Abstract
A highly sensitive second-generation hepatitis C virus (HCV) core antigen assay has recently been developed. We compared viral disappearance and first-phase kinetics between commercially available core antigen (Ag) assays, Lumipulse Ortho HCV Ag (Lumipulse-Ag), and a quantitative HCV RNA PCR assay, Cobas Amplicor HCV Monitor test, version 2 (Amplicor M), to estimate the predictive benefit of a sustained viral response (SVR) and non-SVR in 44 genotype 1b patients treated with interferon (IFN) and ribavirin. HCV core Ag negativity could predict SVR on day 1 (sensitivity = 100%, specificity = 85.0%, accuracy = 86.4%), whereas RNA negativity could predict SVR on day 7 (sensitivity = 100%, specificity = 87.2%, accuracy = 88.6%). None of the patients who had detectable serum core Ag or RNA on day 14 achieved SVR (specificity = 100%). The predictive accuracy on day 14 was higher by RNA negativity (93.2%) than that by core Ag negativity (75.0%). The combined predictive criterion of both viral load decline during the first 24 h and basal viral load was also predictive for SVR; the sensitivities of Lumipulse-Ag and Amplicor-M were 45.5 and 47.6%, respectively, and the specificity was 100%. Amplicor-M had better predictive accuracy than Lumipulse-Ag in 2-week disappearance tests because it had better sensitivity. On the other hand, estimates of kinetic parameters were similar regardless of the detection method. Although the correlations between Lumipulse-Ag and Amplicor-M were good both before and 24 h after IFN administration, HCV core Ag seemed to be relatively lower 24 h after IFN administration than before administration. Lumipulse-Ag seems to be useful for detecting the HCV concentration during IFN therapy; however, we still need to understand the characteristics of the assay.
Hepatitis C virus (HCV) infection causes a slowly progressive disease which can lead to chronic hepatitis, liver cirrhosis, and hepatocellular carcinoma (28, 30). Successful interferon (IFN) therapy for HCV leads to persistently undetectable serum viral levels and histological improvement (9, 11) and improves the survival of chronic hepatitis C patients by preventing liver-related deaths (36). A meta-analysis study including data from randomized trials showed that retreatment of nonresponders with a combination of IFN-α2b and ribavirin (RBV) for 24 weeks was associated with only 14% sustained virological response (SVR) in genotype 1-infected patients (4). When a combination of pegylated interferon (IFN) and RBV was used as retreatment for 48 weeks, a 46% SVR rate was reached; however, patients infected with genotype 1 still had a limited chance of achieving SVR (12).
Studies aimed at understanding the predictive value of SVR and non-SVR in the absence or presence of serum RNA during IFN therapy within 2 days (32), 1 week (18), 2 weeks (17), 1 month (3, 6, 13, 15, 29, 39), or 3 months (23) have been reported. The biphasic or triphasic initial decline in the level of serum HCV RNA after IFN therapy has also been characterized and analyzed mathematically (8, 14, 21, 27, 40). The exponential and dose-dependent first phase is a 0.5- to 2.5-log decline in the serum virus concentration within 24 h. The first-phase response is attributed to IFN blocking viral production or release and a rapid free virion clearance rate. A slower second-phase decline in serum viral levels is observed after the first phase and may reflect the rate of clearance of infected hepatocytes and the effectiveness of IFN in blocking viral production.
Viral kinetic studies have been analyzed predominantly by the HCV RNA assay using the PCR method. Although the PCR assay is very sensitive in detecting the serum HCV RNA, the results sometimes have problems of specificity and precision, and blind comparisons have significant error rates (37). Methods for detecting viral antigens (Ag) were developed by applying a monoclonal antibody to the HCV core Ag (19, 33, 35); however, the assays have been insufficient for clinical application because of their low sensitivity and the requirement for complicated specimen pretreatment. An accurate and specific new HCV core Ag detection assay system (total HCV core Ag assay) (2) has recently been developed and is commercially available in European countries (trak-C assay) (7, 20, 24, 25, 31); it has a lower detection level limit of 1.5 pg/ml, which is equivalent to 20 KIU/ml. More recently, Lumipulse Ortho HCV Ag (Lumipulse-Ag), with a lower detection level limit of 50 fmol/liter (equivalent to 1.0 pg/ml), was developed in Japan (1, 34). The dynamic range of Lumipulse-Ag (from 50 to 50,000 fmol/liter, equivalent to 1.0 to 1,000 pg/ml) is broader than that of the trak-C assay (1.0 to 100 pg/ml) and the PCR quantitative assay, Cobas Amplicor HCV Monitor test (Amplicor-M). Because HCV core Ag is stable, no extra precautions are needed for storing samples. An easy, simple, low-cost new HCV core Ag detecting system seems to be useful for assessing and monitoring IFN treatment of HCV. Only a few predictive studies for IFN-RBV combination therapy (24, 25) and no studies of first-phase viral kinetics have been established for the HCV core Ag assay so far. In the present study, we compared the viral disappearance rates and kinetic data between Lumipulse-Ag and Amplicor-M to estimate the predictive benefit of SVR and non-SVR with IFN-RBV combination therapy.
