Abstract
Background:
Literature on arthroscopic stabilization in adolescent patients participating in collision and contact sports is limited, as most studies include adolescents within a larger sample group comprised primarily of adults.
Purpose:
To review the outcomes of arthroscopic Bankart repair for anterior shoulder instability in an adolescent population participating in collision and contact sports.
Study Design:
Case series; Level of evidence, 4.
Methods:
This retrospective review included 39 shoulders in 37 adolescent (≤19 years) athletes who underwent primary arthroscopic Bankart repair using suture anchors with at least 2-year follow-up. All patients had a history of trauma to their shoulder resulting in an anterior dislocation. Outcome measures included patient satisfaction, the visual analog scale (VAS) for pain, American Shoulder and Elbow Surgeons (ASES) score, and Rowe score. Recurrence of dislocation and return to sporting activity were also assessed.
Results:
The mean age at the time of surgery was 16.9 years (range, 15-19 years), and the mean follow-up was 6.3 years (range, 4.3-10.0 years); 58.6% of patients participated in collision sports. Time to surgery after the initial dislocation episode was 9.2 months (range, 0.5-36.2 months). Four shoulders (10.3%) had dislocation events postoperatively. The majority (78.1%) of patients returned to sports at the same level of competition. Mean VAS was 0.49 ± 1.0, and the mean ASES and Rowe scores were 92.8 ± 12.6 and 85.0 ± 24.2, respectively. Univariate analyses demonstrated that subjective functional outcomes were negatively correlated with recurrence (ASES, P = .005; Rowe, P = .001) and failure to return to sport (ASES, P = .016; Rowe, P = .004). Independent variables shown to have no significant relationship to functional outcomes included age, follow-up, number of preoperative dislocations, time to surgery, sport classification, competition level, tear extent, number of anchors, concurrent Hill-Sachs lesion, and repair of a superior labral anterior-posterior (SLAP) lesion.
Conclusion:
Arthroscopic Bankart repair is an effective surgical option for traumatic shoulder instability in adolescents participating in collision and contact sports. At a minimum 4-year follow-up, arthroscopic Bankart repair effectively restored stability in 90% of cases; 80% returned to their preinjury level of sport.
Keywords: anterior shoulder instability, glenoid labrum, Bankart, labral repair, adolescents
Since Bankart3 described recurrent shoulder dislocation in 1923, various treatment options have been proposed to address anterior dislocations and instability. Currently, open and arthroscopic procedures are widely used, and considerable debate exists as to which one represents the best option for the patient. In recent years, many studies have emerged to address arthroscopic repairs in athletes, in whom shoulder instability events have been shown to occur at a rate of 0.12 per 1000 exposures.24 Athletes participating in collision sports (eg, football and rugby) and contact sports (eg, wrestling and basketball) are at a notably high risk for injury.7,10,18–20,27 Recurrent dislocation is common in this population, particularly in young athletes where the reported rate of recurrence after arthroscopic Bankart repair ranges from 5.1% to 31%.4,6,8,9,14,15,18,20,32
However, a review of the literature on collision and contact athletes revealed that the majority of these included heterogeneous patient populations and have combined adult and adolescent athletes.4,8,14,18,22,25,32 In addition, the level of sport involvement and classification in terms of contact are often not clearly defined. Although excellent short-term results have been reported, there have been few studies specifically examining arthroscopic Bankart repairs in the adolescent population.6,9,15,20 However, only 1 study included athletes participating in collision sports.20 Athletic participation is common among adolescents, with more than half of all high school students participating in school-sanctioned sports during the 2014-2015 academic year.1 With increasing student participation in high school athletics over the past decade, traumatic anterior shoulder dislocations continue to be more prevalent. Improving our knowledge of these common injuries is crucial to help drive targeted evidence-based treatment strategies.
The purpose of this study was to review the clinical and functional outcomes after arthroscopic Bankart repair in a group of adolescent athletes participating in collision and contact sports. We sought to identify any demographic, injury, and surgical factors affecting patient-reported functional outcomes. Secondarily, we sought to characterize recurrent instability events and the success of return to sport. We hypothesized that excellent results would be observed in this population at a minimum 2-year follow-up.
