Abstract
Background:
The safest and most effective technique for anterior cruciate ligament (ACL) reconstruction in skeletally immature patients is currently unknown.
Purpose:
To evaluate the functional and patient-reported outcomes of a specific all-epiphyseal ACL reconstruction technique in which the graft, bone tunnels, and fixation do not cross the knee growth plates.
Study Design:
Case series; Level of evidence, 4.
Methods:
Twenty-seven patients (23 boys, 4 girls; mean age, 11 years; range, 8-15 years) underwent an all-epiphyseal ACL reconstruction with a single femoral transverse epiphyseal tunnel and primarily split tibial epiphyseal tunnels. Outcomes were evaluated in terms of the manual Lachman test, range of motion, pain, return to activity, angular or leg-length deformity on imaging, and International Knee Documentation Committee (IKDC) or Pedi-IKDC score an average of 3.8 years postoperatively, with a minimum 2-year follow-up.
Results:
The mean IKDC score was 94 ± 11. There were no growth arrests, but 3 patients had knee overgrowth, and 2 required a subsequent guided growth procedure. The ACL graft failed in 4 patients (15%), and 2 patients had contralateral ACL tears (7%). There were 5 subsequent ipsilateral meniscal tears, 4 of which were retears of a repaired meniscus. Ipsilateral knee reinjury significantly correlated with the number of associated injuries at the time of index surgery (P = .040) and the number of sports played (P = .029).
Conclusion:
All-epiphyseal ACL reconstruction resulted in excellent long-term functional outcomes, despite a high rate of complications (48%) and secondary procedures (37%) in this highly active cohort. The incidence of graft failure was similar to other standard ACL reconstruction techniques for patients younger than 20 years.
Keywords: ACL, pediatric sports medicine, all-epiphyseal, reconstruction, growth plate, physis
The safest and most effective surgical treatment for very young athletes with anterior cruciate ligament (ACL) tears is yet to be determined. In children with ACL tears who return to sport without reconstruction, outcomes are very poor, with some osteoarthritic (OA) changes in the decades after initial injury.1,3,10,14,23 These poor outcomes and early onset of OA are understandable in ACL-deficient youths who desire to be highly active but have recurrent instability episodes and meniscal and articular cartilage damage.3 While a substantial proportion of pediatric patients who tear their ACL sustain a meniscal tear,24 delaying ACL reconstruction appears to increase the incidence of meniscal tears10,23 or may cause a repairable meniscus tear to become irreparable. Concomitant meniscus damage with ACL-injured patients worsens outcomes relative to ACL-injured patients with intact menisci; however, the combination of meniscal damage with insufficient ACL stability in active youth likely drives the worst scenario for long-term outcomes.20,31,34
Several studies have emphasized the need for early treatment in skeletally immature athletes to minimize episodes of instability that can lead to meniscal and articular cartilage damage.9,13,15 However, an adult-style ACL surgery with a graft and tunneling across a child’s open growth plates can tether or arrest growth.6,11,15 Anderson2 pioneered an anatomic transepiphyseal technique for pediatric ACL reconstruction with a femoral epiphyseal tunnel with femoral epiphyseal suspensory fixation and a tibial epiphyseal tunnel with tibial metaphyseal post fixation. All-epiphyseal techniques of anatomic ACL reconstruction were developed to completely avoid drilling through or tethering the knee growth plates, placing the graft and its fixation all within the epiphysis of both the femur and tibia. Currently, there are no clinical results published on the postoperative outcomes and complications of all-epiphyseal ACL surgery with greater than 2 years minimum follow-up. The purpose of this study was to report on the functional and patient-reported outcomes as well as complications of an all-epiphyseal ACL reconstructive technique in skeletally immature patients.
Methods
Sample Selection
Informed consent was waived for this retrospective study. A medical records search identified consecutive patients who had an all-epiphyseal ACL reconstruction for an ACL tear and a minimum 2-year follow-up. Routine bone age assessments were performed prior to surgery to confirm skeletal immaturity. All-epiphyseal ACL reconstruction was indicated in children with at least 2 years of growth remaining based on radiographic bone age.10 Surgeries were performed by 2 pediatric orthopaedic surgeons specializing in sports medicine at a single institution between 2006 and 2012. Characteristics of the patient sample are reported in Table 1.
TABLE 1.
