Abstract
BACKGROUND
Prostate cancer (PCa) outcomes are impacted by socioeconomic and biological factors. Ethnicity plays a role in the former but little is known about the responsiveness of metastatic PCa to androgen deprivation therapy (ADT) among races.
METHODS
The Surveillance, Epidemiology, and End Results (SEER) registry was used to identify men diagnosed with distant de novo metastatic PCa from 2004–2012. Patterns of presentation, overall survival (OS), and PCa-specific mortality (PCSM) were determined for each race. E3805 clinical trial data were also retrospectively reviewed to assess outcome of ADT and ADT plus docetaxel by race.
RESULTS
Of all PCa diagnoses in SEER, distant de novo metastatic disease was diagnosed in 4.2% of non-Hispanic whites, 5.8% of Hispanic whites, 5.7% of blacks, 5.5% of Asians/Pacific Islanders, and 8.8% of American Indians/Alaska natives (AI/AK) (p<0.001 by Chi-squared test). Median OS differed by race, with a greater OS observed in Asians (30 months) than in the other races (24–25 months) (p<0.001). Asians also had a superior median PCSM (54 months) compared to the other races (35–40 months) (p<0.001). In E3805, chemohormonal therapy was associated with a median OS of 58.1 months (95% CI 48.8–72.9) and 57.6 (95% CI 27.7–57.6) months in non-Hispanic whites and blacks, respectively. Few Asians participated in E3805.
CONCLUSIONS
Asian men have a greater median OS and PCSM for distant de novo metastatic PCa than men of other race. Non-Hispanic whites and blacks treated with ADT or chemohormonal therapy have comparable outcomes.
Keywords: race, ethnicity, prostate cancer, survival, chemotherapy
INTRODUCTION
There will be an estimated 180,890 prostate cancer (PCa) cases and 26,120 deaths in the USA in 2016.1, 2 Lethal PCa is due to metastatic disease, which may occur by relapse following curative-intent local therapy or as de novo metastatic PCa. An estimated 4% of metastatic PCa will be de novo at diagnosis, and it is postulated that these men may have worse outcomes compared to those that relapse.1–4 Notably, outcomes in this population have consistently been poor, with one study finding no improvement in survival in men presenting with de novo disease between 1988 and 2009 and a median overall survival (OS) of 30 months.3
It is recognized that black men with PCa have worse outcomes compared to other races. The age-adjusted number of deaths per 100,000 was 49.8 in blacks compared to 20.7 in non-Hispanic whites from 2007–2011;5 this has been attributed in part to more advanced disease at diagnosis as well socioeconomic factors. However, whether this holds true in men diagnosed with de novo metastatic disease has not been studied extensively, and it is unknown whether a survival difference between races persists. In the metastatic setting, androgen deprivation therapy (ADT) is standard and outcomes are more likely driven by biological factors.
Regarding death from PCa, a meta-analysis found blacks had a worse OS and cancer-specific survival (CSS) than whites.6 While the difference in OS was eliminated controlling for known confounders, a difference in CSS remained.6 However, there was no difference in outcome between whites and blacks when restricting analysis to de novo metastatic disease, specifically.6 This finding was recently corroborated, with no difference in OS or CSS between whites and blacks presenting with de novo PCa in the prostate-specific antigen (PSA) era observed.3 Of note, this study found Asian men had a significantly better outcome than other races.3 It was also observed in the SWOG studies during the PSA era that black race did not impact outcome for metastatic PCa treated with ADT whereas previous studies reported poorer outcomes for blacks.7
Outcomes, by race, for metastatic castration-resistant prostate cancer have been assessed.8, 9 Clinical trials suggest blacks have a shorter time to PSA progression than whites but no difference in OS.8 A larger study of pooled clinical trial data confirmed no difference in OS between blacks and whites.9
Recently, the E3805 (CHAARTED) trial showed a 13.6 month improvement in median OS with early chemohormonal therapy (CHT) with ADT plus docetaxel over ADT alone in men with metastatic hormone-sensitive PCa.10 Additionally, it was found that men with high volume disease (presence of visceral metastases or ≥4 bone metastases with ≥1 beyond the vertebra or pelvis) appeared to derive the greatest benefit.10 It is unknown whether race predicted response to CHT.
There is currently a paucity of data regarding patterns of presentation and survival of de novo metastatic PCa by race. Moreover, it is unknown whether different races derive the same benefit from CHT for high volume metastatic hormone-sensitive PCa. We hypothesized that survival differences exist between races in men that present with de novo metastatic PCa. Thus, we performed descriptive statistics to detail the survival data for patients of different race with distant de novo metastatic PCa from a large population-based patient database. In addition, we explored whether survival differences existed between races in the E3805 clinical trial.
