Abstract
OBJECTIVE
We aimed to determine the effect of elevated BMI over time on the progression to type 1 diabetes in youth.
RESEARCH DESIGN AND METHODS
We studied 1,117 children in the TrialNet Pathway to Prevention cohort (autoantibody-positive relatives of patients with type 1 diabetes). Longitudinally accumulated BMI above the 85th age- and sex-adjusted percentile generated a cumulative excess BMI (ceBMI) index. Recursive partitioning and multivariate analyses yielded sex- and age-specific ceBMI thresholds for greatest type 1 diabetes risk.
RESULTS
Higher ceBMI conferred significantly greater risk of progressing to type 1 diabetes. The increased diabetes risk occurred at lower ceBMI values in children <12 years of age compared with older subjects and in females versus males.
CONCLUSIONS
Elevated BMI is associated with increased risk of diabetes progression in pediatric autoantibody-positive relatives, but the effect varies by sex and age.
Introduction
Studies report conflicting data regarding the roles of weight and obesity on type 1 diabetes risk (1–5). Most studies limit analyses to BMI at a single time point prior to diabetes diagnosis. Further, the influence of sex and age remain unexplored. We evaluated the longitudinal influence of cumulative excess BMI (ceBMI), a calculated aggregate measure of BMI elevation over time, on progression to type 1 diabetes in children of the TrialNet Pathway to Prevention (PTP) cohort.
Research Design and Methods
The TrialNet PTP study screened 3,285 individuals from March 2004 to June 2014 and monitored them for progression to diabetes through November 2015 (6). This analysis included participants aged 2–18 years at their first BMI evaluation with ≥2 BMI measurements before 20 years of age (n = 1,117). Baseline was defined as the first visit with a BMI evaluation.
Standard protocol oral glucose tolerance test and HbA1c were obtained at each visit (7). Diabetes was diagnosed according to American Diabetes Association criteria (8). HbA1c ≥6.5% was part of confirmatory testing (9).
BMI was calculated as weight (kg)/height (m2). ceBMI was adopted to measure persistent BMI elevation ≥85th percentile for age- and sex-adjusted BMI. Weighted sums of the differences between actual BMI and the corresponding 85th percentile at each BMI assessment were calculated (10,11) and then further annualized to accommodate irregular timing of BMI assessment in relation to time to diabetes or censoring (for calculation of ceBMI, see Supplementary Data). For individuals who progressed to diabetes, the last BMI used was ≥6 months prior to diagnosis date.
Statistical Considerations
Pearson χ2 tests, Fisher exact tests, Wilcoxon rank-sum tests, Kruskal-Wallis tests, and nonparametric Spearman rank correlation tests were used as appropriate. Analyses of BMI were based on relevant Centers for Disease Control and Prevention cutoffs (www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm). ceBMI was analyzed as both a continuous measure and a dichotomized measure. ceBMI ≥0 indicated that an individual’s average BMI was ≥85th age- and sex-adjusted percentile during the observation period.
The primary outcome was time to type 1 diabetes (i.e., time from first BMI evaluation to date of diagnosis). Those not diagnosed with type 1 diabetes were censored at their last follow-up or enrollment in a prevention trial. Kaplan-Meier methods assessed distribution differences in the time to type 1 diabetes among groups, and Cox proportional hazards models evaluated the influence of continuous and categorical variables. Assumptions for proportionality of hazards were tested. All time-to-event analyses were adjusted for age, sex, and antibody number confirmed at screening (single vs. multiple). Additional adjustment for the presence of the highest-risk HLA genotype (i.e., DR3-DQ2/DR4-DQ8) did not alter significance of the results. Recursive partitioning analysis was used to identify critical cut points for ceBMI and age at first BMI evaluation for influence on diabetes development and risk stratification of time-to-event (12) (rpart package in R).
Inferential tests were two-sided. Any P values <0.05 (0.1 for interaction terms) were considered significant. All analyses were conducted in R (version 3.1.2; Windows; Microsoft).