Clinical Presentation of Anterior Cruciate Ligament Tears in Skeletally Immature Patients
| Sample Characteristics | n (%) |
|---|---|
| Patients | 27 (100) |
| Sex | |
| Male | 23 (85) |
| Female | 4 (15) |
| Laterality | |
| Right | 16 (59) |
| Left | 11 (41) |
| Athletes | 25 (93) |
| Mechanism of injury | 27 (100) |
| Football | 9 (33) |
| Soccer | 5 (19) |
| Basketball | 3 (11) |
| Bicycle | 2 (7) |
| Motorized vehicle | 2 (7) |
| Other | 6 (22) |
| Associated injuries | 13 (48) |
| Lateral meniscus tear | 8 (30) |
| Medial meniscus tear | 3 (11) |
| Tibial plateau (Segond) fracture | 2 (7) |
| Medial collateral ligament tear | 1 (4) |
| Patella fracture | 1 (4) |
| Preoperative physical examination | |
| Positive Lachman test | 27 (100) |
| Pain | 21 (78) |
| Swelling | 20 (74) |
| Effusion | 19 (70) |
| Instability | 15 (56) |
| Popping | 10 (37) |
| Valgus | 2 (7) |
| Leg-length discrepancy | 0 (0) |
| Preoperative Characteristics | Mean ± SD (Range) |
| Chronological age, y | 11.4 ± 1.9 (8.5-15.3) |
| Bone age, y | 11.8 ± 1.8 (8.5-14.0) |
| Height, cm | 148 ± 12 (130-172) |
| Weight, kg | 45 ± 13 (29-76) |
| Body mass index, kg/m2 | 20.3 ± 3.9 (14.5-33.9) |
| Knee flexion, deg | 123 ± 24 (70-140) |
| Knee extension, deg | 3 ± 4 (0-10) |
Surgical Technique
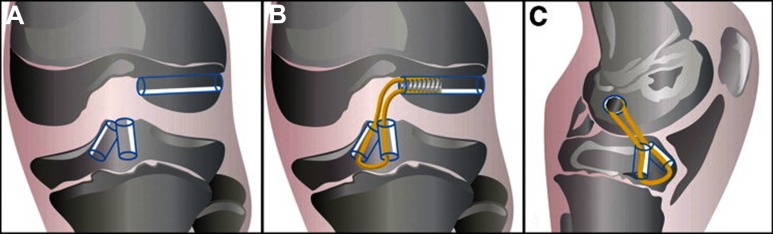
Patients were treated with an all-epiphyseal ACL reconstruction technique with quadruple-hamstring tendon graft, as described by Lykissas et al21 (Figure 1). Hamstring tendons were harvested, doubled, and sewn side-by-side with the thinner proximal end of the gracilis attached to the thicker distal end of the semitendinosus. The doubled free ends of the graft were approximately 4.5 to 5.5 mm in diameter. Tendons were tensioned at 15 pounds of force on a graft board. A 2- to 3-mm notchplasty was performed in 25 patients (93%), leaving the stumps of the ACL for anatomic reference.
Figure 1.
The modified all-epiphyseal anterior cruciate ligament reconstruction technique. (A) A femoral tunnel and split tibial tunnel are placed entirely within the distal femoral and proximal tibial epiphysis, respectively. (B) A biocomposite interference screw is used to fix the graft into the femoral tunnel. A 1-cm cortical bone bridge between the 2 tibial tunnels is maintained. (C) Correct position of the femoral tunnel in the lateral plane with the looped end of the graft around the anteromedial tibial epiphysis. Reprinted with permission from Lykissas et al.21
Next, the femoral tunnel guide pin was placed outside-in either freehand via the technique described by Anderson2 or with a posterior cruciate ligament guide (Femoral PCL Marking Hook; Arthrex) placed through the lateral infrapatellar portal with the scope view through the medial portal. Fluoroscopy (anteroposterior and lateral) confirmed that the pin tip was in the ACL footprint and was at least 4 to 5 mm distal to the growth plate.
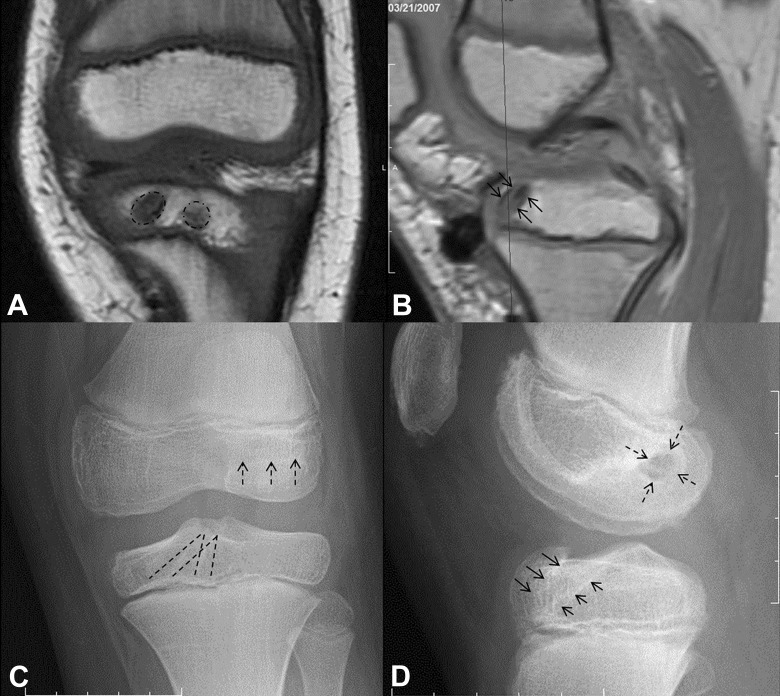
Under lateral fluoroscopy, split (double) tibial tunnels were created within the epiphysis in 24 of 27 patients, with a median split tunnel size of 5 mm (range, 4-6 mm) (Figure 2, A-D). Looping the graft over the cortical bone bridge between the split tunnels in the tibia provided rock solid graft fixation and smaller diameter tunnels in the thin tibial epiphysis versus a single tunnel. Three patients had a single tibial epiphyseal tunnel ranging from 7 to 9 mm in diameter. One of the split tibial tunnels was drilled at the medial border of the patellar tendon and the other approximately 10 mm more medial to the first tunnel, with both tunnels converging into the tibial ACL footprint (Figure 1A). Initially, the tunnels were drilled freehand, and later, they were drilled using a tibial guide (Acufex Director Drill Guide; Smith & Nephew). With the split tibial tunnel technique, initially the 2 doubled free ends of the graft were pulled together into the knee via the single femoral tunnel (median, 7 mm; range, 6-9 mm), and the free ends were then separated and pulled out of the knee through the 2 split tibial tunnels. The doubled free ends of the graft were tied in a square knot over the tibial epiphyseal bone bridge and oversewn with No. 2 fiberwire suture. The femoral side was fixed via the technique of Anderson2 with an ENDOBUTTON (Smith & Nephew) and washer or an XTENDOBUTTON (Smith & Nephew) (n = 14). In our current variation of the technique, we draw the doubled free ends of the graft up through split tibial tunnels, which join together in the notch to become a quadruple graft, and the 4 strands exit the notch through the single femoral tunnel via the technique described by Lykissas et al.21 We fixate the graft in the tunnel using an outside-in placed, 25- to 30-mm-long biocomposite screw (Genesys Matryx Interference Screw; ConMed Linvatec) of a diameter the same size as the tunnel diameter (n = 11) (Figure 1, B and C). Two patients were treated with an ENDOBUTTON on the femoral side and screw fixation on the tibial side. Other procedures performed during the index ACL surgery were lateral meniscus repair (n = 4), medial meniscus repair (n = 2), and partial lateral meniscectomy (n = 2). Three meniscal tears were left alone due to small size and stability on probing.
