Abstract
Background
Implant breakage after the fixation of traumatic fractures is rare; however, when it occurs, it is debilitating for the patients and a challenge for surgeons. The purpose of this study was to analyze and identify the independent risk factors for implant breakage of traumatic fractures treated with plate osteosynthesis.
Methods
We reviewed the medical records of patients with a fracture to any part of their four extremities, clavicle, hand or foot, who underwent surgical plate osteosynthesis from January 2005 to January 2015, and who sustained a subsequent implant breakage. Kaplan–Meier univariate and multivariate Cox regressions were performed to identify independent associations of potential risk factors for implant breakage in this cohort.
Results
We identified 168 patients who underwent plate osteosynthesis surgery and had subsequent internal fixator breakage. The mean patient age was 40.63 ± 16.71 years (range, 3 to 78 years), with 72.0% (121) males and 28.0% (47) females. The average time between surgery and implant breakage was 12.85 ± 12.42 months (range, 1 to 60 months). In the final regression model, we show that inserting screws close to the fracture line is an independent predictive risk factor for implant breakage (HR, 2.165, 95%CI, 1.227 to 3.822; P = 0.008).
Conclusions
We found that inserting screws close to the fracture line is related to an increased risk of internal fixator breakage in patients treated with plate osteosynthesis after fracture. Plates with additional holes likely lead to an increased risk of implant breakage, presumably because surgeons cannot resist inserting extra screws into the holes adjacent to the fracture line, which reduces the stiffness of the plate. We have addressed this problem by designing a plate without holes adjacent to the fracture line.
Keywords: Traumatic fracture, Plate osteosynthesis, Risk factors, Implant breakage, Internal fixation
Background
Internal fixator breakage occurs in approximately 3.5% to 13.3% of patients during internal fixation surgery follow-up [1, 2]. These complications are a challenge for even the most experienced surgeons, and can cause the patient substantial functional impairments, such as persistent and prolonged physical and psychological disabilities.
Previous studies show that risk factors for implant breakage include age, American Society of Anesthesiologists (ASA) score, fall from a height, body mass index, systemic patient comorbidities, patient postoperative noncompliance, local pathology at the fracture site, surgeons who treat a high number of patients, and surgeon technical error; this includes the use of specially designed plates rather than plates routinely used by other surgeons for treatment [3–6]. Several fixation characteristics linked with construct strength and resilience have been biomechanically evaluated and found to be related to the risk of failure, including the number of screws, the density of screws (number of screws/the number of plate holes), and the working length (plate length spanning the fracture site between two screws on each side adjacent to the fracture) [7–10]. However, there is limited data available in the literature to validate these concepts from a clinical perspective.
This study aims to investigate a large population of patients who experienced implant breakage after plate of a traumatic fracture(s) to determine the risk factors associated with this specific complication.
Methods
Data sources
We retrieved and reviewed the medical records of patients who were admitted to the Third Hospital of Hebei Medical University in China from January 2005 to January 2015. We included in the study patients who had any fracture to the four extremities, clavicle, hand or foot, who underwent treatment via closed reduction or open reduction and plate osteosynthesis, and who subsequently developed an implant breakage. We excluded patients who sustained direct trauma from the internally fixed fracture, those who experienced a pathological fracture, those with a psychiatric disorder, and those who suffered traumatic brain injury.
We recorded specific characteristics related to the: (1) patient (age, sex, residence, body mass index (BMI), osteoporosis, ASA classification, and medical comorbidities); (2) fracture (side of fractured limb, mechanism of injury, fractured site, fractured bones, fracture pattern, AO/OTA classification, seasonality, open/closed fracture, number of fractures); (3) surgery (shape and type of the used plate, number of used plates, ancillary fixation, number of ancillary K-wires, number of ancillary screws, inserting screws closely adjacent to the fracture line, number of empty screw holes adjacent to the fracture line, number of plate holes, number of plate screws, name and level of the surgeon performing the operation, open or closed reduction of the fracture, postoperative complication), and (4) implant breakage (breakage site within/outside the fracture line, screw slack off the hole, type of broken plate, and most possible underlying cause for the breakage).
All radiographs were reviewed by professors working in the Department of Orthopedic Surgery. If there were any disagreements in assessing the data, a final decision was made by discussion and consensus (Fig. 1).
Fig. 1.

