Abstract
Allergic bronchopulmonary aspergillosis (ABPA) is a pulmonary disorder that often occurs in patients with asthma or cystic fibrosis (CF) and is characterized by a hypersensitivity response to the allergens of the fungus Aspergillus fumigatus. In patients with CF, growth of A. fumigatus hyphae within the bronchial lumen triggers an immunoglobulin E (IgE)-mediated hypersensitivity response that results in airway inflammation, bronchospasm, and bronchiectasis. In most published studies, the prevalence of ABPA is about 8.9% in patients with CF. Since the clinical features of this condition overlap significantly with that of CF, ABPA is challenging to diagnose and remains underdiagnosed in many patients. Diagnosis of ABPA in CF patients should be sought in those with evidence of clinical and radiologic deterioration that is not attributable to another etiology, a markedly elevated total serum IgE level (while off steroid therapy) and evidence of A. fumigatus sensitization. Management of ABPA involves the use of systemic steroids to reduce inflammation and modulate the immune response. In patients who do not respond to steroids or cannot tolerate them, antifungal agents should be used to reduce the burden of A. fumigatus allergens. Recent studies suggest that omalizumab may be an effective option to reduce the frequency of ABPA exacerbations in patients with CF. Further randomized controlled trials are needed to better establish the efficacy of omalizumab in managing patients with CF and ABPA.
Key words: Allergic bronchopulmonary aspergillosis, allergic fungal mycosis, cystic fibrosis
Cystic fibrosis (CF) is an autosomal recessive life-limiting multisystem disorder that results from defective functioning of the CF transmembrane conductance regulator (CFTR) protein.[1] CFTR is a complex glycoprotein (1480 amino acids) encoded by the CFTR gene, which is located on the long arm of chromosome 7 (7q31.2).[2] Physiologic activity of CFTR is necessary to maintain the normal consistency of respiratory and gastrointestinal secretions, which in turn is vital for innate immunity and proper digestion and absorption of nutrients.[3] In patients with CF, a genetic defect leads to defective functioning of the CFTR protein, which results in diverse pathologic manifestations including bronchiectasis, sinonasal polyposis, pancreatic insufficiency, and infertility.[4] Progressive destruction of lung parenchyma and decline in pulmonary function are the major life-limiting complications of CF.
Allergic bronchopulmonary aspergillosis (ABPA) is a pulmonary disorder that often occurs in patients with asthma or CF and is caused by hypersensitivity to the allergens of Aspergillus fumigatus.[5]A. fumigatus is a ubiquitous, spore-forming fungus that has been associated with multiple pulmonary disorders including ABPA, aspergilloma, invasive aspergillosis, allergic asthma, and hypersensitivity pneumonitis.[6] In patients with CF, growth of A. fumigatus hyphae within the bronchial lumen triggers an immunoglobulin E (IgE)-mediated hypersensitivity response with resultant bronchial inflammation and airway destruction and fibrosis (bronchiectasis). Patients often experience wheezing, pulmonary infiltrates, and a central (proximal) pattern of bronchiectasis.[7] Because of the overlapping features of ABPA with asthma, CF, and other diseases, this condition often remains underdiagnosed and there may be a long delay (of up to 10 years) between the first occurrence of symptoms and subsequent diagnosis.[8] In some countries, ABPA may be confused with other diseases, such as pulmonary tuberculosis, in nearly one-third of cases.[9]
Given that CF and ABPA have overlapping clinical, radiographic, and immunologic features, the diagnosis of ABPA in patients with CF remains challenging. Consequently, a number of international conferences have been organized and guidelines have been published to standardize the diagnosis and management of ABPA in CF patients.[10] Over the past one decade, newer therapies for ABPA in patients with CF have been developed and shown to be effective.[11] In this review, we present the epidemiology, clinical features, diagnostic evaluation, and management of ABPA in CF patients in the light of the currently available evidence.
Literature Search
In order to collate literature for this review, we performed a search of three large databases (PubMed, Ovid, and Medline) on March 23, 2016. Queries were performed using the keywords “Allergic bronchopulmonary aspergillosis” AND “Cystic fibrosis.” We limited our search by restricting to articles published after the year 2000. This was done to ensure that only the most recently available data were collated for this review. Duplicate entries and articles which focused on pulmonary disorders other than ABPA were excluded. Abstracts of articles deemed relevant to this review were read by the authors of this study. We retrieved full texts of all the included publications (systematic reviews (SRs), clinical trials, observational studies, laboratory studies, and review articles) that discussed ABPA in patients with CF. Reference lists of these articles were also reviewed to include articles that were deemed relevant to this review. The total number of relevant publications identified and the overall literature review process are summarized in Figure 1. Information from these articles was organized into several key areas identified by mutual consensus among authors. A critical appraisal of the reviewed literature is provided herein.
Figure 1.
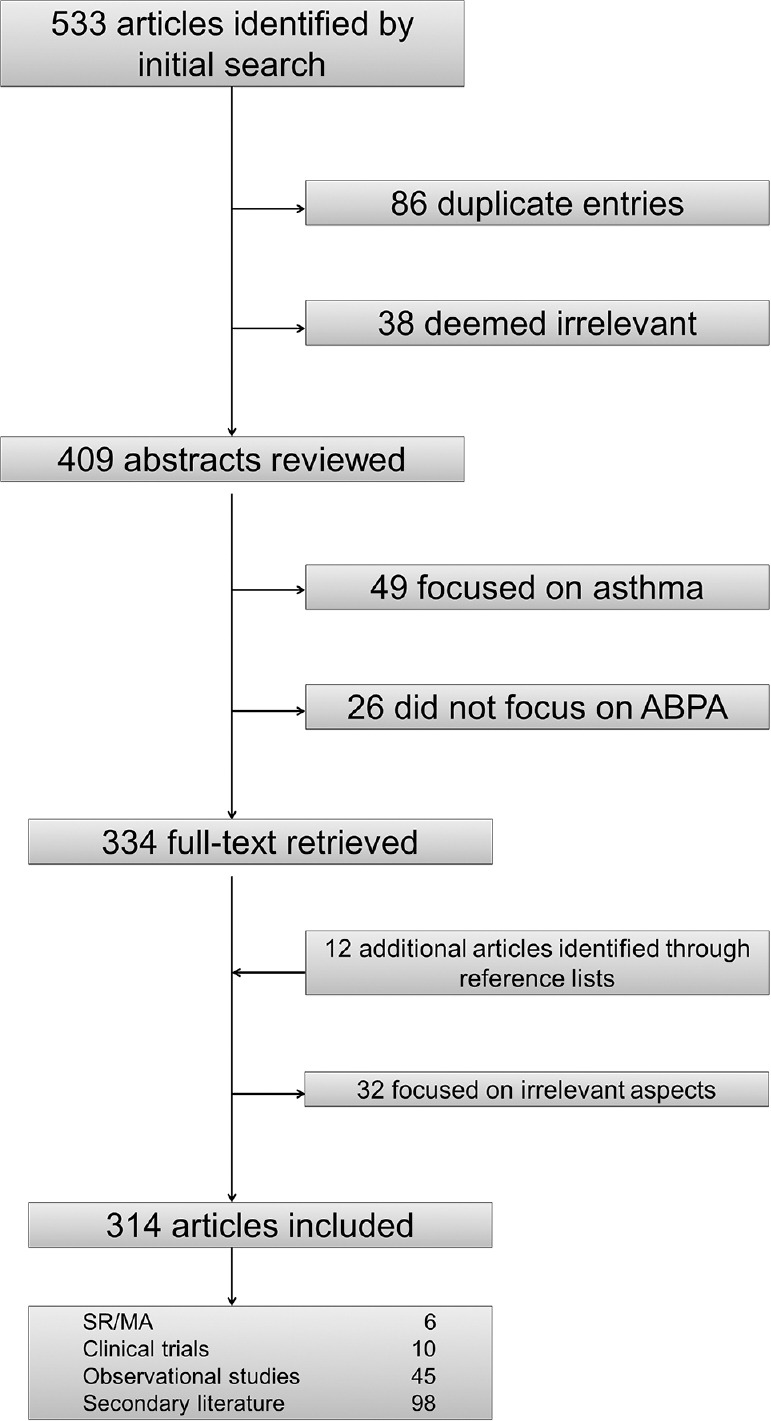
A flow chart depicting the inclusion and exclusion of articles for the purpose of this review. ABPA = Allergic bronchopulmonary aspergillosis; MA = Meta-analyses; SR = Systematic reviews
Epidemiology
In a study by Sudfeld et al. using the John Hopkins Cystic Fibrosis Integrative Microbiology Database, close to 36% of individuals with CF were found to grow A. fumigatus in airway cultures, and the prevalence of A. fumigatus colonization increased from 1997 to 2007.[12] Aspergillus sensitization (AS) in patients with CF as diagnosed by the measurement of A. fumigatus-specific IgE has been shown to be nearly 32.8%.[13,14,15,16,17,18,19] Studies using skin prick testing have reported even higher estimates ranging from 42.8% to 65% in some series.[19,20,21,22,23,24,25]