Figure 2.
(A and B) Magnetic resonance image of the knee in a 10-year-old boy who underwent a split tibial tunnel all-epiphyseal anterior cruciate ligament (ACL) reconstruction showing the tight fit in the thin proximal tibial epiphysis. (A) The dashed circles on the coronal view mark the 2 split tibial tunnels. (B) The arrows on the lateral view mark 1 of the split tibial tunnels. The split tibial tunnels have a smaller diameter than a single tunnel, usually 4.5 to 5.5 mm for each split tunnel compared with 7 to 8 mm for a single tunnel. (C and D) Radiographs of an 8-year-old boy who underwent a split tibial tunnel all-epiphyseal ACL reconstruction at 2.5 years after surgery. (C) On the anteroposterior radiograph, the dashed arrows mark the inferior edge of the horizontal femoral tunnel, and the dashed lines mark the edges of the split tibial tunnel. (D) On the lateral radiograph, the dashed arrows mark the edges of the femoral tunnel, and the solid arrows mark the edges of the split tibial tunnels, which overlap on this view.
Postoperatively, patients were placed in a simple knee immobilizer and allowed to bear weight as tolerated. After 1 week, the immobilizer was discontinued, and physical therapy was started. Crutches were typically discontinued at 2 to 4 weeks postoperatively when the patient had regained knee extension, adequate quadriceps strength, and good balance and gait. Return to sports was allowed approximately 6 to 9 months postoperatively after the patient had regained 85% to 90% strength symmetry on Biodex (Biodex Medical Systems) testing and passed hop and agility tests.
Outcome Measures
We report the manual Lachman and pivot shift test results of each patient at their final postoperative clinical visit. Parent-/patient-reported functional outcomes included either the International Knee Documentation Committee Subjective Knee Form (IKDC)12 or its pediatric version, known as the Pedi-IKDC.17 The Pedi-IKDC is a modification of the adult IKDC with questions that are appropriately worded for children aged 10 to 18 years. A recent study showed that the Pedi-IKDC and the IKDC had statistically similar scores when administered to a group of adolescent patients with knee injuries.28 The Pedi-IKDC questionnaire was mailed to eligible patients, and if they did not return the questionnaire or opt out of the study within 2 weeks, then they were called and invited to complete the questionnaire over the phone. For patients who did not complete the Pedi-IKDC by mail or over the phone, their clinical IKDC scores were used, as the IKDC questionnaire is routinely completed by patients during clinic as part of standard care.
Statistical Analyses
Descriptive statistics were used to characterize the sample. Multivariable logistic regressions were performed with age, sex, sports activity, time to surgery, and associated injury combined in the same analysis as predictors of the dichotomous outcomes of having an associated injury or not or having a reinjury or not. Multivariable linear regression was used to determine whether these same factors predicted Pedi-IKDC/IKDC scores. Pedi-IKDC/IKDC scores were compared between fixation approaches and patients with and without reinjury using Mann-Whitney tests, with medians and interquartile ranges reported.
Results
Functional Outcomes
Twenty-seven patients underwent all-epiphyseal ACL reconstruction on average 4.4 ± 6.2 months (range, 0.6-33.2 months) after a primary ACL tear. Twenty-one patients (75%) had clinical follow-up a mean 3.6 ± 1.4 years (range, 2.0-6.6 years) after surgery. All patients achieved full extension and had within 5 degrees of full flexion (mean, 139° ± 2°; range, 135°-140°). Seventeen of 21 patients (81%) returned to sports and recreational activities, and 14 of 21 patients (67%) had no pain. Twelve of 21 patients (57%) had returned to sports and recreational activities with no pain and full flexion and extension.