MATERIALS AND METHODS
SEER Registry
The National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) 18 Registry contains representative cancer statistics from an estimated 28% of the American population. Data on men diagnosed with de novo metastatic disease is available from 2004 onward. Thus, we obtained data on stage of PCa at diagnosis, by race, for men of known age with an International Classification of Diseases for Oncology Third Edition (ICD-O-3) / World Health Organization 2008 site recode of ‘prostate’ from 2004–2012.11, 12 Cases were categorized as low-intermediate risk localized, high risk localized, locoregional stage IV, or distant metastatic PCa (Supplementary Materials). Races were categorized as non-Hispanic white, Hispanic white, black, Asian/Pacific Islander, American Indian/Alaska native, and unknown (Supplementary Materials).
Survival data for men diagnosed with distant de novo metastatic PCa was obtained from SEER. Cases were selected with the following criteria: actively followed, malignant behavior, known age, and cases in research database. Cases that did not contain survival data were excluded. OS was observed from time of diagnosis until death, in months, with a cutoff of December 2012. Prostate-cancer specific mortality (PCSM) utilized a cause of death defined as dead due to cancer using SEER’s cause-specific death classification.
E3805 Clinical Trial
The primary objective of E3805 (CHAARTED; ClinicalTrials.gov number NCT00309985) was to evaluate whether early CHT in metastatic hormone-sensitive PCa improved OS over ADT alone. This study enrolled patients with metastatic hormone-sensitive PCa who were either treatment naive or within 120 days of starting ADT for metastatic disease. Patients were randomized to either ADT alone or CHT with ADT plus docetaxel dosed at 75 mg per meter of body-surface area every 3 weeks for 6 cycles. Patients were stratified by a number of factors, including volume of metastases (high versus low) and age. From July 2006 to December 2012, a total of 790 patients were enrolled and randomized.
Total numbers and percentages of men of different race (non-Hispanic white, Hispanic white, black, Asian, and Native American) by disease volume and history of prior local therapy were extracted and presented descriptively. Those without a history of prior local therapy were presumed to have presented with de novo metastatic disease whereas those with prior local therapy were presumed to have relapsed. Total number of deaths and median OS were calculated for each race in each treatment arm by intention-to-treat analysis. OS was calculated from date of randomization until death.
Statistical Analysis
Proportions of patients diagnosed with de novo metastatic PCa, by race, were compared by the Chi-square test. Proportions of non-Hispanic whites were compared pairwise to Hispanic whites, blacks, Asians, and American Indians by the Chi-square test. Survival was calculated using the Kaplan-Meier method and 95% confidence intervals (CI), with the Log-rank test used to assess for a difference in survival by race. Univariable analysis of PCSM was conducted using Fine and Gray competing risks regression, with point estimates obtained by fitting a null model (no covariates) to each race. Multivariable analysis using competing risks regression without or with adjustment for patient demographic variables (marital status, county income, county education level, patient age, metropolitan versus non-metropolitan county) was then performed to test whether a different PCSM existed between each race compared to non-Hispanic whites. Continuous variables were dichotomized around the median of each covariate, with county type of residence defined as per USDA Rural-Urban Continuum codes. Analyses were conducted using SEER*Stat and Stata MP 14.0 (SEER) and SAS Version 9.4 (E3805) with statistical significance defined as a 2-sided p-value <0.05.
RESULTS
SEER Registry Data
From 2004–2012, a total of 450,076 men were diagnosed with low-intermediate risk localized PCa (92.0%), 8,961 with high risk localized PCa (1.8%), 8,104 with locoregional stage IV PCa (1.7%), and 22,322 with distant metastatic PCa (4.6%). By race, the majority of diagnoses were among non-Hispanic whites across all stages, with 316,808 low-intermediate risk localized PCa (70.4%), 6,459 high-risk localized PCa (72.1%), 5,692 locoregional stage IV PCa (70.2%), and 14,528 distant metastatic PCa (65.1%). Within each race, a higher proportion of Hispanic whites and non-whites were diagnosed with distant metastatic disease (5.7%) than non-Hispanic whites (4.2%) (p<0.001) (Table 1). Proportions of men of each race presenting with distant de novo metastatic PCa by year of diagnosis are presented in Supplemental Table 1 and Supplemental Figure 1 (Supplementary Materials). The proportion of men diagnosed with distant de novo disease was higher in 2012 compared to 2004 in non-Hispanic whites (p<0.001), Hispanic whites (p=0.001), blacks (p=0.027), and Asians (p=0.010), but not in American Indians (p=0.791) or men of unknown race (p=0.242).
Table 1.
