Abstract
Intramural haematoma is a rare complication of oral anticoagulant therapy, occurring in 1 in 2500 patients treated with warfarin. This report describes a 71-year-old gentleman who presented with tachycardia, vomiting and abdominal distension on a background of anticoagulation for a metallic aortic valve. He was found to have a supratherapeutic international normalized ratio (INR) of 9.9 with an extensive small bowel intramural haematoma and secondary small bowel obstruction. He was successfully managed non-operatively with fluid resuscitation, INR reversal, bowel rest and nasogastric decompression. The patient's presentation was atypical with a lack of classic symptoms such as abdominal pain. This highlights the importance of considering intramural haematoma as a differential diagnosis for gastrointestinal symptoms in anticoagulated patients.
INTRODUCTION
Intramural haematoma is a rare complication of oral anticoagulant therapy, occurring in 1 in 2500 patients treated with warfarin [1]. The majority of intramural haematomas are small and can be managed non-operatively [2]. The following case demonstrates an extensive warfarin-related small bowel intramural haematoma with secondary bowel obstruction that was effectively managed non-operatively.
CASE REPORT
A 71-year-old gentleman was referred by his general practitioner with tachycardia. He reported a 2-day history of nausea, abdominal discomfort, and bloating with three episodes of bilious vomiting. He denied any pain, change in bowel habits or infective symptoms. He passed a normal bowel motion on the day of presentation and had no evidence of upper or lower gastrointestinal bleeding. His comorbid medical conditions were hypertension, hypercholesterolaemia and metallic aortic valve replacement. His regular medications included eplerenone, bisoprolol, fenofibrate and warfarin. The patient admitted taking a double dose of warfarin (4 mg daily) for the past 30 days. On arrival in the Emergency Department, his heart rate was 140 b.p.m., however, other haemodynamic parameters were normal. His abdomen was distended but soft and non-tender with active bowel sounds and no peritonism. Other system examinations were unremarkable and he had no stigmata of active bleeding. Electrocardiogram indicated rapid atrial fibrillation, which was managed with intravenous magnesium sulphate and beta blockade followed by an amiodarone infusion. Laboratory results showed a leukocytosis (white cell count 21 × 109/l), normal haemoglobin 152 g/l, elevated C-reactive protein 77 mg/l, lactate 4.6 mmol/l and supratherapeutic international normalized ratio (INR) of 9.9. The patient received urgent surgical review, fluid resuscitation and INR reversal with intravenous vitamin K, prothrombinex and two units of fresh frozen plasma. Bedside abdominal ultrasound indicated intra-abdominal free fluid which was further investigated with a computed tomography (CT) mesenteric angiogram. This showed circumferential, hyperdense bowel wall thickening involving a long segment of small bowel up to the mid-ileum (Fig. 1). The bowel wall density was 50–60 Hounsfield units, consistent with an intramural haematoma. The duodenum and the stomach were dilated with no associated transition point and the distal ileum and the colon were decompressed. Haemoperitoneum was noted adjacent to the liver and spleen (Fig. 2). Normal contrast enhancement was demonstrated in the major abdominal vasculature. The patient was admitted to the intensive care unit (ICU) for monitoring and non-operative management with bowel rest, nasogastric decompression and intravenous fluids. Warfarin was withheld and no venous thromboembolism prophylaxis administered due to his high bleeding risk. Repeat INR 5 hours after presentation was 1.5. The patient remained haemodynamically stable in ICU with no evidence of active bleeding. He reverted to sinus rhythm after 2 days of amiodarone infusion and did not require surgical intervention or blood transfusion. Diet was progressed and he was transferred to the ward on Day 3. Cardiology advised that the patient was unsuitable for NOAC (new oral anticoagulant) therapy and he was recommenced on warfarin at 1 mg daily. He was discharged on Day 6 with plan for outpatient warfarin titration. On discharge, the patient was asymptomatic, opening his bowels and tolerating full diet with INR 1.2 and stable haemoglobin of 102 g/l.
