Abstract
Teenage mothers are at high risk for maternal and neonatal complications. This study aimed to evaluate the socioeconomic circumstances of teenage pregnancy, and determine whether these increased risks remained after adjustment for socioeconomic circumstances in Korea. Using the National Health Insurance Corporation database, we selected women who terminated pregnancy, by delivery or abortion, from January 1, 2010 to December 31, 2010. Abortion, delivery type, and maternal complications were defined based on the International Classification of Diseases-10th Revision. We compared teenagers (13–19 years at the time of pregnancy termination) with other age groups and investigated differences based on socioeconomic status, reflected by Medical Aid (MA) and National Health Insurance (NHI) beneficiaries. We used multivariate analysis to define the factors associated with preterm delivery. Among 463,847 pregnancies, 2267 (0.49%) involved teenagers. Teenage mothers were more likely to have an abortion (33.4%) than deliver a baby when compared with other age groups (20.8%; P < 0.001). About 14.4% of teenage mothers had never received prenatal care throughout pregnancy. Among teenage mothers, 61.7% of MA recipients made fewer than 4 prenatal care visits (vs 38.8% of NHI beneficiaries) (P < 0.001). Teenage mothers more often experienced preterm delivery and perineal laceration (P < 0.001). Teenage mothers (<20 years) were 2.47 times more likely to have preterm delivery than older mothers (20–34 years; P < 0.001). Teenage mothers had higher risk of inadequate prenatal care and subsequently of preterm delivery, which remained significantly higher after adjusting for socioeconomic confounding variables and adequacy of prenatal care in Korean teenagers (P < 0.001).
Keywords: National Health Insurance, prenatal care, preterm delivery, teenage pregnancy
1. Introduction
Teenage pregnancy, defined as pregnancy in girls aged 10 to 19 years, is a major public health issue. More than 16 million babies (11% of all births globally) are born to adolescent girls.[1] Although most teenage pregnancies occur in developing countries, this is also a major concern in developed countries.[1,2]
Teenage mothers are at high risk of maternal and neonatal complications. Delivery in adolescents is a leading cause of death in young women,[1] and the associated obstetric complications include maternal anemia, hypertensive disease in pregnancy, preterm birth, urinary tract infection, and so on.[3,4] Furthermore, the perinatal death rate is higher in neonates born to adolescent mothers, and the risk of neonatal morbidities is also increased.[5–7]
It is controversial whether adverse pregnancy outcomes are derived from the deprived socioeconomic status of such mothers[8–10] or their biological immaturity.[5,6,11] These conflicting results may be explained by the heterogeneity of study design, differences in the medical care system related to socioeconomic status, or differences in the size of the study population.
To examine this issue, the study evaluated the socioeconomic circumstances of teenage pregnancies, and determined whether teenage pregnancies are at higher risk even after adjustment for socioeconomic circumstances in Korea.
2. Methods
2.1. Data source
To investigate pregnancy, prenatal care, and delivery among teenage mothers in Korea comprehensively, we used the data from the National Health Insurance Corporation (NHIC) database, which is the sole healthcare insurer in Korea, enabling provision of uniform medical care to all Korean citizens. The NHIC accumulates all medical records, including personal information, based on medical claim data submitted from healthcare providers.
