Abstract
Objective
To estimate whether postpartum visit attendance was improved in women exposed to a postpartum patient navigation program compared with those who received care immediately prior to the program's initiation, and to assess whether other postpartum health behaviors improved during the intervention period.
Methods
This is a prospective observational study of women enrolled in a patient navigation program compared to women receiving care prior to the program. Navigating New Motherhood was a postpartum patient navigation program for adult, English-speaking women receiving prenatal care at a Medicaid-based university clinic. In 2015, Navigating New Motherhood introduced a clinic-level change in which a navigator was hired and assumed supportive and logistical responsibilities for enrolled patients between delivery and postpartum visit completion. We compared medical record data from women who enrolled in Navigating New Motherhood to those of women receiving care in the same clinic for one year immediately prior to Navigating New Motherhood. The primary outcome was postpartum visit attendance. Secondary outcomes included WHO Tier 1 or 2 contraception uptake and other health services measures. We conducted bivariable and multivariable analyses.
Results
Of the 225 women approached for Navigating New Motherhood participation after program initiation, 96.9% (N=218) enrolled; these women were compared to 256 women in the historical cohort. Most women on both groups were racial or ethnic minorities and all had Medicaid insurance. There were no important differences in demographic, clinical, or health services characteristics between groups, though women in Navigating New Motherhood were more likely to transfer into the clinic for prenatal care and to deliver babies admitted to the NICU. The primary outcome, return for postpartum care, was more common among women in Navigating New Motherhood (88.1% vs. 70.3%, p<0.001), a difference that persisted after adjustment for potential confounding factors (aOR 3.57, 95% CI 2.11-6.04). Women in Navigating New Motherhood also were more likely to receive a WHO Tier 1 or 2 contraceptive method (aOR 1.56, 95% 1.02-2.38), postpartum depression screening (aOR 2.82, 95% CI 1.79-4.43), and influenza (aOR 2.10, 95% CI 1.38-3.19) and HPV vaccination (aOR 2.33, 95% CI 1.25-4.33).
Conclusions
Implementation of a postpartum navigation program was associated with improved retention in routine postpartum care and frequency of contraception uptake, depression screening, and vaccination.
INTRODUCTION
The postpartum period is a time of rapid and intense change in the life of a mother and her family. Engaging with the health care system during this period enables mothers to receive medical, emotional, and social support from her healthcare team. This support includes management of the mother's chronic comorbid conditions as well as monitoring of pregnancy-specific conditions that have implications for her long-term health.1 Postpartum care also provides access to desired contraception, which allows the mother to plan the timing of her next pregnancy.1,2
The importance of postpartum care has been reinforced by the U.S. Department of Health and Human Services as well as the American College of Obstetricians and Gynecologists.1-3 Nonetheless, postpartum appointment attendance is poor1,4, and substantial disparities in postpartum care uptake exist based on insurance type, race and ethnicity, level of education, age, and socioeconomic status.5-10 Data from the National Committee on Quality Assurance demonstrated that approximately 80% of women with commercial insurance completed a postpartum visit while only 60% of Medicaid enrollees did so.11,12 Further, Hispanic and non-Hispanic black race or ethnicity have been associated with poor postpartum health care utilization.5,8,13,14
Patient navigation has been defined as a barrier-focused, longitudinal, patient-centered intervention that offers services to an individual patient for a defined set of health services.15 Patient navigation includes developing patient-navigator relationships to offer support for patient-level barriers to accessing care for a specific health concern or episode.15,16 Given previous patient navigation successes in initiating and keeping at-risk women connected to healthcare resources16-23, we considered patient navigation to be a promising, patient-centered approach for improving the quality and quantity of postpartum care received by a low-resource population.
Thus, we aimed to develop a postpartum patient navigation program, Navigating New Motherhood, to enhance uptake of postpartum care in a community of low-income, largely minority women. The primary objective was to estimate whether postpartum visit attendance was improved in women exposed to the Navigating New Motherhood intervention compared to those who received care immediately prior to the program's initiation. The secondary objective was to assess other postpartum health behaviors, including receipt of contraception, during the intervention period.
