Abstract
Objective
To estimate the association between state Medicaid coverage of medically necessary abortion and severe maternal morbidity and in-hospital maternal mortality in the U.S.
Methods
We used data on pregnancy-related hospitalizations from the Nationwide Inpatient Sample from 2000 to 2011 (weighted n=38,016,845). State-level Medicaid coverage of medically necessary abortion for each year was determined from Guttmacher Institute reports. We used multivariable logistic regression to examine the association between state Medicaid coverage of abortion and severe maternal morbidity and in-hospital maternal mortality, overall and stratified by payer.
Results
The unadjusted rate of severe maternal morbidity was lower among Medicaid-paid hospitalizations in states with Medicaid coverage of medically necessary abortion, relative to those in states without such coverage (62.4 vs. 69.3 per 10,000). Among Medicaid-paid hospitalizations in states with Medicaid coverage of medically necessary abortion, there were 8.5 per 10,000 fewer cases (95% CI 4.0,16.5) of severe maternal morbidity in adjusted analyses, relative to those in states without such Medicaid coverage. Similarly, there were 10.3 per 10,000 fewer cases (95% CI 3.5,17.2) of severe maternal morbidity in adjusted analyses among private insurance-paid hospitalizations in states with Medicaid coverage of medically necessary abortion, relative to those in states without such Medicaid coverage. The adjusted rate of in-hospital maternal mortality was not different for Medicaid-paid hospitalizations in states with and without Medicaid coverage of medically necessary abortion (9.2 and 9.0 per 100,000, respectively), nor for private-insurance paid hospitalizations (5.6 and 6.1 per 100,000, respectively).
Conclusions
State Medicaid coverage of medically necessary abortion was associated with an average 16% decreased risk of severe maternal morbidity. An association between state Medicaid coverage of medically necessary abortion and a reduced risk of severe maternal morbidity was observed in women covered by both Medicaid and private insurance. Results suggest that Medicaid coverage of medically necessary abortion is not harmful to maternal health.
INTRODUCTION
Severe maternal morbidity and maternal mortality in the U.S. are on the rise.1,2 Access to induced abortion may reduce these risks in some populations. 3 Recent research suggests that both unintended pregnancy and chronic health conditions are risk factors for maternal morbidity.4 Women with unintended pregnancies might develop significa nt health problems as a consequence of not seeking out and engaging with adequate prenatal care. 5
Further, women who begin pregnancies with pre-existing medical conditions and who lack access to medically necessary abortion may go on to have severe maternal morbidity or mortality.6
In the U.S., however, access to induced abortion is not universal. Under the policy known as the Hyde Amendment, federal funding cannot be spent on abortion except in cases of life endangerment, rape, or incest. This policy may have a major impact on pregnant women who receive Medicaid, the joint state-federal program which is the largest single payer for perinatal care.7 Thirty-three states and Washington, DC provide no Medicaid coverage of induced abortion. In 17 states, Medicaid programs choose to provide coverage of medically necessary abortion using state-only funding.8
Our objective was to estimate the association between state Medicaid programs’ coverage of medically necessary abortions and in-hospital maternal mortality and hospitalizations for severe maternal morbidity among U.S. women from 2000–2011. We expected that state Medicaid programs’ coverage of medically necessary abortions should reduce severe maternal morbidity and mortality through improved access to safe abortions for women who would otherwise experience unwanted or high-risk pregnancies. We therefore hypothesized that women who had pregnancy-related hospitalizations in states with Medicaid coverage of medically necessary abortions would have significantly lower risks of severe maternal morbidity and in-hospital maternal mortality, relative to those women had hospitalizations in states without such policies.
MATERIALS AND METHODS
We obtained a large, nationally-representative sample of hospital discharge data from Nationwide Inpatient Sample (NIS) from 2000–2011 via the Healthcare Cost and Utilization Project (HCUP) administered by the Agency for Healthcare Research and Quality.9 After 2011, the NIS changes its sampling strategy and no longer included indicators of which states hospitalizations occurred in; therefore, we include only data through 2011. These data represent the largest source of all-payer administrative data in the United States, and contain uniform data elements from nearly all U.S. states on diagnosis and procedure codes, diagnosis related groups, severity and comorbidities, patient characteristics, and hospital characteristics.
We used ICD-9-CM diagnosis and procedure codes and Diagnosis Related Group (DRG) codes to hierarchically identify delivery, antenatal, and postpartum hospitalizations for women ages <15 years or >44 years in 47 states with data available in any year from 2000–2011 (unweighted n= 10,131,942 hospitalizations).10–12 We excluded cases with missing information on the payer for the hospitalization (unweighted n=18,473; <1% of cases),, and hospitalizations with missing data on mortality (unweighted n=2,102; <1% of cases). For some states and years, data on patient race were not reported for administrative reasons (e.g., state hospital discharge data collection systems did not capture race or less populous states chose not to report race to protect patient privacy). Because maternal race is an important predictor of severe maternal morbidity and mortality and is associated with state of residence, it is critical to control for patient race in our analyses. Following previous research, we chose to exclude data from states and years where race was not reported.13 This resulted in excluding data for 22% (unweighted n=2,282,556) of pregnancy-related hospitalizations in our study. However, because race data are missing for administrative reasons, missingness should not be associated with state Medicaid policy status nor outcomes, and we do not expect this exclusion to introduce selection bias. Our analytic sample included data from 43 states on 7,828,811 pregnancy-related hospitalizations.