2.2. Operational definitions of teenage mother, abortion, delivery, and maternal complications
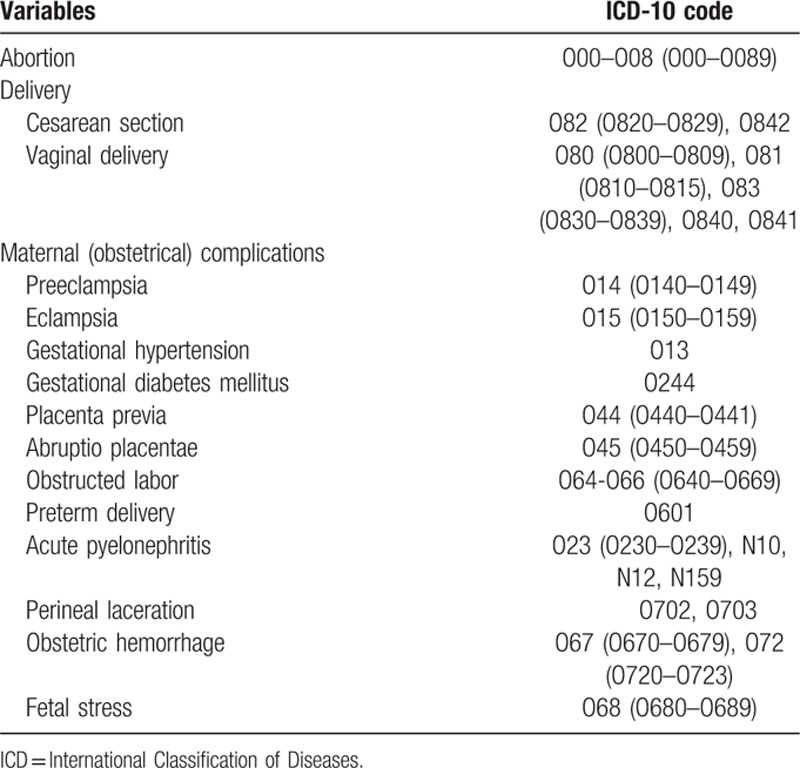
In this study, a teenage mother refers to a female aged 13 to 19 years at the time of pregnancy termination. Abortion, the type of delivery, and maternal complications were defined based on the International Classification of Diseases-10th Revision (ICD-10) (Table 1).
Table 1.
The definition of abortion, delivery, and maternal (obstetrical) complications.
2.3. Patient selection and data processing
Using the NHIC database, we selected women whose pregnancy terminated, by delivery or abortion, between January 1, 2010 and December 31, 2010. The total number of subjects was 463,847 women, and we divided these mothers into a teenage mother group (2267) and a nonteenage mother group (461,580). After excluding cases of abortion, the final database consisted of 367,088 mothers (teenage mothers: n = 1509 and nonteenage mothers: n = 367,088). To this database, we then connected each person's medical records and personal information in NHIC database.
2.4. Statistical analysis
We compared the teenage group with the other age groups, and then also investigated whether there were any differences in the teenage group according to their socioeconomic status. As a proxy indicator reflecting socioeconomic status, we divided subjects into Medical Aid (MA) recipients (poor family group) and National Health Insurance (NHI) beneficiaries (not poor). We assessed the adequacy of prenatal care using the Kessner index, which is based on the total number of prenatal care visits during pregnancy; if a pregnant woman saw a doctor on more than 9 occasions, it is considered “adequate”; if she visited a doctor on 5 to 8 occasions, it is considered “intermediate”; and if she visited a doctor fewer than 4 times, it is considered “inadequate.” The level of income was categorized according to 3 levels using the NHI premium as a proxy indicator: high level (upper 25% of premiums), intermediate level (middle 50% of premiums), and low level (lower 25% of premiums).
Frequency analyses were performed to describe pregnancy outcomes, prenatal care utilization, and maternal complications. Pearson chi-square test and Student t test were used to examine the differences not only between the teenage group and other age groups, but also between the NHI beneficiary group and the MA recipient group among teenage mothers. To define the factors associated with preterm delivery and inadequate prenatal care, multivariate analyses were performed using logistic regression. All analyses were completed using SPSS, version 19.0 (IBM, Chicago, IL). All statistical tests were 2-sided, and a P value <0.05 was considered statistically significant.
2.5. Ethical statement
The study was approved and the need for informed consent was waived by the Institutional Review Board (IRB No. 07–2015–5).