MATERIALS AND METHODS
This is a prospective observational study of women enrolled in a patient navigation program compared to women receiving care prior to the program. Navigating New Motherhood was a patient navigation program initiated within a hospital-based women's health clinic at Northwestern Memorial Hospital, a university tertiary care center located in Chicago, Illinois. This clinic provides care to a diverse population of largely minority women seeking gynecologic and obstetric care; it also serves as a maternal-fetal medicine referral site for women with publicly-funded prenatal care who require subspecialty care during pregnancy. Low-income women in Illinois have universal access to Medicaid assistance for pregnancy, childbirth, and 60 days of postpartum care24, although state- and city-level data suggest many women do not receive adequate routine postpartum care.4,7 Prior to Navigating New Motherhood, women seen in this practice were responsible for calling the clinic to schedule their postpartum visit; clinic staff did not provide appointment reminders, logistical assistance, or other postpartum support on a routine basis.
The patient-centered Navigating New Motherhood program combined best practices as suggested from quality improvement science and research studies to address barriers to postpartum care.1,6,18,25 This program hired one full-time patient navigator who was already experienced navigating low-income women through women's health cancer screening and treatment. The navigator had master's level education and was experienced both in patient navigation and research assistance but was not a health care professional. Training specific to postpartum care was given through one-on-one discussions with clinic nurses, medical assistants, and physicians. The navigator worked with the social worker and breastfeeding support counselor to learn about the services they provide. Through these iterative discussions and shadowing sessions, the navigator integrated herself into the clinic. She introduced herself to patients at their late third-trimester prenatal visits. She surveyed the weekday inpatient postpartum census and approached all eligible participants for recruitment, which was performed during the inpatient hospitalization on or after postpartum day 1. The navigator was not available for recruitment on weekends, evenings or holidays. The navigator met with each eligible new mother in her hospital room to offer support, describe the Navigating New Motherhood program, and enroll interested participants. Participants underwent in-person, face-to-face survey assessments of demographic information, health behaviors, and health priorities and preferences.
At the time of enrollment, the navigator coordinated with clinic staff to schedule the patient's six-week postpartum appointment as well as any earlier visits recommended by the medical team (such as for wound follow-up, blood pressure checks, or mental health assessment1). Appointment times were communicated in person or by phone, text, or email, per patient preference. Reminders were sent by the navigator one week after delivery, one week prior to appointment, and one day prior to the appointment. The navigator offered additional services as needed, including connection to health care providers for maternal or neonatal clinical concerns, psychosocial support, appointment and logistical support, assistance with social work needs (such as identifying food or transportation resources), or connection to mental health care providers. Additionally, during the postpartum hospitalization, the navigator offered brief written and verbal counseling about the benefits of and options for contraception and breastfeeding.
During postpartum appointments, the navigator met with each woman to ensure all questions were answered, to serve as a bridge between patient and clinical care team, to help patients schedule additional appointments, such as for primary care or subspecialists, and to provide resources for primary care facilities that would serve as a medical home. The navigator also coordinated appointments for patients who required follow-up for contraception, such as for permanent contraception procedures or other needs (placement of or follow-up for a contraceptive implant or intrauterine device). If patients did not return for postpartum care, the navigator continued to attempt to contact participants weekly up until 12 weeks postpartum, at which point no further attempts to reschedule the patient were made and the patient was considered lost to follow-up. If the patient was successfully contacted after missing her initial postpartum appointment, the navigator helped reschedule the appointment.
This analysis compared women who received patient navigation in the year after introduction of the Navigating New Motherhood program (May 30, 2015 to May 30, 2016) with those who received care in the year immediately prior to Navigating New Motherhood initiation. Eligibility criteria included delivery of a fetus in the second trimester or later on the labor and delivery unit. Women were included regardless of neonatal survival. Exclusion criteria included being <18 years of age or non-English speaking. Women with HIV were also excluded because they participated in a multidisciplinary perinatal HIV program that included built-in support services. The Institutional Review Board of Northwestern University approved this study, and all participants in Navigating New Motherhood provided written, informed consent; a waiver of consent was authorized for record review-only participants.
Sample size goals were based on clinic administrative data from 2014, which demonstrated a postpartum follow-up rate of 65%. In order to detect a relative 20% increase in postpartum return during the Navigating New Motherhood intervention period with 80% power and an alpha=0.05, 189 women were needed in each arm of the study, for a total of 378 participants. The annual number of deliveries for this clinic was approximately 350. In order to account for ineligibility, fluctuations in clinic volume, and eligible participants who did not enroll, we projected a study duration of one year, and planned a priori to conduct evaluation of Navigating New Motherhood by analyzing outcomes for 12 months prior to and after initiation of the program.