The main exposure was state Medicaid coverage of medically necessary abortions. Although all state Medicaid programs cover abortion in the cases of life endangerment, rape, or incest, medically necessary abortions are defined as those needed to protect a woman’s health. Medically necessary abortion was defined by the US Supreme Court in as a professional judgment made by a physician “exercised in the light of all factors - physical, emotional, psychological, familial, and the woman’s age - relevant to the wellbeing of the patient.”14 We used data collected by the Guttmacher Institute for each state and year indicating that 17 state Medicaid programs provided optional coverage of medically necessary abortions using state-only funding during the study time period.8. Coverage of medically necessary abortion was constant in all states across our study time period. Because we cannot measure state-level differences in Medicaid policy implementation, our results should be interpreted as the average of heterogeneous associations between Medicaid policies and outcomes.
We used the definitions published by the Centers for Disease Control and Prevention to identify severe maternal morbidity among pregnancy related hospitalizations (Table 1).15 There is no single definition of severe maternal morbidity, and hospital discharge data may make it difficult to differentiate variability within diagnoses that might constitute severe maternal morbidity.16 Specifically, we used ICD-9-CM codes for each hospital discharge to identify the presence of any of 24 indicator conditions for severe maternal morbidity. We excluded blood transfusion from our definition of severe maternal morbidity because it is far more common than other morbidities and is collinear with other morbidities. We created a binary measure having any severe maternal morbidity during a hospitalization.
Table 1.
Indicators of severe maternal morbidity and related diagnosis and procedure codes
| Severe Maternal Morbidity | ICD-9-CM Code(s) |
|---|---|
| Diagnosis Codes | |
| Acute myocardial infarction | 410.xx |
| Acute renal failure | 584.x, 669.3x |
| Adult respiratory distress syndrome | 518.5, 518.81, 518.82, 518.84,799.1 |
| Amniotic fluid embolism | 673.1x |
| Aneurysm | 441.xx |
| Cardiac arrest or ventricular fibrillation | 427.41, 427.42, 427.5 |
| Disseminated intravascular coagulation | 286.6, 286.9, 666.3x |
| Eclampsia | 642.6x |
| Heart failure during procedure or surgery | 669.4x, 997.1 |
| Internal injuries of thorax, abdomen, and pelvis | 860.xx–869.xx |
| Intracranial injuries | 800.xx, 801.xx, 803.xx, 804.xx, 851.xx–854.xx |
| Puerperal cerebrovascular disorders | 430, 431, 432.x, 433.xx, 434.xx, 436, 437.x, 671.5x, 674.0x, 997.2, 999.2 |
| Pulmonary edema | 428.1, 518.4 |
| Severe anesthesia complications | 668.0x, 668.1x, 668.2x |
| Sepsis | 038.xx, 995.91, 995.92 |
| Shock | 669.1x, 785.5x, 995.0, 995.4, 998.0 |
| Sickle cell anemia with crisis | 282.62, 282.64, 282.69 |
| Thrombotic embolism | 415.1x, 673.0x, 673.2x, 673.3x, 673.8x |
| Procedure codes | |
| Cardio monitoring | 89.6x |
| Conversion of cardiac rhythm | 99.6x |
| Hysterectomy | 68.3x–68.9 |
| Operations on heart and pericardium | 35.xx, 36.xx, 37.xx, 39.xx |
| Temporary tracheostomy | 31.1 |
| Ventilation | 93.90, 96.01–96.05, 96.7x |
Note: Includes all diagnoses and procedures identified by the Centers for Disease Control and Prevention as indicating severe maternal morbidity during hospitalizations, except blood transfusion.
In-hospital maternal mortality was based on a variable indicating whether or a not a patient was discharged alive. If a hospital discharge for a pregnancy-related hospitalization had a value indicating that the patient died in the hospital, it was considered a maternal death.
We used measures of whether each patient was covered by Medicaid vs. other type of insurance (private insurance, self-pay, charity, or other insurance such as Medicare or military health plans). We also included a categorical measure of maternal race and ethnicity, defined as non-Hispanic white, non-Hispanic black, non-Hispanic Asian or Pacific Islander, non-Hispanic other race, or Hispanic ethnicity. We created a restricted cubic spline for maternal age at the time of hospitalization. We included a state-level measure of the annual proportion of adult obesity, based on state-representative population survey data published by the Centers for Disease Control and Prevention,17 to account for the correlation between state obesity rates and both health care policy and adverse maternal outcomes. We used a measure of obesity for all adults because state-representative data on obesity in pregnancy is not available for all states or all years in our study.