Results
We analyzed a total of 1,117 pediatric subjects of the PTP cohort between the ages of 2 and 18 years (median: 10.1 years; interquartile range [IQR]: 6.7–13.3 years), of whom 20% (n = 220) developed diabetes. Median first BMI percentile was 63.8% (IQR: 36.6–84.8%), with 14% overweight (BMI ≥85th to <95th percentile) and 11% obese (≥95th percentile). ceBMI ranged from −10 to 15.1 kg/m2 (median: −1.86 kg/m2; IQR: −3.6 to −0.03 m2/kg). Nearly 25% of subjects had ceBMI values ≥0 kg/m2 representing sustained excess BMI above the Centers for Disease Control and Prevention thresholds of overweight/obesity (Supplementary Table 1).
Higher ceBMI was associated with significantly greater risk of progression to type 1 diabetes, which persisted after adjusting for age at first BMI evaluation, antibody number, and sex. For each 1-kg/m2 increase in ceBMI, there was a 6.3% increased relative risk of type 1 diabetes progression (hazard ratio [HR]: 1.063 [95% CI 1.03–1.10]; P = 0.0006). Individuals who, on average, were persistently overweight or obese (ceBMI ≥0) had a 63% greater type 1 diabetes risk, adjusted for age, sex, and antibody number (HR: 1.63 [95% CI: 1.22–2.18]; P = 0.0009).
Age at baseline was a significant independent risk factor for type 1 diabetes progression (HR: 0.94; P = 0.0006), adjusted for ceBMI, sex, and antibody status. A significant interaction between age and sex together with ceBMI in relation to time to diabetes (P = 0.072) triggered investigation of age- and sex-specific strata. By recursive partitioning algorithms, we first identified 12 years as the age cut point that best discriminated risk for type 1 diabetes progression for the combined cohort and for males or females independently. Recursive partitioning analysis as well as multivariable model-based diagnostics identified cut points for ceBMI that best differentiated risk for disease progression (ceBMI diabetes risk threshold). The ceBMI diabetes risk threshold was lower in children <12 years, regardless of sex (−1.4 kg/m2), than in older children (4.6 kg/m2). That is, the increase in type 1 diabetes risk occurs at lower levels of sustained excess BMI in younger children.
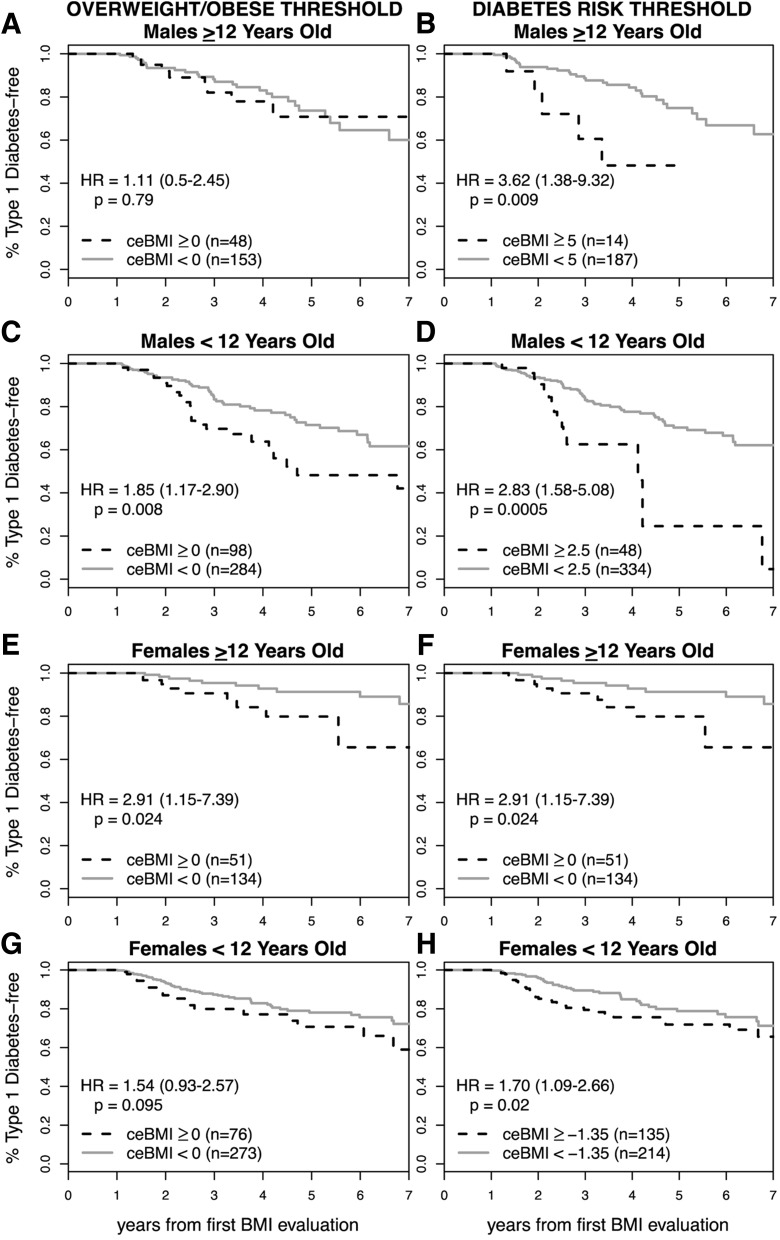
Males overall had a higher ceBMI diabetes risk threshold influencing progression to type 1 diabetes than females, suggesting an increased sensitivity to BMI in female subjects. Males ≥12 years of age were least affected by ceBMI and had a risk threshold (5 kg/m2) much higher than the threshold defining overweight/obese. In contrast, females <12 years old appeared to be most influenced by body weight, as the ceBMI risk threshold was −1.35 kg/m2, suggesting that BMI percentiles below the overweight/obese threshold still increase type 1 diabetes risk in this subgroup (Fig. 1).