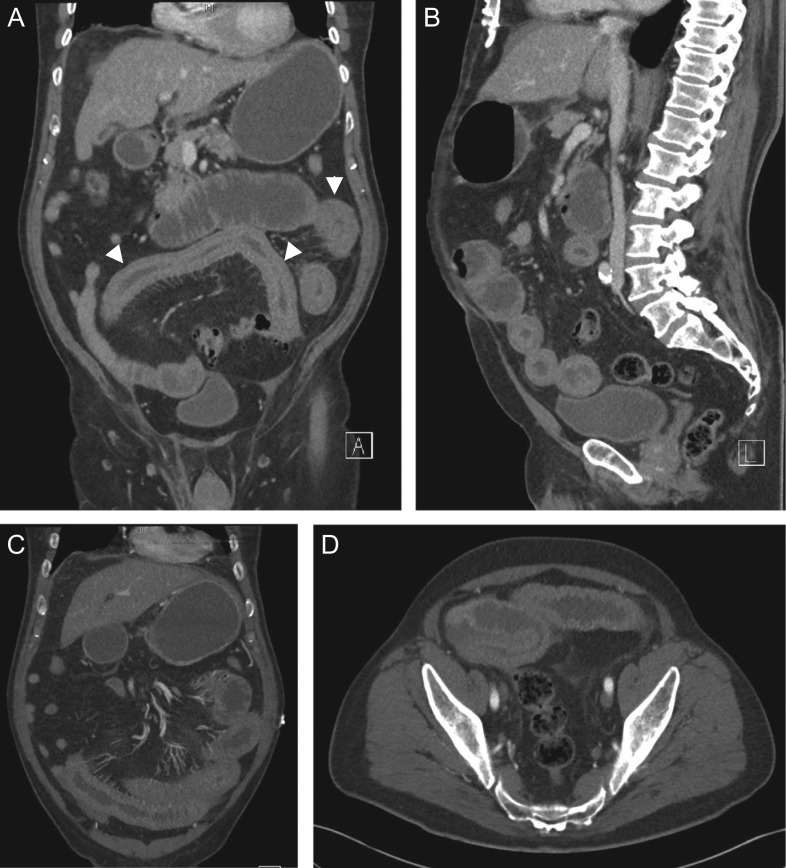
Figure 1:
Coronal (A, C), sagittal (B) and axial (D) CT showing small bowel intramural haematoma up to the mid-ileum with associated oedema causing obstruction and proximal small bowel and gastric dilatation.
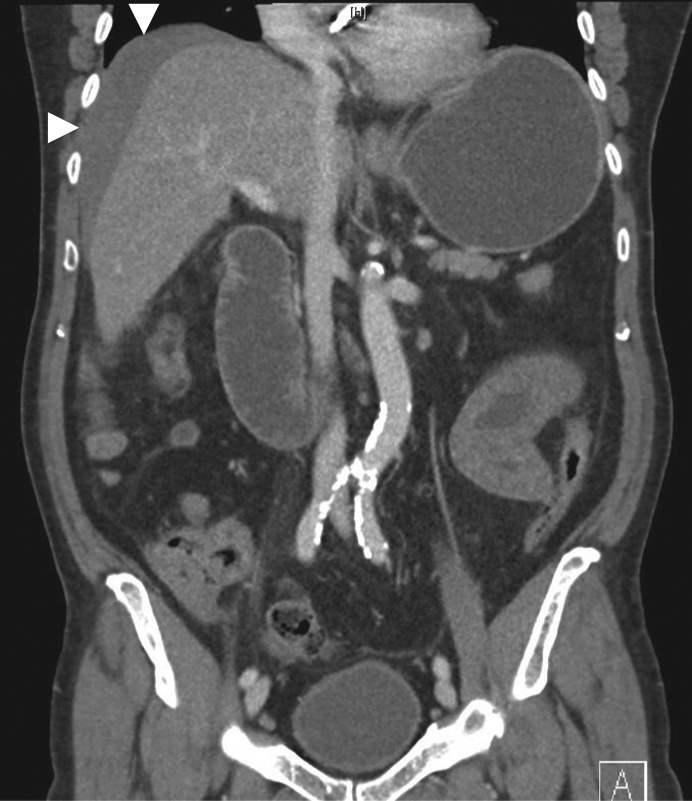
Figure 2:
Coronal CT showing haemoperitoneum adjacent to the liver.
DISCUSSION
Intestinal intramural haematoma is characterized by separation of the intestinal wall layers due to slow haemorrhage from terminal arteries in the submucosa. It is a rare cause of small bowel obstruction [2, 3]. Over 90% of cases occur secondary to blunt abdominal trauma [2]. The leading cause of non-traumatic ‘spontaneous’ intramural haematoma is supratherapeutic anticoagulation with warfarin [3]. Risk factors associated with gastrointestinal bleeding on warfarin include previous gastrointestinal bleed, advanced age, comorbidities (including atrial fibrillation, renal insufficiency and chronic liver disease) and co-administration with antiplatelet agents or medications that compete for metabolism by CYP3A4 enzymes (such as fenofibrate, as seen in this case) [4, 5]. Although NOACs (rivaroxaban, apixaban and dabigatran) have reduced risk of intracranial haemorrhage, major bleeding into any site and all-cause mortality compared to warfarin, they are associated with increased risk of major gastrointestinal bleeding (RR1.25) due to their intraluminal anticoagulant activity [4, 6].
Other predisposing factors for spontaneous intramural haematoma include coagulopathies (e.g. haemophilia, von Willebrand's disease, idiopathic thrombocytopaenic purpura), haematological malignancies (e.g. leukaemia, lymphoma and myeloma), vasculitis, pancreatitis, chemotherapy, endoscopic biopsy or injection [2, 7, 8]. Spontaneous intramural haematoma involves the small bowel in 85% of cases (particularly the jejunum); however, rare cases of isolated oesophageal, gastric, colonic and rectal haematoma have also been described [2]. In contrast, traumatic intramural haematoma usually involves the duodenum due to its relatively fixed retroperitoneal location and close relationship to the lumbar spine [2]. Spontaneous intramural haematomas are generally more extensive, with average length of 23 cm [2].