The primary outcome was return to the postpartum visit, which was defined as a return to the clinic by 12 weeks postpartum. To be considered return to postpartum care, the postpartum visits must have included attention to routine postpartum health topics, including contraception, maternal health, infant feeding, mood, and transitions of care. Thus, for example, a one-week blood pressure check without attention to other topics and without subsequent return to care was not considered a postpartum visit. In addition, we did not consider patient self-report of receiving postpartum care at a different site as completion of the postpartum visit for the study purposes due to inability to confirm receipt of care.
Multiple secondary outcomes were assessed. Regarding contraception, we assessed both whether the method initiated was a World Health Organization (WHO) Tier 1 or 2 contraceptive method and whether the method was a long-acting reversible contraceptive (LARC) method.26 WHO Tier 1 included contraceptive implant, intrauterine devices, and permanent contraception (vasectomy, tubal occlusion, or hysterectomy); permanent contraception was only considered completed if already performed by the time of the postpartum visit. WHO Tier 2 methods included combined hormonal contraception (pill, patch, ring), injectable methods, and lactational amenorrhea. Other secondary outcomes assessed included completion of a postpartum 2-hour glucose tolerance test for women with gestational diabetes mellitus27; completion of a postpartum depression screen1; breastfeeding (exclusive or partial) at the postpartum visit; receipt of an influenza vaccine at or by the postpartum visit; and initiation or subsequent dose of human papillomavirus (HPV) vaccination for eligible women.
Maternal demographic and clinical characteristics were compared between the two groups (i.e., women before and after Navigating New Motherhood) using chi-squared and Mann-Whitney U tests, as appropriate. Potential confounders (p<0.05 on bivariable analyses) were then retained in multivariable logistic regression models in order to estimate adjusted odds ratios and 95% confidence intervals for the primary and secondary outcomes. We maintained all data in REDCap (Research Electronic Data Capture, Northwestern University) and utilized Stata v.14 (StataCorp, College Station, TX) for analysis. All tests were two-sided and p<0.05 defined statistical significance.
Finally, we performed a planned secondary analysis of the Navigating New Motherhood cohort year in order to further assess if the findings were due to Navigating New Motherhood versus to other changes in the clinical environment. Thus, we compared differences in baseline characteristics and outcomes of women (age 18 and over) who enrolled in Navigating New Motherhood compared to those who did not enroll after initiation of the program, due to either being missed, declining, or being ineligible for language criteria. The same analytic methods were utilized.
RESULTS
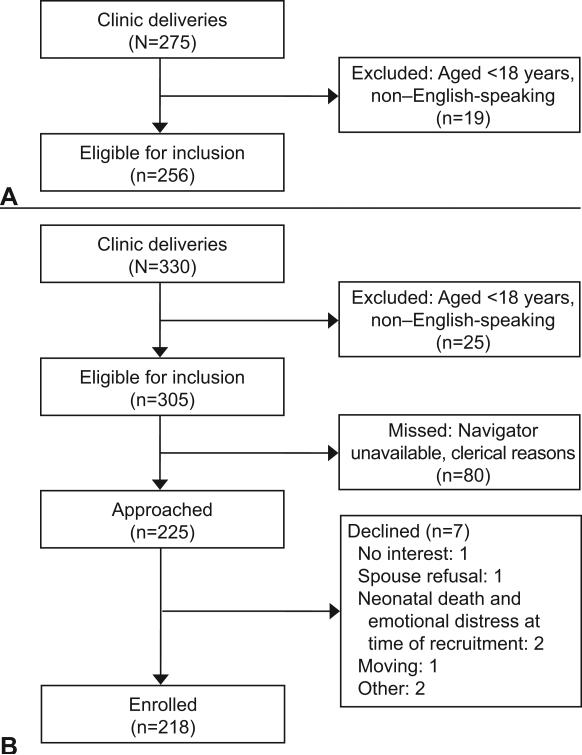
Prior to initiation of Navigating New Motherhood, 275 women delivered who had received prenatal care in this clinic, of whom 93.1% (N=256) would have been eligible for Navigating New Motherhood based on age and language-based inclusion criteria. These 256 women constituted the study group prior to program initiation. After Navigating New Motherhood initiation, 330 women delivered who had received prenatal care in this clinic, of whom 92.4% (N=305) were eligible for inclusion. Of the 225 women (68.2%) who were approached regarding participation, 96.9% agreed to enroll. Thus, the final Navigating New Motherhood cohort constituted 218 enrolled women (Figure 1).
Figure 1.
Participant flow before (A) and after (B) Navigating New Motherhood implementation.