Prevalence of ABPA in patients with asthma has generally been reported to be around 1%–3%.[26] In contrast, estimates of the prevalence of ABPA in patients with CF have been reported to be much higher.[19] Point estimates of prevalence vary widely depending on the diagnostic criteria used, population studied (children vs. adults), and geographic region of the study. Adult patients with CF tend to have a higher prevalence of ABPA as compared to children. For instance, Chotirmall et al. reported a 12% prevalence rate of ABPA in adult CF patients in Ireland using the CF Foundation (CFF) diagnostic criteria.[27] Using the same diagnostic criteria, Jubin et al. reported a prevalence rate of 9.4% in children with CF in France.[28] Moreover, the prevalence of ABPA in CF patients differs greatly from one region to the other. In the Epidemiologic Study of Cystic Fibrosis registry based on the United States and Canada, the prevalence of ABPA has been estimated to be only 2%.[26] On the other hand, a significantly higher prevalence of 7.8% has been noted in the Epidemiologic Registry of CF (ERCF) from Europe.[29] Finally, the prevalence of ABPA also varies significantly depending on the diagnostic criteria used for the diagnosis. As an example, Fillaux et al. reported the prevalence of ABPA in children with CF in France to be nearly 13.5%.[30] In another study from France, Fillaux et al. determined the prevalence of ABPA in children with CF using the CFF diagnostic criteria, which was strikingly lower (3.4%) than the previous estimate (13.5%).[31]
In a SR published in 2015, Maturu and Agarwal analyzed the results of 45 studies reporting the prevalence of ABPA and concluded that there was significant publication bias and heterogeneity among the published studies.[29] The prevalence of ABPA in these studies varied significantly ranging from 3% to 25% with a pooled prevalence of 8.9% (95% confidence interval: 7.4%–10.7%).
Pathogenesis
AS, defined as the presence of either immediate cutaneous hypersensitivity to A. fumigatus antigens or A. fumigatus-specific IgE antibodies in the serum, is the first step in the pathogenesis of ABPA.[32] In patients with ABPA, exposure to A. fumigatus spores and hyphae results in an IgE-mediated hypersensitivity response. This allergic response to A. fumigatus antigens leads to a number of clinical and immunologic manifestations, which culminate in ABPA. Before delving into the immunopathogenesis of ABPA, it would be useful to review the biology of A. fumigatus itself.
A. fumigatus is an ascomycete belonging to the subdivision Deuteromycotina within the fungal kingdom.[33] While A. fumigatus is considered the most common allergenic species within the Aspergillus genus, other species within this genus also have important medical importance. Aspergillus clavatus has been implicated in producing allergenic responses and possibly ABPA.[34] Moreover, Aspergillus terreus and Aspergillus flavus species have been reported to possess amphotericin B resistance.[35] This may have important therapeutic implications for patients.
A. fumigatus generally grows easily on routine bacteriological and mycological media and is capable of growing at temperatures ≥50°C. The ability to grow rapidly at 37°C is an important pathogenic feature and allows the rapid progression of invasive disease.[36] Moreover, A. fumigatus spores are very small in size (3–5 μm), which enable them to reach deeper into the smaller airways. At the same time, a thick hydrophobic protein coat allows these spores to evade phagocytosis by macrophages—the first line of immune defense against A. fumigatus.[37] Upon reaching the alveoli, spores germinate to produce fungal hyphae. Neutrophils and monocytes serve as the second line of defense for the body by killing fungal hyphae through opsonin-dependent and opsonin-independent mechanisms. On the other hand, A. fumigatus possesses a number of virulence factors to evade the immune system.[38] These virulence factors include superoxide dismutases, catalases, mannitol, proteases, ribotoxin, phthioic acid, phospholipases, gliotoxin, and a hemolysin. While these virulence factors have a definitive role in the pathogenesis of invasive aspergillosis, many of these proteins are antigenic and can be the target of immune responses in patients with ABPA.[39]
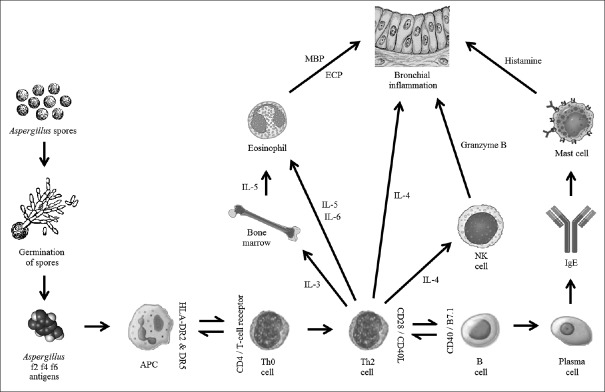
In patients with CF, CFTR dysfunction leads to abnormal mucociliary clearance of secretions. When such patients are exposed to A. fumigatus spores, impaired mucociliary clearance and defective innate immune responses lead to accumulation and persistence of fungal spores within the smaller airways.[40] Germination of spores leads to the formation of fungal hyphae and release of antigens, proteases, phospholipases, and other virulence factors. Such factors damage airway epithelial cells and allow a large dose of antigenic factors access to the interstitial and vascular compartments.[41] Antigen-presenting cells possessing human leukocyte antigen (HLA)-DR5 or HLA-DR2 process these antigens and present peptides in association with major histocompatibility complex Class II to CD4+ T-cells located within the bronchoalveolar lymphoid tissue.[13] This results in the activation of T-cells and release of inflammatory cytokines that favor a CD4+ Th2 response. A predominant CD4+ Th2 response in patients with ABPA is thought to be related to genetically determined factors and explains why all patients with CF do not develop ABPA despite having CFTR dysfunction.[42]
Activation of CD4+ Th2 cells leads to the activation of a humoral immune response, which entails production of IgE-producing B-lymphocytes and plasma cells. In addition, the release of cytokines, such as interleukin-4 (IL-4), IL-5, and IL-13, results in enhanced formation and differentiation of eosinophils and isotype switching of B-cells to IgE.[43] Interestingly, experimental studies have shown that B-cells from patients with ABPA have higher sensitivity to IL-4 and spontaneously produce larger amounts of IgE, IgG, and IgA antibodies against A. fumigatus antigens.[44] Some laboratory evidence suggests that this may be accounted for by polymorphisms in the IL-4 receptor α-chain (IL-4Rα), which result in a gain-of-function effect and promote exaggerated synthesis of IgE antibodies.[45]
Attachment of IgE to mast cells and cross-linking of IgE molecules result in mast cell degranulation and release of histamine, leukotrienes (LTB), and other mediators, which precipitate bronchospasm and other manifestations of a hypersensitivity response. Eosinophils are also important effector cells in patients with ABPA and are recruited by cytokines, such as LTB4, platelet-activating factor, eotaxin, monocyte chemoattractant protein-3 (MCP-3), and Regulated on Activation, Normal T cell-Expressed and Secreted (RANTES).[46] Eosinophils possess Fc receptors for IgE, IgG, and IgA; binding of A. fumigatus-specific IgG, IgA, and IgE molecules to these receptors and their cross-linking results in degranulation of eosinophils. Release of major basic protein, eosinophil cationic protein, and eosinophil-derived neurotoxin from eosinophils damages airway epithelial cells and further aggravates bronchial inflammation [Figure 2].[47]
Figure 2.