MATERIALS AND METHODS
Patients and treatment regimen.
Adult patients with consecutive genotype 1b HCV-RNA positive, abnormal alanine aminotransferase (ALT) levels and histologically consistent chronic hepatitis C were eligible for this study. All patients gave written informed consent before treatment, and the protocol was approved by the ethics committee of each participating center. Patients with cirrhosis or patients coinfected with HBV were excluded. All patients received 6 MU of IFN-α2b every day for 2 weeks and then thrice weekly for 22 weeks. RBV was given orally for a total dose of 600 mg (body weight, <60 kg) or 800 mg (body weight, ≥60 kg) per day for 24 weeks. An SVR was defined as a normal serum ALT level and undetectable serum HCV RNA and HCV core Ag 24 weeks after discontinuation of therapy. A non-SVR was defined as the response in patients who did not show SVR.
Determination of serum HCV RNA, HCV genotypes, and HCV core Ag.
The HCV genotype was determined using a commercially available probe assay which can distinguish genotypes 1a, 1b, 2a, 2b, and 3a of HCV (Monitor Genotype; Roche Diagnostics, Tokyo, Japan). Serum HCV RNA levels were determined by a Cobas Amplicor HCV Monitor test, version 2 (Amplicor-M) (Roche Diagnostics). For quantification of serum HCV core Ag, Lumipulse Ortho HCV Ag (Lumipulse-Ag) (Ortho Clinical Diagnostics, Tokyo, Japan) was used as specified by the manufacturer. The lower detection limit for each assay kit was 0.5 KIU/ml in Amplicor-M and50 fmol/liter in Lumipulse-Ag.
Viral kinetic parameters.
Viral load at baseline (V0) and on day 1 (V1) and the viral load decline 24 h after IFN administration (ɛ) were calculated using HCV core Ag and HCV RNA data by nonlinear fitting as described elsewhere (27). Whenever HCV core Ag and HCV RNA levels were below the sensitivity of each assay, a value of 50 fmol/liter and 0.5 KIU/ml were arbitrarily used for calculation because those were the lower limit for each assay.
Statistical analysis.
The statistical significance of differences between groups was analyzed using the Mann-Whitney U-test, Fisher's exact test, and the Wilcoxon signed-rank test. Sensitivity was calculated as the ratio of the number of patients who gave SVR to the number of patients predicted to give SVR. Specificity was defined as the ratio of the number of patients who became non-SVR to the number of patients predicted to give non-SVR by our criteria. The positive predictive value (PPV) was defined as the proportion of patients with the factor who responded to treatment. The negative predictive value (NPV) was defined as the proportion of patients without the factor who did not respond to treatment. Accuracy was defined as the ratio of the number of patients correctly predicted to be SVR or non-SVR to the total number of patients.
RESULTS
Patient characteristics.
Forty-nine genotype 1b-infected patients were enrolled, of whom 44 completed the study as per protocol. The demographic characteristics of the patients are shown in Table 1. There was no statistical significance in the 6-month IFN-RBV combination therapy between SVR and non-SVR patients with respect to age, gender, body weight, baseline ALT levels, and platelet counts. We also observed no significance with respect to baseline viral loads detected by HCV core Ag or HCV RNA (Table 1).
TABLE 1.
Baseline clinical and virological characteristics of the comparison of SVR and non-SVR
| Characteristic | SVR (n = 10) | Non-SVR (n = 34) | P |
|---|---|---|---|
| Age (yr)a | 60.5 (29-66) | 60.0 (21-70) | 1.000 |
| Gender (female/male)b | 4/6 | 10/24 | 0.701 |
| Body weight (kg)a | 61.85 (47.0-75.5) | 66.35 (40.4-86.4) | 0.712 |
| ALT (IU/liter)a | 74.5 (17-402) | 75.5 (28-206) | 0.906 |
| Platelet (×10/liter)a | 16.95 (11.6-25.3) | 14.75 (10.1-28.7) | 0.114 |
| Liver histology | |||
| Activity (A0/A1/A2/A3) | 1/1/8/0 | 2/11/21/0 | 0.350 |
| Fibrosis (F0/F1/F2/F3) | 1/3/6/0 | 0/9/19/6 | 0.132 |
| HCV RNA (kIU/ml)a | 290 (90.1-4,100) | 660 (81-40,000) | 0.130 |
| HCV core Ag (fmol/liter)a | 4,800 (207-16,829) | 6,154 (726.2-50,000) | 0.245 |
Values are expressed as medians (range); groups were compared by the Mann-Whitney U-test except for gender.
