Abstract
Diabetes prevalence in Tanzania was estimated at 9.1% in 2012 among adults aged 24–65 years — higher than the HIV prevalence in the general population at that time. Health systems in lower- and middle-income countries are not designed for chronic health care, yet the rising burden of non-communicable diseases such as diabetes demands chronic care services. To inform policies on diabetes care, we conducted a study on the health services in place to diagnose, treat and care for diabetes patients in rural Tanzania. The study was an exploratory and descriptive study involving qualitative methods (in-depth interviews, observations and document reviews) and was conducted in a rural district in Tanzania. Fifteen health providers in four health facilities at different levels of the health care system were interviewed. The health care organization elements of the Innovative Care for Chronic Conditions (ICCC) framework were used to guide assessment of the diabetes services in the district. We found that diabetes care in this district was centralized at the referral and district facilities, with unreliable supply of necessary commodities for diabetes care and health providers who had some knowledge of what was expected of them but felt ill-prepared for diabetes care. Facility and district level guidance was lacking and the continuity of care was broken within and between facilities. The HMIS could not produce reliable data on diabetes. Support for self-management to patients and their families was weak at all levels. In conclusion, the rural district we studied did not provide diabetes care close to the patients. Guidance on diabetes service provision and human resource management need strengthening and policies related to task-shifting need adjustment to improve quality of service provision for diabetes patients in rural settings.
Keywords: Chronic health care, diabetes services, Innovative Care for Chronic Conditions framework, leadership in service delivery, rural district, Tanzania
Introduction
Key Messages
A know–do gap exists among providers regarding diabetes care provision.
Self-management support to patients is limited and sometimes contradictory.
Guidance for diabetes services at facility and district levels must be strengthened if diabetes services are to be provided according to the ICCC framework in this rural district.
Non-communicable diseases (NCDs) are the leading causes of death worldwide (Alwan, 2010), contributing to 68% of the 56 million deaths globally in 2011. Around 80% of those deaths (30 million) occurred in low- and middle-income countries (LMICs), and 48% in LMICs occurred in persons under 70 years of age (Whiting et al. 2011). In Tanzania, NCDs accounted for 31% of all deaths in 2011 (WHO 2014). The global NCD crisis prompted the World Health Organization (WHO) to set a worldwide goal to reduce NCD deaths by 2% each year (Beaglehole et al. 2011a). To achieve this goal, comprehensive responses covering prevention and control of NCDs must be instituted. Although primary prevention is important for any response to NCDs, effective and affordable health services have to be delivered to persons already afflicted by NCDs (WHO 2013).
Health systems in LMICs were designed for acute disease management (Whiting et al. 2003; Beaglehole et al. 2008; Rabkin and Nishtar 2011). Yet management of chronic conditions is fundamentally different from acute care, because chronic conditions place greater demands on patients, families, health systems and governments due to, for instance, continued follow-up for disease monitoring and adherence to long-term treatment (Rabkin and Nishtar 2011). Among the priority NCDs in LMICs are diabetes, cardiovascular diseases, cancers and Chronic Obstructive Airway Diseases (United Republic of Tanzania [URT] 2008; Beaglehole et al. 2011b ), which were responsible for an estimated 2, 12, 3 and 3%, respectively, of all deaths in Tanzania in 2010 (WHO 2014).
In response, the Tanzanian government has set up an NCD unit within the Ministry of Health and Social Welfare. It has also included within the Health Sector Strategic Plan IV of 2015–2020 a strategic objective to gradually step up diagnostic and therapeutic capacities for NCDs (URT 2015). Patients with chronic diseases such as diabetes are also exempted from user fees in Tanzania, in an effort to make chronic disease services more accessible (Mubyazi 2008). At community level, documented NCD-related activities are only provided by private health facilities; they include teaching primary school pupils and general communities about healthy lifestyles (Metta et al. 2014). Nevertheless, over 60% of persons with diabetes in Tanzania do not know they have it (Kavishe et al. 2015) indicating weaknesses in health seeking behaviour, screening and case detection (Metta et al. 2015).
A 2012 Tanzanian national survey estimated diabetes prevalence at 9.1% among adults aged 25–64 years (WHO 2012), higher than the latest national HIV prevalence estimate of 5.1% (TACAIDS 2013) and a significant increase from the estimated 2.5% diabetes prevalence in 1984 among persons aged 20 years and above (Ahren 1984). There is limited data on the trend of the prevalence of diabetes in rural Tanzania. It is however, likely that this prevalence has also increased as findings from different surveys of rural populations over the years seem to suggest.
An increase in diabetes prevalence was noted in rural Tanzanian populations, from 0.9% in the 1980s to 1.3% in 2000 (Ramaiya 2005). The 2012 national survey estimated diabetes prevalence in 38 randomly sampled rural districts at 9.4% among males and 9.1% among females aged 25–64 years, although sample size estimation and sampling for the survey did not consider rural–urban differences (Kaguruki 2015). Tanzania’s health system is generally resource-limited—for instance, the human resources for health (HRH) shortage was estimated at 56% in 2014 (URT, 2014). The HRH shortage is more severe in rural areas—e.g. in 2014, 74% of medical doctors worked in urban-based hospitals. Thus rural areas have worse access, availability and readiness indicators for diabetes and other health services than urban areas (Ministry of Health and Social Welfare 2013; USAID 2013b). A 2014 study of 24 rural and urban Tanzanian health facilities found that in most of the facilities diagnostic equipment, guidelines and essential medications were inadequate and that training, management and reporting systems were weak for diabetes and hypertension care, especially in rural health facilities (Peck et al. 2014). These findings support earlier Tanzanian studies which concluded that diabetes services need improvement (McLarty et al. 1996; Kolling et al. 2010).
Currently, specific national-level strategies to tackle diabetes include the stipulation in the National Package of Essential Health Interventions for Tanzania (NPEHIT), that dispensaries and health centres should provide diabetes-related preventive services, perform routine blood pressure and blood sugar checks, diagnose and treat diabetes and keep records of patients for follow-up. The NPEHIT is only a list of suggested interventions for common diseases in Tanzania, for each level of health care service (United Republic of Tanzania, Ministry of Health 2000).
The Innovative Care for Chronic Conditions (ICCC) framework was developed to guide LMICs to adapt their health systems to provide better care for chronic diseases (Sheri Pruit et al. 2002). It suggests that, for better patient outcomes, the health providers, the patient with his/her family and the community (micro level) must be prepared, informed and motivated in their interactions, supported by a health care organization that works closely with the broader community (meso level), all in an overarching positive policy environment (macro level). This framework has been used to guide strategy development for chronic care in South Africa (Oni et al., 2014) but has not been operationalized level in sub-Saharan Africa (van Olmen et al. 2012).
Currently, it is not known how health providers in rural settings are dealing with the increasing number of diabetes patients and how they perceive their roles in diabetes care in the existing health care system. This article therefore, aims to add to the current evidence base, by presenting a qualitative description of how diabetes is dealt with in rural health care systems, guided by the ICCC framework, in order to inform policy makers what to improve in care for diabetes and other NCDs.