The anteroposterior radiograph of proximal femur shows the plate breakage and nonunited proximal femoral shaft fracture
Statistical analysis
Statistical analyses were performed with SPSS21.0 (IBM, USA) software. A P value <0.05 was considered significant. Cox proportional-hazard regression models were used to perform survival analyses, to identify the risk factors for plate breakage, and to calculate hazard ratios (HRS). A univariate analysis was performed using Kaplan–Meier curves. Kaplan–Meier curves also provided a graphical comparison of survivorship for the procedures that were used over the period of the study, with the time of implant breakage as the end-point.
Results
Of the 201 patients identified who underwent surgery from January 2005 to January 2015, 168 patients met the inclusion criteria for the study. The mean age of the population was 40.63 ± 16.71 years (range, 3 to 78 years). Among these patients, 72% (121) were male and 28% (47) were female. The average time between internal fixation surgery and implant breakage was 12.85 ± 12.42 months (range, 1 to 60 months). Implant breakage occurred in 117 patients within less than 1 year, and this accounts for 70% of all cases (Fig. 2).
Fig. 2.
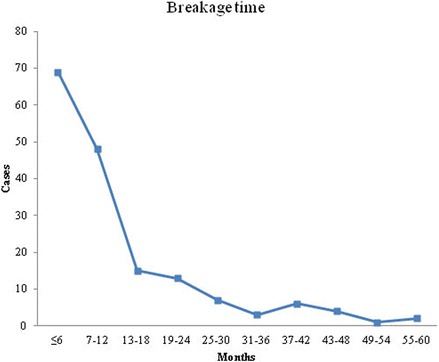
The interval between plate osteosynthesis surgery and implant breakage and the corresponding number of cases with implant breakage during the study period
The risk factors that were investigated are listed in Table 1. According to the Kaplan–Meier univariate analysis, implant breakage was associated with the weight or not weight limbs (χ 2 = 14.466, P < 0.001), the type of broken plate (χ 2 = 17.456, P < 0.001), breakage site within/outside the fracture line (χ 2 = 5.196, P cps 0.023), the number of plate holes (χ 2 = 17.119, P < 0.001), the number of plate screws (χ 2 = 6.604, P = 0.037), and inserting screws closely adjacent to the fracture line (χ 2 = 5.674, P = 0.017, Fig. 3).
Table 1.
Characteristics of Patients with Internal fixation breakage
| Issues | Interval between internal fixation and implant breakage, months (M (QR)) | n(%) | χ 2 value | P value |
|---|---|---|---|---|
| Patients characteristics | ||||
| Age (years) | 5.212 | 0.634 | ||
| 0–10 | 6.0 | 3(1.8) | ||
| 11–20 | 6.0(9.0) | 9(5.4) | ||
| 21–30 | 8.0(11.2) | 32(19.0) | ||
| 31–40 | 9.0(21.3) | 44(26.2) | ||
| 41–50 | 10.0(8.0) | 29(17.3) | ||
| 51–60 | 10.5(16.2) | 22(13.1) | ||
| 60–69 | 9.0(14.0) | 23(13.7) | ||
| 70+ | 8.5(21.2) | 6(3.6) | ||
| Gender | 0.008 | 0.927 | ||
| Male | 9.0(12.5) | 121(72.0) | ||
| Female | 9.0(14.0) | 47(28.0) | ||
| Body Mass Index (BMI kg/cm2) | 5.398 | 0.249 | ||
| < 18.5 | 10.0 | 1(0.6) | ||
| 18.5–23.9 | 6.5(11.0) | 56(33.3) | ||
| 24.0–27.9 | 9.0(8.5) | 56(33.3) | ||
| 28–30 | 10.0(17.0) | 39(23.2) | ||
| ≥ 30 | 10.8(8.3) | 16(9.5) | ||