3. Results
3.1. General characteristics and main pregnancy outcomes
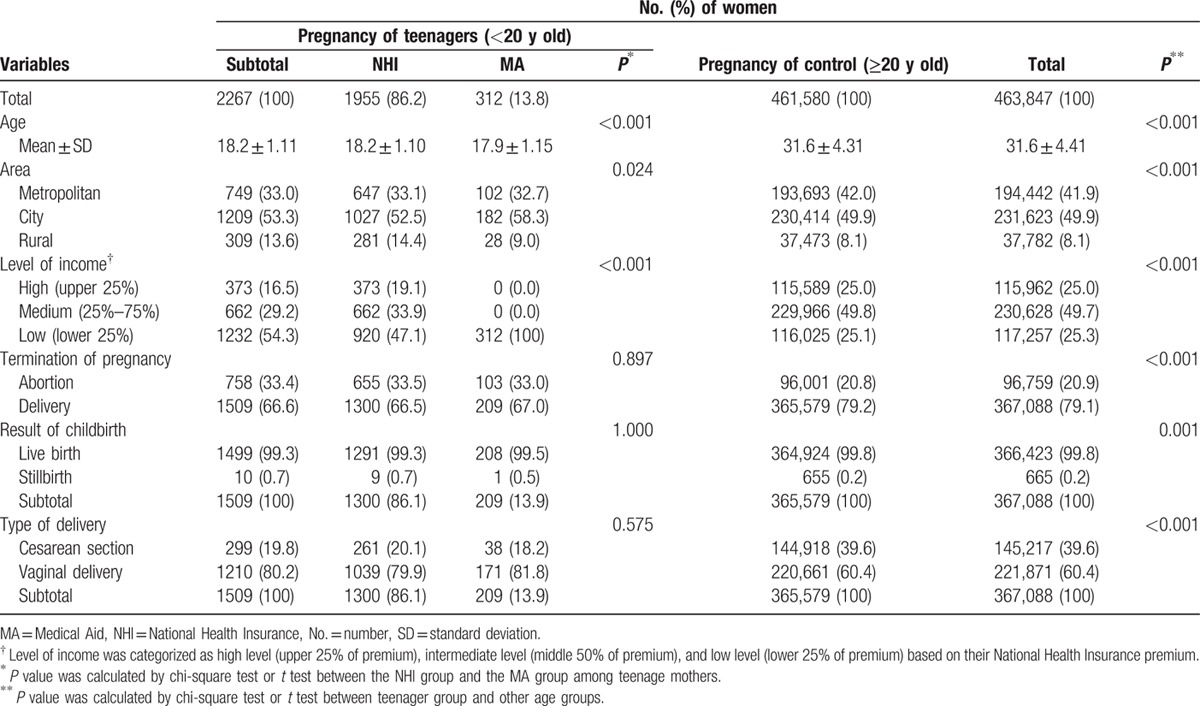
Compared with other age groups, teenage mothers were more likely to live in rural areas and to be from a low-income family (P < 0.001). They also showed higher rates of abortion (P < 0.001), stillbirths (P = 0.001), and vaginal delivery (P < 0.001) when compared with control (≥20 years old). Among teenage mothers, there were no significant differences in the rates of abortion, stillbirth, and vaginal delivery between the NHI beneficiary group and the MA recipient group. However, MA mothers were more likely to be younger and to live in metropolitan or city areas (P = 0.024) (Table 2).
Table 2.
General characteristics and main pregnancy outcomes.
3.2. Prenatal care utilization and its adequacy
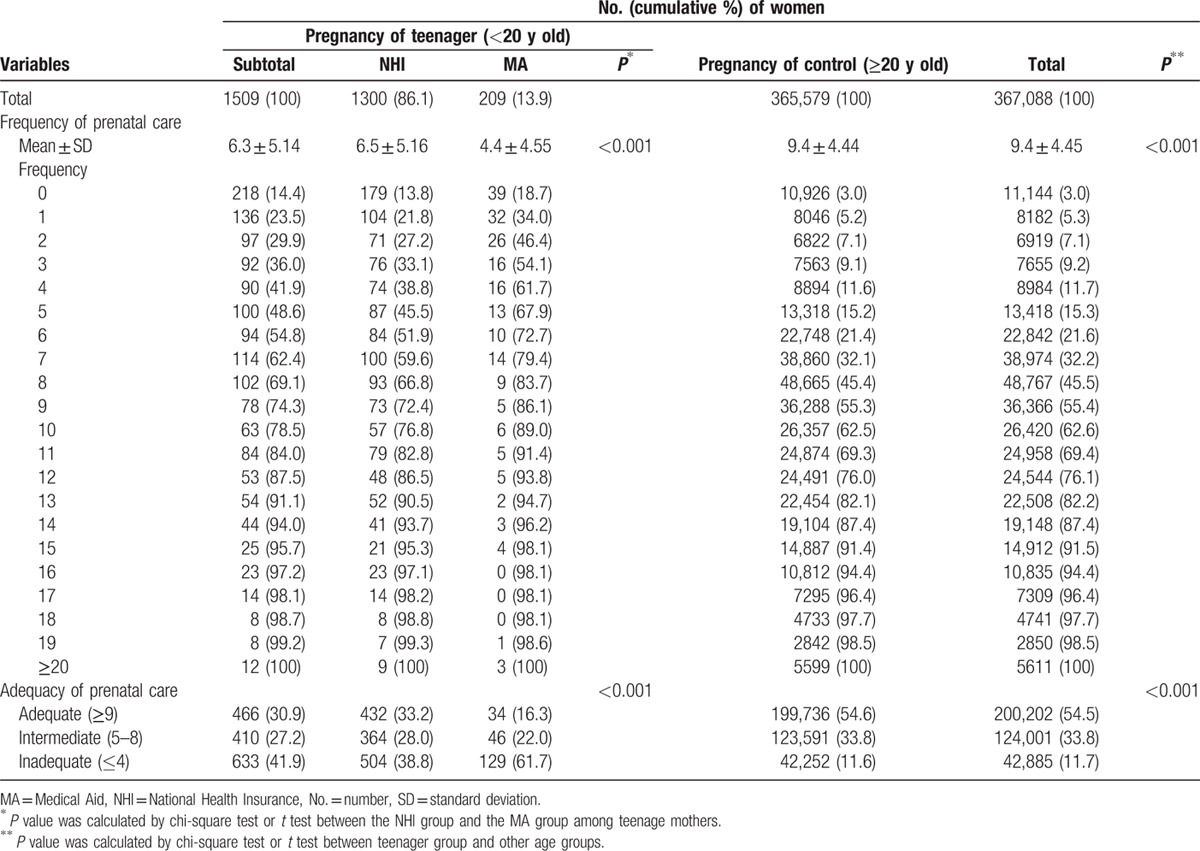
Teenage mothers utilized prenatal care less than did other age groups (P < 0.001). The average number of visits for prenatal care was 6.3, whereas that in the nonteenage mother group was 9.4 (P < 0.001). More seriously, 14.4% of teenage mothers had never received any prenatal care throughout their whole pregnancy. In