Methods
Patient Selection
We retrospectively reviewed a consecutive series of adolescent patients who underwent primary arthroscopic Bankart repair with a minimum follow-up of 2 years. All surgical procedures were performed by 2 fellowship-trained sports medicine surgeons between 2004 and 2012. Patients were identified through a Current Procedural Terminology code search of an institutional computerized database using the code 29806 (arthroscopic shoulder capsulorrhaphy). We included those patients aged 10 to 19 years, consistent with the World Health Organization’s definition of adolescence.33 Cases were limited to collision, contact, or limited contact athletes according to criteria established by the American Academy of Pediatrics28 (Table 1). All patients, including limited contact (eg, baseball) athletes, had a history of a traumatic injury to their shoulder resulting in an anterior glenohumeral dislocation confirmed on history, physical examination, and magnetic resonance imaging (MRI) findings. Dislocation was defined as an instability event requiring manual reduction. Furthermore, all patients had a Bankart lesion confirmed at the time of surgery. Those with an extension of the lesion into the superior labrum (ie, superior labrum anterior-posterior [SLAP] tear) or posterior labrum were also included, and there were no limits regarding concomitant procedures. Exclusion criteria for this study were (1) less than 2-year follow-up in the patient’s medical record, (2) atraumatic or multidirectional instability, (3) patients with posterior instability as documented in the chart, (4) glenoid bone loss greater than 20% as assessed on preoperative MRI,31 (5) an engaging Hill-Sachs lesion identified during standardized examination under anesthesia,5 (6) an associated full-thickness rotator cuff tear, and (7) humeral avulsion of the glenohumeral ligament. Twenty-seven patients failed to meet the appropriate criteria and were excluded from the cohort. A detailed flow diagram is included in Figure 1. In total, 37 patients (39 shoulders) met the inclusion criteria.
TABLE 1.
Classification of Sports by Contacta
| Collision | Contact | Limited contact |
|---|---|---|
| Football | Basketball | Baseball |
| Ice hockey | Wrestling |
aAccording to the American Academy of Pediatrics.
Figure 1.
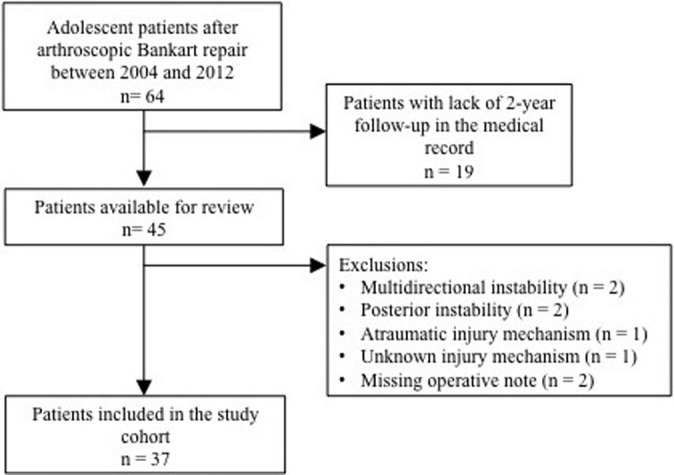
Flow diagram outlining patient selection.
Operative Technique
The same arthroscopic technique was used in each case. Preoperatively, all patients received an interscalene nerve block with in-dwelling catheter. Surgery was performed with patients in the lateral decubitus position with the operative extremity placed in balanced suspension at approximately 60° of abduction using 10 to 15 pounds of axial traction. A standard posterior viewing portal was established in addition to 2 anterior working portals in the rotator interval. One was placed lower, just superior to the subscapularis tendon; the other was placed higher, just inferior to the biceps tendon. Systematic diagnostic arthroscopy was performed, and any intra-articular pathology was addressed. Complete mobilization of the anterior labrum from the glenoid neck was done to prevent a nonanatomic, less functional repair. A small burr was then used to create a bleeding bed of bone along the neck of the glenoid. The drill guide for the 3-mm BioComposite SutureTac anchor (Arthrex) was introduced through the inferior cannula and positioned on the face of the glenoid as close to the 6 o’clock position as possible. A pilot hole was drilled and the anchor was then tapped into the glenoid. A suture passer was used to shuttle 1 of the suture limbs through the capsule and labrum. The goal was to get a healthy capsular bite, grabbing inferior to the anchor in an effort to shift the tissue superiorly, reducing capsular volume. Knots were tied arthroscopically using low-profile sliding knots with care to keep the knots away from the glenoid face. Any posterior labral pathology was addressed in a similar fashion. In cases where a type II SLAP tear was also present, a shaver was used to debride the superior glenoid neck. After needle localization, a drill guide was placed percutaneously through the muscular portion of the supraspinatus into the glenohumeral joint. Anchors were placed along the superior glenoid. A spinal needle was introduced into the joint from the Neviaser portal and passed under the superior labrum. A No. 1 PDS (polydioxanone) suture (Ethicon) was used to shuttle one of the suture limbs under the labrum. Both limbs were brought out through the anterior cannula and tied with a sliding knot. Nonabsorbable sutures were used for skin closure, and a shoulder sling with abduction pillow was placed. All patients were discharged home with instructions to remove the interscalene catheter 3 to 4 days postoperatively.
Postoperative Management
Postoperative rehabilitation was initiated 5 to 7 days from the time of surgery and consisted of 5 separate phases. The shoulder sling with abduction pillow was worn during the first 6 weeks. During that time, passive and gentle active assistive range of motion (ROM) exercises were initiated, but no active external rotation, extension, or abduction of the shoulder was allowed. During weeks 5 through 6, the patient worked to gradually improve ROM and stretching exercises were begun. Phase 2 goals included working to gradually restore full ROM (ideally by week 10), restoring muscular strength and balance, and enhancing neuromuscular control. More aggressive strengthening and ROM were progressed to meet functional demands (ie, overhead athletes). In cases where a concomitant SLAP tear was repaired, no isolated biceps contractions were allowed until week 5. Phases 3 and 4 focus on strength, power, and endurance, as well as the progression of functional activities. At 7 months, patients return to sport activities. The timing and goals of each phase are presented in Table 2.
