Abstract
Objectives
Dual lipid-lowering and anti-inflammatory properties of statins may lead to survival benefits in patients with rheumatoid arthritis (RA). However, data on this topic are limited, and the role of statins in RA remains unclear. We examined the association of statin use with overall mortality among RA patients in a general population context.
Methods
We conducted an incident user cohort study with time-stratified propensity score matching using a UK general population database. The study population included individuals aged ≥20 years who had a diagnosis of RA and the use of at least one disease modifying anti-rheumatic drug (DMARD) between January 2000 and December 2012. To closely account for potential confounders, we compared propensity score matched cohorts of statin initiators and comparators (non-initiators) within 1-year cohort accrual blocks.
Results
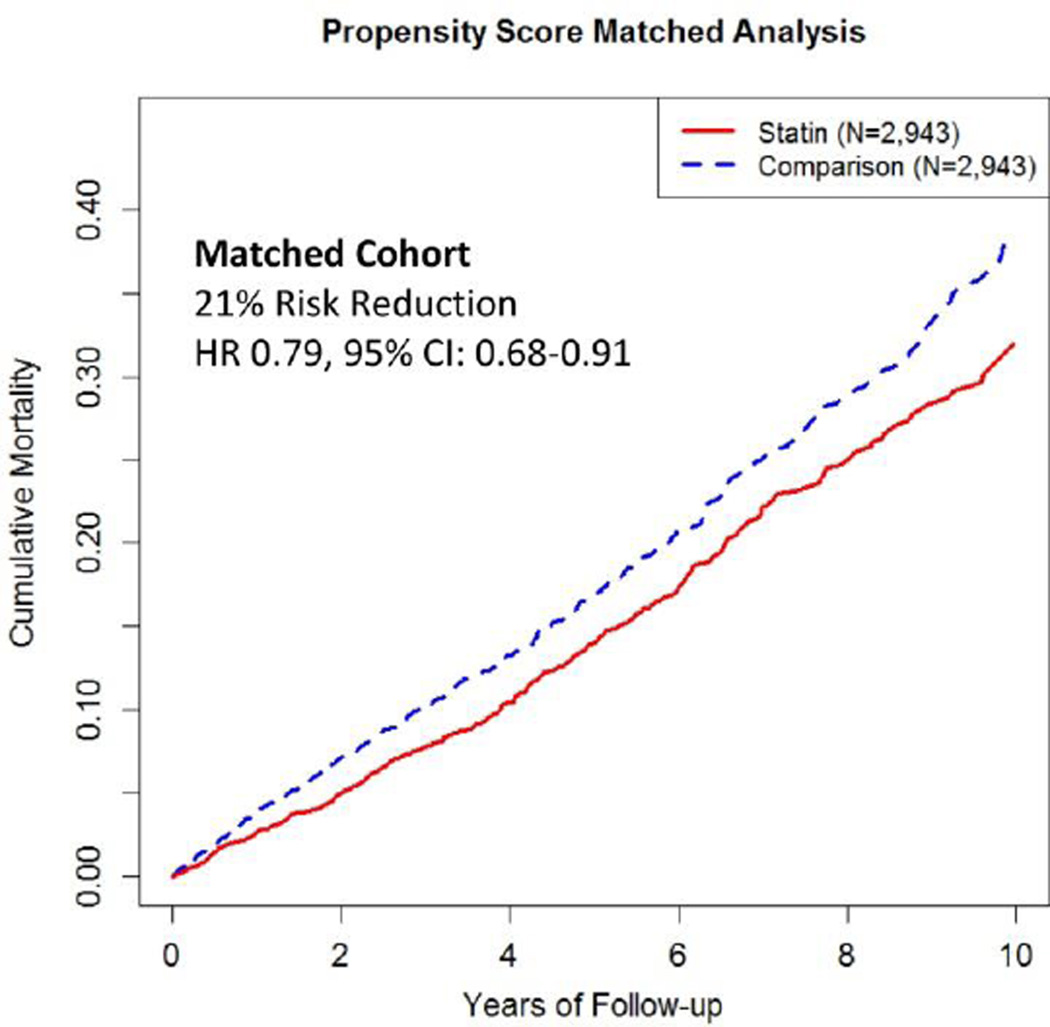
There were 432 deaths during follow up (mean=4.51 years) of the 2,943 statin initiators for an incidence rate of 32.6/1000 person-years (PY), while the 513 deaths among 2,943 matched comparators resulted in an incidence rate of 40.6/1000 PY. Baseline characteristics were well-balanced across the two groups. Statin initiation was associated with a 21% lower risk of all cause mortality (HR 0.79, 95% CI 0.68–0.91). When we defined RA by its diagnosis code alone (not requiring DMARD use), the corresponding HR was 0.81 (95% CI 0.74–0.90).