A diagram depicting the model of pathogenesis of allergic bronchopulmonary aspergillosis. APC = Antigen-presenting cell; ECP = Eosinophil cationic protein; HLA = Human leukocyte antigen; IL = Interleukin; MBP = Major basic protein; NK = Natural killer
Airway epithelial cells also contribute to the inflammatory response in ABPA by producing pro-inflammatory cytokines including IL-6, IL-8, and MCP-1.[48] Moreover, continuous damage to the epithelial cell layer triggers repair processes, which induce an influx of extracellular matrix proteins into the airway lumen. A. fumigatus spores and hyphae can attach to these matrix proteins and persist indefinitely within the smaller airways.[49] Attachment of fungal spores and hyphae to the smaller airways allows A. fumigatus antigens to continuously aggravate inflammatory responses as well as elaborate factors that worsen damage to airway epithelial cells and induce mast cell degranulation. Over a long period of time, ongoing bronchial inflammation and pulmonary damage result in the development of bronchiectasis.[50]
Here, it should be noted that some of the immunopathogenic responses seen in patients with ABPA are similar to those seen in patients with atopic asthma. However, patients with ABPA tend to have a greater burden of A. fumigatus allergens, which accumulate and persist within the smaller airways.[51] Moreover, patients with ABPA usually have IgE antibodies directed against A. fumigatus antigens Asp f2, Asp f4, and/or Asp f6. This is in contrast with patients with atopic asthma, who usually possess IgE antibodies directed against Asp f1 and/or Asp f3 antigens.[39,52,53,54,55] In addition, B-cells and mast cells from patients with ABPA demonstrate hyperresponsiveness, which may be partly accounted for by polymorphisms in the IL-4Rα chain.[56] Finally, patients with ABPA have HLA haplotypes which promote exaggerated CD4+ Th2 responses and continued synthesis of IgE. HLA-DR2 and HLA-DR5 restriction in patients with ABPA has been reported by Chauhan et al.[57] More specifically, studies have shown that HLA-DRB1*1501 and HLA-DRB1*1503 confer the highest risk of developing ABPA.[58] Conversely, HLA-DQ2 (HLA-DQB1*0201 in particular) provides relative protection against the development of ABPA.[59]
Clinical Features
Patients with ABPA classically present with wheezing and often have evidence of bronchospasm and airway hyperresponsiveness in the preceding 6 months. Some patients may complain of coughing up mucus plugs or sputum containing brown, black, or green specks.[60] In patients with CF, ABPA often presents with worsening pulmonary function and evidence of new infiltrates on chest radiographs or computed tomography (CT). Sputum smear showing A. fumigatus hyphae or sputum culture growing A. fumigatus are nonspecific findings and may be seen in CF patients with or without ABPA.[61] Laboratory findings suggestive of ABPA include peripheral eosinophilia and markedly elevated total serum IgE levels. Skin prick testing to A. fumigatus antigens is positive in all patients with ABPA, though it is nonspecific and is detectable in nearly 20%–25% of patients with persistent asthma.[62] Serum precipitins to A. fumigatus are also detectable, and serum levels of A. fumigatus-specific IgE and IgG antibodies are elevated.[63] Patients with long-standing ABPA have evidence of central bronchiectasis (typically within the central two-thirds of lung parenchyma) on CT scans. On plain chest radiographs, patients may have evidence of fleeting opacities or infiltrates. Other signs described in the literature include ring sign (circumferential bronchial wall thickening), tram-track appearance (nontapering, dilated bronchi appearing as parallel lines), and/or finger-in-glove sign (mucus plugging within dilated bronchi).[64] While many radiologic findings seen in ABPA can be caused by CF itself, there are some features that are relatively specific for ABPA. These features include central varicose or cystic bronchiectasis, infiltrates that completely resolve with steroid treatment, and high-attenuation mucus plugs.[65]
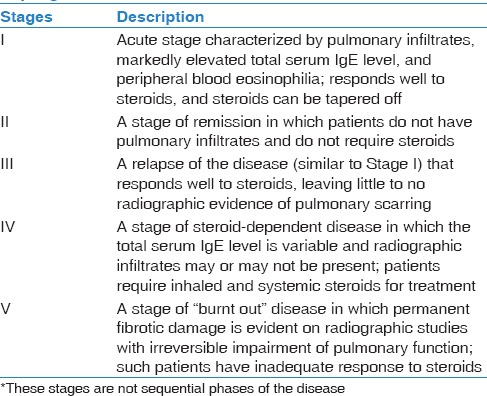
A staging system of ABPA has been published in the literature, although it was originally formulated for patients with asthma and ABPA.[66] The stages in this system are not arranged in a chronologic order and patients do not sequentially pass from one stage to the next. This five-staging system for ABPA is summarized in Table 1 (adapted from Stevens et al.[10]).
Table 1.
Stages of allergic bronchopulmonary aspergillosis*
Diagnosis
Traditionally, diagnosis of a classic case of ABPA has been based on the following essential criteria: (1) Asthma or airflow obstruction; (2) positive skin reactivity to A. fumigatus; (3) serum total IgE level > 1000 ng/mL; (4) elevated serum A. fumigatus-specific IgE and IgG; and (5) central bronchiectasis.[67] However, these criteria have been formulated and used extensively in patients with ABPA and asthma. Patients with CF have pulmonary function abnormalities at baseline and develop recurrent pulmonary exacerbations due to a wide variety of causes. Diagnosis of ABPA in such patients is challenging and the need for having distinct diagnostic criteria has been long recognized. Consequently, the CFF consensus criteria for the diagnosis of ABPA in patients with CF were formulated and published in 2003 [Table 2].[10]
Table 2.
Cystic Fibrosis Foundation – Consensus Conference criteria for diagnosis of allergic bronchopulmonary aspergillosis in patients with cystic fibrosis
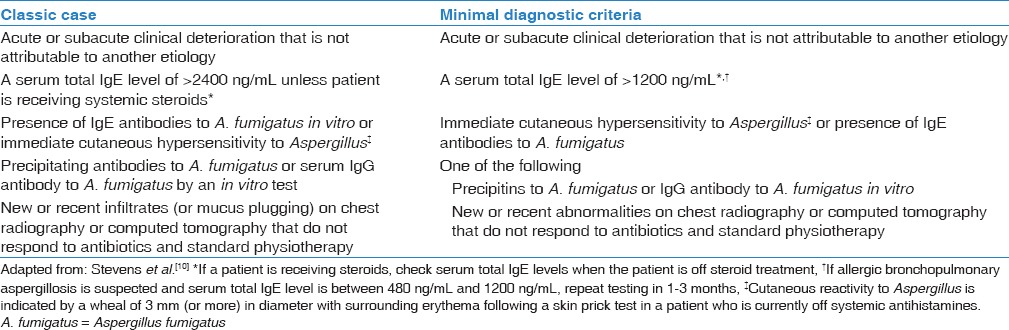
As per the CFF consensus criteria, minimal diagnostic criteria for ABPA in CF patients require evidence of acute or subacute clinical deterioration not attributable to another etiology, total serum IgE level >1200 ng/mL while off steroids, immediate cutaneous reactivity to A. fumigatus antigens or demonstration of A. fumigatus-specific IgE antibodies in vitro, and one of the following: (1) Serum precipitins to A. fumigatus; (2) demonstration of A. fumigatus-specific IgG antibodies in vitro; or (3) new or recent abnormalities on pulmonary radiologic imaging, which do not respond to antibiotics and chest physiotherapy. Moreover, patients who have a high suspicion of ABPA, but in whom the total serum IgE level is 200–500 ng/mL, the total serum IgE level should be repeated in 1–3 months.