Figure 1.
Effect of ceBMI on type 1 diabetes risk comparing traditional overweight/obese ceBMI definitions to age- and sex-specific ceBMI diabetes risk thresholds. Proportion type 1 diabetes–free pediatric subjects of the PTP cohort according to age (≥12 vs. <12 years old) and sex strata (males vs. females). A, C, E, and G: Assessment of overweight/obese threshold based on the 85th percentile for age- and sex-adjusted BMI. Dotted lines indicate ceBMI ≥0 (overweight/obese); solid gray indicates ceBMI <0 (nonoverweight/obese). B, D, F, and H: Assessment of ceBMI diabetes risk thresholds identified by recursive partitioning. Dotted lines indicate greater than or equal to age- and sex-specific ceBMI diabetes risk threshold; solid gray indicates less than age- and sex-specific ceBMI diabetes risk threshold. All models adjusted for antibody number (single vs. multiple).
Conclusions
Our study is the first to apply ceBMI methodology to type 1 diabetes, and results support that sustained elevation of BMI is associated with type 1 diabetes progression, with effects varying by sex and age. Older age diluted the effect of elevated BMI on type 1 diabetes progression as seen by a lower ceBMI diabetes risk threshold in individuals <12 years old compared with those ≥12 years old. This age-dependent effect of sustained excess BMI on type 1 diabetes progression is present in both sexes, but females were more sensitive to the effect of elevated BMI.
These findings lend insight into prior studies that reported inconsistent results of the effects of BMI on type 1 diabetes risk (2–5). Beyond incorporation of longitudinal data, ceBMI measurement offers the additional advantage of an unrestricted upper limit compared with BMI percentile and may offer greater resolution than BMI Z-score.
Limitations include the lack of Tanner staging and sex hormone measurements that could elucidate mechanisms of the identified age- and sex-specific ceBMI diabetes risk thresholds. Our study was not designed to specifically address the effects of acute changes in BMI on disease onset, and the small number of diabetes events in some age and sex strata further hindered this ability. Finally, we investigated an at-risk cohort of autoantibody-positive relatives of patients with type 1 diabetes; although this cohort was heterogeneous, the results may not be broadly applicable to the general population.
Our results indicate that sustained elevation of BMI is associated with increased progression to type 1 diabetes in an at-risk pediatric population and that the BMI 85th percentile may not appropriately differentiate this risk for all pediatric subjects. Our data suggest that lifestyle modifications may delay disease onset in an at-risk population and suggest age- and sex-specific ceBMI thresholds to implement such changes.
Supplementary Material
Article Information
Funding. The sponsor of the trial was the Type 1 Diabetes TrialNet PTP Study Group. The Type 1 Diabetes TrialNet PTP Study Group is a clinical trials network funded by the National Institutes of Health through the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Allergy and Infectious Diseases, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, through the cooperative agreements U01-DK-061010, U01-DK-061034, U01-DK-061042, U01-DK-061058, U01-DK-085465, U01-DK-085453, U01-DK-085461, U01-DK-085463, U01-DK-085466, U01-DK-085499, U01-DK-085504, U01-DK-085505, U01-DK-085509, U01-DK-103180, U01-DK-103153, U01-DK-085476, and U01-DK-103266 and JDRF. This work was also partially supported by National Institutes of Health grants K12-DK-094726 (to C.T.F.) and U01-DK-103180-01 (to M.J.R.).