Total diagnoses of PCa by stage and race from 2004–2012.
| All races N (%) | White Non-Hisp N (%) | White Hisp N (%) | Black N (%) | Asian/PI N (%) | AI/AK N (%) | Unknown N (%) | |
|---|---|---|---|---|---|---|---|
| Low-int risk | 450,076 (92.0) | 316,808 (92.2) | 35,559 (90.3) | 63,660 (91.1) | 20,009 (90.5) | 1,452 (86.0) | 12,588 (97.1) |
| High risk | 8,961 (1.8) | 6,459 (1.9) | 720 (1.8) | 1,107 (1.6) | 513 (2.3) | 43 (2.5) | 119 (0.9) |
| Locoregional Stage IV | 8,104 (1.7) | 5,692 (1.7 | 790 (2.0) | 1,122 (1.6) | 383 (1.7) | 46 (2.7) | 71 (0.5) |
| Distant Metastatic | 22,322 (4.6) | 14,528 (4.2) | 2,295 (5.8) | 3,958 (5.7) | 1,211 (5.5) | 148 (8.8) | 182 (1.4) |
| Total | 489,463 | 343,487 | 39,364 | 69,847 | 22,116 | 1,689 | 12,960 |
Low-intermediate risk PCa = T1-2N0/XM0/X
High risk PCa = T3N0/XM0/X
Locoregional Stage IV PCa = T4 and/or N1M0/X
Distant Metastatic = M1
Hisp = Hispanic
PI = Pacific Islander
AI = American Indian
AK = Alaskan native
Next, survival data for men diagnosed with distant de novo metastatic PCa were obtained. Twenty-nine of the 22,322 patients were excluded due to lack of survival data. Median OS among 22,293 evaluable cases was 25 months, and the 1-, 3-, and 5-year OS was 71.5%, 36.7%, and 22.4%, respectively. By race, median OS was 24 months in non-Hispanic whites, 25 months in Hispanic whites, 24 months in blacks, 30 months in Asians, and 23 months in American Indians. Specifically, Hispanic whites and Asians had a greater 5-year OS than non-Hispanic whites (p<0.001), while there was no statistical difference in survival between non-Hispanic whites and blacks (p=0.057) and American Indians (p=0.398). Overall survival, by race, is shown in Table 2.
Table 2.
OS by race for men diagnosed with distant metastatic PCa
| All races (N= 22,293) | White Non-Hisp (N= 14,509) | White Hisp (N= 2,294) | Black (N= 3,954) | Asian/PI (N= 1,208) | AI/AK (N= 147) | Unknown (N=181) | |
|---|---|---|---|---|---|---|---|
| 1 yr | 71.5% | 70.8% | 73.4% | 71.0% | 75.8% | 65.7% | 86.4% |
| 2 yr | 50.2% | 49.5% | 51.2% | 49.1% | 57.5% | 47.3% | 70.9% |
| 3 yr | 36.7% | 35.4% | 39.2% | 37.0% | 44.8% | 32.4% | 57.8% |
| 4 yr | 27.9% | 26.6% | 31.4% | 28.0% | 34.9% | 26.8% | 50.4% |
| 5 yr | 22.4% | 21.1% | 25.9% | 22.4% | 29.9% | 19.0% | 40.4% |
Regarding PCSM, 241 men were excluded from analysis due to lack of survival data or unknown cause of death. In the remaining 22,052 evaluable cases with distant de novo metastatic PCa, median time to death from PCa was 40 months. The 1-, 3-, and 5-year PCSM was 21.1%, 47.8%, and 58.5%, respectively. Median PCSM was 38 months in non-Hispanic whites, 40 months in Hispanic whites, 40 months in blacks, 54 months in Asians, and 35 months in American Indians. Consistent with OS data, Asians had the greatest time to death from PCa among the races (Tables 3 and 4). While Hispanic whites had better PCSM than non-Hispanic whites on univariable analysis (Hazard ratio (HR) 0.93, 95% CI 0.87–1.00; p=0.045), this difference lost statistical significance upon multivariable analysis (Table 4). Asians, however, retained a near 20% decreased risk of death from PCa compared with non-Hispanic whites independent of sociodemographic factors (Table 4). Notably, when year of diagnosis was included in the model, later year of diagnosis was predictive of reduced risk of PCSM (HR 0.97, 95% CI 0.96–0.98; p<0.001), and there was no interaction between race and year of diagnosis (p>0.3 in all cases, model not shown).
Table 3.