The groups were comparable in maternal age, self-reported race and ethnicity, marital status, gravidity or parity, and number of prenatal visits (Table 1). Women in the Navigating New Motherhood cohort were more likely to have transferred into this clinic for prenatal care (37.3% vs. 15.8%, p<0.001) after initial prenatal care elsewhere, which was due to the expansion of the fetal health program within the co-located children's hospital. Navigating New Motherhood enrollees were also more likely to have asthma (14.7% vs. 8.6%, p=0.04). There were no other differences in maternal clinical history.
Table 1.
Maternal demographic and clinical characteristics prior to and after Navigating New Motherhood
| Prior to Navigating New Motherhood (N=256) | After Navigating New Motherhood (N=218) | p-value | |
|---|---|---|---|
| Age (years) | 29.2 (5.7) | 28.9 (5.1) | 0.56 |
| Race/ethnicity | 0.36 | ||
| Non-Hispanic white | 24 (9.4) | 28 (12.8) | |
| Non-Hispanic black | 133 (52.0) | 108 (49.5) | |
| Hispanic | 83 (32.4) | 71 (32.6) | |
| Asian | 10 (3.9) | 10 (4.6) | |
| Other | 6 (2.3) | 1 (0.5) | |
| Married | 76 (31.3) | 67 (31.0) | 0.95 |
| Gravidity | 3 (2,4) | 3 (2,5) | 0.32 |
| Primiparous | 75 (29.3) | 65 (29.8) | 0.90 |
| Maternal-fetal medicine patient | 86 (33.7) | 81 (37.3) | 0.42 |
| Total number of prenatal visits (excluding transfers of care) | 10.1 (3.2) | 9.4 (3.1) | 0.12 |
| Transfer of antenatal care | 40 (15.8) | 81 (37.2) | <0.001 |
| Asthma | 22 (8.6) | 32 (14.7) | 0.04 |
| Depression | 37 (14.7) | 33 (16.2) | 0.66 |
| Diabetes | 52 (20.3) | 33 (15.1) | 0.14 |
| Intended long-acting reversible contraception uptake | 139 (54.3) | 122 (56.0) | 0.72 |
Data displayed as N(%), mean(SD), or median(IQR).
There were few significant differences in the delivery characteristics of women in the two groups (Table 2). Women exposed to Navigating New Motherhood had a greater frequency of neonates with NICU admission (21.7% vs. 11.6%, p=0.003).
Table 2.
Delivery outcomes prior to and after Navigating New Motherhood
| Prior to Navigating New Motherhood (N=256) | After Navigating New Motherhood (N=218) | p-value | |
|---|---|---|---|
| Gestational age at delivery (weeks) | 38.2 (2.5) | 38.3 (3.1) | 0.25 |
| Mode of delivery | 0.66 | ||
| Spontaneous vaginal delivery | 166 (64.8) | 142 (65.1) | |
| Operative vaginal delivery | 5 (2.0) | 7 (3.2) | |
| Cesarean delivery | 85 (33.2) | 69 (31.7) | |
| Gestational hypertension or preeclampsia | 20 (7.8) | 24 (11.0) | 0.23 |
| Postpartum hemorrhage | 18 (7.0) | 13 (6.0) | 0.64 |
| Blood transfusion | 11 (4.3) | 6 (2.8) | 0.37 |
| Excess hospital length of stay (>2 for vaginal delivery, >4 for cesarean delivery) | 11 (4.3) | 16 (7.3) | 0.16 |
| Postpartum readmission | 6 (2.3) | 6 (2.8) | 0.78 |
| Endometritis | 7 (2.7) | 2 (0.9) | 0.19 |
| Wound complications | 7 (2.7) | 2 (0.9) | 0.19 |
| Neonatal intensive care unit admission | |||
| Overall | 29 (11.6) | 47 (21.7) | 0.003 |
| Excluding transfers of care | 20 (9.5) | 20 (14.7) | 0.14 |
| Neonatal birthweight (grams) | 3213 (591) | 3106 (695) | 0.14 |
Data displayed as N(%) or mean(SD).
