Abstract
Background:
There are limited data regarding associated factors of return to sports activities at more than 5 years after anterior cruciate ligament (ACL) reconstruction.
Purpose:
To test interrelationships between patient characteristics, concomitant articular lesions, graft laxity, and maintenance of sports activities at 5 to 10 years after ACL reconstruction. It was hypothesized that at 5 to 10 years after the operation in young adult men, maintenance of greater activity level and better knee function would be associated with greater preinjury activity level, younger age at reconstruction, absence of concomitant articular lesions, and minimal graft laxity at follow-up.
Study Design:
Case series; Level of evidence, 4.
Methods:
One hundred six men with autologous hamstring ACL reconstruction between the ages of 18 and 35 years were reviewed at 5 to 10 years after surgery. Excluded patients had contralateral ACL tear, revision reconstruction, or another injury impairing function. Fifty-five patients were eligible and available for follow-up. Independent variables included preinjury Tegner score, time interval from injury to surgery, smoking status, age, articular lesions, KT side-to-side difference, and pivot-shift grade. Main outcome measures were Tegner activity level, International Knee Documentation Committee (IKDC) subjective score, and Knee injury and Osteoarthritis Outcome Scale (KOOS) score at 5 to 10 years after surgery.
Results:
Greater Tegner activity level at follow-up was associated in a regression model with greater preinjury Tegner activity level (correlation coefficient, 0.423; P = .01), lower KT difference (correlation coefficient, –0.278; P = .04), and negative pivot shift (correlation coefficient, –0.277; P = .05). Younger age at operation predicted return to greater Tegner activity level in a univariate analysis (correlation coefficient, –0.266; P = .05) but not in a regression model (not significant). Chondral lesions at surgery predicted lower IKDC subjective scores (71.4 ± 14.3 vs 84.1 ± 11.5; P < .01) and KOOS scores but did not affect maintenance of sports activities.
Conclusion:
At 5 to 10 years after autologous hamstring ACL reconstruction in young men, predictors of greater sports activity level are primarily high preinjury activity level and reestablishment of knee laxity. Younger age at operation and moderate chondral lesions have lower impact in this respect.
Keywords: ACL, autologous hamstrings, Tegner score, KT, transtibial
The primary goal of anterior cruciate ligament (ACL) reconstruction is to enable young athletes to maintain their preinjury sports activities. Nevertheless, it has been shown that return to preinjury sports levels was achieved in less than two-thirds of patients at 3 years40 and in less than half at longer follow-up.2 Furthermore, return to sports at 1 year after surgery was not indicative of maintaining high sports levels at longer follow-up.2 To date, several studies have provided outcomes at 5 or more years after surgery.∥ Yet, these studies were subjected to limitations, which included combining outcomes for heterogeneous graft sources9,33,38 and for multiple surgical techniques,14 referring to a wide range of ages for a reported outcome9,22,31,34,42 or not indicating age,25,33 not differentiating between men and women,9,11,17,22,25,31,34,42 and lacking functional testing.2,9,33,38 In large cohorts, outcomes were limited to patient-reported questionnaires.2,38 Since results of ACL reconstruction might be affected by the type of graft,15,29,30 surgical technique,3,7 patient age,15,19 and sex6,28 and since knee kinematics are sex specific,21 conclusions drawn from such heterogeneous reports may be ambiguous and nonspecific.
Recently, the American Academy of Orthopedic Surgeons highlighted a specific group of interest with evidence-based guidelines on management of ACL injuries.35 Surgical reconstruction was supported specifically for young adults aged 18 to 35 years using single-bundle intra-articular reconstruction with autologous hamstring graft and either a transtibial or an independent tunnel technique.35 The current study was designed to be specific and evaluate this traditionally highly active population (18- to 35-year-old men) at 5 to 10 years after autologous hamstring transtibial ACL reconstruction. The objective was to identify factors associated with improved function and maintenance of sports activities at 5 to 10 years after the operation. We hypothesized that at 5 to 10 years, greater sports activity level and better knee function would be associated with greater preinjury activity level, younger age at reconstruction, absence of concomitant articular lesions, and minimal graft laxity at follow-up.