PCSM by race for men diagnosed with distant de novo metastatic PCa
| All races (N= 22,052) | White Non-Hisp (N=14,418) | White Hisp (N=2,216) | Black (N=3,921) | Asian/PI (N=1,175) | AI/AK (N=145) | Unknown (N=177) | |
|---|---|---|---|---|---|---|---|
| 1 yr | 21.1% | 21.3% | 19.5% | 22.1% | 18.4% | 26.9% | 9.1% |
| 2 yr | 37.5% | 37.8% | 37.7% | 38.8% | 30.2% | 41.4% | 21.4% |
| 3 yr | 47.8% | 48.7% | 46.8% | 47.9% | 39.7% | 50.8% | 30.3% |
| 4 yr | 54.5% | 55.2% | 53.5% | 54.7% | 47.8% | 56.4% | 37.7% |
| 5 yr | 58.5% | 59.1% | 57.5% | 58.8% | 51.6% | 62.2% | 46.5% |
Table 4.
Proportional hazard models for PCSM
| Covariates | Multivariable Analysis
|
||
|---|---|---|---|
| HR | 95% CI | p-value | |
|
| |||
| Race | |||
| White Non-Hisp | 1.00 | – | Ref |
| White Hisp | 0.94 | 0.87–1.01 | 0.094 |
| Black | 1.00 | 0.94–1.06 | 0.982 |
| Asian/Pacific Islanders | 0.81 | 0.74–0.89 | <0.001 |
| AI/AK | 1.23 | 0.95–1.59 | 0.119 |
|
| |||
| Marital status | |||
| Unmarried | 1.00 | – | Ref |
| Married or domestic partner | 0.89 | 0.86–0.93 | <0.001 |
|
| |||
| County-wide median family income | |||
| <$66,610 | 1.00 | – | Ref |
| ≥$66,610 | 1.05 | 0.99–1.10 | 0.078 |
|
| |||
| % adults not completing high school | |||
| ≥14.1% | 1.00 | – | Ref |
| <14.1% | 0.96 | 0.92–1.01 | 0.114 |
|
| |||
| Age at diagnosis (years) | |||
| ≤73 | 1.00 | – | Ref |
| >73 | 1.18 | 1.13–1.23 | <0.001 |
|
| |||
| County type of residence | |||
| Non-metropolitan | 1.00 | – | Ref |
| Metropolitan | 0.95 | 0.89–1.01 | 0.129 |
E3805 Clinical Trial Data
From 2006–2012, a total of 790 men were enrolled in E3805, with race and ethnicity known in 719 patients. Of these, 201 had received prior local therapy (28.0%) compared to 517 that had no prior therapy and presumed to have presented with de novo metastatic disease (72.0%). Non-Hispanic whites made up the vast majority of participants regardless of stage at diagnosis (82.8%) with 174 previously treated with local therapy and 420 presumed de novo metastatic at diagnosis. Similar to SEER, proportionally more Hispanic whites and blacks with de novo metastatic PCa were enrolled than non-Hispanic whites, however the difference was not statistically significant (p=0.07); notably, a higher percentage of Hispanic white, black, Asian, and American Indian men had high volume metastatic disease than did non-Hispanic whites (p=0.004) (Table 5).
Table 5.
Distribution of disease volume and prior local therapy by race in E3805
| White Non-Hisp (N=595) |
White Hisp (N=38) |
Black (N=76) |
Asian/PI (N=8) |
AI/AK (N=2) |
Total (N=719) |
|
|---|---|---|---|---|---|---|
| Disease volume | ||||||
| High | 371 (62.4%) | 31 (81.6%) | 55 (72.4%) | 6 (75.0%) | 2 (100.0%) | 465 (64.7%) |
| Low | 224 (37.6%) | 7 (18.4%) | 21 (27.6%) | 2 (25.0%) | 0 | 254 (35.3%) |
| Prior local therapy | ||||||
| No | 420 (70.7%) | 30 (78.9%) | 60 (78.9%) | 5 (62.5%) | 2 (100.0%) | 517 (72.0%) |
| Yes | 174 (29.3%) | 8 (21.1%) | 16 (21.1%) | 3 (37.5%) | 0 | 201 (28.0%) |
| Missing | 1 | 0 | 0 | 0 | 0 | 1 |
Survival, by race, for men in the ADT alone arm and ADT plus docetaxel arm is shown in Figure 1A and 1B, respectively. Median OS of those randomized to ADT alone was 45.2 months (95% CI 34.5–49.5) for non-Hispanic whites (62% with protocol-defined high volume disease), 34.1 months (95% CI 22.5-NA) for blacks (with 72% high volume disease), and not reached for Hispanic whites, Asians, or American Indians. In the ADT plus docetaxel arm, non-Hispanic whites and blacks had comparable outcomes, with a median OS of 58.1 months (95% CI 48.8–72.9) in non-Hispanic whites and 57.6 months (95% CI 27.7–57.6) in blacks (p=0.44). Total numbers of evaluable patients and deaths, by race and within each arm, are shown in Table 6.
Figure 1.