Fisher's exact test.
Disappearance of serum HCV core Ag or HCV RNA during therapy.
There were 10 SVR patients (22.7%) who remained HCV RNA negative and HCV core Ag negative throughout the follow-up period and had sustained normalization of serum ALT levels. Four patients were HCV core Ag negative on day 1, whereas no patients were negative for HCV RNA on day 1. All patients (four of four) who were negative for HCV core Ag on day 1 achieved SVR (sensitivity = 100%, specificity = 85.0%, accuracy = 86.4%) (Table 2). None of the patients achieved negative results for HCV RNA by Amplicor-M on day 1, while five patients were HCV RNA negative on day 7; all patients (five of five) who were negative for HCV RNA on day 7 achieved SVR (sensitivity = 100%, specificity = 87.2%, accuracy = 88.6%). The specificity of Lumipulse-Ag increased on day 7 and reached 100% on day 14. The specificity was 77.3% on day 1 and also reached 100% on day 14 by Amplicor-M. None of the patients who had detectable serum core Ag or RNA on day 14 achieved SVR (specificity = 100%). All 10 SVR patients were both core Ag and RNA negative on day 14 (PPV = 100%). Core Ag and RNA negativity on day 14 could predict 23 and 31 non-SVR patients out of 34 (NPV = 67.6 and 91.2%, respectively) (Tables 2 and 3).
TABLE 2.
Treatment results and disappearance of serum viral load
| Ag or RNA and time | Presence of Ag or RNA | No. giving SVR (n = 10) | No. giving non-SVR (n = 34) | Fisher exact P-value |
|---|---|---|---|---|
| HCV core Ag | ||||
| Day 1 | − | 4 | 0 | 0.00150 |
| + | 6 | 34 | ||
| Day 7 | − | 8 | 6 | 0.000551 |
| + | 2 | 28 | ||
| Day 14 | − | 10 | 11 | 0.000141 |
| + | 0 | 23 | ||
| HCV RNA | ||||
| Day 1 | − | 0 | 0 | NAa |
| + | 10 | 34 | ||
| Day 7 | − | 5 | 0 | 0.000232 |
| + | 5 | 34 | ||
| Day 14 | − | 10 | 3 | <0.0001 |
| + | 0 | 31 |
P value was not calculable because none of the patients had negative HCV RNA on day 1.
TABLE 3.
Viremia at different time points after IFN therapy as a predictor of treatment response
| Negativity and time | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|
| HCV core Ag | |||||
| Day 1 | 100 | 85.0 | 40.0 | 100 | 86.4 |
| Day 7 | 57.1 | 93.3 | 80.0 | 82.4 | 81.8 |
| Day 14 | 47.6 | 100 | 100 | 67.6 | 75.0 |
| HCV RNA | |||||
| Day 1 | 0 | 77.3 | 0 | 100 | 77.3 |
| Day 7 | 100 | 87.2 | 50.0 | 100a | 88.6 |
| Day 14 | 76.9 | 100 | 100 | 91.2a | 93.2a |
P < 0.05.
Viral kinetics assay.
We analyzed the decline in the viral load within the initial 24 h (ɛ) and found that a >90% decline (1.00-log decline) in core Ag and an 87% decline (0.89 log decline) in RNA levels gave a specificity of 100% and sensitivities of 35.7 and 33.3%, respectively. Thus, failure to drop 1.00 log in core Ag and 0.89 log in RNA predict non-SVR. The thresholds of the baseline viral load (V0), which gave 100% specificity for the prediction of SVR in Lumipulse-Ag and Amplicor-M, were 17,000 fmol/liter and 5,000 kIU/ml, respectively. A total of 10 of 37 with Lumipulse-Ag and 10 of 36 with Amplicor-M achieved SVR under those criteria (the sensitivities were 27.0 and 27.8%, respectively). When we assessed viral load after 24 h (V1), the thresholds that gave 100% specificity for the prediction of non-SVR were 850 fmol/liter with Lumipulse-Ag and 120 kIU/ml with Amplicor-M, and the sensitivities were 34.5 and 38.5%, respectively. The viral-load decline during the initial 24 h of IFN treatment (ɛ), basal viral loads (V0), and viral loads on day 1 (V1) detected by Lumipulse-Ag and Amplicor-M and the correlation between the three values were investigated. When we combined the criteria of both ɛ (1.00-log decline in the core Ag assay and 0.89-log decline in the RNA assay) and V0 (17,000 fmol/liter in Lumipulse-Ag and 5,000 kIU/ml in Amplicor-M), the sensitivities with Lumipulse-Ag and Amplicor-M were 45.5% (accuracy = 72.7%) and 47.6% (accuracy = 75.0%), respectively, while the specificities were both 100%. The predictive efficiencies did not improve when we assessed the data in combination with ɛ and V1 instead of ɛ and V0 with both Lumipulse-Ag and Amplicor-M.