| Residence | 2.043 | 0.153 | ||
| Urban | 7.0(9.0) | 36(21.4) | ||
| Rural | 9.0(12.8) | 132(78.6) | ||
| Osteoporosis | 0.746 | 0.388 | ||
| None | 9.0(12.0) | 149(88.7) | ||
| Yes | 9.0(16.0) | 19(11.3) | ||
| ASA classification | 2.444 | 0.486 | ||
| 1 | 8.0(8.0) | 17(10.1) | ||
| 2 | 9.0(13.5) | 133(79.2) | ||
| 3 | 8.0(17.0) | 15(8.9) | ||
| 4 | 10.0(4.0) | 3(1.8) | ||
| Medical comorbidities | 6.829 | 0.145 | ||
| None | 9.0(13.0) | 141(83.9) | ||
| Diabetes | 6.0(6.0) | 9(5.4) | ||
| Hypertension | 11.0(11.0) | 10(6.0) | ||
| Cardiovascular system disease | 4.0(7.0) | 7(4.2) | ||
| Others* | 5.0 | 1(0.6) | ||
| Fracture characteristics | ||||
| Fracture pattern | 3.012 | 0.390 | ||
| Comminuted fracture(s) | 9.3(14.0) | 70(41.7) | ||
| Wedge fracture(s) | 6.0(8.5) | 78(46.4) | ||
| Oblique fracture(s) | 14.0(23.0) | 13(7.7) | ||
| Transverse fracture(s) | 10.0(26.0) | 7(4.2) | ||
| AO/OTA classification | 0.103 | 0.950 | ||
| Type A | 9.0(13.5) | 46(27.4) | ||
| Type B | 9.0(10.0) | 88(52.4) | ||
| Type C | 8.5(14.3) | 34(20.2) | ||
| Fractured bones | 3.288 | 0.511 | ||
| Humerus | 9.5(18.7) | 16(9.5) | ||
| Radius/ulna | 10.0(8.0) | 15(8.9) | ||
| Femur | 9.0(14.0) | 87(51.8) | ||
| Tibia/fibula | 9.0(11.0) | 37(22.0) | ||
| Others (Hand, foot and clavicle) | 6.0(10.0) | 13(7.7) | ||
| Weight/not weight limbs | 14.466 | <0.001* | ||
| Lower limb (Weight bearing bones) | 7.0(7.0) | 133(79.2) | ||
| Upper limb (Non-weighted bearing bones) | 18.0(18.0) | 35(20.8) | ||
| The side of fracture limbs | 0.182 | 0.670 | ||
| Left | 9.0(13.0) | 92(54.8) | ||
| Right | 9.5(13.0) | 76(45.2) | ||
| Seasonality | 1.490 | 0.685 | ||
| Spring | 10.5(19.0) | 46(27.4) | ||
| Summer | 9.5(9.0) | 40(23.8) | ||
| Autumn | 7.0(9.7) | 37(22.0) | ||
| Winter | 9.0(14.0) | 45(26.8) | ||
| Open/closed fracture | 0.016 | 0.899 | ||
| Open fracture | 8.5(13.2) | 26(15.5) | ||
| Closed fracture | 9.0(13.3) | 142(84.5) | ||
| Mechanism of injury | 3.600 | 0.463 | ||
| Motor vehicle accident | 9.0(13.0) | 99(58.9) | ||
| Pedestrian fall | 8.5(10.9) | 44(26.2) | ||
| Crush | 11.5(21.8) | 8(4.8) | ||
| Fall from height | 11.0(10.1) | 14(8.3) | ||
| Sport accident | 6.0(7.0) | 3(1.8) | ||
| Number of fracture(s) | 2.031 | 0.362 | ||
| 1 | 9.0(12.5) | 145(86.3) | ||
| 2 | 6.0(14.5) | 14(8.3) | ||
| > 2 | 6.0(10.5) | 9(5.4) | ||
| Operation related issues | ||||
| Number of used plates | 1.560 | 0.212 | ||
| 1 | 12.6(13.0) | 159(94.6) | ||
| 2 | 17.4(25.0) | 9(5.4) | ||
| The shape of used plates | 0.961 | 0.916 | ||
| Straight | 9.0(13.3) | 150(89.3) | ||
| L-shape | 9.0(7.7) | 8(4.8) | ||
| T-shape | 6.0(17.0) | 7(4.2) | ||
| Y-shape | 24.0 | 1(0.6) | ||
| O-shape | 11.0 | 2(1.2) | ||
| Ancillary fixation | 0.427 | 0.935 | ||
| None | 9.0(10.0) | 106(63.1) | ||
| K-wire(s) | 11.0(14.0) | 19(11.3) | ||
| Screw(s) | 9.0(14.0) | 42(25.0) | ||