A total of 22 complications occurred in 13 of 27 patients (48%) (Table 2). There were 9 reinjuries, including 3 ACL retears, 1 lax ACL graft, and 5 meniscal tears (1 new medial tear, 4 retears; 3 lateral, 2 medial). All 4 ACL graft failures occurred within 1.5 years after the initial surgery and required a revision all-epiphyseal ACL reconstruction. There were no cases of bony growth arrest or bone undergrowth. Although no patients exhibited growth arrest, overgrowth was identified in 3 patients. One patient showed 2 cm of limb overgrowth on the operative side 2 years after surgery that spontaneously resolved by 5.3 years. Another patient developed 2.7 cm of limb overgrowth, likely related to surgical stimulation near the growth plate, which necessitated a percutaneous screw hemiepiphysiodesis 4.3 years after surgery. Based on Moseley’s graph, this patient was projected to correct down to a 5-mm leg-length discrepancy by skeletal maturity.27 The third patient developed 2 cm of limb overgrowth and experienced progressive valgus bilaterally, which was greater on the operative side due to proximal medial tibial overgrowth (Figure 3). This patient was noted to have ossification of the proximal medial periosteum just 1 month after her ACL injury (Figure 3, A-D), which appears to have initiated progressive valgus that increased after her ACL surgery that she underwent 10 months later (Figure 3E). This patient was initially treated with bilateral distal femur-guided growth, but correction was incomplete on the surgical side at skeletal maturity, and she underwent an ipsilateral open wedge proximal tibial osteotomy. Her leg-length discrepancy had resolved after 5 years, but she became obese and continued to have pain, mild symmetric residual genu valgum, and reported the worst Pedi-IKDC/IKDC score of 49. We believe that elevating her hamstring tendons off of the proximal tibia with a periosteal flap during her ACL autograft harvest exacerbated her preoperative valgus overgrowth. Two patients had notch impingement, which presented as loss of knee extension requiring repeat notchplasty. Two patients had postoperative skin infections, including a stitch reaction and a rash with pain and discoloration. One patient with trochlear dysplasia suffered recurrent patellar dislocations and was treated with a medial patellofemoral ligament reconstruction. One patient had a nondisplaced lateral femoral condyle impaction fracture (unrelated to femoral bone tunnel) and a lateral meniscus tear 3.2 years after the initial surgery that was left untreated. The functional and patient-reported outcomes of these patients with complications can be found in Table 3. Two patients (7%) had injuries to the contralateral knee, including 2 ACL tears and 1 meniscus tear (Table 2). Two of the 3 patients with a single tibial tunnel reinjured their knee (ACL retear and medial meniscus retear). Patients who received an ENDOBUTTON had a mean follow-up of 4.87 years (range, 3.4-5.9 years), while patients with an interference screw had a mean follow-up of 3.43 years (range, 2.0-6.6 years). Seven of 14 patients (50%) with ENDOBUTTON femoral fixation reinjured their knee and required additional procedures, whereas only 2 of 11 patients (18%) with an interference screw for femoral fixation reinjured their knee and required additional procedures. Neither of the 2 patients with both an ENDOBUTTON and screw fixation suffered reinjury.
TABLE 2.
Complications and Additional Proceduresa
| n (%) | |
|---|---|
| Complications | 13 (48) |
| ACL retear | 3 (11) |
| Lax ACL graft | 1 (4) |
| Leg-length discrepancy (≥2 cm) | 3 (11) |
| Lateral meniscus tear | 3 (11) |
| Medial meniscus tear | 2 (7) |
| Notch impingement | 2 (7) |
| Hardware displaced/prominent | 2 (7) |
| Postoperative skin infection | 2 (7) |
| Patellar dislocation | 1 (4) |
| Lateral femoral condyle fracture | 1 (4) |
| Genu valgum | 1 (4) |
| Additional procedures | 10 (37) |
| Revision surgery | 4 (15) |
| Notchplasty | 2 (7) |
| Lateral meniscus repair | 1 (4) |
| Medial meniscus repair | 1 (4) |
| Knee hemiepiphysiodesis | 1 (4) |
| Distal femur epiphysiodesis | 1 (4) |
| MPFL reconstruction | 1 (4) |
| Proximal tibial lateral opening wedge osteotomy | 1 (4) |
| Contralateral knee injuries | 2 (7) |
| ACL tear | 2 (7) |
| Meniscus tear | 1 (4) |
aACL, anterior cruciate ligament; MPFL, medial patellofemoral ligament.
Figure 3.
Knee radiographs of a 9-year-old girl with an anterior cruciate ligament (ACL) tear show proximal tibial bone spur formation (arrow), which appeared preoperatively from (A) the time of injury to (B) 1 week, (C) 1 month, and (D) 8 months later, prior to split tibial tunnel all-epiphyseal ACL reconstruction. (E) Immediate postoperative and (F) 2-year follow-up anteroposterior knee radiographs show increasing bilateral genu valgum. (G) Two-year follow-up anteroposterior lower extremity radiograph shows bilateral genu valgum, which was treated with bilateral hemiepiphysiodesis. (H) At 3.7 years, radiographs continue to show genu valgum and development of a leg-length discrepancy, which was treated with a proximal tibial lateral opening wedge osteotomy. (I) At 5 years, her genu valgum had improved and her leg-length discrepancy had resolved.