The primary outcome, postpartum visit attendance, was significantly more frequent in women in the NNM program (88.1% vs. 70.3%, p<0.001) (Table 3). After adjusting for differences between groups (NICU admission, asthma, and transfer of care), this finding remained statistically significant (aOR 3.57, 95% CI 2.11-6.04). Uptake of a WHO Tier 1 or 2 contraceptive method, receipt of postpartum depression screen, receipt of influenza vaccine, and receipt of HPV vaccination also were improved in the women exposed to Navigating New Motherhood. Each of these findings remained statistically significant on multivariable logistic regression (Table 3). There were no differences in the frequency of completion of a postpartum glucose tolerance test (when indicated) or of continued breastfeeding until the postpartum visit.
Table 3.
Postpartum health services and contraception uptake prior to and after Navigating New Motherhood
| Bivariable analyses | Multivariable analysis | ||||
|---|---|---|---|---|---|
| Prior to Navigating New Motherhood (N=256) | After Navigating New Motherhood (N=218) | p-value | OR (95% CI) | aOR (95% CI)* | |
| Primary outcome | |||||
| Postpartum visit attendance | 180 (70.3) | 192 (88.1) | <0.001 | 3.12 (1.91-5.09) | 3.57 (2.11-6.04) |
| Secondary outcomes | |||||
| WHO Tier 1 or 2 contraception uptake | 167 (65.2) | 161 (73.9) | 0.04 | 1.51 (1.01-2.24) | 1.56 (1.02-2.38) |
| LARC uptake | 83 (33.6) | 88 (40.4) | 0.07 | 1.41 (0.97-2.06) | 1.48 (1.00-2.20) |
| Completion of GTT (if eligible) | 9 (30.0) | 10 (47.6) | 0.20 | 2.12 (0.67-6.76) | 2.79 (0.80-9.70) |
| Received postpartum depression screen | 160 (62.8) | 177 (81.2) | <0.001 | 2.56 (1.68-3.92) | 2.82 (1.79-4.43) |
| Breastfeeding at postpartum visit | 97 (55.8) | 102 (53.4) | 0.65 | 0.91 (0.60-1.37) | 0.94 (0.60-1.45) |
| Received influenza vaccine | 152 (59.8) | 161 (73.9) | 0.001 | 1.90 (1.28-2.81) | 2.10 (1.38-3.19) |
| Received HPV vaccination (if eligible) | 27 (26.5) | 29 (33.3) | 0.01 | 2.29 (1.28-4.11) | 2.33 (1.25-4.33) |
Data displayed as N(%)
aOR, adjusted odds ratio; CI, confidence interval; WHO, World health organization; LARC, long-acting reversible contraception; GTT, glucose tolerance test; HPV, human papillomavirus
Controlling for transfer of care, asthma, and NICU admission
Women who delivered during the intervention period but did not enroll (due to ineligibility by language criteria, declining enrollment, or being missed) were more likely to be Hispanic (46.3% vs. 32.6%, p<0.001), primiparous (57.7% vs. 29.8%, p<0.001), to have transferred prenatal care (49.5% vs. 37.2%, p=0.04), and to have diabetes (24.7% vs. 15.1%, p=0.04). Compared to those who did not participate, Navigating New Motherhood participants demonstrated a significantly increased rate of postpartum visit attendance (88.1% vs. 62.9%, p<0.001), which remained statistically significant when accounting for differences between groups in the multivariable logistic regression model (aOR 5.88, 95% CI 2.98-11.61). Participants also had a statistically significantly greater likelihood of uptake of a WHO Tier 1 or 2 contraceptive method, initiation of a LARC method, receiving a postpartum depression screen, and receiving HPV vaccination (Table 4).
Table 4.