Clinical presentation of intramural haematoma varies depending on haematoma site and extent and may range from mild non-specific symptoms to severe obstruction and peritonitis [2]. Abdominal pain is the most common presenting symptom and a degree of small bowel obstruction occurs in 85% of cases [2]. The above case was atypical as the patient lacked the classic symptom of abdominal pain. In 40% of cases, rupture of the haematoma results in intraluminal haemorrhage presenting as haematemesis, frank rectal bleeding or malaena [8]. Intramesenteric or retroperitoneal bleeding may also occur, particularly with duodenal involvement [9]. Supratherapeutic INR and leukocytosis are common; however, presence of anaemia is variable, with incidence ranging from 7.6 to 84.6% in case series [3].
Non-contrast abdominal CT is the most valuable imaging modality. Diagnostic features include circumferential bowel wall thickening, intramural hyperdensity, luminal narrowing and intestinal obstruction [2]. Ultrasound is non-specific and may show intra-abdominal free fluid and intestinal wall thickening with an echogenic submucosa [2, 8].
Intramural haematomas are rarely life-threatening and can predominantly be managed non-operatively [3]. As demonstrated above, the mainstay of management is early diagnosis with appropriate resuscitation, reversal of anticoagulation (including anticoagulant cessation, administration of intravenous vitamin K, prothrombinex, fresh frozen plasma or factor concentrates as required) and management of obstructive symptoms [2]. Surgery is advised only for patients with peritonitis at presentation, active haemorrhage, suspected ischaemia, intestinal perforation or deterioration despite medical management [2].
Symptoms typically resolve within 4–6 days of non-operative management [2]. Complete haematoma resorption may take weeks to months; however, it is generally safe to recommence anticoagulant therapy after the acute episode provided it remains within therapeutic limits [2].
Despite its low incidence, intramural haematoma should be considered as a differential diagnosis in anticoagulated patients who present with gastrointestinal symptoms, even in the absence of abdominal pain. This case demonstrates the importance of early diagnosis and the role of non-operative management of an extensive small bowel intramural haematoma.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Bettler S, Montani S, Bachmann F. Incidence of intramural digestive system hematoma in anticoagulation. Epidemiologic study and clinical aspects of 59 cases observed in Switzerland (1970–1975). Schweiz Med Wochenschr 1983;113:630–6. [PubMed] [Google Scholar]
- 2. Abdel Samie A, Theilmann L. Detection and management of spontaneous intramural small bowel hematoma secondary to anticoagulant therapy. Expert Rev Gastroenterol Hepatol 2012;6:553–9. [DOI] [PubMed] [Google Scholar]
- 3. Altintoprak F, Dikicier E, Akyuz M, Deveci U, Arslan Y, Gunduz Y, et al. A retrospective review of patients with non-traumatic spontaneous intramural hematoma. Turk J Gastroenterol 2013;24:392–9. [DOI] [PubMed] [Google Scholar]
- 4. Di Minno A, Spadarella G, Spadarella E, Tremoli E, Di Minno G. Gastrointestinal bleeding in patients receiving oral anticoagulation: current treatment and pharmacological perspectives. Thromb Res 2015;136:1074–81. [DOI] [PubMed] [Google Scholar]
- 5. Kwon K, Young Cheung D, Seo Y, Bum Kim S, Nam Bae K, Jin Kim H, et al. Supportive management resolved a colonic intramural hematoma in an anticoagulant user. Intern Med 2014;53:1505–9. [DOI] [PubMed] [Google Scholar]
- 6. Desai J, Kolb J, Weitz J, Aisenberg J. Gastrointestinal bleeding with the new oral anticoagulants—defining the issues and the management strategies. Thromb Haemost 2013;110:205–12. [DOI] [PubMed] [Google Scholar]
- 7. Köseoğlu H, Solakoğlu T, Atalay R, Bolat A, Akin E, Yürekli Ö, et al. Anticoagulant-induced intramural duodenal haematoma presenting with upper-gastrointestinal haemorrhage. Arab J Gastroenterol 2013;14:180–2. [DOI] [PubMed] [Google Scholar]
- 8. Zammit A, Grech Marguerat D, Caruana C. Anticoagulation-induced spontaneous intramural small bowel haematomas. Case Rep 2013;2013:bcr2013008831–bcr2013008831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Altinkaya N, Parlakgumus A, Demir S, Alkan O, Yildirim T. Small bowel obstruction caused by intramural hematoma secondary to warfarin therapy: a report of two cases. Turk J Gastroenterol 2011;22:199–202. [DOI] [PubMed] [Google Scholar]