Conclusions
Statin initiation is associated with a lower risk of mortality among RA patients. The magnitude of association is similar to that seen in previous randomized trials among the general population.
Keywords: Rheumatoid Arthritis, Statin, Mortality, Cardiovascular Disease
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic, inflammatory arthritis associated with systemic inflammation and characterized by substantial disability and premature mortality. [1–4] This increased risk of mortality is associated with more severe disease activity and is likely due in part to higher levels of systemic inflammation in patients with RA. [5–8]
Hydroxymethylglutaryl-coenzyme A reductase inhibitors, or “statins,” reduce mortality by up to 30% in patients with coronary artery disease (CAD) and congestive heart failure (CHF). [9–13] Statins also confer a survival benefit in primary prevention in the general population, with two recent meta-analyses showing a 9% and 14% reduced risk of mortality associated with statin use. [14,15] The JUPITER (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) trial demonstrated that rosuvastatin decreases the risk of cardiovascular (CV) events or cardiovascular mortality in otherwise healthy individuals who have low LDL cholesterol but elevated high-sensitivity C-reactive protein (hsCRP). [16] Subjects treated with rosuvastatin also experienced a 20% reduction in all cause mortality (p=0.02).
Statins have not only lipid lowering effects, but also anti-inflammatory properties that involve regulating leukocyte-endothelial cell adhesion, reducing nitric oxide (NO) production and decreasing levels of inflammatory cytokines such as TNF-alpha, IL-1 and IL-6. [17,18] Indeed, a randomized controlled trial of RA patients found that the addition of statins to standard disease modifying anti-rheumatic drug (DMARD) therapy resulted in an improvement in clinical parameters such as disease activity score and swollen joint count as well as in inflammatory markers. [19] The dual benefits of lipoprotein improvement and anti-inflammatory effects might be expected to confer a survival benefit to RA patients, at least similar to and potentially greater than that seen among the general population without a history of CVD or inflammatory disease. A recent randomized trial was initiated to examine the impact of atorvastatin in preventing CV events in RA patients (Trial of Atorvastatin for the Primary Prevention of Cardiovascular Events in Patients with Rheumatoid Arthritis [TRACE-RA]); however, the trial was terminated early due to the low event rate. [20,21] To help address this knowledge gap, we evaluated the association of statin initiation with the risk of death among individuals with RA in a general population context.
METHODS
Data Source
We used The Health Improvement Network (THIN), a computerized medical record database entered by general practitioners (GPs) in the UK. Data on approximately 10.2 million patients are systematically recorded and sent anonymously to THIN. Approximately 97% of the UK population is registered with a GP, [22] making THIN data representative of the general population of the UK. [23] Information in THIN includes demographic information, details from GP visits, diagnoses from specialists’ visits and hospital admissions, laboratory tests, and additional information including height, weight, alcohol use and smoking status. The Read classification system is used to code specific diagnoses, [24] and prescriptions written by the GP are coded in THIN using the Multilex classification system, a standard drug terminology library used in the UK that includes information on drug formulation and strength. During office visits, GPs record patient health information using a computerized system, and they receive training and feedback to ensure that data recording is accurate. [25] Data from THIN therefore reflect routine medical practices in a population-based setting and have been shown to be valid for use in epidemiologic and clinical studies. [26]
Study Population
Our study population included individuals aged ≥20 years who had a recorded diagnosis of RA and use of at least one DMARD between January 2000 and December 2012 (see supplementary file for RA diagnostic codes and DMARDs). This definition of RA has been shown to have a specificity of 96% in the UK General Practice Research Database (GPRD) [27] and has been used to accurately identify RA cases in healthcare utilization data. [28] Study cohort members were required to have ≥ 1 years of enrollment with the general practice before entering the study cohort. Individuals were excluded if they were current or prior statin users or if they had incomplete records of covariates (cholesterol level, body mass index [BMI], drinking status and smoking status). A secondary definition of RA using only an RA diagnostic code without requiring the use of a DMARD was applied as a sensitivity analysis.
The Propensity Score Matched Cohorts Stratified by Time Blocks
Confounding by indication, where baseline characteristics of compared groups differ in ways that alter outcome risk, can be a major concern in observational studies of medication effects; we therefore employed propensity score-matching to address this threat to validity. Further, to address potential secular trends in statin use and mortality risk, cohorts were matched within the same calendar year (i.e., 13 blocks from January 2000 to December 2012).
Within each annual cohort accrual block, statin initiators were defined as patients who started a statin during that year, while eligible patients who did not start a statin were their potential matches. Propensity scores (predicted probability of statin initiation) were estimated using logistic regression, separately for each cohort accrual block. For each statin initiator, we identified a propensity score matched subject who did not initiate a statin during the accrual block using a 5-to-1 digit “greedy matching” algorithm. [29,30] The initiation date was used as the index date for that patient, and a random date within the one-year block was assigned as the index date for non-initiators.
