Abstract
Background:
Failure rates of knee ligament surgery may be high, and the impact of osseous alignment on surgical outcome remains controversial. Basic science studies have demonstrated that osseous malalignment can negatively affect ligament strain and that realignment procedures may improve knee joint stability.
Hypothesis/Purpose:
The purpose of this review was to summarize the clinical evidence concerning the impact of osseous malalignment and realignment procedures in knee ligament surgery. The hypotheses were that lower extremity malalignment would be an important contributor to knee ligament surgery failure and that realignment surgery would contribute to increased knee stability and improved outcome in select cases.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
According to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a systematic electronic search of the PubMed database was performed in November 2015 to identify clinical studies investigating (A) the influence of osseous alignment on postoperative stability and/or failure rates after knee ligament surgery and (B) the impact of osseous realignment procedures in unstable knees with or without additional knee ligament surgery on postoperative knee function and stability. Methodological quality of the studies was assessed using the Oxford Centre for Evidence-Based Medicine Levels of Evidence and the Coleman Methodological Score (CMS).
Results:
Of the 1466 potentially relevant articles, 28 studies fulfilled the inclusion and exclusion criteria. Average study quality was poor (CMS, 40). For part A, studies showed increased rerupture rate after anterior cruciate ligament (ACL) replacement in patients with increased tibial slope. Concerning the posterior cruciate ligament (PCL)/posterolateral corner (PLC)/lateral collateral ligament (LCL), varus malalignment was considered a significant risk factor for failure. For part B, studies showed decreased anterior tibial translation after slope-decreasing high tibial osteotomy in ACL-deficient knees. Correcting varus malalignment in PCL/PLC/LCL instability also showed increased stability and better outcomes.
Conclusion:
In cases of complex knee instability, the 3-dimensional osseous alignment of the knee should be considered (eg, mechanical weightbearing line and tibial slope). In cases of failed ACL reconstruction, the tibial slope should be considered, and slope-reducing osteotomies are often helpful in the patient revised multiple times. In cases of chronic PCL and/or PLC instability, osseous correction of the varus alignment may reduce the failure rate and is often the first step in treatment. Changes in the mechanical axis should be considered in all cases of instability accompanied by early unicompartmental osteoarthritis.
Keywords: knee instability, osseous geometry, tibial slope, ACL revision, high tibial osteotomy
Primary anterior cruciate ligament reconstruction (ACLR) generally leads to a good outcome and has a revision rate of between 1.6% and 2.1%, as reported in the Swedish National Knee Ligament Registry.7 With follow-up longer than 10 years, the ACL graft rupture rate increases to 6% (range, 0%-3%) and clinical failure occurs in approximately 10% of ACLR cases (range, 2%-26%).11 Revision of a previously reconstructed ACL shows even higher rerupture rates of approximately 13.7%.59 Furthermore, outcomes with subsequent revisions are dismal, with only 4 of 15 (27%) patients returning to their prior levels of activity.20 Additionally, based on long-term follow-up, osteoarthritis develops in 21% to 48% of patients after combined ACL, meniscus, and cartilage injuries but in only 0% to 13% of patients with isolated ACL rupture.46
Combined surgical interventions of ACLR and high tibial osteotomy (HTO) are performed in cases of medial compartment osteoarthritis and ACL insufficiency.34 In a systematic review that included 11 studies, simultaneous HTO and ACLR showed good restoration of anterior stability, alleviation of medial compartment osteoarthritis, improvement in subjective evaluations, and a predictable return to recreational sports.34 In addition to alteration of the weightbearing line with HTO, the 3-dimensional osseous geometry has an important impact on knee stability—an observation that has been verified in several basic science studies but has been studied less frequently in clinical settings.1,3,17,18,29,47,50,54
In a landmark biomechanical cadaveric study, Agneskirchner et al1 demonstrated the role of the tibial slope in anteroposterior knee stability, which is most important in cases of ACL or posterior cruciate ligament (PCL) rupture.18,47,50,54 Giffin et al19 investigated the effect of increasing the anterior-posterior slope on knee kinematics and in situ forces of the cruciate ligaments in 10 cadaveric knees. The authors found that an increased tibial slope led to a relative anterior shift in the resting position of the knee, which was most prominent during knee extension and diminished during knee flexion. In addition, the knee was translated anteriorly throughout the range of motion. The authors concluded that increasing the tibial slope may be beneficial in reducing tibial sag and increasing stability in a PCL-deficient knee. In a computer model study, Shelburne et al51 found that changes in the tibial slope affect tibial shear forces, anterior tibial translation, and knee ligament loading during activities of daily living, such as standing, squatting, and walking. Furthermore, coronal plane alignment (varus/valgus) is important for collateral ligament stability, especially in cases of posterolateral corner (PLC) instability.29 van de Pol et al53 showed that pronounced varus alignment with lateral joint opening (varus thrust) can also lead to increased forces on the ACL. Furthermore, medial collateral ligament tension is influenced by the coronal alignment.2,21 However, there are also contradictory findings, and overall, the relevance of these basic science results to clinical outcome is very vague at present.17
The primary aim of this systematic review was to summarize current clinical knowledge about the influence of 3-dimensional osseous knee alignment on knee ligament surgery outcomes. The secondary aim was to investigate the role of realignment surgery on knee stability with or without knee ligament reconstruction. The hypothesis was that 3-dimensional knee alignment would be an important contributor to recurrent instability and graft failure after knee ligament surgery and that realignment surgery would contribute to increased knee stability and improved outcome in selected cases.
Methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.39 A systematic electronic search of the PubMed database was performed in November 2015 to identify clinical studies investigating (A) the influence of osseous alignment on postoperative stability and/or failure rates after knee ligament surgery and (B) the impact of osseous realignment procedures in unstable knees with or without additional knee ligament surgery on postoperative knee function and stability. The following search terms were used in the title and abstract fields: (((Knee) AND (Anterior cruciate ligament OR ACL OR posterior cruciate ligament OR PCL OR posterolateral corner OR PLC OR lateral collateral ligament OR LCL OR fibular collateral ligament OR FCL OR posteromedial corner OR PMC OR medial collateral ligament OR MCL OR multiligament OR stability OR instability)) AND (Varus OR valgus OR alignment OR malalignment OR slope OR thrust OR hyperextension OR osteotomy)) NOT (Arthroplasty OR knee replacement). No limits were placed on the date of publication. In addition to the electronic search, the reference lists of all included articles and review articles identified from the electronic search were manually searched for additional relevant articles.
For the purpose of this systematic review, only clinical studies that specifically investigated the following were included: the influence of lower-limb alignment on postoperative stability and/or failure after knee ligament surgery, the influence of realignment osteotomy with or without additional knee ligament surgery on knee stability, and the results of revision ligament reconstruction with additional realignment surgery in patients in whom malalignment was considered the primary reason for failure of the reconstruction procedure. Additional inclusion criteria were as follows: English- or German-language studies, studies published online or in print in a peer-reviewed journal, studies reporting the results of 5 or more patients, studies on patients of any age, and clinical trials of all levels of evidence. The exclusion criteria were as follows: meeting abstracts and proceedings, in vitro or animal studies, clinical studies with insufficient outcome data, and any other type of article, such as technical notes, case reports, or narrative or systematic reviews.
Two reviewers (T.T., M.J.F.) independently screened the titles and abstracts of all articles for relevance according to the inclusion and exclusion criteria. If no abstract was available, the full-text article was obtained to assess the relevance of the study. The full text of all articles that were not excluded during the initial screening process was obtained and reviewed by the same 2 reviewers for possible inclusion in the systematic review. Any disagreement on article eligibility was resolved through discussion until a consensus was reached. For each study that met the inclusion criteria, the author names, year of publication, purpose, study design, follow-up protocol, main results, and level of evidence according to the Oxford Centre for Evidence-Based Medicine were recorded.58 Data were extracted by 1 reviewer (M.J.F.) and verified by a second reviewer (T.T.). Any disagreement was resolved via consensus among the reviewers.
Quality Assessment
Two reviewers (T.T., M.J.F.) independently evaluated all included studies and assigned a level of evidence (level 1-4).38 The methodological quality of each study was evaluated using the Coleman Methodology Score (CMS).10 The CMS is calculated from a 2-part, 10-item questionnaire, scored from 0 to 100 (excellent, 85-100; good, 70-84; fair, 55-69; poor, <55), that has been used in the evaluation of both randomized controlled trials and nonrandomized controlled trials.
Results
Literature Search
Through the electronic and manual search of the relevant reference lists, a total of 1466 potentially relevant articles were identified. After screening the title and abstract of the articles followed by analysis of the full text, a total of 28 studies fulfilled the inclusion and exclusion criteria and were included in this systematic review. The search results are summarized in Figure 1.
Figure 1.
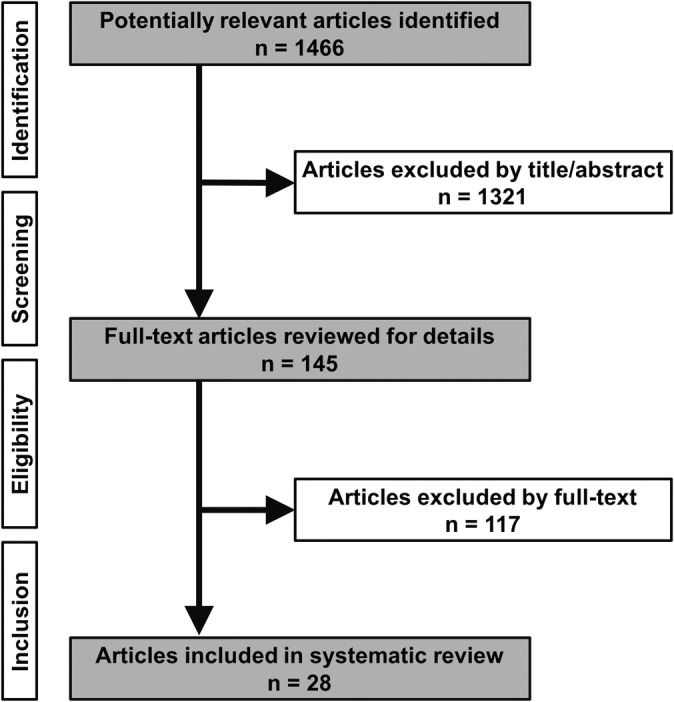
Flowchart of the search strategy in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
No clinical studies investigating the influence of osseous alignment or realignment surgery in cases of medial instability or repair/reconstruction of the medial ligamentous structures were identified.
Quality Assessment
The average CMS of the included studies was 40.1. The primary limitation was the study design in most studies (0.4/15). No prospective controlled or randomized study was performed. Other limitations included the lack of description of postoperative rehabilitation and assessment of patient compliance with rehabilitation (0.2/10) as well as outcome assessment (2.5/15). Strengths of these studies included a mean follow-up duration of longer than 24 months (4/5) in most studies, the use of appropriate outcome measures (8.1/10), and diagnostic certainty (4.3/5).
