifty percent paw withdrawal threshold (A) and RDD measured as H2-to-H1 amplitude ratio (B) in controls, STZ diabetic (STZ) rats, STZ + 3-OMG rats, and STZ diabetic rats treated with insulin (STZ + Insulin) after 8 weeks of diabetes. For A, data are presented as group median ± interquartile range. **P < 0.01, *P < 0.05 compared with STZ by the Kruskal-Wallis test followed by the Dunn multiple comparisons test. For B, data are presented as group mean ± SEM. **P < 0.01, *P < 0.05 compared with STZ by one-way ANOVA followed by the Tukey post hoc test. C and D: Upper panel shows Western blots of KCC2 and actin protein in lumbar dorsal (C) or ventral (D) spinal cord of control (C), STZ diabetic (STZ), and insulin-treated STZ diabetic (STZ+I) rats. Lower panel shows KCC2 intensity normalized to actin loading control. Data are presented as mean ± SEM, with N = 5 animals/group, and pooled from three independently run Western blots. *P < 0.05 by one-way ANOVA followed by the Tukey post hoc test.
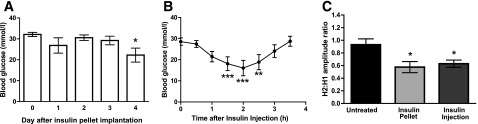
Short-term Insulin Treatment Reverses Impaired RDD in Diabetic Rats
STZ diabetic rats that were untreated for 8 weeks subsequently received either a subcutaneous insulin pellet releasing 2 IU insulin/day or 4 IU insulin injected at 12-h intervals. Diabetic rats that received an insulin pellet did not show a significant reduction in blood glucose levels until the 4th day after implantation (Fig. 2A), and values remained higher than in controls (Table 1). In contrast, insulin acutely reduced blood glucose within 2 h, although animals remained hyperglycemic (Fig. 2B). The effect of insulin resolved within 3.5 h so that rats receiving insulin injections were exposed to two short periods of diminished hyperglycemia per day. RDD, measured on day 4 after initiation of both treatment regimes, and 12 h after the last insulin injection, was significantly improved in both insulin treatment groups (P < 0.05) (Fig. 2C) compared with untreated diabetic rats and was equivalent to that of control animals (Fig. 1B). Loss of RDD can be reversed by short-term insulin replacement, which dissociates correction of RDD deficits from immediate restoration of normoglycemia.
Figure 2.
Blood glucose values after implantation of an insulin pellet (A) or after a single subcutaneous injection of 4 IU insulin (B) in otherwise untreated STZ diabetic rats. Data are group mean ± SEM of N = 6/group. *P < 0.05, **P < 0.01, ***P < 0.001 compared with time 0 by repeated-measures ANOVA followed by the Dunnett post hoc test. C: RDD measured in these two groups of diabetic rats and in untreated diabetic rats (untreated) 4 days after initiation of insulin therapy and 12 h after the last insulin injection. Data are group mean ± SEM of N = 6/group. *P < 0.05 vs. untreated diabetic rats by one-way ANOVA followed by the Dunnett post hoc test.
RDD Is Impaired in Experimental Type 2 Diabetes
ZDF rats, a model of type 2 diabetes, developed hyperglycemia (20.2 ± 2.2 mmol/L) by 8 weeks of age that persisted until the end of the study and was accompanied by indices of neuropathy that matched those of STZ diabetic rats (Table 1). RDD was not significantly different from lean control rats at 8 weeks of age but was significantly impaired at 20 and 32 weeks (P < 0.05), paralleling onset of tactile allodynia (Supplementary Fig. 1).