The variables included in the logistic regression model consisted of RA duration prior to the index date, socio-demographic factors, BMI, lifestyle factors, comorbidities, medication use, and healthcare utilization. Specifically, socio-demographic information included age at the index date, sex, and the Townsend Deprivation Index score, an indicator for economic status. [31,32] Lifestyle factors included smoking status and alcohol use. Comorbidities included MI, atrial fibrillation, ischemic heart disease, peripheral vascular disease, CHF, valvular heart disease, transient ischemic attack, other circulatory disease, stroke, hypertension, chronic obstructive pulmonary disease, chronic kidney disease (stage ≥3), liver disease, diabetes, cancer, pneumonia or infection, dementia, depression, venous thromboembolism, and varicose veins. Medications included nitrates, angiotensin-converting-enzyme inhibitors, angiotensin receptor blockers, beta-blockers, calcium channel blockers, aspirin, non-steroidal anti-inflammatory drugs (NSAIDs), loop diuretics, hydrochlorothiazide (HCTZ), thiazide-like diuretics, potassium sparing diuretics, insulin, DMARDs, glucocorticoids, biologic medications, and anticoagulants. Laboratory measurements included total cholesterol levels. Healthcare utilization variables included the number of general practitioner visits, hospitalizations, referrals and number of medications as assessed over the two years prior to the index date.
Statistical Analysis
The outcome of interest was all-cause mortality as defined by the death date recorded in THIN. Statin initiators and matched non-initiators began accruing risk time from the index date until death, disenrollment in THIN or the end of the study period, whichever came first. Statin initiators and non-initiators in each cohort retained their original exposure status throughout the follow-up. This approach maintains the comparability of these two exposure groups in terms of the baseline characteristics and provides conservative estimates, similar to an intent-to-treat approach used in clinical trials.
We used Cox proportional hazard models to estimate the association of statin initiation with the risk of all-cause mortality, stratified by 1-year cohort accrual blocks. Survival plots were generated as estimates of cumulative mortality to identify time trends in the occurrence of death. We repeated the same analyses limited to individuals with only a record of RA but not requiring use of a DMARD. We conducted subgroup analyses stratified by sex, age group (<60 years versus 60–69 years vs ≥70 years), the Townsend Deprivation Index score (≤ 2 versus > 2), RA duration (≤ 5 years versus > 5 years), and history of circulatory disease. As a sensitivity analysis, we used symmetric trimming with the cut point at the 5th percentiles and 95th percentiles of the propensity score matching. [33] Finally, we performed the same analysis excluding patients with a history of CVD (i.e. MI, ischemic heart disease, transient ischemic attack, stroke). To address the potential for statin initiators to discontinue the drug over time, we performed sensitivity analyses with follow-up time truncated at 1 year, 2 years, and 3 years for all subjects. For all hazard ratios (HRs), we calculated 95% confidence intervals (CIs). All P-values were two-sided. All statistical analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
RESULTS
There were an average 264 statin initiators and 3,495 statin non-initiators among the RA subjects who were eligible for propensity score matching and cohort inclusion in each 1 year accrual block. When statin initiators were compared to randomly chosen non-initiators using 1:1 matching, statin initiators had a higher prevalence of cardiovascular disease (CVD), coronary heart disease risk factors, other comorbidities and use of cardiovascular-related and other medications (n=3,438 in each group; Table 1 and Supplementary Table 1). During the follow up of these unmatched cohorts, 532 died in the statin initiator group and 374 died in the non-initiator group (HR 1.46, 95% CI 1.28–1.67; Supplemental Figure 1).
Table 1.