TABLE 3.
Characterization of Patients With Complications After All-Epiphyseal ACL Reconstructiona
| Patient | Sex | Age, y | BMI, kg/m2 | Associated Injuries | Concomitant Procedure | Complication(s) | Additional Procedures | Years to Follow-up | Pedi-IKDC/IKDC Score | Clinical Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 13.7 | 20.0 | Medial meniscus tear, Segond fracture | Medial meniscus repair |
|
Medial meniscus repair at 2.5 y | 3.4 | — | No RTS, pain, full ROM at 3.5 y |
| 2 | Male | 8.7 | 17.5 | None | None | ACL retear on femoral side at 3.1 y | ACL revision at 3.3 y | 6.6 | 100 at 6.6 y | RTS, no pain, full ROM at 6.6 y |
| 3 | Male | 10.6 | 17.2 | None | None | Notch impingement at 6 wk | Notchplasty at 6 wk | 5.2 | 100 at 5.2 y | — |
| 4 | Male | 11.7 | 16.5 | Lateral meniscus tear | None |
|
MPFL reconstruction at 4.2 y | 5.9 | RTS, no pain, lacks 5° of flexion, mild varus at 5.9 y | |
| 5 | Male | 9.5 | 21.5 | None | None |
|
Notchplasty at 1.6 y ACL revision at 3.1 y | 5.1 | 87 at 5.1 y | No RTS, pain, full ROM at 4.2 y |
| 6 | Male | 9.4 | 19.4 | Lateral meniscus tear | None |
|
Distal femur epiphysiodesis at 4.3 y | 4.5 | 87 at 3.5 y | RTS, no pain, full ROM, 2.7-cm leg length deformity at 4.5 y |
| 7 | Female | 11.1 | 19.9 | Lateral meniscus tear | Partial lateral meniscectomy |
|
ACL revision, hardware removal at 1.5 y | 4.8 | 87 at 3.7 y | RTS, pain, full ROM at 4.8 y |
| 8 | Female | 10.0 | 33.9 | Lateral meniscus tear, medial collateral ligament tear, Segond fracture | Partial lateral meniscectomy | 2-cm leg length deformity at 2.1 y | Hemiepiphysiodesis at 2.3 y Proximal tibia osteotomy, hardware removal at 3.7 y | 4.9 | 49 at 4.1 y | RTS, pain, lacks 5° of extension, valgus at 4.9 y |
| 9 | Female | 9.3 | 14.5 | Anterior tibia subluxation | None | 2-cm leg length discrepancy at 2 y | None | 5.3 | 100 at 4.2 y | RTS, pain, full ROM at 5.3 y |
| 10 | Male | 11.8 | 18.7 | Lateral meniscus tear | Lateral meniscus repair | Lateral meniscus retear at 2.6 y | Lateral meniscus repair at 2.8 y | 4.7 | 93 at 4.7 y | RTS, no pain at 4.7 y |
| 11 | Male | 8.5 | 21.8 | None | None | Suture abscess at 2 wk | None | 2.8 | — | RTS, pain, full ROM, valgus at 2.8 y |
| 12 | Male | 13.2 | 22.2 | Lateral meniscus tear | Lateral meniscus repair | ACL retear from tibial side at 1.8 y | ACL revision at 1.8 y | 2.3 | 100 at 2.2 y | Not RTS, no pain, full ROM at 2.2 y |
| 13 | Male | 14.3 | 22.4 | None | None | Calf/ankle pain, discoloration, rash at 1 wk | None | 2.0 | 93 at 2.0 y | Not RTS, no pain, full ROM at 2.0 y |
aACL, anterior cruciate ligament; BMI, body mass index; IKDC, International Knee Documentation Committee; MPFL, medial patellofemoral ligament; Pedi-IKDC, pediatric version of the IKDC; ROM, range of motion; RTS, returned to sports.
Waiting longer to have surgery did not increase the likelihood of having an associated injury (P = .27) (Table 4). However, patients with an associated injury at the time of index ACL surgery were more likely to reinjure their knee, regardless of age, sex, sports activities, and time to surgery (P = .040) (Table 4). Patients who participated in a greater number of sports were also more likely to reinjure their knee, regardless of age, sex, time to surgery, and associated injuries (P = .029) (Table 4).
TABLE 4.
Prognotistic Factors of All-Epiphyseal Anterior Cruciate Ligament Reconstruction Outcomesa
| Associated Injury, β (P) | Reinjury, β (P) | Pedi-IKDC/IKDC Score, β (P) | |
|---|---|---|---|
| Age | 0.36 (.21) | −0.35 (.35) | 0.06 (.97) |
| Sex | −24.54 (>.99) | 4.37 (.080) | −10.06 (.19) |
| No. of sports | 0.13 (.77) | 1.84 (.029)b | 1.77 (.37) |
| Time to surgery | −0.51 (.27) | 0.04 (.81) | −0.06 (.86) |
| Associated injury | — | –3.81 (.040)b | –5.30 (.34) |
aIKDC, International Knee Documentation Committee.
bStatistically significant (P < .05).