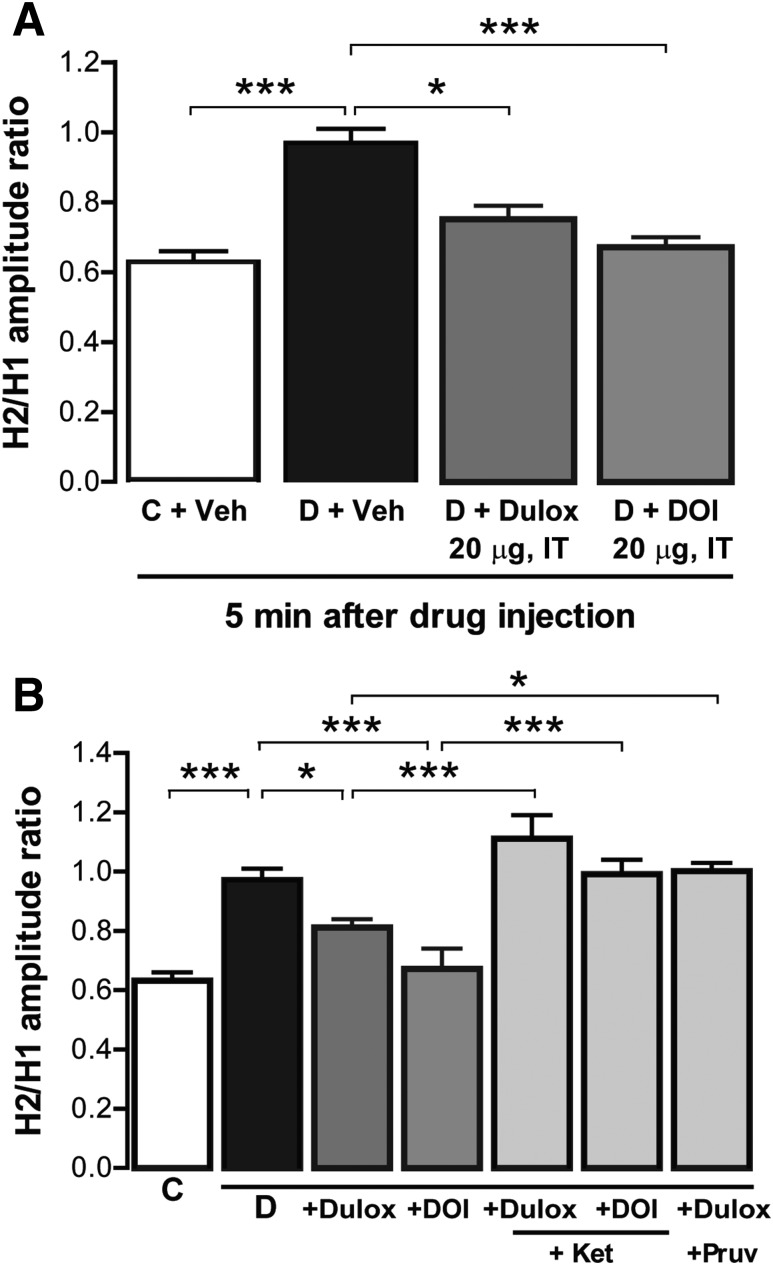
Duloxetine and DOI Restore RDD in Diabetic Rats in a 5-HT2A Receptor–Dependent Fashion
Tactile allodynia in STZ diabetic rats is reversed by the serotonin-norepinephrin reuptake inhibitor duloxetine and the 5-HT2A/C receptor agonist DOI in a 5-HT2A receptor–dependent fashion (17). We investigated whether the antiallodynic effects of these agents could be predicted by their effects on RDD deficits. STZ diabetic rats had significantly impaired RDD compared with controls (P < 0.001) (Fig. 3A). Intrathecal administration of either duloxetine (20 μg) or DOI (20 μg) significantly (P < 0.05) restored RDD within 5 min of administration with similar relative efficacy and in agreement with the previously reported magnitude of effect on tactile allodynia (17).
Figure 3.
RDD in control (C) and STZ diabetic (D) rats measured 5 min after IT delivery of vehicle (Veh), 20 µg duloxetine (Dulox), or 20 µg DOI (A) or the above followed 5 min later by either ketanserin (Ket) or pruvanserin (Pruv) also at 20 μg (B). Data are group mean + SEM of N = 6–8/group. *P < 0.05, ***P < 0.001 vs. indicated group by one-way ANOVA followed by the Tukey post hoc test.
The 5-HT2A/D receptor antagonist ketanserin (20 μg intrathecal [IT]) or 5-HT2A receptor antagonist pruvanserin (20 μg IT), administered 5 min after duloxetine or DOI, reversed the restoration of RDD within 10 min, whereas this persisted in vehicle-treated animals (Fig. 3B), confirming that 5-HT2A receptor activation mediated the restoration of RDD.
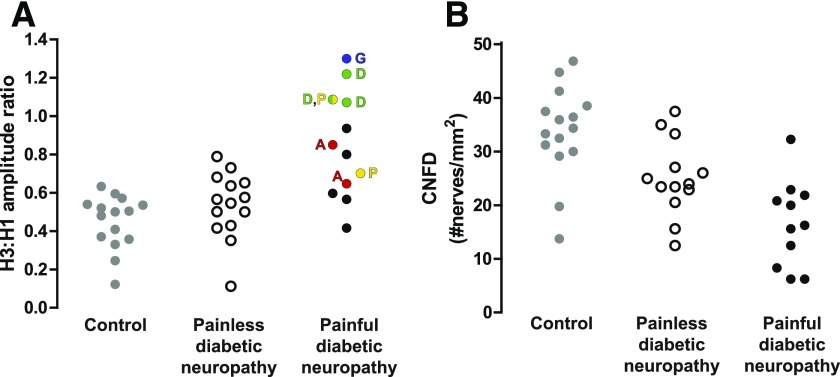
Patients With Painful Diabetic Neuropathy Have Impaired RDD
To explore the translational potential of these findings, we investigated RDD in subjects with type 1 diabetes and painful or painless diabetic neuropathy and healthy control subjects. Clinical characteristics are summarized in Table 2. Diabetes duration and HbA1c were comparable between patients with painful and painless neuropathy. Of the 13 patients with painful diabetic neuropathy, two took duloxetine, one pregabalin, one gabapentin, one amitriptyline, and one duloxetine and pregabalin in combination (Fig. 5A). Both the NSP (P < 0.0001) and NDS (P < 0.01) were significantly higher in patients with diabetes, irrespective of pain status, compared with control subjects. NSP was significantly higher in patients with diabetes with painful compared with painless neuropathy. Patients with diabetes with painful and painless diabetic neuropathy had a reduction in PMCV (P < 0.0001), SSCV (P < 0.0001), PMamp (P < 0.0001), and SSamp (P < 0.01) and increased VPT (P < 0.001) and cold (P < 0.01) and warm (P < 0.01) perception thresholds compared with control subjects. Structural measures of small-fiber neuropathy including IENFD (P < 0.01), CNFD (P < 0.0001), CNBD (P < 0.001), and CNFL (P < 0.001) were significantly reduced in both groups of patients with diabetes. CNFD was significantly lower in patients with painful compared with painless diabetic neuropathy (P < 0.05), but there was no significant difference for other small- or large-fiber parameters.