Management
The goal of management in patients with CF and ABPA is to prevent the development of lung fibrosis and retard decline in pulmonary function.[68] Treatment of ABPA involves addressing two different aspects of the disease: (a) Attenuating the immunologic response and inflammation; and (b) reducing the burden of A. fumigatus allergens present in the airways. The former can be achieved through the use of anti-inflammatory and immunomodulatory drugs, while the latter is accomplished by employing antifungal therapy.
Treatment guidelines for the management of ABPA in CF have been based heavily on expert opinion and observational data.[10] Systemic corticosteroids and itraconazole have been considered the mainstay of therapy for ABPA.[69] Adjunctive measures, such as the use of inhaled corticosteroids, bronchodilators, anti-LTB drugs, and environmental manipulation, are also frequently employed.[70] More recently, small-scale studies have shown that omalizumab may be an effective treatment for patients with ABPA.[71]
Systemic corticosteroids are considered the first-line therapy for patients with CF and ABPA.[10] Prednisolone at a dose of 0.5–2.0 mg/kg/day (or an equivalent steroid) should be employed as an initial therapy in all patients. After a period of 1–2 weeks, dosage should be modified to prednisolone 0.5–2.0 mg/kg every other day. Subsequently, the dose of corticosteroids should be reduced slowly based on the patient's clinical response. In general, corticosteroids should be tapered off over a period of 2–3 months. Some patients may relapse during the corticosteroid taper; in such cases, increasing the dose of corticosteroids and addition of itraconazole is usually useful.[70] Once patients demonstrate signs of clinical improvement, corticosteroids should be tapered off.
Corticosteroids are useful in ABPA owing to their anti-inflammatory and immunosuppressive effects. Corticosteroids reduce the expression of phospholipase A2, pro-inflammatory cytokines, and other inflammatory mediators through their interaction with glucocorticoid response elements.[72] Furthermore, corticosteroids also reduce the serum IgE level by downregulating immunoglobulin production, increasing the apoptosis of B-lymphocytes, and reducing the expression of integrins and other adhesion molecules.[73]
Itraconazole is an azole antifungal drug that should be used in patients with ABPA who: (a) Respond poorly to corticosteroids; (b) relapse during tapering of corticosteroids; (c) develop corticosteroid toxicity; or (d) become corticosteroid dependent.[10,70] Since corticosteroids do not possess antifungal properties, therapy with corticosteroids alone does not affect the burden of A. fumigatus present in the airways. Itraconazole, being an azole antifungal drug, inhibits fungal 14α-demethylase enzyme leading to depletion of ergosterol, accumulation of sterol precursors, and alteration in the structure of the fungal plasmalemma.[74] As itraconazole possesses antifungal properties, it inhibits the growth of Aspergillus species and reduces the overall allergen burden. This in turn helps attenuate the overall inflammatory response in patients with ABPA. However, itraconazole does not possess any anti-inflammatory or immunomodulatory property of itself.[75] Therefore, it should not be used as the first-line therapy and should only be instituted in conjunction with corticosteroids. The usual dose of itraconazole is 5 mg/kg/day which may be administered in one or two divided doses. In general, a 3–6 month course of itraconazole therapy is sufficient. Liver function tests should be obtained at baseline, 1 month, and for every 3 months thereafter, or if there is a suspicion of liver dysfunction.[76] Routine monitoring of itraconazole levels is not recommended, but testing for itraconazole level should be considered for patients who respond poorly to itraconazole and those in whom there is a suspicion of inadequate absorption or noncompliance.[10] In some patients with CF who do not achieve adequate serum itraconazole levels, especially those with severe pancreatic insufficiency, use of a cyclodextrin-based liquid formulation (if available) or higher dosage itraconazole capsules may be useful.[77] Following the completion of itraconazole therapy, it is necessary to keep patients in regular follow-up to assess whether itraconazole therapy actually reduced the frequency of ABPA relapses.
Other adjunctive measures are also employed frequently in the management of patients with CF and ABPA. Use of inhaled bronchodilators and inhaled steroids may be reasonable in such patients as they ameliorate bronchospasm and modulate the local inflammatory response.[78] Manipulation of patients' environment to reduce the burden of A. fumigatus spores may be also tried.[79] While such a prophylactic maneuver seems intuitive, it has not been proven to reduce the frequency of relapses.
The management of patients with CF and ABPA is sometimes confounded by the fact that several clinical features of ABPA overlap with those of CF exacerbation due to bacterial infection, asthma, or a variety of other causes.[80] Due to this reason, the decision to treat a CF patient for ABPA may be uncertain in some clinical situations. As per the CFF consensus conference guidelines, patients with a definitive diagnosis of ABPA should receive treatment for ABPA. Likewise, patients who have only serologic evidence of AS with stable pulmonary function and no new clinical features should not be treated for ABPA. However, in cases where patients have evidence of AS and worsening pulmonary function, with or without radiographic infiltrates, a trial of treatment for CF-related pulmonary infection should be given first. In patients who do not respond to therapy and have evidence of AS, treatment for ABPA and/or asthma exacerbation should be instituted. Most patients who develop pulmonary decompensation with new radiographic infiltrates, serum IgE level between 500–1000 IU/mL, history of AS, and no response to therapy for CF exacerbation have ABPA and respond well to treatment for ABPA.[10]
Recent studies have explored the use of other antifungal agents in the treatment of ABPA with encouraging results. In a retrospective study, Hilliard et al. reported the use of voriconazole monotherapy in 13 patients with ABPA.[81] Voriconazole therapy afforded a significant improvement in pulmonary function tests and serologic tests. In another retrospective study, Chishimba et al. reported the efficacy of voriconazole and posaconazole in twenty patients with asthma and ABPA.[82] Both drugs were found to produce a significant improvement in radiologic and serologic parameters. Based on its theoretical efficacy, nebulized amphotericin B has been used to successfully treat ABPA in a 14-year-old CF patient awaiting lung transplantation.[83] In a small case series from Belgium, Proesmans et al. reported the efficacy of nebulized amphotericin B in treating 7 patients with ABPA (2 of whom had ABPA associated with CF).[84] While these reports are encouraging, further prospective, controlled studies are needed to better establish the efficacy and safety of these agents for the treatment of ABPA in patients with CF.