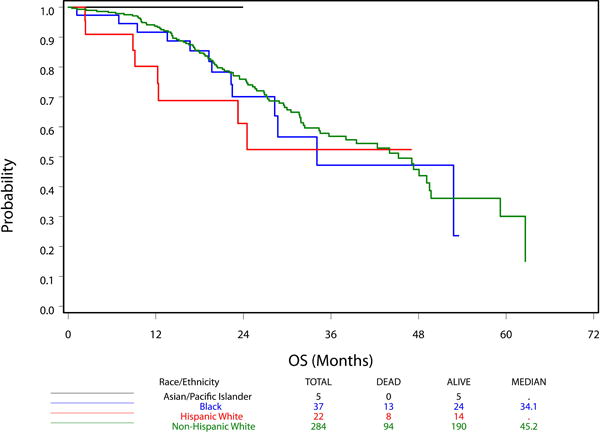
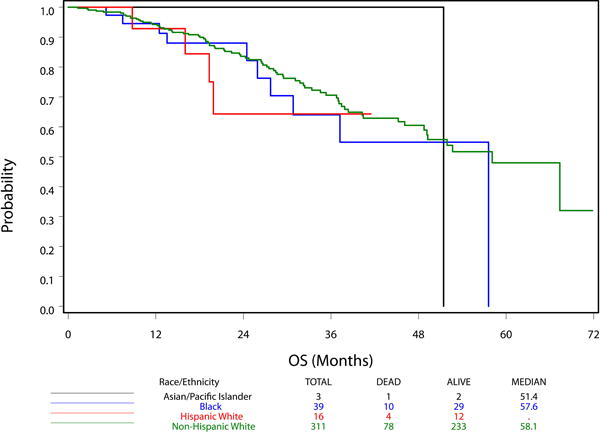
OS by race for men in E3805 in the ADT alone arm (A) and ADT plus docetaxel arm (B)
Table 6.
OS by race and treatment arm in E3805
| Arm B (ADT alone) | White Non-Hisp | White Hisp | Black | Asian/PI | AI/AK |
|---|---|---|---|---|---|
| Sample size | 284 | 22 | 37 | 5 | 1 |
| Number of deaths | 94 | 8 | 13 | 0 | 0 |
| Median OS (95% CI; months) | 45.2 (34.5, 49.5) | NR1 (12.3, –) | 34.1 (22.5, –) | NR (–, –) | NA2 |
| Arm A (ADT + docetaxel) | White Non-Hisp | White Hisp | Black | Asian/PI | AI/AK |
|---|---|---|---|---|---|
| Sample size | 311 | 16 | 39 | 3 | 1 |
| Number of deaths | 78 | 4 | 10 | 1 | 1 |
| Median OS (95% CI; months) | 58.1 (48.8, 72.9) | NR1 (19.3, –) | 57.6 (27.7, 57.6) | 51.4 (–, –) | NA2 |
Median not reached
Individual data could not be reported.
PCSM in E3805, by arm, is shown in Table 7. The PCSM in the ADT alone arm for the total population was 6.0%, 39.5%, and 59.7% at 1-, 3-, and 5-years, respectively. That in the ADT plus docetaxel arm was 4.1%, 25.1%, and 48.7%. Small numbers of non-white participants and limited number of events as of last follow-up preclude further comparison at this time.
Table 7.
PCSM by race and treatment arm in E3805
| Arm B (ADT alone) | All races | White Non-Hisp | White Hisp | Black | Asian/PI | AI/AK |
|---|---|---|---|---|---|---|
| 1 yr | 6.0% | 5.2% | 19.8% | 5.6% | 0% | 0% |
| 2 yr | 21.1% | 19.2% | 38.9% | 27.2% | NA | NA |
| 3 yr | 39.5% | 37.7% | 47.6% | 50.1% | NA | NA |
| 4 yr | 47.4% | 46.9% | NA | 50.1% | NA | NA |
| 5 yr | 59.7% | 60.5% | NA | NA | NA | NA |
| Arm A (ADT + docetaxel) | All races | White Non-Hisp | White Hisp | Black | Asian/PI | AI/AK |
|---|---|---|---|---|---|---|
| 1 yr | 4.1% | 4.5% | 0% | 2.8% | 0% | 0% |
| 2 yr | 13.4% | 13.3% | 28.5% | 9.3% | 0% | 0% |
| 3 yr | 25.1% | 24.9% | 28.5% | 27.4% | 0% | 0% |
| 4 yr | 33.9% | 34.0% | NA | 36.6% | 0% | NA |
| 5 yr | 48.7% | 44.9% | NA | NA | NA | NA |
DISCUSSION
This study using a large population-based database supports the notion that, in the PSA era, the OS and PCSM of blacks diagnosed with distant de novo metastatic PCa does not differ from non-Hispanic Whites. Moreover, this finding was despite a greater proportion of blacks presenting with distant metastatic disease. Interestingly, we found that Asians had superior survival compared to the other races when accounting for socioeconomic factors. These data are potentially discordant with those from the E3805 clinical trial, where blacks experienced a numerically inferior survival with ADT alone compared to non-Hispanic whites. However, this may be due to the greater proportion of blacks with high volume disease, and due to a smaller number of blacks precluding a reliable statistical comparison between the 2 races at this time. Importantly, there was no apparent difference in outcome between non-Hispanic whites and blacks treated with CHT, highlighting the generalized benefit of this approach.