| K-wire(s) and Screw(s) | 8.0 | 1(0.6) | ||
| Number of ancillary K-wire(s) | 0.071 | 0.965 | ||
| 0 | 9.0(13.0) | 149(88.7) | ||
| 1 | 8.5(11.5) | 8(4.8) | ||
| > 1 | 11.0(14.0) | 11(6.5) | ||
| Number of ancillary screw(s) | 7.751 | 0.054 | ||
| 0 | 9.0(10.0) | 126(75.0) | ||
| 1 | 8.0(6.8) | 20(11.9) | ||
| 2 | 9.0(24.0) | 11(6.5) | ||
| > 2 | 19.0(21.0) | 11(6.5) | ||
| Inserting screws closely adjacent to the fracture line | 5.674 | 0.017* | ||
| None | 9.0(13.0) | 146(86.9) | ||
| Yes | 5.5(8.3) | 22(13.1) | ||
| Number of empty screw holes adjacent to the fracture line | 6.245 | 0.182 | ||
| 0 | 5.5(8.3) | 22(13.1) | ||
| 1 | 10.0(13.0) | 76(45.2) | ||
| 2 | 8.5(16.3) | 40(23.8) | ||
| 3 | 9.0(8.8) | 22(13.1) | ||
| > 4 | 9.0(19.5) | 8(4.8) | ||
| The type of used plate | 0.122 | 0.727 | ||
| Plate(s) | 9.5(10.5) | 71(42.3) | ||
| Locked plate(s) | 9.0(13.0) | 97(57.7) | ||
| Surgeon performing the operation | 0.003 | 0.953 | ||
| Chief physician | 9.0(12.5) | 129(76.8) | ||
| Associate chief physician | 9.0(14.0) | 39(23.2) | ||
| Open or closed reduction of the fracture | 0.460 | 0.498 | ||
| Open reduction and internal fixation | 9.0(12.8) | 164(97.6) | ||
| Closed reduction and internal fixation | 21.0(17.3) | 4(2.4) | ||
| Postoperative complication(s) | 6.170 | 0.187 | ||
| None | 8.0(16.0) | 35(20.8) | ||
| Fracture nonunion | 9.0(11.8) | 112(66.7) | ||
| Fracture delayed union | 6.0(35.0) | 6(3.6) | ||
| Infection | 9.0(14.5) | 9(5.4) | ||
| Others | 30.0(42.8) | 6(3.6) | ||
| Postsurgical infection(s) | 0.313 | 0.855 | ||
| None | 9.0(12.5) | 154(91.7) | ||
| Superficial infection | 9.0(18.3) | 8(4.8) | ||
| Deep infection | 7.5(18.2) | 6(3.6) | ||
| Number of plate holes | 17.119 | <0.001* | ||
| < 5 | 25.5(24.5) | 22(13.1) | ||
| 5–10 | 8.0(8.3) | 69(41.1) | ||
| 11–15 | 9.0(12.0) | 60(35.7) | ||
| > 15 | 6.0(5.5) | 17(10.1) | ||
| Number of inserted screws | 6.604 | 0.037* | ||
| < 5 | 12.0(25.0) | 40(23.8) | ||
| 5–10 | 9.0(9.0) | 104(61.9) | ||
| 10 | 7.0(7.5) | 24(14.3) | ||
| Breakage characteristics | ||||
| Breakage site within/outside the fracture line | 5.196 | 0.023* | ||
| Within | 8.0(10.0) | 132(78.6) | ||
| Outside | 11.0(17.3) | 36(21.4) | ||
| Screw slack off the hole | 0.068 | 0.794 | ||
| None | 9.0(13.0) | 125(74.4) | ||
| Yes | 9.0(13.0) | 43(25.6) | ||
| Type of broken plate | 17.456 | <0.001* | ||
| Plate(s) | 6.5(8.1) | 114(67.9) | ||
| Screw(s) | 12.0(19.5) | 54(32.1) | ||
| Most possible underlying cause of breakage | 6.384 | 0.172 | ||
| Internal fixator improper selection | 10.0(21.8) | 36(21.4) | ||
| Premature postoperative training | 10.0(15.0) | 39(23.2) | ||
| Too short of a plate utilized | 7.0(8.6) | 34(20.2) | ||
| Screw(s) in inappropriate location | 5.0(11.0) | 39(23.2) | ||
| Others | 8.0(8.3) | 20(11.9) | ||
*Significant at α = 0.05
Fig. 3.