Part A: Clinical Studies Investigating the Influence of Osseous Alignment on Postoperative Stability and Failure Rates After Knee Ligament Surgery
Anterior Cruciate Ligament
A total of 10 studies were identified (Table 1). One study had level 2 evidence, 6 studies had level 3 evidence, and 3 studies had level 4 evidence. In a prospective multicenter study of patients undergoing revision ACLR, malalignment was rated as the cause of failure in 4% of patients. However, the authors did not provide details about the type of malalignment.37 With regard to coronal malalignment (varus/valgus), the results of the included studies are inconclusive. Won et al57 observed that patients undergoing revision ACLR were significantly more likely to have varus malalignment >5° than patients undergoing primary ACLR. Noyes and Barber-Westin42 found that varus alignment was a factor contributing to failure of ACLR procedures in 25% of patients. On the other hand, Kim et al28 compared the results of patients with different amounts of primary varus malalignment undergoing ACLR and did not observe any differences in functional outcome. However, it must be noted that patients with a varus thrust (double and triple varus) were excluded from the study by Kim et al.28 With regard to sagittal malalignment, the selected studies are more conclusive. Webb et al55 found that the mean tibial slope was significantly greater in patients with ACL graft tear after ACLR compared with patients with no further injury. Patients with a tibial slope of 12° or higher had a 59% incidence of further ACL injury, compared with 23% for those with a tibial slope <12°. Li et al32 found significantly greater lateral slope and medial slope in patients with graft failure after ACLR, but the effect of the lateral slope was greater than that of the medial slope. Christensen et al9 also found a significantly steeper lateral slope in female patients with early graft failure but did not observe a significant difference in this parameter among male patients. In another study, Li et al33 observed statistically significant correlations of the medial and lateral tibial slopes with postoperative anterior tibial translation after ACLR. Patients with a steeper medial or lateral slope showed a higher risk of anterior tibial translation of 5 mm or greater.
TABLE 1.
Clinical Studies Investigating the Influence of Osseous Alignment on Postoperative Stability and Failure Rates After ACLRa
| Author(s), Year | Purpose | Study Design | Follow-up | Main Results | Level of Evidence |
|---|---|---|---|---|---|
| The MARS Group et al, 201037 | To provide a descriptive analysis of demographic and clinical features of patients undergoing revision ACLR |
|
— |
|
2 |
| Kim et al, 201128 | To evaluate whether stability and function differ in patients after ACLR with differing degrees of preoperative primary varus malalignment |
|
45 mo |
|
4 |
| Won et al, 201357 | To investigate whether patients undergoing revision ACLR have varus malalignment more frequently than patients undergoing primary ACLR |
|
— |
|
3 |
| Noyes and Barber-Westin, 200642 | To determine factors that may have caused failure of 32 ACLR procedures in 21 patients undergoing revision ACLR (secondary purpose) |
|
— |
|
4 |
| Saito et al, 201549 | To compare postoperative outcomes after anatomic db ACLR between cases of extreme knee hyperextension and cases of normal to mild hyperextension |
|
28 mo |
|
3 |
| Webb et al, 201355 | To investigate whether higher PTS is associated with increased risk for further ACL injuries after ACLR |
|
15 y |
|
3 |
| Li et al, 201432 | To investigate the association between PTS and failure after ACLR |
|
32.5 mo |
|
3 |
| Christensen et al, 20159 | To determine whether patients with a higher lateral PTS are at greater risk of early graft failure after ACLR |
|
6.9 y |
|
3 |
| Li et al, 201433 | To analyze the relationship between PTS and anterior tibial translation after sb ACLR |
|
27.5 mo |
|
3 |
| Hohmann et al, 201025 | To investigate the relationship between knee functionality and PTS after ACLR |
|
21.1 mo |
|
4 |
aACLR, anterior cruciate ligament reconstruction; db, double-bundle; HTO, high tibial osteotomy; MAD, mechanical axis deviation; MRI, magnetic resonance imaging; OA, osteoarthritis; PTS, posterior tibial slope; sb, single-bundle.
Posterior Cruciate Ligament, Posterolateral Corner, and/or Lateral Collateral Ligament
Three studies were identified, and all of them had level 4 evidence (Table 2). Summarizing the results of the 3 studies, varus malalignment must be regarded as a significant risk factor for failure after PCL and/or PLC reconstruction procedures.31,43,44 No selected clinical study analyzed the influence of the tibial slope on outcomes after PCL or PLC surgery.
TABLE 2.
Clinical Studies Investigating the Influence of Osseous Alignment on Postoperative Stability and Failure Rates After Reconstruction of the PCL, PLC, and/or LCLa
| Author(s), Year | Purpose | Study Design | Follow-up | Main Results | Level of Evidence |
|---|---|---|---|---|---|
| Noyes et al, 200644 | To determine the factors responsible for failed PLC procedures |
|
17 mo |
|
4 |
| Noyes and Barber-Westin, 200543 | To determine the factors contributing to failure after PCL reconstruction |
|
42 mo |
|
4 |
| Lee et al, 201231 | To evaluate the reasons for failure of primary PCL reconstruction |
|
36.3 mo |
|
4 |
aLCL, lateral collateral ligament; MRI, magnetic resonance imaging; PCL, posterior cruciate ligament; PLC, posterolateral corner.