Omalizumab, a humanized anti-IgE monoclonal antibody, has recently received much attention as a potentially useful steroid-sparing agent. Several observational studies have reported the efficacy of omalizumab in reducing the need for steroids and overall exacerbation rates in patients with ABPA.[85,86,87,88] Tillie-Leblond et al. reported the use of omalizumab in 16 adult patients with asthma and ABPA.[89] Omalizumab significantly reduced the need for steroids and the overall number of exacerbations in this study. In another study by Emiralioglu et al., the use of omalizumab in six patients with CF and ABPA reduced the total serum IgE levels, improved respiratory symptoms, and decreased the need for steroids.[90] A small randomized, double-blinded, placebo-controlled trial (with a cross-over design) of omalizumab in adult patients with asthma and ABPA was published in 2015. This trial showed that omalizumab successfully reduced the frequency of exacerbations and decreased surface-bound IgE and FcεR1 (high-affinity receptor for crystallizable fragment [Fc] region of IgE) levels.[91] However, a large multicenter, double-blinded, placebo-controlled trial (www.clinicaltrials.gov identifier number NCT00787917) of omalizumab in CF patients with ABPA was terminated prematurely by Novartis® pharmaceuticals due to poor enrollment and retention of patients. Consequently, a recent Cochrane SR concluded that the use of omalizumab in CF patients with ABPA cannot be unequivocally recommended given the absence of validated data from randomized controlled trials.[92]
Natural Course and Outcome
In patients with CF, development of ABPA has been associated with a progressive decline in pulmonary function. In a prospective study of 122 children with CF, Kraemer et al. assessed the effect of ABPA on pulmonary function.[93] They reported that development of ABPA in patients with CF was associated with a rapid decline in all parameters of pulmonary function including forced expiratory indices (forced expiratory volume in 1 s [FEV1] and forced expiratory flow at 50% vital capacity). Moreover, decline in pulmonary function was worst among CF patients with ABPA when compared to CF patients free from Pseudomonas aeruginosa, CF patients infected with Pseudomonas aeruginosa, and CF patients with atopy but no evidence of ABPA. In an epidemiologic study based on data from the ERCF, Mastella et al. found that the presence of ABPA in CF patients was associated with a lower FEV1 at all ages.[29] Interestingly, in a retrospective cohort study, Amin et al. showed that colonization of CF patients with A. fumigatus (in the absence of ABPA) is an independent risk factor for hospitalization.[95] However, unlike ABPA, chronic infection with A. fumigatus does not adversely affect pulmonary function by itself.[11]
Future Directions
Guidelines for the management of ABPA hitherto have been mostly based on observational, low-quality evidence, and there is a general dearth of well-designed controlled trials to guide the management of ABPA in patients with CF.[10,80] Fortunately, a number of trials are currently ongoing to address key questions in the management of ABPA.[11] One randomized trial is comparing the efficacy of oral glucocorticoids to oral itraconazole monotherapy (NCT01321827), another comparing oral glucocorticoids to oral voriconazole (NCT01621321), and a third one comparing oral glucocorticoids to combined oral glucocorticoid–itraconazole therapy (NCT0244009). Moreover, as steroid therapy is often complicated by systemic toxicity,[96] alternative treatment options for ABPA are being actively explored.[11] Omalizumab appears to be an effective steroid-sparing drug that reduces the frequency of relapse and exacerbations in patients with ABPA.[85,86,87,88,89] More evidence from larger randomized clinical trials will further substantiate its role in the management of ABPA.[92] Some other studies are currently underway to evaluate the efficacy of amphotericin B for the management of ABPA. One randomized controlled trial is exploring the role of nebulized liposomal amphotericin B in maintaining remission in patients with asthma and ABPA (NCT00787917). Another randomized trial aims to compare inhaled glucocorticoid monotherapy to nebulized amphotericin B deoxycholate combined with inhaled glucocorticoids in reducing the frequency of exacerbations (NCT01857479). The results of these clinical trials will provide an evidence base to rationalize the management of ABPA over the next decade.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Strausbaugh SD, Davis PB. Cystic fibrosis: A review of epidemiology and pathobiology. Clin Chest Med. 2007;28:279–88. doi: 10.1016/j.ccm.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Mornon JP, Lehn P, Callebaut I. Molecular models of the open and closed states of the whole human CFTR protein. Cell Mol Life Sci. 2009;66:3469–86. doi: 10.1007/s00018-009-0133-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riordan JR. The cystic fibrosis transmembrane conductance regulator. Annu Rev Physiol. 1993;55:609–30. doi: 10.1146/annurev.ph.55.030193.003141. [DOI] [PubMed] [Google Scholar]
- 4.Sheppard MN, Nicholson AG. The pathology of cystic fibrosis. Curr Diagn Pathol. 2002;8:50–9. [Google Scholar]
- 5.Bains SN, Judson MA. Allergic bronchopulmonary aspergillosis. Clin Chest Med. 2012;33:265–81. doi: 10.1016/j.ccm.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Tunnicliffe G, Schomberg L, Walsh S, Tinwell B, Harrison T, Chua F. Airway and parenchymal manifestations of pulmonary aspergillosis. Respir Med. 2013;107:1113–23. doi: 10.1016/j.rmed.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 7.Knutsen AP, Slavin RG. Allergic bronchopulmonary aspergillosis in asthma and cystic fibrosis. Clin Dev Immunol. 2011;2011:843763. doi: 10.1155/2011/843763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Almeida MB, Bussamra MH, Rodrigues JC. Allergic bronchopulmonary aspergillosis in paediatric cystic fibrosis patients. Paediatr Respir Rev. 2006;7:67–72. doi: 10.1016/j.prrv.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Chakrabarti A, Sethi S, Raman DS, Behera D. Eight-year study of allergic bronchopulmonary aspergillosis in an Indian teaching hospital. Mycoses. 2002;45:295–9. doi: 10.1046/j.1439-0507.2002.00738.x. [DOI] [PubMed] [Google Scholar]
- 10.Stevens DA, Moss RB, Kurup VP, Knutsen AP, Greenberger P, Judson MA, et al. Allergic bronchopulmonary aspergillosis in cystic fibrosis – State of the art: Cystic Fibrosis Foundation consensus conference. Clin Infect Dis. 2003;37(Suppl 3):S225–64. doi: 10.1086/376525. [DOI] [PubMed] [Google Scholar]
- 11.Moss RB. Treating allergic bronchopulmonary aspergillosis: The way forward. Eur Respir J. 2016;47:385–7. doi: 10.1183/13993003.01816-2015. [DOI] [PubMed] [Google Scholar]
- 12.Sudfeld CR, Dasenbrook EC, Merz WG, Carroll KC, Boyle MP. Prevalence and risk factors for recovery of filamentous fungi in individuals with cystic fibrosis. J Cyst Fibros. 2010;9:110–6. doi: 10.1016/j.jcf.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeaske R, Bruns WT, Fink JN, Greenberger PA, Colby H, Liotta JL, et al. Immune responses to Aspergillus in cystic fibrosis. J Allergy Clin Immunol. 1988;82:73–7. doi: 10.1016/0091-6749(88)90054-1. [DOI] [PubMed] [Google Scholar]