particular, the average number of prenatal care visits in the MA group among teenage mothers was 4.4, which was about 2 occasions fewer than those of the teenage NHI group and about 5 occasions fewer than those of the other age groups (P < 0.001). The proportion of teenage mothers receiving inadequate prenatal care was thus significantly higher (41.9%) than for the other age groups (11.6%; P < 0.001). Among the teenage groups, this number was higher in the MA group (61.7%) than in the NHI group (38.8%; P < 0.001) (Table 3).
Table 3.
Prenatal care utilization and its adequacy.
3.3. Maternal complications
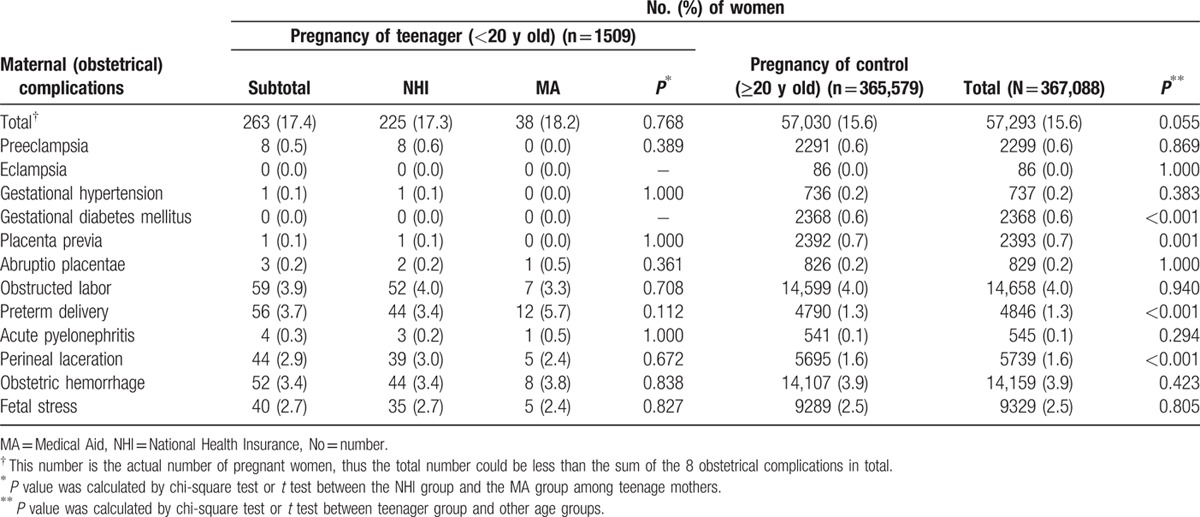
There were no significant differences between the teenage and other age groups in terms of maternal complications, other than gestational diabetes mellitus (P < 0.001), placenta previa (P = 0.001), preterm delivery (P < 0.001), and perineal laceration (P < 0.001). In particular, teenage mothers were more likely to experience preterm delivery and perineal laceration (P < 0.001; Table 4). Among teenagers, the rate of preterm delivery and perineal laceration was not different between the MA group and the NHI group.