Methods
Primary ACL reconstructions performed between 2004 and 2010 in a single sports medicine injury clinic were identified. All subjects received primary autologous quadrupled hamstring graft ACL reconstruction using a transtibial approach. For tunnel locations, the following principles were applied as suggested previously4,13: The internal tip of the ACL tibia guide was placed 7 mm anterior to the posterior cruciate ligament (PCL), in line with the posterior edge of the anterior horn of the lateral meniscus, between the medial and lateral tibial eminences, planning the exit of the guide pin at the posteromedial aspect of the native ACL footprint. The external starting point of the guide pin on the tibia was midway between the tibial tubercle and the posteromedial border of the tibia. The femoral tunnel guide pin was drilled through a 6-mm offset femoral guide, which was placed at the 10:30 clockface position in the intercondylar notch and against the posterior femoral condyle cortex (this left a 1- to 2-mm back wall for graft tunnel diameters of 8-10 mm). All reconstructions were performed by the same surgical group that comprised 2 experienced sports injury and arthroscopy fellowship-trained senior orthopaedic surgeons. Inclusion criteria were (1) male sex; (2) ACL tear related to sport activity only; (3) age at surgery 18 to 35 years; (4) ACL reconstruction only, without concomitant ligament reconstruction; and (5) 5- to 10-year follow-up. Exclusion criteria were (1) contralateral ACL tear, (2) revision ACL reconstruction during follow-up or magnetic resonance imaging–documented ACL graft tear with instability awaiting revision, and (3) another significant lower limb injury.
Patients were contacted for a follow-up evaluation in the clinic at 5 to 10 years after surgery. Demographic variables included type of sport activity at injury, time from injury to surgery, smoking status, age at operation, follow-up time, and meniscal and chondral lesions identified during surgery. Chondral lesion was considered “positive” for Outerbridge grade 2 or higher26 in accordance with other long-term studies.38 Tegner39 and Marx24 activity level scores were recorded before injury and at latest follow-up. Subjective functional outcome questionnaires included the International Knee Documentation Committee (IKDC) subjective score,1 Knee injury and Osteoarthritis Outcome Score (KOOS),32 and Short Form (SF)–36 score.27 Side-to-side anterior knee laxity difference was measured using a KT-1000 knee arthrometer (MEDmetric) with the knee at 25° of flexion and a 30-pound anteriorly directed force. The pivot-shift test23 was graded as either 0 (no pivot shift), 1+ (pivot glide), or 2+ (pivot shift clunk).18 All measurements were performed in all patients by 1 independent investigator (I.H.) who was not one of the surgeons who performed the index surgery. Limb symmetry index (LSI) was indicated for the single-leg hop for distance and the side-to-side hop as recommended for this population.6,8
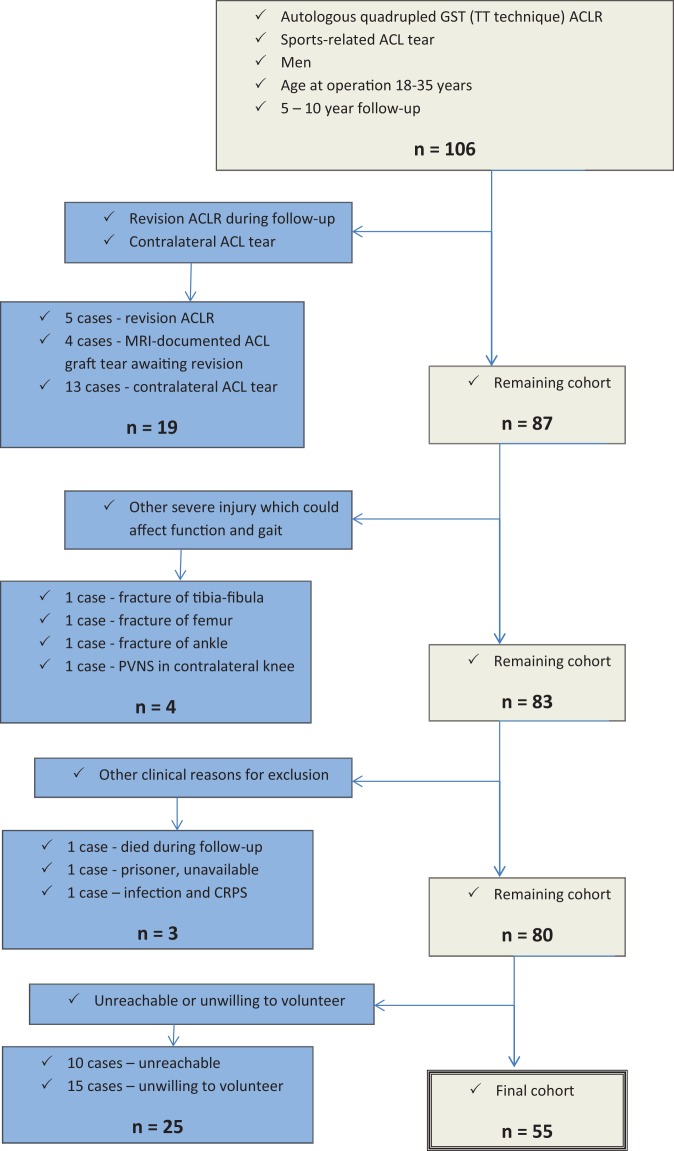
One hundred six patients fulfilled the initial inclusion criteria, of which 23 fulfilled the exclusion criteria during follow-up, leaving 83 patients eligible at 5 to 10 years after the operation. Of these 83 patients, 55 (67%) were available for study-specific follow-up evaluation (Figure 1).