We focused on type 2 diabetes mellitus because of its rising prevalence among rural populations in Tanzania, and its diagnosis requires simple diagnostic equipment that can be readily operated at primary health care settings in LMICs (Maher et al. 2012).
Methods
This qualitative study’s main research question is: How do health providers perceive and experience the organization and delivery of care and treatment services for diabetes in a rural district, according to the health care organization elements of the ICCC framework?
The study was developed using the health care organization roles stipulated in the ICCC framework and focused on diabetes service delivery in a rural district in Tanzania. The health care organization’s roles (described in Table 1) cover five main areas: promoting continuity and coordination; encouraging leadership through quality and incentives; organizing and equipping health care teams; using information systems; and supporting self-management and prevention.
Table 1.
Roles of health care organizations according to ICCC
| Health care organization roles according to ICCC | Description of the roles according to ICCC |
|---|---|
| Promote continuity and coordination |
|
| Encourage quality through leadership and incentives |
|
| Organize and equip health care teams |
|
| Use information systems |
|
| Support self- management and prevention |
|
Adapted from Sheri Pruit et al. (2002).
An additional element that emerged from data.
Study setting
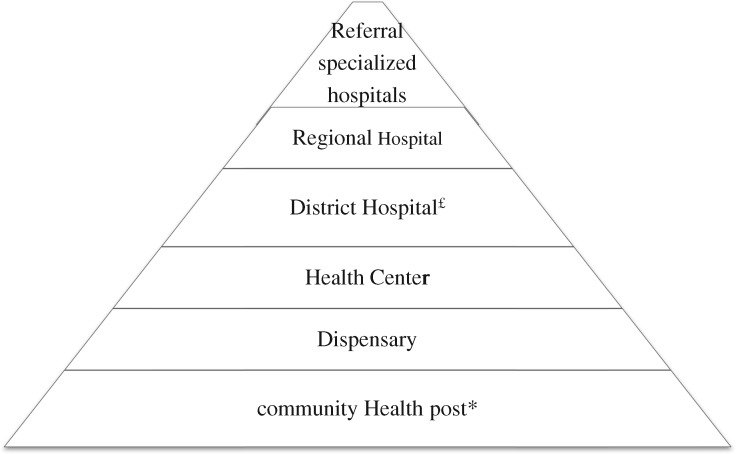
The study was conducted in four health facilities—a referral-hospital, a district-hospital, a health centre and a dispensary—representing the different levels of health care in Tanzania (Figure 1). The selected dispensary was the only one offering HIV treatment and care services (chronic care services) in the study district. The health centre was selected because it received referred patients from the selected dispensary and referred patients to the district hospital. The referral hospital was included because it received referred patients from the selected district hospital, although it was in a different district neighbouring the study district. The selected dispensary, health centre and district-hospital were public health facilities. The referral-hospital was owned by a faith-based organization (FBO), and received some financial and HRH support from the government. It operated at the level of regional hospital. Health facilities at different levels were selected to capture experiences and practices at different levels of health care in rural settings.
Figure 1.
Levels of health care services in Tanzania. *Not consistently available in every village. £Some districts rely on hospitals owned by faith based organizations that are designated district hospitals. These health care service levels are also the health facility levels. Lower-level health facilities refer patients to the immediate higher-level for more advanced services, i.e. the referral lines.
The selected rural district was in southern Tanzania, where the first author’s research institution has focused most of its research activities. It was, therefore, more convenient to work in this district. It was also selected because it had a dispensary that offered chronic diseases care services (HIV care and treatment services), and had comparable socio-economic indicators and health service structure to other rural districts in Tanzania. In 2012, its population was 265 203 persons, of whom 38.5% were 25 years and above (Ministry of Finance, United Republic of Tanzania 2013). Ninety one percent of adults were employed in agriculture, growing mainly rice, bananas and maize. In 2004, electricity was the main source of energy for 1.1% of the population, and literacy in the district was estimated at 65% (National Bureau of Statistics [NBS] 2004). These statistics compare well to the average of 3% of Tanzanian rural populations using electricity and 66.1% average literacy level for Tanzanian rural populations (NBS 2011). There were no official data on diabetes prevalence in the district, but in the district of the referral-hospital it was 4.8%, in 2012/13 (Ramadhani et al. 2014).
Public health services in the district comprised one district-hospital, three health centres and 33 dispensaries. Most public health facilities are headed by clinicians—health providers with medical training. In Tanzania, they include clinical officers (secondary school graduates with three years of basic clinical training), assistant medical officers (clinical officers with a further 2 years clinical training) and medical doctors, including specialists. The district hospital had one medical doctor, who was the hospital in-charge and also served as the district medical officer, expected to oversee health activities in the district. One health centre was headed by a clinical officer, and the other two by assistant medical officers. All three health centres offered outpatient, HIV care and treatment, reproductive and child health (RCH) and basic laboratory services. Two of them had operating theatres for obstetric emergencies. The dispensaries were headed by clinical officers and offered basic outpatient and RCH services. They did not have laboratories, but all performed rapid malaria and HIV testing. The ratio of health workers (all cadres) to population in the district is estimated at 2.1 per 1000 population which is within the range of 0.3–3.0 per 1000 population for rural districts in Tanzania (Munga and Maestad 2009). The district also had eight FBO-owned health facilities; a hospital and seven dispensaries, which did not offer diabetes services but offered similar services to public dispensaries. Among the FBO-owned health facilities, only the hospital has capacity to provide diabetes services. According to reports, it served 60 diabetes patients in 2012.
Study design and recruitment of participants
This was an exploratory and descriptive study using in-depth interviews, observations and document reviews. Interviews elicited individual-level views on health providers’ practices and the current care and treatment of diabetes patients. The availability of supplies and equipment was observed, and documents were reviewed to assess health provider’s documentation practices.
Participants were purposively sampled from a list of eligible health providers at each health facility by researchers, with help from facility in-charges who clarified their functions. The sampling criteria were that the health providers provided diabetes care, were expected to interact with suspected diabetes patients, or were responsible for diabetes-related health information. The hospital and clinic in-charges at the district hospital and referral hospital, respectively, introduced the researchers to the health providers and the researchers recruited the participants. At the health centre and the dispensary, the facility in-charges (clinical officers for both health facilities) and a second clinician (clinical officer for both health facilities) were all interviewed. We sampled 20 providers for the interviews; however, five district hospital providers could not participate (Table 2) due to: providers feeling unable to discuss diabetes due to perceived limited experience with its care and treatment [one nutritionist and one medical attendant (nurse assistant)]; absence for practical reasons (two clinical officers) and refusal to participate due to lack of benefits (one assistant medical officer). It is worth noting that non-clinician health providers at the dispensary, health centre and district hospital were not directly involved in diabetes care hence the concentration of clinicians in the study sample. Recruitment was stopped because saturation of information regarding emerging issues was reached in the data collected.