TABLE 2.
Rehabilitation Protocola
| Phase | Timing | Goals |
|---|---|---|
| 1 | Weeks 0-6 | Protect the repair |
| Prevent negative effects of immobilization | ||
| Promote dynamic stability and proprioception | ||
| Diminish pain and inflammation | ||
| 2 | Weeks 7-14 | Restore full ROM |
| Preserve the integrity of the repair | ||
| Restore muscular strength and balance | ||
| Enhance neuromuscular control | ||
| 3 | Weeks 15-20 | Improve muscular strength, power, and endurance |
| Gradually initiate functional activities | ||
| 4 | Weeks 21-24 | Enhance muscular strength, power, and endurance |
| Progress functional activities | ||
| 5 | Months 7-9 | Gradual return to sport activities |
aROM, range of motion.
Clinical Evaluation
Operative and clinical notes were extracted from medical records. Preoperative assessment included age, mechanism and severity of injury, as well as the number of instability events prior to repair. Intraoperative findings included examination under anesthesia, number of anchors used in the repair, and any additional abnormal findings noted. Postoperative assessment included recurrence of dislocation and any postoperative complications. Patient-reported outcomes and functional activity levels were evaluated using the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES),21 Rowe Score for Instability,29 and visual analog scale (VAS) for pain. Patient satisfaction was assessed with 0- to 10-point scale scores, where 0 was considered “completely dissatisfied” and 10 considered “completely satisfied.” Return to sport was directly assessed using a special questionnaire. Patients were also asked about their ability to return to sports.
Statistical Analyses
Descriptive statistics were calculated. Continuous variables were expressed as means and ranges or standard deviations (SDs), and categorical variables were expressed as number and percentage. The normality of distribution of dependent variables (ASES and Rowe scores) was tested using the Shapiro-Wilk test. Univariate analysis was performed. The associations between nominal and dichotomous independent variables and clinical outcomes were analyzed using the Kruskal-Wallis test and Wilcoxon rank-sum test, respectively. The correlations between continuous independent variables and clinical outcomes were examined using Spearman rank correlation. Multiple linear regression analyses were performed to identify variables that were predictive of ASES and Rowe scores. Independent variables that had a P value of <.2 from the univariate analyses were included in each of the 2 multivariate analyses. Statistical significance was set at P ≤ .05. All data were tabulated in Microsoft Excel (2012 version; Microsoft) and analyses conducted using PASW Statistics 21.0.
Results
Athlete Characteristics
Athlete characteristics are summarized in Table 3. The mean age at the time of surgery was 16.9 years (range, 15-19 years), and the mean follow-up was 6.3 years (range, 4.3-9.9 years). More than half (58.6%) of the patients participated in collision sports, and the majority (69%) had multiple preoperative dislocations prior to surgical intervention. Time to surgery after the initial dislocation episode was 8.9 months (range, 0.5-25.7 months), and the most common mechanism of injury was a tackle during football. The nondominant arm was involved in 5 patients.
TABLE 3.
Athlete Characteristicsa
| Characteristic | Data (n = 39 shoulders) |
|---|---|
| Age at surgery, y | 16.9 ± 1.5 |
| Sex | |
| Male | 38 (96.6) |
| Female | 1 (3.4) |
| Dominant side affected | |
| No | 5 (13) |
| Yes | 34 (87) |
| Follow-up, mo | 75.2 ± 18.5 |
| Sport classification | |
| Collision | 24 (61.5) |
| Contact | 5 (12.8) |
| Limited contact | 10 (25.6) |
| Sport | |
| Football | 22 (56.4) |
| Baseball | 10 (25.6) |
| Basketball | 3 (7.7) |
| Wrestling | 2 (5.1) |
| Hockey | 2 (5.1) |
| Level of competition | |
| High school | 28 (71.8) |
| College | 8 (20.5) |
| Recreational | 3 (7.7) |
| Mechanism of injury | |
| Diving for ball | 8 (20.5) |
| Fall | 1 (2.6) |
| Hyperabduction | 6 (15.4) |
| Tackle | 24 (61.5) |
| Preoperative instability episodes | |
| Single | 12 (30.8) |
| Multiple | 27 (69.2) |
| Instability Severity Index scoreb | 6.6 (0.8) |
| Time to surgery, mo | 8.9 ± 9.6 |
aData are reported as mean ± SD or n (%).
bBalg F, Boileau P.2
Arthroscopic Findings
Arthroscopic findings are reported in Table 4. A nonengaging Hill-Sachs lesion was observed in 33 shoulders (84.6%). The extent of the labrum tear was quantified with use of clock-face coordinates. The mean magnitude of injury was 3.9 hours (range, 1-8 hours). The mean number of anchors used for the Bankart repair was 4.6 ± 1.7. After placement of anterior anchors, additional anchors were placed posteriorly (beyond the 6 o’clock position) in 1 patient (2.6%). A type II SLAP tear was present and repaired in 9 shoulders (23.1%). The mean number of anchors used for the SLAP repair was 1.8 (range, 1-3). Three patients underwent an additional procedure at the same time as the index stabilization. These included rotator interval closure in 2 patients (5.1%) and subacromial decompression with partial-thickness rotator cuff repair in 1 patient (2.6%).