Figure 1.
Flowchart of study cohort. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; CRPS, complex regional pain syndrome; GST, gracilis and semitendinosus; MRI, magnetic resonance imaging; PVNS, pigmented villonodular synovitis; TT, transtibial.
Statistical Analysis
Data included numbers with percentages for nonmetric variables and means with standard deviations and ranges for continuous variables. Continuous variables were checked for normality using the Shapiro-Wilk test. The Student t test was used for comparing mean values between variables with normal distribution. The Mann-Whitney nonparametric test was used for comparing variables where the assumption of normality was rejected. Nominal variables were analyzed with chi-square or Fisher exact tests. Correlations were calculated with Pearson or Spearman rank tests, each where appropriate. The following interrelationships were tested: KT difference and pivot-shift grade versus all knee function and activity level outcome measures at follow-up (ie, IKDC subjective, KOOS, SF-36, Tegner and Marx activity level scores, and hop test LSI), patient demographics and injury characteristics (ie, age at operation and follow-up, year of operation and number of years of follow-up, interval between injury and surgery, smoking status [yes/no], preinjury Tegner and Marx activity level scores, medial meniscectomy and medial meniscus repair [yes/no], lateral meniscectomy and lateral meniscus repair [yes/no], and chondral lesions [yes/no]) versus KT difference and all knee function and activity level outcome measures at follow-up, and IKDC subjective score versus Tegner and Marx activity level scores at follow-up. For Tegner and Marx activity level scores at latest follow-up, which were associated with multiple demographic and outcome measures, linear regression models were built to evaluate the relationships between the activity level score and all independent variables, which were significantly associated with the activity level score in the univariate analyses. Level of statistical significance was set at .05. All statistical analyses were performed using the IBM SPSS-22 software package.
Results
The preinjury median Tegner score was 7 and Marx score 12 (Table 1). Forty-four (80%) patients tore their ACL playing soccer or basketball. Thirty-three (60%) patients had concomitant intra-articular lesions observed during surgery besides the ACL tear (Table 1).
TABLE 1.
Patient Demographics and Injury Characteristicsa
| Variable | |
|---|---|
| Patient demographics | |
| Age at operation, y, mean (range) | 25.3 (18-34) |
| Body mass index, kg/m2, mean (range) | 24.1 (20-31) |
| Smoking status, yes/no, n | 15/40 |
| Preinjury Tegner, median (range) | 7 (6-10) |
| Preinjury Marx, median (range) | 12 (8-16) |
| Injury-surgery interval, mo, mean ± SD | 13.4 ± 20.9 |
| Follow-up time, y, mean (range) | 7.1 (5-10) |
| Type of sports at injury, n | |
| Soccer | 30 |
| Basketball | 14 |
| Martial arts | 6 |
| Othersb | 5 |
| Concomitant knee lesions, No. of cases | |
| No concomitant lesions | 22 |
| Chondral lesionsc | 11 |
| MM tear resected | 14 |
| LM tear resected | 19 |
| MM tear repaired | 6 |
| LM tear repaired | 2 |
| MM and LM tears resected | 7 |
| MM/LM tear resected and chondral lesion | 6 |
aLM, lateral meniscus; MM, medial meniscus.
bOne case in each of the following sport: volleyball, gymnastics, handball, dancing, badminton.
cLesions considered Outerbridge grade 2 or higher (ie, worse) that involved the femoral or tibial condyles.
Return to preinjury Tegner activity level was documented in 22 (40%) patients (Table 2). Mean IKDC subjective, KOOS-knee symptoms, KOOS-pain, and SF-36 physical functioning scores were in the range 80 to 90. Mean hop symmetry indexes were “nearly normal.”10
TABLE 2.