Table 4.
Maternal (obstetrical) complications.
3.4. Factors associated with preterm delivery and inadequate prenatal care
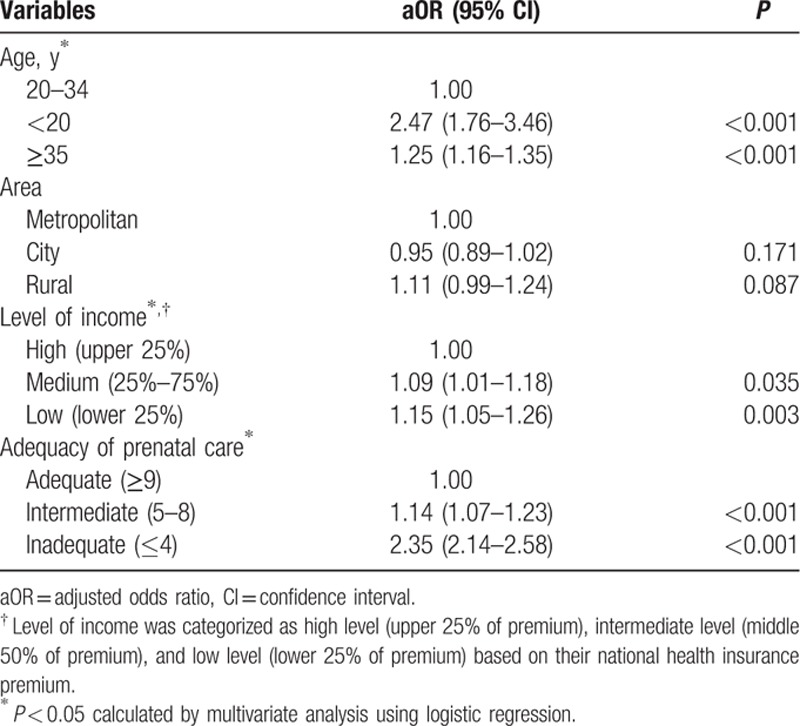
To define the factors associated with preterm delivery, we conducted logistic regression analysis to adjust for the effect of variables (age group, living area, type of insurance, level of income, and adequacy of prenatal care). Teenage mothers were 2.47 times, and those aged 35 years and older were 1.25 times more likely to experience preterm delivery, than the reference age group (20–34 years; P < 0.001). Compared with women living in metropolitan areas, women living in rural areas had a 1.11 times higher risk of preterm delivery (P = 0.087). In particular, low-income (1.15 times) and middle-income families (1.09 times) had a higher risk of preterm delivery than did high-income families (P < 0.001). Lastly, women receiving inadequate prenatal care were 2.35 times more likely to experience preterm delivery than women who had received appropriate prenatal care (P < 0.001; Table 5).
Table 5.
Factors associated with preterm delivery.
4. Discussion
The principal findings of this study were as follows:
The rate of teenage pregnancy in Korea was 0.49% and teenage mothers were more likely to live in rural areas and to be affiliated with low-income families.
Teenage pregnancies were associated with a higher rate of abortion, stillbirth, and vaginal delivery, and were more likely to be associated with inadequate prenatal care and subsequent risk of preterm delivery.
Among teenagers, the mean number of prenatal care visits was significantly lower in the MA group than in the NHI group.
The risk of preterm delivery in teenage mothers was significantly higher even after adjustment for living area, type of insurance, level of income, and adequacy of prenatal care.