Correlation between HCV core Ag and HCV RNA before and after IFN administration.
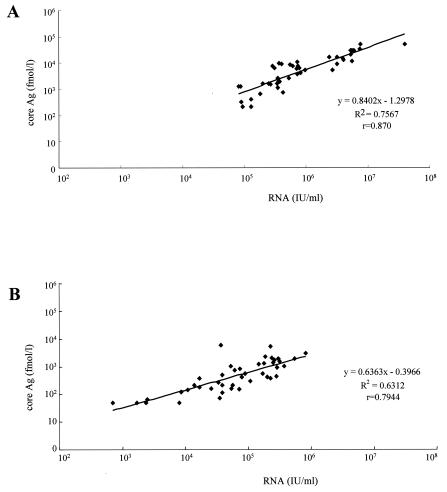
We found a good correlation between HCV core Ag and HCV RNA levels not only for basal levels but also for those on day 1 (r = 0.870, P < 0.05 and r = 0.794, P < 0.05, respectively). However, we found that the correlation coefficients evaluated before and after IFN administration were different (Fig. 1). HCV core Ag levels were relatively higher in the basal viral loads than 1 day after IFN therapy compared with the levels of HCV RNA.
FIG. 1.
Correlation between HCV core Ag and HCV RNA before (A) and 24 h after (B) therapy. Correlations were good both before and 24 h after therapy (r = 0.870 and 0.794, respectively), although the coefficient was smaller 24 h after therapy than before therapy (P < 0.05). The HCV RNA level was relatively higher than that of core Ag 24 h after therapy.
DISCUSSION
It is better to differentiate between non-SVR and SVR patients as fast as possible during IFN-RBV combination therapy because this therapy is expensive and is associated with several severe adverse reactions. If we can distinguish SVR from non-SVR patients on the basis of viral kinetics in the early stages, we can avoid unnecessary IFN therapy. Early clearance of viremia (3, 6, 13, 15, 17, 18, 29, 32, 39) has been reported to be a strong predictor of SVR, using multivariate analysis of IFN monotherapy. Several predictions of therapeutic response on the basis of early viral clearance have also been reported for IFN-RBV combination therapy. The sensitivity and specificity were said to estimate the predictive benefit in these reports; however, they seemed to depend on the procedure of the HCV detection assay.
We found 100% sensitivity in the prediction of SVR by the HCV RNA assay after 1 week of IFN-RBV combination therapy and 100% sensitivity by the HCV core Ag assay on day 1. The different time points of HCV disappearance between Lumipulse-Ag and Amplicor-M could be due mainly to the different sensitivities of the assay systems. Amplicor-M has higher sensitivity for HCV detection, resulting in an HCV-positive result on day 1 after initial IFN administration in some SVR patients given the 6-month combination therapy. Since the sensitivity of Lumipulse-Ag was lower than that of Amplicor-M, this system could precisely predict SVR earlier than could the use of HCV RNA measurements.
The response to IFN-RBV combination therapy is so much better than the response to IFN monotherapy that some SVR still existed in patients in whom the HCV RNA level was positive 4 weeks after the start of therapy (26); however, early viral clearance was generally associated with SVR in IFN-RBV combination therapy (10). Brouwer et al. reported that the disappearance of serum HCV RNA at week 4 was highly predictive of non-SVR (specificity = 100%) and that SVR was achieved in 46% of patients in whom HCV RNA was cleared by week 4 (sensitivity = 46%) of the 6-month combination therapy (3). In the present study, we also found that the specificity was 100% at week 2 with both Lumipulse-Ag and Amplicor-M and the sensitivities were 47.6 and 76.9%, respectively. Because of its higher sensitivity, Amplicor-M could detect more non-SVR on day 14 than could Lumipulse-Ag.
On the other hand, the decrease in viral load within 24 h of the initial IFN injection has been used for the prediction of SVR in combination therapy. Jessner et al. reported that the reduction in viral load within 24 h following a single injection of IFN could be a good predictor of non-SVR in 6-month combination therapy (16). They administered an initial 10 MU followed by a secondary 5 MU of IFN 1 week later. They achieved 100% specificity for non-SVR prediction in patients who did not show more than a 70% reduction in viral load within 24 h of receiving the initial 10 MU of IFN, with 61% sensitivity; 83% sensitivity was obtained after the later 5-MU administration. We found that none of the patients gave SVR in whom the viral load declined less than 90% (1.00-log decline) of the initial load within 24 h by the core Ag assay, whereas the viral load declined less than 87% (0.89-log decline) by the RNA assay, with 35.7 and 33.3% sensitivity, respectively. The sensitivity of predicting SVR in our data was calculated to be lower than that in Jessner's report. This difference may be due to the patient distribution. We investigated 44 genotype 1b-infected patients, while Jessner et al. included 29 genotype 1a- and 1b-infected patients. Although changes in viral load seem to be important for therapeutic prediction, further study is required before we can understand the predictive benefit of a viral decline within 24 h of the initial injection.