Activity Levels, Subjective Function Perceptions, and Hop Tests at Follow-upa
| Score | |
|---|---|
| Activity level | |
| Tegner score, median (range) | 7 (2-10) |
| Marx score, median (range) | 4 (0-16) |
| Return to preinjury Tegner score, n (%) | 22 (40) |
| Return to preinjury Marx score, n (%) | 6 (11) |
| Subjective function perceptions, mean ± SD | |
| IKDC subjective score | 81.5 ± 13 |
| KOOS | |
| Knee symptoms | 82.9 ± 13.3 |
| Pain | 86.9 ± 13 |
| Activities of daily living | 93.9 ± 9.2 |
| Sports | 73.9 ± 19.9 |
| Quality of life | 57.9 ± 23.8 |
| SF-36 | |
| Physical functioning | 86.2 ± 12.7 |
| Role limitations due to physical health | 72.3 ± 36.9 |
| Bodily pain | 78.8 ± 20.4 |
| General health | 79.6 ± 16.4 |
| Vitality, energy, fatigue | 64.5 ± 15.4 |
| Social functioning | 92.2 ± 13.0 |
| Role limitations due to emotional problems | 84.2 ± 33.9 |
| Emotional well-being | 79.6 ± 11.4 |
| Hop test LSI, mean ± SD | |
| Single-leg hop test | 92.9 ± 14.3 |
| Side-to-side hop test | 93.2 ± 17.6 |
aIKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; LSI, limb symmetry index; SF, Short Form.
No significant differences in any outcome measure were found between patients who did compared with those who did not have meniscus surgery. However, when 11 patients who had chondral lesions were compared with 43 patients without chondral lesions during surgery, the former showed inferior scores for IKDC subjective (71. 4 ± 14.3 vs 84.1 ± 11.5, P < .01), KOOS-knee symptoms (77.5 ± 10.7 vs 84.2 ± 13.8, P = .04), KOOS-pain (81.6 ± 12.4 vs 88.3 ± 13.1, P = .04), KOOS-sports (61.4 ± 21.8 vs 77.8 ± 18, P = .02), and SF-36 social functioning (87.8 ± 13.7 vs 93.1 ± 12.8, P = .04) at follow-up.
KT-1000 side-to-side difference at follow-up was a mean 2.7 ± 2.3 mm. In 47 (86%) cases, the side-to-side difference was ≤5 mm (Figure 2), considered “normal” or “nearly normal.”10
Figure 2.
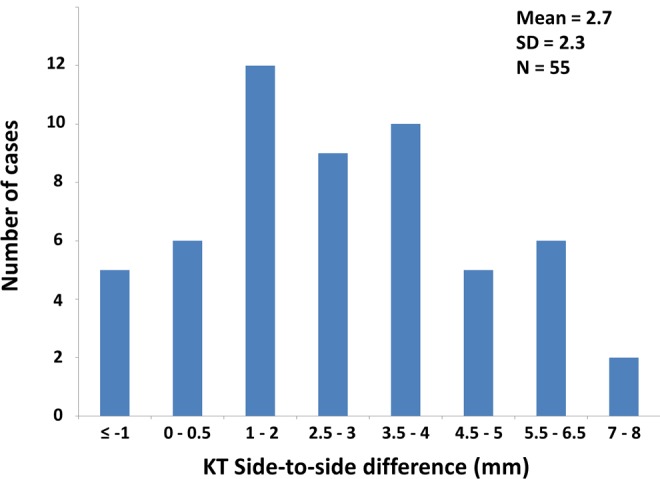
KT-1000 side-to-side difference distribution at follow-up.
Return to greater activity level was associated with younger age at operation (Figure 3), greater preinjury activity level (Table 3), minimal KT-1000 difference (Figure 4), and negative pivot shift (Table 3) at follow-up. Linear regression models for Tegner and Marx activity level scores at latest follow-up versus all associated factors showed significant associations between return to greater activity level and greater preinjury activity level score, lower KT-1000 difference at follow-up, and negative pivot shift (Table 4). To reduce the potential of patients with KT difference greater than 4.0 mm skewing the results, the regression analyses were repeated for the subgroup of patients with KT ≤4.0 mm (n = 42). This showed that a greater Tegner score at follow-up was still correlated with higher preinjury Tegner score (correlation coefficient, 0.437; P < .01) and with lower KT (correlation coefficient, –0.344; P < .01) and pivot shift at follow-up (correlation coefficient, –0.241; P = .04).
Figure 3.
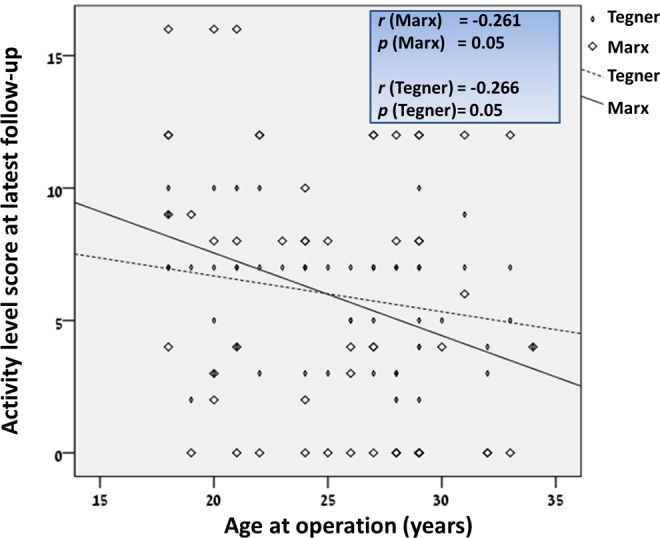
Correlations between activity level scores at follow-up and age at operation.