TABLE 4.
Arthroscopic Findingsa
| Characteristic | Data (n = 39 shoulders) |
|---|---|
| Hill-Sachs lesion, n | 33 (84.6) |
| SLAP repair, n | 9 (23.1) |
| Tear extent, h | 3.9 ± 1.6 |
| Superior anchor position, h | 2 ± 1.3 |
| Inferior anchor position, h | 5.6 ± 0.6 |
| Anchors used (Bankart), n | 4.6 ± 1.7 |
| Anchors used (SLAP), n | 1.8 ± 0.7 |
| Additional procedures, n | 4 (10.3) |
aData are reported as mean ± SD or n (%). SLAP, superior labral anterior-posterior.
Complications
One superficial portal site infection resolved after a short course of oral antibiotics. One patient had a transient sensory brachial plexopathy due to interscalene anesthesia that resolved within 8 weeks of surgery. Neither complication resulted in recurrent instability.
Recurrent Instability
Four shoulders (10.3%) had dislocation events postoperatively; all were traumatic. One was a 15-year-old male baseball player who sustained a recurrence while diving for a ball 3 years after his initial surgery. Although he was able to return to sports with a brace, he continued to have pain and instability symptoms. Another patient was a 19-year-old male recreational basketball player who redislocated 2 years postoperatively during a basketball game. He underwent open revision without any subsequent instability episodes. The third patient was a 15-year-old male basketball player who redislocated 13 months postoperatively. He underwent open revision by another surgeon but continued to have pain and instability symptoms. The last patient was an 18-year-old high school football player who redislocated 1 year postoperatively during a tackle while playing with a semiprofessional football team. He chose nonoperative treatment and quit playing football after the injury.
Return to Sports
Return to sports data were available for 36 of 37 patients (97.3%). A total of 32 patients (88.9%) attempted to return to sports postoperatively. Of those, 25 patients (78.1%) were able to return to sports at the same level for at least 1 season. Three patients graduated high school and did not attempt return. One patient who was a high school senior did not return for other reasons. Seven patients (21.9%) were unable to return to sports or had to return at a lower level of competition. Three of those were patients who sustained their initial injury during high school football but were multisport athletes. One was able to return to football but was unable to get back to pitching in baseball due to pain. The second patient sustained a contralateral scaphoid fracture and did not return to football. He was trying out for the school’s baseball team at the time of follow-up. The third patient was able to return to football but was unable to wrestle secondary to fear of reinjury. Three athletes were unable to return to sport due to recurrent instability; 1 underwent nonoperative treatment and elected to quit his sport. The other 2 patients both received surgical treatment with soft tissue procedures for recurrent instability. The remaining athlete who was unable to return to sport underwent repeat arthroscopy for persistent shoulder pain. All patients who had subsequent surgical intervention cited shoulder limitations as the reason for inability to continue playing sports.
Subjective Outcome Measures
Subjective questionnaires and functional outcome measures were available for 90% of patients. Mean VAS was 0.49 ± 1.0, and the mean ASES and Rowe scores were 92.8 ± 12.6 and 85.0 ± 24.2, respectively. The mean satisfaction score was 8.9 ± 1.9. Eighty percent of patients reported satisfaction scores of 8 points or higher (10 being “completely satisfied”) (Table 5).
TABLE 5.
Clinical Outcomesa
| Outcome Measure | Data |
|---|---|
| VAS | 0.49 ± 1.0 |
| ASES | 92.8 ± 12.6 |
| Rowe | 85.0 ± 24.2 |
| Patient satisfactionb | 8.9 ± 1.9 |
| Recurrence | |
| Yes | 4 (10.3) |
| No | 35 (89.7) |
| Return to sport | |
| Did not attempt return | 4 (11.1) |
| Attempted return | 32 (86.4) |
| Able to return | 25 (78.1) |
| Unable to return | 7 (21.9) |
aData are reported as mean ± SD or n (%). ASES, American Shoulder and Elbow Surgeons; VAS, visual analog scale.
bMeasured by a 0- to 10-point subjective scale.
Univariate analyses demonstrated that subjective functional outcomes were negatively correlated with recurrence (ASES, P = .005; Rowe, P = .001) and failure to return to sport (ASES, P = .016; Rowe, P = .004). Independent variables shown to have no significant relationship to subjective functional outcomes included age, follow-up, number of preoperative dislocations, time to surgery, sport classification, competition level, tear extent, number of anchors, concurrent Hill-Sachs lesion, and repair of a SLAP lesion (Table 6).