Patient-Reported Outcomes
Twenty-three patients (85%) completed either the Pedi-IKDC (n = 10) or IKDC (n = 13) an average of 3.8 ± 1.3 years (range, 2.0-6.6 years) after surgery. The mean Pedi-IKDC/IKDC score was 94 ± 11 (range, 49-100). Pedi-IKDC/IKDC scores did not differ by age, sex, sports activities, time to surgery, or associated injuries (Table 4). There was not a significant learning curve (r = 0.06, P = .79). However, 5 patients (19%) had a score below 90, and all 5 had been treated with an ENDOBUTTON, with 4 having complications (Table 3). The 1 remaining patient did not have an ipsilateral complication but did have an ACL tear in the contralateral knee (score, 79).
Discussion
ACL injuries are being diagnosed more commonly in skeletally immature patients, who present a unique set of treatment challenges due to the open growth plates around the knee. Several ACL reconstruction techniques have been developed to avoid penetrating the growth plate, but the incidence and range of complications after ACL reconstruction in these patients has not been well documented. To our knowledge, this study is the first to report on complications as well as functional and patient-reported outcomes of an all-epiphyseal ACL reconstruction technique in patients with wide open growth plates (at a mean age of 11.4 years).
After a mean 3.6 years, all 27 patients had a normal Lachman test scores and nearly full flexion and extension, and the majority had returned to full activities and sports (81%) and had no pain (67%). There were 4 graft failures (15%). With regard to delay of treatment, our patients underwent surgical reconstruction at a mean 4.4 months after initial injury, but this ranged from 18 days to 33 months. There was no correlation between surgical delay and increased associated injuries such as meniscal tears. This finding is in agreement with Funahashi et al8 and Moksnes et al26 but in contrast to Dumont et al5and Lawrence et al,18 who showed pediatric patients with delayed treatment to have higher rates of meniscal and knee chondral surface damage. Not surprisingly, our study found knee reinjury to be more common in patients with associated injuries at index ACL surgery (P = .040) and in those who played more sports (P = .029).
The mean IKDC/Pedi-IKDC score of our sample was 94 ± 11, which is comparable to the scores reported with the transepiphyseal technique of Anderson2 (mean IKDC score, 96.5), the physeal-sparing technique of Kocher et al17 (mean IKDC score, 89.5), and several other transphyseal techniques16,18,22,32 (mean IKDC score range, 83-95). In comparison, nonoperative treatment has been found to result in a mean IKDC score of 85 at 3 years after injury.25
This all-epiphyseal ACL reconstruction technique, which confines the bone tunnels and fixation entirely to the epiphysis, restores the pediatric ACL anatomy and theoretically eliminates the risk of growth arrest or tethering that can complicate a transphyseal adult-style technique. We did not find any growth arrest in our patient cohort, but the epiphyseal bone tunnels only clear the growth plate by 1 to 2 mm, and in some areas, the tunnels touch the growth plate. If the horizontal femoral tunnel is drilled slightly proximal, it could damage a large swath of the growth plate. To avoid this, we typically start the femoral tunnel guide pin approximately 8 mm distal to the femoral growth plate and aim slightly proximal to target the anatomic footprint of the ACL in the posterior-lateral notch. The tibial epiphysis is more problematic, and even when the downsized 4.5- to 5.5-mm split tunnels in the tibial epiphysis are perfectly centered in the ossific epiphyseal nucleus, there is often only an up to 2-mm margin between the knee joint surface and the growth plate (Figure 2, A-D).
Based on these overgrowth complications, we now recommend avoiding or minimizing any periosteal stripping during surgery. All hamstring tendons harvested in this study had adequate length for the ACL reconstruction, and thus, the extra length gained from periosteal elevation of the hamstring graft is unnecessary. Anderson2 also identified overgrowth on the operative side in 3 of 4 patients with leg-length discrepancies subsequent to transepiphyseal ACL reconstruction. Koch et al15 identified significant overgrowth in 2 patients and minor leg-length discrepancies in 4 other patients who underwent epiphyseal ACL reconstruction. Fractures or surgery near an open growth plate can stimulate bone overgrowth. In their meta-analysis of 935 patients, Frosch et al7 reported a 1.8% incidence of leg-length differences or limb axis deviations after operative treatment of ACL ruptures in children and adolescents. Thus, we recommend close follow-up for leg length and knee angular changes after any pediatric ACL surgery. When overgrowth is identified early, it can be corrected with a minimally invasive guided growth procedure.19
Epidemiological data from highly active cohorts who return to sport exceed 20% second ACL injury rates (ipsilateral graft failure and contralateral ACL) in just the first year after return to sport.29,30 In populations younger than 20 years, nearly one-third of patients suffer second ACL injuries.33 In the current cohort, 4 of the 27 patients (15%) suffered a failure of the ACL graft, and 2 patients (7%) suffered a contralateral ACL tear. All 4 graft failures had previously been treated with a 7-mm femoral tunnel, with 1 graft fixated through a single 7-mm tibial tunnel with a biocomposite screw (femoral side tear), 1 graft fixated through 4.5- and 5.5-mm tibial tunnels with a bioabsorbable screw (tibial side tear), 1 graft fixated through 5.0- and 5.5-mm tibial tunnels with an ENDOBUTTON that had displaced (unknown side tear), and 1 graft fixated through two 5.0-mm tibial tunnels with an ENDOBUTTON (lax not torn). Recently, the MOON group identified a high ACL retear rate (37.5%) in the 10- to 19-year age group.13 In another study, a nonanatomic “over the top” doubled semitendinosis autograft reconstruction with a transphyseal tibial tunnel yielded an ipsilatearal 25% retear rate in skeletally immature patients.4
During the early postoperative period, the graft fixation method is key to overall integrity of the reconstruction. Tensile loads on the ACL during routine daily activities are reported to be at most 20% of its failure capacity.27 As reported by Anderson,2 with his transepiphyseal technique, the load to failure of the femoral fixation (1345 N) and tibial fixation (830 N) exceeds the normal tensile loads on the ACL. One of our 3 ACL retears involved lack of biologic incorporation and loss of fixation of the femoral ENDOBUTTON/XTENDOBUTTON construct. There were no tibial fixation failures or femoral interference screw fixation failures. Ultimately, all knees had a negative Lachman and pivot shift tests despite our postoperative protocol of immediate postoperative weightbearing as tolerated.