Selected Baseline Characteristics in the Unmatched and Propensity-Score Matched Cohorts
| Baseline Characteristics | Unmatched* Cohort | Propensity-Score Matched Cohort | ||
|---|---|---|---|---|
| Statin Initiators (N=3,438) |
Non-Initiators (N=3,438) |
Statin Initiators (N=2,943) |
Non-Initiators (N=2,943) |
|
| Demographics | ||||
| Age, years, | 65.4 | 62.4 | 65.3 | 65.7 |
| Male, % | 35.5 | 26.0 | 34.4 | 34.7 |
| Socio-Economic Deprivation Index Score** |
2.8 | 2.7 | 2.8 | 2.8 |
| RA Characteristics | ||||
| RA Duration, years | 10.1 | 10.2 | 10.0 | 10.3 |
| Lifestyle factors | ||||
| BMI, kg/m2 | 27.9 | 27.1 | 27.9 | 28.0 |
| Smoking | ||||
| Current, % | 21.4 | 18.2 | 21.0 | 20.5 |
| Past, % | 35.9 | 28.6 | 35.5 | 36.1 |
| None, % | 42.8 | 53.2 | 43.5 | 43.5 |
| Alcohol Use | ||||
| Current, % | 69.5 | 71.5 | 70.3 | 70.9 |
| Past, % | 4.5 | 3.3 | 4.4 | 4.1 |
| None, % | 27.0 | 25.2 | 25.3 | 25.0 |
| Measures of comorbidity | ||||
| Charlson index | 1.2 | 0.9 | 1.1 | 1.1 |
| Myocardial Infarction,% | 9.9 | 1.4 | 7.0 | 6.4 |
| Ischemic Heart Disease, % | 19.8 | 4.2 | 15.3 | 15.1 |
| Peripheral Vascular Disease, % | 3.0 | 0.5 | 2.5 | 2.4 |
| Congestive Heart Failure, % | 4.2 | 1.9 | 3.8 | 3.6 |
| Transient Ischemic Attack, % | 5.2 | 1.1 | 4.8 | 4.7 |
| Stroke, % | 5.7 | 1.4 | 5.0 | 5.2 |
| Hypertension, % | 54.8 | 42.3 | 53.9 | 54.7 |
| Chronic Kidney Disease, % | 9.0 | 8.0 | 9.2 | 9.3 |
| Diabetes, % | 20.4 | 5.6 | 18.9 | 19.8 |
| Medications | ||||
| Antihypertensive medicine, % | 69.5 | 47.2 | 66.9 | 68.0 |
| Aspirin, % | 37.0 | 9.8 | 32.0 | 31.6 |
| NSAIDs, % | 58.5 | 60.3 | 58.3 | 58.0 |
| Loop diuretics, % | 14.0 | 9.7 | 13.0 | 13.2 |
| Thiazide-like diuretic, % | 3.1 | 1.9 | 2.8 | 3.0 |
| DMARDs, % | 100.0 | 100.0 | 100.0 | 100.0 |
| Glucocorticoids, % | 37.4 | 33.9 | 36.8 | 36.4 |
| Laboratory measurements | ||||
| Cholesterol, mg/dl | 233.2 | 206.8 | 231.0 | 231.0 |
| Health Care Utilization | ||||
| General Practice visits*** | 17.4 | 15.2 | 17.1 | 17.0 |
| Hospitalizations*** | 0.9 | 0.6 | 0.8 | 0.9 |
| Referrals*** | 1.0 | 0.9 | 1.0 | 1.0 |
| Number of Medications Prescribed*** | 3.5 | 3.2 | 3.5 | 3.6 |
A non-initiator was randomly selected to match to each initiator within 1-year cohort accrual block.
Socio-Economic Deprivation Index Score was measured by the Townsend Deprivation Index, which was grouped into quintiles from 1 (least deprived) to 5 (most deprived).
Frequency during the past two year.
In comparison, after propensity score matching, the baseline characteristics were well balanced between the two groups (n=2,943 in each group; Table 1 and Supplementary Table 1). The standardized differences of the baseline characteristics ranged from 0 to 3% (all p-values > 0.2), which were well within the often used guideline of 10%. [34] Patients in the matched cohort were 34% male and had a mean age of 65 years. There were 432 deaths in the statin initiator group and 513 deaths in the non-initiator group during the follow up period (mean 4.51 years and 4.29 years in the initiator and comparator groups, respectively; Table 2). The corresponding incidence rates were 32.6 and 40.6 per 1000 person years, respectively, and the hazard ratio for mortality associated with statin initiation was 0.79 (95% CI 0.68–0.91) (Table 2, Figure 1). The HRs in the analyses with follow up truncated at 1 year, 2 years and 3 years were 0.65 (95% CI 0.48–0.89), 0.70 (95% CI 0.55–0.88), and 0.76 (95% CI 0.62–0.93), respectively (Table 2).
Table 2.
Hazard Ratios for Mortality Associated with Statin Initiation According to the Follow-up Period
|
RA defined by diagnosis code and DMARD use |
Statin Initiator (N=2,943) | Non- Initiator (N=2,943) | |||||
|
Death Cases (n) |
Mean Follow Up (Years) |
IR (case/1,000py) |
Death Cases (n) |
Mean Follow Up (Years) |
IR (case/1,000py) |
HR (95% CI) | |
| Total follow-up | 432 | 4.51 | 32.56 | 513 | 4.29 | 40.64 | 0.79 (0.68 to 0.91) |
| 1 year follow-up | 72 | 0.94 | 26.09 | 106 | 0.92 | 39.05 | 0.65 (0.48 to 0.89) |
| 2 year follow-up | 132 | 1.76 | 25.44 | 187 | 1.72 | 36.97 | 0.70 (0.55 to 0.88) |
| 3 year follow-up | 195 | 2.47 | 26.76 | 252 | 2.40 | 35.75 | 0.76 (0.62 to 0.93) |
|
RA defined by diagnosis code |
Statin Initiator (N=6,401) | Non- Initiator (N=6,401) | |||||
|
Death Cases (n) |
Mean Follow Up (Years) |
IR (case/1,000py) |
Death Cases (n) |
Mean Follow Up (Years) |
IR (case/1,000py) |
HR (95% CI) | |
| Total follow-up | 1027 | 4.57 | 35.12 | 1118 | 4.34 | 40.20 | 0.81 (0.74 to 0.90) |
| 1 year follow-up | 173 | 0.94 | 28.88 | 234 | 0.92 | 39.54 | 0.73 (0.60 to 0.89) |
| 2 year follow-up | 323 | 1.75 | 28.76 | 429 | 1.72 | 39.07 | 0.74 (0.63 to 0.85) |
| 3 year follow-up | 459 | 2.46 | 29.19 | 586 | 2.38 | 38.40 | 0.76 (0.66 to 0.86) |
Figure 1.
