Abstract
Black esophagus is a rare, multifactorial disease. A case of acute black esophagus following pancreatic resection is presented. The patient referred us with a specific gastrointestinal bleeding. An esophagogastroduodenoscopy confirmed the diagnosis. We performed conservative treatment with complete esophageal re-epithelization and negative follow-up for stenosis or necrosis relapse.
INTRODUCTION
Acute esophageal necrosis, commonly referred to ‘black esophagus’, is a rare multifactorial condition, characterized by endoscopic images of diffuse, circumferential black mucosal discoloration in the distal esophagus that stops abruptly at the gastroesophageal junction [1].
The most common clinical presentation (90%) is acute upper GI bleeding and this represents a diagnostic challenge.
The authors report a case of a patient with acute esophageal necrosis (AEN) developed after pancreatic resection surgery.
CASE REPORT
A 72-year-old man was referred to our division with obstructive jaundice. Medical history was unremarkable.
Laboratory investigation and radiological imaging revealed a neoplasia of the ampulla of Vater not amenable to removal by endoscopic techniques.
It was decided to perform duodenocefalopancreasectomy (Whipple resection). Postoperative course was unremarkable and the patient was discharged on 12th postoperative day.
Two weeks later, the patient presented to the emergency department with hematemesis. Laboratory investigations detected anemia and an esophagogastroduodenoscopy (EGD) showed a circumferentially black-appearing mucosa at the inferior third of the esophagus (Fig. 1). The gastro-jejunal anastomosis was pervious to the passage of the instrument and no biopsies were performed.
Figure 1:
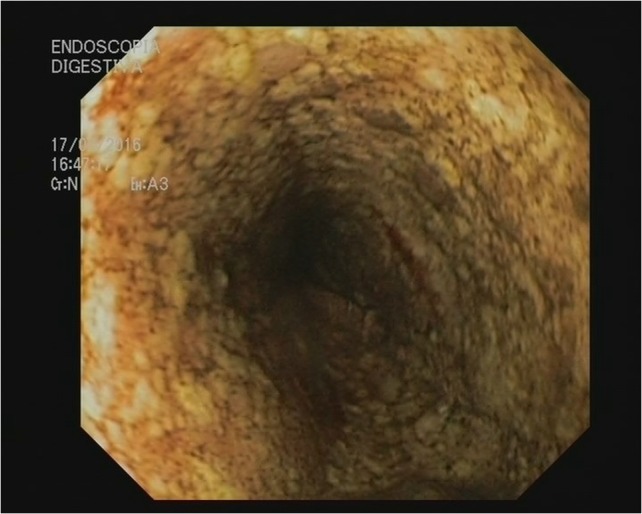
Black esophagus: AEN.
Subsequent computed tomography (CT)-scan revealed thickness of the wall of middle and inferior esophagus with a reduction of vascularization.
The patient was treated with hemotransfusion, total parenteral nutrition and high-dose proton pump inhibitor (PPI). There were no signs or symptoms of esophageal rupture.
Another EGD was performed a week later and revealed a complete esophageal re-epithelization (Fig. 2). Oral feeding was resumed and the patient was discharged. Follow-up was negative for stenosis or necrosis relapse.
Figure 2:
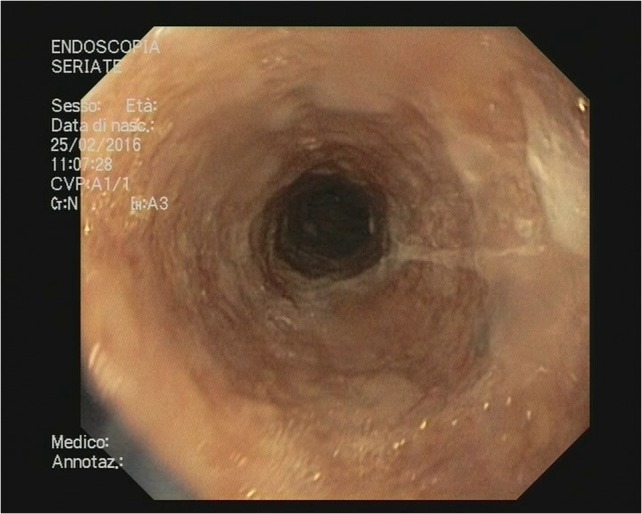
Esophageal re-epithelization.