Furthermore, the combination of viral decline within 24 h (ɛ) and the viral load on day 1 (V1) was reported to have a good predictive value (22). We also obtained better sensitivity along with 100% specificity when using this combination of criteria (sensitivities were 45.5% with the core Ag assay and 47.6% with the RNA assay) than using single criteria. These authors reported better prediction when using a combination of ɛ and V1 than using ɛ and V0 in studies of IFN monotherapy. In the present study, we observed that sensitivity and accuracy did not improve with the combination of ɛ and V1 compared to ɛ and V0 in IFN-RBV combination therapy. It seemed that the prediction of the criteria would be different according to the combination with RBV.
The predictive efficiency of viral kinetics for IFN therapy has been achieved mainly by using the RNA PCR assay. Application of a commercially available quantification system for determination of HCV RNA levels may be limited by underestimation of highly viremic sera as described for the Amplicor-M (5), although a Cobas TaqMan HCV assay, which has an increased upper cutoff limit, is being developed. The upper limit of the Cobas Amplicor HCV test version 2 is 850 kIU/ml, which is not always enough to assess the viral levels before IFN treatment, especially in genotype 1-infected patients. In our series, 16 of 44 patients had viral loads above 850 kIU/ml, which required dilution of the sera. In contrast, the dynamic range of Lumipulse-Ag is broader than that of Amplicor-M, and all the samples in our series could be assayed without dilution.
When we compared core Ag and RNA PCR assays in first-phase viral kinetics for predicting SVR and non-SVR, none of the patients achieved SVR with a 90% (1.00 log) decline in core Ag levels, which was similar to the results of PCR. The sensitivities were also similar in the two detection systems in the criteria giving 100% specificity. Amplicor-M, however, achieved a better predictive accuracy than did the core Ag assay when evaluated 2 weeks after the start of therapy because this assay is more sensitive. On the other hand, the cost of Lumipulse-Ag is 73% lower than that of Amplicor-M. Because of its stability and low cost, along with the advantages described above, the HCV core Ag assay system seems to have an advantage in detecting HCV concentrations in large clinical trials in many countries including developing countries, but we need to understand the characteristics of these assays to select the assay system suitable for the aim of each study. The Ag assay may have utility, but further studies are needed to determine when therapy can be discontinued based on a failure to observe a drop in Ag levels. To our knowledge, this is the first study in which patients with chronic HCV infection were monitored by HCV core Ag in the first phase of IFN-RBV therapy.
Another novel finding of this study was the different HCV RNA core Ag ratio before and 24 h after IFN therapy. Although the correlation between the levels with the core Ag assay and the RNA PCR assay was good both in basal viral load (V0) and viral load 24 h after IFN administration (V1), the correlation coefficients were different (Fig. 1). The results of the core Ag assay were relatively lower for V1 than for V0. An exponential first-phase viral decline, which was attributed to the direct effects of IFN in blocking HCV production or release and very rapid free virion clearance based on mathematical modeling (21, 27), began within 24 h of IFN administration. We had speculated that the serum core Ag level might be greater in V1 than in V0 because destroyed HCV particles without RNA would appear in the serum. However, a different result was obtained. Although the exact reason was unclear, these findings might be valuable in our understanding of the mechanism of rapid viral decline within 24 h of IFN administration. Further precise determination of first-phase viral kinetics by both assay systems might clarify further the mechanisms of the antiviral effects of IFNs.
Acknowledgments
We are grateful to the participants in the Keio Study Group on Treatment of Chronic Hepatitis C, who contributed to the database used for the present report: S. Tanaka, National Tokyo Medical Center, Tokyo; J. Nishida, Tokyo Dental Collage Ichikawa General Hospital, Chiba; N. Tsukada, Saiseikai Central Hospital, Tokyo; T. Yoshida, Saitama Social Insurance Hospital, Saitama; K. Kashiwazaki, Kyosai Tachikawa Hospital, Tokyo; and H. Yoshida, Eiju General Hospital, Tokyo.