The unit of analysis was each hospitalization. We calculated weighted descriptive statistics of the study population, overall and stratified by whether or not hospitalizations occurred in states with optional Medicaid coverage of medically necessary abortions. We used logistic regression to first assess whether state Medicaid coverage of medically necessary abortions was associated with the risk of severe maternal morbidity. Next, we extended the model to include women’s individual Medicaid enrollment status, with an interaction term between the state Medicaid abortion policy and Medicaid enrollment status. This allowed us to determine if the policy had different effects on risks between women with Medicaid coverage (among whom we would expect the policy to decrease the risk of mortality and severe maternal morbidity) and women with private insurance coverage (among whom we would expect weaker or no effects). From the regression results, we calculated the average predicted risks and 95% confidence intervals of severe maternal morbidity among women with Medicaid and private insurance coverage, with hospitalizations occurring in states with and without Medicaid coverage of medically necessary abortion. We repeated the analyses with maternal mortality as the outcome. Per the STROBE Statement (Strengthening the Reporting of Observational Studies in Epidemiology), statistical testing is conducted only for hypothesis tests and is not presented for descriptive data.18 All analysis used Stata’s SVY commands to account for the complex sampling methodology of the NIS data.
We conducted an a priori sensitivity analyses to examine the robustness of our results. Our primary analyses defined severe maternal morbidity as the presence of a diagnosis of one of 24 conditions during hospitalization, regardless of length of stay for the hospitalization. Prior research has required a long hospital stay as a condition to define severe maternal morbidity for delivery hospitalizations, as conditions may be over-recorded in hospital discharge data.1 We replicated our main analyses restricting severe maternal morbidity as hospitalizations for which length of stay was in the top 50th percentile for vaginal or Cesarean delivery, and during which women did not die during the hospitalization (all antenatal and postpartum hospitalizations were included).
The University of Pittsburgh Institutional Review Board determined that this study was exempt because it involved only the analysis of de-identified hospital discharge data.
RESULTS
In our NIS sample of 43 states across 12 years, 42.7% of pregnancy-related hospitalizations occurred in states with Medicaid coverage of medically necessary abortions (Table 2). Our study included a weighted 38,016,957 pregnancy-related hospitalizations, 41% of which were paid for by Medicaid. In comparison, there were 45,043,714 births in the U.S. over that time period,19 an estimated 45% of which were paid for by Medicaid.7 Relative to hospitalizations occurring in states without Medicaid coverage of medically necessary abortion, hospitalizations occurring in states with Medicaid coverage of medically necessary abortion tended have slightly older patients (mean age 29 years vs. 27 years) and had considerably more racial diversity (54% non-white patients vs. 43% non-white patients) (Table 3). Hospitalizations occurring in states with Medicaid coverage of medically necessary abortion were less likely than their counterparts to be paid for by Medicaid (38% vs. 44%).
Table 2.
State Medicaid coverage of medically necessary abortion in 43 states, 2000–2011
| Medicaid coverage of medically necessary abortion | States | Weighted No. of pregnancy-related hospitalizations |
|---|---|---|
| Yes | Alaska, Arizona, California, Connecticut, Hawaii, Illinois, Massachusetts, Maryland, Montana, New Jersey, New Mexico, New York, Oregon, Vermont, Washington | 5,858,953 |
| No | Arkansas, Colorado, Florida, Georgia, Iowa,a Indiana, Kansas, Kentucky, Louisiana Maine, Michigan, Missouri, Mississippi, Montana, North Carolina, Nebraska, New Hampshire, New Mexico, Nevada, Oklahoma, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, Wyoming | 9,848,834 |
Although Iowa Medicaid may cover medically necessary abortions, the governor must individually approve any abortion paid for by Medicaid.
Note: Minnesota, North Dakota, Ohio, and West Virginia are not included because these states do not report data on patient race. Alabama, Delaware, and Idaho are not included because no data were available in the National Inpatient Sample from 2000–2011.
Table 3.