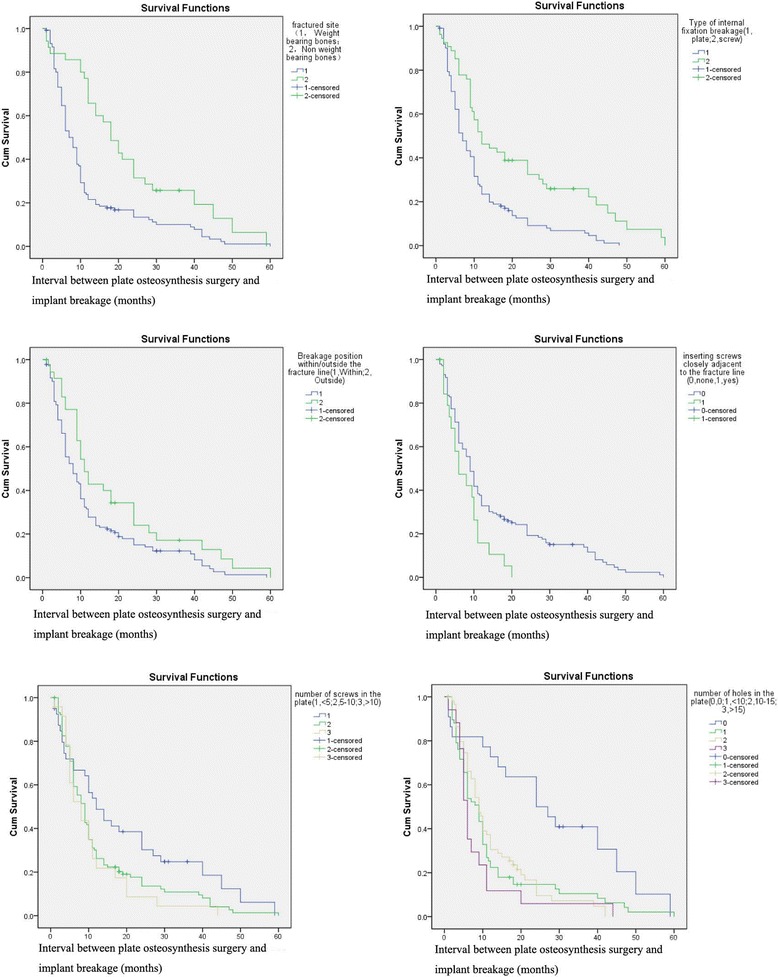
Kaplan-Meier survival curves of each of the covariates
Table 2 shows the results from the multivariate Cox regression analysis, which was used to assess the association of risk factors after adjusting for all other potential risk factors. In the final model, “inserting screws adjacent to the fracture line” was identified to be independently predictive of having implant breakage (HR, 2.165; 95% CI, 1.227 to 3.822; P = 0.008), with a 2.165-times increased risk of causing internal fixator breakage (Fig. 4). In the study, 13.1% of surgeons did not adhere to the principle for screw placement, and inserted screws closely adjacent to the fracture line.
Table 2.
Potential Predictors of Internal fixation breakage
| Predictor | B | SE | Wald | P value | HR | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| Weight/not weight limbs | -0.533 | 0.315 | 2.859 | 0.091 | 0.587 | 0.316 | to | 1.089 |
| Type of broken plate | -0.352 | 0.290 | 1.474 | 0.225 | 0.703 | 0.399 | to | 1.241 |
| Breakage site within/outside the fracture line | -0.143 | 0.278 | 0.266 | 0.606 | 0.866 | 0.502 | to | 1.494 |
| Inserting screws closely adjacent to the fracture line | 0.772 | 0.290 | 7.100 | 0.008* | 2.165 | 1.227 | to | 3.822 |
| Number of plate hole(s) | 2.855 | 0.414 | ||||||
| < 5 | -0.993 | 0.649 | 2.343 | 0.126 | 0.370 | 0.104 | to | 1.321 |
| 5–10 | -0.459 | 0.379 | 1.468 | 0.226 | 0.632 | 0.301 | to | 1.328 |
| 11–15 | -0.442 | 0.331 | 1.781 | 0.182 | 0.643 | 0.336 | to | 1.230 |
| Number of plate screw(s) | 2.633 | 0.268 | ||||||
| < 5 | 0.651 | 0.447 | 2.128 | 0.145 | 1.918 | 0.799 | to | 4.604 |
| 5–10 | 0.194 | 0.317 | 0.374 | 0.541 | 1.214 | 0.652 | to | 2.260 |
*P < 0.05 through multivariate Cox regression analysis
Fig. 4.