Table 2.
Demographic, clinical, and neuropathy variables in control subjects and patients with and without painful diabetic neuropathy
| Control subjects (n = 15) | Painful diabetic neuropathy (n = 13) | Painless diabetic neuropathy (n = 14) | |
|---|---|---|---|
| Age (years) | 48 ± 16 | 57 ± 12 | 52 ± 17 |
| Duration of diabetes (years) | N/A | 32 ± 16 | 26 ± 19 |
| HbA1c (%) | 5.5 ± 0.4 | 7.9 ± 0.9*** | 9.1 ± 1.9*** |
| NDS (0–10) | 0.1 ± 0.2 | 3.3 ± 1.5** | 3.1 ± 1.4** |
| NSP (0–38) | 0.1 ± 0.2 | 6.6 ± 3.5***++ | 2.4 ± 2.1* |
| VPT (V) | 5.7 ± 5.7 | 18.3 ± 13*** | 16.8 ± 11.4*** |
| Cold perception threshold (°C) | 28.8 ± 2.0 | 23.4 ± 5.3** | 26.1 ± 3.5** |
| Warm perception threshold (°C) | 37.2 ± 2.5 | 42.3 ± 4.0** | 40.6 ± 4.0* |
| SSamp (µV) | 18.7 ± 9.6 | 6.6 ± 4.6** | 10.8 ± 7.7** |
| SSCV (m/s) | 51.7 ± 3.1 | 40.6 ± 7.9*** | 42.2 ± 6.2*** |
| PMamp (mV) | 5.9 ± 2.0 | 1.9 ± 1.2*** | 2.8 ± 2.3** |
| PMCV (m/s) | 49.9 ± 4.4 | 37.8 ± 6.9*** | 38.9 ± 8.4*** |
| H-reflex latency (ms) | 32.4 ± 3.9 | 37.1 ± 3.7** | 36.1 ± 3.3* |
| H-reflex amplitude (µV) | 2,024.7 ± 596.0 | 959.2 ± 927.3 | 1,071.4 ± 957.9 |
| IENFD (no./mm) | 10.6 ± 4.0 | 4.2 ± 1.5* | 4.9 ± 3.1** |
| CNFD (no./mm2) | 33.7 ± 8.6 | 16.6 ± 8.0***+ | 24.7 ± 7.4* |
| CNFL (mm/mm2) | 25.6 ± 6.3 | 13.6 ± 6.2*** | 18.1 ± 5.5** |
| CNBD (no./mm2) | 91.3 ± 41.4 | 35.6 ± 1.4*** | 47.4 ± 26.7** |
Results are expressed as mean ± SD. N/A, not applicable. Statistically significant differences identified with the Kruskal-Wallis test followed by Dunn post hoc test for multiple comparisons:
*P < 0.05,
**P < 0.01, and
***P < 0.001 for control subjects against diabetic neuropathy groups;
+P < 0.05 and ++P < 0.01 for painful diabetic neuropathy against painless diabetic neuropathy.
Figure 5.
Tibial H-reflex RDD exhibits variability in patients with painful diabetic neuropathy but does show a relationship with pain VAS. A: Individual values for RDD at 1-Hz stimulation in control subjects (filled gray circles) and patients with painless (open circles) or painful (filled black/colored circles) diabetic neuropathy. Antineuropathic pain medication is indicated by letters adjacent to the relevant data point. A, amitriptyline; D, duloxetine; G, gabapentin; P, pregabalin. B: Dot plots of individual values for CNFD in control subjects and patients with painless or painful diabetic neuropathy.
Representative H-reflex waveforms collected at 1-Hz stimulation in subjects with and without painful neuropathy are presented in Fig. 4A. RDD increased progressively in all groups with increasing stimulation frequency but was significantly attenuated in patients with painful diabetic neuropathy compared with control subjects at frequencies of 0.5 Hz (P < 0.05), 1 Hz (P < 0.001), 3 Hz (P < 0.05), and 5.0 Hz (P < 0.05) (Fig. 4B) and at 1 Hz in patients with painful compared with those with painless diabetic neuropathy (P < 0.01). The magnitude of RDD in individual patients with painful diabetic neuropathy showed considerable variance (Fig. 5A), but there was a significant correlation between RDD and VAS score at 1 Hz (rs = 0.688; P = 0.01). RDD magnitude at 1 and 3 Hz significantly correlated with NSP but showed no significant correlation with physiological or structural measures of small- or large-fiber neuropathy (Table 3).
Figure 4.