Weighted descriptive characteristics of pregnancy-related hospitalizations in 43 states from 2000–2011, overall and stratified by state Medicaid coverage of medically necessary abortion
| Overall | State with Coverage of Medically Necessary Abortion | State without Coverage of Medically Necessary Abortion | |
|---|---|---|---|
| Mean maternal age, years (SE) | 27.6 (0.06) | 28.5 (0.11) | 26.9 (0.07) |
| Race, n (%) | |||
| White | 4,098,830 (52.6) | 1,522,883 (46.1) | 2,575,947 (57.4) |
| Black | 1,040,550 (13.3) | 331,451 (10.0) | 709,099 (15.7) |
| Hispanic | 1,880,081 (23.8) | 1,006,088 (29.9) | 873,933 (19.2) |
| Asian or Pacific Islander or American Indian | 436,961 (5.5) | 603,093 (9.1) | 130,868 (2.9) |
| Multiple or Other | 372,366 (4.8) | 155,383 (4.8) | 216,983 (4.8) |
| Payer for hospitalization, n (%) | |||
| Medicaid | 3,238,472 (41.3) | 1,280,333 (38.4) | 1,958,139 (43.5) |
| Other payera | 4,590,316 (58.7) | 2,041,565 (61.6) | 2,548,751 (56.5) |
| Type of hospitalization, n (%) | |||
| Delivery hospitalization | 7,699,983 (98.4) | 3,272,012 (98.6) | 4,427,971 (98.2) |
| Antenatal hospitalization | 122,667 (1.6) | 47,229 (1.4) | 75,438 (1.7) |
| Postpartum hospitalization | 6,138 (<1) | 2,657 (<1) | 3,481 (<1) |
| State level characteristics | |||
| Mean proportion of obese adultsb (SE) | 23.5 (0.09) | 21.8 (0.11) | 24.7 (0.14) |
| Medicaid coverage of medically necessary abortion, n (%) | 3,321,898 (42.7) | 3,321,898 (100) | 0 (0) |
Notes: Unweighted Ns and weighted proportions and means shown. States with Medicaid coverage of medically necessary abortion are: AK, CA, CT, HI, IL MA, MD, MT, NJ, NM, NY, OR, VT. States without Medicaid coverage of medically necessary abortion are: AR, AZ, CO, FL, GA, IA, IN, KS, KY, LA, ME, MI, MO, MS, NC, NE, NH, NV, OK, PA, RI, SC, SD, TN, TX, UT, VA, WI, WY.
Other payers include private insurance, Medicare, other public, charity care, or self-pay
Based on data from the Behavioral Risk Factor Surveillance System in each state and year
Among women with Medicaid-paid hospitalizations, the unadjusted rate of severe maternal morbidity was 66.6 per 10,000 pregnancy-related hospitalizations; this rate was lower for hospitalizations occurring in states with Medicaid coverage of medically necessary abortion relative to those occurring in states without Medicaid coverage (62.4 per 10,000 vs. 69.3 per 10,000) (Table 4). The rates of the five most frequently occurring severe maternal morbidities among women with Medicaid (disseminated intravascular coagulation, heart failure during procedure, eclampsia, adult respiratory distress syndrome, and acute renal failure) were lower among hospitalizations in states with Medicaid coverage of medically necessary abortion, relative to hospitalizations in states without such coverage.
Table 4.
Weighted rates of severe maternal morbidity and mortality among Medicaid-paid pregnancy-related hospitalizations in 43 states from 2000–2011, overall and stratified by state Medicaid coverage of medically necessary abortion
| Severe maternal morbidity | Overall | State with Coverage of Medically Necessary Abortion | State without Coverage of Medically Necessary Abortion | |||
|---|---|---|---|---|---|---|
| Weighted n | rate per 10,000 (95% CI) | Weighted n | rate per 10,000 (95% CI) | Weighted n | rate per 10,000 (95% CI) | |