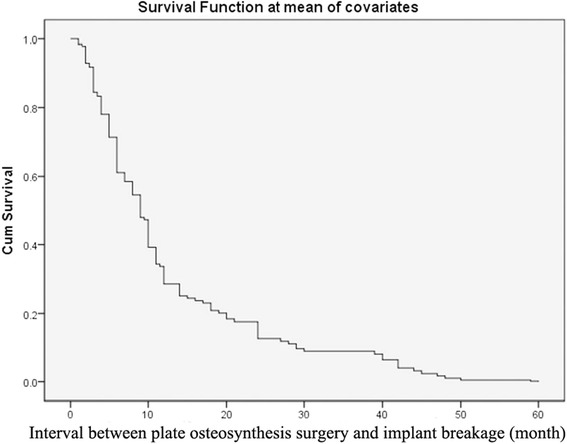
Cox survival function curves for each of the covariates
Discussion
Plate osteosynthesis of a fracture is a common procedure with well-established efficacy for achieving union, reducing pain, and improving function in appropriately selected patients [11–13]. However, the occurrence of plate-screw construct breakage is hard to avoid. The rate of nonunion for mid-shaft clavicle fractures is 1.4% [14], whereas that of femoral fractures is 6% to 17% [15–18]. In recent years, there has been an increase in the frequency of implant breakage along with the increasing use of plate fixation; yet, there are few studies describing the factors that contribute to this complication. The present study used a long-term follow-up of a large patient population to identify the independent risk factors associated with plate fixation breakage among patients with traumatic fractures.
Our single-factor analysis showed that the risk of fracture was associated with the weight or not weight limbs, the type of broken plate, breakage site within/outside the fracture line, the number of plate holes, the number of plate screws, and inserting screws closely adjacent to the fracture line. A multivariate Cox regression analysis confirmed that inserting screws adjacent to the fracture line was related to an increased risk of implant breakage for patients who had a fracture of the limbs, clavicle, hands, or feet. Previous studies have reported various risk factors for implant breakage, including being female, higher comorbidity scores, surgeons with fewer years’ experience, the use of longer plates, among other factors [19, 20]; we did not identify any of these factors as risk factors in our study.
In the current study, most implant breakages occurred within the first year, just as showed in Table 1. Most patients were aged between 20 and 50 years (62.5%), were male (72.0%), overweight (66.0%), and from a rural area (78.6%). Patients at risk were more likely to have experienced a high-energy trauma (73.8%) or complex fracture (88.1%) to a lower limb (79.2%), with failure occurring as a result of plate breakage (67.9%).
Plate osteosynthesis can provide relative stability, keep the fracture in a better biological position, and promote callus formation and fracture healing [21]. For complex fractures, recommendations are to use longer plates but without placing screws into the holes adjacent to the fracture line. In addition, increasing the bridging plate-work length to help distribute the stress over a larger area of the plate and thereby minimize the risk of breakage is advised. Similar rules exist for the treatment of simple and comminuted fractures, with surgeons advised against placing screws into the holes adjacent to the fracture line [22, 23]. For comminuted fractures, leaving these holes empty allows for slight movement among the fracture fragments, which is beneficial for callus formation within a reasonable scope of strain [24].
Many previous studies have shown that following biological and bridge plate techniques can obtain good radiological and functional results [25–28]. In the current study, most of the surgeons (86.9%) did not place the screws close to the fracture line; however, 13.1% of surgeons did not adhere to the principle for screw placement, and this caused an increase in the rate of plate breakage.
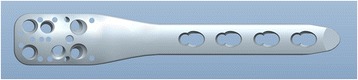
The presence of holes positioned adjacent to the fracture line provides an opportunity for their use, which is against recommendations. Thus, we suggest that it is unnecessary for these plates to be manufactured with these additional holes. We therefore designed a plate without holes at a part of the plate (patent number: ZL201520890025.3), and we suggest this part can be placed adjacent to the fracture line (Fig. 5). For example, surgeons can position the portion without holes in the middle for a ulnar shaft fracture, at the distal part as used in the fixation of supercondylar femoral fracture, or at the proximal part as used in the fixation of surgical neck fractrue of the humerus (Fig. 6). Another feature is that the part of the plate without holes is thickest, becoming thinner gradually to both ends (Fig. 5). This kind of plate will improve the mechanical strength of the whole plate-screw construct and subsequently reduce the risk of implant breakage.
Fig. 5.
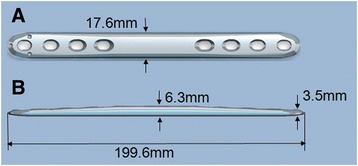
The newly-designed individual plate is featured without holes in one part of the plate, which part should be placed adjacent to the fracture line. Another is that the part without holes is the thickest, becoming thinner gradually to both ends. (a, anteroposterior view; b, lateral view)
Fig. 6.
The newly-designed plate used in the fixation of surgical neck fractrue of the humerus with proximal part without holes
Limitations
Our study has a few limitations. First, this was a retrospective study, and inevitable recall bias exists. Second, we did not distinguish between bridge plating fixation and compression fixation because both principles were used in many of the cases and they are difficult (and somewhat unnecessary) to distinguish. Third, it is not certain precisely when the construct breakage occurred, with breakage time determined as the time of the latest radiographic evidence.