Part B: Clinical Studies Investigating the Influence of Realignment Osteotomy With or Without Ligament Reconstruction on Postoperative Knee Function
Function of the ACL-Deficient Knee
A total of 11 studies were identified, and all of them had level 3 or 4 evidence (Table 3). The stabilizing effect of isolated osteotomy on the ACL-deficient knee joint remains controversial. For example, Williams et al56 reported that HTO alone had no effect on results of the Lachman test or pivot shift; however, 67% of patients receiving HTO alone reported a decrease in instability symptoms. Nevertheless, several studies have found significantly improved functional knee scores and stability after isolated valgus HTO, but procedures combining HTO with single-stage or 2-stage ACLR typically resulted in better outcomes.6,30,41,45 In patients undergoing combined HTO and ACLR, 2 studies have found that postoperative anterior tibial translation correlated with the postoperative tibial slope.14,60 For example, Dejour et al14 reported that the more the slope was increased during HTO, the greater the postoperative anterior tibial translation on unilateral weightbearing. In 2 studies, a second revision ACLR was performed in combination with anterior closing wedge slope-reducing HTO in patients with ACL graft failure in association with a posterior tibial slope of 12° or higher.13,52 Both studies reported that stability could be restored in all patients without significant loss of range of motion. Based on gait analysis, HTO combined with ACLR significantly decreased peak knee adduction moment and knee internal rotation moment, and these changes correlated with the decrease in static varus alignment.27,36
TABLE 3.
Clinical Studies Investigating the Influence of Osseous Realignment With/Without Ligament Reconstruction on the Function of the ACL-Deficient Kneea
| Author(s), Year | Purpose | Study Design | Follow-up | Main Results | Level of Evidence |
|---|---|---|---|---|---|
| Noyes et al, 199341 | To compare the results of 3 different treatment modalities for younger patients with varus malalignment and chronic ACL deficiency |
|
58 mo |
|
3 |
| Dejour et al, 199414 | To analyze the results of patients undergoing simultaneous ACLR and HTO |
|
3.6 y |
|
4 |
| Lattermann and Jakob, 199630 | To compare 3 different treatment options for patients with ACL deficiency, varus malalignment, and medial OA |
|
5.8 y |
|
3 |
| Badhe and Forster, 20026 | To report the results of ligament reconstruction with HTO in cases of ACL-, PCL-, and PLC ligament–deficient knees |
|
2.8 y |
|
4 |
| Williams et al, 200356 | To evaluate the results of patients with ACL deficiency, symptomatic OA in the medial compartment, and varus malalignment treated with closed-wedge HTO alone or together with ACLR |
|
45.8 mo |
|
4 |
| Zaffagnini et al, 201360 | To evaluate the clinical and radiographic outcomes after sb over-the-top ACLR and concomitant lateral closing-wedge HTO in patients with varus angulated ACL-deficient knees |
|
6.5 y |
|
4 |
| Noyes et al, 200045 | To evaluate the outcome of operative treatment in patients with ACL deficiency and double- or triple-varus knee syndromes |
|
4.5 y |
|
4 |
| Kean et al, 200927 | To evaluate the effects of simultaneous HTO and ACLR on 3-dimensional gait patterns and muscle activity |
|
12 mo |
|
4 |
| Marriott et al, 201536 | To investigate changes in gait biomechanics after combined medial open-wedge HTO and ACLR |
|
68 mo |
|
4 |
| Sonnery-Cottet et al, 201452 | To evaluate the clinical outcome of combined re-revision ACLR and proximal tibial anterior closing-wedge osteotomy in patients with recurrent graft failure in association with increased PTS |
|
31.6 mo |
|
4 |
| Dejour et al, 201513 | To evaluate the outcome of second revision ACLR combined with tibial deflexion osteotomy for correction of excessive PTS |
|
4.0 y |
|
4 |
aACLR, anterior cruciate ligament reconstruction; db, double-bundle; HTO, high tibial osteotomy; LARS, Ligament Advanced Reconstruction System; MRI, magnetic resonance imaging; OA, osteoarthritis; PCL, posterior cruciate ligament; PLC, posterolateral corner; PTS, posterior tibial slope; sb, single-bundle.
Function of the PCL-, PLC-, and/or LCL-Deficient Knee
A total of 5 studies were identified, and all of them had level 4 evidence. The main findings of the analyzed studies are summarized in Table 4. There is agreement among the studies that realignment osteotomy can improve knee function and stability in PLC- and PCL-deficient knees. Based on the available evidence, valgus-producing medial open-wedge HTO can be considered an effective treatment method in patients with isolated or combined posterolateral instability and varus malalignment.4,6,40 Isolated open-wedge HTO has been shown to improve stability in several cases without the need for secondary ligament reconstruction. Whether increasing the tibial slope further improves outcome in these patients remains controversial.4,40 In patients with symptomatic hyperextension after failed PCL reconstruction, anterior open-wedge flexion HTO without revision PCL reconstruction has been shown to significantly improve knee function.48
TABLE 4.