| Diagnosis Codes | ||||||
| Disseminated intravascular coagulation | 30,670 | 19.5 (18.0,21.0) | 10,859 | 17.4 (15.9,18.7) | 19,811 | 20.9 (18.7,23.2) |
| Heart failure during procedure or surgery | 29,178 | 18.6 (16.9,20.2) | 11,004 | 17.6 (15.9,19.3) | 18,174 | 19.2 (16.8,21.6) |
| Eclampsia | 16,262 | 10.4 (9.7,11.0) | 5,749 | 9.2 (8.5,9.9) | 10,513 | 11.1 (10.1,12.1) |
| Adult respiratory distress syndrome | 10,235 | 6.5 (6.1,6.9) | 3,661 | 5.9 (5.3,6.4) | 6,574 | 6.9 (6.4,7.5) |
| Acute renal failure | 6,829 | 4.3 (4.0,4.7) | 2,613 | 4.2 (3.7,4.7) | 4,216 | 4.5 (4.0,4.9) |
| Sepsis | 5,870 | 3.7 (3.5,4.0) | 2,400 | 3.8 (3.5,4.2) | 3,470 | 3.7 (3.3,4.0) |
| Puerperal cardiovascular disorders | 4,928 | 3.1 (2.9,3.4) | 2,014 | 3.2 (2.9,3.6) | 2,914 | 3.1 (2.7,3.4) |
| Shock | 4,623 | 2.9 (2.7,3.2) | 2,066 | 3.3 (2.9,3.7) | 2,557 | 2.7 (2.4,3.0) |
| Severe anesthesia complications | 2,985 | 1.9 (1.7,2.0) | 1,308 | 2.1 (1.8,2.4) | 1,677 | 1.8 (1.6,1.9) |
| Thrombotic embolism | 2,951 | 1.9 (1.7,2.1) | 1,156 | 1.9 (1.6,2.2) | 1,795 | 1.9 (1.6,2.1) |
| Pulmonary edema | 2,659 | 1.7 (1.4,2.0) | 1,023 | 1.6 (1.1,2.2) | 1,636 | 1.7 (1.5,1.9) |
| Sickle cell anemia with crisis | 2,145 | 1.4 (1.1,1.6) | 756 | 1.2 (0.9,1.5) | 1,389 | 1.5 (1.1,1.9) |
| Internal injuries of thorax, abdomen, and pelvis | 1,405 | 0.9 (0.7,1.0) | 445 | 0.7 (0.5,0.9) | 960 | 1.0 (0.8,1.2) |
| Cardiac arrest or ventricular fibrillation | 1,164 | 0.7 (0.6,0.8) | 401 | 0.6 (0.5,.07) | 763 | 0.8 (0.7,0.9) |
| Amniotic fluid embolism | 668 | 0.4 (0.4,0.5) | 281 | 0.5 (0.3,0.6) | 387 | 0.4 (0.3,0.5) |
| Acute myocardial infarction | 373 | 0.2 (0.2,0.3) | 169 | 0.3 (0.2,0.4) | 204 | 0.2 (0.1,0.3) |
| Aneurysm | 210 | 0.1 (0.01,0.2) | 81 | 0.1 (0.01,0.2) | 129 | 0.1 (0.01,0.2) |
| Intracranial injuries | 211 | 0.1 (0.01,0.2) | 45 | 0.1 (0.01,0.1) | 166 | 0.2 (0.01,0.2) |
| Procedure Codes | ||||||
| Hysterectomy | 11,986 | 7.7 (7.1,8.2) | 4,942 | 7.9 (7.0,8.8) | 7,044 | 7.4 (6.6,8.2) |
| Ventilation | 11,030 | 7.0 (6.6,7.4) | 4,483 | 7.2 (6.6,7.8) | 6,546 | 6.9 (6.4,7.5) |
| Operations on heart and pericardium | 10,322 | 6.6 (6.1,7.1) | 3,664 | 5.9 (5.2,6.5) | 6,658 | 7.0 (6.5,7.7) |
| Cardio monitoring | 7,549 | 4.8 (1.4,8.2) | 4,321 | 6.9 (1.7,12.1) | 3,228 | 3.4 (1.0,7.8) |
| Conversion of cardiac rhythm | 1,169 | 0.7 (0.6,0.8) | 519 | 0.8 (0.7,1.0) | 650 | 0.7 (0.5,0.8) |
| Temporary tracheostomy | 409 | 0.2 (0.2,0.2) | 120 | 0.2 (0.1,0.2) | 289 | 0.3 (0.2,0.4) |
| Any severe maternal morbidity | 104,550 | 66.6 (62.3,70.8) | 38,902 | 62.4 (56.7,68.0) | 65,648 | 69.3 (63.4,75.2) |
| In-hospital mortality | 1,423 | 0.9 (0.8,1.0) | 584 | 0.9 (0.8,1.0) | 839 | 0.9 (0.7,1.0) |
| Any morbidity or mortality | 105,260 | 67.0 (62.8,71.2) | 39,228 | 62.9 (57.2,68.6) | 66,033 | 69.7 (63.8,75.6) |
Notes: Severe maternal morbidity defined by the presence of ICD-9-CM diagnosis or procedure codes recorded in the hospitalization record. States with Medicaid coverage of medically necessary abortion are: AK, CA, CT, HI, IL MA, MD, MT, NJ, NM, NY, OR, VT. States without Medicaid coverage of medically necessary abortion are: AR, AZ, CO, FL, GA, IA, IN, KS, KY, LA, ME, MI, MO, MS, NC, NE, NH, NV, OK, PA, RI, SC, SD, TN, TX, UT, VA, WI, WY.