Conclusions
Using multivariate Cox regression analysis, we show that there is an increased risk of implant breakage in patients who had a fracture of the four extremities, clavicle, hand or foot after plate osteosynthesis fixation when screws were placed in the holes of the plate adjacent to the fracture line. The data also suggests that the newly-designed individual plates without holes in a part of the plate, which part should be placed adjacent to the fracture line, can help reduce the risk of implant breakage. Additional prospective studies are warranted to compare this new plate type with existing instrumentation to confirm that the placement of screws near the fracture line affect the treatment of traumatic fractures.
Acknowledgements
We thank Dr. Wei Chen and Dr. Zhiyong Hou for their assistance in the analysis of the data and radiographs.
Funding
None
Availability of data and materials
All data is available at http://zhlngkykfdzzz.cthhmu.com/docs/AuthorPark/default.aspx?pageindex=2. This is the websit of The Chinese Journal of Geriatric Orthopaedics and Rehabilitation, which is a department of our hospital. The website of our hospital is http://www.cthhmu.com/. The dataset used in the current study has never been reported previously in any other journal.
Authors’ contributions
YZ designed the study; HL and WC searched the relevant studies and abstracted the data; PY and NY analyzed and interpreted the data; HL and WC wrote the draft; HL, XY and YZ revised the manuscript. YZ approved the final version of the manuscript. All authors have read and approved the final submitted manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
All patients have signed the informed consents and agreed their data to be analyzed and published.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the 3rd Hospital of Hebei Medical University. All patients agreed to participate in this study and signed the informed consents.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ASA
American Society of Anesthesiologists
- BMI
Body mass index
- HRS
Calculate hazard ratios
Contributor Information
Hongzhi Lv, Email: lvhongnuo@126.com.
Wenli Chang, Email: drchangwenli@qq.com.
Peizhi Yuwen, Email: yuwenpeizhi@163.com.
Na Yang, Email: yangna4444@126.com.
Xiaoli Yan, Email: yanxiaolilv@126.com.
Yingze Zhang, Email: zhangyingzelv@126.com.
References
- 1.Adam P, Bonnomet F, Ehlinger M. Advantage and limitations of a minimally-invasive approach and early weight bearing in the treatment of tibial shaft fractures with locking plates. Orthop Traumatol Sur. 2012;98(98):564–9. doi: 10.1016/j.otsr.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 2.Thapa S, Thapa SK, Dhakal S, Marasini R, Hamal B, Rai RK, et al. A comparative study of fracture shaft of femur in adults treated with broad dynamic compression plate versus intramedullary interlocking nail. JCMS-Nepal. 2016;12(2):66–9. [Google Scholar]
- 3.Ding L, He Z, Xiao H, Chai L, Xue F. Factors affecting the incidence of aseptic nonunion after surgical fixation of humeral diaphyseal fracture. J Orthop Sci. 2014;19(6):973–7. doi: 10.1007/s00776-014-0640-1. [DOI] [PubMed] [Google Scholar]
- 4.Belmont PJ, Jr, Davey S, Rensing N, et al. Patient-based and surgical risk factors for 30-day postoperative complications and mortality after ankle fracture fixation. J Orthop Trauma. 2015;29(12):e476–e82. doi: 10.1097/BOT.0000000000000328. [DOI] [PubMed] [Google Scholar]
- 5.Soong M, Leerdam RV, Guitton TG, Got C, Katarincic J, Ring D. Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg [Am] 2011;36(1):3–9. doi: 10.1016/j.jhsa.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 6.Gardner MJ, Evans JM, Dunbar RP. Failure of fracture plate fixation. J Am Acad Orthop Surg. 2009;17(10):647–57. doi: 10.5435/00124635-200910000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Gautier E, Ch S. Biological internal fixation—guidelines for the rehabilitation. Ther Umsch. 2003;60(12):729–35. doi: 10.1024/0040-5930.60.12.729. [DOI] [PubMed] [Google Scholar]
- 8.Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003;34(Suppl 2):B63–76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 9.Stoffel K, Dieter U, Stachowiak G, Gächter A, Kuster MS. Biomechanical testing of the LCP—how can stability in locked internal fixators be controlled? Injury. 2003;34(Suppl 2):B11–B9. doi: 10.1016/j.injury.2003.09.021. [DOI] [PubMed] [Google Scholar]