- 14.Nicolai T, Arleth S, Spaeth A, Bertele-Harms RM, Harms HK. Correlation of IgE antibody titer to Aspergillus fumigatus with decreased lung function in cystic fibrosis. Pediatr Pulmonol. 1990;8:12–5. doi: 10.1002/ppul.1950080106. [DOI] [PubMed] [Google Scholar]
- 15.Hutcheson PS, Rejent AJ, Slavin RG. Variability in parameters of allergic bronchopulmonary aspergillosis in patients with cystic fibrosis. J Allergy Clin Immunol. 1991;88(3 Pt 1):390–4. doi: 10.1016/0091-6749(91)90102-t. [DOI] [PubMed] [Google Scholar]
- 16.el-Dahr JM, Fink R, Selden R, Arruda LK, Platts-Mills TA, Heymann PW. Development of immune responses to Aspergillus at an early age in children with cystic fibrosis. Am J Respir Crit Care Med. 1994;150(6 Pt 1):1513–8. doi: 10.1164/ajrccm.150.6.7952609. [DOI] [PubMed] [Google Scholar]
- 17.Hutcheson PS, Knutsen AP, Rejent AJ, Slavin RG. A 12-year longitudinal study of Aspergillus sensitivity in patients with cystic fibrosis. Chest. 1996;110:363–6. doi: 10.1378/chest.110.2.363. [DOI] [PubMed] [Google Scholar]
- 18.Wojnarowski C, Eichler I, Gartner C, Götz M, Renner S, Koller DY, et al. Sensitization to Aspergillus fumigatus and lung function in children with cystic fibrosis. Am J Respir Crit Care Med. 1997;155:1902–7. doi: 10.1164/ajrccm.155.6.9196093. [DOI] [PubMed] [Google Scholar]
- 19.Maturu VN, Agarwal R. Prevalence of Aspergillus sensitization and allergic bronchopulmonary aspergillosis in cystic fibrosis: Systematic review and meta-analysis. Clin Exp Allergy. 2015;45:1765–78. doi: 10.1111/cea.12595. [DOI] [PubMed] [Google Scholar]
- 20.Torres-Lozano C, Núñez-Núñez ME, Pedroza-Meléndez A, Lezana FJ, Huerta-López JG. Respiratory allergy in Mexican patients with cystic fibrosis. Allergol Immunopathol (Madr) 1999;27:294–7. [PubMed] [Google Scholar]
- 21.Henry M, Bennett DM, Kiely J, Kelleher N, Bredin CP. Fungal atopy in adult cystic fibrosis. Respir Med. 2000;94:1092–6. doi: 10.1053/rmed.2000.0918. [DOI] [PubMed] [Google Scholar]
- 22.Máiz L, Cuevas M, Quirce S, Cañón JF, Pacheco A, Sousa A, et al. Serologic IgE immune responses against Aspergillus fumigatus and Candida albicans in patients with cystic fibrosis. Chest. 2002;121:782–8. doi: 10.1378/chest.121.3.782. [DOI] [PubMed] [Google Scholar]
- 23.Skov M, McKay K, Koch C, Cooper PJ. Prevalence of allergic bronchopulmonary aspergillosis in cystic fibrosis in an area with a high frequency of atopy. Respir Med. 2005;99:887–93. doi: 10.1016/j.rmed.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 24.Baxter CG, Dunn G, Jones AM, Webb K, Gore R, Richardson MD, et al. Novel immunologic classification of aspergillosis in adult cystic fibrosis. J Allergy Clin Immunol. 2013;132:560–6. doi: 10.1016/j.jaci.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 25.Baxter CG, Moore CB, Jones AM, Webb AK, Denning DW. IgE-mediated immune responses and airway detection of Aspergillus and Candida in adult cystic fibrosis. Chest. 2013;143:1351–7. doi: 10.1378/chest.12-1363. [DOI] [PubMed] [Google Scholar]
- 26.Geller DE, Kaplowitz H, Light MJ, Colin AA. Allergic bronchopulmonary aspergillosis in cystic fibrosis: Reported prevalence, regional distribution, and patient characteristics. Scientific Advisory Group, Investigators, and Coordinators of the Epidemiologic Study of Cystic Fibrosis. Chest. 1999;116:639–46. doi: 10.1378/chest.116.3.639. [DOI] [PubMed] [Google Scholar]
- 27.Chotirmall SH, Branagan P, Gunaratnam C, McElvaney NG. Aspergillus/allergic bronchopulmonary aspergillosis in an Irish cystic fibrosis population: A diagnostically challenging entity. Respir Care. 2008;53:1035–41. [PubMed] [Google Scholar]
- 28.Jubin V, Ranque S, Stremler Le Bel N, Sarles J, Dubus JC. Risk factors for Aspergillus colonization and allergic bronchopulmonary aspergillosis in children with cystic fibrosis. Pediatr Pulmonol. 2010;45:764–71. doi: 10.1002/ppul.21240. [DOI] [PubMed] [Google Scholar]
- 29.Mastella G, Rainisio M, Harms HK, Hodson ME, Koch C, Navarro J, et al. Allergic bronchopulmonary aspergillosis in cystic fibrosis. A European epidemiological study. Epidemiologic Registry of Cystic Fibrosis. Eur Respir J. 2000;16:464–71. doi: 10.1034/j.1399-3003.2000.016003464.x. [DOI] [PubMed] [Google Scholar]
- 30.Fillaux J, Brémont F, Murris M, Cassaing S, Rittié JL, Tétu L, et al. Assessment of Aspergillus sensitization or persistent carriage as a factor in lung function impairment in cystic fibrosis patients. Scand J Infect Dis. 2012;44:842–7. doi: 10.3109/00365548.2012.695454. [DOI] [PubMed] [Google Scholar]
- 31.Fillaux J, Brémont F, Murris M, Cassaing S, Tétu L, Segonds C, et al. Aspergillus sensitization or carriage in cystic fibrosis patients. Pediatr Infect Dis J. 2014;33:680–6. doi: 10.1097/INF.0000000000000231. [DOI] [PubMed] [Google Scholar]
- 32.Menzies D, Holmes L, McCumesky G, Prys-Picard C, Niven R. Aspergillus sensitization is associated with airflow limitation and bronchiectasis in severe asthma. Allergy. 2011;66:679–85. doi: 10.1111/j.1398-9995.2010.02542.x. [DOI] [PubMed] [Google Scholar]
- 33.Latgé JP. Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev. 1999;12:310–50. doi: 10.1128/cmr.12.2.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sarma PU, Banerjee B, Bir N, Kurup VP. Immunodiagnosis of allergic bronchopulmonary aspergillosis. Immunol Allergy Clin North Am. 1998;18:525–47. [Google Scholar]
- 35.Laham MN, Carpenter JL. Aspergillus terreus, a pathogen capable of causing infective endocarditis, pulmonary mycetoma, and allergic bronchopulmonary aspergillosis. Am Rev Respir Dis. 1982;125:769–72. doi: 10.1164/arrd.1982.125.6.769. [DOI] [PubMed] [Google Scholar]
- 36.Latgé JP. The pathobiology of Aspergillus fumigatus. Trends Microbiol. 2001;9:382–9. doi: 10.1016/s0966-842x(01)02104-7. [DOI] [PubMed] [Google Scholar]
- 37.Hohl TM, Feldmesser M. Aspergillus fumigatus: Principles of pathogenesis and host defense. Eukaryot Cell. 2007;6:1953–63. doi: 10.1128/EC.00274-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tomee JF, Kauffman HF. Putative virulence factors of Aspergillus fumigatus. Clin Exp Allergy. 2000;30:476–84. doi: 10.1046/j.1365-2222.2000.00796.x. [DOI] [PubMed] [Google Scholar]
- 39.Banerjee B, Greenberger PA, Fink JN, Kurup VP. Immunological characterization of Asp f 2, a major allergen from Aspergillus fumigatus associated with allergic bronchopulmonary aspergillosis. Infect Immun. 1998;66:5175–82. doi: 10.1128/iai.66.11.5175-5182.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chotirmall SH, McElvaney NG. Fungi in the cystic fibrosis lung: Bystanders or pathogens? Int J Biochem Cell Biol. 2014;52:161–73. doi: 10.1016/j.biocel.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 41.Chotirmall SH, Al-Alawi M, Mirkovic B, Lavelle G, Logan PM, Greene CM, et al. Aspergillus-associated airway disease, inflammation, and the innate immune response. Biomed Res Int. 2013;2013:723129. doi: 10.1155/2013/723129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muro M, Mondejar-López P, Moya-Quiles MR, Salgado G, Pastor-Vivero MD, Lopez-Hernandez R, et al. HLA-DRB1 and HLA-DQB1 genes on susceptibility to and protection from allergic bronchopulmonary aspergillosis in patients with cystic fibrosis. Microbiol Immunol. 2013;57:193–7. doi: 10.1111/1348-0421.12020. [DOI] [PubMed] [Google Scholar]