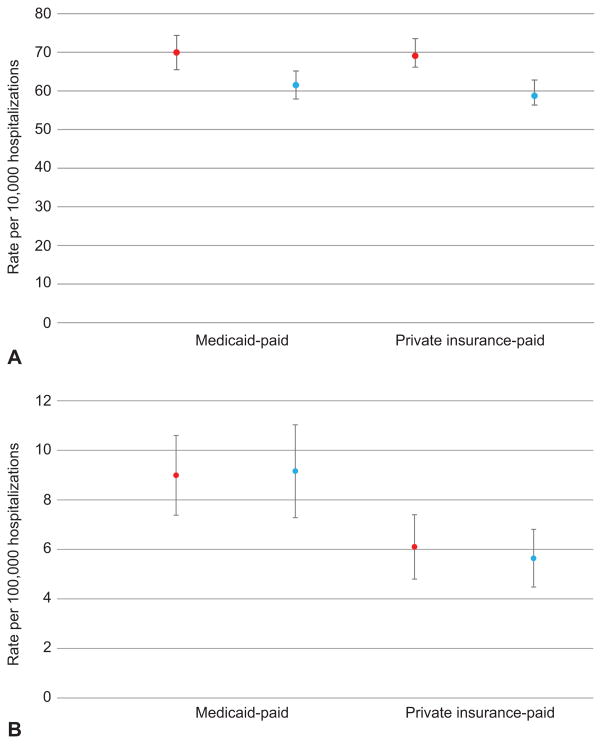
Figure 1 shows the adjusted risks of severe maternal morbidity and maternal mortality, by state Medicaid coverage of medically necessary abortion and stratified by whether or not Medicaid paid for the hospitalization. After stratifying on payer at hospitalization, we found that among hospitalizations paid by Medicaid, those occurring in states providing Medicaid coverage of medically necessary abortion had 8.5 per 10,000 (95% CI 4.0,16.5 per 10,000) fewer cases of severe maternal morbidity (61.5 per 10,000, 95% CI 56.1,65.1) than those occurring in states without such coverage (70.0 per 10,000, 95% CI 65.1,75.8). Likewise, among private insurance-paid hospitalizations, there were 10.3 per 10,000 (95% CI 3.5,17.2 per 10,000) fewer cases of severe maternal morbidity in states with Medicaid coverage of medically necessary abortion (58.7 per 10,000, 95% CI 53.4,64.0) relative to those in states without such coverage (69.1 per 10,000, 95% CI 64.8,73.3). Results did not meaningfully differ in magnitude or direction when we varied the definition of severe maternal morbidity based on length of hospital stay, among women who did not die, in our sensitivity analysis. Across both Medicaid and private paid hospitalizations, state Medicaid coverage of medically necessary abortion was associated with an adjusted average of 9.5 per 10,000 fewer cases of severe maternal morbidity, which translates to an average 16% risk reduction.
Figure 1.
Average predicted risk of severe maternal morbidity (A) and in-hospital maternal mortality (B) among hospitalizations in states with and without Medicaid coverage of medically necessary abortion, according to whether the hospitalization was paid by Medicaid or private insurance. Hospitalizations occurring in states with Medicaid coverage of medically necessary abortion had a statistically significant risk reduction of an average of 9.5 cases of severe maternal morbidity per 10,000 (95% confidence interval [CI]: 3.0–16.0; P=.004). Red dots indicate hospitalizations in states without Medicaid coverage of medically necessary abortion; blue dots indicate hospitalizations in states with Medicaid coverage of medically necessary abortion. Average predicted risks derived from weighted logistic regression models adjusting for race, age, payer for the hospitalization (Medicaid compared with private insurance), mean state body mass index among adults, and year.
Among women with Medicaid, the unadjusted rate of in-hospital mortality was 9.1 per 100,000 pregnancy-related hospitalizations, which did not differ significantly by state Medicaid abortion coverage status (Table 4). The average predicted risk of in-hospital maternal mortality was not different among Medicaid-paid hospitalizations in states with (9.2 per 100,000, 95% CI 7.3,11.0) or without (9.0 per 100,000, 95% CI 7.4,10.6) Medicaid coverage of medically necessary abortion. Likewise, there was no significant difference in in-hospital mortality among private insurance-paid hospitalizations in states with (5.6 per 100,000, 95% CI 4.5-,6.8) or without (6.1 per 100,000, 95% CI 4.8,7.4) Medicaid coverage of medically necessary abortion.
DISCUSSION
State Medicaid coverage of medically necessary abortion was associated with an average 16% decreased risk of severe maternal morbidity. Women residing in states with state-funded Medicaid coverage of medically necessary abortion had lower risks of severe maternal morbidity during pregnancy-related hospitalizations compared with women who resided in states without such Medicaid coverage. This was true regardless of if the hospitalization itself was paid for by Medicaid or private insurance. Such Medicaid coverage was not associated with risk of in-hospital maternal mortality.
There are several potential explanations for these findings. Medicaid coverage of medically necessary abortion may reduce the number of medically risky pregnancies, and therefore reduce the risk of severe maternal morbidity and mortality during pregnancy-related hospitalizations. Interestingly, state Medicaid coverage of medically necessary abortion was associated with similar reductions in the risk of severe maternal morbidity among both Medicaid-paid and private insurance-paid hospitalizations. This finding, while surprising at first blush, is consistent with a sizable body of health economics research suggesting that policy adoption in one payer may have spillover effects among other payers.20–22 One likely mechanism for such spillover effects is that Medicaid payment policies may drive practice pattern norms, and physicians are likely to provide similar care to all patients regardless of payer.23 It follows that coverage of medically necessary abortion in Medicaid may affect provision of abortion services among women with both Medicaid and private insurance. This possible interpretation of our findings should be read with caution, as our study was not intended to explicitly test for spillover effects.