- 10.Sanders R, Haidukewych GJ, Milne T, Dennis J, Latta LL. Minimal versus maximal plate fixation techniques of the ulna: the biomechanical effect of number of screws and plate length. J Orthop Trauma. 2002;16(3):166–71. doi: 10.1097/00005131-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Pennington SD, Duralde XA. Locking plate fixation for proximal humerus fractures. Am J Orthop. 2014;43(7):302–8. [PubMed] [Google Scholar]
- 12.Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. Orthop Traumatol Sur. 2009;91(7):1689–97. doi: 10.2106/JBJS.H.00133. [DOI] [PubMed] [Google Scholar]
- 13.Ruchholtz S, Hauk C, Lewan U, Franz D, Kühne C, Zettl R. Minimally invasive polyaxial locking plate fixation of proximal humeral fractures: a prospective study. J Trauma. 2011;71(6):1737–44. doi: 10.1097/TA.0b013e31823f62e4. [DOI] [PubMed] [Google Scholar]
- 14.Mckee RC, Whelan DB, Schemitsch EH, Mckee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. JBJS. 2012;94(8):675–84. doi: 10.2106/JBJS.J.01364. [DOI] [PubMed] [Google Scholar]
- 15.Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma. 2006;20(3):190–6. doi: 10.1097/00005131-200603000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18(8):509–20. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Haidukewych G, Sems SA, Huebner D, Horwitz D, Levy B. Results of polyaxial locked-plate fixation of periarticular fractures of the knee. J Bone Joint Surg Am. 2007;89(3):614–20. doi: 10.2106/JBJS.F.00510. [DOI] [PubMed] [Google Scholar]
- 18.Ricci WM BJ., Jr Operative management of periprosthetic femur fractures in the elderly using biological fracture reduction and fixation techniques. Injury. 2007;38(Suppl 3):S53–8. doi: 10.1016/j.injury.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 19.Leroux T, Wasserstein D, Henry P, Khoshbin A, Dwyer T, Ogilvie-Harris D, et al. Rate of and risk factors for reoperations after open reduction and internal fixation of midshaft clavicle fractures: a population-based study in Ontario. Canada J Bone Joint Surg Am. 2014;96(13):1119–25. doi: 10.2106/JBJS.M.00607. [DOI] [PubMed] [Google Scholar]
- 20.Ricci WM, Streubel PN, Morshed S, Collinge CA, Nork SE, Gardner MJ. Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. J Orthop Trauma. 2014;28(2):83–9. doi: 10.1097/BOT.0b013e31829e6dd0. [DOI] [PubMed] [Google Scholar]
- 21.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg (Br) 2002;84(84):1093–110. doi: 10.1302/0301-620X.84B8.13752. [DOI] [PubMed] [Google Scholar]
- 22.Schmidtmann U, Knopp W, Wolff C, Stürmer KM. Results of elastic plate osteosynthesis of simple femoral shaft fractures in polytraumatized patients. An alternative procedure. Unfallchirurg. 1997;100(12):949–56. doi: 10.1007/s001130050217. [DOI] [PubMed] [Google Scholar]
- 23.Stürmer KM. Elastic plate osteosynthesis, biomechanics, indications and technique in comparison with rigid osteosynthesis. Unfallchirurg. 1996;99(11):816–29. doi: 10.1007/s001130050061. [DOI] [PubMed] [Google Scholar]
- 24.Perren SM. The concept of biological plating using the limited contact-dynamic compression plate (LC-DCP). Scientific background, design and application. Injury. 1991;22(Suppl 1):1–41. [PubMed] [Google Scholar]
- 25.Baumgaertel F, Gotzen L. The “biological” plate osteosynthesis in multi-fragment fractures of the para-articular femur. A prospective study. Unfallchirurg. 1994;97(2):78–84. [PubMed] [Google Scholar]
- 26.Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H. Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury. 1997;28(1):A31–41. doi: 10.1016/S0020-1383(97)90113-3. [DOI] [PubMed] [Google Scholar]
- 27.Wenda K, Runkel M, Degreif J, Rudig L. Minimally invasive plate fixation in femoral shaft fractures. Injury. 1997;28(Suppl 1):A13–9. doi: 10.1016/S0020-1383(97)90111-X. [DOI] [PubMed] [Google Scholar]
- 28.Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004;18(8):528–35. doi: 10.1097/00005131-200409000-00008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data is available at http://zhlngkykfdzzz.cthhmu.com/docs/AuthorPark/default.aspx?pageindex=2. This is the websit of The Chinese Journal of Geriatric Orthopaedics and Rehabilitation, which is a department of our hospital. The website of our hospital is http://www.cthhmu.com/. The dataset used in the current study has never been reported previously in any other journal.