Teenage pregnancy has previously been associated with socioeconomic deprivation.[12–14] This association has been confirmed by the fact that most teenage pregnancy cases worldwide occur in developing countries.[1] In the current study, teenage mothers were more likely to live in rural areas and come from poor families. This is consistent with previous results, which showed that, even in developed countries, teenage pregnancy is strongly related to social factors. In a study from Finland, teenage mothers were also more likely to live in rural areas, smoke, and misuse alcohol or drugs.[2] A time-course analysis has shown that there was an overall decline in teenage pregnancy overall over the past several decades, but that the rate ratio for deprived areas has increased in the United Kingdom.[12]
In addition to the fact that teenage pregnancy is more likely to occur in a socially deprived society, social factors themselves can also affect the adequacy of prenatal care among teenagers. Because of social and economic barriers, teenage mothers are less likely to attend prenatal care clinics, which can affect maternal and neonatal outcomes. In the current study, the mean number of antenatal clinic visits by teenagers and other age groups was 6.3 and 9.4, respectively. Inadequate prenatal care was more prominent in the MA group than the NIH group among teenagers, and the rate of inadequate prenatal care (defined as the number of prenatal care visits ≤4) reached 61.7% in teenagers in the MA group, suggesting that economic barriers also increased the risk of inadequate prenatal care. In Korea, the type of health insurance (MA vs NIH: poor family group vs nonpoor group) can reflect the socioeconomic status, and the ratio of MA to NIH users is reported to be about 4% to 96%.
Strikingly, 14% of teenage mothers had never received prenatal care throughout their pregnancy. This lower number of visits to prenatal care institutions is also attributed to the cultural uniqueness of Koreans. Most pregnant teenage girls are not married and an unwed pregnancy is still considered socially shameful in Korea. Under these circumstances, teenagers often conceal their pregnancy and move away from their families, preventing them from undergoing routine medical check-ups.
Both social deprivation and subsequent inadequate prenatal care can result in increased obstetric complications in teenage mothers. Even in a welfare society, teenagers are more likely to attend fewer than half of the recommended visit, and inadequate prenatal care among teenagers is a risk factor for eclampsia, urinary tract infection, and adverse neonatal outcomes.[2] To date, it has been controversial as to whether an adverse teenage pregnancy outcome is derived from a deprived socioeconomic status or from biological immaturity.[5,6,11] Indeed, adverse obstetric outcomes in teenage pregnancy can result from poor socioeconomic conditions, and the subsequent inadequate care, or from risky health behaviors. In several previous studies, teenage pregnancy itself was not a significant risk factor for adverse outcome after adjustment for socioeconomic factors.[8–10] However, in the current study, we found that the risk of preterm delivery in teenage pregnancy remained increased, even after adjustment for the adequacy of prenatal care and for socioeconomic status (such as living area, type of insurance, level of income). This is consistent with a previous study from the United States, where teenage groups were associated with increased risk for preterm delivery, low birth weight, and neonatal mortality, even after restricting the analysis to white married mothers with appropriate education levels, adequate prenatal care, and without smoking or alcohol use.[5]
Biologically speaking, the relatively small-sized uterus and short cervix typical of gynecological immaturity in teenagers may result in susceptibility to a higher risk of preterm delivery.[15] In the study by Stevens-Simon et al,[16] younger adolescents (<16 years old) had significantly shorter cervices than older adolescents (16–19 years old), and a short cervix was the only significant predictor of preterm delivery. Furthermore, competition between the fetus and adolescent mother for nutrients, and the relative nutritional deprivation of both the fetus and adolescent mother may explain the risk of maternal anemia, low birth weight, and preterm delivery.[17]
The strength of the current study is that the study was based on a well-organized national database. The NHIC is the only healthcare insurer of Korea, covering the whole Korean population. However, NHIC database does not link the information between mother and child, so that we could not analyze neonatal outcomes, such as birth weight. Further studies using other databases will be required to evaluate the association between teenage pregnancy and neonatal outcomes after adjustment for socioeconomic confounding factors.
4.1. Implication for practice and/or policy
Our results may indicate that teenage pregnancy should be managed from 2 aspects. First, from the viewpoint of the implications of our findings for public health practice and policy, our society should focus on public health policies that can improve the adequacy of prenatal care in teenagers. Second, from the viewpoint of maternal–fetal medicine, teenage pregnancy itself should be managed as a high-risk pregnancy, because of its natural medical characteristic or biological immaturity in teenagers.
5. Conclusions
In conclusion, teenage mothers in Korea have a higher risk of inadequate prenatal care and subsequent preterm delivery. Furthermore, the risk of preterm delivery in teenage pregnancy was significantly increased even after adjusting for socioeconomic confounding variables and the adequacy of prenatal care in Korean teenagers.