Clinical Studies Investigating the Influence of Osseous Realignment With/Without Ligament Reconstruction on the Function of the PCL-, PLC-, and/or LCL-Deficient Kneea
| Author(s), Year | Purpose | Study Design | Follow-up | Main Results | Level of Evidence |
|---|---|---|---|---|---|
| Badhe and Forster, 20026 | To report the results of ligament reconstruction with HTO in cases of ACL-, PCL-, and PLC-deficient knees |
|
2.8 y |
|
4 |
| Naudie et al, 200440 | To assess the functional outcome of medial open-wedge HTO in patients with posterolateral instability and hyperextension-varus thrust |
|
56 mo |
|
4 |
| Arthur et al, 20074 | To assess the functional outcomes of patients with grade 3 posterolateral instability and varus malalignment treated with open-wedge HTO |
|
37 mo |
|
4 |
| Ayerza et al, 20125 | To investigate the functional outcome of open-wedge osteotomy of the lateral tibial plateau in patients with posterolateral rotatory instability due to depression of the lateral tibia plateau |
|
5.4 y |
|
4 |
| Reichwein and Nebelung, 200748 | To assess the functional outcome of flexion HTO in patients with symptomatic hyperextension after failed PCL reconstruction |
|
20 mo |
|
4 |
aACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; HTO, high tibial osteotomy; IKDC, International Knee Documentation Committee; LARS, Ligament Advanced Reconstruction System; LCL, lateral collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner; PTS, posterior tibial slope.
Discussion
The most important findings of the present systematic review were that there is clinical evidence supporting osseous malalignment as a factor contributing to failure of knee ligament surgery and that realignment surgery can improve function and stability, especially in cases of PLC insufficiency and in combination with revision ACL surgery.
Valgus HTO is considered a well-established option for isolated unicompartmental degenerative joint disease and combined ligament instability. Its clinical value has been emphasized recently.34,57 Two recent systematic reviews have reported the results of valgus HTO in cases of knee instability,8,12 and another systematic review has reported the clinical outcomes of simultaneous HTO and ACLR.34 However, these studies presented clinical and radiographic outcomes in general without specifically analyzing the influence of osseous malalignment or realignment surgery on knee stability in detail. Less well understood is the influence of osseous alignment on ligament stability, especially the importance of the tibial slope. In many basic science studies, important roles of the tibial slope on ACL/PCL stability and of valgus alignment in LCL/PLC stability have been shown.†† However, the results of basic science studies are not easily translatable to the clinical setting.
Based on the findings of this systematic review, osseous alignment influences failure rates after ACLR. Several clinical studies (with level 3 evidence) showed an increased failure rate after ACL reconstruction among patients with a steep posterior tibial slope (PTS).9,32,33,55 Slope-reducing HTO appears to reduce the graft rupture rate and to increase knee stability in these cases. In particular, second revision ACLR appears to benefit from a reduced PTS through HTO.13,52 Reduced PTS and varus may protect the reconstructed ACL from fatigue failure.13 Surgeons should therefore be especially aware of the potential impact of PTS on revision ACLR. In this regard, the surgeon should bear in mind that open-wedge HTO tends to increase the slope, whereas closed-wedge HTO tends to decrease the PTS.15,24 Unintentionally increased tibial slopes might play a role in the increased incidence of ACL ruptures.17 Hinterwimmer et al23 highlighted the use of sagittally placed Kirschner wires to perform the appropriate amount of correction in open-wedge HTO.
Regarding primary ACLR, the evidence in the current literature is not conclusive, but there is a trend toward a relevant effect of posterior slope reduction on ACLR success. However, the absolute amount of slope reduction necessary is presently unknown. Coronal plane correction in primary varus knees is probably not necessary to achieve knee stability28; however, in double or triple varus knees, basic science studies have shown increased strain on the ACL, which may cause the reconstructed ACL to fail.22,53 Additionally, correction of associated varus or valgus malalignment protects the joint from further degeneration.
In contrast to the ACL, in which clinical studies have shown an influence of the tibial slope on failure rates, little clinical data regarding the PCL are available.31,43 Noyes and Barber-Westin43 investigated the failure mechanism of 52 PCL-reconstructed knees and found that varus malalignment contributed to failure in 31% of cases. However, no detailed analysis of the tibial slope was performed. Again, Noyes et al,44 in another analysis of failure in 57 consecutive posterolateral operative procedures, showed that untreated varus malalignment contributed to failure in 37% of cases. Regarding this high failure rate, it is currently understood that in cases of posterolateral instability and severe varus alignment, the varus malalignment should be corrected either before ligament stabilization or as a combined procedure. In this study, the role of the tibial slope in ligament stability has not been investigated. Reichwein and Nebelung48 investigated 15 cases of high tibial slope–increasing osteotomy for revision of PCL instability. They found a significant improvement in International Knee Documentation Committee scores in this challenging group of patients. Naudie et al40 investigated 16 patients (17 knees) with symptomatic hyperextension–varus thrust treated via open-wedge HTO. Four patients had a PCL injury, 7 a combined PCL and PLC injury, and 5 a capsuloligamentous laxity. After a mean follow-up period of 56 months, the Tegner and Lysholm scores and the 5-point visual analog scores for knee stability and satisfaction were assessed. In addition, radiographs were analyzed to determine changes in femorotibial and mechanical axis alignment, tibial slope, and patellar height. In all patients, the Tegner and Lysholm score significantly improved after HTO. However, 30% of patients showed persistent instability and underwent a secondary PCL reconstruction to restore posterior stability. The authors concluded that open-wedge HTO is a good treatment for select patients with a symptomatic varus thrust. Arthur et al4 prospectively investigated 21 patients with combined grade 3 posterolateral instability and varus deformity. Patients were either treated with medial-opening HTO and second-stage ligament reconstruction (62%) or with HTO alone (38%). The mean follow-up duration was 37 months. In 38% (8/21) of patients, second-stage PLC reconstruction was not necessary because the outcome had been sufficiently improved by HTO. The authors concluded that medial open-wedge HTO is an effective first method of treatment for patients with varus knees and chronic combined posterolateral knee injuries.