Table 2.
Number of providers sampled and those eventually recruited by cadre and facility
| Facility | Cadres of participants recruited |
|||||||
|---|---|---|---|---|---|---|---|---|
| Sampled providers | Consultant Physiciana | Medical Officea | Assistant Medical Officera | Clinical Officera | Nursing Officerb | Medical Attendantb | Total recruited | |
| Referral | 6 | 1 | 2 | 1 | – | 1 | 1 | 6c |
| District | 10 | – | – | 3 | 2 | – | – | 5 |
| Health centre | 2 | – | – | – | 2 | – | – | 2 |
| Dispensary | 2 | – | – | – | 2 | – | – | 2 |
| Total | 20 | 1 | 2 | 4 | 6 | 1 | 1 | 15 |
Consultant physician, Medical doctors, Assistant medical officers and a clinical officers are all clinicians which means a health worker with medical training.
A nursing staff member, who performs nursing duties. A medical attendant is like a nurse assistant.
All (n = 6) providers assigned to the diabetes clinic of the referral hospital were interviewed.
Data collection and analysis
Data were collected between June and July 2013. Interviews were conducted by a team comprising the first author and two trained research assistants with a social science background. The interview guides addressed perceptions of providers’ practices regarding the care and treatment of diabetes patients and handling diabetes information. The first author conducted the observations by visiting outpatient settings—clinic rooms, pharmacies and laboratories—to see what supplies and equipment were available and their functional status. She also reviewed documents stored or in use at the outpatient settings for documentation practices—reports, patient attendance registers and patient notes.
We interviewed 15 participants using Kiswahili language. The interview guides and the observation checklists were all adapted after pre-testing. Text transcripts of interviews were anonymized and cross-checked with the audio transcripts for quality by the first author before being imported into NVivo 10 (QSR International Pty Ltd, Australia).
All transcripts, observations and document review findings were analyzed in their original language. Code development was largely informed by the ICCC framework and new codes that emerged from the transcripts were added. The NPEHIT guided the analysis of the availability of diabetes services at the different health facility levels. Analysis took place according to main themes emerging from the data and related to the ICCC: (1) availability and preparedness for diabetes services; (2) guidance and support for diabetes services; (3) promotion of continuity and coordination; (4) information systems and their use; and (5) supporting self-management. Observation and document review notes were typed into Word documents and analyzed in the same way as the interviews.
Information from the different sources was triangulated by comparing the findings from observations, document review and the interviews, and identifying similarities or contrasts. Issues emerging were further clarified through phone calls or face-to-face meetings with some district and referral hospital providers and the district medical officer.
Results
The selected facilities were in a referral line and differed in capacities, workforce and workload (Table 3). Fifteen providers were interviewed. The majority were male and clinicians. Most had spent over 10 years in clinical service; their ages ranged from 28 to 57 years (median 47 years). Referral-facility participants had spent a median of 3.5 years working in the diabetes clinic (range 1–7 years).
Table 3.
Features of the four facilities included in the study
| Facility level | Medical doctors | Nurses | Medical attendants | Patients/month | Bed capacity | DM testa | HIV care | Consultation fee (Tshb) |
|---|---|---|---|---|---|---|---|---|
| Dispensary | 0 | 1 | 2 | 1651 | None | No | Yes | 1500c |
| Health centre | 0 | 2 | 8 | 770 | 21 | No | Yes | 1500b |
| District | 2 | 21 | 61 | 5100 | 121 | Yes | Yes | 2000 |
| Referral | 8 | 78 | 106 | 7574 | 400 | Yes | Yes | 5000 |
Test for diabetes available.
Chronic disease patients are exempt from paying any fee at public facilities.
The fee includes charges for any medication dispensed.
Theme 1:availability and preparedness for diabetes services
The availability of services, equipment and commodities and preparedness of facilities and health providers for diabetes care were explored.
Availability of services
Providers indicated that diabetes treatment and care services were available at the referral and district hospitals, as providers there could diagnose and treat diabetes. The referral-hospital had a designated clinic for diabetes operating three days a week, and a clinic coordinator. Records showed that 495 diabetes patients were registered there. According to referral-hospital providers, the clinic’s care team had four clinicians, including the coordinator, and two nursing staff (Table 2). The 2012 district-hospital report showed that only 11 diabetes patients had been seen there in the whole year. District-hospital diabetes services were provided by the same clinicians who were scheduled to serve at the general outpatient department and there was no coordinator of diabetes services.
Providers at the health centre and dispensary described the diabetes services they offered as ‘pre-diagnosis’, denoting the lack of diabetes diagnosis, care or treatment services at those facilities; patients suspected of having diabetes were referred to higher-level health facilities.
… for diabetes, it’s not treatment level, it is what we call pre-diagnosis; that is we listen to the history of the patient. After that, if it is symptoms of diabetes, we advise them to go to the District hospital or the referral hospital. …they continue with the clinic there because here we do not have the diabetes clinic or medication for diabetes.” Health-centre provider
Equipment and supplies for diabetes care
Availability of equipment for diabetes care, as observed at the facilities, is presented in Table 4.
Table 4.
Availability of supplies and equipment for diabetes care by facility level
| ICCCa requirement | Operationalization of ICCC description | Findings by facility level | |||
|---|---|---|---|---|---|
| Medical equipment and supplies | List recommended by IDAb guidelines | Referral hospital | District hospital | Health centre | Dispensary |
| Urine strips for glucose, ketones and proteins | A and Fc | A and F | None | None | |
| Blood glucose meter | A and F | A and F | None | None | |
| Appropriate glucose strips | A and F | A and F | None | None | |
| Sphygmomanometer | A and F | A and F | A and F | A and F | |
| Cuff sizes for sphygmomanometer | One size | One size | One size | One size | |
| Weight scale | A and F | A and F | A and F | A and F | |
| Height scale | A and F | None | None | None | |
| Monofilament | None | None | None | None | |
| Prescribed for secondary-level facilities and first-level referral facilities | |||||
| Tuning fork and patellar hammer | None | None | Not expected at health centre level | Not expected at dispensary | |
| Ophthalmoscope | A and F | None | |||
| Biochemistry analyzer: | |||||
| • Glucose | None | None | |||
| • Lipids | None | None | |||
| • Renal functions | A and F | A and NFd | |||
| • Glycated hemoglobin | None | None | |||
| Laboratory | Laboratory services | A and F | A and F | A and NF | None |
| Essential medications for diabetes | List recommended by STGe | ||||
| Chlorpropamide | None | None | None | None | |
| Glibenclamide | Available | Available | None | None | |
| Gliclazide | None | None | None | None | |
| Tolbutamide | None | None | None | None | |
| Metformin | None | None | None | None | |
| Glucagon injection | None | None | Not expected at health centres | Not expected at dispensary level | |
| Insulin short acting | Available | None | |||
| Insulin intermediate acting | None | None | |||
| Insulin long acting | Available | None | |||
| Decision-making | Guidelines/algorithms | None | None | None | None |
Innovative care for chronic conditions.