Tibial H-reflex RDD is attenuated in patients with painful diabetic neuropathy. A: Representative electromyogram traces showing M and H waves in response to three consecutive stimulations at 1-Hz frequency in a patient with painless (upper triplicate) and painful (lower triplicate) diabetic neuropathy. Note the decline of the H-wave amplitude in the traces from the patient with painless neuropathy that illustrates RDD. B: RDD, expressed as H3-to-H1 ratio, at ascending stimulation frequencies in control subjects (n = 15: filled gray circles, solid line) and patients with painless (n = 14: open circles, large dashed line) and painful (n = 13: filled black circles, small dashed line) diabetic neuropathy. Data are group mean ± SEM. Statistically significant differences were identified with the Kruskal-Wallis test followed by Dunn post hoc test for multiple comparisons: *P < 0.05, ***P < 0.001 for painful diabetic neuropathy against control group; ++P < 0.01 for painful diabetic neuropathy against painless diabetic neuropathy.
Table 3.
Correlations between RDD and large- and small-fiber parameters
| RDD (Hz) |
|||||
|---|---|---|---|---|---|
| 0.3 | 0.5 | 1 | 3 | 5 | |
| Age | 0.070 | 0.036 | 0.153 | 0.115 | 0.028 |
| Diabetes duration | 0.247 | −0.031 | 0.116 | 0.220 | 0.215 |
| Significance | NS | NS | NS | NS | NS |
| NDS | −0.133 | 0.240 | 0.199 | 0.374 | 0.354 |
| Significance | NS | NS | NS | NS | NS |
| NSP | 0.111 | 0.193 | 0.431 | 0.395 | 0.307 |
| Significance | NS | NS | 0.028 | 0.049 | NS |
| VPT | −0.094 | −0.046 | 0.124 | 0.133 | −0.056 |
| Significance | NS | NS | NS | NS | NS |
| Cold perception threshold | −0.243 | −0.189 | −0.341 | −0.354 | −0.255 |
| Significance | NS | NS | NS | NS | NS |
| Warm perception threshold | 0.248 | −0.013 | 0.210 | 0.059 | 0.048 |
| Significance | NS | NS | NS | NS | NS |
| SSamp | −0.307 | 0.005 | −0.247 | −0.226 | −0.207 |
| Significance | NS | NS | NS | NS | NS |
| SSCV | −0.212 | 0.021 | −0.258 | −0.126 | −0.157 |
| Significance | NS | NS | NS | NS | NS |
| PMamp | −0.167 | −0.084 | −0.179 | −0.141 | −0.132 |
| Significance | NS | NS | NS | NS | NS |
| PMCV | −0.087 | −0.064 | −0.318 | −0.222 | −0.180 |
| Significance | NS | NS | NS | NS | NS |
| Hmax | −0.222 | −0.056 | −0.243 | −0.157 | −0.250 |
| Significance | NS | NS | NS | NS | NS |
| IENFD | −0.215 | −0.307 | −0.032 | −0.096 | 0.136 |
| Significance | NS | NS | NS | NS | NS |
| CNFD | −0.2524 | 0.046 | −0.367 | −0.018 | −0.250 |
| Significance | NS | NS | NS | NS | NS |
| CNFL | −0.176 | 0.071 | −0.350 | −0.150 | −0.365 |
| Significance | NS | NS | NS | NS | NS |
| CNBD | −0.2864 | 0.037 | −0.326 | −0.264 | −0.346 |
| Significance | NS | NS | NS | NS | NS |
Data are Spearman correlations (rs) and significance (P) between RDD and NDS, NSP, quantitative sensory tests, electrophysiology, and corneal and skin innervation. Significant correlations are in boldface type.
Patients With Painful Diabetic Neuropathy Have Corneal Nerve Loss
CNFD was reduced in patients with diabetes both painless (P < 0.05) and painful (P < 0.001) diabetic neuropathy compared with control subjects and further reduced in patients with painful compared with painless diabetic neuropathy (P < 0.05) (Table 2 and Fig. 5B). Measures of corneal innervation showed no significant correlation with pain VAS within the painful neuropathy group (CNFD, rs= −0.134, NS; CNFL, rs = −0.370, NS; CNBD, rs = −0.217, NS) although across the diabetic neuropathy cohort pain VAS showed a significant negative correlation with CNFD (rs = −0.567; P = 0.004) and CNFL (rs = −0.404; P = 0.04).
Discussion
We previously reported loss of RDD in a rat model of type 1 diabetes (14) and identified the contribution of spinal disinhibition to neuropathic pain states (15). The present preclinical studies show that RDD deficits in STZ-injected rats are not due to STZ neurotoxicity. Firstly, RDD deficits did not occur in STZ-injected rats pretreated with 3-OMG, a nontoxic, nonmetabolizable glucose derivative that protects pancreatic β-cells from destruction by STZ (23). Secondly, impaired RDD was absent in STZ-injected rats given extended insulin treatment from the onset of hyperglycemia. Thirdly, RDD deficits also developed in the ZDF rat model of type 2 diabetes. As both models of diabetes mirrored the neuropathy phenotype of many patients with diabetes by exhibiting concurrent conduction slowing and thermal hypoalgesia, these findings strengthen the potential clinical relevance of RDD as a biomarker for spinal disinhibition in patients with either type 1 or type 2 diabetes.