TABLE 6.
Results of Univariate Analysesa
| P Value | ||
|---|---|---|
| Characteristic | ASES | Rowe |
| Age at surgery | .789 | .424 |
| Sex | .347 | .373 |
| Hand dominance | .104 | .049 b |
| Follow-up | .113 | .302 |
| Sport classification | .120 | .109 |
| Sport | .228 | .211 |
| Level of competition | .828 | .696 |
| Mechanism of injury | .182 | .151 |
| Instability Severity Index score | .918 | .779 |
| Preoperative instability episodes | .882 | .744 |
| Hill-Sachs lesion | .792 | .970 |
| SLAP repair | .442 | .194 |
| Tear extent | .783 | .910 |
| Bankart extent | .280 | .715 |
| Anchors used (Bankart) | .072 | .324 |
| Anchors used (SLAP) | .339 | .521 |
| Recurrence | .004 b | .001 b |
| Return to sport | .016 b | .004 b |
| Time to surgery | .381 | .109 |
aBoldfaced P values indicate inclusion in the multivariate regression analysis (P < .2). ASES, American Shoulder and Elbow Surgeons; SLAP, superior labral anterior-posterior.
bStatistically significant (P < .05).
Multivariate regression analyses were run to evaluate how well independent risk factors predicted ASES and Rowe scores. Risk factors and their coefficients are shown in Table 7. For ASES score, the independent risk factors injury side, follow-up duration, collision, injury mechanism, number of Bankart anchors, postoperative recurrence, and return to sport significantly predicted score: F(10, 17) = 3.215, P = .0167, R 2 = 0.654. Within this analysis, only postoperative recurrence added significantly to the prediction (P = .011). For Rowe score, the independent risk factors injury side, collision, injury mechanism, SLAP tear, postoperative recurrence, return to sport, and time to surgery significantly predicted score: F(10, 17) = 10.62, P < .001, R 2 = 0.862. Within this analysis, only postoperative recurrence added significantly to the prediction (P < .001). The results of these analyses indicate that athletes who have postoperative recurrence tend to have lower ASES and Rowe scores.
TABLE 7.
Independent Risk Factors Predicting Clinical Outcome Scores Identified by Multivariate Regression Analysesa
| ASES | Rowe | |||
|---|---|---|---|---|
| Variable | R 2 | P Value | R 2 | P Value |
| Hand dominance | ||||
| Nondominant | –15.92 | .109 | –26.41 | .062 |
| Follow-up | 0.001 | .741 | N/A | N/A |
| Sport classification | ||||
| Contact | 3.96 | .691 | 10.56 | .410 |
| Limited contact | –8.19 | .580 | 7.71 | .664 |
| Mechanism of injury | ||||
| Fall | –2.11 | .911 | 27.86 | .242 |
| Hyperabduction | –6.79 | .454 | –2.47 | .808 |
| Tackle | –6.88 | .648 | 9.78 | .596 |
| SLAP repair | ||||
| Yes | N/A | N/A | –10.73 | .102 |
| Anchors used (Bankart) | –1.3 | .385 | N/A | N/A |
| Recurrence | ||||
| Yes | –20.99 | .011b | –55.71 | <.001b |
| Return to sport | ||||
| Yes | –1.6 | .777 | 3.37 | .592 |
| Time to surgery | N/A | N/A | –0.02 | .083 |
aFor ASES, dominant-sided injury, collision, diving for ball, no postoperative recurrence, and no return to sport serve as the reference group. For Rowe, dominant-sided injury, collision, diving for ball, no SLAP tear, no postoperative recurrence, and no return to sport serve as the reference group. ASES, American Shoulder and Elbow Surgeons; N/A, not applicable; SLAP, superior labral anterior-posterior.
bStatistically significant (P < .05).
Discussion
The principal findings of this study suggest that arthroscopic Bankart repair is an effective surgical option for traumatically induced shoulder instability in adolescents participating in collision and contact sports at mid-term follow-up. At a minimum of 4 years after surgery, shoulder stability was effectively restored in 90% of cases; 80% returned to their preinjury level of sport. Arthroscopic Bankart repair provided excellent subjective functional outcomes. Variables significantly associated with lower ASES and/or Rowe scores were postoperative recurrence and failure to return to sports.