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or JDRF.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. C.T.F. designed the analysis and study design, researched data, and wrote the manuscript. S.M.G. analyzed the data, contributed statistical support, and contributed to the writing of the manuscript. Y.-F.L., C.E.-M., I.M.L., R.B., D.J.B., H.R., A.M., and S.E.G. reviewed and edited the manuscript and contributed to the discussion. M.J.R. contributed to the data analysis design and interpretation of results and critically revised the manuscript. All authors are members of the Type 1 Diabetes TrialNet Study Group. M.J.R. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 76th Scientific Sessions of the American Diabetes Association, New Orleans, LA, 10–14 June 2016.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-2331/-/DC1.
A complete list of the Type 1 Diabetes TrialNet Study Group can be found in the Supplementary Data online.
References
- 1.Wilkin TJ. The accelerator hypothesis: weight gain as the missing link between type I and type II diabetes. Diabetologia 2001;44:914–922 [DOI] [PubMed] [Google Scholar]
- 2.Elding Larsson H, Vehik K, Haller MJ, et al.; TEDDY Study Group . Growth and risk for islet autoimmunity and progression to type 1 diabetes in early childhood: the Environmental Determinants of Diabetes in the Young Study. Diabetes 2016;65:1988–1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meah FA, DiMeglio LA, Greenbaum CJ, et al.; Type 1 Diabetes TrialNet Study Group . The relationship between BMI and insulin resistance and progression from single to multiple autoantibody positivity and type 1 diabetes among TrialNet Pathway to Prevention participants. Diabetologia 2016;59:1186–1195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuchlbauer V, Vogel M, Gausche R, et al. High birth weights but not excessive weight gain prior to manifestation are related to earlier onset of diabetes in childhood: ‘accelerator hypothesis’ revisited. Pediatr Diabetes 2014;15:428–435 [DOI] [PubMed] [Google Scholar]
- 5.Sosenko JM, Krischer JP, Palmer JP, et al.; Diabetes Prevention Trial–Type 1 Study Group . A risk score for type 1 diabetes derived from autoantibody-positive participants in the Diabetes Prevention Trial–Type 1. Diabetes Care 2008;31:528–533 [DOI] [PubMed] [Google Scholar]
- 6.Greenbaum CJ, Mandrup-Poulsen T, McGee PF, et al.; Type 1 Diabetes Trial Net Research Group; European C-Peptide Trial Study Group . Mixed-meal tolerance test versus glucagon stimulation test for the assessment of beta-cell function in therapeutic trials in type 1 diabetes. Diabetes Care 2008;31:1966–1971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sosenko JM, Mahon J, Rafkin L, et al.; Diabetes Prevention Trial-Type 1 and TrialNet Study Groups . A comparison of the baseline metabolic profiles between Diabetes Prevention Trial-Type 1 and TrialNet Natural History Study participants. Pediatr Diabetes 2011;12:85–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Diabetes Association Standards of medical care in diabetes—2014. Diabetes Care 2014;37(Suppl. 1):S14–S80 [DOI] [PubMed] [Google Scholar]
- 9.Skyler JS, Greenbaum CJ, Lachin JM, et al.; Type 1 Diabetes TrialNet Study Group . Type 1 Diabetes TrialNet–an international collaborative clinical trials network. Ann N Y Acad Sci 2008;1150:14–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JM, Gebremariam A, Vijan S, Gurney JG. Excess body mass index-years, a measure of degree and duration of excess weight, and risk for incident diabetes. Arch Pediatr Adolesc Med 2012;166:42–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouchard DR, Porneala B, Janssen I, et al. Risk of type 2 diabetes and cumulative excess weight exposure in the Framingham Offspring Study. J Diabetes Complications 2013;27:214–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu P, Krischer JP; Type 1 Diabetes TrialNet Study Group . Prognostic classification factors associated with development of multiple autoantibodies, dysglycemia, and type 1 diabetes—a recursive partitioning analysis. Diabetes Care 2016;39:1036–1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.