Prostate Cancer Presentation
Patterns of PCa presentation by stage have been evaluated previously. One series found an equivalent number of whites and blacks presented with metastatic disease in an equal access medical center from 1991–1997.13 Notably, these data were collected during the time that PSA screening became widespread. More recently, Ryan et al. showed a reduction in the proportion of men presenting with metastatic disease in a large PCa registry.14 While black race and lower socioeconomic status were associated with an increased likelihood of metastasis at presentation on univariable analysis, this finding was not confirmed on multivariable analysis, with biologic factors (higher serum PSA and Gleason grade) being the only associated variables. Moreover, the proportion of whites and blacks presenting with metastatic PCa in this series remained consistent over time.14 The number of men diagnosed with distant de novo metastatic PCa in SEER is consistent with these prior results, with 4.2% of non-Hispanic whites and 5.7% of blacks presenting with metastatic disease. Interestingly, our SEER results do suggest a slight increase in the proportion of men presenting with distant de novo metastatic PCa over time – a pattern that pre-dates the 2012 US Preventive Services Task Force recommendation against routine PSA screening. It remains to be seen whether this translates into an increased rate per 100,000 of de novo metastatic disease in the modern era.
Prostate Cancer Survival
Regarding survival, a study examining SEER-Medicare data of men aged >65 years found that blacks had a higher risk of death from earlier stage (but not metastatic) PCa than whites.15 By stage, Muralidhar et al. showed that the 5-year PCSM was 41.1% in patients that presented with distant disease.16 Interestingly, the authors found whites to have a greater increase in conditional survival over time compared to non-whites with locoregional but not distant metastatic disease.16 This study highlights the fact that long-term survivors of metastatic PCa can have a continued reduction in their risk of PCSM with time, potentially due to more biologically indolent disease.
Prostate cancer and Race
By race, Tangen et al. demonstrated that median OS in men with metastatic PCa has improved from 30–33 months in the pre-PSA era to 49 months in the PSA era based on data from 3 large randomized, controlled trials.7 Importantly, this study showed a dramatic improvement in survival in blacks between the eras (median OS of 27 months pre-PSA versus 48 months after PSA implementation). Furthermore, survival in blacks was shown to be equivalent to whites (49 months) in the PSA era.7 Additionally, prospective registry data from an underserved, inner city hospital found a 5-year CSS of 65.6% in 129 men with de novo metastatic disease; 97.7% of men in this study were black.17 While these data are consistent with those from E3805, they are in disagreement with our findings from SEER, with a median OS of 24 months in non-Hispanic whites and blacks (25 months in the entire population) and 5-year PCSM of 58.5% for the entire population (59.1% non-Hispanic whites, 58.8% blacks). It is possible the lower survival seen in SEER reflects a more real-world outcome as opposed to clinical trial conditions or small hospital registry series. Moreover, our data from SEER reflects solely patients diagnosed with distant de novo metastatic PCa and not those that relapsed; it is speculated that distant de novo disease represents a more aggressive variant with worse outcomes, with clinical trials often including a heterogeneous population of patients metastatic at first diagnosis and relapsed disease after therapy for localized disease.
Prostate Cancer in Asians
Our study showed greater OS and superior PCSM among Asians compared to the other races in SEER. An important consideration is whether outcomes in Asian-Americans are similar or different to residents of Asia. Notably, 5-year survival for Japanese men diagnosed with distant de novo metastatic PCa ranges from 39.6–61.8%.18–20 Furthermore, studies of Chinese and Taiwanese men with metastatic PCa found a 5-year OS of 40.0–41.4%.21–23 These results are similar to the outcomes found for Asians in the SEER registry, with a 5-year OS of 29.9% and a PCSM of 51.6% in Asians in the United States. Differences between study methodology, access to healthcare, and environmental factors may account for the observed variability between these series.