DISCUSSION
Black esophagus (AEN) was first defined in 1990 by Goldenberg et al. Incidence is estimated between 0.1% and 0.28%. However, the disease may be underestimated due to the subtle clinical presentation and the healing properties of esophageal mucosa.
Men are four times more commonly affected than women and the peak incidence occurs at the sixth decade of life [1].
Etiology is multifactorial and usually several factors act simultaneously determining the clinical presentation. The most important are tissue hypoperfusion, altered gastric motility with acid reflux, impaired local barrier defenses associated with decrease of metabolic reserves [2, 3].
AEN may arise in the setting of hemodynamic shock, diabetes, vascular disease, thromboembolic phenomena, sepsis, immunosoppression, chronic diseases, alcohol abuse, malnutrition, multiple organ failure, recent surgery, tumors, gastric volvulus and ketoacidosis.
The most frequent clinical presentation (90%) is upper gastrointestinal bleeding with hematemesis and melena. Other symptoms include abdominal pain, dysphagia, nausea, fever and syncope [2, 4].
Laboratory tests may show anemia and leukocytosis and CT scan can reveal thickening of distal esophagus, stomach distension and a possible obstruction to gastric emptying.
EGD is essential to diagnose the disease documenting diffuse, circumferential black mucosa which abruptly stops in the Z-line.
It has been proposed an endoscopic staging of the disease: pre-necrotic esophagus (Stage 0), black esophagus (Stage 1), ‘chess-board’ esophagus (Stage 2) and re-epithelized esophagus (Stage 3) [1].
Differential diagnosis includes malignant melanoma, acanthosis nigricans, corrosive agents ingestion and infectious diseases [2].
Possible complications are perforation, esophageal stenosis and stricture formation, microbial superinfection which can lead to mediastinitis and abscess formation.
Therapeutic approaches consist of treating underlying conditions with fluid resuscitation, nil-per-os, total parenteral nutrition and intravenous PPIs or histamine receptor blocker.
The use of naso-gastric tube is not recommended due to the risk of perforation. Antimicrobial therapy should be reserved to the patients with suspected esophageal perforation, sepsis or impaired immune function [5].
Surgical treatment is to perform only with a perforated esophagus with mediastinitis or abscess formation and for the treatment of the late esophageal stricture [6].
Prognosis of black esophagus is poor with a mortality rate of 32% and it depends on underlying illnesses even if deaths secondary to esophageal necrosis occur in <6% of cases [1].
AUTHORS’ CONTRIBUTIONS
Marta Bonaldi and Corrado Sala were involved in the clinical management of the patients and drafted the manuscript. Giorgio Fratus, Pierpaolo Mariani and Lorenzo Novellino were involved in the surgical and clinical management of the patients and reviewed the manuscript. All authors read and approved the final manuscript.
CONFLICTS OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol 2007;42:29–38. [DOI] [PubMed] [Google Scholar]
- 2. Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroentero 2010;16:3219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ben Soussan E, Savoye G, Hochain P, Hervè S, Antonietti M, Lemoine F, et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc 2002;56:2013–7. [DOI] [PubMed] [Google Scholar]
- 4. Ramos R, Mascarenhas J, Duarte P, Vicente C, Casteleiro C. Acute esophageal necrosis: a retrospective case series. Rev Esp Enferm Dig 2008;100:583–5. [DOI] [PubMed] [Google Scholar]
- 5. Kim YH, Choi SY. Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis. World J Gastroentero 2007;13:5662–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Groenveld RL, Bijlsma A, Steenvoorde P, Ozdemir A. A black perforated esophagus treated with surgery: report of a case. World J Gastroentero 2013;5:199–201. [DOI] [PMC free article] [PubMed] [Google Scholar]