International Diabetes Association, Africa (2006). Type 2 Diabetes Clinical Guidelines for SSA.
A and F—Available and functional.
A and NF - Available and not functional.
STG—Ministry of Health, Tanzania (2007). Standard Treatment Guidelines.
According to referral- and district-hospital providers and triangulated by observation, the referral and district hospitals had most of the primary-level requirements available but lacked secondary-level equipment and supplies for monitoring diabetes complications and long-term blood sugar control. These providers stated that stock-outs of diabetes medication and laboratory reagents were frequent enough to require attention, because when they occurred, providers’ work was affected in several ways. At the referral hospital, reported effects included patients having to buy diabetes medication from private drug vendors for more than at the facility. At the district hospital, the effects included having to refer patients for basic services such as testing for blood sugar to the referral hospital, and patients leaving untreated. Equipment, supplies and medication for diabetes diagnosis, monitoring and treatment were lacking at the health centre and dispensary.
Perceptions on preparedness and organization of providers
Providers reported that they needed further training on diabetes care and management, due to perceived continuous changes in care practices. All reported receiving pre-service training on diabetes care, and some had received in-service training on diabetes management ranging from one day to two weeks in duration and from 1 to 5 years since the training. Some providers from all levels expressed an understanding of the importance of personalized attention for lifestyle interventions but felt deficient in the skills needed to provide it. Others even asked for specific staff to provide that service, envisaging a more proactive role than merely providing information at the facility
In the services for changing lifestyle of a person, we don’t have that person. Those services of following up that person in detail like services of outreach programmes of may be going to know a patient’s home, how they live and others we don’t have. We only ask him to know what they do which is not adequate… (Referral-hospital provider)
According to both referral- and district-hospital providers, clinicians dominated patient management. For example, according to some district-hospital providers, only clinicians managed diabetes patients, and no other cadre had a role in decision making on patient care or education at the district hospital.
Theme 2: guidance and support for diabetes services
We sought providers’ perceptions on how facility- and district-level authorities guided or supported diabetes services. Providers at the referral hospital’s diabetes clinic thought that the clinic received significant support from the hospital management in the form of clinic rooms, reducing the consultation fee for diabetes services from Tsh7000 (US$4.29)1 to TSh4000 (US$2.45) since 2012, and allocating staff to the diabetes clinic since 2006.
In contrast, district-hospital providers reported feeling that diabetes services were neglected by the district-hospital management and the district health authority compared with HIV or tuberculosis services, which had designated district coordinators, clinics and staff.
…….But for TB there is a designated section, designated doctor who deals with TB, if you leave that on the side of the district, there is a designated person who goes round the district dealing with TB. And HIV the same thing, there is coordinators of HIV who goes round the district. This is why am saying these diseases I see are arranged (organized) in a better way. They are closely dealt with then follows other diseases like diabetes and hypertension which are taken like other diseases. (District hospital provider)
They said that diabetes patients visiting the district-hospital were exempt from any fees, including for drugs, as government policy prescribed.
Referral- and district-hospital providers perceived that strategic direction and targets for diabetes care from regional or district authorities were lacking, because they did not know any designated regional or district coordinators for diabetes, as there were for HIV or malaria. The district medical officer echoed those sentiments.
Theme 3: continuity of care and coordination of services
We explored the extent of continuity of care at three levels; within facilities, between different levels of facilities and at community level.
Continuity within health facilities
At the referral-hospital, patients were scheduled to return each month, with little flexibility to accommodate their needs.
R: “Yes every month we ask them to come back but of course ….some patients ask to return after two months because of the way life is (financial hardships). They have grounded reasons but our fear is that if they come after 2 months their condition will have deteriorated.”
I: “So what do you do with these patients?”
R: “…they have to follow the schedule.” (Referral-hospital provider)
Scheduling of follow-up visits for diabetes patients at the district-hospital depended on the clinician’s perception of their condition. District-hospital providers indicated that there was no organization of diabetes services within the facility, and that this inconvenienced patients who were sometimes sent from one provider to another before receiving care.
…I can schedule a patient to come on a certain day but on that day I am not stationed to see outpatients… If fortunately they find me it is fine I will serve them. If they don’t, I have to find another clinician for the patient… (District-hospital provider)
At the health centre and dispensary, providers perceived no obligation to provide diabetes care; monitoring of diabetes patients was usually based on providers’ assessment of the patients’ need and their willingness to help. At the health centre, e.g. clinicians had arranged to refill diabetes medication for two elderly patients out of sympathy, even though the facility did not routinely stock it. They did this by directly ordering the patients’ medication along with their routine medication orders, without contacting the referral diabetes clinic which had diagnosed and registered the patients.
On organization of care for patients with additional chronic diseases besides diabetes, referral-hospital providers reported serving patients with both diabetes and cardiovascular conditions for both conditions on the same visit, and using the same patient file and notebook, as confirmed by document review. Records also indicated that patients’ minor ailments were treated at the same time. However, this was not true for a combination of diabetes and HIV.
….you can find a good example say a patient with the problem of pressure that is raised but also is HIV positive and attends that HIV clinic. While there, they think his pressure that day as they saw it (is very high), he needs to get immediate consultation. They will tell him “please go there at the (blood) pressure clinic before you go home.” But if his (blood) pressure is not raised they allow him to go home and tell him to attend the (blood) pressure clinic on the scheduled day and so the patient will come on the scheduled day. (Referral-hospital provider)
Furthermore, both referral- and district-hospital providers said they did not trace patients who failed to return for scheduled visits. At the referral-hospital, providers acknowledged the importance of tracing patients who had missed their visits but perceived limitations in financial means, staff numbers, and long distances involved for some patients. At the district hospital, they could not identify who had missed scheduled visits, as these were not systematically recorded. Providers did not seem aware of opportunities for tracing patients—for instance, through community-based care providers who traced HIV patients at both the district- and referral-hospitals.
Continuity between different-level facilities
According to providers, linkages between different levels of facilities meant that providers referred suspected or known diabetes patients to a higher-level facility offering diabetes care. Thus, dispensary providers would always refer to district- or referral-hospitals, as health centres did not offer diabetes care. Most providers from all facility levels reported referral letters being written and given to diabetes patients, suspected or known, to present at the higher-level facility. However, they complained that they rarely received feedback on patient management from the higher-level facility. This feedback was considered very important for diabetes care because when the patient returned, the referring provider had to continue treating this patient and needed to know what had been done at the other facility. Whereas referrals from the health centre and dispensary were due to a lack of diagnostic or treatment services, referral- and district-hospital providers reported referring mainly patients with complications. However, at the district hospital a lack of supplies such as blood sugar testing supplies also prompted referrals.