TABLE 3.
Relationships Between Tegner and Marx Scores at Follow-up Compared With Pivot Shift and Preinjury Scores
| Independent Variable | Latest Follow-up Score, Median (Range) | |
|---|---|---|
| Tegner Score | Marx Score | |
| Pivot shift grade 0 (n = 12) | 7 (7-10) | 10 (2-16) |
| Pivot shift grade 1+ (n = 24) | 7 (2-10) | 6 (0-16) |
| Pivot shift grade 2+ (n = 19) | 5 (2-9) | 0 (0-12) |
| P value | <.01a | .01b |
| Tegner preinjury 6, 7 (n = 34) | 5 (2-9) | 4 (0-12) |
| Tegner preinjury 9, 10 (n = 21) | 7 (2-10) | 9 (0-16) |
| P value | <.01 | <.01 |
| Marx preinjury 8-12 (n = 29) | 5 (2-9) | 4 (0-12) |
| Marx preinjury 13-16 (n = 26) | 7 (2-10) | 8.5 (0-16) |
| P value | .02 | .01 |
aPivot 0 vs 1+; pivot 0 vs 2+.
bPivot 0 vs 2+.
Figure 4.
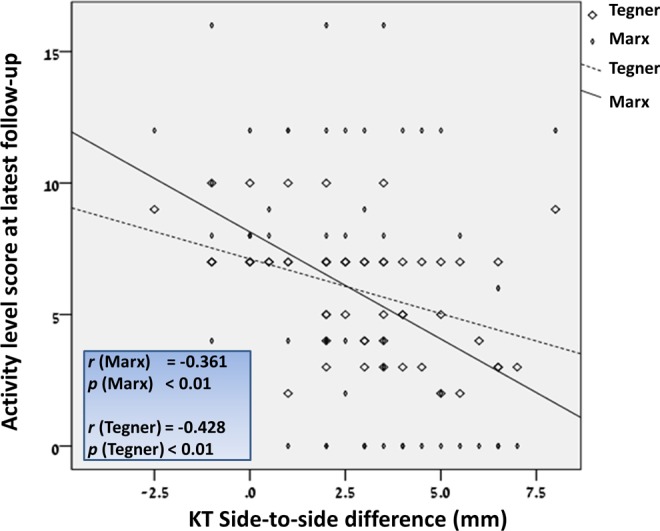
Correlations between activity level scores at follow-up and KT side-to-side difference.
TABLE 4.
Linear Regression Model for Tegner and Marx Scores at Follow-up Compared With All Associated Factorsa
| Dependent Variable | Independent Variable | Standardized Correlation Coefficient βb | P Valueb |
|---|---|---|---|
| Tegner latest follow-up score | Tegner preinjury score | 0.423 (0.437) | .01 (<.01) |
| Marx preinjury score | –0.164 | .29 | |
| KT side-to-side differencec | –0.278 (–0.344) | .04 (<.01) | |
| Pivotc | –0.277 (–0.241) | .05 (.04) | |
| Age at operation | –0.191 (–0.17) | .12 (.17) | |
| Marx latest follow-up score | Tegner preinjury score | 0.405 (0.457) | .02 (<.01) |
| Marx preinjury score | –0.088 | .60 | |
| KT side-to-side differencec | –0.292 (–0.326) | .05 (.01) | |
| Pivotc | –0.135 (–0.154) | .38 (.25) | |
| Age at operation | –0.165 (–0.093) | .21 (.49) |
aBoldfaced values indicate statistical significance.
bResults appear in parentheses for subgroup regression analyses of only patients who had KT side-to-side difference ≤4.0 mm (n = 42) using 4 independent variables: Tegner preinjury score, KT side-to-side difference, pivot grade, and age at operation.
cAt latest follow-up.
Positive correlations were demonstrated between IKDC subjective score versus Tegner and Marx activity level scores at follow-up (correlation coefficient, 0.27; P = .04 and correlation coefficient, 0.32; P = .02, respectively).
Smoking status and time interval between injury and surgery were not associated with outcome measures (not significant for all comparisons).