Surgical correction of osseous alignment also has upper limits, beyond which no further correction should be made. We recommend that correction of the tibial slope should not lead to hyperextension greater than 5° in cases of ACL surgery or 0° of extension in cases of PCL surgery because knee function would otherwise be compromised.
Limitations
Regarding these complex cases, there is still a lack of high-quality clinical studies. Nearly all included studies had level 3 or 4 evidence. Only 1 study with level 2 evidence could be included. For the rare cases of PCL/PLC/LCL instability, only level 4 evidence was available. Given the heterogeneity in the study design, patient selection, and surgical techniques, no quantitative comparison across studies or meta-analysis was possible. However, since a total of 28 clinical studies could be included, several recommendations for clinical work were generated (level 3 evidence).
Furthermore, measuring the tibial slope on radiographs is occasionally difficult, and multiple measurement methods exist, although they produce different normal values.17 Commonly used methods for measuring coronal alignment and the tibial slope on radiographs are displayed in Figure 2. Magnetic resonance imaging (MRI) techniques enabling independent measurement of the medial and lateral tibial slopes have been described but have only rarely been used to date.26 Some studies measured the medial and lateral tibial slopes independently while others did not. To improve future research and to make studies comparable, a uniform method to measure the tibial slope should be defined. In general, long lateral knee radiographs should be preferred over short radiographs.16 If MRI is used, the circle method described by Hudek et al26 may be the preferred method since it has been shown to be the most repeatable method.35
Figure 2.
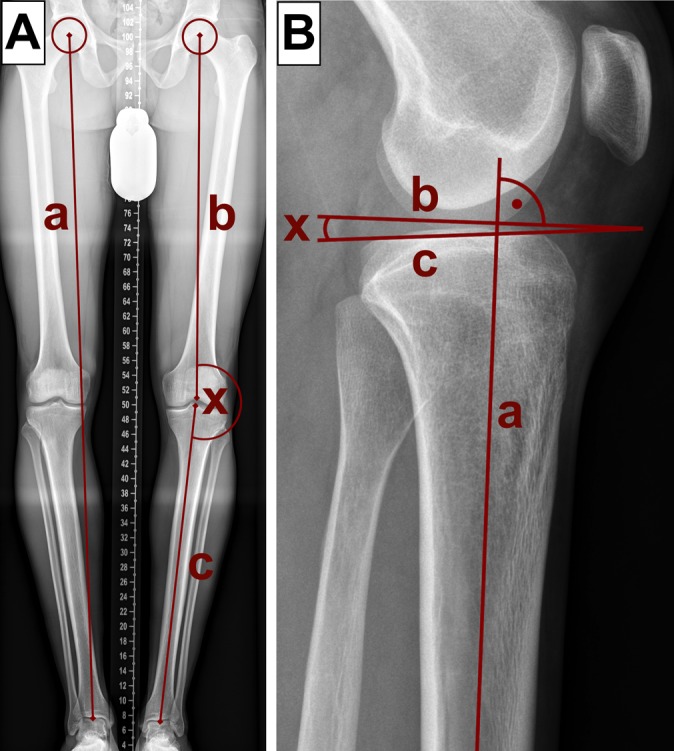
(A) Coronal alignment is analyzed using the weightbearing line of the lower limb (a) and the mechanical tibiofemoral angle (x), which is defined as the angle between the mechanical axes of the femur (b) and tibia (c), respectively. (B) The tibial slope is defined as the angle (x) between a line (b) perpendicular to the proximal anatomical axis of the tibia (a) and a tangent along the tibial plateau (c).
Conclusion
When treating cases of knee instability, the 3-dimensional osseous alignment of the knee should be analyzed. Basic parameters warranting analysis include the mechanical weightbearing axis and the tibial slope. Although no recommendations for realignment procedures in primary ACLR are currently available, in revision cases, changes in the tibial slope should be considered, and correction of abnormal slope is recommended in cases of the multiply revised ACL (level 3 evidence). In contrast, in cases of PLC instability, osseous correction of a varus thrust is often the first step in treatment, occasionally rendering secondary ligamentous stabilization unnecessary (level 4 evidence). Recommendations for the PCL regarding the tibial slope cannot be drawn from the clinical literature, but beneficial effects are suspected based on basic science studies. No clinical data are available for medial-sided knee instability or osseous alignment. Changes in the mechanical axis should be considered in all cases of knee instability together with early unicompartmental osteoarthritis. Future studies should focus on the amount of slope correction and whether slope correction plays a role in primary ACLR. Furthermore, the quality of future studies should be improved, especially by including control groups and randomizing treatment.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: T.T. is a consultant for Arthrex and Bauerfeind. J.P. is a consultant for Stryker. S.H. is a consultant for Arthrex. M.T.H. is a consultant for Depuy Synthes and Smith & Nephew; received a research grant from Mathys; and is a paid speaker for Arthrex and Zimmer. A.B.I. is a consultant for Arthrex and receives royalties from Arthrex and Arthrosurface.