The goals of arthroscopic Bankart repair are to restore shoulder stability and the native biomechanics of the shoulder to alleviate discomfort and restore function. In both the pediatric and young adult populations, the natural history after primary anterior shoulder dislocation has been extensively studied. A systematic review and meta-analysis by Olds et al23 revealed that adolescents (aged 14-18 years) were 24 times more likely to experience recurrent instability after a first-time traumatic anterior shoulder dislocation than children younger than 14 years old. Hovelius11 reported on a large cohort of teenagers and young adults in which 2 or more recurrences occurred in 55% of patients (≤22 years old) who received nonoperative treatment. In a prospective study with 25-year follow-up, 60% of patients aged 12 to 16 years experienced a recurrence.12 In a 10-year prospective study by Hovelius et al,13 the authors reported that 40% of their 12- to 19-year-old patients ultimately required surgical stabilization. Furthermore, they found that the incidence of mild to moderate osteoarthritis after conservative treatment for anterior shoulder dislocation was 20%. Recent studies have reported decreased rates of recurrent instability and improved outcomes in patients treated with surgical stabilization.4,10,16
More recent studies have focused on the outcomes of arthroscopic anterior stabilization in adults using validated shoulder outcome scores. Milchteim et al22 examined the results of arthroscopic Bankart repair using suture anchors in 89 highly active patients with a mean age of 21.9 years. The success rate was 94% at a mean follow-up of 5 years. Ozturk et al26 reported on a series of 53 patients aged younger than 25 years who underwent arthroscopic capsulolabral repair with an 87% clinical success rate and a mean follow-up of 27 months. Voos et al32 reported on a series of 73 patients with a mean age of 32.6 years who underwent arthroscopic Bankart repair. The clinical success rate was 82% after a mean follow-up of 2.7 years. All of these studies concluded that arthroscopic stabilization should be considered an effective surgical option in the young, athletic population.
In contrast, other authors have found that major risk factors for recurrence after arthroscopic Bankart repair include younger age (≤20 years), those in competitive sports, and contact or forced-overhead athletes.2 They recommended that those patients with more than 6 points on the Instability Severity Index score have an unacceptably high (70%) recurrence risk and should be advised to undergo open surgery. Interestingly, the recurrence rate in our cohort was 10.3% despite a mean Instability Severity Index score of 6.6. Reasons for these findings are unclear, but of note, the treating surgeons in this study did not utilize the Instability Severity Index scoring system in the decision-making process. Furthermore, while it was not the purpose of this study to examine risk factors for recurrence, our study found no correlation between Instability Severity Index score and patient-reported outcomes. These results illustrate that arthroscopic Bankart repair can be an effective treatment option in young athletes.
Despite the abundance of studies on the adult population, there remain limited data on arthroscopic Bankart repair in adolescents. Deitch et al9 were among the first to address clinical outcomes of arthroscopic Bankart repair using suture anchors in this younger population. They retrospectively examined 32 patients between 11 and 18 years of age who sustained a traumatic anterior shoulder dislocation; 50% of patients underwent surgical stabilization, and at a mean 4-year follow-up, the recurrence rate was 31% and the mean postoperative Single Assessment Numeric Evaluation (SANE) and Rowe scores were 77.3 and 75.6, respectively. In contrast, Jones et al15 reported on a series of 32 shoulders in 30 patients aged 11 to 18 years with a mean follow-up of 25.2 months. The mean postoperative SANE score was 92, and recurrent instability developed in 15.6% of patients. A study by Mazzocca et al20 examined the results of arthroscopic Bankart repair in 13 collision and 5 contact athletes younger than 20 years. With a mean follow-up period of 37 months, the average postoperative ASES was 90 while the postoperative Rowe scores in collision and contact athletes were 94.2 and 92, respectively. Instability recurred in 11% of patients after 2 years. Castagna et al6 investigated the outcomes in 67 patients (aged 13-18 years) participating in overhead or contact sports with a mean follow-up of 63 months. The authors reported mean postoperative SANE, ASES, and Rowe scores of 87.2, 84.1, and 85, respectively. The recurrence rate was 21%, and the authors determined that type of sport practiced was associated with recurrence rate. Overall, the subjective functional outcomes in our patient cohort fell between those reported in the literature, and notably, our recurrence rate of 10.3% is slightly lower than those previously reported for an adolescent population.
Collision athletes have been reported to be at an increased risk of redislocation after arthroscopic stabilization for anterior shoulder instability.7,20,27 Cho et al7 compared 14 collision athletes to 15 noncollision athletes with a mean age of 21.1 years. At a mean follow-up of 62.1 months, there were no differences in subjective functional outcomes or ability to return to preinjury sports activity levels between the groups. However, the collision group had a higher recurrence rate (28.6% vs 6.7%). Rhee et al27 reviewed 16 collision athletes (5 football players) with a mean age of 18.2 years. At a mean follow-up of 66.8 months, instability had recurred in 25% of patients, and only 4 patients were able to return to preinjury activity levels. While those studies focused on Bankart repairs, we reported on Bankart tears seen specifically in the adolescent population. In fact, to our knowledge, this is the largest study to report on the outcomes and rates of revision for arthroscopic Bankart repair specifically in adolescent athletes participating in collision and contact sports. Our recurrence rate is slightly lower (10.3% vs 11%) than that in the series of Mazzocca et al,20 while the proportion of athletes who participated in collision sports was similar (66.7% vs 72.2%).