Comparison of primary and secondary outcomes between Navigating New Motherhood participants and non-participants in the intervention year
| Bivariable analyses | Multivariable analysis | ||||
|---|---|---|---|---|---|
| Non-participant (N=97) | Participant (N=218) | p-value | aOR (95% CI)* | ||
| Primary outcome | |||||
| Postpartum visit attendance | 61 (62.9) | 192 (88.1) | <0.001 | 4.36 (2.44-7.79) | 5.88 (2.98-11.61) |
| Secondary outcomes | |||||
| WHO Tier 1 or 2 contraception uptake | 50 (51.6) | 161 (73.9) | <0.001 | 2.67 (1.61-4.38) | 2.80 (1.59-4.93) |
| LARC uptake | 25 (25.8) | 88 (40.4) | 0.01 | 1.95 (1.15-3.31) | 2.25 (1.25-4.05) |
| Completion of GTT (if eligible) | 8 (47.1) | 10 (47.6) | 0.97 | 1.02 (0.28-3.68) | 1.30 (0.28-6.03) |
| Received postpartum depression screen | 55 (56.7) | 177 (81.2) | <0.001 | 3.30 (1.95-5.58) | 6.12 (3.18-11.77) |
| Breastfeeding at postpartum visit | 35 (57.4) | 102 (53.4) | 0.59 | 0.85 (0.48-1.52) | 0.72 (0.37-1.38) |
| Received influenza vaccine | 71 (74.0) | 161 (73.9) | 0.98 | 0.99 (0.58-1.72) | 1.08 (0.59-2.00) |
| Received HPV vaccination (if eligible) | 8 (24.2) | 29 (33.3) | 0.28 | 1.92 (0.85-4.33) | 3.70 (1.31-10.46) |
Data displayed as N(%)
aOR, adjusted odds ratio; CI, confidence interval; WHO, World health organization; LARC, long-acting reversible contraception; GTT, glucose tolerance test; HPV, human papillomavirus
Controlling for maternal race and ethnicity, primiparity, transfer of care, and diabetes
DISCUSSION
Postpartum care represents a critical transition point to evaluate the well-being of mothers, prepare them for optimal long-term health, and leverage increased access to health care into lifelong benefits for the mother and family 1,2,28 One approach to promoting retention in postpartum care is patient navigation. Our data demonstrate that a multifaceted, patient-centered navigation program is significantly associated with improved postpartum retention in care as well as improvements in such postpartum outcomes as contraception uptake, depression screening, and vaccination. This conclusion is buttressed by the secondary analysis in which women who were and were not enrolled in the Navigating New Motherhood program but received care during the same time period were compared. This analysis showed that participants in Navigating New Motherhood were significantly more likely to have better health services outcomes compared to women who did not participate in the program. Such an analysis removes the possibility of an unrelated secular trend accounting for differences observed.
Consistent with other reports, our clinic patients had inadequate receipt of postpartum care prior to Navigating New Motherhood, despite having an established perinatal medical home and 60 days of Illinois Medicaid coverage following delivery.4 The American College of Obstetricians and Gynecologists (the College) has suggested strategies for increasing postpartum care attendance, including prenatal counseling about the importance of postpartum care, assistance of clinical and other support staff, scheduling postpartum visits during prenatal care or the postpartum hospitalization, and use of technology for reminders.1 Navigating New Motherhood combined several of the College-recommended strategies for increasing postpartum care, including face-to-face counseling, early appointment planning, assistance with appointment coordination, and direct clinic-based systems changes. However, Navigating New Motherhood was multifaceted, including both staff and patient logistical support and patient psychosocial support, and thus it is not possible to determine whether the outcomes were due to the entire package of navigator support versus a single component, such as appointment scheduling.
Our findings are comparable to other programs attempting systems-wide change in postpartum health care provision. In the Queen Emma Clinic Postpartum Follow-Up Initiative in Hawaii, postpartum follow-up rates improved from 72% to 86% by scheduling postpartum visits while the woman was hospitalized after birth; breastfeeding at the postpartum visit and contraception uptake also increased.25 In contrast to their program, we also demonstrated improvement in postpartum depression screening and vaccination receipt. Our findings are also consistent with other studies that demonstrated improved postpartum uptake of HPV vaccination after implementation of different health services approaches.20,29
Navigating New Motherhood included several unique, multidisciplinary features to address patient barriers to care. First, acknowledging that reliance on busy clinicians to provide navigation is unrealistic, we designed Navigating New Motherhood to function without physicians performing duties beyond routine clinical care. We believe this feature of the program significantly enhanced its ability to succeed in this busy, urban, teaching hospital. Navigating New Motherhood seamlessly integrated a dedicated patient navigator into clinic staff, thus enhancing the quality of communication when patients had clinical concerns and reducing burdens on patients, staff and clinical providers. Navigating New Motherhood also uniquely sought patient input regarding preferences for communication, such that the majority of communication occurred via text message; this inclusion of patient preferences is likely key to patient acceptance of the program. Consistent with the core processes of patient navigation, Navigating New Motherhood focused heavily on relationship-building, improved patient-provider communication and instrumental interventions for barrier reduction.16 Further, the diverse cohort of patients with a variety of medical needs, antepartum experiences, and delivery outcomes enhances generalizability of the findings. Finally, a unique strength of this study is its goal of supporting a lower resourced population. Achieving women's health equity requires focused attention to individuals and communities for whom health inequities are the greatest. As such, programs like Navigating New Motherhood that are designed to promote health equity via caring for those at greatest risk of failed postpartum follow-up will be needed to achieve the Healthy People 2020 goal of an increase in number of women who attend a postpartum visit.3
However, there were several limitations to consider. This study was performed at a single, large academic tertiary care medical center. Not only is this center a referral site for higher-level obstetric and neonatal care, which changes the complexity of patients referred to this practice, but it also has the benefit of resources such as a social worker and breastfeeding counselor. The results may thus not be fully generalizable to community clinic settings; however, the presence of other pre-existing resources in this clinic would only bias the findings toward the null. Second, we focused on English-speaking patients due to limitations of navigation staff; future work will need to include Spanish and other languages to assess whether these outcomes are also observed in other groups. Such work could also address whether patient-navigator native language as well as racial and ethnic concordance could benefit the patient-navigator relationship. Additionally, the navigator was a single individual, and thus we were unable to provide 100% coverage for all eligible patients. Further, this study was not a randomized trial, but instead was planned as a comparison between the Navigating New Motherhood enrollees and historical cohort; thus, there may be selection bias in the cohort enrolled in Navigating New Motherhood. Future investigation of postpartum patient navigation via randomized trial methodology will be important to addressing potential unmeasured confounders.