……in that, a patient comes here you find I order the test (blood sugar) and they tell you there are no reagents in the laboratory. Now me, how do I help this patient when I don’t know his/her blood sugar level?………so you find on that basis only you arrive at a decision to tell the patient that I am writing for you a letter to go to another facility. (District-hospital provider)
Involvement of family and the community
Providers reported involvement of patients’ relatives—mainly close family members such as parents, children, spouses and siblings—in patient care, including escorting patients to facilities for appointments or when ill, or monitoring their adherence to lifestyle changes. This involvement was usually initiated by providers; sometimes by family members themselves. Providers involved relatives in discussions about lifestyle changes, and asked them to help patients adhere to the changes while at home. This appeared especially important for elderly patients including the occasional ones at the health centre.
Sometimes, an elderly patient comes. Now, getting these messages to him that he needs to do this and that for his health, you fail to understand each other especially if he came without any escort… (Referral-hospital provider)
…we sent for a family member to come with the patient and we told him about the situation of their relative (the patient) and we gave him education about how to ensure the patient was following instructions properly. (Health-centre provider)
No diabetes-related activity at community level was reported at any study facility. Referral-hospital providers reported the existence of a diabetes patients’ support group but stated they were not involved with it.
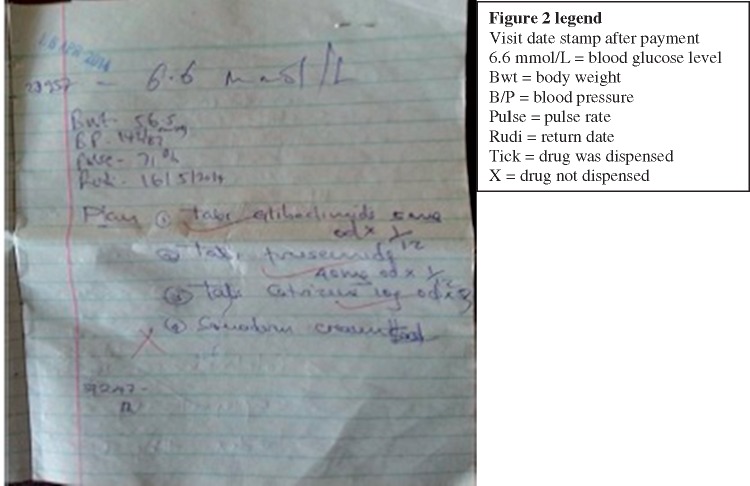
Theme 4: information systems and their use
Within the referral- and district-hospitals, according to providers, different outpatient service providers involved in a particular visit documented their interaction with the patient in a notebook which documented patients’ clinical information, some laboratory results, prescriptions and dispensation markings. Providers indicated that patients knew to bring this notebook; otherwise, patients would buy one at nearby vendors if the old one was full or forgotten.
Internal referrals at these two hospitals were made verbally by telephone or by writing in the notebooks or internal referral notes. At the referral-hospital, clinic-held patient files provided a back-up source of previous notes.
At both referral- and district-hospitals, the notes in the patient’s notebook and those in the clinic-held patient files at the referral-hospital were very brief and concerned the index visit, with little indication of a long-term plan of patient care except for the return date (Figure 2). The quote below illustrates how providers used these notes during consultation.
…and we (clinicians) compare fasting blood sugar that he had and the blood glucose level (measured today) and ask how is his progress, then we know what to do with him… (Referral-hospital provider)
Figure 2.
Entry into the patient booklet for one visit to the referral facility.
According to providers who also cared for admitted diabetes patients at the referral- and district-hospitals, patient notes were documented in separate inpatient files that were not linked to outpatient documentation. However, at the referral-hospital, discharged diabetes patients were directed to the diabetes clinic to book appointments.
The referral-hospital’s documentation system, according to observation, included a patient register, an appointment book, an attendance book, and the clinic-held patient files. However, referral-hospital providers reported that the information collected was not used in analysing patients’ response to management, identifying those who missed their appointments or tracking patients at their homes. At the district-hospital, aggregated diabetes information was captured along with other outpatient information on age and diagnosis among other variables in the paper-based health management information system (HMIS). Providers reported not using the information in any way.
Reports on diabetes care at referral- and district-hospitals consisted of patient numbers per time period. The clinic coordinator and provider handling diabetes information at the referral-hospital reported not using the reports but sending them to hospital managers. At the district-hospital, the 2012 annual report recorded only 11 diabetes patients being served as outpatients—which the provider handling information at the facility considered to be inaccurate. He also reported that the overall district reports were used mainly for planning at district level by the council health management team, which did not have any specific plans for diabetes care at the last planning period (2012/2013).
According to providers at the health centre and the dispensary, their HMIS recording did not include diabetes diagnosis because they could not make that diagnosis. A review of current HMIS records revealed no record of diabetes patients seen, even at the health centre where two patients had been treated earlier.
Theme 5: support self-management
Under this theme, we explored how providers perceived the support they gave patients to be able to manage their condition. Most referral- and district-hospital providers reported giving advice on lifestyle changes in diet, physical activity, medication use and clinic attendance for acute management and routine monitoring, despite feeling poorly skilled to do so. Some of them mentioned giving advice on foot care. For the occasional diabetes patients who presented at the health centre and dispensary, providers there only mentioned giving patients dietary information.
It emerged that providers at the same facility sometimes gave conflicting lifestyle messages, especially on diet—e.g. regarding the necessity of using ‘special’ foods that were actually not easily available to patients.
…Our foods that are common here are rice and maize meal but if you advise them on other foods they say they don’t have money although we usually advise them to eat sorghum meal but they say sorghum is expensive here and it is not available here so the big challenge is the food and how to get it. (Referral-hospital provider)
…and here I don’t advise the patient to use foods that are not in his surroundings — for example, asking a patient to use sorghum meal when there is no sorghum in his surroundings, maybe there is rice and potatoes so …the important thing is I tell him eat what you eat but one piece and the rest of the meal be vegetables that is little carbohydrates but from what is found around him. (Referral-hospital provider)
Overall no educational materials for diabetes patients were identified except at the referral-hospital. Here, there was a bundle of pamphlets in the local language without technical terms on self-management that included symptoms of high and low blood sugars and how patients could deal with both. The pamphlets were not government documents but had been developed for the referral-hospital with the support of well-wishers (external university). Only one provider recounted reading and giving them to patients.
And on top of advice I give them and read to them the pamphlet which are there (pointing to cupboard in nurses room). These help the patient to read for themselves because they are in simple Swahili but we have to ask the patient if they can read. If they cannot read we ask them to bring with them a relative who will help them to continue reading it at home as they learn together. (Referral hospital provider)
Some referral- and district-hospital providers recounted that they sometimes offered support on clinical decision-making regarding blood sugar results of tests done at home using personal blood sugar testing machines. The support was given either by telephone or during clinic visits.