Time to Death for the Propensity-Score Matched Cohort of Patients with Rheumatoid Arthritis
Sensitivity Analyses
When we repeated the analysis with a less restrictive definition of RA (diagnostic code only), more patients qualified (n=6,401 in each group), but the association between statin initiation and mortality did not change materially (HR 0.81, 95% CI 0.74 to 0.90) (Table 2). When we examined the association between statin initiation and mortality in a number of different subgroups, the inverse association with statin initiation persisted (Table 3). We excluded patients with a prior history of CVD and found that statin use was still associated with a 25% reduction in all cause mortality (HR 0.75, 95% CI 0.61–0.92). Finally, after we performed the 5th and 95th percentile symmetry trimming of our propensity score matched cohorts, our results remained similar (HR 0.77, 95% CI 0.66– 0.90).
Table 3.
Association Between Statin Initiation and Mortality According to Different Populations
| Hazard Ratio (95% CI) | |
|---|---|
| All Patients | 0.79 (0.68 to 0.91) |
| By Age, years | |
| <60 | 0.79 (0.40 to 1.58) |
| 60–69 | 0.77 (0.56 to 1.07) |
| 70–90 | 0.77 (0.63 to 0.94) |
| By Sex, | |
| Male | 0.75 (0.58 to 0.98) |
| Female | 0.71 (0.59 to 0.86) |
| By Socio-Economic Deprivation Index Score | |
| ≤ 2 | 0.70 (0.54 to 0.89) |
| > 2 | 0.73 (0.60 to 0.86) |
| By RA duration, years | |
| ≤ 5 | 0.75 (0.57 to 1.00) |
| > 5 | 0.73 (0.60 to 0.87) |
| By Baseline Cholesterol Level, mg/dl | |
| ≤ 230 | 0.77 (0.61 to 0.97) |
| > 230 | 0.70 (0.57 to 0.85) |
| By history of circulatory disease* | |
| No | 0.72 (0.49 to 1.06) |
| Yes | 0.81 (0.69 to 0.94) |
Defined as MI, atrial fibrillation, ischemic heart disease, peripheral vascular disease, congestive heart failure, valvular heart disease, transient ischemic attack, stroke or hypertension
DISCUSSION
In this large cohort study of RA patients derived from the general population, we found that statin initiation was associated with a 21% lower risk of all-cause mortality among patients with RA. This association was apparent from the first year through the subsequent years of follow-up. These associations were independent of age, sex, BMI, socio-economic status, relevant comorbidities, cardiovascular medication use, total cholesterol levels, and healthcare utilization. Further, subgroup analyses suggested no meaningful heterogeneity of the inverse association according to key covariates (age, sex, socio-economic status, RA duration, baseline cholesterol levels, and history of circulatory disease). Importantly, the magnitude of inverse association between statin use and mortality was similar to that observed in many previous studies of non-RA patients, [9,10,16]. However, the magnitude was slightly greater than that observed in two recent meta-analyses of statin use for primary prevention in the general population. [14,15] Although the differences were small, this finding may not be surprising in light of the fact that RA patients are at a higher risk for CVD than the general population, and could benefit from the dual anti-inflammatory [19] and lipid-lowering effects of statins in a way that the general population may not. [35]
The increased risk of CVD and premature mortality in RA, as well as the contribution of inflammation to this risk, has given rise to considerable interest in the cardioprotective role of statins in RA. To our knowledge, the current study is the first to evaluate the association of statin initiation with all-cause mortality in patients with RA irrespective of whether they had a history of CVD. One previous study attempted to assess the potential survival impact of the prevalent use of statins in 430 RA patients, and reported a 64% reduction in mortality. [36] However, approaches investigating prevalent users (as opposed to incident users) are vulnerable to selecting patients who are already tolerating and benefitting from statins (i.e., selection bias). The current study adopted an incident user design as well as an intent-to-treat analytic approach to help emulate the paradigm of randomized controlled trials. An additional study of statins in secondary prevention of CVD showed that patients with inflammatory joint disease treated with high dose statins, including 199 patients with RA, had a similar reduction in lipid levels and CV events as those without RA. [37] Given the relatively small number of RA patients in this analysis, it remains unclear if there was sufficient power to detect a germane subgroup effect (by presence of RA), although it is interesting to note that the HR in this study was nearly identical to the one in our current study.