Our 5 postoperative meniscal tears are concerning because the purpose of ACL reconstruction is to stabilize the knee and protect against meniscal tears. Four of these tears were retears of a repaired meniscus. Most were repaired using an inside-out technique, using either 2-0 Ethibond Excel or 2-0 PDS II suture (Ethicon). We have since switched to 2-0 FiberWire high-strength sutures (Arthrex), which may reduce this high rate of retear. Our cohort had other knee injuries, such as patellar dislocation and lateral femoral condyle fracture, that appeared to be unrelated to the child’s ACL reconstruction on the ipsilateral knee, and 2 ACL tears and a meniscal tear to the opposite knee (Table 2). We feel that these were markers of the child’s high sports activity level.
Multiple techniques have been described for physeal-sparing ACL reconstruction. Parker et al29 described reconstruction by passing hamstring tendons through the anterior aspect of the tibia and over the top of the lateral femoral condyle. Micheli et al23 used the iliotibial band as the graft and passed it outside the lateral femoral condyle and through the intercondylar notch, which was then sutured to the periosteum of the proximal tibia. These techniques may be limited in their ability to reproduce native knee isometry, and more anatomic reconstructions, such as the one used here, have been developed. Our all-epiphyseal femoral and tibial tunnels were drilled independently and entered the joint in the anatomic footprint of the native ACL.
The results of our study must be interpreted within the context of its limitations and retrospective design. While all patients within our study population received the same basic all-epiphyseal reconstruction, there were differences in technique throughout the course of the study, including femoral fixation and tibial tunnel design. Despite being one of the largest and youngest pediatric ACL sample sizes reported in the literature, we were still only able to report on 27 patients due to the requirement of at least 2-year follow-up. As with any new technique, there was a gradual evolution of the technique and learning curve for the 2 surgeons involved. The cohort of cases reported represents our initial learning curve. We currently triple our semitendinosus to increase the diameter of the graft and perform a notchplasty to avoid graft impingement. Further study will need to be undertaken to see whether these surgical modifications change the results of this procedure. Last, both the Pedi-IKDC and IKDC were used interchangeably as functional outcome measures in this study, and preoperative scores were not evaluated.
A split tibial tunnel technique for all-epiphyseal ACL reconstruction returned 81% of very young athletes to sports. There were 4 ipsilateral ACL autograft failures (15%) and 2 contralateral ACL tears (7%). There were 5 subsequent ipsilateral meniscal tears, 4 of which were retears of a repaired meniscus. There were no reported cases of growth arrest, but 3 patients had knee overgrowth, and 2 patients required a subsequent guided growth procedure. Functional results were excellent, with a mean IKDC/Pedi-IKDC score of 94 ± 11 for the cohort at a mean of 3.8 years after reconstruction.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: E.J.W. is a paid consultant for and holds an ACL patent with OrthoPediatrics.
Ethical approval for this study was obtained from the Institutional Review Board at Cincinnati Children’s Hospital Medical Center.