At home, some patients know how to test themselves very well and sometimes you see him he has come and tells me man I see my blood sugar is refusing to come down I have tested twice but I cannot see what I am doing wrong… (District-hospital provider)
The majority of referral- and district-hospital providers reported that most diabetes patients did not return to the facilities for their routine monitoring and that those who returned commonly had uncontrolled blood sugar. This situation was associated with patients’ poor socio-economic status, poor comprehension, long distances to the health facilities, tendency to ignore lifestyle advice, and use of traditional medicines. Some providers expressed their wishes to have patient expenses minimized by subsidizing drug costs and by bringing diabetes services closer to patients, as they felt these practices could ease patients’ financial burden. Although they acknowledged patients’ difficulties, these providers said that they continued prescribing medication and giving information, hoping that patients would somehow solve their problems.
I: “So how do you help these patients?”
P: “…………… but now our ability to help is diminished when there are no drugs in the hospital, we cannot remove money from our pockets and buy for them the drugs. So we listen to them and write down what they should get, so that they can go and they may get help with their treatment there (elsewhere).” (District-hospital provider)
Discussion
This study has shown that the health centre and dispensary did not provide diabetes care. Diabetes services were centralized at the referral and district facilities, where the supply of necessary commodities was unreliable and health providers had some knowledge of what was expected of them but felt ill-prepared for diabetes care. Diabetes management was dominated by clinicians. We also found that district and facility level guidance and support were lacking and that continuity of care was broken within and between facilities. Furthermore, data on diabetes from the HMIS were inaccurate and unreliable for planning, and where they were available they were not used. Support for self-management for patients and their families was weak at all levels.
Service availability and leadership
The NPEHIT recommendations for dispensaries and health centres to provide diabetes-related promotive, preventive and some treatment services (United Republic of Tanzania Ministry of Health 2000) were not applied in our setting. Another Tanzanian study reported similar findings concluding that most services for NCDs were provided at hospital level (Peck et al. 2014). The fact that over 70% of Tanzanians live in rural areas and most rural health facilities are dispensaries (Ministry of Health and Social Welfare 2013) calls for decentralization of diabetes services to lower-level primary care facilities. This has been successfully done for HIV care and treatment services in rural LMIC settings (Bedelu et al. 2007). In rural, Ethiopia decentralization of diabetes services was reported to improve access to and utilization of the services (Watkins and Alemu 2003). The essential role of primary care services in the management of chronic diseases includes ensuring continuity of patient care and meeting the clinical needs of patients with less severe disease (Rothman and Wagner 2003). Whereas decentralization would improve access of services for rural populations, a financing mechanism that is reliable and affordable to rural populations for diabetes services and other chronic diseases is also required if universal health access and coverage are to be achieved in Tanzania (Mtei et al. 2014), as we found that financial barriers were perceived to be limiting service utilization. Financial barriers to diabetes service utilization have also been reported in a study from eastern Nigeria (Nwankwo et al. 2010). To this end, Nolte et al. (2003) propose that financing mechanisms for chronic diseases must minimize out-of-pocket payment by users, to improve involvement of patients in their own chronic care (Nolte and McKee 2008).
Despite the existence of a national NCD control unit (Metta et al. 2014), there was a lack of guidance for diabetes services in terms of strategies or targets from the regional or district level, which could partly explain the lack of a diabetes agenda in the 2012/13 district health plan. The situation is likely to be similar in other LMICs, most of which lacked a policy, strategy or action plan for diabetes control, making it unlikely for local-level health plans to include strategies and targets for diabetes care (WHO 2015). Without prioritizing diabetes services in the district plan, actions to improve access to and quality of these services at lower level health facilities cannot be supported. As is the case for HIV (Prime Minister's Office, United Republic of Tanzania 2013), ensuring that there are qualified responsible persons for diabetes and other NCDs services at regional, district and facility levels will create accountability for the quality of diabetes care in rural areas. Lack of guidance at the district-hospital led to failures in coordination and quality of services and inconvenience to patients, as there was no diabetes service coordinator and providers had no standard of diabetes service provision. With neither systems in place within facilities to use data to inform service adaptation nor policy direction on diabetes from the district level, providers had no means of adapting to the problems they encountered which could lead to inertia in diabetes services.
Human resources for health
The 2009 clinical practice guidelines for management of type 2 diabetes in Tanzania lists the minimum staffing requirement at primary health care diabetes services as a nurse, a village health worker (a form of community health worker), a medical doctor, a clinical officer or assistant medical officer and a diabetes educator (APHYTA 2009), envisioning a division of diabetes care functions among various cadres according to their training. Our findings suggest that availing this number and mix of cadres is unrealistic in this or other LMIC rural settings where the HRH crisis is worse (WHO 2006). Therefore, adaptation of strategies such as task-shifting may be reasonable for rural health facilities and may facilitate the decentralization of diabetes services to lower-level facilities. Tasks have been successfully shifted in decentralized HIV services in Tanzania, including in our district, and in diabetes and other NCD service provision in Ethiopia, Cameroon and South Africa (Mamo et al. 2007; Gill et al. 2008; Zachariah et al. 2009; Labhardt et al. 2010). However, to facilitate task-shifting for diabetes and other chronic disease services, the Tanzanian policy and legal environment will need to be reviewed, as a 2013 report found that policy and legal documents were silent on task-shifting (USAID 2013a).
Whereas it has been shown in other Tanzanian settings that health workers lacked knowledge on diabetes care (Peck et al. 2014), health providers in our study seemed to have some knowledge of what was expected of them but did not practice according to that knowledge. Although providers gave reasons for not performing tasks, such as financial and geographical constraints for not tracking patients, there seemed to be minimal effort to improve the services in terms of patient referral, patient recording and patient education practices, especially at the district-hospital.
These observations point to a know–do gap, which has also been demonstrated among reproductive and child health service providers in Tanzanian and is thought to exist across Africa among health workers in general (Soucat and Scheffler 2013). The know–do gap is associated with low levels of motivation and professionalism (Leonard and Masatu 2010). Motivation of workers determines their performance and their performance determines the quality of services they deliver (Dussault and Dubois 2003). In our setting, low motivation and lack of guidance to providers could be possible factors contributing to the performance limitations as there was no drive for providers to perform. Improving human resources management and assuring guidance and support in diabetes care at facility level could address the know–do gap and improve performance of health providers in rural settings (Soucat and Scheffler 2013).
Health information system, supplies management
Both population and facility-based information systems are crucial for patient and service management, monitoring and evaluation. Our findings show that the limitations of the existing HMIS in addressing chronic care needs include incoherent patient record keeping within facilities and poor linkage of patient information between the referring and the referral health facility. Such limitations have led to the design of disease-specific parallel information systems such as for HIV. However, this approach has further weakened the health system by disintegrating functions for specific diseases (National AIDs Control Programme [NACP], 2012). In Swaziland and Ethiopia, HIV-specific documentation tools and systems were adopted for diabetes care and rapidly improved the quality of diabetes care and treatment (Rabkin et al. 2012). This shows the similarity in information needs for chronic diseases; the opportunity is to integrate chronic disease information management. Additionally, information on diabetes patient load at facility level is necessary to meaningfully plan the services and supplies required. In our setting, high proportions of undiagnosed diabetes, poor access of diagnostic services and poor documentation at facilities may partly be responsible for the lack of reliable patient data. Studies in other LMICs have suggested that context-specific policies are needed to improve accessibility of essential medication for chronic diseases (Mendis et al. 2007). For rural Tanzania, these policies should address planning for supplies informed by reliable patient information and practices in timely commodity ordering and delivery mechanisms.