Our findings expand upon prior evidence for the beneficial effects of statins in RA which have been indirectly drawn from: 1) studies evaluating intermediate markers of CVD and premature mortality in RA; [38–40] 2) anti-rheumatic and lipid findings from studies evaluating RA disease outcomes; [19] and 3) studies evaluating statin effects in other patient populations, such as the JUPITER trial. [16] For example, statins have shown promising results including improvement of endothelial function, [38] a reduction in arterial stiffness,[39] and regression of carotid artery plaque height [40] in patients with RA. In the TARA trial, along with demonstrating that RA disease activity improved significantly in the atorvastatin group compared to placebo, total cholesterol, low density lipoprotein cholesterol, and triglyceride levels also declined substantially. [19] Finally, the applicability of findings from the JUPITER trial to patients with RA has been argued on the basis of RA itself being a risk factor for CVD and early mortality.
The strengths of our study are worthy of discussion. This is a large-scale study conducted among the general population with a substantial number of statin initiators and a sufficient number of outcomes to produce meaningful estimates. Indeed, the strength of a large-scale observational study such as this one is of particular importance in light of the recent TRACE-RA trial that was terminated prematurely due to a low event rate. [20,21] In pharmacoepidemiologic studies such as this one, confounding by indication can pose a problem and bias results. Indeed, in our unmatched analysis, the baseline characteristics of RA patients who were taking statins were quite different from those who were not taking statins; in particular, the initiators had more CVD and comorbidities and more use of cardiovascular medications. As such, one would expect that statin use might actually be associated with a higher risk of mortality due to this increased prevalence of comorbidities among statin initiators, and this was in fact the case in the comparison of our unmatched cohorts (Supplementary Figure 1). However, after we employed propensity score matching to our cohorts (thereby balancing baseline covariate distributions), we found that statin initiation was associated with a lower risk of mortality. In addition, matching within 1 year blocks flexibly allows for changes in the relative importance of potential confounding variables to be accounted for at different times. Although matching could result in less generalizability, we were able to match nearly 90% of the statin initiators, making generalizability less of a concern.
Potential limitations of our study also deserve comment. While our study found a lower risk of mortality associated with statin initiation among RA patients, we were unable to address cause-specific mortality, as these data are generally incomplete within THIN. Nevertheless, knowledge of the overall lower mortality risk associated with statin use among RA patients is critically significant in and of itself. We hypothesize that the lower mortality rate associated with statins stems from the reduction of cardiovascular-specific mortality in RA patients, and this speculation calls for future studies that address cause-specific mortality outcomes. Because our study was a complete case analysis that excluded patients with missing values, it is possible that this could affect the pool of statin non-users as they may be less likely to have cholesterol values recorded. However, exclusion of these patients would be unlikely to affect our results significantly and, if anything, would bias towards more conservative estimates of the role of statins. While we do not have information about disease activity in the THIN database, it is unlikely that it would have significantly influenced a physician’s decision to initiate a statin, making it improbable that disease activity would be acting as a confounder. Furthermore, our matched cohorts were well balanced for use of glucocorticoids, NSAIDs, biologics and by definition, all patients were required to use a DMARD, making it unlikely that there was meaningful imbalance in use of these drugs between the two groups. Finally, while our propensity score matching allowed us to control many variables, our study was observational, and thus we cannot exclude the possibility that there was residual or unknown confounding.
In conclusion, we found that statin initiation was associated with a 21% lower risk of mortality among patients with RA. The magnitude of the inverse association between statin use and mortality among RA patients was similar to that seen in previous randomized trials among non-RA patients. While awaiting definitive randomized trial evidence on the topic (which is challenging to obtain, as demonstrated by the recent experience of the TRACE-RA trial [20,21]), statin initiation appears to be associated with a lower risk of mortality in RA patients.
Supplementary Material
Acknowledgments
None
Funding: This work was supported in part by a grant from the NIH (P60AR047785).
Footnotes
Competing Interests: None
Contributorship:
Sara R. Schoenfeld: Design, Analysis and Draft
Leo Lu: Design, Analysis, Data Extraction and Draft
Sharan K. Rai: Analysis and Draft
John D. Seeger: Analysis and Draft
Yuqing Zhang: Design, Analysis and Draft
Hyon K. Choi: Design, Analysis and Draft
Ethical approval information: Ethical approval was obtained from The Health Improvement Network (THIN) Institutional Review Board.