- 43.Knutsen AP, Mueller KR, Levine AD, Chouhan B, Hutcheson PS, Slavin RG. Asp f I CD4+ TH2-like T-cell lines in allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 1994;94(2 Pt 1):215–21. doi: 10.1016/0091-6749(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 44.Knutsen AP, Mueller KR, Hutcheson PS, Slavin RG. T- and B-cell dysregulation of IgE synthesis in cystic fibrosis patients with allergic bronchopulmonary aspergillosis. Clin Immunol Immunopathol. 1990;55:129–38. doi: 10.1016/0090-1229(90)90074-z. [DOI] [PubMed] [Google Scholar]
- 45.Hershey GK, Friedrich MF, Esswein LA, Thomas ML, Chatila TA. The association of atopy with a gain-of-function mutation in the alpha subunit of the interleukin-4 receptor. N Engl J Med. 1997;337:1720–5. doi: 10.1056/NEJM199712113372403. [DOI] [PubMed] [Google Scholar]
- 46.Kurup VP, Mauze S, Choi H, Seymour BW, Coffman RL. A murine model of allergic bronchopulmonary aspergillosis with elevated eosinophils and IgE. J Immunol. 1992;148:3783–8. [PubMed] [Google Scholar]
- 47.Tomee JF, Wierenga AT, Hiemstra PS, Kauffman HK. Proteases from Aspergillus fumigatus induce release of proinflammatory cytokines and cell detachment in airway epithelial cell lines. J Infect Dis. 1997;176:300–3. doi: 10.1086/517272. [DOI] [PubMed] [Google Scholar]
- 48.Kauffman HF. Immunopathogenesis of allergic bronchopulmonary aspergillosis and airway remodeling. Front Biosci. 2003;8:e190–6. doi: 10.2741/990. [DOI] [PubMed] [Google Scholar]
- 49.Ladarola P, Lungarella G, Martorana PA, Viglio S, Guglielminetti M, Korzus E, et al. Lung injury and degradation of extracellular matrix components by Aspergillus fumigatus serine proteinase. Exp Lung Res. 1998;24:233–51. doi: 10.3109/01902149809041532. [DOI] [PubMed] [Google Scholar]
- 50.Hogaboam CM, Blease K, Mehrad B, Steinhauser ML, Standiford TJ, Kunkel SL, et al. Chronic airway hyperreactivity, goblet cell hyperplasia, and peribronchial fibrosis during allergic airway disease induced by Aspergillus fumigatus. Am J Pathol. 2000;156:723–32. doi: 10.1016/S0002-9440(10)64775-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Becker JW, Burke W, McDonald G, Greenberger PA, Henderson WR, Aitken ML. Prevalence of allergic bronchopulmonary aspergillosis and atopy in adult patients with cystic fibrosis. Chest. 1996;109:1536–40. doi: 10.1378/chest.109.6.1536. [DOI] [PubMed] [Google Scholar]
- 52.Crameri R, Hemmann S, Ismail C, Menz G, Blaser K. Disease-specific recombinant allergens for the diagnosis of allergic bronchopulmonary aspergillosis. Int Immunol. 1998;10:1211–6. doi: 10.1093/intimm/10.8.1211. [DOI] [PubMed] [Google Scholar]
- 53.Hemmann S, Nikolaizik WH, Schöni MH, Blaser K, Crameri R. Differential IgE recognition of recombinant Aspergillus fumigatus allergens by cystic fibrosis patients with allergic bronchopulmonary aspergillosis or Aspergillus allergy. Eur J Immunol. 1998;28:1155–60. doi: 10.1002/(SICI)1521-4141(199804)28:04<1155::AID-IMMU1155>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 54.Hemmann S, Ismail C, Blaser K, Menz G, Crameri R. Skin-test reactivity and isotype-specific immune responses to recombinant Asp f 3, a major allergen of Aspergillus fumigatus. Clin Exp Allergy. 1998;28:860–7. doi: 10.1046/j.1365-2222.1998.00329.x. [DOI] [PubMed] [Google Scholar]
- 55.Banerjee B, Kurup VP, Greenberger PA, Hoffman DR, Nair DS, Fink JN. Purification of a major allergen, Asp f 2 binding to IgE in allergic bronchopulmonary aspergillosis, from culture filtrate of Aspergillus fumigatus. J Allergy Clin Immunol. 1997;99(6 Pt 1):821–7. doi: 10.1016/s0091-6749(97)80017-6. [DOI] [PubMed] [Google Scholar]
- 56.Ober C, Leavitt SA, Tsalenko A, Howard TD, Hoki DM, Daniel R, et al. Variation in the interleukin 4-receptor alpha gene confers susceptibility to asthma and atopy in ethnically diverse populations. Am J Hum Genet. 2000;66:517–26. doi: 10.1086/302781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chauhan B, Santiago L, Hutcheson PS, Schwartz HJ, Spitznagel E, Castro M, et al. Evidence for the involvement of two different MHC class II regions in susceptibility or protection in allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 2000;106:723–9. doi: 10.1067/mai.2000.109913. [DOI] [PubMed] [Google Scholar]
- 58.Chauhan B, Knutsen Ap, Hutcheson PS, Slavin RG, Bellone CJ. T cell subsets, epitope mapping, and HLA-restriction in patients with allergic bronchopulmonary aspergillosis. J Clin Invest. 1996;97:2324–31. doi: 10.1172/JCI118675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chauhan B, Santiago L, Kirschmann DA, Hauptfeld V, Knutsen AP, Hutcheson PS, et al. The association of HLA-DR alleles and T cell activation with allergic bronchopulmonary aspergillosis. J Immunol. 1997;159:4072–6. [PubMed] [Google Scholar]
- 60.Agarwal R. Allergic bronchopulmonary aspergillosis. Chest. 2009;135:805–26. doi: 10.1378/chest.08-2586. [DOI] [PubMed] [Google Scholar]
- 61.Bakare N, Rickerts V, Bargon J, Just-Nübling G. Prevalence of Aspergillus fumigatus and other fungal species in the sputum of adult patients with cystic fibrosis. Mycoses. 2003;46:19–23. doi: 10.1046/j.1439-0507.2003.00830.x. [DOI] [PubMed] [Google Scholar]
- 62.Nikolaizik WH, Weichel M, Blaser K, Crameri R. Intracutaneous tests with recombinant allergens in cystic fibrosis patients with allergic bronchopulmonary aspergillosis and Aspergillus allergy. Am J Respir Crit Care Med. 2002;165:916–21. doi: 10.1164/ajrccm.165.7.2109008. [DOI] [PubMed] [Google Scholar]
- 63.Nikolaizik WH, Moser M, Crameri R, Little S, Warner JO, Blaser K, et al. Identification of allergic bronchopulmonary aspergillosis in cystic fibrosis patients by recombinant Aspergillus fumigatus I/a-specific serology. Am J Respir Crit Care Med. 1995;152:634–9. doi: 10.1164/ajrccm.152.2.7633719. [DOI] [PubMed] [Google Scholar]
- 64.Mintzer RA, Rogers LF, Kruglik GD, Rosenberg M, Neiman HL, Patterson R. The spectrum of radiologic findings in allergic bronchopulmonary aspergillosis. Radiology. 1978;127:301–7. doi: 10.1148/127.2.301. [DOI] [PubMed] [Google Scholar]
- 65.Logan PM, Müller NL. High-attenuation mucous plugging in allergic bronchopulmonary aspergillosis. Can Assoc Radiol J. 1996;47:374–7. [PubMed] [Google Scholar]
- 66.Patterson R, Greenberger PA, Radin RC, Roberts M. Allergic bronchopulmonary aspergillosis: Staging as an aid to management. Ann Intern Med. 1982;96:286–91. doi: 10.7326/0003-4819-96-3-286. [DOI] [PubMed] [Google Scholar]
- 67.Greenberger PA, Patterson R. Diagnosis and management of allergic bronchopulmonary aspergillosis. Ann Allergy. 1986;56:444–8. [PubMed] [Google Scholar]