The efficacy of extended insulin replacement in preventing RDD deficits in STZ diabetic rats cannot distinguish between hypoinsulinemia or hyperglycemia as the primary pathogenic mechanism. We therefore compared treatment using a subcutaneous insulin pellet to generate a continuous mild reduction of hyperglycemia with insulin injections that produced acute and transient reductions of hyperglycemia. Both regimens resulted in restoration of RDD, disassociating impaired RDD from ambient hyperglycemia. There is increasing awareness that insulin has direct effects on the nervous system. Insulin receptors are present in primary sensory neurons and at nociceptor termination sites in the spinal cord dorsal horn (24,25). In diabetic rodents, local insulin administration to the periphery (26,27) or spinal cord (28) ameliorated indices of neuropathy and neuropathic pain (29) without impacting systemic hyperglycemia. Systemically delivered insulin also crosses the blood-brain barrier to activate central nervous system insulin receptors (30). The trophic effect of insulin extends to patients with diabetes, as continuous subcutaneous insulin infusion improved corneal nerve density without altering HbA1c (31). The onset of impaired RDD in ZDF rats, a model of type 2 diabetes, could potentially argue against a pathogenic role of insulin deficiency per se. However, RDD appeared only at an age where both insulinopenia and insulin resistance are features of the model (32,33). Insulin resistance has also been reported in peripheral nerves of type 2 diabetic rodents (34). As the time course of impaired RDD coincided with that of tactile allodynia, impaired RDD appears to be a biomarker of neuropathic pain in models of both type 1 and type 2 diabetes.
For further testing of the association between RDD and neuropathic pain, the effects of the 5-HT2A/C receptor agonist DOI and the serotonin-norepinephrine reuptake inhibitor duloxetine were evaluated in relation to RDD in diabetic rats. Both agents alleviate neuropathic pain in diabetic rats in a 5-HT2A/C–dependent fashion (17), and reversal of its effects on RDD by ketanserin and pruvanserin indicate actions mediated through 5-HT2A–binding sites. Duloxetine is recommended for painful diabetic neuropathy but has moderate overall efficacy and good effect in only a subgroup of patients (2). Interestingly, patients with diabetes with painful neuropathy and less efficient conditioned pain modulation, suggestive of spinal disinhibition, show greater therapeutic responses to duloxetine (35). The rapid restoration of allodynia and RDD by both drugs suggests that RDD could be useful for identification of therapies that selectively target neuropathic pain arising from spinal disinhibition and allows identification of patients most likely to respond to therapies targeting this axis.
The pertinence of our preclinical studies to humans is supported by observations that RDD is conserved across species, including humans (36,37). Indeed, the H-reflex in normal anesthetized rats shows a frequency dependence that is remarkably similar in magnitude to that observed in awake humans (15,38,39), while deficits caused in rats by the metabolic injury of diabetes are notably similar to those seen in anesthetized rats and awake humans after physical spinal cord injury (10,11,13,15,38). To test the potential for clinical translation of RDD as a biomarker for the pain generator site, we compared RDD in patients with painful and painless diabetic neuropathy with that of control subjects. While initial H-wave amplitude was reduced in both groups of patients with diabetes, RDD was impaired only in patients with painful diabetic neuropathy. This impairment was unrelated to the severity of neuropathy, as there was no significant correlation between RDD and measures of large- or small-fiber dysfunction. However, patients with higher pain scores had greater RDD attenuation, suggesting that spinal inhibitory dysfunction coexists with, and may contribute to, the pain phenotype in a subgroup of subjects with painful diabetic neuropathy.
Although RDD directly measures muscle depolarization in response to motor output from the spinal cord, it is modulated by spinal inhibitory systems (12,14) and therefore can provide information about spinal processing of sensory inputs. Use of other electrophysiological testing paradigms, such as evaluation of the nociceptive flexion reflex, a nociceptor-specific reflex elicited in response to stimulation of Aδ and C fibers, could provide additional information about how spinal processing is altered during painful diabetic neuropathy. Indeed, a recent study suggests that painful diabetic neuropathy is associated with enhanced nociceptive flexion reflex (40), but it is unclear whether this is due to increased peripheral sensitivity or altered spinal reflex processing. Future studies should address whether an enhanced nociceptive flexion reflex is associated with impaired RDD or an independent phenomenon.
Several of the patients with painful neuropathy were already taking the antineuropathic pain medications duloxetine, pregabalin, or amitriptyline, and we could not therefore undertake a systematic quantification of their effects on clinical pain and RDD. However, three of four patients with the most impaired RDD were taking duloxetine, whereas patients on amitriptyline or pregabalin tended to have RDD values within the range observed in patients with painless diabetic neuropathy and control subjects. Both amitriptyline and duloxetine increase serotonin and norepinephrine levels, which enhance descending inhibition (41). However, amitriptyline also inhibits 5-HT2A receptors (42) and therefore may not be able to reverse spinal disinhibition due to impaired GABAA receptor–mediated inhibition arising from decreased spinal KCC2 (43). We speculate that patients with impaired RDD indicative of impaired spinal inhibition may find duloxetine to be an efficacious treatment for their neuropathic pain. Further studies investigating the predictive value of RDD for the response to neuropathic pain treatment with specific agents will be important to test the premise that therapeutic responses may be significantly improved by accurately phenotyping patients and tailoring therapy that is mechanistically appropriate. A parallel approach focusing on peripherally driven pain has been tested in two randomized placebo controlled studies in which the best response to treatment with oxcarbazepine (44) and lignocaine 5% patch (45) was achieved in patients with an irritable nociceptor phenotype and preserved small-fiber function. Ultimately a battery of tests designed to identify peripheral and central pain generator sites may be optimal to identify therapy for achieving optimal efficacy.