Lastly, Navigating New Motherhood was a labor-intensive program, requiring grant support for a full-time, trained patient navigator. A cost analysis was outside of the scope of this study, but merits future investigation. As patient navigator has yet to be a recognized job classification within perinatal clinical care teams, future work may consider how the navigator's tasks could be incorporated into existing clinic staff to enhance program sustainability. Patient navigators across the nation are largely funded through grants or other philanthropic efforts, and thus, whether postpartum navigation is cost effective requires evaluation.
In summary, Navigating New Motherhood was associated with substantial improvements in postpartum care receipt as well as other postpartum health care delivery markers. Patient navigation in perinatal healthcare settings may be an important strategy to promoting women's health equity.
Acknowledgments
Supported by the Northwestern Memorial Foundation / Friends of Prentice FY2015 Grants Initiative. Lynn M. Yee is supported by the NICHD K12 HD050121-11.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has indicated that he or she has met the journal's requirements for authorship.
Presented as a poster at the Society for Maternal-Fetal Medicine 37th Annual Meeting, in Las Vegas, Nevada, on January 23-28, 2017.
REFERENCES
- 1.American College of Obstetricians and Gynecologists' Committee on Obstetric Practice Optimizing Postpartum Care, Committee Opinion No. 666. Obstetrics and Gynecology. 2016;127:e187–92. doi: 10.1097/AOG.0000000000001487. [DOI] [PubMed] [Google Scholar]
- 2.ACOG . In: Guidelines for Perinatal Care. 7th ed. ACOG, editor. Washington, DC: Oct, 2012. [Google Scholar]
- 3. [October 27, 2016];Healthy People 2020: Postpartum health and behavior. 2016 at www.healthypeople.gov/2020/topics-objectives/objective/mich-19.
- 4.Harney C, Dude A, Haider S. Factors associated with short interpregnancy interval in women who plan postpartum LARC: a retrospective study. Contraception. 2016 doi: 10.1016/j.contraception.2016.08.012. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Bennett W, Chang H, Levine D, et al. Utilization of primary and obstetric care after medically complicated pregnancies: an analysis of medical claims data. Journal of General Internal Medicine. 2014;29:636–45. doi: 10.1007/s11606-013-2744-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bryant A, Haas J, McElrath T, McCormick M. Predictors of compliance with the postpartum visit among women living in Healthy Start project areas. Maternal and Child Health Journal. 2006;10:511–6. doi: 10.1007/s10995-006-0128-5. [DOI] [PubMed] [Google Scholar]
- 7.Rankin K, Haider S, Caskey R, Chakraborty A, Roesch P, Handler A. Healthcare utilization in the postpartum period among Illinois women with Medicaid paid claims for delivery, 2009-2010. Maternal and Child Health Journal. 2016 doi: 10.1007/s10995-016-2043-8. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilcox A, Levi E, Garrett J. Predictors of non-attendance to the postpartum follow-up visit. Maternal and Child Health Journal. 2016 doi: 10.1007/s10995-016-2184-9. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Lu M, Prentice J. The postpartum visit: Risk factors for nonuse and association with breastfeeding. American Journal of Obstetrics and Gynecology. 2002;187:1329–36. doi: 10.1067/mob.2002.126848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiBari J, Yu S, Chao S, Lu M. Use of postpartum care: Predictors and barriers. Journal of Pregnancy. 2014;530769:1–8. doi: 10.1155/2014/530769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Committee on Quality Assurance . Improving Quality and Patient Experience: The State of Health Care Quality 2013. National Committee for Quality Assurance; Washington, DC: 2013. [Google Scholar]
- 12.National Committee on Quality Assurance . Continuous Improvement and the Expansion of Quality Measurement: The State of Health Care Quality 2011. National Committee for Quality Assurance; Washington, DC: 2011. [Google Scholar]