The overall return-to-sport rate in our study was 78.1%, as 25 of 32 patients who attempted to return were ultimately able to return to sports at the same level of competition. This is consistent with several previous reports. Jones et al15 found that 93% (25/27) of adolescent patients who identified themselves as athletes successfully returned to their respective sport after arthroscopic Bankart repair. All athletes returned at their preinjury level. Similarly using suture anchors, Mazzocca et al20 reported that 100% of the 18 collision and contact athletes in their study returned to their level of competition by a mean 5.7 months after surgery. Castagna et al6 reported that 100% (65/65) of athletes returned to play sports after arthroscopic Bankart repair with suture anchors, but only 81.5% (53/65) came back at their preinjury level. The varied return-to-sport outcomes in the literature can be explained by the study populations evaluated, as differences in follow-up periods or patient background (eg, sport classification, level of competition, or physical status) could have affected the difference in rates between our study and previous research.
In our study, multiple independent risk factors predicted ASES and Rowe scores. Of these factors, postoperative recurrence was the only one that contributed significantly to the prediction. Athletes who had postoperative recurrence were predicted to score 21 and 56 points lower for ASES and Rowe evaluations, respectively. Naturally, a recurrent injury would negatively affect the patient’s subjective outcome. Moreover, both outcome scores are heavily weighted toward stability so it is not surprising that these scores are lower in patients with recurrence. Despite assessing ADLs, ability to return to sport may not be a predictor of ASES or Rowe score due to floor and ceiling effect limitations and nonspecific question constriction.17,30 This could possibly explain why return to sport was significant in univariate analysis but not in the multiple regression models with ASES and Rowe scores as the dependent variables. To our knowledge, the present study is the first to describe an association between injury to a nondominant shoulder and subjective outcome after arthroscopic Bankart repair. However, while a nondominant shoulder injury was associated with lower Rowe scores on univariate analysis, this finding did not significantly contribute to the regression prediction. Again, this can be explained by the limitations in content validity of the Rowe scoring system for measuring levels of function. Nevertheless, adolescents suffering an injury to their nondominant shoulder should be counseled regarding a greater risk of a lower functional outcome after surgery, especially when other factors that place them at greater risk for failing to return to sport are identified.
The results of this study must be interpreted based on the following limitations. This was a retrospective study with no comparison group to contrast our technique directly with another method for treating patients who sustained primary traumatic anterior shoulder dislocation. Our data do not reflect long-term outcomes, and it is possible that some of these athletes would have recurrent pain or instability with longer follow-up. Additionally, 27 patients did not have adequate 2-year follow-up and were not included in the study cohort, and it is possible that if they had a recurrence, they sought treatment elsewhere. The sample size was fairly small, but this is explained by a variety of factors. For one, the study involved just 2 treating surgeons, and the senior author did not begin seeing patients in our clinic full-time until April 1, 2011. Furthermore, we only examined patients in collision, contact, and limited-contact sports according to a previously established guideline for sport classification. There is high variability in the classification of different sports, which makes comparison difficult. Most previous studies did not define how they classified sport type and/or included patients in noncontact sports. Nevertheless, this study does represent one of the largest investigations of Bankart tears in this specific, homogeneous population.
Conclusion
Arthroscopic Bankart repair is an effective surgical option for traumatically induced anterior shoulder instability in adolescents participating in collision and contact sports. At a minimum 4-year follow-up, arthroscopic Bankart repair effectively restored stability in 90% of cases; 80% returned to their preinjury level of sport.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Arthrex Inc provides research support to the Andrews Research and Education Foundation (AREF), a nonprofit organization. AREF sponsors an orthopaedic sports medicine fellowship, of which J.R.A. is the director and R.V.O. is the assistant director.
Ethical approval for this study was obtained by Baptist Hospital–Pensacola.
References
- 1. Athletics participation survey. 2015-16. NFHS Handbook_2007-08 NFHS Handbook.qxd. http://www.nfhs.org/ParticipationStatics/PDF/2014-15_Participation_Survey_Results.pdf. Accessed January 18, 2016.