References
- 1. Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124:575–584. [DOI] [PubMed] [Google Scholar]
- 2. Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23:852–861. [DOI] [PubMed] [Google Scholar]
- 3. Amis AA. Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21:197–205. [DOI] [PubMed] [Google Scholar]
- 4. Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med. 2007;35:1844–1850. [DOI] [PubMed] [Google Scholar]
- 5. Ayerza MA, Suarez F, Costa-Paz M, Muscolo DL. Can wedge osteotomy correct depression of the lateral tibial plateau mimicking posterolateral rotatory knee instability? Clin Orthop Relat Res. 2012;470:986–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Badhe NP, Forster IW. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc. 2002;10:38–43. [DOI] [PubMed] [Google Scholar]
- 7. Björnsson H, Andernord D, Desai N, et al. No difference in revision rates between single- and double-bundle anterior cruciate ligament reconstruction: a comparative study of 16,791 patients from the Swedish National Knee Ligament Register. Arthroscopy. 2015;31:659–664. [DOI] [PubMed] [Google Scholar]
- 8. Cantin O, Magnussen RA, Corbi F, Servien E, Neyret P, Lustig S. The role of high tibial osteotomy in the treatment of knee laxity: a comprehensive review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3026–3037. [DOI] [PubMed] [Google Scholar]
- 9. Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:2510–2514. [DOI] [PubMed] [Google Scholar]
- 10. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2–11. [DOI] [PubMed] [Google Scholar]
- 11. Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1566–1571. [DOI] [PubMed] [Google Scholar]
- 12. Dean CS, Liechti DJ, Chahla J, Moatshe G, LaPrade RF. Clinical outcomes of high tibial osteotomy for knee instability: a systematic review. Orthop J Sports Med. 2016;4:2325967116633419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:2846–2852. [DOI] [PubMed] [Google Scholar]
- 14. Dejour H, Neyret P, Boileau P, Donell ST. Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthop Relat Res. 1994;299:220–228. [PubMed] [Google Scholar]
- 15. El-Azab H, Halawa A, Anetzberger H, Imhoff AB, Hinterwimmer S. The effect of closed- and open-wedge high tibial osteotomy on tibial slope: a retrospective radiological review of 120 cases. J Bone Joint Surg Br. 2008;90:1193–1197. [DOI] [PubMed] [Google Scholar]
- 16. Faschingbauer M, Sgroi M, Juchems M, Reichel H, Kappe T. Can the tibial slope be measured on lateral knee radiographs? Knee Surg Sports Traumatol Arthrosc. 2014;22:3163–3167. [DOI] [PubMed] [Google Scholar]
- 17. Feucht MJ, Mauro CS, Brucker PU, Imhoff AB, Hinterwimmer S. The role of the tibial slope in sustaining and treating anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21:134–145. [DOI] [PubMed] [Google Scholar]
- 18. Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35:1443–1449. [DOI] [PubMed] [Google Scholar]
- 19. Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376–382. [DOI] [PubMed] [Google Scholar]
- 20. Griffith TB, Allen BJ, Levy BA, Stuart MJ, Dahm DL. Outcomes of repeat revision anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:1296–1301. [DOI] [PubMed] [Google Scholar]
- 21. Hetsroni I, Lyman S, Pearle AD, Marx RG. The effect of lateral opening wedge distal femoral osteotomy on medial knee opening: clinical and biomechanical factors. Knee Surg Sports Traumatol Arthrosc. 2014;22:1659–1665. [DOI] [PubMed] [Google Scholar]
- 22. Hinckel BB, Demange MK, Gobbi RG, Pecora JR, Camanho GL. The effect of mechanical varus on anterior cruciate ligament and lateral collateral ligament stress: finite element analyses. Orthopedics. 2016;39:e729–e736. [DOI] [PubMed] [Google Scholar]
- 23. Hinterwimmer S, Beitzel K, Paul J, et al. Control of posterior tibial slope and patellar height in open-wedge valgus high tibial osteotomy. Am J Sports Med. 2011;39:851–856. [DOI] [PubMed] [Google Scholar]
- 24. Hohmann E, Bryant A, Imhoff AB. The effect of closed wedge high tibial osteotomy on tibial slope: a radiographic study. Knee Surg Sports Traumatol Arthrosc. 2006;14:454–459. [DOI] [PubMed] [Google Scholar]
- 25. Hohmann E, Bryant A, Reaburn P, Tetsworth K. Does posterior tibial slope influence knee functionality in the anterior cruciate ligament-deficient and anterior cruciate ligament-reconstructed knee? Arthroscopy. 2010;26:1496–1502. [DOI] [PubMed] [Google Scholar]
- 26. Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467:2066–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kean CO, Birmingham TB, Garland JS, et al. Moments and muscle activity after high tibial osteotomy and anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2009;41:612–619. [DOI] [PubMed] [Google Scholar]
- 28. Kim SJ, Moon HK, Chun YM, Chang WH, Kim SG. Is correctional osteotomy crucial in primary varus knees undergoing anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2011;469:1421–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. LaPrade RF, Engebretsen L, Johansen S, Wentorf FA, Kurtenbach C. The effect of a proximal tibial medial opening wedge osteotomy on posterolateral knee instability: a biomechanical study. Am J Sports Med. 2008;36:956–960. [DOI] [PubMed] [Google Scholar]
- 30. Lattermann C, Jakob RP. High tibial osteotomy alone or combined with ligament reconstruction in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc. 1996;4:32–38. [DOI] [PubMed] [Google Scholar]