Data Sharing Statement: At this moment there are no additional unpublished data.
REFERENCES
- 1.Ogdie A, Haynes K, Troxel AB, et al. Risk of mortality in patients with psoriatic arthritis, rheumatoid arthritis and psoriasis: a longitudinal cohort study. Ann Rheum Dis. 2014 Jan;73(1):149–153. doi: 10.1136/annrheumdis-2012-202424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bjornadal L, Baecklund E, Yin L, et al. Decreasing mortality in patients with rheumatoid arthritis: results from a large population based cohort in Sweden, 1964–95. J Rheumatol. 2002 May;29(5):906–912. [PubMed] [Google Scholar]
- 3.Maradit-Kremers H, Crowson CS, Nicola PJ, et al. Increased unrecognized coronary heart disease and sudden deaths in rheumatoid arthritis: a population-based cohort study. Arthritis Rheum. 2005 Feb;52(2):402–411. doi: 10.1002/art.20853. [DOI] [PubMed] [Google Scholar]
- 4.Avina-Zubieta JA, Choi HK, Sadatsafavi M, et al. Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum. 2008 Dec 15;59(12):1690–1697. doi: 10.1002/art.24092. [DOI] [PubMed] [Google Scholar]
- 5.Sattar N, McCarey DW, Capell H, et al. Explaining how "high-grade" systemic inflammation accelerates vascular risk in rheumatoid arthritis. Circulation. 2003 Dec 16;108(24):2957–2963. doi: 10.1161/01.CIR.0000099844.31524.05. [DOI] [PubMed] [Google Scholar]
- 6.Goodson NJ, Symmons DP, Scott DG, et al. Baseline levels of C-reactive protein and prediction of death from cardiovascular disease in patients with inflammatory polyarthritis: a ten-year followup study of a primary care-based inception cohort. Arthritis Rheum. 2005 Aug;52(8):2293–2299. doi: 10.1002/art.21204. [DOI] [PubMed] [Google Scholar]
- 7.Wolfe F, Michaud K, Gefeller O, et al. Predicting mortality in patients with rheumatoid arthritis. Arthritis Rheum. 2003 Jun;48(6):1530–1542. doi: 10.1002/art.11024. [DOI] [PubMed] [Google Scholar]
- 8.Pincus T, Brooks RH, Callahan LF. Prediction of long-term mortality in patients with rheumatoid arthritis according to simple questionnaire and joint count measures. Ann Intern Med. 1994 Jan 1;120(1):26–34. doi: 10.7326/0003-4819-120-1-199401010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994 Nov 19;344(8934):1383–1389. [PubMed] [Google Scholar]
- 10.Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med. 1998 Nov 5;339(19):1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 11.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002 Jul 6;360(9326):7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 12.Horwich TB, MacLellan WR, Fonarow GC. Statin therapy is associated with improved survival in ischemic and non-ischemic heart failure. J Am Coll Cardiol. 2004 Feb 18;43(4):642–648. doi: 10.1016/j.jacc.2003.07.049. [DOI] [PubMed] [Google Scholar]
- 13.Alehagen U, Benson L, Edner M, et al. Association Between Use of Statins and Outcomes in Heart Failure With Reduced Ejection Fraction: A Prospective Propensity Score Matched Cohort Study of 21,864 Patients in the Swedish Heart Failure Registry. Circ Heart Fail. 2015 Jan 9; doi: 10.1161/CIRCHEARTFAILURE.114.001730. [DOI] [PubMed] [Google Scholar]
- 14.Cholesterol Treatment Trialists' (CTT) Collaborators. Mihaylova B, Emberson J, Blackwell L, et al., editors. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012 Aug 11;380(9841):581–590. doi: 10.1016/S0140-6736(12)60367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane database Syst Rev. 2013 Jan 31;1:CD004816. doi: 10.1002/14651858.CD004816.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. The N Engl J Med. 2008 Nov 20;359(21):2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 17.Abeles AM, Pillinger MH. Statins as antiinflammatory and immunomodulatory agents: a future in rheumatologic therapy? Arthritis Rheum. 2006 Feb;54(2):393–407. doi: 10.1002/art.21521. [DOI] [PubMed] [Google Scholar]
- 18.Jain MK, Ridker PM. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005 Dec;4(12):977–987. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- 19.McCarey DW, McInnes IB, Madhok R, et al. Trial of Atorvastatin in Rheumatoid Arthritis (TARA): double-blind, randomised placebo-controlled trial. Lancet. 2004 Jun 19;363(9426):2015–2021. doi: 10.1016/S0140-6736(04)16449-0. [DOI] [PubMed] [Google Scholar]