References
- 1. Aichroth P, Patel D, Zorrilla P. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. Bone Joint J. 2002;84:38–41. [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients. J Bone Joint Surg Am. 2003;85:1255–1263. [DOI] [PubMed] [Google Scholar]
- 3. Angel KR, Hall DJ. Anterior cruciate ligament injury in children and adolescents. Arthroscopy. 1989;5:197–200. [DOI] [PubMed] [Google Scholar]
- 4. Demange MK, Camanho GL. Nonanatomic anterior cruciate ligament reconstruction with double-stranded semitendinosus grafts in children with open physes: minimum 15-year follow-up. Am J Sports Med. 2014;42:2926–2932. [DOI] [PubMed] [Google Scholar]
- 5. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40:2128–2133. [DOI] [PubMed] [Google Scholar]
- 6. Edwards TB, Greene CC, Baratta RV, Zieske A, Willis RB. The effect of placing a tensioned graft across open growth plates. J Bone Joint Surg Am. 2001;83:725–734. [DOI] [PubMed] [Google Scholar]
- 7. Frosch KH, Stengel D, Brodhun T, et al. Outcomes and risks of operative treatment of rupture of the anterior cruciate ligament in children and adolescents. Arthroscopy. 2010;26:1539–1550. [DOI] [PubMed] [Google Scholar]
- 8. Funahashi KM, Moksnes H, Maletis GB, Csintalan RP, Inacio MC, Funahashi TT. Anterior cruciate ligament injuries in adolescents with open physis: effect of recurrent injury and surgical delay on meniscal and cartilage injuries. Am J Sports Med. 2014;42:1068–1073. [DOI] [PubMed] [Google Scholar]
- 9. Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja R. Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992;8:229–233. [DOI] [PubMed] [Google Scholar]
- 10. Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. Am J Med Sci. 1959;238:393. [Google Scholar]
- 11. Henry J, Chotel F, Chouteau J, Fessy MH, Bérard J, Moyen B. Rupture of the anterior cruciate ligament in children: early reconstruction with open physes or delayed reconstruction to skeletal maturity? Knee Surg Sports Traumatol Arthrosc. 2009;17:748–755. [DOI] [PubMed] [Google Scholar]
- 12. Iversen M, Lee B, Connell P, Andersen J, Anderson A, Kocher M. Validity and comprehensibility of the international knee documentation committee subjective knee evaluation form in children. Scand J Med Sci Sports. 2010;20:e87–e95. [DOI] [PubMed] [Google Scholar]
- 13. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kannus P, Jarvinen M. Knee ligament injuries in adolescents. Eight year follow-up of conservative management. Bone Joint J. 1988;70:772–776. [DOI] [PubMed] [Google Scholar]
- 15. Koch PP, Fucentese SF, Blatter SC. Complications after epiphyseal reconstruction of the anterior cruciate ligament in prepubescent children. Knee Surg Sports Traumatol Arthrosc. 2016;24:2736–2740. [DOI] [PubMed] [Google Scholar]
- 16. Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am. 2005;87:2371–2379. [DOI] [PubMed] [Google Scholar]
- 17. Kocher MS, Smith JT, Iversen MD, et al. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39:933–939. [DOI] [PubMed] [Google Scholar]
- 18. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582–2587. [DOI] [PubMed] [Google Scholar]
- 19. Lemaitre G, Salle de Chou E, Pineau V, et al. ACL reconstruction in children: a transphyseal technique. Orthop Traumatol Surg Res. 2014;100(4 suppl):S261–S265. [DOI] [PubMed] [Google Scholar]
- 20. Lykissas MG, Jain VV, Manickam V, Nathan S, Eismann EA, McCarthy JJ. Guided growth for the treatment of limb length discrepancy: a comparative study of the three most commonly used surgical techniques. J Pediatr Orthop B. 2013;22:311–317. [DOI] [PubMed] [Google Scholar]
- 21. Lykissas MG, Nathan ST, Wall EJ. All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients: a surgical technique using a split tibial tunnel. Arthrosc Tech. 2012;1:e133–e139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5-to 10-year follow-up—a systematic review. J Knee Surg. 2009;22:347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Micheli LJ, Rask B, Gerberg L. Anterior cruciate ligament reconstruction in patients who are prepubescent. Clin Orthop Relat Res. 1999;364:40–47. [DOI] [PubMed] [Google Scholar]
- 24. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18:955–959. [DOI] [PubMed] [Google Scholar]
- 25. Moksnes H, Engebretsen L, Eitzen I, Risberg MA. Functional outcomes following a non-operative treatment algorithm for anterior cruciate ligament injuries in skeletally immature children 12 years and younger. A prospective cohort with 2 years follow-up. Br J Sports Med. 2013;47:488–494. [DOI] [PubMed] [Google Scholar]
- 26. Moksnes H, Engebretsen L, Risberg MA. Performance-based functional outcome for children 12 years or younger following anterior cruciate ligament injury: a two to nine-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2008;16:214–223. [DOI] [PubMed] [Google Scholar]
- 27. Nathan ST, Lykissas MG, Wall EJ. Growth stimulation following an all-epiphyseal anterior cruciate ligament reconstruction in a child. JBJS Case Connector. 2013;3:e14. [DOI] [PubMed] [Google Scholar]
- 28. Oak SR, O’Rourke C, Strnad G, et al. Statistical comparison of the pediatric versus adult IKDC Subjective Knee Evaluation Form in adolescents. Am J Sports Med. 2015;43:2216–2221. [DOI] [PubMed] [Google Scholar]
- 29. Parker AW, Drez D, Cooper JL. Anterior cruciate ligament injuries in patients with open physes. Am J Sports Med. 1994;22:44–47. [DOI] [PubMed] [Google Scholar]
- 30. Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE. Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2011;41:553–559. [DOI] [PubMed] [Google Scholar]
- 31. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. [DOI] [PubMed] [Google Scholar]
- 32. Shelbourne KD, Gray T, Wiley BV. Results of transphyseal anterior cruciate ligament reconstruction using patellar tendon autograft in tanner stage 3 or 4 adolescents with clearly open growth plates. Am J Sports Med. 2004;32:1218–1222. [DOI] [PubMed] [Google Scholar]
- 33. Streich NA, Barié A, Gotterbarm T, Keil M, Schmitt H. Transphyseal reconstruction of the anterior cruciate ligament in prepubescent athletes. Knee Surg Sports Traumatol Arthrosc. 2010;18:1481–1486. [DOI] [PubMed] [Google Scholar]
- 34. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641–647. [DOI] [PubMed] [Google Scholar]