In addition to RDD impairment, patients with diabetes with painful neuropathy also had a significant reduction in CNFD, confirming our previous findings (46) and in keeping with accruing data showing greater small-fiber pathology (47,48) and autonomic deficits (49) in patients with painful diabetic neuropathy. However, there was no significant correlation between corneal innervation and RDD status, suggesting that these pathologies may be independent of each other. This raises the intriguing possibility that these distinct biomarkers could be used together to refine our understanding of the underlying pathophysiology of pain in individual patients.
The present discovery study represents a first attempt to translate RDD analysis from experimental animals to patients with diabetes with neuropathic pain, albeit in a cross-sectional study with a relatively small sample size. There is clearly a need for larger cross-sectional and longitudinal studies to define the normative range for RDD in humans and to develop criteria to define abnormal RDD that can be applied to individual subjects for phenotyping purposes. Some patients with severe neuropathy have unobtainable tibial H-reflexes, potentially limiting the utility of RDD to those with mild to moderate neuropathy. Nevertheless, impaired RDD and a reduction in CNFD could together provide a means to more accurately phenotype patients with painful diabetic neuropathy. Such phenotyping could allow a more stratified approach to designing clinical trials of drugs in subjects with painful diabetic neuropathy and ultimately a more personalized therapeutic approach, based on site of pain generation and mechanism of drug action.
Supplementary Material
Article Information
Acknowledgments. The authors thank Victor Arballo and Veronica Lopez (University of California, San Diego) for expert technical assistance.
Funding. This research was funded by awards from the National Institutes of Health (NIH) (DK-057629 and NS-081082) and the American Diabetes Association (1-17-ICTS-062) to N.A.C. and from the NIH (1DP3DK104386-01) and JDRF International (27-2008-362) to R.A.M.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. A.G.M. and C.L.-K. were responsible for conception and design of the study, acquisition of data, analysis and interpretation of data, drafting the manuscript and revising it critically for important intellectual content, and final approval of the version to be submitted. S.A., M.F., and I.N.P. were responsible for acquisition and analysis of data and final approval of the version to be submitted. M.Z. was responsible for analysis of data, revising the manuscript critically for important intellectual content, and final approval of the version to be submitted. T.M.-Z. and K.F. were responsible for acquisition and analysis of preclinical data, revision of the manuscript for important intellectual content, and final approval of the version to be submitted. G.P., M.S.F., and H.F. were responsible for acquisition of data and final approval of the version to be submitted. M.T. was responsible for acquisition and analysis of data and final approval of the version to be submitted. M.J. was responsible for analysis of data and final approval of the version to be submitted. C.G.J. was responsible for conception and design of preclinical studies, acquisition and analysis of data, revision of the manuscript for important intellectual content, and final approval of the version to be submitted. A.J.M.B. was responsible for conception and design of the study and final approval of the version to be submitted. N.E. was responsible for conception and design of the study, revising the manuscript critically for important intellectual content, and final approval of the version to be submitted. N.A.C. was responsible for conception and design of the study, acquisition of data, analysis and interpretation of data, revising the manuscript critically for important intellectual content, and final approval of the version to be submitted. R.A.M. was responsible for conception and design of the study, analysis and interpretation of data, revising the manuscript critically for important intellectual content, and final approval of the version to be submitted. R.A.M. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-1181/-/DC1.