REFERENCES
- 1.Aoyagi, K., C. Ohue, K. Iida, T. Kimura, E. Tanaka, K. Kiyosawa, and S. Yagi. 1999. Development of a simple and highly sensitive enzyme immunoassay for hepatitis C virus core antigen. J. Clin. Microbiol. 37:1802-1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouvier-Alias, M., K. Patel, H. Dahari, S. Beaucourt, P. Larderie, L. Blatt, C. Hezode, G. Picchio, D. Dhumeaux, A. U. Neumann, J. G. McHutchison, and J. M. Pawlotsky. 2002. Clinical utility of total HCV core antigen quantification: a new indirect marker of HCV replication. Hepatology 36:211-218. [DOI] [PubMed] [Google Scholar]
- 3.Brouwer, J. T., B. E. Hansen, H. G. Niesters, and S. W. Schalm. 1999. Early prediction of response in interferon monotherapy and in interferon-ribavirin combination therapy for chronic hepatitis C: HCV RNA at 4 weeks versus ALT. J. Hepatol. 30:192-198. [DOI] [PubMed] [Google Scholar]
- 4.Cheng, S. J., P. A. Bonis, J. Lau, N. Q. Pham, and J. B. Wong. 2001. Interferon and ribavirin for patients with chronic hepatitis C who did not respond to previous interferon therapy: a meta-analysis of controlled and uncontrolled trials. Hepatology 33:231-240. [DOI] [PubMed] [Google Scholar]
- 5.Choo, Q. L., K. H. Richman, J. H. Han, K. Berger, C. Lee, C. Dong, C. Gallegos, D. Coit, R. Medina-Selby, P. J. Barr, et al. 1991. Genetic organization and diversity of the hepatitis C virus. Proc. Natl. Acad. Sci. USA 88:2451-2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Civeira, M. P., and J. Prieto. 1999. Early predictors of response to treatment in patients with chronic hepatitis C. J. Hepatol. 31(Suppl. 1):237-243. [DOI] [PubMed] [Google Scholar]
- 7.Cividini, A., A. Cerino, A. Muzzi, M. Furione, C. Rebucci, L. Segagni, M. Gatti, V. Barnaba, and M. U. Mondelli. 2003. Kinetics and significance of serum hepatitis C virus core antigen in patients with acute hepatitis C. J. Clin. Microbiol. 41:2144-2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cotler, S. J., J. E. Layden, A. U. Neumann, and D. M. Jensen. 2003. First phase hepatitis C viral kinetics in previous nonresponders patients. J. Viral Hepat. 10:43-49. [DOI] [PubMed] [Google Scholar]
- 9.Davis, G. L., L. A. Balart, E. R. Schiff, K. Lindsay, H. C. Bodenheimer, Jr., R. P. Perrillo, W. Carey, I. M. Jacobson, J. Payne, J. L. Dienstag, et al. for the Hepatitis Interventional Therapy Group. 1989. Treatment of chronic hepatitis C with recombinant interferon alfa. A multicenter randomized, controlled trial. N. Engl. J. Med. 321:1501-1506. [DOI] [PubMed] [Google Scholar]
- 10.Davis, G. L., R. Esteban-Mur, V. Rustgi, J. Hoefs, S. C. Gordon, C. Trepo, M. L. Shiffman, S. Zeuzem, A. Craxi, M. H. Ling, and J. Albrecht for the International Hepatitis Interventional Therapy Group. 1998. Interferon alfa-2b alone or in combination with ribavirin for the treatment of relapse of chronic hepatitis C. N. Engl. J. Med. 339:1493-1499. [DOI] [PubMed] [Google Scholar]
- 11.Di Bisceglie, A. M., P. Martin, C. Kassianides, M. Lisker-Melman, L. Murray, J. Waggoner, Z. Goodman, S. M. Banks, and J. H. Hoofnagle. 1989. Recombinant interferon alfa therapy for chronic hepatitis C. A randomized, double-blind, placebo-controlled trial. N. Engl. J. Med. 321:1506-1510. [DOI] [PubMed] [Google Scholar]
- 12.Fried, M. W., M. L. Shiffman, K. R. Reddy, C. Smith, G. Marinos, F. L. Goncales, Jr., D. Haussinger, M. Diago, G. Carosi, D. Dhumeaux, A. Craxi, A. Lin, J. Hoffman, and J. Yu. 2002. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N. Engl. J. Med. 347:975-982. [DOI] [PubMed] [Google Scholar]
- 13.Gavier, B., M. A. Martinez-Gonzalez, J. I. Riezu-Boj, J. J. Lasarte, N. Garcia, M. P. Civeira, and J. Prieto. 1997. Viremia after one month of interferon therapy predicts treatment outcome in patients with chronic hepatitis C. Gastroenterology 113:1647-1653. [DOI] [PubMed] [Google Scholar]