- 20.Peters MJ, Nurmohamed MT. Cardiovascular risk management in rheumatoid arthritis: are we still waiting for the first step? Arthritis Res Ther. 2013 Mar 19;15(2):111. doi: 10.1186/ar4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kitas GD, Nightingale P, Armitage J, et al. Trial of atorvastatin for the primary prevention of cardiovascular events in patients with rheumatoid arthritis (TRACE RA) Ann Rheum Dis. 2015;74(Suppl2):688. [Google Scholar]
- 22.Simon C. Overview of the GP Contract. InnovAiT. 2008;1:134–139. [Google Scholar]
- 23.Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care. 2004;12(3):171–177. doi: 10.14236/jhi.v12i3.124. [DOI] [PubMed] [Google Scholar]
- 24.Stuart-Buttle CD, Read JD, Sanderson HF, et al. A language of health in action: Read Codes, classifications and groupings. Proc AMIA Annu Fall Symp. 1996:75–79. [PMC free article] [PubMed] [Google Scholar]
- 25.Epic. THIN data from EPIC: a guide for researchers. London: EPIC; 2007. [Google Scholar]
- 26.Lewis JD, Schinnar R, Bilker WB, et al. Validation studies of the health improvement network (THIN) database for pharmacoepidemiology research. Pharmacoepidemiol Drug Saf. 2007 Apr;16(4):393–401. doi: 10.1002/pds.1335. [DOI] [PubMed] [Google Scholar]
- 27.Thomas SL, Edwards CJ, Smeeth L, et al. How accurate are diagnoses for rheumatoid arthritis and juvenile idiopathic arthritis in the general practice research database? Arthritis Rheum. 2008 Sep 15;59(9):1314–1321. doi: 10.1002/art.24015. [DOI] [PubMed] [Google Scholar]
- 28.Kim SY, Servi A, Polinski JM, et al. Validation of rheumatoid arthritis diagnoses in health care utilization data. Arthritis Res Ther. 2011 Feb 23;13(1):R32. doi: 10.1186/ar3260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seeger JD, Williams PL, Walker AM. An application of propensity score matching using claims data. Pharmacoepidemiol Drug Saf. 2005 Jul;14(7):465–476. doi: 10.1002/pds.1062. [DOI] [PubMed] [Google Scholar]
- 30.Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res. 2011 May;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morris R, Carstairs V. Which deprivation? A comparison of selected deprivation indexes. J Public Health Med. 1991 Nov;13(4):318–326. [PubMed] [Google Scholar]
- 32.Townsend P, Phillimore P, Beattie A. Health and deprivation: Inequality and the North. London: Croom Helm; 1988. [Google Scholar]
- 33.Sturmer T, Rothman KJ, Avorn J, et al. Treatment effects in the presence of unmeasured confounding: dealing with observations in the tails of the propensity score distribution--a simulation study. Am J Epidemiol. 2010 Oct 1;172(7):843–854. doi: 10.1093/aje/kwq198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. The Central Role of the Propensity Score in Observational Studies for Causal Effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- 35.Sever PS, Poulter NR, Chang CL, et al. Evaluation of C-reactive protein before and on-treatment as a predictor of benefit of atorvastatin: a cohort analysis from the Anglo-Scandinavian Cardiac Outcomes Trial lipid-lowering arm. J Am Coll Cardiol. 2013 Aug;62(8):717–729. doi: 10.1016/j.jacc.2013.02.098. [DOI] [PubMed] [Google Scholar]
- 36.Sheng X, Murphy MJ, Macdonald TM, et al. Effectiveness of statins on total cholesterol and cardiovascular disease and all-cause mortality in osteoarthritis and rheumatoid arthritis. J Rheumatol. 2012 Jan;39(1):32–40. doi: 10.3899/jrheum.110318. [DOI] [PubMed] [Google Scholar]
- 37.Semb AG, Kvien TK, DeMicco DA, et al. Effect of intensive lipid-lowering therapy on cardiovascular outcome in patients with and those without inflammatory joint disease. Arthritis Rheum. 2012 Sep;64(9):2836–2846. doi: 10.1002/art.34524. [DOI] [PubMed] [Google Scholar]
- 38.Hermann F, Forster A, Chenevard R, et al. Simvastatin improves endothelial function in patients with rheumatoid arthritis. J Am Coll Cardiol. 2005 Feb 1;45(3):461–464. doi: 10.1016/j.jacc.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 39.Van Doornum S, McColl G, Wicks IP. Atorvastatin reduces arterial stiffness in patients with rheumatoid arthritis. Ann Rheum Dis. 2004 Dec;63(12):1571–1575. doi: 10.1136/ard.2003.018333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rollefstad S, Ikdahl E, Hisdal J, et al. Rosuvastatin induced carotid plaque regression in patients with inflammatory joint diseases: The RORA-AS study. Arthritis Rheum. 2015 doi: 10.1002/art.39114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.