References
- 1.Abbott CA, Malik RA, van Ross ER, Kulkarni J, Boulton AJ. Prevalence and characteristics of painful diabetic neuropathy in a large community-based diabetic population in the U.K. Diabetes Care 2011;34:2220–2224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finnerup NB, Attal N, Haroutounian S, et al. . Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 2015;14:162–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Javed S, Petropoulos IN, Alam U, Malik RA. Treatment of painful diabetic neuropathy. Ther Adv Chronic Dis 2015;6:15–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campbell CM, Kipnes MS, Stouch BC, et al. . Randomized control trial of topical clonidine for treatment of painful diabetic neuropathy. Pain 2012;153:1815–1823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Themistocleous AC, Ramirez JD, Shillo PR, et al. . The Pain in Neuropathy Study (PiNS): a cross-sectional observational study determining the somatosensory phenotype of painful and painless diabetic neuropathy. Pain 2016;157:1132–1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tesfaye S, Boulton AJ, Dickenson AH. Mechanisms and management of diabetic painful distal symmetrical polyneuropathy. Diabetes Care 2013;36:2456–2465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee-Kubli CA, Calcutt NA. Painful neuropathy: mechanisms. Handb Clin Neurol 2014;126:533–557 [DOI] [PubMed]
- 8.Tesfaye S, Boulton AJ, Dyck PJ, et al.; Toronto Diabetic Neuropathy Expert Group . Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 2010;33:2285–2293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edwards RRDR, Dworkin RH, Turk DC, et al. . Patient phenotyping in clinical trials of chronic pain treatments: IMMPACT recommendations. Pain 2016;157:1851–1871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishikawa K, Ott K, Porter RW, Stuart D. Low frequency depression of the H wave in normal and spinal man. Exp Neurol 1966;15:140–156 [DOI] [PubMed] [Google Scholar]
- 11.Calancie B, Broton JG, Klose KJ, Traad M, Difini J, Ayyar DR. Evidence that alterations in presynaptic inhibition contribute to segmental hypo- and hyperexcitability after spinal cord injury in man. Electroencephalogr Clin Neurophysiol 1993;89:177–186 [DOI] [PubMed] [Google Scholar]
- 12.Matsushita A, Smith CM. Spinal cord function in postischemic rigidity in the rat. Brain Res 1970;19:395–410 [DOI] [PubMed] [Google Scholar]
- 13.Kakinohana O, Hefferan MP, Nakamura S, et al. . Development of GABA-sensitive spasticity and rigidity in rats after transient spinal cord ischemia: a qualitative and quantitative electrophysiological and histopathological study. Neuroscience 2006;141:1569–1583 [DOI] [PubMed] [Google Scholar]
- 14.Jolivalt CG, Lee CA, Ramos KM, Calcutt NA. Allodynia and hyperalgesia in diabetic rats are mediated by GABA and depletion of spinal potassium-chloride co-transporters. Pain 2008;140:48–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee-Kubli CA, Calcutt NA. Altered rate-dependent depression of the spinal H-reflex as an indicator of spinal disinhibition in models of neuropathic pain. Pain 2014;155:250–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sultan A, Gaskell H, Derry S, Moore RA. Duloxetine for painful diabetic neuropathy and fibromyalgia pain: systematic review of randomised trials. BMC Neurol 2008;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mixcoatl-Zecuatl T, Jolivalt CG. A spinal mechanism of action for duloxetine in a rat model of painful diabetic neuropathy. Br J Pharmacol 2011;164:159–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jolivalt CG, Frizzi KE, Guernsey L, et al. . Peripheral neuropathy in mouse models of diabetes. Curr Protoc Mouse Biol 2016;6:223–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidson E, Coppey L, Lu B, et al. The roles of streptozotocin neurotoxicity and neutral endopeptidase in murine experimental diabetic neuropathy. Exp Diabetes Res 2009;2009;431980 [DOI] [PMC free article] [PubMed]
- 20.Lauria G, Hsieh ST, Johansson O, et al. European Federation of Neurological Societies/Peripheral Nerve Society Guideline on the use of skin biopsy in the diagnosis of small fiber neuropathy. Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society. Eur J Neurol 2010;17:903–912, e44–49
- 21.Polydefkis M, Hauer P, Sheth S, Sirdofsky M, Griffin JW, McArthur JC. The time course of epidermal nerve fibre regeneration: studies in normal controls and in people with diabetes, with and without neuropathy. Brain 2004;127:1606–1615 [DOI] [PubMed] [Google Scholar]
- 22.Chen X, Graham J, Dabbah MA, et al. . Small nerve fiber quantification in the diagnosis of diabetic sensorimotor polyneuropathy: comparing corneal confocal microscopy with intraepidermal nerve fiber density. Diabetes Care 2015;38:1138–1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossini AA, Like AA, Dulin WE, Cahill GF Jr. Pancreatic beta cell toxicity by streptozotocin anomers. Diabetes 1977;26:1120–1124 [DOI] [PubMed] [Google Scholar]
- 24.Kou ZZ, Li CY, Tang J, et al. . Down-regulation of insulin signaling is involved in painful diabetic neuropathy in type 2 diabetes. Pain Physician 2013;16:E71–E83 [PubMed] [Google Scholar]
- 25.Sugimoto K, Murakawa Y, Sima AA. Expression and localization of insulin receptor in rat dorsal root ganglion and spinal cord. J Peripher Nerv Syst 2002;7:44–53 [DOI] [PubMed] [Google Scholar]