Study limitations and strengths
Although the rural district was selected partly for convenience, it was similar in health service structure and socio-economic profile to other Tanzanian rural districts (Ministry of Health and Social Welfare 2013). We enrolled mostly clinicians in this study, which limited the scope of health providers’ perceptions. This situation arose however, because non-clinician cadres were not involved in diabetes care in the public facilities we studies, hence felt uncomfortable and incompetent to discuss it. The ICCC framework had not been validated for our setting however, this was the only relevant framework we could identify and we used it to guide our exploration and map the situation in rural Tanzania. The study’s strength lies in triangulation of information by comparing findings from interviews, document reviews and observations.
Conclusion
This study has described providers’ perceptions and approaches in dealing with diabetes in a rural setting, which could be built on to strengthen health systems for chronic disease services like diabetes. We found that in the current health system, guidance and support must first be established in diabetes care, and management of health workers’ performance improved to address the know–do gap, to assure quality services. Furthermore, policies related to task-shifting and design of HMIS need to ensure that services are brought closer to people even in rural settings. As most chronic diseases have similar demands on health systems in rural facilities, an integrated approach to addressing diabetes care will strengthen the health system for diabetes and other chronic diseases in general.
Ethical approval
The study was approved by the institutional review boards of the Ifakara Health Institute (IHI) in Tanzania and the National Institute for Medical Research (NIMR/HQ/R8.a/vol IX/1459 (10/1/2013). Each respondent provided written consent to participate, except one who chose to consent verbally.
All authors have read and approved this manuscript in its current form.
Acknowledgements
This work was supported by the Netherlands Organization for International Co-operation in Higher Education (NICHE/TZA/005) and the Ifakara Health Institute, Tanzania.
Conflict of interest statement. None declared.
Footnotes
US$1 = 1631.5 Tanzania shillings in June 2013
References
- Ahren B. 1984. Diabetes mellitus at a rural hospital in northwestern Tanzania. Tropical and Geographical Medicine 36: 237–42. [PubMed] [Google Scholar]
- Alwan DA. 2010. Global Status Report of Non-Communicable Diseases 2010. Italy: WHO. [Google Scholar]
- APHYTA (Association of physicians of Tanzania). 2009. Clinical Practice Guidelines for Management of Type 2 Diabetes in Tanzania. Dar es Salaam, Tanzania: APHYTA. [Google Scholar]
- Beaglehole R, Bonita R, Alleyne G. et al. 2011a. UN high-level meeting on non-communicable diseases: addressing four questions. The Lancet 378: 449–55. [DOI] [PubMed] [Google Scholar]
- Beaglehole R, Bonita R, Horton R. et al. 2011b. Priority actions for the non-communicable disease crisis. The Lancet 377: 1438–47. [DOI] [PubMed] [Google Scholar]
- Beaglehole R, Epping-Jordan J, Patel V. et al. 2008. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. The Lancet 372: 940–9. [DOI] [PubMed] [Google Scholar]
- Bedelu M, Ford N, Hilderbrand K. et al. 2007. Implementing antiretroviral therapy in rural communities: the Lusikisiki model of decentralized HIV/AIDS care. Journal of Infectious Diseases 196: S464–8. [DOI] [PubMed] [Google Scholar]
- Dussault G, Dubois CA.. 2003. Human resources for health policies: a critical component in health policies. Human Resources for Health 1: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill G, Price C, Shandu D, Dedicoat M, Wilkinson D.. 2008. An effective system of nurse‐led diabetes care in rural Africa. Diabetic Medicine 25: 606–11. [DOI] [PubMed] [Google Scholar]
- Kaguruki G. 2015. Tanzania STEPs Survey on Non-Communicable diseases and Risk Factors: 2012, personal communication, 1st July 2015. Unpublished document.
- Kavishe B, Biraro S, Baisley K. et al. 2015. High prevalence of hypertension and of risk factors for non-communicable diseases (NCDs): a population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Medicine 13: 126.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolling M, Winkley K, Von Deden M.. 2010. For someone who's rich, it's not a problem. Insights from Tanzania on diabetes health-seeking and medical pluralism among Dar es Salaam's urban poor Research. Globalization and Health 6: 8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labhardt ND, Balo JR, Ndam M. et al. 2010. Task shifting to non-physician clinicians for integrated management of hypertension and diabetes in rural Cameroon: a programme assessment at two years. BMC Health Services Research 10: 339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard KL, Masatu MC.. 2010. Professionalism and the know‐do gap: exploring intrinsic motivation among health workers in Tanzania. Health Economics 19: 1461–77. [DOI] [PubMed] [Google Scholar]
- Maher D, Ford N, Unwin N. et al. 2012. Priorities for developing countries in the global response to non-communicable diseases. Globalization and Health 8: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamo Y, Seid E, Adams S, Gardiner A, Parry E.. 2007. A primary healthcare approach to the management of chronic disease in Ethiopia: an example for other countries. Clinical Medicine 7: 228–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MCLarty D, Unwin N, Kitange H, Alberti K.. 1996. Diabetes mellitus as a cause of death in sub‐Saharan Africa: results of a community‐based study in Tanzania. Diabetic Medicine 13: 990–5. [DOI] [PubMed] [Google Scholar]
- Mendis S, Fukino K, Cameron A. et al. 2007. The availability and affordability of selected essential medicines for chronic diseases in six low-and middle-income countries. Bulletin of the World Health Organization 85: 279–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metta E, Bailey A, Kessy F. et al. 2015. “In a situation of rescuing life”: meanings given to diabetes symptoms and care-seeking practices among adults in Southeastern Tanzania: a qualitative inquiry. BMC Public Health 15: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metta E, Msambichaka B, Mwangome M. et al. 2014. Public policy, health system, and community actions against illness as platforms for response to NCDs in Tanzania: a narrative review. Global Health Action 7: 23439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Finance, United Republic of Tanzania. 2013. The 2012 Population and Housing Census: Population Distribution by Administrative Areas. Dar es Salaam: National Bureau of Statistics. [Google Scholar]
- Ministry of Health and Social Welfare. 2013. Tanzania Service Availability and Readiness Assessment Report 2012. Dar Es Salaam: Ministry of Health and Social Welfare. [Google Scholar]