- 14.Herrmann, E., A. U. Neumann, J. M. Schmidt, and S. Zeuzem. 2000. Hepatitis C virus kinetics. Antiviral Ther. 5:85-90. [PubMed] [Google Scholar]
- 15.Izopet, J., J. L. Payen, L. Alric, K. Sandres, J. P. Charlet, J. P. Vinel, M. Duffaut, J. P. Pascal, and J. Puel. 1998. Baseline level and early suppression of serum HCV RNA for predicting sustained complete response to alpha-interferon therapy. J. Med. Virol. 54:86-91. [DOI] [PubMed] [Google Scholar]
- 16.Jessner, W., M. Gschwantler, P. Steindl-Munda, H. Hofer, T. Watkins-Riedel, F. Wrba, C. Mueller, A. Gangl, and P. Ferenci. 2001. Primary interferon resistance and treatment response in chronic hepatitis C infection: a pilot study. Lancet 358:1241-1242. [DOI] [PubMed] [Google Scholar]
- 17.Kagawa, T., K. Hosoi, S. Takashimizu, K. Kawazoe, K. Mochizuki, M. Wasada, N. Nagata, J. Uchiyama, A. Nakano, Y. Nishizaki, N. Watanabe, and S. Matsuzaki. 1998. Comparison of two interferon alfa treatment regimens characterized by an early virological response in patients with chronic hepatitis C. Am. J. Gastroenterol. 93:192-196. [DOI] [PubMed] [Google Scholar]
- 18.Karino, Y., J. Toyota, M. Sugawara, K. Higashino, T. Sato, T. Ohmura, T. Suga, Y. Okuuchi, and T. Matsushima. 1997. Early loss of serum hepatitis C virus RNA can predict a sustained response to interferon therapy in patients with chronic hepatitis C. Am. J. Gastroenterol. 92:61-65. [PubMed] [Google Scholar]
- 19.Kashiwakuma, T., A. Hasegawa, T. Kajita, A. Takata, H. Mori, Y. Ohta, E. Tanaka, K. Kiyosawa, T. Tanaka, S. Tanaka, N. Hattori, and M. Kohara. 1996. Detection of hepatitis C virus specific core protein in serum of patients by a sensitive fluorescence enzyme immunoassay (FEIA). J. Immunol. Methods 190:79-89. [DOI] [PubMed] [Google Scholar]
- 20.Lagging, L. M., C. E. Garcia, J. Westin, R. Wejstal, G. Norkrans, A. P. Dhillon, and M. Lindh. 2002. Comparison of serum hepatitis C virus RNA and core antigen concentrations and determination of whether levels are associated with liver histology or affected by specimen storage time. J. Clin. Microbiol. 40:4224-4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lam, N. P., A. U. Neumann, D. R. Gretch, T. E. Wiley, A. S. Perelson, and T. J. Layden. 1997. Dose-dependent acute clearance of hepatitis C genotype 1 virus with interferon alfa. Hepatology. 26:226-231. [DOI] [PubMed] [Google Scholar]
- 22.Layden, J. E., T. J. Layden, K. R. Reddy, R. S. Levy-Drummer, J. Poulakos, and A. U. Neumann. 2002. First phase viral kinetic parameters as predictors of treatment response and their influence on the second phase viral decline. J. Viral Hepat. 9:340-345. [DOI] [PubMed] [Google Scholar]
- 23.Lee, W. M., K. R. Reddy, M. J. Tong, M. Black, D. J. van Leeuwen, F. B. Hollinger, K. D. Mullen, N. Pimstone, D. Albert, and S. Gardner for The Consensus Interferon Study Group. 1998. Early hepatitis C virus-RNA responses predict interferon treatment outcomes in chronic hepatitis C. Hepatology 28:1411-1415. [DOI] [PubMed] [Google Scholar]
- 24.Lunel, F., P. Veillon, I. Fouchard-Hubert, V. Loustaud-Ratti, A. Abergel, C. Silvain, H. Rifflet, A. Blanchi, X. Causse, Y. Bacq, and C. Payan. 2003. Antiviral effect of ribavirin in early non-responders to interferon monotherapy assessed by kinetics of hepatitis C virus RNA and hepatitis C virus core antigen. J. Hepatol. 39:826-33. [DOI] [PubMed] [Google Scholar]
- 25.Maynard, M., P. Pradat, P. Berthillon, G. Picchio, N. Voirin, M. Martinot, P. Marcellin, and C. Trepo. 2003. Clinical relevance of total HCV core antigen testing for hepatitis C monitoring and for predicting patients' response to therapy. J. Viral Hepat. 10:318-323. [DOI] [PubMed] [Google Scholar]
- 26.McHutchison, J. G., S. C. Gordon, E. R. Schiff, M. L. Shiffman, W. M. Lee, V. K. Rustgi, Z. D. Goodman, M. H. Ling, S. Cort, and J. K. Albrecht for the Hepatitis Interventional Therapy Group. 1998. Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C. N. Engl. J. Med. 339:1485-1492. [DOI] [PubMed] [Google Scholar]