An alternate explanation for our findings is that there is an unmeasured population-level confounder or confounders causing lower severe maternal morbidity rates and is associated with state Medicaid coverage of medically necessary abortion. The fact that we observed reduced risk of severe maternal morbidity among all hospitalizations, regardless of payer, might suggest that there are other state-level factors associated with Medicaid coverage of medically necessary abortion that also lead to reduced severe maternal morbidity. One such factor might be geographic region. Notably, no states in the southern U.S. cover medically necessary abortion via Medicaid, and to the extent that geographic region is causally associated with different cultural and medical risk factors for severe maternal morbidity, this might explain our results. A second factor might be that state Medicaid coverage of medically necessary abortion is correlated with other state-level policies that facilitate access to induced abortion and might be causally associated with reduced risk of severe maternal morbidity. Specifically, we note that of the 17 states that provided Medicaid coverage of medically necessary abortion, only 4 had any policy to impose restrictions on access to abortion services (known as Targeted Regulation of Abortion Providers, or TRAP, laws).24 This latter explanation is consistent with our hypothesis that increased access to medically necessary abortion would be associated with reduced risk of severe maternal morbidity and mortality.
However, there is also reason to suspect that state Medicaid coverage of medically necessary abortion is independently associated with reduced risk of severe maternal morbidity. In some states, coverage of medically necessary abortion was implemented via legislative or regulatory mechanisms, and in others, court decisions required coverage of medically necessary abortion in Medicaid programs. It is not immediately apparent what unmeasured state-level factor would be simultaneously associated with various legislative and court decisions and is causally related to severe maternal morbidity.
It is unlikely that our results are explained by an over-representation of lower-risk pregnancies in states with Medicaid coverage of medically necessary abortion. On the contrary, in our study, pregnancy-related hospitalizations that occurred in states with Medicaid coverage of medically necessary abortion had populations that were older and more racially diverse, which would be expected to increase rates of adverse maternal outcome.
Given the observed reduction in the risk of severe maternal morbidity, it is surprising that we did not find an association between Medicaid coverage of medically necessary abortion and reduction in in-hospital maternal mortality. Our measure of maternal mortality is limited to in-hospital mortality. The rarity of this outcome might limit our ability to detect small differences in risk by state Medicaid policy status.
This study has limitations. First, this is an observational study and we cannot definitively establish a causal relationship between state Medicaid coverage of medically necessary abortion and outcomes. To address this limitation, we conducted sensitivity analyses to test the robustness of our findings, and our analyses have controlled for observable factors that might confound the relationship between state Medicaid policy status and maternal mortality and severe maternal morbidity. We cannot, however, rule out the possibility of unmeasured confounding. Second, the hospital discharge data we used do not allow us to follow patients over time, or measure prenatal care or antepartum clinical risk factors. The lack of these data limit our ability to draw firm conclusions about the hypothesized mechanism of the association between coverage of medically necessary abortion and severe maternal morbidity. Third, we are unable to determine from hospital discharge data whether women residing in states with Medicaid coverage of medically necessary abortion did in fact have greater use of abortion services. There might be variation in women’s access to abortion services even within the group of states that provide Medicaid coverage of medically necessary abortion, which would make our estimates less precise. Fourth, there is likely to be geographic variation in practices related to coding certain conditions during pregnancy-related hospitalizations; however, we have no reason to expect such variation to be systematically associated with our exposure or outcomes of interest. Strengths of our study include the use of a large, national dataset that provides high external validity, and our ability to draw comparisons in outcomes both by state and by the payer for the hospitalizations.
Our findings are consistent with the hypothesis that Medicaid coverage of medically necessary abortion does not harm maternal health and is associated with reduced risk of severe maternal morbidity during pregnancy-related hospitalizations. Such evidence is important as legislators and the courts consider whether state abortion restriction policies are needed to protect maternal health,25 and as federal policymakers consider the health implications of the Hyde amendment.26
Acknowledgments
Supported in part by the Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) Program under Award Number K12HD043441 (Dr. Jarlenski). Dr. Hutcheon is the recipient of New Investigator Awards from the Canadian Institutes of Health Research and the Michael Smith Foundation for Health Research.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has indicated that he or she has met the journal’s requirements for authorship.