The superior survival of Asians in the SEER results of our study suggests a possible biological difference between the races with respect to risk of relapse after therapy for localized disease and responsiveness to therapy, given potentially similar environmental exposures in this American population. Indeed, one small retrospective study from Hawaii found that Japanese men had improved outcomes when treated with hormonal therapy compared to white men at the same institution, with race emerging as a significant prognostic variable on multivariable analysis.24 A presumption is that differences between races is due to factors at a genomic level, with one study having evaluated mutational differences in the androgen receptor (AR) gene between blacks and whites; the investigators showed a higher rate of both germline and somatic mutations in the AR gene in blacks than in whites and suggested that this may account for differences in disease presentation and natural history.25 As such, it is plausible that genomic differences may contribute to the better survival in Asians seen in this study. That said, cultural differences between races can impact environmental exposures, with differences in diet and other lifestyle factors possibly affecting survival.
Limitations
Our work has limitations and should be interpreted in the context of its design. Race classification in SEER is derived from medical records and death certificates, with misclassification bias a concern. Moreover, numbers for Asians and American Indians were small in both SEER and E3805, therefore conclusions drawn from outcomes in these populations should be viewed with caution. Similarly, relatively fewer Hispanic whites and blacks were enrolled in E3805, restricting the statistical comparison of survival between the races. Lastly, survival data in SEER were calculated from the date of diagnosis until death while those in E3805 were from time of randomization until death; it is possible that this may account for some of the difference in outcome seen between the 2 cohorts, however given the median time from ADT start to randomization in E3805 was 1.2 months (with 87% of patients starting ADT prior to randomization)10 the effect of this difference is estimated to be minimal.
Conclusions
In conclusion, we have shown using a population-based registry that survival in black men diagnosed with distant de novo metastatic prostate cancer is similar to that of non-Hispanic white men; Asian men lived longer than men of other races, and further work is necessary to elucidate the cause of this phenomenon. These findings remain to be reproduced in the clinical trial setting of E3805, with presently too few events having occurred for blacks that received ADT alone and few Asian participants to make survival comparisons by race for men that received ADT alone. Importantly, however, chemohormonal therapy did confer a comparable survival advantage to blacks compared to non-Hispanic whites, with no differential effect on survival by race observed. As such, clinicians may have confidence in the potential benefit of chemohormonal therapy in black men with metastatic hormone-sensitive prostate cancer and, after discussing the risks and benefits, consider offering such treatment to appropriate patients.
Supplementary Material
Acknowledgments
Funding sources: none
Footnotes
Brandon Bernard, MD: data curation; investigation; writing – original draft; writing – review & editing
Vinayak Muralidhar, MD: formal analysis; methodology; writing – original draft; writing – review & editing
Yu-Hui Chen, MS, MPH: formal analysis; visualization; writing – review & editing
Srikala S. Sridhar, MD: supervision; writing – review & editing
Edith Mitchell, MD: writing – review & editing
Curtis A. Pettaway, MD: writing – review & editing
Michael Carducci, MD: writing – review & editing
Paul L. Nguyen, MD: writing – review & editing
Christopher J. Sweeney, MBBS: conceptualization; methodology; project administration supervision; writing – review & editing
Potential conflicts of interest: none
References
- 1.SEER cancer statistics factsheets: Prostate cancer. Available from URL: http://seer.cancer.gov/statfacts/html/prost.html [accessed November 10, 2015.
- 2.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2012. National Cancer Institute; Bethesda, MD: http://seer.cancer.gov/csr/1975_2012/, based on November 2014 SEER data submission, posted to the SEER web site, April 2015. [Google Scholar]
- 3.Wu JN, Fish KM, Evans CP, Devere White RW, Dall’Era MA. No improvement noted in overall or cause-specific survival for men presenting with metastatic prostate cancer over a 20-year period. Cancer. 2014;120:818–823. doi: 10.1002/cncr.28485. [DOI] [PubMed] [Google Scholar]
- 4.Gravis G, Boher JM, Joly F, et al. Androgen Deprivation Therapy (ADT) Plus Docetaxel Versus ADT Alone in Metastatic Non castrate Prostate Cancer: Impact of Metastatic Burden and Long-term Survival Analysis of the Randomized Phase 3 GETUG-AFU15 Trial. Eur Urol. 2015 doi: 10.1016/j.eururo.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 6.Evans S, Metcalfe C, Ibrahim F, Persad R, Ben-Shlomo Y. Investigating Black-White differences in prostate cancer prognosis: A systematic review and meta-analysis. Int J Cancer. 2008;123:430–435. doi: 10.1002/ijc.23500. [DOI] [PubMed] [Google Scholar]
- 7.Tangen CM, Hussain MH, Higano CS, et al. Improved overall survival trends of men with newly diagnosed M1 prostate cancer: a SWOG phase III trial experience (S8494, S8894 and S9346) J Urol. 2012;188:1164–1169. doi: 10.1016/j.juro.2012.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thatai LC, Banerjee M, Lai Z, Vaishampayan U. Racial disparity in clinical course and outcome of metastatic androgen-independent prostate cancer. Urology. 2004;64:738–743. doi: 10.1016/j.urology.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 9.Halabi S, Small EJ, Vogelzang NJ, Barrier RC, Jr, George SL, Gilligan TD. Impact of race on survival in men with metastatic hormone-refractory prostate cancer. Urology. 2004;64:212–217. doi: 10.1016/j.urology.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 10.Sweeney CJ, Chen YH, Carducci M, et al. Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N Engl J Med. 2015;373:737–746. doi: 10.1056/NEJMoa1503747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Surveillance, Epidemiology, and End Results (SEER) Program SEER*Stat Database: Incidence - SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2014 Sub (2000–2012) <Katrina/Rita Population Adjustment> - Linked to County Attributes - Total U.S., 1969–2012 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2015, based on the November 2014 submission.