Discussion
The main finding was that greater activity level at 5 to 10 years after surgery was primarily associated with greater activity level before injury and with reestablishment of symmetric knee laxity and negative pivot shift. Among these, preinjury activity level had the strongest association (highest correlation coefficient value). This may be related to multiple factors such as improved postural control; greater motivation; more strict standards of training and rehabilitation, which likely characterize higher level athletes; as well as other factors. On the other hand, knee graft laxity at follow-up as a second important predictor of ongoing sports maintenance depends more on factors related to the surgery itself and the early phases of rehabilitation. Moreover, because preinjury activity level is a nonmodifiable factor once an injury occurs, focus should be applied to reestablishment of normal knee laxity, which should be at top priority from both the surgeon’s as well as the athlete’s perspective to improve the athlete’s chances of maintaining desired high-level sports activities. In this regard, a resilient graft with high tissue quality should be used with restored anatomical insertions and firm fixations at the graft-bone interface followed by the implementation of individualized task-based instead of time-based rehabilitation principles to avoid reinjury at the early phases before graft healing and maturation with sufficient neuromuscular recovery occurs.12 Exploring specific factors responsible for increased side-to-side knee laxity in some cases of this series was beyond the scope of the study. Nevertheless, poor graft tissue quality was unlikely a reason for increased laxity at follow-up since only autograft tissue was used with a measured quadrupled graft diameter of ≥8 mm in all cases but 1, which corresponds to the accepted diameter threshold associated with reduced failure rates in hamstring ACL reconstruction.5 Inaccurate tunnel placement could nevertheless be a reason for increased laxity in some of these cases, but tunnel location was not systematically evaluated on radiographs or other imaging in this series. As for rehabilitation, although all patients received guidelines that focused on closed kinetic chain strengthening during the first 3 months after surgery, the actual rehabilitation was not strictly and systematically supervised.
The relationships observed between greater activity levels and lower KT differences at latest follow-up are, to the best of our knowledge, a new finding that supports the value of the instrumented knee laxity test as a meaningful outcome measure for assessing likelihood of maintaining high-level sports activities at this relatively long follow-up. Others did not identify significant association between KT difference and level of activity at minimum 2-year follow-up and concluded that only elimination of the pivot shift but not normalization of KT difference was a valuable measure of ligament laxity, which was associated with greater activity level at follow-up.18 That study, however, was not specific in relation to graft source (25 patients had autologous hamstring grafts and 177 had autologous patellar tendon grafts), sex (57% men), age (range, 14-60 years), and instrumented knee laxity examinations (assessment performed by 4 assistants),18 all of which may have been masking relationships between instrumented knee laxity tests and return to activities that were identified in the selective group tested in this study. The variation in follow-up KT difference in this series is similar to another observation at 7 years after ACL reconstruction with similar graft source,22 which supports the generalizability of the study.
Concomitant meniscus tears or chondral lesions were not associated with activity levels at follow-up, although chondral lesions were associated with inferior IKDC subjective, KOOS, and SF-36 scores. Thus, maintaining high-level sport activities was primarily achieved via reestablishment of normal knee laxity, regardless of accompanying chondral lesions. One explanation could be that knee impairment due to chondral lesions (ie, primarily pain) might be managed by modalities such as muscle strengthening, shoe wear, intra-articular injections, and other medications, while abnormal knee laxity can hardly be managed in these chronic cases and may therefore be more critical in preventing ongoing participation in cutting-pivoting sports. It should be remembered, however, that there were 11 patients with chondral lesions of the 55 patients in this cohort, so there is also potential for a type-2 statistical error (ie, a false negative interpretation). The adverse effect of chondral knee lesions on subjective outcomes after ACL reconstruction corresponds with other studies that showed that chondral lesions were more detrimental to subjective knee scores compared with meniscal resections at 5 to 15 years after ACL reconstruction.36
Younger age at operation in this 18- to 35-year-old group was associated with maintenance of greater activity level only in the univariate analysis (with a relatively low correlation coefficient) and not in the linear regression model, which then accounted for all associated factors. This supports viewing the 18- to 35-year-old population as a single age group for the purpose of exploring predictive factors of ongoing high-level sport activities after ACL reconstruction at 5 to 10 years, and it is supported by others who were viewing this age group as relatively homogeneous in this respect.35
Hop tests indicated normal LSI values,10 corresponding to previous assessments at 5 or more years after hamstring ACL reconstruction,11,17 and were not associated with other outcome measures. Nevertheless, while these tests were selected based on previous recommendations,6,8 it is possible that both tests were not sensitive enough to identify functional deficits. Eccentric hamstring tests may have been more sensitive in this respect, but this was not performed. Furthermore, the successful completion of a criterion-based rehabilitation program with quadriceps strength assessment using a knee dynamometer was not performed, so quadriceps strength deficits may have existed in some patients.