- 2. Balg F, Boileau P. The instability severity index score. Bone Joint J. 2007;89:1470–1477. [DOI] [PubMed] [Google Scholar]
- 3. Bankart ASB. Recurrent or habitual dislocation of the shoulder-joint. Br Med J. 1923;2:1132–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576–580. [DOI] [PubMed] [Google Scholar]
- 5. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. [DOI] [PubMed] [Google Scholar]
- 6. Castagna A, Delle Rose G, Borroni M, et al. Arthroscopic stabilization of the shoulder in adolescent athletes participating in overhead or contact sports. Arthroscopy. 2012;28:309–315. [DOI] [PubMed] [Google Scholar]
- 7. Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy. 2006;22:947–953. [DOI] [PubMed] [Google Scholar]
- 8. DeBerardino TM, Arciero RA, Taylor DC, Uhorchak JM. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes. Two- to five-year follow-up. Am J Sports Med. 2001;29:586–592. [DOI] [PubMed] [Google Scholar]
- 9. Deitch J, Mehlman CT, Foad SL, Obbehat A, Mallory M. Traumatic anterior shoulder dislocation in adolescents. Am J Sports Med. 2003;31:758–763. [DOI] [PubMed] [Google Scholar]
- 10. Good CR, MacGillivray JD. Traumatic shoulder dislocation in the adolescent athlete: advances in surgical treatment. Curr Opin Pediatr. 2005;17:25–29. [DOI] [PubMed] [Google Scholar]
- 11. Hovelius L. Anterior dislocation of the shoulder in teen-agers and young adults. Five-year prognosis. J Bone Joint Surg Am. 1987;69:393–399. [PubMed] [Google Scholar]
- 12. Hovelius L. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am. 2008;90:945. [DOI] [PubMed] [Google Scholar]
- 13. Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg. 1996;78:1677–1684. [DOI] [PubMed] [Google Scholar]
- 14. Ide J, Maeda S, Takagi K. Arthroscopic Bankart repair using suture anchors in athletes: patient selection and postoperative sports activity. Am J Sports Med. 2004;32:1899–1905. [DOI] [PubMed] [Google Scholar]
- 15. Jones KJ, Wiesel B, Ganley TJ, Wells L. Functional outcomes of early arthroscopic Bankart repair in adolescents aged 11 to 18 years. J Pediatr Orthop. 2007;27:209–213. [DOI] [PubMed] [Google Scholar]
- 16. Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21:55–63. [DOI] [PubMed] [Google Scholar]
- 17. Kocher MS, Horan MP, Briggs KK, Richardson TR, O’Holleran J, Hawkins RJ. Reliability, validity, and responsiveness of the American Shoulder and Elbow Surgeons subjective shoulder scale in patients with shoulder instability, rotator cuff disease, and glenohumeral arthritis. J Bone Joint Surg Am. 2005;87:2006–2011. [DOI] [PubMed] [Google Scholar]
- 18. Larrain MV, Montenegro HJ, Mauas DM, Collazo CC, Pavón F. Arthroscopic management of traumatic anterior shoulder instability in collision athletes: analysis of 204 cases with a 4- to 9-year follow-up and results with the suture anchor technique. Arthroscopy. 2006;22:1283–1289. [DOI] [PubMed] [Google Scholar]
- 19. Lawton RL, Choudhury S, Mansat P, Cofield RH, Stans AA. Pediatric shoulder instability: presentation, findings, treatment, and outcomes. J Pediatr Orthop. 2002;22:52–61. [PubMed] [Google Scholar]
- 20. Mazzocca AD, Brown FM, Jr, Carriera DS, Hayden J, Romeo AA. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33:52–60. [DOI] [PubMed] [Google Scholar]
- 21. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587–594. [DOI] [PubMed] [Google Scholar]
- 22. Milchteim C, Tucker SA, Nye DD, et al. Outcomes of Bankart repairs using modern arthroscopic technique in an athletic population. Arthroscopy. 2016;32:1263–1270. [DOI] [PubMed] [Google Scholar]
- 23. Olds M, Donaldson K, Ellis R, Kersten P. In children 18 years and under, what promotes recurrent shoulder instability after traumatic anterior shoulder dislocation? A systematic review and meta-analysis of risk factors. Br J Sports Med. 2016;50:1135–1141. [DOI] [PubMed] [Google Scholar]
- 24. Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37:1750–1754. [DOI] [PubMed] [Google Scholar]
- 25. Owens BD, DeBerardino TM, Nelson BJ, et al. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med. 2009;37:669–673. [DOI] [PubMed] [Google Scholar]
- 26. Ozturk BY, Maak TG, Fabricant P, et al. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy. 2013;29:1922–1931. [DOI] [PubMed] [Google Scholar]
- 27. Rhee YG, Ha JH, Cho NS. Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med. 2006;34:979–985. [DOI] [PubMed] [Google Scholar]
- 28. Rice SG, American Academy of Pediatrics Council on Sports Medicine and Fitness. Medical conditions affecting sports participation. Pediatrics. 2008;121:841–848. [DOI] [PubMed] [Google Scholar]
- 29. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 30. Skare Ø, Schrøder CP, Mowinckel P, Reikerås O, Brox JI. Reliability, agreement and validity of the 1988 version of the Rowe Score. J Shoulder Elbow Surg. 2011;20:1041–1049. [DOI] [PubMed] [Google Scholar]
- 31. Stecco A, Guenzi E, Cascone T, et al. MRI can assess glenoid bone loss after shoulder luxation: inter- and intra-individual comparison with CT. Radiol Med. 2013;118:1335–1343. [DOI] [PubMed] [Google Scholar]
- 32. Voos JE, Livermore RW, Feeley BT, et al. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38:302–307. [DOI] [PubMed] [Google Scholar]
- 33. World Health Organization. Adolescent development. http://www.who.int/maternal_child_adolescent/topics/adolescence/dev/en/. Accessed February 12, 2016.