- 12.Surveillance Research Program, National Cancer Institute SEER*Stat software
- 13.Freedland SJ, Sutter ME, Naitoh J, Dorey F, Csathy GS, Aronson WJ. Clinical characteristics in black and white men with prostate cancer in an equal access medical center. Urology. 2000;55:387–390. doi: 10.1016/s0090-4295(99)00461-6. [DOI] [PubMed] [Google Scholar]
- 14.Ryan CJ, Elkin EP, Small EJ, Duchane J, Carroll P. Reduced incidence of bony metastasis at initial prostate cancer diagnosis: data from CaPSURE. Urol Oncol. 2006;24:396–402. doi: 10.1016/j.urolonc.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Taksler GB, Keating NL, Cutler DM. Explaining racial differences in prostate cancer mortality. Cancer. 2012;118:4280–4289. doi: 10.1002/cncr.27379. [DOI] [PubMed] [Google Scholar]
- 16.Muralidhar V, Mahal BA, Nguyen PL. Conditional cancer-specific mortality in T4, N1, or M1 prostate cancer: implications for long-term prognosis. Radiat Oncol. 2015;10:155. doi: 10.1186/s13014-015-0470-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Winer AG, Sfakianos JP, Hyacinthe LM, McNeil BK. A 10-year analysis of metastatic prostate cancer as an initial presentation in an underserved population. Int Braz J Urol. 2014;40:316–321. doi: 10.1590/S1677-5538.IBJU.2014.03.04. [DOI] [PubMed] [Google Scholar]
- 18.Matsuda T, Ajiki W, Marugame T, et al. Population-based survival of cancer patients diagnosed between 1993 and 1999 in Japan: a chronological and international comparative study. Jpn J Clin Oncol. 2011;41:40–51. doi: 10.1093/jjco/hyq167. [DOI] [PubMed] [Google Scholar]
- 19.Fujimoto H, Nakanishi H, Miki T, et al. Oncological outcomes of the prostate cancer patients registered in 2004: report from the Cancer Registration Committee of the JUA. Int J Urol. 2011;18:876–881. doi: 10.1111/j.1442-2042.2011.02895.x. [DOI] [PubMed] [Google Scholar]
- 20.Kitagawa Y, Ueno S, Izumi K, et al. Clinical outcomes and nadir prostate-specific antigen (PSA) according to initial PSA levels in primary androgen deprivation therapy for metastatic prostate cancer. World J Urol. 2015 doi: 10.1007/s00345-015-1621-5. [DOI] [PubMed] [Google Scholar]
- 21.Chia SE, Tan CS, Lim GH, Sim X, Lau W, Chia KS. Incidence, mortality and five-year relative survival ratio of prostate cancer among Chinese residents in Singapore from 1968 to 2002 by metastatic staging. Ann Acad Med Singapore. 2010;39:466–471. [PubMed] [Google Scholar]
- 22.Chen XQ, Huang Y, Li X, et al. Efficacy of maximal androgen blockade versus castration alone in the treatment of advanced prostate cancer: a retrospective clinical experience from a Chinese medical centre. Asian J Androl. 2010;12:718–727. doi: 10.1038/aja.2010.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen CH, Tzai TS, Huang SP, et al. Clinical outcome of Taiwanese men with metastatic prostate cancer compared with other ethnic groups. Urology. 2008;72:1287–1292. doi: 10.1016/j.urology.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 24.Fukagai T, Namiki TS, Carlile RG, Yoshida H, Namiki M. Comparison of the clinical outcome after hormonal therapy for prostate cancer between Japanese and Caucasian men. BJU Int. 2006;97:1190–1193. doi: 10.1111/j.1464-410X.2006.06201.x. [DOI] [PubMed] [Google Scholar]
- 25.Koochekpour S, Buckles E, Shourideh M, et al. Androgen receptor mutations and polymorphisms in African American prostate cancer. Int J Biol Sci. 2014;10:643–651. doi: 10.7150/ijbs.8974. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