Smoking was not associated with worse outcomes, which corresponds with some previously published data16 but opposes others.19,38 We therefore recommend being cautious in interpreting this finding and advise to cease smoking before undergoing this type of reconstructive surgery based on previously discussed adverse consequences of cigarette smoking on orthopaedic surgery.20
In terms of KOOS–activities of daily living and SF-social functioning, excellent scores were documented, but in terms of return to sports, 40% of patients were active at their preinjury sports level based on the Tegner scale. This corresponds to a recent self-reported questionnaire-based study that showed 140 of 314 (44%) patients were participating at their preinjury level at 2 to 7 years after surgery.2 Another study reported data after autologous hamstring ACL reconstruction at 7 years and showed a median Tegner score of 6 (range, 2-9),22 which is slightly less favorable compared with the median score of 7 (range, 2-10) observed in this investigation. Lower scores in that study may be related to the fact that it referred to a heterogeneous population and incorporated both sexes as well as diversity of age groups (range, 15-59 years).22 The current study further emphasizes the importance of reporting not only type of activity (eg, Tegner scale) but also frequency of activity (eg, Marx scale) in a young population as 2 distinct quantifications of sports participation. While 40% of patients were active at their preinjury Tegner sports level at follow-up, less than 20% were active at their preinjury sports intensity, as determined using the Marx scale. The pronounced decline in Marx score was also demonstrated in another study that showed marked decline in this score 2 to 6 years after ACL reconstruction. Of note, it is possible that not every case of decline in activity level score was a direct consequence of suboptimal knee recovery, and some patients may have modified their activities because of other reasons of changing lifestyle. This, however, was unlikely in most patients since positive correlations were demonstrated between subjective knee perceptions, as represented by IKDC-subjective score, versus latest activity levels, as represented by Tegner and Marx scores, which supports that patients with higher satisfaction and confidence regarding their knee function (ie, IKDC-subjective score) were also those who were involved in greater activity levels at follow-up and vice versa.
Limitations of this study include the retrospective design and the fact that only 67% of eligible patients were available for latest follow-up. Thirteen patients (12.3% of the initial 106 patient cohort) with contralateral ACL tear were excluded since side-to-side differences could not provide meaningful data. This is similar to other studies that documented an 11.8% occurrence of contralateral ACL tears at more than 5 years of follow-up.41 This could have resulted in loss of well-functioning knees, since patients with particularly excellent rehabilitation after ACL reconstruction were shown to sustain 3-fold contralateral ACL tears compared with patients with slower recovery.37 Another 9 patients (8.5% of the initial 106 patient cohort) were excluded in this study due to ipsilateral ACL graft tears, which is slightly higher compared with the 5.8% reported by others.41 Moreover, long-term studies create difficulties in isolating outcomes of specific surgery because additional injuries can happen during follow-up. This was documented in 4 patients (3.8% of the initial 106 patient cohort) who sustained femoral and tibial fractures. Despite all exclusions, this investigation is still a larger series of young adult men at more than 5 years after autologous hamstring transtibial ACL reconstruction compared with previous investigations with fewer than 30 cases in comparable populations.9,11,17,33,34,42
Conclusion
At 5 to 10 years after autologous hamstrings ACL reconstruction in young men, predictors of greater sports activity level are primarily high preinjury activity level and reestablishment of knee laxity. Younger age at operation and moderate chondral lesions have lower impact in this respect.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Helsinki Committee at the Meier General Hospital, Kfar Saba, Israel (0215-13-MMC).
References
- 1. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; International Knee Documentation Committee. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34:128–135. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40:41–48. [DOI] [PubMed] [Google Scholar]
- 3. Chalmers PN, Mall NA, Cole BJ, Verma NN, Bush-Joseph CA, Bach BR., Jr Anteromedial versus transtibial tunnel drilling in anterior cruciate ligament reconstructions: a systematic review. Arthroscopy. 2013;29:1235–1242. [DOI] [PubMed] [Google Scholar]
- 4. Chhabra A, Diduch DR, Blessey PB, Miller MD. Recreating an acceptable angle of the tibial tunnel in the coronal plane in anterior cruciate ligament reconstruction using external landmarks. Arthroscopy. 2004;20:328–330. [DOI] [PubMed] [Google Scholar]
- 5. Conte EJ, Hyatt AE, Gatt CJ, Jr, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30:882–890. [DOI] [PubMed] [Google Scholar]