- 31. Lee SH, Jung YB, Lee HJ, Jung HJ, Kim SH. Revision posterior cruciate ligament reconstruction using a modified tibial-inlay double-bundle technique. J Bone Joint Surg Am. 2012;94:516–522. [DOI] [PubMed] [Google Scholar]
- 32. Li Y, Hong L, Feng H, Wang Q, Zhang H, Song G. Are failures of anterior cruciate ligament reconstruction associated with steep posterior tibial slopes? A case control study. Chin Med J (Engl). 2014;127:2649–2653. [PubMed] [Google Scholar]
- 33. Li Y, Hong L, Feng H, et al. Posterior tibial slope influences static anterior tibial translation in anterior cruciate ligament reconstruction: a minimum 2-year follow-up study. Am J Sports Med. 2014;42:927–933. [DOI] [PubMed] [Google Scholar]
- 34. Li Y, Zhang H, Zhang J, Li X, Song G, Feng H. Clinical outcome of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction for medial compartment osteoarthritis in young patients with anterior cruciate ligament-deficient knees: a systematic review. Arthroscopy. 2015;31:507–519. [DOI] [PubMed] [Google Scholar]
- 35. Lipps DB, Wilson AM, Ashton-Miller JA, Wojtys EM. Evaluation of different methods for measuring lateral tibial slope using magnetic resonance imaging. Am J Sports Med. 2012;40:2731–2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Marriott K, Birmingham TB, Kean CO, Hui C, Jenkyn TR, Giffin JR. Five-year changes in gait biomechanics after concomitant high tibial osteotomy and ACL reconstruction in patients with medial knee osteoarthritis. Am J Sports Med. 2015;43:2277–2285. [DOI] [PubMed] [Google Scholar]
- 37. MARS Group, Wright RW, Huston LJ, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38:1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Marx RG, Wilson SM, Swiontkowski MF. Updating the assignment of levels of evidence. J Bone Joint Surg Am. 2015;97:1–2. [DOI] [PubMed] [Google Scholar]
- 39. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 40. Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32:60–70. [DOI] [PubMed] [Google Scholar]
- 41. Noyes FR, Barber SD, Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees. A two- to seven-year follow-up study. Am J Sports Med. 1993;21:2–12. [DOI] [PubMed] [Google Scholar]
- 42. Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am J Sports Med. 2006;34:553–564. [DOI] [PubMed] [Google Scholar]
- 43. Noyes FR, Barber-Westin SD. Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33:646–654. [DOI] [PubMed] [Google Scholar]
- 44. Noyes FR, Barber-Westin SD, Albright JC. An analysis of the causes of failure in 57 consecutive posterolateral operative procedures. Am J Sports Med. 2006;34:1419–1430. [DOI] [PubMed] [Google Scholar]
- 45. Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28:282–296. [DOI] [PubMed] [Google Scholar]
- 46. Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–1443. [DOI] [PubMed] [Google Scholar]
- 47. Petrigliano FA, Suero EM, Voos JE, Pearle AD, Allen AA. The effect of proximal tibial slope on dynamic stability testing of the posterior cruciate ligament– and posterolateral corner–deficient knee. Am J Sports Med. 2012;40:1322–1328. [DOI] [PubMed] [Google Scholar]
- 48. Reichwein F, Nebelung W. High tibial flexion osteotomy for revision of posterior cruciate ligament instability [in German]. Unfallchirurg. 2007;110:597–602. [DOI] [PubMed] [Google Scholar]
- 49. Saito K, Hatayama K, Terauchi M, Hagiwara K, Higuchi H, Takagishi K. Clinical outcomes after anatomic double-bundle anterior cruciate ligament reconstruction: comparison of extreme knee hyperextension and normal to mild knee hyperextension. Arthroscopy. 2015;31:1310–1317. [DOI] [PubMed] [Google Scholar]
- 50. Shelburne KB, Kim HJ, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29:223–231. [DOI] [PubMed] [Google Scholar]
- 51. Shelburne KB, Pandy MG, Torry MR. Comparison of shear forces and ligament loading in the healthy and ACL-deficient knee during gait. J Biomech. 2004;37:313–319. [DOI] [PubMed] [Google Scholar]
- 52. Sonnery-Cottet B, Mogos S, Thaunat M, et al. Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:1873–1880. [DOI] [PubMed] [Google Scholar]
- 53. van de Pol GJ, Arnold MP, Verdonschot N, van Kampen A. Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med. 2009;37:481–487. [DOI] [PubMed] [Google Scholar]
- 54. Voos JE, Suero EM, Citak M, et al. Effect of tibial slope on the stability of the anterior cruciate ligament–deficient knee. Knee Surg Sports Traumatol Arthrosc. 2012;20:1626–1631. [DOI] [PubMed] [Google Scholar]
- 55. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament–reconstructed patient. Am J Sports Med. 2013;41:2800–2804. [DOI] [PubMed] [Google Scholar]
- 56. Williams RJ, 3rd, Kelly BT, Wickiewicz TL, Altchek DW, Warren RF. The short-term outcome of surgical treatment for painful varus arthritis in association with chronic ACL deficiency. J Knee Surg. 2003;16:9–16. [PubMed] [Google Scholar]
- 57. Won HH, Chang CB, Je MS, Chang MJ, Kim TK. Coronal limb alignment and indications for high tibial osteotomy in patients undergoing revision ACL reconstruction. Clin Orthop Relat Res. 2013;471:3504–3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85-A:1–3. [PubMed] [Google Scholar]
- 59. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94:531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zaffagnini S, Bonanzinga T, Grassi A, et al. Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc. 2013;21:934–941. [DOI] [PubMed] [Google Scholar]