Footnotes
Abbreviations: aOR = adjusted odds ratio, CI = confidence interval, ICD-10 = International Classification of Diseases-10th Revision, MA = Medical Aid, similar scheme of Medicaid in the United States, NHI = National Health Insurance, NHIC = National Health Insurance Corporation, SD = standard deviation, WHO = World Health Organization.
SHL and SML contributed equally to this work.
Funding: This study was supported by a research fund from Seoul National University College of Medicine (No. 800–20140001) and a grant from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (No. HI13C0729).
Competing interests: The authors declare that they have no competing interests.
References
- 1.World Health Organization. WHO Guidelines on Preventing Early Pregnancy and Poor Reproductive Health Outcomes Among Adolescents in Developing Countries. Geneva: World Health Organization; 2011. [accessed March 1, 2016] http://whqlibdoc.who.int/publications/2011/9789241502214_eng.pdf [PubMed] [Google Scholar]
- 2.Leppälahti S, Gissler M, Mentula M, et al. Is teenage pregnancy an obstetric risk in a welfare society? A population-based study in Finland, from 2006 to 2011. BMJ Open 2013; 3:e003225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta N, Kiran U, Bhal K. Teenage pregnancies: obstetric characteristics and outcome. Eur J Obstet Gynecol Reprod Biol 2008; 137:165–171. [DOI] [PubMed] [Google Scholar]
- 4.Jolly MC, Sebire N, Harris J, et al. Obstetric risks of pregnancy in women less than 18 years old. Obstet Gynecol 2000; 96:962–966. [DOI] [PubMed] [Google Scholar]
- 5.Chen XK, Wen SW, Fleming N, et al. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. Int J Epidemiol 2007; 36:368–373. [DOI] [PubMed] [Google Scholar]
- 6.Chen CW, Tsai CY, Sung FC, et al. Adverse birth outcomes among pregnancies of teen mothers: age-specific analysis of national data in Taiwan. Child Care Health Dev 2010; 36:232–240. [DOI] [PubMed] [Google Scholar]
- 7.Mukhopadhyay P, Chaudhuri RN, Paul B. Hospital-based perinatal outcomes and complications in teenage pregnancy in India. J Health Popul Nutr 2010; 28:494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Vienne CM, Creveuil C, Dreyfus M. Does young maternal age increase the risk of adverse obstetric, fetal and neonatal outcomes: a cohort study. Eur J Obstet Gynecol Reprod Biol 2009; 147:151–156. [DOI] [PubMed] [Google Scholar]
- 9.Loto OM, Ezechi OC, Kalu BK, et al. Poor obstetric performance of teenagers: is it age- or quality of care-related? J Obstet Gynaecol 2004; 24:395–398. [DOI] [PubMed] [Google Scholar]
- 10.Raatikainen K, Heiskanen N, Verkasalo PK, et al. Good outcome of teenage pregnancies in high-quality maternity care. Eur J Public Health 2006; 16:157–161. [DOI] [PubMed] [Google Scholar]
- 11.Conde-Agudelo A, Belizán JM, Lammers C. Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: cross-sectional study. Am J Obstet Gynecol 2005; 192:342–349. [DOI] [PubMed] [Google Scholar]
- 12.McCall SJ, Bhattacharya S1, Okpo E2, et al. Evaluating the social determinants of teenage pregnancy: a temporal analysis using a UK obstetric database from 1950 to 2010. J Epidemiol Commun Health 2015; 69:49–54. [DOI] [PubMed] [Google Scholar]
- 13.McLeod A. Changing patterns of teenage pregnancy: population based study of small areas. BMJ 2001; 323:199–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uren Z, Sheers D, Dattani N. Teenage conceptions by small area deprivation in England and Wales, 2001–2002. Health Stat Q 2007; 33:34–39. [PubMed] [Google Scholar]
- 15.Stevens-Simon C1, Beach RK, McGregor JA. Does incomplete growth and development predispose teenagers to preterm delivery? A template for research. J Perinatol 2002; 22:315–323. [DOI] [PubMed] [Google Scholar]
- 16.Stevens-Simon C, Barrett J, McGregor JA, et al. Short cervix: a cause of preterm delivery in young adolescents? J Matern Fetal Med 2000; 9:342–347. [DOI] [PubMed] [Google Scholar]
- 17.Gibbs CM, Wendt A, Peters S, et al. The impact of early age at first childbirth on maternal and infant health. Paediatr Perinat Epidemiol 2012; 26:259–284. [DOI] [PMC free article] [PubMed] [Google Scholar]