- 6. Engelen-van Melick N, van Cingel RE, Tijssen MP, Nijhuis-van der Sanden MW. Assessment of functional performance after anterior cruciate ligament reconstruction: a systematic review of measurement procedures. Knee Surg Sports Traumatol Arthrosc. 2013;21:869–879. [DOI] [PubMed] [Google Scholar]
- 7. Fauno P, Kaalund S. Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy. 2005;21:1337–1341. [DOI] [PubMed] [Google Scholar]
- 8. Gustavsson A, Neeter C, Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;14:778–788. [DOI] [PubMed] [Google Scholar]
- 9. Hanypsiak BT, Spindler KP, Rothrock CR, et al. Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med. 2008;36:671–677. [DOI] [PubMed] [Google Scholar]
- 10. Hefti F, Muller W, Jacob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. [DOI] [PubMed] [Google Scholar]
- 11. Heijne A, Hagstromer M, Werner S. A two- and five-year follow-up of clinical outcome after ACL reconstruction using BPTB or hamstring tendon grafts: a prospective intervention outcome study. Knee Surg Sports Traumatol Arthrosc. 2015;23:799–807. [DOI] [PubMed] [Google Scholar]
- 12. Herrington L, Myer G, Horsley I. Task based rehabilitation protocol for elite athletes following anterior cruciate ligament reconstruction: a clinical commentary. Phys Ther Sport. 2013;14:188–198. [DOI] [PubMed] [Google Scholar]
- 13. Howell SM, Gittins ME, Gottlieb JE, Traina SM, Zoellner TM. The relationship between the angle of the tibial tunnel in the coronal plane and loss of flexion and anterior laxity after anterior cruciate ligament reconstruction. Am J Sports Med. 2001;29:567–574. [DOI] [PubMed] [Google Scholar]
- 14. Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21:412–417. [DOI] [PubMed] [Google Scholar]
- 15. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, MOON Consortium, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Keays SL, Bullock-Saxton JE, Keays AC, Newcombe PA, Bullock MI. A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and gracilis tendon graft. Am J Sports Med. 2007;35:729–739. [DOI] [PubMed] [Google Scholar]
- 18. Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:629–634. [DOI] [PubMed] [Google Scholar]
- 19. Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish national anterior cruciate ligament register. Arthroscopy. 2014;30:803–810. [DOI] [PubMed] [Google Scholar]
- 20. Kwiatkowski TC, Hanley EN, Jr, Ramp WK. Cigarette smoking and orthopedic consequences. Am J Orthop. 1996;25:590–597. [PubMed] [Google Scholar]
- 21. Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Gender differences exist in neuromuscular control patterns during the pre-contact and early stance phase of an unanticipated side-cut and cross-cut maneuver in 15-18 years old adolescent soccer players. J Electromyogr Kinesiol. 2009;19:e370–e379. [DOI] [PubMed] [Google Scholar]
- 22. Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med. 2007;35:740–748. [DOI] [PubMed] [Google Scholar]
- 23. Losee RE. Concepts of the pivot shift. Clin Orthop Relat Res. 1983;172:45–51. [PubMed] [Google Scholar]
- 24. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213–218. [DOI] [PubMed] [Google Scholar]
- 25. O’Neill DB. Arthroscopically assisted reconstruction of the anterior cruciate ligament: a follow-up report. J Bone Joint Surg Am. 2001;83:1329–1332. [DOI] [PubMed] [Google Scholar]
- 26. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg. 1961;43:752–757. [DOI] [PubMed] [Google Scholar]
- 27. Patel AA, Donegan D, Albert T. The 36-item short form. J Am Acad Orthop Surg. 2007;15:126–134. [DOI] [PubMed] [Google Scholar]
- 28. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42:1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish registry of knee ligament reconstruction. Am J Sports Med. 2014;42:278–284. [DOI] [PubMed] [Google Scholar]
- 30. Reinhardt KR, Hetsroni I, Marx RG. Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010;41:249–262. [DOI] [PubMed] [Google Scholar]
- 31. Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33:1337–1345. [DOI] [PubMed] [Google Scholar]
- 32. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 33. Ruiz AL, Kelly M, Nutton RW. Arthroscopic ACL reconstruction: a 5-9 year follow-up. Knee. 2002;9:197–200. [DOI] [PubMed] [Google Scholar]
- 34. Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med. 2006;34:1933–1940. [DOI] [PubMed] [Google Scholar]
- 35. Shea KG, Carey JL, Richmond J, et al. The American Academy of Orthopaedic Surgeons evidence-based guideline on management of anterior cruciate ligament injuries. J Bone Joint Surg Am. 2015;97:672–674. [DOI] [PubMed] [Google Scholar]
- 36. Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med. 2000;28:446–452. [DOI] [PubMed] [Google Scholar]
- 37. Sousa PL, Krych AJ, Cates RA, Levy BA, Stuart MJ, Dahm DL. Return to sport: does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? [published online ahead of print July 24, 2015] Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3697-2. [DOI] [PubMed] [Google Scholar]
- 38. Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum six years after ACLR: a population cohort study. Am J Sports Med. 2011;39:348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 40. Walden M, Hagglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50:744–750. [DOI] [PubMed] [Google Scholar]
- 41. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:1060–1069. [DOI] [PubMed] [Google Scholar]