- 27.Neumann, A. U., N. P. Lam, H. Dahari, D. R. Gretch, T. E. Wiley, T. J. Layden, and A. S. Perelson. 1998. Hepatitis C viral dynamics in vivo and the antiviral efficacy of interferon-alpha therapy. Science 282:103-107. [DOI] [PubMed] [Google Scholar]
- 28.Niederau, C., S. Lange, T. Heintges, A. Erhardt, M. Buschkamp, D. Hurter, M. Nawrocki, L. Kruska, F. Hensel, W. Petry, and D. Haussinger. 1998. Prognosis of chronic hepatitis C: results of a large, prospective cohort study. Hepatology 28:1687-1695. [DOI] [PubMed] [Google Scholar]
- 29.Orito, E., M. Mizokami, K. Suzuki, K. Ohba, T. Ohno, M. Mori, K. Hayashi, K. Kato, S. Iino, and J. Y. Lau. 1995. Loss of serum HCV RNA at week 4 of interferon-alpha therapy is associated with more favorable long-term response in patients with chronic hepatitis C. J. Med. Virol. 46:109-115. [DOI] [PubMed] [Google Scholar]
- 30.Poynard, T., P. Bedossa, P. Opolon, and The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. 1997. Natural history of liver fibrosis progression in patients with chronic hepatitis C. Lancet 349:825-232. [DOI] [PubMed] [Google Scholar]
- 31.Rebucci, C., A. Cerino, A. Cividini, L. Timo, M. Furione, and M. U. Mondelli. 2003. Monitoring response to antiviral therapy for patients with chronic hepatitis C virus infection by a core-antigen assay. J. Clin. Microbiol. 41:3881-3884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saito, H., H. Ebinuma, I. Satoh, S. Miyaguchi, S. Tada, N. Iwabuchi, N. Kumagai, K. Tsuchimoto, T. Morizane, and H. Ishii. 2000. Immunological and virological predictors of outcome during interferon-alpha therapy of chronic hepatitis C. J. Viral Hepat. 7:64-74. [DOI] [PubMed] [Google Scholar]
- 33.Takahashi, K., H. Okamoto, S. Kishimoto, E. Munekata, K. Tachibana, Y. Akahane, H. Yoshizawa, and S. Mishiro. 1992. Demonstration of a hepatitis C virus-specific antigen predicted from the putative core gene in the circulation of infected hosts. J. Gen. Virol. 73:667-672. [DOI] [PubMed] [Google Scholar]
- 34.Tanaka, E., K. Kiyosawa, A. Matsumoto, T. Kashiwakuma, A. Hasegawa, H. Mori, O. Yanagihara, and Y. Ohta. 1996. Serum levels of hepatitis C virus core protein in patients with chronic hepatitis C treated with interferon alfa. Hepatology 23:1330-1333. [DOI] [PubMed] [Google Scholar]
- 35.Tanaka, T., J. Y. Lau, M. Mizokami, E. Orito, E. Tanaka, K. Kiyosawa, K. Yasui, Y. Ohta, A. Hasegawa, S. Tanaka, et al. 1995. Simple fluorescent enzyme immunoassay for detection and quantification of hepatitis C viremia. J. Hepatol. 23:742-745. [DOI] [PubMed] [Google Scholar]
- 36.Yoshida, H., Y. Arakawa, M. Sata, S. Nishiguchi, M. Yano, S. Fujiyama, G. Yamada, O. Yokosuka, Y. Shiratori, and M. Omata. 2002. Interferon therapy prolonged life expectancy among chronic hepatitis C patients. Gastroenterology 123:483-491. [DOI] [PubMed] [Google Scholar]
- 37.Zaaijer, H. L., H. T. Cuypers, H. W. Reesink, I. N. Winkel, G. Gerken, and P. N. Lelie. 1993. Reliability of polymerase chain reaction for detection of hepatitis C virus. Lancet 341:722-724. [DOI] [PubMed] [Google Scholar]
- 38.Zanetti, A. R., L. Romano, M. Brunetto, M. Colombo, G. Bellati, and C. Tackney. 2003. Total HCV core antigen assay: a new marker of hepatitis C viremia for monitoring the progress of therapy. J. Med. Virol. 70:27-30. [DOI] [PubMed] [Google Scholar]
- 39.Zeuzem, S., J. H. Lee, A. Franke, B. Ruster, O. Prummer, G. Herrmann, and W. K. Roth. 1998. Quantification of the initial decline of serum hepatitis C virus RNA and response to interferon alfa. Hepatology 27:1149-1156. [DOI] [PubMed] [Google Scholar]
- 40.Zeuzem, S., J. M. Schmidt, J. H. Lee, B. Ruster, and W. K. Roth. 1996. Effect of interferon alfa on the dynamics of hepatitis C virus turnover in vivo. Hepatology 23:366-371. [DOI] [PubMed] [Google Scholar]