- 13.Bromley E, Nunes A, Phipps M. Disparities in pregnancy healthcare utilization between Hispanic and non-Hispanic white women in Rhode Island. Maternal and Child Health Journal. 2012;16:1576–82. doi: 10.1007/s10995-011-0850-5. [DOI] [PubMed] [Google Scholar]
- 14.Levine L, Nkonde-Price C, Limaye M, Srinivas S. Factors associated with postpartum follow-up and persistent hypertension among women with severe preeclampsia. Journal of Perinatology. 2016 doi: 10.1038/jp.2016.137. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wells K, Battaglia T, Dudley D, et al. Patient navigation: State of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jean-Pierre P, Hendren S, Fiscella K, et al. Understanding the processes of patient navigation to reduce disparities in cancer care: perspectives of trained navigators from the field. Journal of Cancer Education. 2011;26:111–20. doi: 10.1007/s13187-010-0122-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paskett E, Dudley D, Young G, et al. Impact of patient navigation interventions on timely diagnostic follow up for abnormal cervical screening. Journal of Women's Health. 2016;25:15–21. doi: 10.1089/jwh.2014.5094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Battaglia T, Darnell J, Ko N, et al. The impact of patient navigation on the delivery of diagnostic breast cancer care in the National Patient Navigation Research Program: a prospective meta-analysis. Breast Cancer Research and Treatment. 2016;158:523–34. doi: 10.1007/s10549-016-3887-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodday A, Parsons S, Snyder F, et al. Impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121:4025–34. doi: 10.1002/cncr.29612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berenson A, Rahman M, Hirth J, Rupp R, Sarpong K. A human papillomavirus vaccination program for low-income postpartum women. American Journal of Obstetrics and Gynecology. 2016;215:318.e1–9. doi: 10.1016/j.ajog.2016.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips C, Rothstein J, Beaver K, Sherman B, Freund K, Battaglia T. Patient navigation to increase mammography screening among inner city women. Journal of General Internal Medicine. 2011;26:123–9. doi: 10.1007/s11606-010-1527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Battaglia T, Bak S, Heeren T, et al. Boston Patient Navigation Research Program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiology, Biomarkers and Prevention. 2012;21:1645–54. doi: 10.1158/1055-9965.EPI-12-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffman H, LaVerda N, Young H, et al. Patient navigation significantly reduces delays in breast cancer diagnosis in the District of Columbia. Cancer Epidemiology, Biomarkers and Prevention. 2012;21:1655–63. doi: 10.1158/1055-9965.EPI-12-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. [October 27, 2016];Women and Medicaid in Illinois. 2010 (at www.nwlc.org/sites/default/files/pdfs/illinois.medicaid_1.pdf.)
- 25.Tsai P, Nakashima L, Yamamoto J, Ngo L, Kaneshiro B. Postpartum follow-up rates before and after the postpartum follow-up initiative at Queen Emma Clinic. Hawaii Medical Journal. 2011;70:56–9. [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization Department of Reproductive Health and Research and Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs Knowledge for Health Project. Family Planning: A Global Handbook for Providers (2011 Update) CCP and WHO; Baltimore and Geneva: 2011. [Google Scholar]
- 27.American College of Obstetricians and Gynecologists Practice Bulletin No. 137: Gestational Diabetes Mellitus. Obstetrics and Gynecology. 2013;122:406–16. doi: 10.1097/01.AOG.0000433006.09219.f1. [DOI] [PubMed] [Google Scholar]
- 28. [October 27, 2016];SMFM White Paper: Pregnancy as a Window to Future Health. 2015 (at www.smfm.org/publications/141-smfm-white-paper-pregnancy-as-a-window-to-future-health.)
- 29.Soon R, Sung S, Cruz M, Chen J, Hiraoka M. Improving Human Papillomavirus (HPV) vaccination in the postpartum setting. Journal of Community Health. 2016 doi: 10.1007/s10900-016-0230-6. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]