- Mtei G, Makawia S, Masanja H.. 2014. Monitoring and evaluating progress towards universal health coverage in Tanzania. PLoS Medicine 11: e1001698.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mubyazi GM. 2008. The Tanzanian Policy on Health-care fee waivers and exemptions in practice as compared with other developing countries: evidence from recent local studies and international literature. East African Journal of Public Health 1: 11–7. [Google Scholar]
- Munga M, Maestad O.. 2009. Measuring inequalities in the distribution of health workers: the case of Tanzania. Human Resources for Health 7: 4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National AIDs Control Programme. 2012. NationalguidelinesforthemanagementofHIVandAIDs. United Republic of Tanzania, Ministry of Health and Social Welfare, 4th edn. Dar Es Salaam: National AIDs Control Programme. [Google Scholar]
- National Bureau of Statistics. 2004. The Regional and District Census Data in Brief. Dar es Salaam: Ministry of Finance. [Google Scholar]
- National Bureau of Statistics. 2011. Tanzania Demographic and Health Survey 2010. Dar es Salaam: Ministry of Finance. [Google Scholar]
- Nolte E, McKee M.. 2008. Caring for people with chronic conditions: a health system perspective. UK: McGraw-Hill Education (UK) http://www.euro.who.int/__data/assets/pdf_file/0006/96468/E91878.pdf, accessed 15 April 2016 [Google Scholar]
- Nwankwo CH, Nandy B, Nwankwo BO.. 2010. Factors influencing diabetes management outcome among patients attending government health facilities in South East, Nigeria. International Journal of Tropical Medicine 5: 28–36. [Google Scholar]
- Oni T, McGrath N, Belue R. et al. 2014. Chronic diseases and multi-morbidity—a conceptual modification to the WHO ICCC model for countries in health transition. BMC Public Health 14: 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peck R, Mghamba J, Van Obberghen F. et al. 2014. Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: a cross-sectional survey. The Lancet Global Health 2: e285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime Minister's Office, United Republic of Tanzania. 2013. Tanzania's Third National Multi-Sectoral Framework on HIV/AIDs: 2013/14 to 2017/18. Dar es Salaam: Prime Minister's Office, United Republic of Tanzania. [Google Scholar]
- Rabkin M, Melaku Z, Bruce K. et al. 2012. Strengthening health systems for chronic care: leveraging HIV programs to support diabetes services in Ethiopia and Swaziland. Journal of Tropical Medicine 2012: 137460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabkin M, Nishtar S.. 2011. Scaling up chronic care systems: leveraging HIV programs to support noncommunicable disease services. Journal of Acquired Immune Deficiency Syndrome 57: S87–90. [DOI] [PubMed] [Google Scholar]
- Ramadhani A, Ramaiya A, Mtenga S. et al. 2014. MZIMA: Longitudinal Cohort Study Progress Report. Serosurvey Round 1 June 2012 – May 2013 [Online]. Dar es Salaam: http://digitallibrary.ihi.or.tz/2872/1/LONGITUDINAL_COHORT_STUDY.pdf, accessed 7 August 2015. [Google Scholar]
- Ramaiya K. 2005. Personal view: Tanzania and diabetes—a model for developing countries? BMJ: British Medical Journal 330: 679. [Google Scholar]
- Rothman AA, Wagner EH.. 2003. Chronic illness management: what is the role of primary care? Annals of Internal Medicine 138: 256–61. [DOI] [PubMed] [Google Scholar]
- Sheri Pruit SA, Epping-Jordan JA, Jesus M. et al. 2002. Innovative Care for Chronic Conditions: Building Blocks for Action. Geneva: Noncommunicable diseases and Mental Health, WHO. [Google Scholar]
- Soucat A, Scheffler R.. 2013. The Labor Market for Health Workers in Africa: A New Look at the Crisis. Washington, DC: World Bank Publications [Google Scholar]
- Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission, National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF International. 2013. Tanzania HIV/AIDS and Malaria Indicator Survey 2011-12. Dar es Salaam, Tanzania: TACAIDS. [Google Scholar]
- United Republic of Tanzania. 2008. Health Sector Strategic Plan III for 2009 - 2015: Partnership for delivering MDGs. Dar Es Salaam: URT. [Google Scholar]
- United Republic of Tanzania. 2014. Human Resource for Health and Social Welfare Strategic Plan 2014 - 2019. Dar Es Salaam, Tanzania: URT. [Google Scholar]
- United Republic of Tanzania. 2015. Health Sector Strategic Plan IV July 2015 – June 2020: Reaching all households with quality health care. Dar es Salaam: URT. [Google Scholar]
- United Republic of Tanzania, Ministry of Health. 2000. National Package of Essential Health Interventions in Tanzania. Dar Es Salaam: URT. [Google Scholar]
- USAID. 2013a. Health Policy Initiative in Tanzania: End-Of-Project Report (2009–2013). Dar es Salaam, Tanzania: USAID. [Google Scholar]
- USAID. 2013b. USAID/Tanzania Health Systems Strengthening Strategy 2013-2018 https://www.usaid.gov/sites/default/files/documents/1860/USA ID%20TZ%20HSS%20Strategy%20Sept%2030%20FINAL.pdf, accessed 20 April 2016.
- Van Olmen J, Scheillevis F, Van Damme W. et al. 2012. Management of chronic diseases in sub-Saharan Africa: cross-fertilisation between HIV/AIDS and diabetes care. Journal of Tropical Medicine 2012: 349312.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins P, Alemu S.. 2003. Delivery of diabetes care in rural Ethiopia: an experience from Gondar. Ethiopian Medical Journal 41: 9–17. [PubMed] [Google Scholar]
- Whiting DR, Guariguata L, Weil C, Shaw J.. 2011. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Research and Clinical Practice 94: 311–21. [DOI] [PubMed] [Google Scholar]
- Whiting DR, Hayes L, Unwin NC.. 2003. Challenges to health care for diabetes in Africa. European Journal of Cardiovascular Risk 10: 103–10. [DOI] [PubMed] [Google Scholar]
- WHO 2006. The World Health Report: 2006: Working Together for Health http://apps.who.int/iris/handle/10665/43432, accessed 16 April 2016.
- WHO. 2012. STEPwise approach to chronic disease risk factor surveillance, Tanzania [Online]. WHO. http://www.who.int/chp/steps/UR_Tanzania_FactSheet_2012.pdf, accessed 1 December 2013.
- WHO. 2013. Global Action Plan: For the Prevention and Control of Non-Communicable Disease 2013-2010 [Online]. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf, accessed 21 April 2016.
- WHO. 2014. Noncommunicable Diseases (NCD) Country Profiles, 2014. [Online]. http://www.who.int/nmh/countries/tza_en.pdf?ua=1, accessed 30 October 2014.
- WHO. 2015. Global Health Observatory Data Repository [Online]. http://apps.who.int/gho/data/node.main.A907?lang=en, accessed 15 April 2016.
- Zachariah R, Ford N, Philips M. et al. 2009. Task shifting in HIV/AIDS: opportunities, challenges and proposed actions for sub-Saharan Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene 103: 549–58. [DOI] [PubMed] [Google Scholar]