References
- 1.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120(5):1029–1036. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 2.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125(1):5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 3.Papiernik E, Zeitlin J, Delmas D, et al. Termination of pregnancy among very preterm births and its impact on very preterm mortality: results from ten European population-based cohorts in the MOSAIC study. BJOG. 2008;115(3):361–368. doi: 10.1111/j.1471-0528.2007.01611.x. [DOI] [PubMed] [Google Scholar]
- 4.Moaddab A, Dildy GA, Brown HL, et al. Health Care Disparity and State-Specific Pregnancy-Related Mortality in the United States, 2005–2014. Obstet Gynecol. 2016;128(4):869–875. doi: 10.1097/AOG.0000000000001628. [DOI] [PubMed] [Google Scholar]
- 5.Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography. 2015;52(1):83–111. doi: 10.1007/s13524-014-0359-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raymond EG, Grimes DA. The comparative safety of legal induced abortion and childbirth in the United States. Obstet Gynecol. 2012;119(2 Pt 1):215–219. doi: 10.1097/AOG.0b013e31823fe923. [DOI] [PubMed] [Google Scholar]
- 7.Markus AR, Andres E, West KD, Garro N, Pellegrini C. Medicaid covered births, 2008 through 2010, in the context of the implementation of health reform. Womens Health Issues. 2013;23(5):e273–280. doi: 10.1016/j.whi.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Guttmacher Instittue. [Accessed May 21, 2016];State Funding of Abortion Under Mediciad. 2016 https://www.guttmacher.org/sites/default/files/state_policy_overview_files/spib_sfam.pdf.
- 9.Healthcare Cost and Utilization Project. [Accessed July 20, 2015];Overview of the National (Nationwide) Inpatient Sample (NIS) 2015 https://www.hcup-us.ahrq.gov/nisoverview.jsp.
- 10.Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12(4):469–477. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 11.Ghaji N, Boulet SL, Tepper N, Hooper WC. Trends in venous thromboembolism among pregnancy-related hospitalizations, United States, 1994–2009. Am J Obstet Gynecol. 2013;209(5):433, e431–438. doi: 10.1016/j.ajog.2013.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuklina EV, Callaghan WM. Cardiomyopathy and other myocardial disorders among hospitalizations for pregnancy in the United States: 2004–2006. Obstet Gynecol. 2010;115(1):93–100. doi: 10.1097/AOG.0b013e3181c4ee8c. [DOI] [PubMed] [Google Scholar]
- 13.Hutcheon JA, Bodnar LM, Simhan HN. Medicaid pregnancy termination funding and racial disparities in congenital anomaly-related infant deaths. Obstet Gynecol. 2015;125(1):163–169. doi: 10.1097/AOG.0000000000000583. [DOI] [PubMed] [Google Scholar]
- 14.Doe v. Bolton, (U.S. Supreme Court 1973).
- 15.Centers for Disease Control and Prevention. [Accessed May 21, 2016];Severe Maternal Morbidity in the United States. 2015 http://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html.
- 16.American College of Obstetricians Gynecologists atSfM-FM. Severe maternal morbidity: screening and review. Am J Obstet Gynecol. 2016;215(3):B17–22. doi: 10.1016/j.ajog.2016.07.050. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease C, Prevention. Vital signs: state-specific obesity prevalence among adults --- United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(30):951–955. [PubMed] [Google Scholar]
- 18.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–835. doi: 10.1097/EDE.0b013e3181577511. [DOI] [PubMed] [Google Scholar]
- 19.Kids Count Data Center. [Accessed January 18, 2017];Indicators: Total Births. 2017 http://datacenter.kidscount.org/data/tables/6052-total-births#detailed/1/any/false/869,36,868,867,133/any/12720.
- 20.Wang YR, Pauly MV, Lin YA. Impact of Maine’s Medicaid drug formulary change on non-Medicaid markets: spillover effects of a restrictive drug formulary. Am J Manag Care. 2003;9(10):686–696. [PubMed] [Google Scholar]
- 21.Dubay L, Kenney G. Expanding public health insurance to parents: effects on children’s coverage under Medicaid. Health Serv Res. 2003;38(5):1283–1301. doi: 10.1111/1475-6773.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baicker K, Robbins JA. MEDICARE PAYMENTS AND SYSTEM-LEVEL HEALTH-CARE USE: The Spillover Effects of Medicare Managed Care. Am J Health Econ. 2015;1(4):399–431. doi: 10.1162/AJHE_a_00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glied S, Zivin JG. How do doctors behave when some (but not all) of their patients are in managed care? J Health Econ. 2002;21(2):337–353. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- 24.Guttmacher Institute. [Accessed October 20, 2016];Targeted Regulation of Abortion Providers. 2016 https://www.guttmacher.org/state-policy/explore/targeted-regulation-abortion-providers.
- 25.Charo RA. Whole Women’s Victory - or Not? N Engl J Med. 2016;375(9):809–811. doi: 10.1056/NEJMp1609167. [DOI] [PubMed] [Google Scholar]
- 26.Salganicoff ARC, Sobel L. [Accessed October 25 2016, 2016];The Hyde Amendment and Coverage for Abortion Services. 2016 http://kff.org/womens-health-policy/perspective/the-hyde-amendment-and-coverage-for-abortion-services/