- 68.Wark PA, Gibson PG. Allergic bronchopulmonary aspergillosis: New concepts of pathogenesis and treatment. Respirology. 2001;6:1–7. doi: 10.1046/j.1440-1843.2001.00289.x. [DOI] [PubMed] [Google Scholar]
- 69.Leon EE, Craig TJ. Antifungals in the treatment of allergic bronchopulmonary aspergillosis. Ann Allergy Asthma Immunol. 1999;82:511–6. doi: 10.1016/S1081-1206(10)63157-2. [DOI] [PubMed] [Google Scholar]
- 70.Mahdavinia M, Grammer LC. Management of allergic bronchopulmonary aspergillosis: A review and update. Ther Adv Respir Dis. 2012;6:173–87. doi: 10.1177/1753465812443094. [DOI] [PubMed] [Google Scholar]
- 71.Kanu A, Patel K. Treatment of allergic bronchopulmonary aspergillosis (ABPA) in CF with anti-IgE antibody (omalizumab) Pediatr Pulmonol. 2008;43:1249–51. doi: 10.1002/ppul.20907. [DOI] [PubMed] [Google Scholar]
- 72.Kaliner M. Mechanisms of glucocorticosteroid action in bronchial asthma. J Allergy Clin Immunol. 1985;76(2 Pt 2):321–9. doi: 10.1016/0091-6749(85)90648-7. [DOI] [PubMed] [Google Scholar]
- 73.Rosenberg M, Patterson R, Roberts M, Wang J. The assessment of immunologic and clinical changes occurring during corticosteroid therapy for allergic bronchopulmonary aspergillosis. Am J Med. 1978;64:599–606. doi: 10.1016/0002-9343(78)90579-x. [DOI] [PubMed] [Google Scholar]
- 74.Salez F, Brichet A, Desurmont S, Grosbois JM, Wallaert B, Tonnel AB. Effects of itraconazole therapy in allergic bronchopulmonary aspergillosis. Chest. 1999;116:1665–8. doi: 10.1378/chest.116.6.1665. [DOI] [PubMed] [Google Scholar]
- 75.Wark PA, Hensley MJ, Saltos N, Boyle MJ, Toneguzzi RC, Epid GD, et al. Anti-inflammatory effect of itraconazole in stable allergic bronchopulmonary aspergillosis: A randomized controlled trial. J Allergy Clin Immunol. 2003;111:952–7. doi: 10.1067/mai.2003.1388. [DOI] [PubMed] [Google Scholar]
- 76.Conway SP, Etherington C, Peckham DG, Brownlee KG, Whitehead A, Cunliffe H. Pharmacokinetics and safety of itraconazole in patients with cystic fibrosis. J Antimicrob Chemother. 2004;53:841–7. doi: 10.1093/jac/dkh175. [DOI] [PubMed] [Google Scholar]
- 77.Lestner J, Hope WW. Itraconazole: An update on pharmacology and clinical use for treatment of invasive and allergic fungal infections. Expert Opin Drug Metab Toxicol. 2013;9:911–26. doi: 10.1517/17425255.2013.794785. [DOI] [PubMed] [Google Scholar]
- 78.Imbeault B, Cormier Y. Usefulness of inhaled high-dose corticosteroids in allergic bronchopulmonary aspergillosis. Chest. 1993;103:1614–7. doi: 10.1378/chest.103.5.1614. [DOI] [PubMed] [Google Scholar]
- 79.Vernon DR, Allan F. Environmental factors in allergic bronchopulmonary aspergillosis. Clin Exp Allergy. 1980;10:217–27. doi: 10.1111/j.1365-2222.1980.tb02100.x. [DOI] [PubMed] [Google Scholar]
- 80.Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, et al. Allergic bronchopulmonary aspergillosis: Review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013;43:850–73. doi: 10.1111/cea.12141. [DOI] [PubMed] [Google Scholar]
- 81.Hilliard T, Edwards S, Buchdahl R, Francis J, Rosenthal M, Balfour-Lynn I, et al. Voriconazole therapy in children with cystic fibrosis. J Cyst Fibros. 2005;4:215–20. doi: 10.1016/j.jcf.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 82.Chishimba L, Niven RM, Cooley J, Denning DW. Voriconazole and posaconazole improve asthma severity in allergic bronchopulmonary aspergillosis and severe asthma with fungal sensitization. J Asthma. 2012;49:423–33. doi: 10.3109/02770903.2012.662568. [DOI] [PubMed] [Google Scholar]
- 83.Hayes D, Jr, Murphy BS, Lynch JE, Feola DJ. Aerosolized amphotericin for the treatment of allergic bronchopulmonary aspergillosis. Pediatr Pulmonol. 2010;45:1145–8. doi: 10.1002/ppul.21300. [DOI] [PubMed] [Google Scholar]
- 84.Proesmans M, Vermeulen F, Vreys M, De Boeck K. Use of nebulized amphotericin B in the treatment of allergic bronchopulmonary aspergillosis in cystic fibrosis. Int J Pediatr. 2010;2010:376287. doi: 10.1155/2010/376287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zirbes JM, Milla CE. Steroid-sparing effect of omalizumab for allergic bronchopulmonary aspergillosis and cystic fibrosis. Pediatr Pulmonol. 2008;43:607–10. doi: 10.1002/ppul.20804. [DOI] [PubMed] [Google Scholar]
- 86.van der Ent CK, Hoekstra H, Rijkers GT. Successful treatment of allergic bronchopulmonary aspergillosis with recombinant anti-IgE antibody. Thorax. 2007;62:276–7. doi: 10.1136/thx.2004.035519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lin RY, Sethi S, Bhargave GA. Measured immunoglobulin E in allergic bronchopulmonary aspergillosis treated with omalizumab. J Asthma. 2010;47:942–5. doi: 10.3109/02770903.2010.491144. [DOI] [PubMed] [Google Scholar]
- 88.Wong R, Wong M, Robinson PD, Fitzgerald DA. Omalizumab in the management of steroid dependent allergic bronchopulmonary aspergillosis (ABPA) complicating cystic fibrosis. Paediatr Respir Rev. 2013;14:22–4. doi: 10.1016/j.prrv.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 89.Tillie-Leblond I, Germaud P, Leroyer C, Tétu L, Girard F, Devouassoux G, et al. Allergic bronchopulmonary aspergillosis and omalizumab. Allergy. 2011;66:1254–6. doi: 10.1111/j.1398-9995.2011.02599.x. [DOI] [PubMed] [Google Scholar]
- 90.Emiralioglu N, Dogru D, Tugcu GD, Yalcin E, Kiper N, Ozcelik U. Omalizumab treatment for allergic bronchopulmonary aspergillosis in cystic fibrosis. Ann Pharmacother. 2016;50:188–93. doi: 10.1177/1060028015624204. [DOI] [PubMed] [Google Scholar]
- 91.Voskamp AL, Gillman A, Symons K, Sandrini A, Rolland JM, O'Hehir RE, et al. Clinical efficacy and immunologic effects of omalizumab in allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol Pract. 2015;3:192–9. doi: 10.1016/j.jaip.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 92.Jat KR, Walia DK, Khairwa A. Anti-IgE therapy for allergic bronchopulmonary aspergillosis in people with cystic fibrosis. Cochrane Database Syst Rev. 2015;11:CD010288. doi: 10.1002/14651858.CD010288.pub3. [DOI] [PubMed] [Google Scholar]
- 93.Kraemer R, Deloséa N, Ballinari P, Gallati S, Crameri R. Effect of allergic bronchopulmonary aspergillosis on lung function in children with cystic fibrosis. Am J Respir Crit Care Med. 2006;174:1211–20. doi: 10.1164/rccm.200603-423OC. [DOI] [PubMed] [Google Scholar]
- 94.Amin R, Dupuis A, Aaron SD, Ratjen F. The effect of chronic infection with Aspergillus fumigatus on lung function and hospitalization in patients with cystic fibrosis. Chest. 2010;137:171–6. doi: 10.1378/chest.09-1103. [DOI] [PubMed] [Google Scholar]
- 95.de Vrankrijker AM, van der Ent CK, van Berkhout FT, Stellato RK, Willems RJ, Bonten MJ, et al. Aspergillus fumigatus colonization in cystic fibrosis: Implications for lung function? Clin Microbiol Infect. 2011;17:1381–6. doi: 10.1111/j.1469-0691.2010.03429.x. [DOI] [PubMed] [Google Scholar]
- 96.Lai HC, FitzSimmons SC, Allen DB, Kosorok MR, Rosenstein BJ, Campbell PW, et al. Risk of persistent growth impairment after alternate-day prednisone treatment in children with cystic fibrosis. N Engl J Med. 2000;342:851–9. doi: 10.1056/NEJM200003233421204. [DOI] [PubMed] [Google Scholar]