- 26.Guo G, Kan M, Martinez JA, Zochodne DW. Local insulin and the rapid regrowth of diabetic epidermal axons. Neurobiol Dis 2011;43:414–421 [DOI] [PubMed] [Google Scholar]
- 27.Chen DK, Frizzi KE, Guernsey LS, Ladt K, Mizisin AP, Calcutt NA. Repeated monitoring of corneal nerves by confocal microscopy as an index of peripheral neuropathy in type-1 diabetic rodents and the effects of topical insulin. J Peripher Nerv Syst 2013;18:306–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brussee V, Cunningham FA, Zochodne DW. Direct insulin signaling of neurons reverses diabetic neuropathy. Diabetes 2004;53:1824–1830 [DOI] [PubMed] [Google Scholar]
- 29.Hoybergs YM, Meert TF. The effect of low-dose insulin on mechanical sensitivity and allodynia in type I diabetes neuropathy. Neurosci Lett 2007;417:149–154 [DOI] [PubMed] [Google Scholar]
- 30.Jolivalt CG, Lee CA, Beiswenger KK, et al. . Defective insulin signaling pathway and increased glycogen synthase kinase-3 activity in the brain of diabetic mice: parallels with Alzheimer’s disease and correction by insulin. J Neurosci Res 2008;86:3265–3274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Azmi S, Ferdousi M, Petropoulos IN, et al. . Corneal confocal microscopy shows an improvement in small-fiber neuropathy in subjects with type 1 diabetes on continuous subcutaneous insulin infusion compared with multiple daily injection. Diabetes Care 2015;38:e3–e4 [DOI] [PubMed] [Google Scholar]
- 32.Shibata T, Takeuchi S, Yokota S, Kakimoto K, Yonemori F, Wakitani K. Effects of peroxisome proliferator-activated receptor-alpha and -gamma agonist, JTT-501, on diabetic complications in Zucker diabetic fatty rats. Br J Pharmacol 2000;130:495–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sugimoto K, Rashid IB, Kojima K, et al. . Time course of pain sensation in rat models of insulin resistance, type 2 diabetes, and exogenous hyperinsulinaemia. Diabetes Metab Res Rev 2008;24:642–650 [DOI] [PubMed] [Google Scholar]
- 34.Grote CW, Groover AL, Ryals JM, Geiger PC, Feldman EL, Wright DE. Peripheral nervous system insulin resistance in ob/ob mice. Acta Neuropathol Commun 2013;1:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yarnitsky D, Granot M, Nahman-Averbuch H, Khamaisi M, Granovsky Y. Conditioned pain modulation predicts duloxetine efficacy in painful diabetic neuropathy. Pain 2012;153:1193–1198 [DOI] [PubMed] [Google Scholar]
- 36.Meinck HM. Occurrence of the H reflex and the F wave in the rat. Electroencephalogr Clin Neurophysiol 1976;41:530–533 [DOI] [PubMed] [Google Scholar]
- 37.Schindler-Ivens S, Shields RK. Low frequency depression of H-reflexes in humans with acute and chronic spinal-cord injury. Exp Brain Res 2000;133:233–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thompson FJ, Reier PJ, Lucas CC, Parmer R. Altered patterns of reflex excitability subsequent to contusion injury of the rat spinal cord. J Neurophysiol 1992;68:1473–1486 [DOI] [PubMed] [Google Scholar]
- 39.Gozariu M, Roth V, Keime F, Le Bars D, Willer JC. An electrophysiological investigation into the monosynaptic H-reflex in the rat. Brain Res 1998;782:343–347 [DOI] [PubMed] [Google Scholar]
- 40.Gordeev SA, Turbina LG, Zus’man AA, Posokhov SI. Study of nociceptive flexion reflex in healthy subjects and patients with chronic neuropathic pain syndrome. Bull Exp Biol Med 2012;154:189–191 [DOI] [PubMed] [Google Scholar]
- 41.Sindrup SH, Otto M, Finnerup NB, Jensen TS. Antidepressants in the treatment of neuropathic pain. Basic Clin Pharmacol Toxicol 2005;96:399–409 [DOI] [PubMed] [Google Scholar]
- 42.Honda M, Nishida T, Ono H. Tricyclic analogs cyclobenzaprine, amitriptyline and cyproheptadine inhibit the spinal reflex transmission through 5-HT(2) receptors. Eur J Pharmacol 2003;458:91–99 [DOI] [PubMed] [Google Scholar]
- 43.Bos R, Sadlaoud K, Boulenguez P, et al. . Activation of 5-HT2A receptors upregulates the function of the neuronal K-Cl cotransporter KCC2. Proc Natl Acad Sci U S A 2013;110:348–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Demant DT, Lund K, Vollert J, et al. . The effect of oxcarbazepine in peripheral neuropathic pain depends on pain phenotype: a randomised, double-blind, placebo-controlled phenotype-stratified study. Pain 2014;155:2263–2273 [DOI] [PubMed] [Google Scholar]
- 45.Demant DT, Lund K, Finnerup NB, et al. . Pain relief with lidocaine 5% patch in localized peripheral neuropathic pain in relation to pain phenotype: a randomised, double-blind, and placebo-controlled, phenotype panel study. Pain 2015;156:2234–2244 [DOI] [PubMed] [Google Scholar]
- 46.Quattrini C, Tavakoli M, Jeziorska M, et al. . Surrogate markers of small fiber damage in human diabetic neuropathy. Diabetes 2007;56:2148–2154 [DOI] [PubMed] [Google Scholar]
- 47.Cheng HT, Dauch JR, Porzio MT, et al. . Increased axonal regeneration and swellings in intraepidermal nerve fibers characterize painful phenotypes of diabetic neuropathy. J Pain 2013;14:941–947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Truini A, Biasiotta A, Di Stefano G, et al. . Does the epidermal nerve fibre density measured by skin biopsy in patients with peripheral neuropathies correlate with neuropathic pain? Pain 2014;155:828–832 [DOI] [PubMed] [Google Scholar]
- 49.Gandhi RA, Marques JL, Selvarajah D, Emery CJ, Tesfaye S. Painful diabetic neuropathy is associated with greater autonomic dysfunction than painless diabetic neuropathy. Diabetes Care 2010;33:1585–1590 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.